Abstract
Non-alcoholic fatty liver disease (NAFLD) represents the most common cause of chronic liver disease in childhood. To date, the “multiple-hit” hypothesis is largely recognized as an explanation of NAFLD pathogenesis and progression. Obesity and features of the metabolic syndrome have been closely linked to NAFLD development. Due to the increased prevalence of obesity worldwide, NAFLD has reached epidemic proportions over time. Given its unfavorable cardiometabolic burden (such as cardiovascular and metabolic consequences), it represents a worrying phenomenon needing a more comprehensive and successful management. Laboratory tests and classical imaging techniques play a pivotal role in NAFLD diagnosis, but novel noninvasive alternative methods to diagnose and monitor NAFLD have been investigated. Currently, lifestyle modifications remain the mainstay treatment, although its efficacy is poor because of the lack of compliance. Pediatric research is focusing on multiple alternative treatments targeting the main pathogenic factors such as insulin-resistance, dyslipidemia, gut-liver axis and microbiota, oxidative stress, and proinflammatory pathways. Results from these studies are promising but larger validation is needed. Innovative therapeutic approaches might add an important piece in the complex knowledge of pediatric NAFLD. We aimed to summarize recent insights into NAFLD diagnosis and treatment in children, with a focus on possible future perspectives in pediatric research.
Keywords: fatty, liver, pediatric, diagnosis, management
Introduction
Non-alcoholic fatty liver disease (NAFLD) represents the most common cause of chronic liver disease in childhood.1,2 It is defined by the histologic evidence of at least 5% of the hepatic steatosis in the absence of other causes of excessive liver fat accumulation, including various conditions ranging from simple hepatic steatosis through non-alcoholic steatohepatitis (NASH), with or without fibrosis, to possibly cirrhosis and end stage liver disease.3
To date, the “multiple-hit” hypothesis (based on interrelations among genetic, epigenetic, and environmental factors) is largely recognized as an explanation of NAFLD pathogenesis and progression.4–8 Interestingly, recent data add novel findings in this complex puzzle. In fact, it has been observed a protective role of both normal maternal pre-pregnancy BMI and long duration of breastfeeding in NAFLD development, suggesting that they might act as NAFLD preventive options.9,10 Similarly, among modifiable risk factors for NAFLD, Mediterranean diet has been observed as both preventive and therapeutic promising approach for NAFLD.11 Obesity and features of the metabolic syndrome have been closely linked to NAFLD development.12 Due to the increased prevalence of obesity worldwide, NAFLD has reached epidemic proportions over time.13 In fact, recent data reported a mean prevalence of NAFLD ranging from 7.6% in general population up to 34.2% in obese children.14
Given its unfavorable cardiometabolic burden and impact on renal function, pediatric NAFLD represents a worrying phenomenon needing a more comprehensive and successful management.15–17 Growing evidence linked the presence of NAFLD in children to cardiovascular and metabolic consequences such as prediabetes, type 2 diabetes, dyslipidemia, and hypertension.13,18
This review aimed to summarize recent insights into NAFLD diagnosis and treatment in children, with a focus on possible future perspectives in pediatric research.
Diagnosis of NAFLD
The first step of NAFLD diagnosis is based on the detection of steatosis through either imaging or liver biopsy and the exclusion other causes of elevated transaminases and hepatic fatty infiltration (e.g., viral infections, autoimmune hepatitis, celiac disease, metabolic liver diseases) by using history and laboratory screening.19,20 To detect this condition, the most common laboratory test is alanine aminotransferase (ALT), although imperfect because of its poor accuracy.16 In fact, a careful evaluation of ALT pediatric thresholds is needed, as major experts also indicated.18,21,22 Additional laboratory tests (AST, AST/ALT ratio, bilirubin, gamma glutamyl transferase (GGT), triglycerides, glucose, insulin, Homeostatic model Assessment of Insulin Resistance) are available for NAFLD assessment.16
New biomarkers
Despite several biomarkers have been linked to the presence of NAFLD, there has also a growing interest regarding newly proposed noninvasive markers.1,23,24
To date, markers of hepatic apoptosis such as cytokeratin 18 (CK-18), soluble Fas, and soluble Fas ligand have shown a significant association in pediatric NAFLD patients.1,23
Recent findings showed the role of the chemerin, a novel adipokine, in predicting both intrahepatic lipid content in obese children and advanced liver steatosis in NAFLD pediatric patients.25,26
Given the pathogenic role of hepatokines in NAFLD, pediatric data demonstrated that both serum fetuin A and fibroblast growth factor (FGF-21) levels were significantly associated with NAFLD.23,27 A high diagnostic value of plasma cathepsin D (CatD) levels in distinguishing children with simple steatosis from those with hepatic inflammation was also reported.28 It has been found that reduced CatD levels showed a better correlation than ALT and CK-18 in NAFLD progression assessment.23,28
In addition, Tumor Necrosis factor-α (TNF-α) might represent a specific noninvasive biomarker predicting the degree of NAFLD progression.29
Pediatric research has been focused on further potential predictors not only of NAFLD (such as adropin, retinol-binding protein 4, and zonulin) but also of NASH (such as plasminogen activator inhibitor 1 and IL-18).23,30–32 Of note, a recent study in obese children demonstrated a significant association between serum IL-18 levels and the degree of hepatic steatosis.33
Imaging
Primary noninvasive tools to detect and measure steatosis are represented by ultrasonography and magnetic resonance imaging.13 Because of its availability, noninvasiveness, and safety, ultrasound imaging is commonly used in clinical practice for the initial evaluation of hepatic steatosis.1,19 Nevertheless, children are often unable to cooperate with awake MRI and sedation or general anesthesia might be required, resulting in an “invasive” technique with potential-related risks. Given that, several strategies to avoid or reduce pediatric sedation – such as sequences with short acquisition time, reducing respiratory motion techniques, and emerging radiological tools – have been developed.34,35
However, the diagnostic gold standard remains liver biopsy, that provides the best overall definition of the disease (degree, severity, and staging).13 Besides the cost and invasiveness of this procedure, its use is further limited in childhood by ethical issues.13,19,36 The ESPGHAN panel indicates the use of liver biopsy to confirm NAFLD diagnosis and in selected cases in NAFLD pediatric patients.37 In fact, children affected by NAFLD can undergo liver biopsy, before or after pharmacological or surgical treatment or in case of suspicion of advanced disease or to exclude other relevant diseases.37 In particular, alternative diagnosis than NAFLD includes a wide spectrum of genetic and metabolic disorders (e.g., inborn errors of metabolism), hepatitis, myopathies, gastrointestinal, nutritional and endocrine diseases, and iatrogenic causes.38
Novel noninvasive techniques for NAFLD assessment
In order to measure hepatic fat, newer magnetic resonance (MR)-based techniques are available. To date, evidence supports MRI, MR Spectroscopy, proton MR spectroscopy (1H-MRS) and, in particular, proton density fat fraction (PDFF) as the most accurate noninvasive imaging tools for NAFLD detection, even in childhood.16,39–41 Of note, PDFF provides fat mapping of the entire liver, by guaranteeing an accurate measurement of the degree of hepatic steatosis in all cases.16,42–44 Given the high cost and limited availability, these methods are at present preferred for research purposes in NAFLD.16
Controlled attenuation parameter (CAP) represents another noninvasive tool useful for NAFLD assessment. It is based on a radiofrequency ultrasound signal incorporated in the transient elastography system (TE) of the FibroScan device.16 It has shown good accuracy in adults NAFLD patients and recent data confirmed these results also in pediatric population.16,45 Considering its noninvasiveness and limited cost, CAP might be a promising tool, but further studies are needed.
