Abstract
Aim
Fluorine-18-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) become an important tool in oncology by combining the metabolic information from 18F-FDG PET with the morphological information of CT. The main objective of this study was to assess the diagnostic value of PET/CT in patients with differentiated thyroid carcinoma (DTC).
Material and Methods
We analyzed 173 PET/CT scans of patients with DTC presenting elevated thyroglobulin (Tg) levels, negative Tg-antibodies levels, negative Iodine-131 whole-body scanning (I-131 WBS) and without any signs of clinical or other imaging technique for tumor recurrence/metastases.
Results
PET/CT scans were positive in 38% of cases (65/173). The sensitivity, specificity, positive predictive values and the accuracy of PET/CT imaging were 88.09%, 98.6%, 93.1% respectively 96.53%. After the PET/CT scan 29 patients underwent surgery, 24 of them continued radio-iodine therapy, 5 patients initiated tyrosine kinase inhibitors treatment and external radiotherapy.
Conclusion
18F-FDG PET/CT is a valuable imaging technique which has the capability of identifying those cases of thyroid recurrence/metastases with elevated Tg levels and negative I-131 WBS. The treatment strategy was changed in 89.2% cases of positive PET/CT scans which shows us that 18F-FDG PET/CT imaging should be integrated into the follow-up programs for DTC patients.
Keywords: 18F-FDG, Differentiated thyroid carcinoma, PET/CT
INTRODUCTION
Differentiated thyroid cancer is generally characterized by a good prognosis and continues to be the most frequent endocrine cancer. The incidence of thyroid cancer is one of the most rapidly increasing in human cancers, especially in the last decade, but despite this situation, it is still considered to be one of the rare cancers (1,2). Different diagnostic methods allow for an accurate diagnosis of the disease and an effective treatment can be achieved, which means an excellent prognosis for these patients.
Differentiated thyroid carcinoma (DTC) is usually represented by a papillary and follicular pattern and it has a very good prognosis with an overall risk of relapse which never exceeds 20% (3, 4).
According to the European Thyroid Association (ETA), American Thyroid Association (ATA), National Cancer Comprehensive Network (NCCN) and other professional associations involved in this pathology, the treatment for patients with DTC starts with thyroidectomy and then depending on the histology, tumour size, tumour invasion of locoregional tissues or structures, local or distant metastases, the treatment continues with radioiodine (RAI) therapy or external beam radiation therapy.
The aim of RAI therapy with Iodine-131 (I-131) is to ablate the thyroid remnant tissue, suspected micro-metastases or persistent disease. Post-treatment I-131 whole-body scanning (WBS) has an important role in the therapeutic management of the patient. WBS is strongly recommended to be performed several days later in order to highlight the I-131 uptake because 25% of imaging shows clinically important lesions which cannot be detected by other imaging methods. Its sensitivity and specificity in demonstrating the residual disease and recurrence are 50-90% respectively 80-100% (5–7).
It is known that 1/3 of metastatic DTC is cured, but the remaining challenging problems are the patients with RAI-refractory disease (RAIRD). It occurs in less than 5% of patients and progressive dedifferentiation of DTC take place by loss of the sodium iodine symporter which is required for the iodine uptake (8–10).
The early diagnostic process of RAIRD is very important for avoiding unnecessary RAI therapy and to make a precise analysis if systematic therapy is appropriate in order to obtain a good balance between overall survival and quality of patient’s life. According to ATA 2015, tyrosine kinase inhibitors are considered the first line systemic therapy, but their use in clinical practice requires a rigorous selection of patients due to their severe adverse effect that deteriorates patients’ quality of life.
The follow-up of patients with DTC after surgery RAI treatment consists in measurements of serum thyroglobulin (Tg), Tg antibodies (anti-Tg), in thyrotropin (TSH) stimulated conditions, neck ultrasound (US) and whole-body scan with 131I (WBS).
Serum Tg is the only tumour marker required and recognized as necessary in assessing this pathology. Normally, in conditions of stimulated TSH and negative anti-Tg, the value of Tg should be undetectable and the only source of positive values is the presence of thyroid parenchymal cells suggesting the metastatic thyroid tissue or normal tissue. According to several published data, the positive predictive value of this marker is 100% and the negative predictive value is 76%. Thus, Tg has become an extremely important marker in monitoring DTC (4,11).
