Abstract
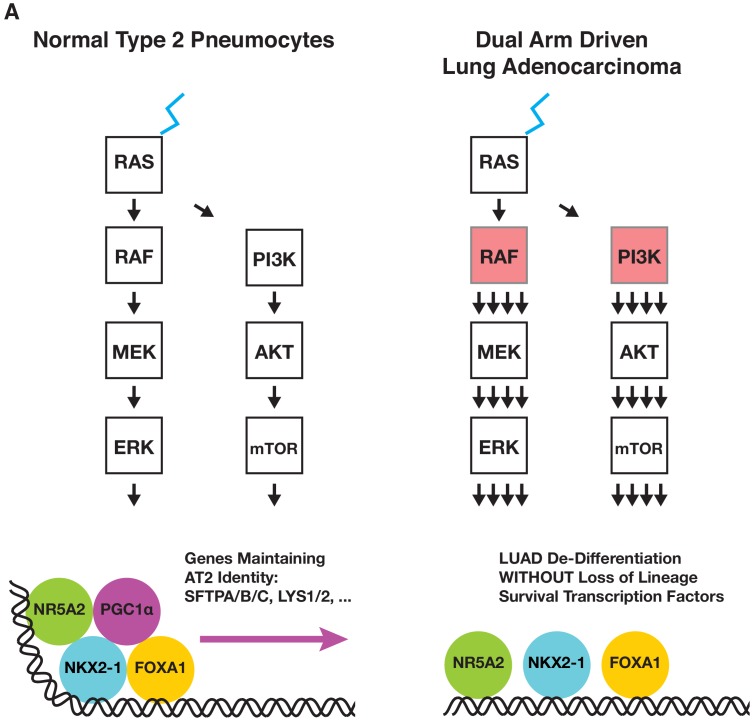
Human lung adenocarcinoma exhibits a propensity for de-differentiation, complicating diagnosis and treatment, and predicting poorer patient survival. In genetically engineered mouse models of lung cancer, expression of the BRAFV600E oncoprotein kinase initiates the growth of benign tumors retaining characteristics of their cell of origin, AT2 pneumocytes. Cooperating alterations that activate PI3’-lipid signaling promote progression of BRAFV600E-driven benign tumors to malignant adenocarcinoma. However, the mechanism(s) by which this cooperation occurs remains unclear. To address this, we generated mice carrying a conditional BrafCAT allele in which CRE-mediated recombination leads to co-expression of BRAFV600E and tdTomato. We demonstrate that co-expression of BRAFV600E and PIK3CAH1047R in AT2 pneumocytes leads to rapid cell de-differentiation, without decreased expression of the transcription factors NKX2-1, FOXA1, or FOXA2. Instead, we propose a novel role for PGC1α in maintaining AT2 pneumocyte identity. These findings provide insight into how these pathways may cooperate in the pathogenesis of human lung adenocarcinoma.
Research organism: Mouse
eLife digest
Cancers appear when changes in the genetic information of a cell, also called mutations, allow it to multiply uncontrollably. The disease we know as “lung cancer” kills more people than any other cancer, but this term actually refers to different types of tumors that appear because of various mutations that happen in different kinds of lung cells.
To complicate matters further, as lung cancer cells become more aggressive, they can stop appearing and behaving like the type of lung cell they came from. Yet, knowing the exact origin of the cancer is key, since it determines which treatment will work best to stop the disease in its tracks.
Despite these differences, many lung cancer cells contain mutations that over-activate two molecular cascades called the MAP kinase and the PI3’-kinase pathways. Under normal conditions, these signaling pathways relay external messages to the inside of the cell, where they help cells multiply. Two separate mutations can respectively over-stimulate either the MAP kinase or the PI3’-kinase pathway, but it was unclear how these could work together to start and maintain aggressive lung tumors. Another unanswered question was how these cancer cells lose the characteristics of the healthy cells they came from.
To address these issues, van Veen et al. genetically engineered mice that carry a mutation which activates the MAP kinase pathway. The lung cells with this genetic change also made a red fluorescent protein that marked cancer cells, so that these could be separated from the rest of the lung and analyzed.
This revealed that cells with only the MAP kinase mutation turned into small and benign tumors that began in lung cells, known as “type 2” cells. The PI3’-kinase mutation alone could not even start a tumor. However, together the mutations made tumors much more aggressive. Cells that carried both mutations also stopped producing proteins normally made by type 2 cells, therefore causing the cells to lose their original identity.
The mice created by van Veen et al. could help to understand how lung cancers develop in these animals and also in human lung cancer patients. Ultimately, this information could be used to design new cancer treatments, especially since both the MAP kinase and PI3’-kinase pathways contain many proteins that can be targeted with drugs.
Introduction
Non-small cell lung cancer (NSCLC) is the leading cause of cancer-related death, with lung adenocarcinoma (LUAD) being the most common NSCLC subtype (Siegel et al., 2016). Due to the morbidity and mortality associated with LUAD, there is an urgent need to better characterize how key genetic drivers contribute to the pathogenesis of this disease. To that end, since the original discovery of KRAS mutations in human lung cancer cells (Capon et al., 1983), it has emerged that ~75% of LUADs display mutational activation of key components of receptor tyrosine kinase (RTK) signaling that, in turn, promote activation of RAS and its key downstream effectors: the RAF→MEK→ERK→MAP kinase (MAPK) and the PI3’-lipid pathways (Cancer Genome Atlas Research Network, 2014; Heist and Engelman, 2012). Moreover, mutational activation of RTKs or downstream signaling proteins (e.g. EGFR/ERBB1, ALK, ROS1, NTRK, BRAF) serve as predictive biomarkers for the clinical deployment of FDA-approved inhibitors of these oncoprotein kinases for the treatment of genetically-defined subsets of lung cancer (Drilon et al., 2018; Hyman et al., 2015; Rosell et al., 2012; Scagliotti et al., 2010; Shaw et al., 2013; Shaw et al., 2014).
Mutational activation of BRAF occurs in ~8% of LUAD, with the most common single mutation (BRAFT1799A) encoding the BRAFV600E oncoprotein kinase (Cancer Genome Atlas Research Network, 2014). To model BRAFV600E driven cancers, we previously described BrafCA mice carrying a CRE-activated allele of Braf that expresses normal BRAF prior to CRE-mediated recombination, after which BRAFV637E (orthologous to human BRAFV600E and for simplicity henceforth referred to as BRAFV600E), is expressed from the endogenous chromosomal locus (Dankort et al., 2007). This mouse has proven useful in modeling many cancer types in which BRAFV600E is implicated as a driver oncoprotein (Charles et al., 2011; Dankort et al., 2009; Sakamoto et al., 2017; Trejo et al., 2013; Wang et al., 2012). Taken together, these studies indicate that BRAF mutation serves as a foundational initiating event for tumorigenesis in many target tissues. However, the progression of benign tumors initiated by BRAFV600E expression into malignant cancer invariably requires additional events such as silencing of tumor suppressors (e.g. INK4A-ARF, TP53, PTEN, CDX2) or activation of cooperating oncogenes (PIK3CA, CTNNB1, c-MYC) (Charles et al., 2014; Dankort et al., 2007; Dankort et al., 2009; Huillard et al., 2012; Juan et al., 2014; Sakamoto et al., 2017; Trejo et al., 2013; Tsao et al., 2004; Yu et al., 2009).
In mouse models of lung carcinogenesis, there are key similarities between the early stages of tumorigenesis observed in response to expression of either the KRASG12D or BRAFV600E oncoproteins (Dankort et al., 2007; Trejo et al., 2012). While tumors initiated by BRAFV600E remain as benign adenomas with certain features of senescence (Dankort et al., 2007; Jackson et al., 2001), a proportion of KRASG12D initiated lung tumors progress to frank adenocarcinomas within six months, most likely due to the ability of KRASG12D to activate the PI3’-kinase signaling pathway (Castellano et al., 2013; Murillo et al., 2018; Rodriguez-Viciana et al., 1994; Vivanco and Sawyers, 2002; Yuan and Cantley, 2008). Consistent with this hypothesis, co-expression of BRAFV600E and PIK3CAH1047R, a mutationally-activated form of PI3’-kinase-α (PI3Kα), in AT2 pneumocytes leads to rapid growth of lung tumors, many of which display progression to frank malignancy bearing various hallmarks of the cognate human disease (Kinross et al., 2012; Trejo et al., 2013). Thus, these genetically manipulated mice provide a unique opportunity to genetically and biochemically separate and analyze the effects of activation of these two critical downstream arms of RTK→RAS signaling individually or in combination.
Whereas the original BrafCA mouse allowed insights into cancer initiation, progression and therapy, there remain many questions that this mouse is inadequately configured to address. For example, it is not trivial to identify and isolate pure populations of tumor cells without significant stromal contamination, particularly in contexts when tumor cells are rare, such as in the earliest stages of tumorigenesis, or in the context of minimal residual disease following pathway-targeted inhibition of BRAFV600E signaling (Dankort et al., 2007). To address these issues we and others have used mice carrying CRE-activated alleles that express fluorescent proteins, such as the mT-mG allele in which the activity of CRE recombinase silences the expression of tdTomato and elicits expression of EGFP (Muzumdar et al., 2007). However, this approach is confounded by the observation that not all cells expressing the desired oncoprotein also express EGFP and vice versa.