Further imaging techniques such as TE and MR elastography are currently used for fibrosis evaluation and differentiation in adults, but results in children, although promising, need to be validated before using in clinical practice.18,46
Several alternative noninvasive methods for diagnosis of liver fibrosis in NAFLD pediatric patients have been proposed.24 Despite various fibrosis scores available in adults (e.g., AST/ALT ratio, AST to platelet ratio index, NAFLD fibrosis score, and fibrosis-4 index), valid alternatives to liver biopsy are still limited.1,23 A pediatric prediction score for steatosis (Pediatric NAFLD score) has been developed, but its accuracy resulted not satisfactory.47,48 Indirect evaluation of NASH in children is still lacking. To date, the “Pediatric predictive NASH model” has been only proposed, with promising validation studies but very limited.49
Recently, it has been proposed a “pediatric NAFLD fibrosis index” –based on age, waist circumference, and triglycerides – as a predictor of liver fibrosis in children.50 In addition, the “Enhanced Liver Fibrosis” test – an algorithm including hyaluronic acid, tissue inhibitor of metalloproteinase 1, and procollagen III N-terminal peptide (P3NP)-represents a screening method for progressive fibrosis with good accuracy but with lack of larger validation studies.51,52 The “Pediatric NAFLD fibrosis score” (based on ALT, GGT, platelet counts, and alkaline phosphatase) has been also developed and seems useful in predicting advanced liver fibrosis, although larger validation is needed.53,54
Of interest, recent promising studies reported novel potential noninvasive approaches in this field by assuming an important role of gut-liver axis perturbations and metabolomics signatures in NAFLD pathogenesis.55–59 In particular, salivary test combined with selected anthropometric parameters might act as useful markers in early identification of obese patients with hepato-metabolic comorbidities.56
Therapeutic approaches in NAFLD
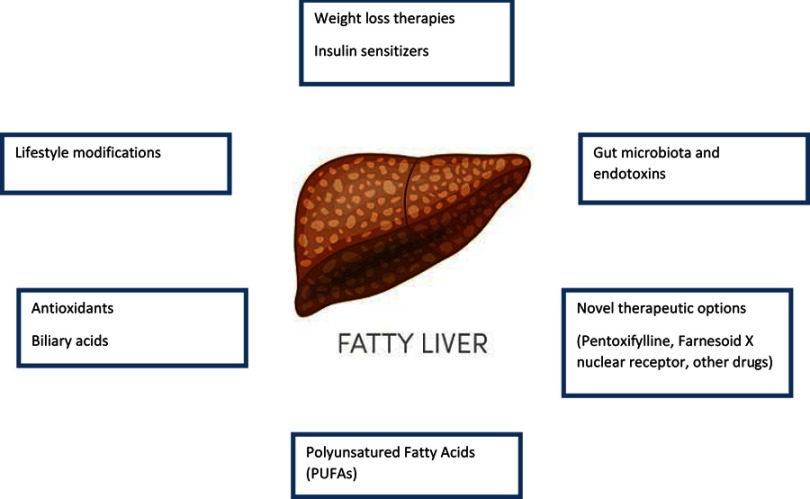
Given the close link between obesity and NAFLD and its cardiometabolic burden, an adequate management is strictly required (Figure 1).
Figure 1.
Available options for pediatric NAFLD treatment.
Abbreviation: NAFLD, non-alcoholic fatty liver disease.
To date, lifestyle modifications represent the mainstay therapy in childhood. No pharmacological treatments are licensed for NAFLD, but several studies are promising.
Lifestyle modifications
Evidence showed a synergistic effect of diet and physical activity in improving both hepatic and extrahepatic insulin sensitivity. Moreover, structured programs of behavior therapy for children with NAFLD showed improvement in insulin-resistance, hepatic fat content, liver enzymes, and in liver disease progression (e.g., grade and stage of hepatic inflammation, fibrosis).60
Due to the difficulty in achieving long-term significant and sustained weight loss through diet and exercise, more effective pharmacological interventions are needed.