Ultrasonography (US) is the simplest and non-invasive method in the assessment of recurrent thyroid disease. There are studies which demonstrate that US should be considered the first diagnostic choice to investigate the local recurrence and lymph nodes metastases (5,12,13).
The changes in aggressiveness of DTC require a special attention for those patients with positive Tg levels in conditions of stimulated TSH, with no clinical or imaging tests of persistent or recurrent disease. In these cases, Fluorine-18 Fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) should be considered.
Normally 18F-FDG PET/CT is not a standard follow-up evaluation method in DTC patients and there is a well-defined situation where 18F-FDG PET/CT plays an important role, so-called TENIS (Tg Elevated and Negative I-131 WBS). In the latest years, 18F-FDG PET/CT has become a valuable tool in oncology by combining the metabolic information from FDG PET with the morphologic resolution of CT.
A positive 18F-FDG PET/CT scan can indicate a poor histological prognosis for the tumour, and the level of the FDG uptake shows the dedifferentiation process which means that the therapeutic management of the patient must be reconsidered (14).
The aim of this study was to assess the value of 18F-FDG PET/CT in restaging DTC patients and to estimate the association of Tg with FDG uptake and other risk factors. The possibility to change the therapeutic management of these patients from our country motivated more this work.
MATERIAL AND METHODS
Around 1370 patients with DTC were treated with RAI therapy in the Nuclear Medicine Department of “Prof. Dr. Ion Chiricuta” Oncological Institute Cluj-Napoca between 2015-2016.
We analyzed retrospectively 173 patients with histopathologically confirmed DTC after total thyroidectomy and RAI therapy, for this period of 2 years.
Informed consent was obtained from all participants included in the study, as in our institution all patients sign an informed consent to the processing of data for scientific purposes. Ethical approval from the institutional review board was not necessary because this is a retrospective study.
Inclusion criteria for 18F-FDG PET/CT studies were: DTC radically treated, elevated Tg levels in TSH stimulated conditions and negative I-131 WBS. Serum Tg and Anti-Tg levels were determined by the immunochemical method by electrochemiluminescence (Tg normal values:3.5-77 ng/mL and <0.04 ng/mL for patients with total thyroidectomy; Anti-TgAb normal values: <115 Ul/mL ). Patients with high anti-Tg levels were excluded from this study.
The mean age of the patients was 51.33 ±14.42 (14 – 81). 67% (n = 116) were females and 33% (n = 57) were males, with a female/male ratio of 2.03.
According to the histopathological findings, 79% (n=136, including 43 cases of follicular variant, 12 cases of sclerosing variant and 7 cases of trabecular variant) were papillary carcinoma and 21% (n= 37, including 12 cases of oncocytic variant and 4 cases of insular carcinoma) were follicular carcinoma.
The patients’ treatments started with total thyroidectomy ± cervical lymph nodes dissection followed-up by RAI therapy.
The opportunity and the doses for RAI therapy are established by a thyroid committee according to the stage and risk group.
The patients were followed up by serum Tg and Anti-Tg levels, by neck US and CT when necessary.
Over the followed-up period patients received additional therapeutic doses of I-131 (1-11 times) and WBS were performed at 24-48 hours after RAI therapy, using a single head Siemens Gamma Camera equipped with a high energy collimator. If there was no abnormal uptake of the images, results were accepted as negative.
All patients who presented elevated Tg levels (>1 ng/mL) after TSH stimulation and negative I-131 WBS, without any signs of clinical or other imaging methods (CT, US) of tumour recurrence were referred for 18F-FDG PET/CT scan.
18F-FDG PET/CT protocol
18F-FDG PET/CT studies were performed after a fasting period of 6 hours. The blood glucose levels between 70 mg/dL – 150 mg/dL were measured before the FDG injection, a special attention has been payed to diabetic patients and the insulin has been administered at least 4 hours prior to 18F-FDG injection.