In order to unequivocally identify BRAFV600E expressing cells we have generated BrafCAT mice carrying a new CRE-activated Braf allele. Like the original BrafCA allele, BrafCAT encodes normal BRAF prior to CRE-mediated recombination, after which the recombined allele expresses a bicistronic BrafT1910A-P2A-tdTomato mRNA encoding both BRAFV600E and the red fluorophore tdTomato. Moreover, here we report the use of BrafCAT mice to explore the cooperation of oncogenic BRAFV600E and PI3KαH1047R in lung carcinogenesis in greater mechanistic detail. In brief, BRAFV600E-driven lung tumors maintain expression of markers of AT2 identity, including the known regulators of AT2 identity, NKX2-1, FOXA1, and FOXA2 (Bruno et al., 1995; Camolotto et al., 2018; DeFelice et al., 2003; Hamvas et al., 2013; Lazzaro et al., 1991; Minoo et al., 1995; Snyder et al., 2013; Stahlman et al., 1996; Winslow et al., 2011; Yuan et al., 2000). By contrast, co-expression of BRAFV600E and PI3KαH1047R leads to development of lung tumors that show variable and widespread loss of expression of markers of AT2 pneumocyte terminal differentiation including the well-characterized surfactant proteins, SFTPA, SFTPB, and SFTPC. Notably reduced expression of AT2 markers begins early in tumor development and occurs despite sustained NKX2-1, FOXA1, and FOXA2 expression in tumor cells. Hence, these data shed light on the mechanisms by which pathways that cooperate in lung tumorigenesis also cooperate to influence the differentiation state of tumor cells. Indeed, these findings bear similarity to observations in human lung adenocarcinomas in which poorly differentiated and metastatic cancers often show loss of expression of functional markers of lung identity despite maintaining expression of NKX2-1 (Yatabe et al., 2002). Consequently, our results may shed light on our understanding of human lung cancer progression and how normal lung epithelial cells may lose their differentiation status following activation of cooperating oncogenic pathways.
Results
Generation of BrafCAT mice
To generate a reporter of BRAFV600E oncoprotein expression, we linked its expression to the expression of the red fluorophore, tdTomato. To accomplish this, we made use of the design of the original BrafCA allele, in which the modified exon 18 and the remainder of the Braf allele is not transcribed prior to the action of CRE recombinase (Dankort et al., 2007) due to the insertion of a triple polyadenylation/mRNA transcription termination signal from SV40 (Figure 1A) (Srinivas et al., 2001). Consequently, we designed a targeting vector containing the final coding exon (22) of mouse Braf in which the stop codon was removed, followed by sequences encoding: 1. an in-frame glycine-serine-glycine-P2A self-cleaving peptide; 2. sequences encoding a membrane-tethered tdTomato-CAAX protein and; 3. a PGK-PURO selectable marker flanked by Frt sites for subsequent removal by FLP recombinase. Following electroporation of this construct into 2H1 BrafCA/+ ES cells, from which the original BrafCA mice were generated, 288 puromycin resistant clones were selected and screened by PCR for homologous recombination of the construct into the distal end of the BrafCA allele (Dankort et al., 2007). However, because the targeted ES cells are heterozygous for both normal Braf and the genetically manipulated BrafCA allele, and because there was no way to direct homologous recombination of the targeting vector to the previously targeted BrafCA allele, we expected to target both homologues. Because BRAF is expressed in ES cells, we reasoned that modification of the normal allele would lead to ES cells with constitutive tdTomato-CAAX expression. Indeed, ~50% of PCR positive ES cell clones displayed constitutive membrane associated red-fluorescence and were used to generate BrafTOM mice, in which tdTomato serves as a marker for any cells expressing normal BRAF (van Veen et al., 2016). By contrast, homologous recombination of the targeting vector into the BrafCA allele should give rise to ES cells that do not express tdTomato due to the strong transcriptional termination signal. However, upon the addition of a cell permeable TAT-CRE protein to these cells, they should initiate the expression of both BRAFV600E and tdTomato (Figure 1B). Hence, this in vitro strategy allowed us to both identify appropriately targeted BrafCAT/+ ES cells and also indicated the appropriate functioning of the BrafCAT allele in response to CRE-mediated recombination prior to the generation of mice.
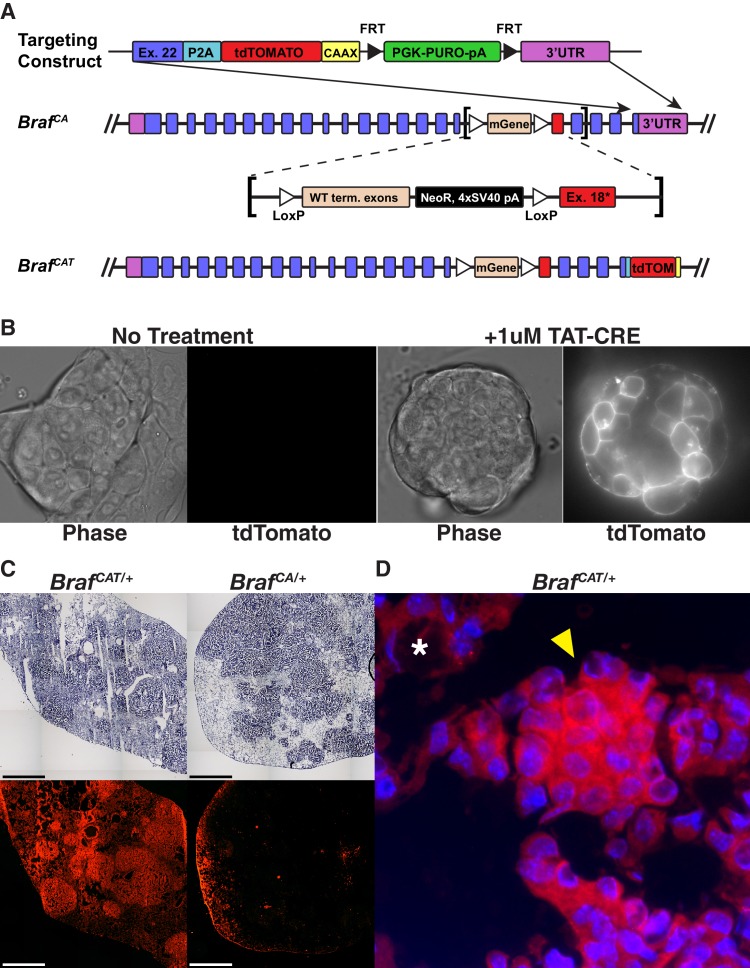
Figure 1. Engineering and validation of a novel genetically engineered mouse model of BRAFV600E driven cancer.
(A) The BrafCAT mouse builds upon the utility of the BrafCA mouse by tying expression of the oncogenic form of BRAF to expression of the red fluorescent protein, tdTomato. (B) Targeted BrafCAT ES cells display membrane associated red fluorescence only after the addition of TAT-CRE. (C) Comparison of Ad-CMV-CRE initiated lung tumor formation and fluorescence in frozen sections from lungs of BrafCAT/+ and BrafCA/+ animals. (D) Lung adenoma found in a BrafCAT animal showing fluorescence in the tumor (arrowhead) and not in the lung parenchyma (asterisk).
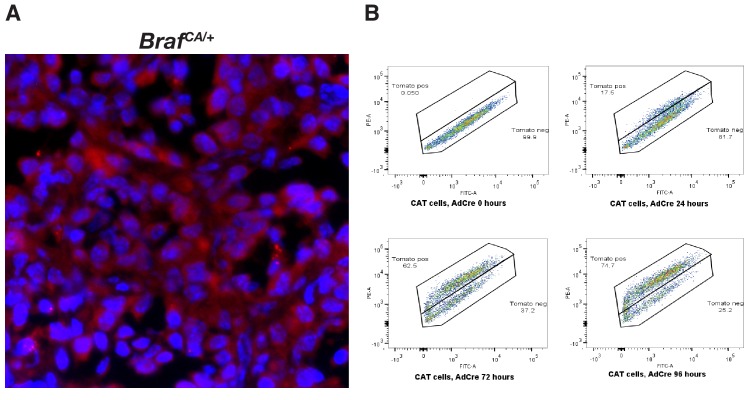
Figure 1—figure supplement 1. Engineering and validation of a novel genetically engineered mouse model of BRAFV600E driven cancer.
BrafCAT mice were generated from an appropriately targeted ES cell clone (1E6). To compare and contrast lung tumorigenesis following CRE-mediated recombination of the BrafCAT versus the original BrafCA allele, mice of the appropriate genotype were infected with 107 pfu of Ad-CMV-CRE and analyzed at 8 weeks post-initiation (p.i.). We observed similar lung tumor formation in BrafCAT versus BrafCA mice (Figure 1C) with the only discernable difference being the red fluorescence of lung tumors arising in the BrafCAT mice (Figure 1C,D and Figure 1—figure supplement 1A). In embryonic fibroblasts (MEFs) derived from BrafCAT mice, tdTomato fluorescence was detected by flow cytometry within 24 hr after expression of CRE and plateaued by 96 hr (Figure 1—figure supplement 1B). Following CRE-mediated recombination of BrafCAT in both MEFs and mouse lung cells (Figure 2B), the total amount of fluorescence from the BrafCAT allele was modest, likely due to being driven by the endogenous Braf promoter. However, tdTomato expressing cells were readily differentiated from autofluorescence by using a channel with no fluorophore (FITC) as a marker of autofluorescence, as has been previously described (Dane et al., 2006). Together, these data indicate that the BrafCAT allele functions analogously to the BrafCA allele for the development of benign lung tumors following CRE-mediated initiation of BRAFV600E expression, and that cells expressing the BRAFV600E-P2A-tdTomato mRNA are readily identified by flow cytometry within a short time frame.