Weight loss therapies
Orlistat is a gastrointestinal lipase inhibitor approved from FDA for obese subjects aged >12 years.60,61 It may be poorly tolerated because of its adverse effects of abdominal pain and steatorrhea. However, NICE recommended its use in children <12 years in selected cases such as in the presence of serious comorbidities.62
Studies reported a modest effect of this drug in weight loss, while results on reducing hepatic steatosis are contrasting.60,63 To date, its use as a key pharmacological agent in pediatric NAFLD treatment is very limited.60,62
Bariatric surgery represents an important therapeutic option in morbidly obese adults who failed lifestyle modifications, providing the best long-term resolution of the cardiovascular and metabolic consequences obesity-related.23,60 Recently, ESPGHAN suggested that morbidly obese adolescents with NAFLD might benefit from its use, but the efficacy of this procedure, although promising, needs to be further investigated.64 A recent pediatric study reported the positive effect of laparoscopic sleeve gastrectomy not only in reversing fibrosis but also in improving several cardiometabolic consequences obesity-related.65 Nevertheless, due to the paucity of available data and the potentially serious complications, bariatric surgery is not currently recommended as a specific treatment for pediatric NAFLD patients.18
Insulin sensitizers
On the basis of the close pathogenic relationship between NAFLD and insulin-resistance, insulin sensitizers treatment has been considered for NAFLD management.1,13
Evidence showed a positive effect of metformin in improving steatosis but not hepatic histology or serum ALT levels, although results are conflicting.13,60 The TONIC study, a large multicenter randomized double-blind pediatric trial, reported no significant variations in both serum ALT and hepatic histology in the treated group compared to placebo during a period of 96 weeks.66 Thiazolidinediones – such as pioglitazone and rosiglitazone – represent another class of insulin sensitizers increasing adipocyte storage capacity through peroxisome proliferator-activated receptors (PPARγ) in white adipose tissue.36 Findings from adults demonstrated the positive effect of pioglitazone on improving steatosis and lobular inflammation in NASH patients, suggesting a potential role in influencing the natural history of NAFLD. Despite its promising effect, at present, this class of drugs has not been licensed for pediatric age because of its cardiovascular consequences and risk of bladder cancer.36,60
Liraglutide, a glucagon-like peptide-1 (GLP-1) agonist, may represent a further promising pharmacological option in NAFLD treatment. In fact, recent studies in adults reported a significant improvement of NASH, but these results need to be largely validated. However, this drug is not approved in pediatrics because of its exclusive use by injection.60
Antioxidants and biliary acids
Given the role of the mitochondrial dysfunction and reactive oxygen species damage in the pathogenesis of NAFLD, several studies have investigated the potential use of antioxidants such as vitamin E, cysteamine bitartrate). To date, results are conflicting and little benefit over lifestyle and dietary interventions is reported. The largest study in this area is the TONIC randomized controlled trial, that demonstrated no significant effect in sustained ALT reduction in NAFLD patients treated with vitamin E supplementation but in improving liver histology (mainly expressed as hepatocellular ballooning and NAFLD Activity Score (NAS)) in biopsy-proven NASH patients.67
Cysteamine bitartrate represents another promising target in NAFLD therapy. The Cysteamine Bitartrate Delayed-Release for the Treatment of NAFLD in Children (CyNCh) trial showed that 52 weeks of cysteamine bitartrate delayed-release treatment had no effects on histologic markers of NAFLD but a significant reduction in both serum ALT activity and lobular inflammation compared to placebo.68
Similarly, data regarding the efficacy of ursodeoxycholic acid (UDCA) in pediatric NAFLD are conflicting. UDCA is a well-known bile acid exerting anti-oxidative, anti-apoptotic, cytoprotective, and immuno-modulatory functions. As in adults, pediatric studies demonstrated no clear evidence supporting the use of UDCA both as single or combined (with vitamin E and/or C, with or without lifestyle interventions) in NAFLD treatment.69,70
Gut microbiota and endotoxins
Growing evidence showed the role of gut microbiota in improving the natural history of NAFLD through the influence on hepatic fat deposition and the regulation of the gut-liver axis.13,36
In fact, small gut bacterial overgrowth in NAFLD patients has been linked to the severity of steatosis.1 Moreover, gut microbiota seems to affect several NAFLD risk factors such as insulin-resistance, fat storage, and energy harvesting. Given that, changes in gut microbial ecology using pre and probiotics and anti-lipopolysaccharides may represent a therapeutic option for NAFLD patients not compliant to lifestyle interventions.36,60,71
There are several randomized clinical trials investigating the potential role of probiotic supplementation on liver function. Recent data showed positive outcomes such as reduction in BMI and NAFLD severity and increased circulating levels of GLP-1 and its activated form (aGLP-1) in treated patients with VSL#3 (a mixture of eight probiotic strains).72 Further studies reported significant reduced transaminase levels and lipid parameters in NAFLD patients treated with probiotics.16,60 Particularly, Lactobacillus Rhamnosus GG also showed promising effects in reducing transaminase levels and reducing liver fibrosis in children with NAFLD compared to controls.73
Nobili et al, studied the distribution of intestinal bifidobacteria and lactobacilli in 61 obese, NAFLD, and NASH children and 54 healthy, age-matched controls. In particular, Lactobacillus mucosae resulted significantly higher in obese NAFLD and NASH children, while Bifidobacterium spp. were more abundant in control subjects, suggesting a protective role of these microorganisms against both obesity and NAFLD development.74 The effect of probiotics on NAFLD was also evaluated in a randomized triple-blind trial on 64 obese children with sonographic NAFLD receiving probiotic capsule (containing Lactobacillus acidophilus ATCC B3208, 3 × 10 colony-forming units [CFU]; Bifidobacterium lactis DSMZ 32269, 6 × 10 CFU; Bifidobacterium bifidum ATCC SD6576, 2 × 10 CFU; Lactobacillus rhamnosus DSMZ 21690, 2 × 10 CFU) or placebo.75 After 12 weeks, a significant decrease in transaminase levels, cholesterol, triglycerides, low-density lipoprotein-C, and waist circumference was observed in the treatment group. A more pronounced percentage of normal liver sonography was also reported in the intervention group rather than in the placebo group.75 Taken together, these findings suggest a role of probiotics in improving pediatric NAFLD. More recently, few promising clinical trials reported an hepato-metabolic improvement in patients treated with probiotics, suggesting a potential anti-fibrotic activity of these compounds.76 Interestingly, new experimental studies in this field support the beneficial role of gut microbiota manipulation in pediatric NAFLD clinical management.76
Longer RCT is nevertheless needed to better define long-term profile of this NAFLD therapeutic option.
