Abstract
Purpose
Hypothyroidism has traditionally been associated with obesity, whereas hyperthyroidism has been linked to being underweight. However, very few studies have assessed these associations. The aim of this work is to evaluate the association between thyroid dysfunction and body mass index (BMI) at baseline and after normalization of the hormone levels.
Patients and methods
A retrospective, observational study of a cohort of otherwise healthy patients that were referred for evaluation of thyroid dysfunction to the Endocrine Department of Pontevedra University Complex Hospital, Spain was conducted. We collected data of BMI and thyroid hormone levels before treatment and after normalization of thyroid function within a follow-up period of 12 months.
Results
A total of 330 patients were initially selected for the study. In order to exclude variables that for any reason could influence on BMI, 235 were excluded for further studies. Another 61 patients were also excluded because incomplete data on their medical records, failure to achieve euthyroidism, or lost to follow-up. Therefore, the eligible final study group consisted of 34 patients (17 with hypothyroidism and 17 with hyperthyroidism). No differences were observed in mean baseline BMI between hypo and hyperthyroid patients (27.07±3.22 vs 26.39±4.44, p=0.609). Overweight or obesity was observed in 76.5% and 58.8% of hypothyroid and hyperthyroid patients, respectively (p=0.23). After normalization of thyroid function, the weight of hypothyroid patients decreased from 70.93±10.06 kg to 68.68±10.14 (p=0.000), while the weight of hyperthyroid patients increased from 65.45±11.64 kg to 68.37±12.80 (p=0.000). Their mean BMI was 26.22±3.36 and 27.57±4.98 (p=0.361) for hypo- and hyperthyroid patients, respectively. 58.8% and 64.7% patients remained in the overweight/obesity range in each group (p=0.72).
Conclusion
Untreated thyroid dysfunction is not associated with BMI. Normalization of thyroid levels significantly changed the weight of patients, but remaining most patients within overweight ranges.
Keywords: hypothyroidism, hyperthyroidism, body mass index, obesity
Introduction
Thyroid disorders are highly prevalent diseases affecting nearly 10% of the population in Spain.1 In a recent study in adults, the prevalence of hypothyroidism was 9.1% and 0.8% for hyperthyroidism.1 Thyroid disorders are the major cause of referral to the Endocrinology Department in our Hospital, reaching 47.6% of all first visits (unpublished data).
Thyroid hormones are involved in multiple physiological processes and regulating basal metabolic rate, promote the adrenergic nervous system to generate heat in response to cold exposure, stimulate gluconeogenesis and both lipolysis and lipogenesis.2 Patients with thyroid dysfunction may experience changes in body weight and body composition.3
Hypothyroidism induces a decreased basal metabolism and thermogenesis, an accumulation of hyaluronic acid and a decreased renal flow, all factors leading to water retention. Severe hypothyroidism states lead to a clinical picture known as myxoedema in which hyperkeratosis of the skin and facial edema could give the patient a false appearance of overweight.4,5 Patients with hypothyroidism have also slow peristalsis causing chronic constipation that may result in weight gain. This weight gain is mainly due to water retention and is not related to an increase in fat mass.3 In addition, some studies have found a higher prevalence of subclinical hypothyroidism among obese patients.6 Altogether, these factors have probably contributed to a general belief of a direct association of hypothyroidism with obesity. The American Thyroid Association in the 2012 guidelines on the management of hypothyroidism makes reference to the absence of evidence in this field. These guidelines mention that hypothyroidism and obesity are often linked at least in the consciousness of the lay public, and that although some observational studies correlate thyrotropin (TSH) levels with body mass index (BMI) others do not.7 To our knowledge, very few studies have directly assessed this topic and no clear association has been established between hypothyroidism and obesity.8
Conversely, hyperthyroidism has traditionally been associated with weight loss and underweight.8 Subjects with hyperthyroidism have an adrenergic hyperstimulation with increased basal metabolism and thermogenesis, and a greater overall energy expenditure resulting in a tendency toward weight loss. Hyperthyroidism can also induce an increased gastrointestinal transit and occasionally anorexia due to the anorexigenic effect of triiodothyronine.4 All these factors may have lead to the belief of a direct association of hyperthyroid states with low weight.9 But, as it happens with the case of hypothyroidism, this relationship has not been clearly established.