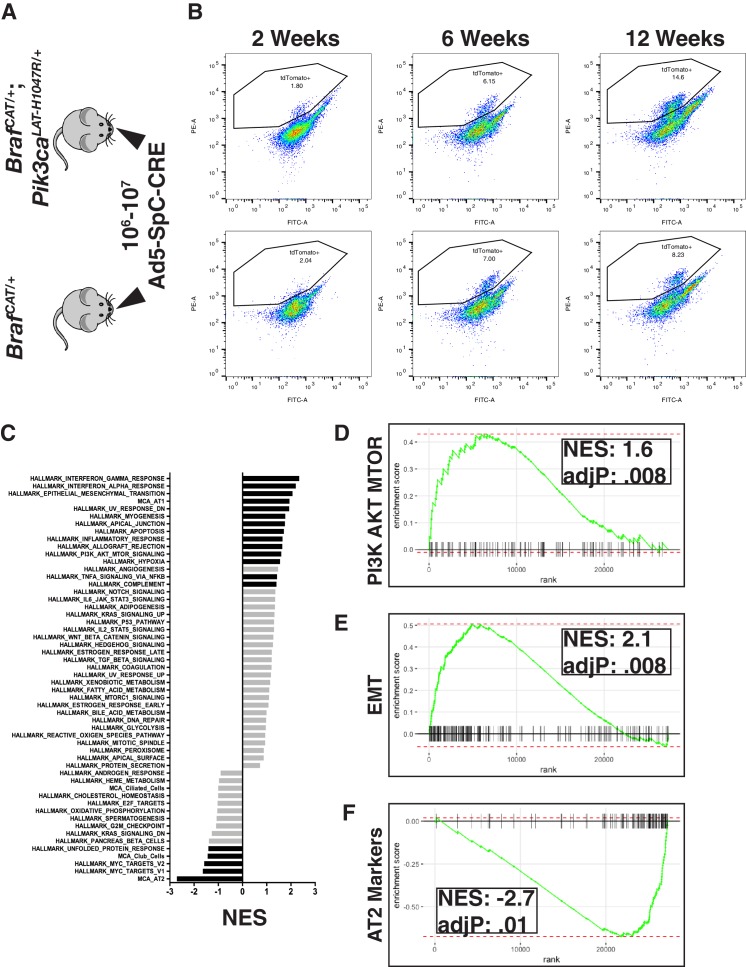
Figure 2. Examining global gene expression changes caused by combination of PI3K and MAPK activation using RNA-SEQ.
(A) Tumors were adenovirally induced in cohorts of BrafCAT/+ and BrafCAT/+;Pik3caLAT-H1047R/+ mice with AT2 specific CRE expression. Mice harvested at 2 or 6 weeks were induced with 107 PFU of Ad5-SpC-CRE, whereas mice harvested at 12 weeks were induced with 106 PFU of Ad5-SpC-CRE. (B) Tumor cells were harvested from each genotype at 2 weeks, 6 weeks, and 12 weeks post tumor induction via tissue dissociation and FACS. (C) GSEA analyses profiling cells sorted from BRAFV600E/PI3KαH1047R driven tumor bearing mice compared to BRAFV600E driven tumor bearing mice, showing all ‘Hallmark’ gene sets along with gene sets constructed from the most specific markers of the cell types of the distal lung epithelium. Black bars indicate adjP <.05, gray bars indicate Benjamini-Hochberg corrected enrichment statistic adjP ≥. 05. Here all time points combined within genotype. (D) GSEA mountain plot showing broad activation of PI3K signaling in BRAFV600E/PI3KαH1047R driven tumor bearing mice; adjP is Benjamini-Hochberg corrected enrichment statistic. (E) GSEA mountain plot showing broad activation of EMT in BRAFV600E/PI3KαH1047R driven tumor bearing mice; adjP is Benjamini-Hochberg corrected enrichment statistic. (F) GSEA mountain plot showing widespread loss of AT2 identity in BRAFV600E/PI3KαH1047R driven tumor bearing mice; adjP is Benjamini-Hochberg corrected enrichment statistic.
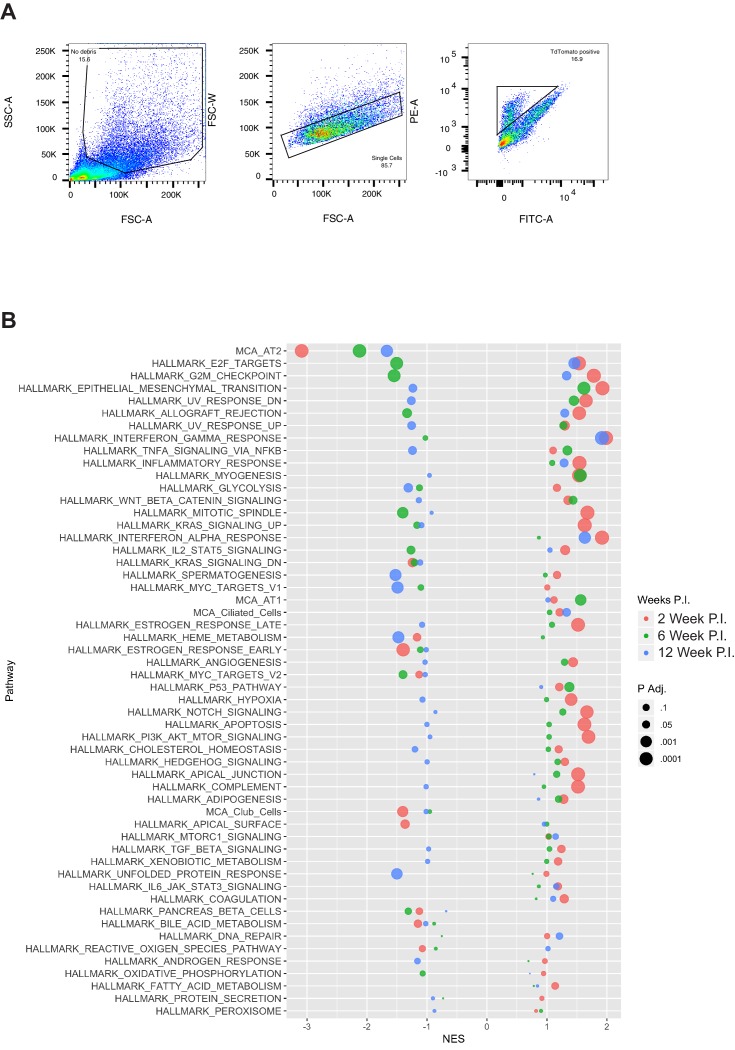
Figure 2—figure supplement 1. Examining global gene expression changes caused by combination of PI3K and MAPK activation using RNA-SEQ.
Messenger RNA expression profiles of BRAFV600E/PI3KαH1047R-driven lung tumors display diminished expression of AT2 pneumocyte specific genes
To address mechanism(s) of cooperation between BRAFV600E and PI3’-lipid signaling in lung cancer progression, lung tumorigenesis was initiated in BrafCAT or BrafCAT; Pik3calat-H1047R (Pik3caHR hereafter) mice (Figure 2A) and analyzed at 2, 6 or 12 weeks p.i. (Figure 2B, for detailed gating strategy see Figure 2—figure supplement 1A). Importantly, to initiate oncoprotein expression solely in AT2 pneumocytes, we utilized Ad5-SpC-CRE, which restricts expression of CRE recombinase to Sftpc expressing cells (Sutherland et al., 2014). tdTomato expressing tumor cells were detectable by flow cytometry in both BrafCAT and BrafCAT; Pik3caHR mice as early as two weeks p.i. (Figure 2B). To identify alterations in mRNA expression that might explain how PI3KαH1047R promotes malignant transformation of lung tumors initiated by BRAFV600E, we performed RNA-Seq analysis of flow sorted tdTomato+ lung tumor cells driven either by BRAFV600E alone or the combination of BRAFV600E plus PI3KαH1047R. To gain a broad view of pathways and processes differing in these two tumor genotypes, we used Gene Set Enrichment Analyses (GSEA) (Figure 2C) on, samples from all time points (for GSEA analyses separated by week see Figure 2—figure supplement 1B). Comparing ‘hallmark’ gene sets (Broad Institute MSigDB: Hallmarks), and consistent with the engineered characteristics of the lung tumor cells, GSEA revealed that PI3K→AKT→MTOR signaling (Figure 2C and D) and epithelial→mesenchymal transition (Figure 2C and E) related genes were significantly elevated in BRAFV600E/PI3KαH1047R-driven lung tumors compared to BRAFV600E-driven tumors. To examine differentiation state we constructed gene sets comprised of the 100 most specific described mRNA markers of the different cell types expressed in the distal lung epithelium (Han et al., 2018; Treutlein et al., 2014) namely alveolar type 1 (AT1) and type 2 (AT2) pneumocytes, as well as club and ciliated cells, hereafter referred to as AT1-100, AT2-100, club-100, and ciliated-100, respectively. Despite these gene sets representing related cell types of the distal lung epithelium, there is only modest overlap between their members, ranging from 2 to 12 of the 100 genes. GSEA using these gene sets demonstrated that, compared to BRAFV600E expressing tumor cells, BRAFV600E/PI3KαH1047R expressing tumor cells showed a significant decrease (adj. p=0.01) in expression of transcripts associated with AT2 cell identity (Figure 2C and F). This effect encompassed nearly all AT2 markers including the classical markers, Sftpa/b/c, and newly described markers detected in many different gene classes including Lcn2 (lipid transporter), Bex2 (transcription factor), and Dlk1 (encoding a non-canonical NOTCH ligand). Together these data suggest that PI3KαH1047R signaling promotes reduced expression of markers of AT2 differentiation. Notably, when examined in parallel with 50 hallmark gene sets and markers of other cell types in the distal lung epithelium, the loss of expression of AT2 mRNAs was the strongest effect observed in association with PI3KαH1047R expression (NES: −2.71, Figure 2C and F). Decreased AT2 marker expression was statistically significant as early as 2 weeks (Figure 3A and Figure 2—figure supplement 1B) and was also observed at 6 weeks (Figure 3B and Figure 2—figure supplement 1B) and 12 weeks (Figure 3C and Figure 2—figure supplement 1B) p.i. Hence the effects of PI3KαH1047R on expression of AT2 differentiation markers initiates more rapidly than has been reported in tumors driven by KRASG12D (Desai et al., 2014), KRASG12D/TP53Null (Winslow et al., 2011), KRASG12D/CTNNB1Δex3 (Pacheco-Pinedo et al., 2011), BRAFV600E/TP53Null (Garnett et al., 2017; Shai et al., 2015), or BRAFV600E/CTNNB1Δex3 (Juan et al., 2014). In addition to reduced AT2 mRNA marker expression, PI3KαH1047R expression elicited a marked increase in AT1 marker expression when comparing all time points (Figure 2C). By contrast to the changes observed in AT2 marker expression, this change was most significant at earlier time points and was no longer observed to be significant by 12 weeks p.i. (Figure 2—figure supplement 1B). Together, these results suggest a capability of PI3’-lipid signaling to influence AT2 pneumocyte identity.