Injected doses of 185 – 600mBq 18F-FDG were calculated according to the patients’ weight and to the EANM procedure guidelines for tumour imaging, version 2.0. Images were acquired with a GE Optima 560 PET/CT with a BGO (Bismuth Germanium Oxide) detector and 16 slices CT, after an uptake period of 60 – 90 minutes. Non-contrast images and PET data were acquired in supine position from the vertex to the middle part of the femur, with arms raised above the head. CT images, with a slice thickness of 3.75mm, were acquired using a low – dose protocol (100-120kV, 50 – 100 auto mA, index noise of 20%) in order to reduce irradiation dose for patients. PET data were acquired in 3D mode with a time of 2.5 minutes/bed. Data were reconstructed using the iterative technique OSEM (ordered subsets expectation maximization) with 2 iterations and 16 subsets.
Coronal, axial and sagittal PET/CT images were evaluated by a team formed from a nuclear medicine physician and a radiologist. All abnormal FDG findings were correlated with other imaging methods (neck US, CT, and MRI), Tg levels and clinical examination of the patients. For all PET/CT studies, SUVlBm (the standardized uptake value lean body mass) was used as a semi-quantitative parameter for 18F-FDG uptake calculation respecting a standard protocol on the workstation (Volumetrix for PET/CT).
For the statistical analyses, we used Statistical Analysis for Social Science 13.0 (SPSS) program. Tumours detecting rates were expressed as the percentage of patients with positive lesions. We expressed qualitative data as percentage and number respectively semi-quantitative data as mean with ranges. In order to describe the continuous data, we used the minimum (min) and maximum (max) values. Pearson’s Chi-square test was used for the comparison of normally distributed parameters and Spearman’s rho Correlation Coefficient was used for non-normally distributed parameters. We considered significant P < 0.05.
RESULTS
According to 18F-FDG PET/CT studies, 38% (n=65) of patients presented abnormal metabolic findings suggesting metastatic or/and local recurrence disease; among them, 60% (n = 39) were females and 40% (n = 26) were males. Regarding the histology, 64% of patients were diagnosed with papillary thyroid carcinoma (n = 42, including 5 cases of sclerosing variant and 2 cases of trabecular), 11% had follicular thyroid carcinoma (n = 7, including 2 cases of insular variant and 2 cases of oncocytic variant) and 25% (n = 16) of patients with combined follicular – papillary type of thyroid carcinoma.
Risk factors of these patients group with positive 18F-FDG PET/CT results were analysed through Pearson Chi-squared and Odds ratio and the presence of initial distant metastases was the most important factor affecting a true positive result and they were statistically significant (p<0.05). Sex, lymph nodes metastases, advanced tumour stages (pT3, pT4) and type of tumour were not statistically significant, but there was an estimated risk in the case of sex; males present a higher risk for a true positive result than females and follicular - papillary carcinoma presents a higher risk for true positive results than other histological types.
All the patients were treated with RAI therapy before the 18F-FDG PET/CT scan. Number of I-131 doses ranged from 1 to 11 with a mean of 3.84 ±2.25 and a median of 3. The mean for administered I-131 activities was 300.14 mCi ± 203.7 and the median was 246.61 mCi.
The mean Tg levels of patients presenting signs of recurrence/metastases on PET/CT were 1032.16 ± 4355.86 (1.26 – 32727.0), in the cases without recurrence/metastases on PET/CT the mean Tg levels were 101.56 ± 376.305 (1.06 – 2896.0). Tg levels were found to be considerably lower in cases without recurrence/metastases on PET/CT relatively into Tg levels with recurrence/metastases.
The mean for SUVlbm value was 8.02 (2.55 – 37.20, median: 5.29). The Spearman’s rho Correlation Coefficient between SUVlbm and Tg levels showed a direct proportional linear correlation but not statistically significant (r=0.103, p=0.413 > 0.05).