Based on these alterations, and from a theoretical point of view, patients with thyroid dysfunction would be expected to return to their body weight prior to the onset of the dysfunction once achieving normal hormone levels with specific therapy. However, several studies have shown that this is not always true.10–14
The aim of our study was to investigate the association between thyroid dysfunction and BMI at baseline and after normalization of the hormone levels.
Materials and methods
We carried out a retrospective, observational, descriptive study on a cohort of patients with thyroid dysfunction that were referred to the Department of Endocrinology at the Pontevedra University Hospital Complex in Spain. Patients were followed-up until results of their thyroid function tests were normal within a 12-month period. The medical records of all patients were reviewed.
The variables collected were gender, age, thyroid dysfunction etiology, TSH levels, free levothyroxine (FT4) levels, presence of thyroid autoimmunity (considered as detection of anti-thyroperoxidase antibodies and/or TSH receptor antibodies), BMI and weight at the time of referral to the Department of Endocrinology and after normalization of thyroid hormone levels after treatment.
Inclusion criteria
Patients over 18 years of age were referred to the Department of Endocrinology for thyroid dysfunction evaluation.
Exclusion criteria
We excluded for the analysis patients with any variable that for any reason could influence on BMI: Hypocalorific diets, tobacco use, recent quit smoking or recreational drug use, severe psychiatric illness, pregnancy and postpartum stages, diabetes mellitus treated with insulin therapy, sulfonylureas, GLP-1 analogues or SGLT-2 inhibitors, prescription of drugs affecting body weight (corticosteroids, antipsychotics, mirtazapine, anticonvulsants, antineoplastic hormone therapy, fluoxetine or topiramate) and other comorbidities such as advanced congestive heart failure, chronic obstructive pulmonary disease, end-stage renal disease or active neoplasm.
Statistical analysis
Statistical analysis was performed using the SPSS software version 16 (SPSS Inc., Chicago, Illinois, USA). Categorical variables were expressed in terms of frequency and percentage, and quantitative variables were expressed as mean and standard deviation, or median and rank in cases of a non-normal distribution. The chi-Square or Fisher’s test was used to find the association between categorical variables. Normality of quantitative variables was verified using the Kolmogorov–Smirnov test. Quantitative variables were compared using the Student’s t-test for variables with a normal distribution and the Wilcoxon test for the remaining variables. Differences were considered to be statistically significant when p<0.05.
The study was approved by the Galician Research Ethics Committee (Ref. Code 2015/142). Patients’ consent to review their medical records was not required by means of a waiver from the Galician Research Ethics Committee. Due to the retrospective nature of the study and the high number of patients we were prevented from obtaining individual consent. Data confidentiality was preserved and the study is compliant with the Declaration of Helsinki.