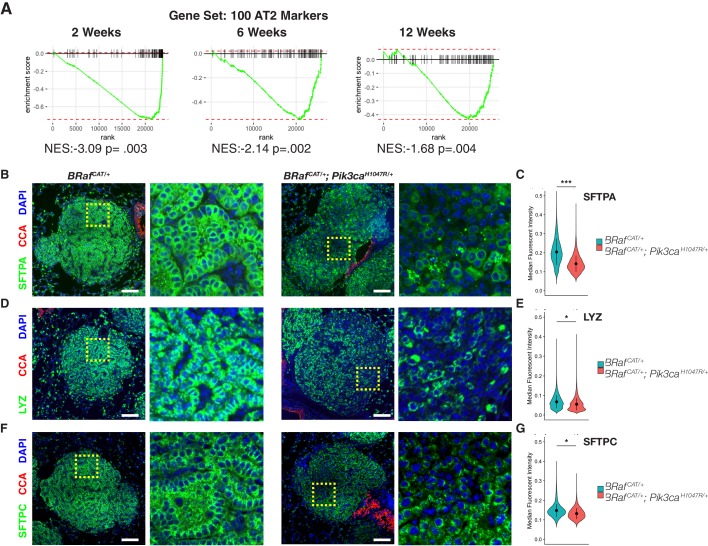
Figure 3. BRAFV600E/PI3KαH1047R Driven Tumors Display Widespread Heterogeneous Loss of AT2 Marker Expression, Whereas BRAFV600E Driven Tumors Maintain AT2 marker expression.
(A) GSEA mountain plots comparing gene expression profiles of cells sorted from BrafCAT/+;Pik3caLAT-H1047R/+ mice to those from BrafCAT/+ mice, using 100 specific markers of AT2 identity as the gene set. Analyses show comparison of tumors from the two genotypes at each time point analyzed; P value is enrichment statistic. (B) Tumors found in BrafCAT/+;Pik3caLAT-H1047R/+ mice have widespread variegated loss of expression of the functional AT2 marker, SFTPA, compared to tumors found in BrafCAT/+ mice. Expression of CCA is seen in airways but not in tumors of either genotype. Dashed boxes highlight areas of increased magnification. Scale bars = 100 um. (C) CellProfiler based quantitation of SFTPA immunofluorescence. Wilcoxon rank sum p value = 0.00013 (D) Tumors found in BrafCAT/+;Pik3caLAT-H1047R/+ mice have widespread loss of expression of the functional AT2 marker, LYZ, compared to tumors found in BrafCAT/+ mice. (E) CellProfiler based quantitation of LYZ immunofluorescence. Wilcoxon rank sum p value = 0.02224 (F) Tumors found in BrafCAT/+;Pik3caLAT-H1047R/+ mice have widespread loss of expression of the functional AT2 marker, SFTPC, compared to tumors found in BrafCAT/+ mice. (G) CellProfiler based quantitation of SFTPC immunofluorescence. Wilcoxon rank sum p value = 0.02323.
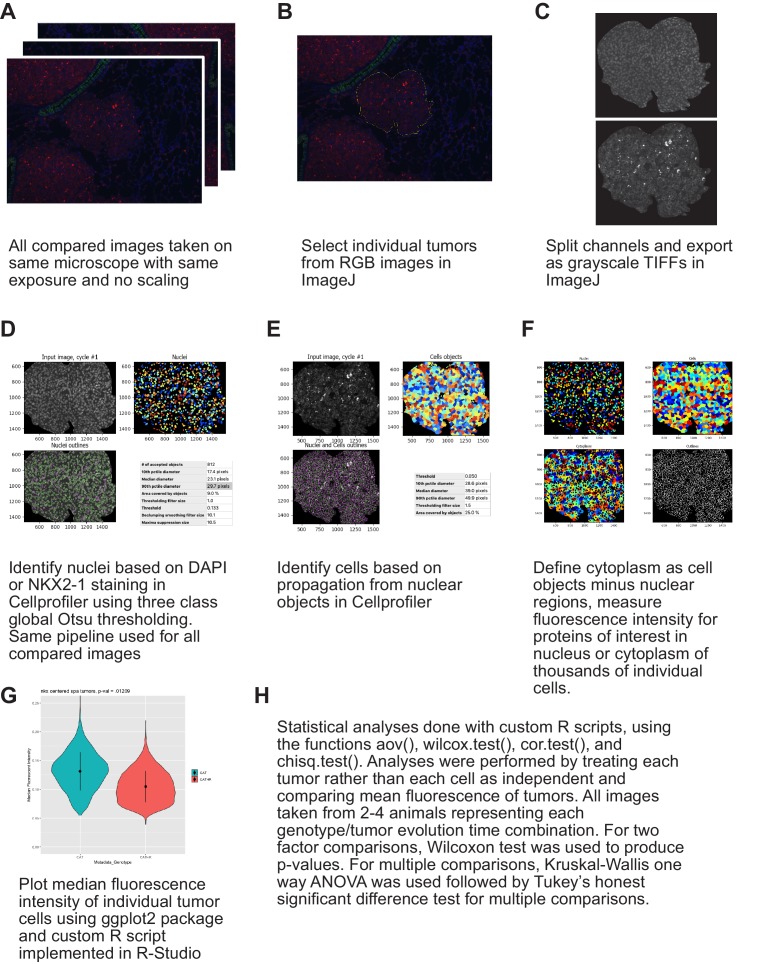
Figure 3—figure supplement 1. Cellprofiler based immunofluorescence quantification strategy.
PI3KαH1047R cooperates with BRAFV600E expression to promote loss of expression of lung tumor differentiation markers
Consistent with the mRNA expression data, Ad5-Sftpc-CRE initiated BRAFV600E/ PI3KαH1047R-driven lung tumors displayed decreased expression of surfactant proteins A and C (SFTPA and SFTPC) and Lysozyme, all of which are AT2 pneumocyte markers (Figure 3B,D and F). We next built a pipeline in CellProfiler, which allows for quantification of immunofluorescence images with single cell resolution in thousands of cells algorithmically (Figure 3—figure supplement 1A–H). By this means we noted significant reductions of SFTPA, SFTPC, and LYZ expression at 12 weeks p.i. (Figure 3C, E and G. Wilcoxon p=0.0001,. 02,. 02 respectively, data from Figure 3—source data 1, 2 and 3).
It has previously been suggested that a population of cells at the bronchioalveolar junction co-expressing SFTPC and club cell antigen (CCA) has properties of bronchio-alveolar stem cells (BASCs) (Kim et al., 2005), and also that ERK1/2 signaling tone allows for expansion of club cell derived tumors (Cicchini et al., 2017). Thus, a hypothesis that might explain our observations is that expression of PI3KαH1047R allows for enhanced expansion of BASC-derived tumors, which express lower levels of AT2 marker genes. We reject this hypothesis based on three lines of evidence. First, there did not appear to be two classes of BRAFV600E/PIK3CAH1047R-induced tumors with respect to AT2 marker expression. Instead, within each tumor we observed variegated loss of AT2 marker expression (Figure 3B,D,F insets). Second, to test whether CCA/SFTPC double positive cells might be the source of emergence of a separate tumor type, we co-stained our AT2 marker panel with antisera to detect expression of club cell antigen (CCA). While CCA staining was readily detectable in airways, it was not observed throughout the BRAFV600E/PI3KαH1047R-driven tumors, including those cells that have reduced AT2 marker expression (Figure 3B,D and F). Finally, we observed tumors arising predominantly within alveolar spaces, a pattern characteristic of AT2-derived tumors, whereas club cell derived tumors tend to arise predominantly at bronchioalveolar duct junctions (Cicchini et al., 2017). Taken together, these data suggest that BRAFV600E/PI3KαH1047R-driven lung tumors arise from AT2 cells but rapidly lose their differentiated identity under the influence of PI3’-lipid signaling.