A novel focus in this challenging field is the gut endotoxin lipopolysaccharides found on the outer cell wall of Gram-negative bacteria.1 In fact, patients with biopsy-proven NAFLD showed increased plasma levels of both proinflammatory cytokines (IL-6, IL-1 β, TNF-α) and lipopolysaccharides, which in turn correlated with the presence of NASH and the NAS.36 This might be due to the role of lipopolysaccharides in activating a proinflammatory pathway involving hepatic stellate cell cytokine production through lipopolysaccharide-induced signaling. So that, the gut endotoxin lipopolysaccharides might represent a promising target that should be further studied.23,36
Polyunsaturated fatty acids (PUFAs)
It has been well demonstrated the positive effect of omega-3 PUFAs such as eicosapentaenoic acid and docosahexaenoic acid (DHA) not only on both hepatic lipid metabolism and adipose tissue function but also as anti-inflammatory agents.13 Several studies have shown their effectiveness in both prevention and treatment of cardiometabolic diseases.23,60 Recent pediatric findings demonstrated that NAFLD patients treated with long-chain PUFAs showed improvements in liver function and hepatic steatosis.36,60 In fact, it has been observed a reduction of liver steatosis after 6 months of DHA supplementation, with a sustained improvement of metabolic profile and a significant decrease of fat liver content over 24 months.77 Another RCT confirmed the beneficial effects of DHA supplementation in children with biopsy-proven NAFLD, demonstrating a significant reduction of hepatic fat fraction assessed by MRI.78
However, results from omega-3 supplementation in NAFLD patients are contrasting, with no effect on the degree of steatosis and liver function observed in treated subjects in some RCTs.70,79
To date, there are also promising RCTs investigating the effects of association of different micronutrients such as DHA, choline, vitamin E, and hydroxytyrosol in NAFLD pediatric patients.80,81
Novel investigational therapeutic options for NAFLD treatment
Findings from adult literature have reported promising effects on NAFLD severity by using common drugs such as statins, angiotensin receptor blockers, and GLP-1 agonists.36 However, there is no current evidence supporting their use at pediatric age.
A large amount of data also reported a positive effect on NASH from pentoxifylline (PTX) use in adult NAFLD patients.60 PTX represents a phosphodiesterase inhibitor blocking TNF-A, a proinflammatory cytokine with a pathogenic role in NASH.60 Given that, it might be a valid therapeutic option that should be investigated also in children with NAFLD.
Another promising class drug under evaluation for adult NAFLD treatment is represented by Farnesoid X nuclear receptor (FXR) agonists. Of note, administration of obeticholic acid, a semisynthetic bile acid, and a potent FXR agonist showed significant improvement in liver histology and a relatively favorable safety profile in patients affected by NASH.60,82 Pruritus was the only side effect reported. Nevertheless, there are no pediatric RCTs to date.
To best of our knowledge, there are four controlled Phase 2 pediatric trials evaluating the effects of different molecules such as losartan, anti-LPS (a monoclonal antibody), cysteamine bitartrate (an aminothiol salt), and metreleptin (a synthetic analog of the hormone leptin).16,83–85
More recently, studies highlighted the potential use of microRNAs – involved in the NAFLD pathogenesis through their role in both inflammation and fibrogenesis in hepatic cells – as therapeutic tools in the management of NAFLD and its progressive forms.86
Conclusion
Pediatric NAFLD has become the leading cause of chronic liver disease in childhood with potential serious cardiometabolic consequences even in youth. Laboratory tests and classical imaging techniques play a pivotal role in NAFLD diagnosis, but novel noninvasive alternative methods to diagnose and monitor NAFLD have been investigated.
To date, multiple treatments are available for pediatric NAFLD, but the global effectiveness is very limited. Currently, lifestyle modifications remain the mainstay treatment, although its efficacy is poor because of the lack of compliance. Pediatric research is focusing on multiple alternative treatments targeting the main pathogenic factors such as insulin-resistance, dyslipidemia, gut-liver axis and microbiota, oxidative stress, and proinflammatory pathways. Results from these studies are promising but larger validation is needed. Innovative therapeutic approaches might add an important piece in the complex knowledge of pediatric NAFLD.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Clemente MG, Mandato C, Poeta M, Vajro P. Pediatric non-alcoholic fatty liver disease: recent solutions, unresolved issues, and future research directions. World J Gastroenterol. 2016;22(36):8078–8093. doi: 10.3748/wjg.v22.i36.8078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marzuillo P, Grandone A, Perrone L, Miraglia Del Giudice E. Understanding the pathophysiological mechanisms in the pediatric non-alcoholic fatty liver disease: the role of genetics. World J Hepatol. 2015;7(11):1439–1443. doi: 10.4254/wjh.v7.i11.1439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feldstein AE, Charatcharoenwitthaya P, Treeprasertsuk S, Benson JT, Enders FB, Angulo P. The natural history of non-alcoholic fatty liver disease in children: a follow-up study for up to 20 years. Gut. 2009;58(11):1538–1544. doi: 10.1136/gut.2008.171280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buzzetti E, Pinzani M, Tsochatzis EA. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism. 2016;65(8):1038–1048. doi: 10.1016/j.metabol.2015.12.012 [DOI] [PubMed] [Google Scholar]