Results
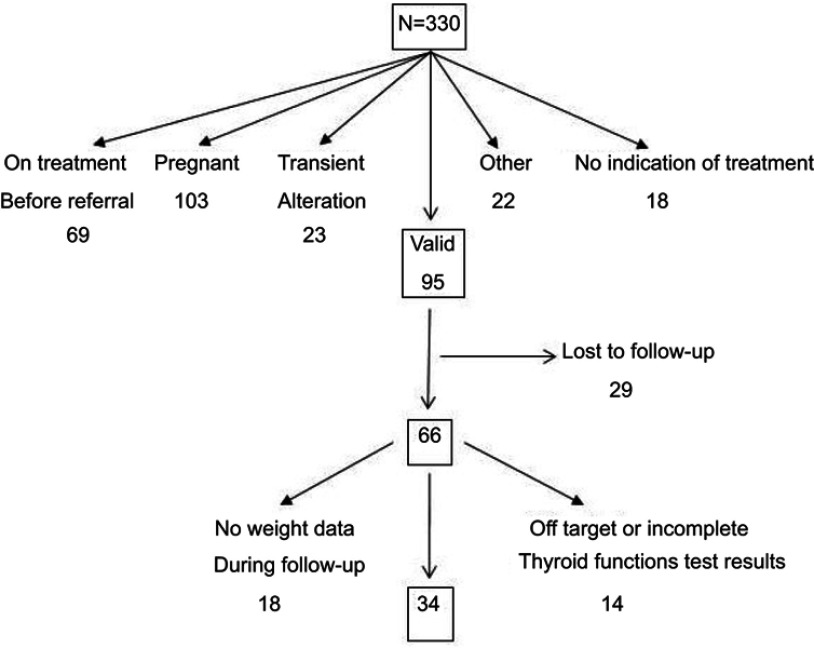
A total of 330 patients were referred to the Department of Endocrinology for thyroid dysfunction evaluation during the study period. Of these, 235 patients were excluded from further analysis for the following reasons: 69 had already initiated treatment for thyroid dysfunction before their first visit to the Department of Endocrinology, 103 were pregnant, 23 were experiencing transient thyroid dysfunction, treatment was not indicated in 18, and 22 were excluded for other reasons. Of the remaining 95 patients, 29 were lost to follow-up, 18 had incomplete medical records, and euthyroidism could not be achieved in the other 14, despite treatment (Figure 1).
Figure 1.
Patient selection flowchart.
Finally, a total of 34 otherwise healthy patients were included for analysis, comprising 6 male (17.6%) and 28 female (82.4%); of these, there were 17 with hyperthyroidism and 17 with hypothyroidism. The mean age was 53.4±20.4 years. The demographic, anthropometric, and biochemical characteristics for these patients are shown in Table 1.
Table 1.
Baseline and post-treatment demographic, anthropometric, and biochemical characteristics of patients with thyroid dysfunction
| Total | Hypothyroid patients | Hyperthyroid patients | p | |
|---|---|---|---|---|
| N | 34 | 17 | 17 | |
| Gender | 28 female (82.4%) | 12 female (70.6%) | 16 female (94.1%) | 0.175 |
| Age | 53.4±20.4 | 55.8±18.7 | 50.3±2 2.4 | 0.386 |
| Height (cm) | 161.82±0.08 | 157.53±0.07 | 0.086 | |
| Baseline weight (kg) | 70.93±10.06 | 65.45±11.64 | 0.152 | |
| Final weight (kg) | 68.68±10.14 | 68.37±12.80 | 0.938 | |
| Baseline BMI (kg/m2) | 27.07±3.22 | 26.39±4.44 | 0.609 | |
| Final BMI (kg/m2) | 26.22±3.36 | 27.57±4.98 | 0.361 | |
| Baseline TSH levels | 23.99±26.35 | 0.03±0.02 | 0.000 | |
| Final TSH levels | 3.27±1.53 | 2.98±1.45 | 0.576 | |
| Baseline T4 levels | 0.67±0.17 | 1.58±0.58 | 0.000 | |
| Final T4 levels | 0.91±0.12 | 0.73±0.23 | 0.009 | |
| Thyroid autoimmunity ATPO TSHrAb |
19 (55.9%) | 8 (47.1%) 8 (47.1%) |
11 (64.7%) 2 (11.7%) 9 (52.9%) |
0.300 |
Notes: TSH: Thyrotropin. Normal range: 0.34–5.6 µU/mL. T4: thyroxine. Normal range: 0.54–1.24 µU/mL. ATPO: anti-thyroperoxidase antibodies. TSHr Ab: Anti TSH receptors antibodies.
Abbreviations: BMI, body mass index; FT4, free thyroxine.
The etiology of hypothyroidism per case was 13 patients with primary hypothyroidism (anti-thyroperoxidase antibodies present in eight cases), two with amiodarone-induced hypothyroidism, one with post-surgical hypothyroidism, and one postradioiodine therapy. Seven patients presented subclinical hypothyroidism (TSH <10 μU/mL) and two presented severe hypothyroidism (TSH 91.00 μU/mL and 46.50 μU/mL, respectively).