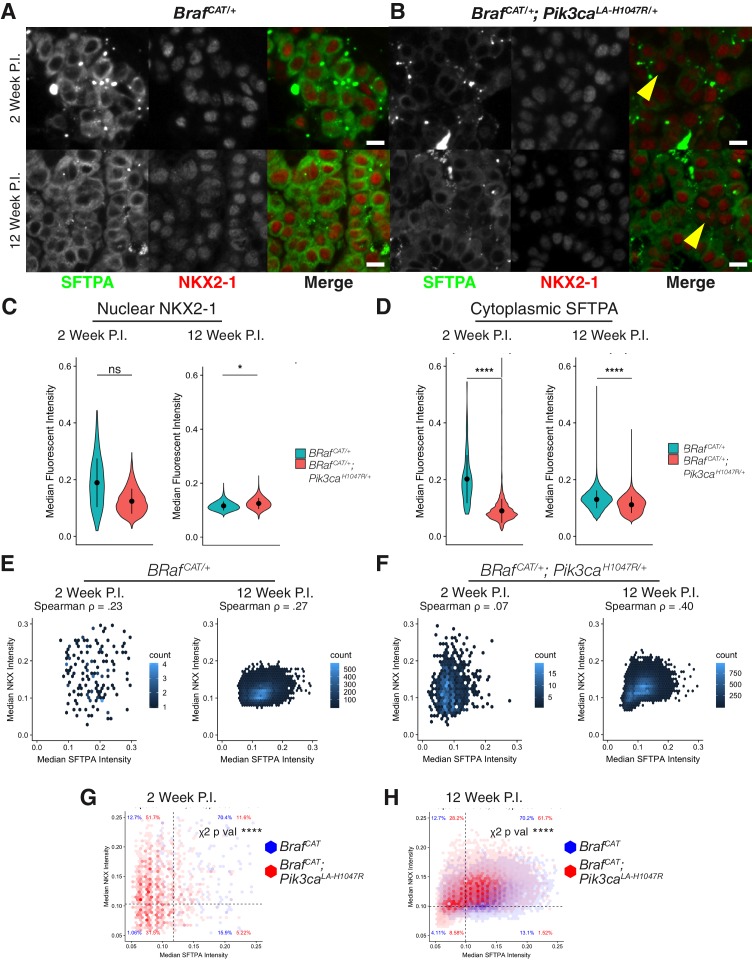
Cooperative signaling between PI3KαH1047R and BRAFV600E promotes de-differentiation of AT2 cells despite expression of NKX2-1
Extensive research demonstrates that the NKX2-1 and FOXA1/2 transcription factors pattern and maintain the differentiated identity of normal lung cells (Bruno et al., 1995; Camolotto et al., 2018; DeFelice et al., 2003; Hamvas et al., 2013; Lazzaro et al., 1991; Minoo et al., 1995; Snyder et al., 2013; Stahlman et al., 1996; Yuan et al., 2000). As these transcription factors also display decreased expression in some models of LUAD (Juan et al., 2014; Snyder et al., 2013; Winslow et al., 2011), we next examined if changes in bulk NKX2-1 or FOXA1/2 expression in BRAFV600E/PIK3CAH1047R-driven lung tumors might explain the observed alterations in AT2 marker gene expression. Analysis of RNA-Seq data showed no consistent decrease of NKX2-1 or FOXA1/2 mRNA expression in BRAFV600E/PIK3CAH1047R-driven lung tumors. As this was initially surprising, we sought to further verify that AT2 identity was lost independent of NKX2-1 expression levels or localization in BRAFV600E/PIK3CAH1047R-driven lung tumors. Dual color immunofluorescence staining demonstrated that the observed loss of AT2 identity is not associated with a decrease or change in nuclear localization of NKX2-1 at either 2 or 12 weeks p.i. (Figure 4A–B). Quantification of immunostaining supports this observation, with no significant alteration in nuclear NKX2-1 staining at 2 weeks, and only a slight but significant increase in nuclear NKX2-1 staining observed when comparing 12 week p.i. BRAFV600E/PIK3CAH1047R-driven tumors to paired BRAFV600E-driven tumors (Figure 4C, data from Figure 4—source data 1). Quantification of the same tumors confirmed a significant decrease of SFTPA staining in BRAFV600E/PIK3CAH1047R-driven tumors first observed at 2 weeks and persisting at 12 weeks p.i. (Figure 4D). Since we performed our quantification with single cell resolution we were able to compare NKX2-1 and SFTPA immunofluorescence staining on a cell-by-cell basis (Figure 4E–H). BRAFV600E-driven tumors show association of NKX2-1 and SFTPA staining consistent across time points (Spearman Rho = 0.23-.27, Figure 4E). BRAFV600E/PIK3CAH1047R-driven tumors by contrast initially show almost no association between levels of NKX2-1 and SFTPA (Spearman Rho = 0.07, Figure 4F), but by 12 weeks p.i. the association of these two markers has increased markedly (Spearman Rho = 0.40, Figure 4F). Because the reduction of SFTPA precedes the observed association of NKX2-1 and SFTPA, we conclude that other factors must explain the rapid reduction in SFTPA expression. Dividing tumor cells into classes representing NKX2−1 ± and SFTPA +/- (for definitions, see Materials and methods) shows significant effects (chi-squared p<0.001) of tumor genotype on co-expression of NKX2-1 and SFTPA (Figure 4G–H). At both 2 and 12 weeks p.i., the largest proportional increase driven by PIK3CAH1047R expression is seen in NKX2-1+/SFTPA- tumor cells (Figure 4G–H), implying that at both early and late time points, decreased expression of NKX2-1 cannot explain the observed decrease in SFTPA expression. Similarly, neither the expression of FOXA1 (Figure 4—figure supplement 1A) nor FOXA2 (Figure 4—figure supplement 1B) at 12 weeks p.i. correlated with decreased SFTPA expression as assessed by immunostaining. Nor is the phosphorylation status of NKX2-1 at a critical ERK targeted residue (pS327) associated with loss of SFTPA expression (Figure 4—figure supplement 1C). Together these data suggest that the decreased expression of markers of AT2 cell differentiation that we observed upon co-activation of PI3’-lipid signaling in BRAFV600E driven tumors is largely independent of the expression levels of these known regulators of AT2 cell identity. We also note that at later time points, repression of NKX2-1, FOXA1, or FOXA2 protein expression in scattered cells may serve to augment the dedifferentiation phenotype that we observed beginning at 2 weeks p.i.
Figure 4. Expression levels and localization of lung lineage survival transcription factors are maintained in BRAFV600E/PI3KαH1047R driven tumors, Including those cells which have lost expression of markers of AT2 identity.
(A) BRAFV600E driven hyperplasia and tumors display widespread expression of both SFTPA and nuclear localization of the lung lineage transcription factor, NKX2-1, at 2 and 12 weeks post initiation. Scale bar = 10 um. (B) BRAFV600E/PI3KαH1047R driven hyperplasia and tumors show decreased SFTPA expression at 2 and 12 weeks post initiation. These tumors maintain broad nuclear expression of NKX2-1, including those cells with decreased SFTPA expression (yellow arrowheads). (C) Quantitation showing no significant difference in NKX2-1 immunoreactivity at 2 weeks post initiation, but a slight increase in nuclear NKX2-1 at 12 weeks post initiation. Wilcoxon rank sum p values = 0.2,. 02 respectively. (D) Significant reduction of SFTPA immunoreactivity seen in BRAFV600E/PI3KαH1047R driven hyperplasia and tumors at both 2 and 12 weeks post initiation. Wilcoxon rank sum p values = 5e-5, 4e-5 respectively. (E) Cytoplasmic SFTPA immunoreactivity plotted versus nuclear NKX2-1 immunoreactivity in BRAFV600E driven hyperplasia and tumors at 2 and 12 weeks post initiation. Similar association seen at both time points (Rho = 0.23,. 27 respectively). (F) Cytoplasmic SFTPA immunoreactivity plotted versus nuclear NKX2-1 immunoreactivity in BRAFV600E/PI3KαH1047R driven hyperplasia and tumors at 2 and 12 weeks post initiation. Relatively lower association seen at 2 weeks compared to 12 weeks (Rho = 0.07,. 40 respectively). (G) Overlay of BRAFV600E/PI3KαH1047R and BRAFV600E driven hyperplasia 2 weeks post initiation. Dashed line for each marker drawn at mean - one standard deviation of BRAFV600E driven tumors. BRAFV600E/PI3KαH1047R driven tumors show fewer SFTPA+, NKX2−1 + cells, most strongly accounted for by an increase in SFTPA-, NKX2−1 + cells. Chi square test associates genotype with distribution, p val <1e-5. (H) Overlay of BRAFV600E/PI3KαH1047R and BRAFV600E driven tumors 12 weeks post initiation. Dashed line for each marker drawn at mean - one standard deviation of BRAFV600E driven tumors. BRAFV600E/PI3KαH1047R driven tumors show fewer SFTPA+, NKX2−1 + cells, most strongly accounted for by an increase in SFTPA-, NKX2−1 + cells. Chi square test associates genotype with distribution, p val <1e-5.