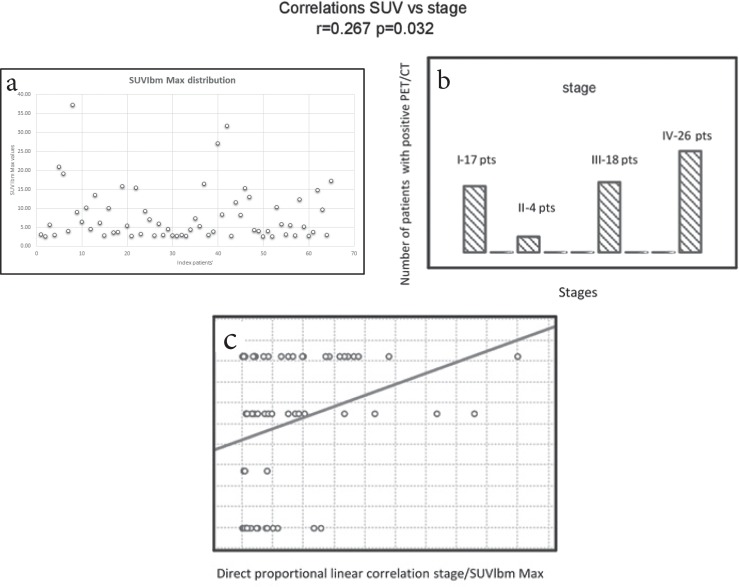
The Spearman’s rho Correlation Coefficient between SUVlbm and patients’ stage correlated significantly (r = 0.267, p = 0.032 <0.05) and showed a direct proportional linear correlation (Fig. 1). 68% of patients with recurrence/metastases on PET/CT were in stages III and IV (n = 44) and 32% were in stages I and II (n = 21) which means that patients in advanced stages showed higher values for SUVlbm. The Spearman’s rho Correlation Coefficient between the initial presence of lymph nodes metastases and SUVlbm was also analysed, and there were no statistically significant findings between these 2 parameters.
Figure 1.
The Spearman’s rho Correlation Coefficient between SUVlbm and patients’ stage a-SUVlbm; b-number of patients in different stages (I,II,III and IV); c- liniar correlation.
18F-FDG PET/CT studies revealed local recurrence and cervical and mediastinal lymph nodes in 58 cases. Pulmonary metastases were also associated in 5 cases, bone metastases in 3 cases (one patient presented 2 foci and 2 of them presented multiple bone metastases and tumour invasion in the soft parts of the abdomen), and 2 cases presented liver metastases.
From the study group of patients with recurrence/metastases on PET/CT, 44% (n= 29) of them underwent surgery in order to remove the abnormal metabolic findings, of which 27 (93%) cases were histopathologically confirmed true positive (tumour recurrence, lymph nodes metastases and bone metastases). For the 2 cases, false positive, the histopathological report was negative and they continued to be followed-up in time. According to ATA guidelines different therapeutic strategies may be approached, including TKI therapy.
Taking into consideration different criteria like SUVlbm value, Tg levels, the clinical history of patients, 37% (n = 24) of them continued the RAI therapy, 11% (n = 7) of patients were followed-up only clinically and radiologically (neck US, CT, MRI), 5% (n= 3) of cases were referred for TKI treatment and 3% (n = 2) of them initiated external radiotherapy.
For the study group of 173 patients the sensitivity, specificity, PPV, NPV, and the accuracy of PET/CT examinations are presented in Table 1.
Table 1.
Statistic indices for the evaluation of 18F – FDG PET/CT
| Sensitivity | Specificity | PPV | NPV | Accuracy |
| 88.09% | 98.6% | 93.1% | 97.2% | 96.53% |
PPV – positive predictive value, NPV – negative predictive value
DISCUSSION
Elevated Tg levels indicate the recurrence or metastases, and I-131 WBS scans are able to localize the tumour. In those situations where I-131 WBS are negative, other imaging techniques, neck US, CT, MRI, are used to localize the recurrent disease. Those three methods are used to locate the anatomical abnormalities, while PET reveals the metabolic abnormalities (15). Therefore combined functional and anatomical imaging techniques can improve the ability to detect recurrence and metastatic disease.
The most common indications for 18F-FDG PET/CT scan in thyroid carcinoma are the positive Tg levels, but negative I-131 WBS and neck US (2,16). There are studies where F18-FDG PET/CT has a good accuracy in the situation of elevated Tg antibodies levels but in this study, we took into consideration only the main indication for PET/CT.