The etiology of hyperthyroidism per case was nine patients with Graves-Basedow disease (all with the presence of TSH receptor antibodies), five with Plummer’s disease or toxic multinodular goiter, one with primary autoimmune hyperthyroidism, one as a secondary condition to the Jod-Basedow phenomenon, and one with unknown etiology.
Thyroid autoimmunity was present in 19 subjects, more than 50% of the sample, according to the two major causes of hypo and hyperthyroidism.
There were no statistically significant baseline differences between the two groups in gender (p=0.175), autoimmunity etiology of the disease (p=0.300), age (p=0.386), or height (p=0.086). As expected, significant differences were observed in baseline levels of FT4 and TSH (p<0.001).
When comparing basal mean weight or BMI, no significant differences were found between hypothyroid and hyperthyroid patients: Basal weight 70.93±10.06 kg vs 65.45±11.64 kg (p=0.152) and BMI 27.07±3.22 kg/m2 vs 26.39±4.44 kg/m2 (p=0.609) for hypo- and hyperthyroid patients, respectively.
After specific treatment and normalization of thyroid hormone levels, there were still no statistically significant differences in body weight between the two groups (68.68±10.14 kg vs 68.37±12.80 kg; p=0.938) or in BMI (26.22±3.36 kg/m2 vs 27.57±4.98 kg/m2 p=0.361) for hypo- and hyperthyroid patients, respectively. 58.8% and 64.7% of the patients remained in the overweight/obesity range in each group (p=0.72).
After treatment and normalization of thyroid function of the 17 hypothyroid patients, the mean patient weight fell from 70.93±10.06 kg to 68.68±10.14 kg (mean difference 2.25±2.01 kg; p<0.001). Statistically significant differences were also observed between patients’ baseline BMI, 27.07±3.22 kg/m2, and final BMI, 26.22±3.36 kg/m2 (mean difference 0.86±0.77; p<0.001).
After treatment and normalization of thyroid function of the 17 patients with hyperthyroidism, the mean baseline weight increased from 65.45±11.64 kg to 68.37±12.80 kg, giving a mean difference of 2.92±3.01 kg (p=0.001). Statistically significant differences were also observed between the patient’s baseline BMI, 26.39±4.44 kg/m2, and post-treatment BMI, 27.57±4.98 kg/m2 (mean difference 1.18±1.22; p=0.001).
Discussion
In our study, no statistically significant differences were observed in the weight or the BMI of hypo- and hyperthyroid patients, neither at diagnosis, nor following normalization of hormone levels after treatment. At baseline, both hypo- and hyperthyroid patient groups demonstrated a non-significant weight difference of approximately 6 kg, and a very similar BMI, respectively, with both groups falling into the overweight range. After treatment and normalization of thyroid function, the difference in weight between the two groups was further reduced. The BMI values also remained similar for both groups.
In addition, after analyzing the two different types of thyroid function disorder (hyper- and hypothyroidism) separately, we observed statistically significant differences between baseline and post-treatment body weight and BMI. Hypothyroid patients experienced a mean weight loss of 2.25±2.01 kg, which is much less than the weight loss described in classic series.6 However, we are unaware of the existence of any recent series that had addressed this topic. Our results may have been influenced by the fact that seven of the hypothyroid patients showed a subclinical hormone alteration (TSH <10 μU/mL). However, it is noteworthy that patients with a greater degree of hypothyroidism (TSH 91.00 and 46.50 μU/mL) experienced a weight loss of less than 2 kg when they reached euthyroid status.
Some authors suggest that weight gain is greater in post-surgical hypothyroidism than in autoimmune hypothyroidism.12 In our study, there was only one case of post-surgical hypothyroidism; this might account for the non-significant weight loss experienced by these patients.