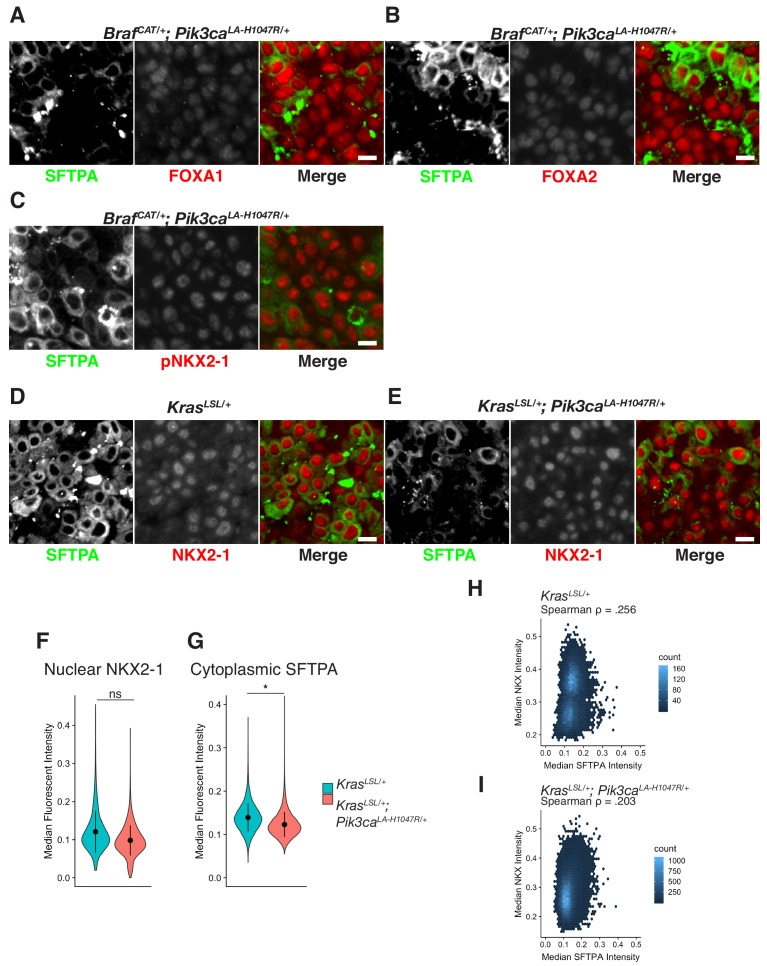
Figure 4—figure supplement 1. Expression levels and localization of lung lineage survival transcription factors are maintained in BRAFV600E/PI3KαH1047R and KRASG12D/PI3KαH1047R Driven Tumors, including those cells which have lost expression of markers of AT2 identity.
To test the generality of our results, we examined KRASG12D (Figure 4—figure supplement 1D) and KRASG12D/PIK3CAH1047R-driven lung tumors (Figure 4—figure supplement 1E) at 16 weeks p.i., a time at which mutationally-activated PI3KαH1047R strongly enhances KRASG12D-driven lung tumorigenesis (Green et al., 2015). Indeed, in this model, we observed a similar and significant decrease in SFTPA expression comparing KRASG12D/PIK3CAH1047R- to KRASG12D-driven tumors (Figure 4—figure supplement 1D,E,G, data from Figure 4—source data 2), which did not correspond to reduced NKX2-1 expression (Figure 4—figure supplement 1E,F). Intriguingly, although mutationally-activated KRASG12D is reported to activate PI3’-lipid signaling in lung tumors (Castellano et al., 2013; Engelman et al., 2008; Gupta et al., 2007b; Molina-Arcas et al., 2013; Murillo et al., 2018; Rodriguez-Viciana et al., 1994), we did not observe extensive loss of SFTPA immunoreactivity in these tumors (Figure 4—figure supplement 1D). Both KRASG12D/PIK3CAH1047R-driven tumors and KRASG12D-driven tumors showed similarly modest association of SFTPA and NKX2-1 expression (Figure 4—figure supplement 1H–I). Taken together these data suggest that either there exist additional factors that regulate AT2 pneumocyte identity independently of the NKX2-1/FOXA1/FOXA2 regulatory axis, or that these well-known regulators of pneumocyte identity require the presence of one or more additional factor(s) for their transcriptional function.
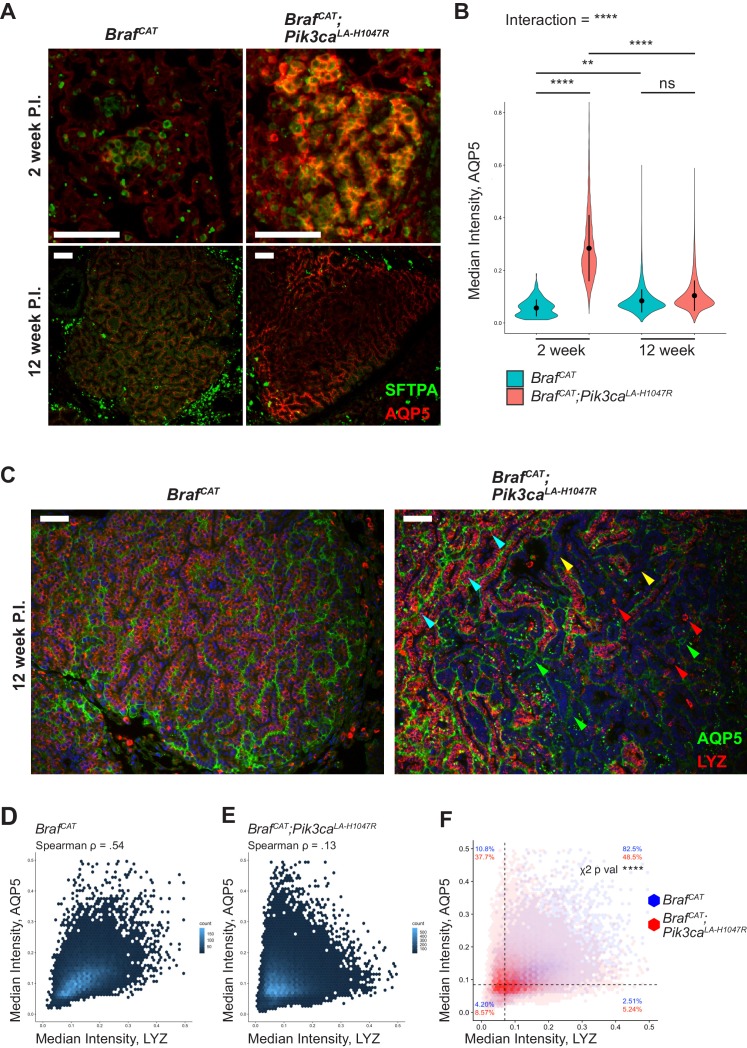
To explore the increase in AT1 marker expression observed in BRAFV600E/PI3KαH1047R-driven tumors in more detail, we immunostained both early and late tumors for the expression of the AT1 marker AQP5. At 2 weeks p.i. we observed a striking increase in AQP5 expression when comparing BRAFV600E/PI3KαH1047R-driven tumors to BRAFV600E-driven tumors (Figure 5A and B, data from Figure 5—source data 1). Interestingly, at 12 weeks p.i. the difference in AQP5 immunoreactivity is no longer significant between BRAFV600E/PI3KαH1047R and BRAFV600E-driven tumors, mirroring our mRNA expression profiling results (Figure 2 and Figure 2—figure supplement 1b). The pattern of AQP5 expression likely explains this finding, as modest AQP5 staining is seen throughout BRAFV600E-driven tumors as previously reported (Trejo et al., 2013), whereas BRAFV600E/PI3KαH1047R-driven tumors show strong AQP5 in some areas and essentially absent AQP5 in other areas (Figure 5A). Co-immunostaining of AQP5 and LYZ showed similar patterns in which BRAFV600E-driven tumors display widespread expression of both of AT1 and AT2 markers (Figure 5C). By contrast, BRAFV600E/PI3KαH1047R-driven tumors show some areas that are double positive for both AQP5 and LYZ (Figure 5C, cyan arrowheads), some areas with only expression of AQP5 (Figure 5C, green arrowheads), some areas with only expression of LYZ (Figure 5C, red arrowheads), and some areas where neither is expressed (Figure 5C, yellow arrowheads). Quantification of these data shows correlation (Spearman Rho = 0.54) between AQP5 and LYZ in BRAFV600E-driven tumors (Figure 5D), but lower correlation (Spearman Rho = 0.13) between these markers in BRAFV600E/PI3KαH1047R-driven tumors (Figure 5E). Comparing these two tumor types directly shows a significant effect of genotype on staining distribution (Figure 5F), with BRAFV600E/PI3KαH1047R-driven tumors showing a strong decrease in AQP5+/LYZ+ double positive cells, with corresponding increases in each of the remaining classes of cells (AQP5+/LYZ-; AQP5-/LYZ+; and AQP5-/LYZ-).
Figure 5. BRAFV600E/PI3KαH1047R and BRAFV600E driven tumors both show effects on differentiation status, with BRAFV600E/PI3KαH1047R driven tumors displaying more profound effects on identity.
(A) BRAFV600E/PI3KαH1047R and BRAFV600E driven hyperplasia both show immunoreactivity of the AT1 marker, AQP5, 2 weeks post initiation with BRAFV600E/PI3KαH1047R driven hyperplasia showing enhanced immunostaining. BRAFV600E/PI3KαH1047R and BRAFV600E driven tumors also show immunoreactivity of AQP5 12 weeks post initiation with BRAFV600E/PI3KαH1047R driven tumors showing a more variable pattern of immunostaining. Scale bars = 100 um. (B) Quantitation demonstrating significant effect of PI3KαH1047R on AQP5 immunoreactivity in BRAFV600E driven tumors 2 weeks post initiation. No difference seen in AQP5 immunoreactivity between BRAFV600E/PI3KαH1047R and BRAFV600E driven tumors 12 weeks post initiation. This appears to be the result of a slight increase in AQP5 immunoreactivity between 2 and 12 weeks in BRAFV600E driven tumors and a more dramatic decrease in AQP5 immunoreactivity between 2 and 12 weeks in BRAFV600E/PI3KαH1047R driven tumors. ANOVA p<1e-5, multiple comparisons done by Tukey’s Honest Significant Difference test, ****: p<1 e −5, **p=0.0014. (C) BRAFV600E driven tumors display widespread immunoreactivity to both AQP5 and the AT2 marker, LYZ, 12 weeks post initiation. BRAFV600E/PI3KαH1047R driven tumors show cells with widely varied expression of differentiation markers, including AQP5+, LYZ+ (Cyan arrows); AQP5-, LYZ+ (Red arrows); AQP5+, LYZ- (Green arrows); and AQP5-, LYZ- (Yellow arrows) cells. Scale bars = 100 um. (D) BRAFV600E driven tumors show relatively high association between AQP5 and LYZ immunoreactivity (Rho = 0.54). (E) BRAFV600E/PI3KαH1047R driven tumors show relatively low association between AQP5 and LYZ immunoreactivity (Rho = 0.13) (F) Overlay of BRAFV600E/PI3KαH1047R and BRAFV600E driven tumors 12 weeks post initiation. Dashed line for each marker drawn at mean - one standard deviation of BRAFV600E driven tumors. BRAFV600E/PI3KαH1047R driven tumors show fewer AQP5+, LYZ + cells, most strongly accounted for by an increase in AQP5+, LYZ- cells, but with increases also seen in AQP5-, LYZ + and AQP5-, LYZ- cells. Chi square test associates genotype with distribution, p val <1e-5.