- 5.Goyal NP, Schwimmer JB. The progression and natural history of pediatric nonalcoholic fatty liver disease. Clin Liver Dis. 2016;20(2):325–338. doi: 10.1016/j.cld.2015.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marzuillo P, Miraglia del Giudice E, Santoro N. Pediatric fatty liver disease: role of ethnicity and genetics. World J Gastroenterol. 2014;20(23):7347–7355. doi: 10.3748/wjg.v20.i23.7347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Di Sessa A, Umano GR, Cirillo G, et al. The membrane-bound O-Acyltransferase7 rs641738 variant in pediatric nonalcoholic fatty liver disease. J Pediatr Gastroenterol Nutr. 2018;67(1):69–74. doi: 10.1097/MPG.0000000000001979 [DOI] [PubMed] [Google Scholar]
- 8.Grandone A, Cozzolino D, Marzuillo P, et al. TM6SF2 Glu167Lys polymorphism is associated with low levels of LDL-cholesterol and increased liver injury in obese children. Pediatr Obes. 2016;11(2):115–119. doi: 10.1111/ijpo.12032 [DOI] [PubMed] [Google Scholar]
- 9.Nobili V, Schwimmer JB, Vajro P. Breastfeeding and NAFLD from the maternal side of the mother-infant dyad. J Hepatol. 2019;70(1):13–14. doi: 10.1016/j.jhep.2018.10.030 [DOI] [PubMed] [Google Scholar]
- 10.Alisi A, Vajro P. Pre-natal and post-natal environment monitoring to prevent non-alcoholic fatty liver disease development. J Hepatol. 2017;67(3):451–453. doi: 10.1016/j.jhep.2017.04.016 [DOI] [PubMed] [Google Scholar]
- 11.Poeta M, Vajro P. Mediterranean diet to prevent/treat nonalcoholic fatty liver disease in children: a promising approach. Nutrition. 2017;43–44:98–99. doi: 10.1016/j.nut.2017.04.005 [DOI] [PubMed] [Google Scholar]
- 12.Manco M. Metabolic syndrome in childhood from impaired carbohydrate metabolism to nonalcoholic fatty liver disease. J Am Coll Nutr. 2011;30(5):295–303. [DOI] [PubMed] [Google Scholar]
- 13.Braun HA, Faasse SA, Vos MB. Advances in pediatric fatty liver disease: pathogenesis, diagnosis, and treatment. Gastroenterol Clin North Am. 2018;47(4):949–968. doi: 10.1016/j.gtc.2018.07.016 [DOI] [PubMed] [Google Scholar]
- 14.Anderson EL, Howe LD, Jones HE, Higgins JP, Lawlor DA, Fraser A. The prevalence of non-alcoholic fatty liver disease in children and adolescents: a systematic review and meta-analysis. PLoS One. 2015;10(10):e0140908. doi: 10.1371/journal.pone.0140908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Di Sessa A, Umano GR, Miraglia Del Giudice E. The association between non-alcoholic fatty liver disease and cardiovascular risk in children. Children (Basel). 2017;4:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Draijer L, Benninga M, Koot B. Pediatric NAFLD: an overview and recent developments in diagnostics and treatment. Expert Rev Gastroenterol Hepatol. 2019;13(5):447–461. doi: 10.1080/17474124.2019.1595589 [DOI] [PubMed] [Google Scholar]
- 17.Marzuillo P, Di Sessa A, Guarino S. et al. Nonalcoholic fatty liver disease and eGFR levels could be linked by the PNPLA3 I148M polymorphism in children with obesity. Pediatr Obes;2019. e12539. doi: 10.1111/ijpo.12539 [DOI] [PubMed] [Google Scholar]
- 18.Vos MB, Abrams SH, Barlow SE, et al. NASPGHAN clinical practice guideline for the diagnosis and treatment of nonalcoholic fatty liver disease in children: recommendations from the Expert Committee on NAFLD (ECON) and the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN). J Pediatr Gastroenterol Nutr. 2017;64(2):319–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Di Sessa A, Marzuillo P, Guarino S, Cirillo G, Miraglia Del Giudice E. When a secondary form of pediatric non-alcoholic fatty liver disease should be suspected? Expert Rev Gastroenterol Hepatol. 2019;13(6):519–521.doi: 10.1080/17474124.2019.1605290 [DOI] [PubMed] [Google Scholar]
- 20.Marzuillo P, Grandone A, Perrone L, Miraglia Del Giudice E. Controversy in the diagnosis of pediatric non-alcoholic fatty liver disease. World J Gastroenterol. 2015;21(21):6444–6450. doi: 10.3748/wjg.v21.i21.6444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Koot BGP, Nobili V. Screening for non-alcoholic fatty liver disease in children: do guidelines provide enough guidance? Obes Rev. 2017;18(9):1050–1060. doi: 10.1111/obr.12556 [DOI] [PubMed] [Google Scholar]
- 22.Vajro P, Lenta S, Socha P, et al. Diagnosis of nonalcoholic fatty liver disease in children and adolescents: position paper of the ESPGHAN Hepatology Committee. J Pediatr Gastroenterol Nutr. 2012;54(5):700–713. doi: 10.1097/MPG.0b013e318252a13f [DOI] [PubMed] [Google Scholar]
- 23.Flisiak-Jackiewicz M, Lebensztejn DM. Update on pathogenesis, diagnostics and therapy of nonalcoholic fatty liver disease in children. Clin Exp Hepatol. 2019;5(1):11–21. doi: 10.5114/ceh.2019.83152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mandelia C, Kabbany MN, Conjeevaram Selvakumar PK, Alkhouri N. The search for noninvasive methods to identify liver fibrosis in children with nonalcoholic fatty liver disease. Biomark Med. 2018;12(3):265–273. doi: 10.2217/bmm-2017-0038 [DOI] [PubMed] [Google Scholar]