The relationship between hypothyroidism and obesity has historically been based on studies with a baseline population selected from obese patients whose thyroid hormone levels were assessed. In several of these studies, higher incidences of hypothyroidism were found in obese patients than in the general population.16,17,18 Based on these findings, some authors have suggested that minor thyroid dysfunction might contribute to significant changes in body weight that could represent a risk factor for overweight and obesity.19 However, these studies are inconclusive in establishing a cause–effect relationship, as the demonstration of a higher incidence of hypothyroidism in obese patients does not necessarily mean that the obesity is caused by the disorder. The relationship between hypothyroidism and obesity seems to be weaker than previously thought, even more in subjects with treated hypothyroidism.
In the hyperthyroidism patients group, weight gain was observed on completion of treatment when the results of the thyroid function test returned to normal. This is a common finding in the literature13,15,20,21 and there are several theories regarding it. Hyperthyroidism induces an increased basal energy expenditure that leads to weight loss as a result of a decrease in the body’s lean and fat mass. When euthyroidism is regained, weight gain occurs at the expense of both compartments.20 Another possible explanation for the tendency of hyperthyroid patients to gain weight after achieving euthyroidism could be related to an increase in post-treatment TSH levels over baseline levels. Hence, this would indicate the presence of relative hypothyroidism within the limits of analytic normality.14 In our study, we were unable to test this hypothesis because of unavailability of patients’ TSH levels prior to the onset of hyperthyroidism.
Our study has a number of limitations that should be taken into account. One of them is that due to the retrospective nature of the study, we could not access information on patients’ TSH levels and weight prior to their developing thyroid dysfunction. In the same line, other chemistry data (for example glucose and cholesterol) were not available. Another limitation to our study derives from the small number of patients finally included for analysis. Weight is a variable that can be influenced by multiple factors; due to this, more than 70% of the patients initially included had to be excluded because of confounding variables that could affect weight, specifically gestation and postpartum states, severe diseases and drugs with proven repercussion on weight. However, this aspect also minimized possible biases. The reason for the high volume of pregnant patients is that the study was conducted before having specific TSH ranges for pregnancy in our population, so we used the ATA ranges. In this context, more than a third of pregnant women were above the upper limit. Thereafter, the upper limit of TSH in pregnancy in our population was calculated resulting in 4 µU/mL, with the consequent fewer referrals. Otherwise, patients with stable mild chronic diseases were not excluded (for example, diabetic subjects well controlled with metformin). Another limitation is that composition body data were not recorded, nor by physical measurements like waist perimeter neither impedance techniques.
Conclusion
In conclusion, hypothyroid and hyperthyroid patients after treatment and normalization of thyroid function have statistically significant changes in BMI, but these do not show great relevance in clinical practice because the BMI remained in the overweight range in both groups.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Valdes S, Maldonado-Araque C, Lago-Sampedro A, et al. Population-based national prevalence of thyroid dysfunction in Spain and associated factors: diabetes study. Thyroid. 2017;27(2):156–166. doi: 10.1089/thy.2016.0353 [DOI] [PubMed] [Google Scholar]
- 2.Liu YY, Brent GA. Thyroid hormone crosstalk with nuclear receptor signaling in metabolic regulation. Trends Endocrinol Metab. 2010;21(3):166–173. doi: 10.1016/j.tem.2009.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Biondi B. Thyroid and obesity: an intriguing relationship. J Clin Endocrinol Metab. 2010;95(8):3614–3617. doi: 10.1210/jc.2010-1245 [DOI] [PubMed] [Google Scholar]