Figure 5—figure supplement 1. BRAFV600E-driven lung tumors show characteristics of bipotent progenitor cells.
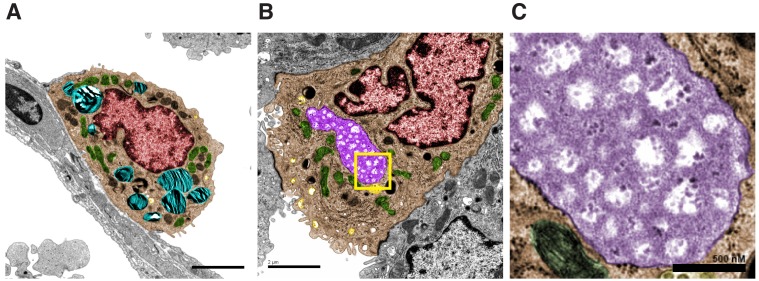
Co-expression of AT1 or AT2 markers in BRAFV600E-driven tumors is reminiscent of what is observed in bipotent progenitor cells, which are reported to give rise to both AT1 and AT2 cells (Desai et al., 2014). To search for additional indicators of a bipotent progenitor like state induced by BRAFV600E→MEK→ERK signaling, we analyzed transmission electron micrographs of BRAFV600E-driven lung tumor sections from suitably manipulated BrafCA mice 11 weeks p.i. Normal AT2 cells display a cuboidal morphology and contain many surfactant rich lamellar bodies (Figure 5—figure supplement 1A, cyan). BRAFV600E-driven tumor cells displayed gross morphological similarities to AT2 cells (Figure 5—figure supplement 1B), but in a subset of tumor cells large vacuoles, not seen in normal AT2 cells, were observed (Figure 5—figure supplement 1B, purple). Enhanced magnification of these structures demonstrated a rough chrysanthemum like pattern of electron dense material (Figure 5—figure supplement 1C) characteristic of glycogen storage (Revel, 1960). As glycogen storage vacuoles are another hallmark of bipotent progenitor cells (Desai et al., 2014), we propose that BRAFV600E→MEK→ERK signaling alone drives AT2 pneumocytes toward this fate. As BRAFV600E/PI3KαH1047R-driven tumors show some cells with co-expression of AT1 and AT2 markers, and many cells with reductions of either or both of these marker classes, we believe the coincident activation of ERK1/2 plus PI3’-lipid signaling promotes more profound de-differentiation of AT2 cells.
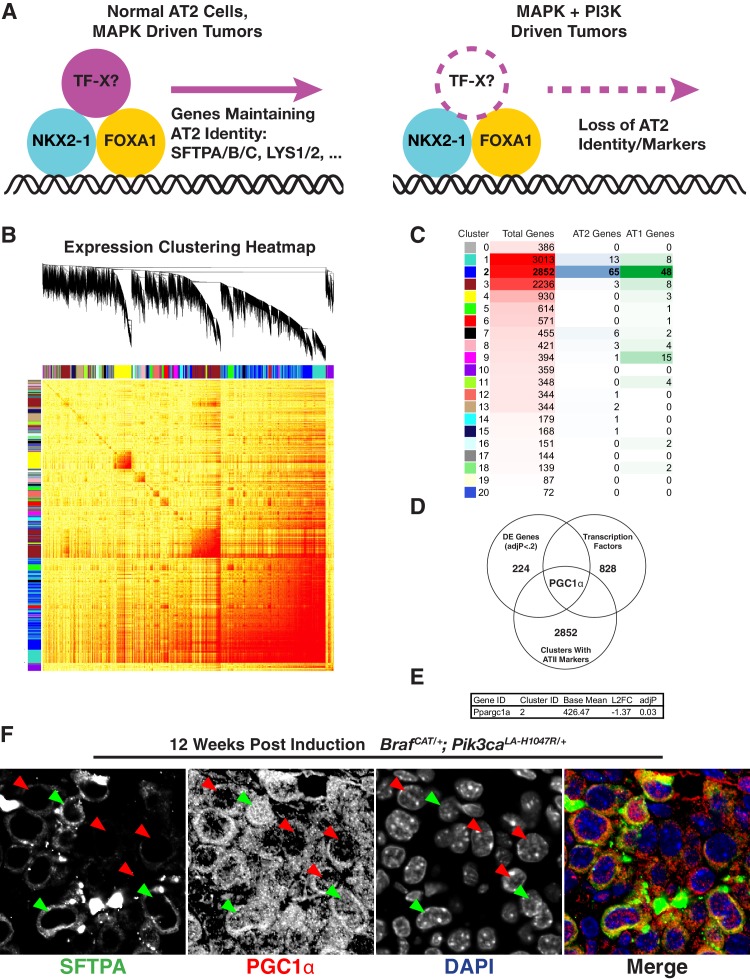
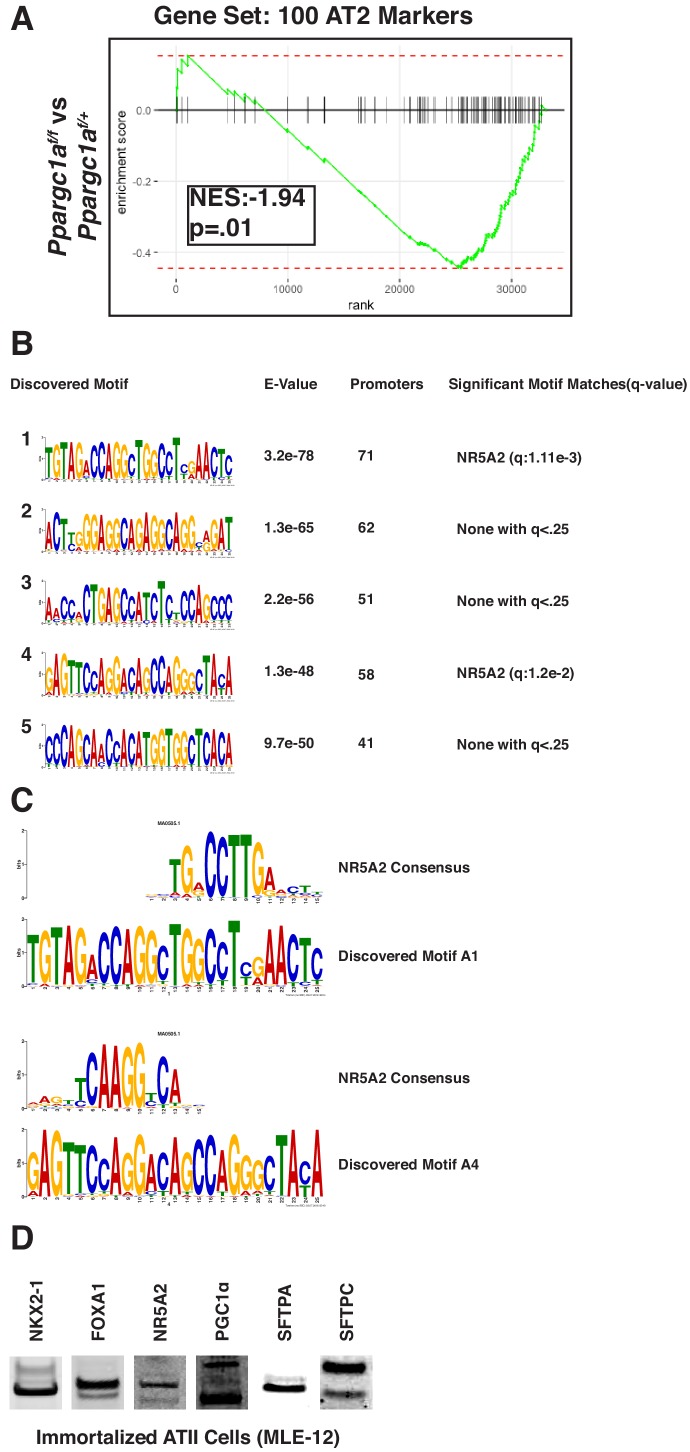
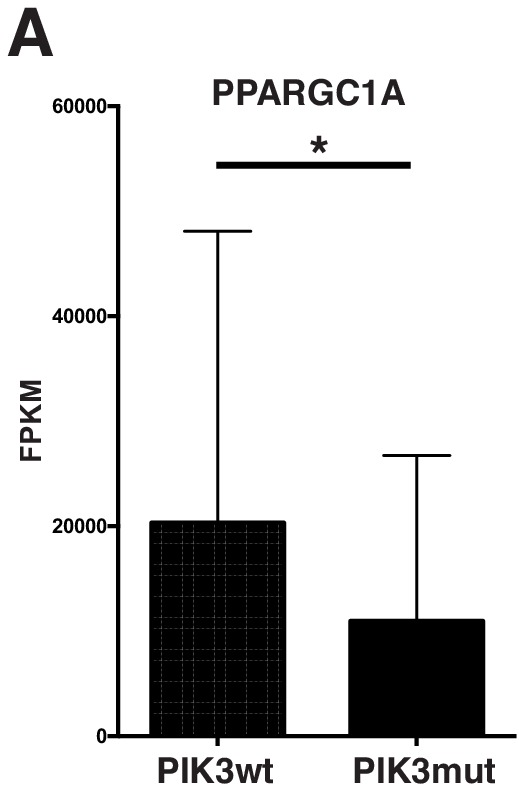
PGC1α expression correlates with AT2 marker expression
To identify novel candidate transcription factors that may participate in the establishment or maintenance of AT2 pneumocyte identity and function (Figure 6A), we took a three-step approach. First, we performed whole transcriptome correlation network analysis using Weighted Gene Correlation Network Analysis (WGCNA) (Langfelder and Horvath, 2008) to identify potentially relevant gene modules (Figure 6B). The majority of the AT2-100 and AT1-100 mRNAs fell into a single cluster (Cluster 2 – Dark blue Figure 6B,C). Next, to identify candidate regulators within cluster 2, we filtered the 2852 mRNAs in this cluster to select for those with demonstrated roles in transcriptional regulation. Finally, we filtered these selected transcription factors for differential expression in BRAFV600E- vs BRAFV600E/PI3KαH1047R-driven lung tumors using a promiscuous cutoff of adjP <0.2. The intersection of these three methods left a single candidate, the nuclear receptor co-activator, PGC1α (Figure 6D). PGC1α is a known transcriptional regulator, clusters with the majority of AT1 and AT2 genes, and its mRNA is significantly decreased in BRAFV600E/PI3KαH1047R-driven tumors compared to BRAFV600E-driven tumors (Figure 6E). The control of PPARGC1A levels by PI3’-lipid signaling may also be true in human lung tumors: those bearing mutations in either PIK3CA, AKT1, or PTEN have significantly reduced PPARGC1A mRNA expression compared to tumors bearing none of these mutations (Figure 6—figure supplement 1A). Finally, we sought to determine if PGC1α expression correlates with maintenance of lung identity on a cell-by-cell basis within BRAFV600E/PI3KαH1047R-driven tumors in mice. Immunostaining revealed that cells with decreased expression of SFTPA lack nuclear PGC1α (Figure 6F, red arrows). Conversely, tumor cells with detectable nuclear localization of PGC1α display readily detectable levels of SFTPA (Figure 6F, green arrows).