- 25.Klusek-Oksiuta M, Bialokoz-Kalinowska I, Tarasow E, Wojtkowska M, Werpachowska I, Lebensztejn DM. Chemerin as a novel non-invasive serum marker of intrahepatic lipid content in obese children. Ital J Pediatr. 2014;40:84. doi: 10.1186/s13052-014-0084-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mohamed AA, Sabry S, Abdallah AM, et al. Circulating adipokines in children with nonalcoholic fatty liver disease: possible noninvasive diagnostic markers. Ann Gastroenterol. 2017;30(4):457–463. doi: 10.20524/aog.2017.0148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lebensztejn DM, Flisiak-Jackiewicz M, Bialokoz-Kalinowska I, Bobrus-Chociej A, Kowalska I. Hepatokines and non-alcoholic fatty liver disease. Acta Biochim Pol. 2016;63(3):459–467. doi: 10.18388/abp.2015_1252 [DOI] [PubMed] [Google Scholar]
- 28.Walenbergh SM, Houben T, Hendrikx T, et al. Plasma cathepsin D levels: a novel tool to predict pediatric hepatic inflammation. Am J Gastroenterol. 2015;110(3):462–470. doi: 10.1038/ajg.2015.29 [DOI] [PubMed] [Google Scholar]
- 29.Manco M, Marcellini M, Giannone G, Nobili V. Correlation of serum TNF-alpha levels and histologic liver injury scores in pediatric nonalcoholic fatty liver disease. Am J Clin Pathol. 2007;127(6):954–960. doi: 10.1309/6VJ4DWGYDU0XYJ8Q [DOI] [PubMed] [Google Scholar]
- 30.Sayin O, Tokgoz Y, Arslan N. Investigation of adropin and leptin levels in pediatric obesity-related nonalcoholic fatty liver disease. J Pediatr Endocrinol Metab. 2014;27(5–6):479–484. doi: 10.1515/jpem-2013-0296 [DOI] [PubMed] [Google Scholar]
- 31.Pacifico L, Bonci E, Marandola L, Romaggioli S, Bascetta S, Chiesa C. Increased circulating zonulin in children with biopsy-proven nonalcoholic fatty liver disease. World J Gastroenterol. 2014;20(45):17107–17114. doi: 10.3748/wjg.v20.i45.17107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Romanowska A, Lebensztejn DM, Skiba E, Tarasow E, Kaczmarski M. Retinol binding protein-4 as a serum biomarker of intrahepatic lipid content in obese children–preliminary report. Acta Biochim Pol. 2011;58(1):35–38. [PubMed] [Google Scholar]
- 33.Flisiak-Jackiewicz M, Bobrus-Chociej A, Tarasow E, Wojtkowska M, Bialokoz-Kalinowska I, Lebensztejn DM. Predictive role of interleukin-18 in liver steatosis in obese children. Can J Gastroenterol Hepatol. 2018;2018:3870454. doi: 10.1155/2018/3870454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jaimes C, Gee MS. Strategies to minimize sedation in pediatric body magnetic resonance imaging. Pediatr Radiol. 2016;46(6):916–927. doi: 10.1007/s00247-016-3613-z [DOI] [PubMed] [Google Scholar]
- 35.Jaimes C, Kirsch JE, Gee MS. Fast, free-breathing and motion-minimized techniques for pediatric body magnetic resonance imaging. Pediatr Radiol. 2018;48(9):1197–1208. doi: 10.1007/s00247-018-4116-x [DOI] [PubMed] [Google Scholar]
- 36.Shah J, Okubote T, Alkhouri N. Overview of updated practice guidelines for pediatric nonalcoholic fatty liver disease. Gastroenterol Hepatol (N Y). 2018;14(7):407–414. [PMC free article] [PubMed] [Google Scholar]
- 37.Dezsofi A, Baumann U, Dhawan A, et al. Liver biopsy in children: position paper of the ESPGHAN Hepatology Committee. J Pediatr Gastroenterol Nutr. 2015;60(3):408–420. [DOI] [PubMed] [Google Scholar]
- 38.Alfani R, Vassallo E, De Anseris AG, et al. Pediatric fatty liver and obesity: not always justa matter of non-alcoholic fatty liver disease. Children (Basel). 2018;5:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Noureddin M, Lam J, Peterson MR, et al. Utility of magnetic resonance imaging versus histology for quantifying changes in liver fat in nonalcoholic fatty liver disease trials. Hepatology. 2013;58(6):1930–1940. doi: 10.1002/hep.26455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Awai HI, Newton KP, Sirlin CB, Behling C, Schwimmer JB. Evidence and recommendations for imaging liver fat in children, based on systematic review. Clin Gastroenterol Hepatol. 2014;12(5):765–773. doi: 10.1016/j.cgh.2013.09.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Di Martino M, Pacifico L, Bezzi M, et al. Comparison of magnetic resonance spectroscopy, proton density fat fraction and histological analysis in the quantification of liver steatosis in children and adolescents. World J Gastroenterol. 2016;22(39):8812–8819. doi: 10.3748/wjg.v22.i39.8812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schwimmer JB, Middleton MS, Behling C, et al. Magnetic resonance imaging and liver histology as biomarkers of hepatic steatosis in children with nonalcoholic fatty liver disease. Hepatology. 2015;61(6):1887–1895. doi: 10.1002/hep.27666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rehm JL, Wolfgram PM, Hernando D, Eickhoff JC, Allen DB, Reeder SB. Proton density fat-fraction is an accurate biomarker of hepatic steatosis in adolescent girls and young women. Eur Radiol. 2015;25(10):2921–2930. doi: 10.1007/s00330-015-3724-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Middleton MS, Van Natta ML, Heba ER, et al. Diagnostic accuracy of magnetic resonance imaging hepatic proton density fat fraction in pediatric nonalcoholic fatty liver disease. Hepatology. 2018;67(3):858–872. doi: 10.1002/hep.29596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Desai NK, Harney S, Raza R, et al. Comparison of controlled attenuation parameter and liver biopsy to assess hepatic steatosis in pediatric patients. J Pediatr. 2016;173:160–164 e161. doi: 10.1016/j.jpeds.2016.03.