- 4.Karmisholt J, Andersen S, Laurberg P. Weight loss after therapy of hypothyroidism is mainly caused by excretion of excess body water associated with myxoedema. J Clin Endocrinol Metab. 2011;96(1):E99–E103. doi: 10.1210/jc.2010-1521 [DOI] [PubMed] [Google Scholar]
- 5.O´Malley B, Hickey J, Nevens E. Thyroid dysfunction-weight problems and the psyche: the patientes´perspective. J Hum Nutr Diet. 2000;13:243–248. doi: 10.1046/j.1365-277x.2000.00238.x [DOI] [Google Scholar]
- 6.Plummer WA. Body weight in spontaneous myxedema; in American Association for the Study of Goiter: transactions of the American Association for the Study of Goiter. Rochester West J Surg Obstet Gynecol. 1940;88–98. [Google Scholar]
- 7.Garber JR, Cobin RH, Gharib H, et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Thyroid. 2012;22(12):1200–1235. doi: 10.1089/thy.2012.0205 [DOI] [PubMed] [Google Scholar]
- 8.Amouzegar A, Kazemian E, Abdi H, et al. Association between thyroid function and development of different obesity phenotypes in euthyroid adults: a nine-year follow-up. Thyroid. 2018;28(4):458–464. doi: 10.1089/thy.2017.0454 [DOI] [PubMed] [Google Scholar]
- 9.Ross DS, Burch HB, Cooper DS, et al. 2016 American Thyroid Association Guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid. 2016;26(10):1343–1421. doi: 10.1089/thy.2016.0229 [DOI] [PubMed] [Google Scholar]
- 10.Nordyke RA, Glibert FI, Harada ASM. Graves´ disease. Influence of age on clinical findings. Arch Interm Med. 1988;148:626–631. doi: 10.1001/archinte.1988.00380030132023 [DOI] [PubMed] [Google Scholar]
- 11.Vanderpump MP, Tunbridge WM. The epidemiology of thyroid diseases In: Braverman LE, Utiger RD, editors. The Thyroid: A Fundamental and Clinical Text. 8th ed. Philadelphia: Lippincott Williams and Wilkins; 2000:467. [Google Scholar]
- 12.Jonklaas J, Nsouli-Maktabi H. Weight changes in euthyroid patients undergoing thyroidectomy. Thyroid. 2011;21(12):1343–1351. doi: 10.1089/thy.2011.0054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rathi MS, Miles JN, Jennings PE. Weight gain during the treatment of thyrotoxicosis using conventional thyrostatic treatment. J Endocrinol Invest. 2008;31(6):505–508. doi: 10.1007/BF03346398 [DOI] [PubMed] [Google Scholar]
- 14.Hoermann R, Midgley J. TSH measurement and its implications for personalised clinical decision-making. J Thyroid Res. 2012;2012:1–9. Art. ID 438037. doi: 10.1155/2012/438037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Crocker MK, Kaplowitz P. Treatment of paediatric hyperthyroidism but not hypothyroidism has a significant effect on weight. Clin Endocrinol (Oxf). 2010;73:752–759. doi: 10.1111/j.1365-2265.2010.03877.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Verma A, Jayaraman M, Kumar HKVS, Modi KD. Hypothyroidism and obesity: cause or effect? Saudi Med J. 2008;29(8):1135–1138. [PubMed] [Google Scholar]
- 17.Mamtani M, Kulkarni H, Dyer TD, et al. Increased waist circumference is independently associated with hypothyroidism in Mexican Americans: replicative evidence from two large, population-based studies. BMC Endocr Disord. 2014;14(46):1–13. doi: 10.1186/1472-6823-14-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Moura Souza A, Sichieri R. Association between serum TSH concentration within the normal range and adiposity. Eur J Endocrinol. 2011;165:11–15. doi: 10.1530/EJE-11-0261 [DOI] [PubMed] [Google Scholar]
- 19.Reihner T. Obesity and thyroid function. Mol Cell Endocrinol. 2010;316:165–171. doi: 10.1016/j.mce.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 20.Greenlund LJ, Nair KS, Brennan MD. Changes in body composition in women following treatment of overt and subclinical hyperthyroidism. Endocr Pract. 2008;14(8):973–978. doi: 10.4158/EP.14.8.973 [DOI] [PubMed] [Google Scholar]
- 21.Dutta P, Bhansali A, Walia R, Khandelwal N, Das S, Masoodi SR. Weight homeostasis and its modulators in hyperthyroidism before and after treatment with carbimazole. Indian J Med Res. 2012;136:242–248. [PMC free article] [PubMed] [Google Scholar]