In our study of 173 patients with negative I-131 WBS and elevated Tg levels, we found that 38% (65/173) of patients presented abnormal findings on 18F-FDG PET/CT. The treatment strategy was changed in 89.2% (58/65) cases of positive PET/CT scan and in 33.5% (58/173) cases for the entire study group. In a literature review regarding clinical indications and controversies of 18F-FDG PET/CT, Salvatori et al. emphasize the fact that the management changes could include the avoidance of surgical procedures or biopsies, further workup with imaging studies or initiation of unnecessary treatment such as external beam therapy or TKI therapy in the cases of advanced disease. In the same paper, it is mentioned that positive 18F-FDG PET/CT findings change the patient management in 20-40% of cases (16).
Taking into consideration the results of our study, we have shown that F18-FDG PET/CT is a useful method in detecting tumour recurrence or other metastases despite the fact that we did not find a statistically significant correlation between Tg levels and SUVlbm and just a direct proportional linear correlation was associated, we found a correlation between SUVlbm and the initial stage of patients which leads to the idea that patients with stage III and IV need special requirements in their follow-up program because of their higher risk of recurrence.
High metabolic activity highlighted on 18F-FDG PET/CT is associated with a poorly differentiated follicular cell which has lost the ability to concentrate RAI and progressively enhance glucose metabolism due to the high cell activity; in this way PET/CT became a powerful diagnostic method of investigation for undifferentiated lesions. In our study, the cases of aggressive variants such as insular, diffuse sclerosing variants of papillary or follicular Hurthle cell carcinoma was rare, and that is why only a number of 5 patient were referred for external radiation beam and TKI therapy.
Even if the 18F-FDG PET/CT studies were performed under optimal conditions there are a high number of negative studies despite the elevated Tg levels. According to Robbins et al. these categories of patients should be integrated into a group of patients where the lack of FDG uptake is related to a lower aggressiveness and slow progression of the disease (17,18). In our study, the patients with negative 18F-FDG PET/CT scans continue to be followed-up and medical decisions were adopted according to the medical history of each patient.
In conclusion, in the opinion of the authors, 18F-FDG PET/CT imaging has the capability of identifying cases of tumour recurrence/metastases in the situations where other imaging methods are negative, including I-131 WBS and elevated Tg levels. Otherwise, this study showed that 18F-FDG PET/CT uptake was associated with advanced stages of the disease and the clinical management was changed in 89.2% cases of positive PET/CT scan which leads to the idea that 18F-FDG PET/CT imaging should be integrated into the follow-up programs of patients with DTC.
Conflict of interest
No author has any potential conflict of interest associated with this research.
References
- 1.Piciu D, Irimie A. Nuclear Endocrinology. Springer International Publishing AG 2012; 2012. Nuclear endocrinology; pp. 1–239. [Google Scholar]
- 2.Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, Pacini F, Randolph GW, Sawka AM, Schlumberger M, Schuff KG, Sherman SI, Sosa JA, Steward DL, Tuttle RM, Wartofsky L. 2015 American Thyroid Association Management. 2016;26(1):1–133. doi: 10.1089/thy.2015.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matteis G De, Raddi M, Fonti R, Pellegrino T. Prognostic role of FDG PET/CT in patients with differentiated thyroid cancer treated with 131-iodine empiric therapy. Med. 2017:1–6. doi: 10.1097/MD.0000000000008344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Irimie A. Surgery of Thyroid Tumors Practical Guide(in Romanian) Chirurgia tiroidei tumorale - Ghid practic. 2006:71–74. [Google Scholar]