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schwimmer JB, Behling C, Angeles JE, et al. Magnetic resonance elastography measured shear stiffness as a biomarker of fibrosis in pediatric nonalcoholic fatty liver disease. Hepatology. 2017;66(5):1474–1485. doi: 10.1002/hep.29241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kotronen A, Peltonen M, Hakkarainen A, et al. Prediction of non-alcoholic fatty liver disease and liver fat using metabolic and genetic factors. Gastroenterology. 2009;137(3):865–872. doi: 10.1053/j.gastro.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 48.Maffeis C, Banzato C, Rigotti F, et al. Biochemical parameters and anthropometry predict NAFLD in obese children. J Pediatr Gastroenterol Nutr. 2011;53(6):590–593. doi: 10.1097/MPG.0b013e31822960be [DOI] [PubMed] [Google Scholar]
- 49.Eng K, Lopez R, Liccardo D, Nobili V, Alkhouri N. A non-invasive prediction model for non-alcoholic steatohepatitis in paediatric patients with non-alcoholic fatty liver disease. Dig Liver Dis. 2014;46(11):1008–1013. doi: 10.1016/j.dld.2014.07.016 [DOI] [PubMed] [Google Scholar]
- 50.Nobili V, Alisi A, Vania A, Tiribelli C, Pietrobattista A, Bedogni G. The pediatric NAFLD fibrosis index: a predictor of liver fibrosis in children with non-alcoholic fatty liver disease. BMC Med. 2009;7:21. doi: 10.1186/1741-7015-7-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nobili V, Parkes J, Bottazzo G, et al. Performance of ELF serum markers in predicting fibrosis stage in pediatric non-alcoholic fatty liver disease. Gastroenterology. 2009;136(1):160–167. doi: 10.1053/j.gastro.2008.09.013 [DOI] [PubMed] [Google Scholar]
- 52.Alkhouri N, Carter-Kent C, Lopez R, et al. A combination of the pediatric NAFLD fibrosis index and enhanced liver fibrosis test identifies children with fibrosis. Clin Gastroenterol Hepatol. 2011;9(2):150–155. doi: 10.1016/j.cgh.2010.09.015 [DOI] [PubMed] [Google Scholar]
- 53.Jackson JA, Konomi JV, Mendoza MV, et al. Performance of fibrosis prediction scores in paediatric non-alcoholic fatty liver disease. J Paediatr Child Health. 2018;54(2):172–176. doi: 10.1111/jpc.13689 [DOI] [PubMed] [Google Scholar]
- 54.Alkhouri N, Mansoor S, Giammaria P, Liccardo D, Lopez R, Nobili V. The development of the pediatric NAFLD fibrosis score (PNFS) to predict the presence of advanced fibrosis in children with nonalcoholic fatty liver disease. PLoS One. 2014;9(8):e104558. doi: 10.1371/journal.pone.0104558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Troisi J, Belmonte F, Bisogno A, et al. Metabolomic salivary signature of pediatric obesity related liver disease and metabolic syndrome. Nutrients. 2019;11:2. doi: 10.3390/nu11020274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Troisi J, Belmonte F, Bisogno A, et al. Salivary markers of hepato-metabolic comorbidities in pediatric obesity. Dig Liver Dis. 2019;51(4):516–523. doi: 10.1016/j.dld.2018.11.009 [DOI] [PubMed] [Google Scholar]
- 57.Pierri L, Saggese P, Guercio Nuzio S, et al. Relations of gut liver axis components and gut microbiota in obese children with fatty liver: a pilot study. Clin Res Hepatol Gastroenterol. 2018;42(4):387–390. doi: 10.1016/j.clinre.2018.03.015 [DOI] [PubMed] [Google Scholar]
- 58.Troisi J, Pierri L, Landolfi A, et al. Urinary metabolomics in pediatric obesity and NAFLD Identifies metabolic pathways/metabolites related to dietary habits and gut-liver axis perturbations. Nutrients. 2017;9:5. doi: 10.3390/nu9050485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Guercio Nuzio S, Di Stasi M, Pierri L, et al. Multiple gut-liver axis abnormalities in children with obesity with and without hepatic involvement. Pediatr Obes. 2017;12(6):446–452. doi: 10.1111/ijpo.12164 [DOI] [PubMed] [Google Scholar]
- 60.Liyanagedera S, Williams RP, Veraldi S, Nobili V, Mann JP. The pharmacological management of NAFLD in children and adolescents. Expert Rev Clin Pharmacol. 2017;10(11):1225–1237. doi: 10.1080/17512433.2017.1365599 [DOI] [PubMed] [Google Scholar]
- 61.Zelber-Sagi S, Kessler A, Brazowsky E, et al. A double-blind randomized placebo-controlled trial of orlistat for the treatment of nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2006;4(5):639–644. doi: 10.1016/j.cgh.2006.02.004 [DOI] [PubMed] [Google Scholar]
- 62.Harrison SA, Fecht W, Brunt EM, Neuschwander-Tetri BA. Orlistat for overweight subjects with nonalcoholic steatohepatitis: a randomized, prospective trial. Hepatology. 2009;49(1):80–86. doi: 10.1002/hep.22575 [DOI] [PubMed] [Google Scholar]
- 63.Yanovski SZ, Yanovski JA. Long-term drug treatment for obesity: a systematic and clinical review. JAMA. 2014;311(1):74–86. doi: 10.1001/jama.2013.281361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nobili V, Vajro P, Dezsofi A, et al. Indications and limitations of bariatric intervention in severely obese children and adolescents with and without nonalcoholic steatohepatitis: ESPGHAN Hepatology Committee Position Statement. J Pediatr Gastroenterol Nutr. 2015;60(4):550–561. [DOI] [PubMed] [Google Scholar]
- 65.Manco M, Mosca A, De Peppo F, et al. The benefit of sleeve gastrectomy in obese adolescents on nonalcoholic steatohepatitis and hepatic fibrosis. J Pediatr. 2017;180:31–37 e32. doi: 10.1016/j.jpeds.2016.08.101 [DOI] [PubMed] [Google Scholar]
- 66.Violi F, Cangemi R. Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis. N Engl J Med. 2010;363(12):1185–1186;author reply 1186. doi: 10.1056/NEJMc1006581 [DOI] [PubMed] [Google Scholar]
- 67.Lavine JE, Schwimmer JB, Van Natta ML, et al. Effect of vitamin E or metformin for treatment of nonalcoholic fatty liver disease in children and adolescents: the TONIC randomized controlled trial. JAMA. 2011;305(16):1659–1668. doi: 10.1001/jama.2011.520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Schwimmer JB, Lavine JE, Wilson LA, et al. In children with nonalcoholic fatty liver disease, cysteamine bitartrate delayed release improves liver enzymes but does not reduce disease activity scores. Gastroenterology. 2016;151(6):1141–1154 e1149. doi: 10.1053/j.gastro.2016.08.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Socha P, Horvath A, Vajro P, Dziechciarz P, Dhawan A, Szajewska H. Pharmacological interventions for nonalcoholic fatty liver disease in adults and in children: a systematic review. J Pediatr Gastroenterol Nutr. 2009;48(5):587–596. doi: 10.1097/MPG.0b013e31818e04d1 [DOI] [PubMed] [Google Scholar]
- 70.Mitchel EB, Lavine JE. Review article: the management of paediatric nonalcoholic fatty liver disease. Aliment Pharmacol Ther. 2014;40(10):1155–1170. doi: 10.1111/apt.12972 [DOI] [PubMed] [Google Scholar]
- 71.Vajro P, Mandato C, D’Aniello R. More on current evidences on probiotics as a novel treatment for non-alcoholic fatty liver disease. Hepat Mon. 2013;13(8):e13780. doi: 10.5812/hepatmon [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Alisi A, Bedogni G, Baviera G, et al. Randomised clinical trial: the beneficial effects of VSL#3 in obese children with non-alcoholic steatohepatitis. Aliment Pharmacol Ther. 2014;39(11):1276–1285. doi: 10.1111/apt.12758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Poeta M, Pierri L, Vajro P. Gut-liver axis derangement in non-alcoholic fatty liver disease. Children (Basel). 2017;4:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nobili V, Putignani L, Mosca A, et al. Bifidobacteria and lactobacilli in the gut microbiome of children with non-alcoholic fatty liver disease: which strains act as health players? Arch Med Sci. 2018;14(1):81–87. doi: 10.5114/aoms.2016.62150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Famouri F, Shariat Z, Hashemipour M, Keikha M, Kelishadi R. Effects of probiotics on nonalcoholic fatty liver disease in obese children and adolescents. J Pediatr Gastroenterol Nutr. 2017;64(3):413–417. doi: 10.1097/MPG.0000000000001422 [DOI] [PubMed] [Google Scholar]
- 76.Putignani L, Alisi A, Nobili V. Pediatric NAFLD: the future role of patient-tailored probiotics therapy. J Pediatr Gastroenterol Nutr. 2016;63(Suppl 1):S6–S8. doi: 10.1097/MPG.0000000000001220 [DOI] [PubMed] [Google Scholar]
- 77.Nobili V, Alisi A, Della Corte C, et al. Docosahexaenoic acid for the treatment of fatty liver: randomised controlled trial in children. Nutr Metab Cardiovasc Dis. 2013;23(11):1066–1070. doi: 10.1016/j.numecd.2012.10.010 [DOI] [PubMed] [Google Scholar]
- 78.Pacifico L, Bonci E, Di Martino M, et al. A double-blind, placebo-controlled randomized trial to evaluate the efficacy of docosahexaenoic acid supplementation on hepatic fat and associated cardiovascular risk factors in overweight children with nonalcoholic fatty liver disease. Nutr Metab Cardiovasc Dis. 2015;25(8):734–741. doi: 10.1016/j.numecd.2015.04.003 [DOI] [PubMed] [Google Scholar]
- 79.Janczyk W, Lebensztejn D, Wierzbicka-Rucińska A, et al. Omega-3 Fatty acids therapy in children with nonalcoholic fatty liver disease: a randomized controlled trial. J Pediatr. 2015;166(6):1358. doi: 10.1016/j.jpeds.2015.01.056 [DOI] [PubMed] [Google Scholar]
- 80.Zohrer E, Alisi A, Jahnel J, et al. Efficacy of docosahexaenoic acid-choline-vitamin E in paediatric NASH: a randomized controlled clinical trial. Appl Physiol Nutr Metab. 2017;42(9):948–954. doi: 10.1139/apnm-2016-0689 [DOI] [PubMed] [Google Scholar]
- 81.Nobili V, Alisi A, Mosca A, et al. The antioxidant effects of hydroxytyrosol and vitamin e on pediatric nonalcoholic fatty liver disease, in a clinical trial: a new treatment? Antioxid Redox Signal. 2019. doi: 10.1089/ars.2018.7704 [DOI] [PubMed] [Google Scholar]
- 82.Neuschwander-Tetri BA, Loomba R, Sanyal AJ, et al. Farnesoid X nuclear receptor ligand obeticholic acid for non-cirrhotic, non-alcoholic steatohepatitis (FLINT): a multicentre, randomised, placebo-controlled trial. Lancet. 2015;385(9972):956–965. doi: 10.1016/S0140-6736(14)61933-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rotman Y, Sanyal AJ. Current and upcoming pharmacotherapy for non-alcoholic fatty liver disease. Gut. 2017;66(1):180–190. doi: 10.1136/gutjnl-2016-312431 [DOI] [PubMed] [Google Scholar]
- 84.Javor ED, Ghany MG, Cochran EK, et al. Leptin reverses nonalcoholic steatohepatitis in patients with severe lipodystrophy. Hepatology. 2005;41(4):753–760. doi: 10.1002/hep.20672 [DOI] [PubMed] [Google Scholar]
- 85.Vos MB, Jin R, Konomi JV, et al. A randomized, controlled, crossover pilot study of losartan for pediatric nonalcoholic fatty liver disease. Pilot Feasibility Stud. 2018;4:109. doi: 10.1186/s40814-018-0306-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Su Q, Kumar V, Sud N, Mahato RI. MicroRNAs in the pathogenesis and treatment of progressive liver injury in NAFLD and liver fibrosis. Adv Drug Deliv Rev. 2018;129:54–63. doi: 10.1016/j.addr.2018.01.009 [DOI] [PubMed] [Google Scholar]