- 5.Aslan A, Sancak S, Aslan M, Ayaz E, Inan I, Ozkanli SS, Alimoglu O, Yikilmaz A. Diagnostic Value of Duplex Doppler Ultrasound Parameters in Papillary Thyroid Carcinoma. Acta Endocrinologica-Bucharest. 2018;14(1):43–48. doi: 10.4183/aeb.2018.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haugen BR, Lin EC. Isotope imaging for metastatic thyroid cancer. Endocrinol Metab Clin North Am. 2001;30(2):469–492. doi: 10.1016/s0889-8529(05)70195-x. [DOI] [PubMed] [Google Scholar]
- 7.Hoang JK, Sosa JA, Nguyen X V., Galvin PL, Oldan JD, Imaging Thyroid Disease Updates, Imaging Approach, and Management Pearls. Radiol Clin North Am. 2015;53(1):145–161. doi: 10.1016/j.rcl.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 8.Gild ML, Topliss DJ, Learoyd D, Parnis F, Tie J, Hughes B, Walsh JP, McLeod DSA, Clifton-Bligh RJ, Robinson BG. Clinical guidance for radioiodine refractory differentiated thyroid cancer. Clin Endocrinol (Oxf) 2018;88(4):529–537. doi: 10.1111/cen.13508. [DOI] [PubMed] [Google Scholar]
- 9.Cooray SD, Topliss DJ. The management of metastatic radioiodine-refractory differentiated thyroid cancer requires an integrated approach including both directed and systemic therapies. Endocrinol Diabetes Metab Case Reports. 2017;2017(1):1–7. doi: 10.1530/EDM-16-0089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lin Y, Wang C, Gao W, Cui R, Liang J. Overwhelming rapid metabolic and structural response to apatinib in radioiodine refractory differentiated thyroid cancer. Oncotarget. 2017;8:42252–42261. doi: 10.18632/oncotarget.15036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Groen AH, Klein Hesselink MS, Plukker JT, Sluiter WJ, van der H-S, AN, Brouwers AH, Lentjes EG, Muller Kobold AC LT. Additional value of a high sensitive thyroglobulin assay in the follow-up of patients with differentiated thyroid carcinoma. Clin Endocrinol (Oxf) 2017;86(3):419–424. doi: 10.1111/cen.13180. [DOI] [PubMed] [Google Scholar]
- 12.Moslehi M, Assadi M. Contribution of ultrasound examination in the detection of neck recurrence in low-risk differentiated thyroid carcinoma patients at first follow-up visits. Nucl Med Rev. 2014;17(1):3–6. doi: 10.5603/NMR.2014.0002. [DOI] [PubMed] [Google Scholar]
- 13.Anand N, Chaudhary N, Mittal MK, Prasad R. Comparison of the efficacy of clinical examination, ultrasound neck and computed tomography in detection and staging of cervical lymph node metastasis in head and neck cancers. Indian J Otolaryngol Head Neck Surg. 2006;59(1):19–23. doi: 10.1007/s12070-007-0005-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Piciu D, Irimie A, Duncea I, Popita V, Straciuc O, Pestean C, Piciu A, Bara A. Positron Emission Tomography - Computer Tomography Fusion Image, with 18-Fluoro-2-Deoxy-D-Glucose in the Follow-Up of Patients with Differentiated Thyroid Carcinoma. Acta Endocrinologica-Bucharest. 2010;6(1):15–26. [Google Scholar]
- 15.Kim TY, Kim WG, Kim WB, Shong YK. Current Status and Future Perspectives in Differentiated Thyroid Cancer. Endocrinol Metab. 2014;29(3):217–225. doi: 10.3803/EnM.2014.29.3.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salvatori M, Biondi B, Rufini V. Imaging in endocrinology: 2-[18F]-fluoro-2-deoxy-D-glucose positron emission tomography/computed tomography in differentiated thyroid carcinoma: clinical indications and controversies in diagnosis and follow-up. Eur J Endocrinol. 2015;173(3):R115–130. doi: 10.1530/EJE-15-0066. [DOI] [PubMed] [Google Scholar]
- 17.Robbins RJ, Wan Q, Grewal RK, Reibke R, Gonen M, Strauss HW, Tuttle RM, Drucker W, Larson SM. Real-time prognosis for metastatic thyroid carcinoma based on 2-[18F]fluoro-2-deoxy-D-glucose-positron emission tomography scanning. J Clin Endocrinol Metab. 2006;91(2):270–272. doi: 10.1210/jc.2005-1534. [DOI] [PubMed] [Google Scholar]
- 18.Kukulska A, Krajewska J, Kołosza Z, Paliczka-Cies Lik E, Puch Z GE, Król A, Kalemba M, Kropin Ska A JB. The role of FDG-PET in localization of recurrent lesions of differentiated thyroid cancer (DTC) in patients with asymptomatic hyperthyroglobulinemia in a real clinical practice. Eur J Endocrinol. 2016;175(5):379–385. doi: 10.1530/EJE-16-0360. [DOI] [PubMed] [Google Scholar]