Figure 6. Loss of PGC1α Expression Correlates With Change in Expression of Lung Markers.
(A) Hypothetical model showing an additional factor cooperating with lung lineage transcription factors that is downregulated upon dual arm mutational activation of growth factor signaling. (B) Weighted gene correlation network analysis (WGCNA) heat map identifies 21 correlated gene expression modules. Gene tree shows relationship of individual genes, where multi-color bars adjacent to heat map identify individual clusters. (C) Table summarizing result of WGCNA analysis and AT1/AT2 memberships. Cluster number is listed adjacent to color corresponding to cluster in (B). For each cluster, shown is the total number of genes along with the number of AT1 and AT2 marker genes from AT1-100 and AT2-100. Cluster two contains the majority of both AT1 and AT2 marker genes. (D) A three factor approach to identify novel regulators of pneumocyte identity. Within the intersection of differentially expressed genes, genes co-regulated with the majority of AT1 and AT2 specific genes, and known transcription factors, lies a single gene, PGC1α. (E) PGC1α is significantly downregulated in BRAFV600E/PI3Kα H1047R driven tumors compared to BRAFV600E driven tumors; adjP is Benjamini-Hochberg corrected P value from DESeq2. (F) Decreased nuclear PGC1α immunoreactivity (red arrows) correlates with loss of AT2 identity on a cell by cell basis. AT2 identity is maintained in those cells which maintain nuclear PGC1α immunoreactivity (green arrows).
Figure 6—figure supplement 1. Mutations predicted to affect the PI3' lipid signaling pathway correlate with decreased PPARGC1A in human lung adenocarcinoma.
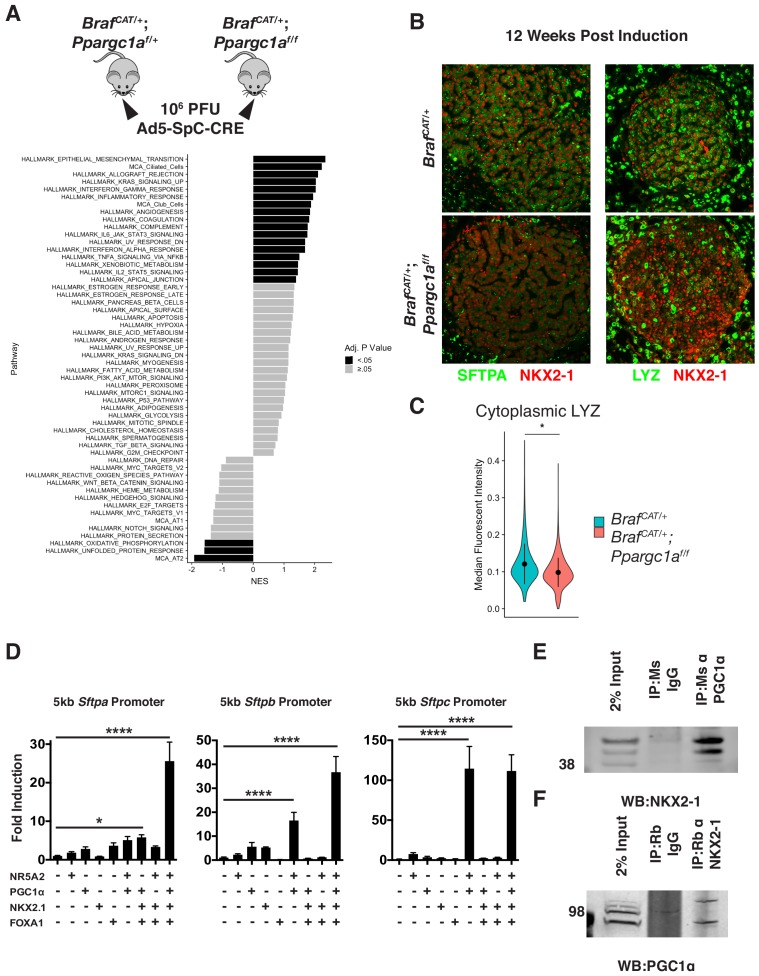
Silencing of PGC1α expression promotes de-differentiation of BRAFV600E-driven lung tumors
To directly test if PGC1α regulates AT2 identity, we crossed a floxed, conditional null allele of Pgc1α (Ppargc1alox/lox) to BrafCAT mice and generated littermate cohorts of BrafCAT; Ppargc1alox/lox, and BrafCAT; Ppargc1alox/+ mice. Lung tumorigenesis was initiated in these mice using 106 pfu Ad5-Sftpc-CRE (Figure 7A) with lungs harvested 12 weeks p.i. for isolation and analysis of tdTomato+ tumor cells by RNA sequencing. As expected, BRAFV600E/PGC1αNull-driven lung tumor cells showed decreasd expression of mRNAs encoding proteins involved in oxidative phosphorylation (Figure 7A). BRAFV600E/PGC1αNull-driven tumors also displayed a widespread decrease in markers of AT2 differentiation status as compared to BRAFV600E-driven tumors that retain PGC1α expression (Figure 7A and Figure 7—figure supplement 1). Interestingly, silencing of PGC1α recapitulated some other aspects of PI3Kα activation, including increasing markers of EMT, but some noticeable differences were observed in mRNA profiles including significant increases in ciliated and club cell markers (Figure 7A). LYZ and SFTPA immunoreactivity in BRAFV600E and BRAFV600E/PGC1αNull-driven tumors validated the decrease in AT2 marker expression in the absence of PGC1α expression (Figure 7B–C, data from Figure 7—source data 1).
Figure 7. PGC1α is required for maintenance of lung identity in BRAFV600E driven tumors.
(A) Tumors were induced in cohorts of BrafCAT/+ and BrafCAT/+;Ppargc1af/f mice via intranasal instillation of 106 PFU Ad5-SpC-CRE and harvested from each genotype 12 weeks post tumor induction via tissue dissociation and FACS. GSEA analyses of hallmark pathways and lung identity gene sets. Black bars indicate adjP <.05, gray bars indicate Benjamini-Hochberg corrected enrichment statistic adjP ≥. 05. (B) Immunostaining confirms decreased expression of the AT2 markers SFTPA and LYZ in BRAFV600E/PGC1αNULL tumors. (C) Quantitation demonstrating a significant decrease of LYZ immunoreactivity in BRAFV600E/PGC1αNULL tumors. Wilcoxon rank sum p val. = 0.0288. (D) Luciferase assays in HEK293T cells demonstrating the cooperation of NKX2-1, FOXA1, PGC1α, and NR5A2 in transactivation of surfactant promoters. All three promoters showed significant induction by ordinary one-way ANOVA (p<0.0001). Comparison of individual groups to mock transfected controls by Dunnett’s test for multiple comparisons: (*) p=0.0189, (****) p<0.0001. (E) Co-Immunoprecipitation of NKX2-1 by immunoprecipitation with a mouse monoclonal antibody recognizing PGC1α but not with IgG. (F) Co-Immunoprecipitation of PGC1α by immunoprecipitation with a mouse monoclonal antibody recognizing NKX2-1 but not with mouse IgG.
Figure 7—figure supplement 1. PGC1α is required for maintenance of lung identity in BRAFV600E driven tumors.
Figure 7—figure supplement 2. Proposed mechanism of PI3’-kinase-α promoting de-differentiation of lung tumors initiated by the BRAFV600E oncoprotein kinase.
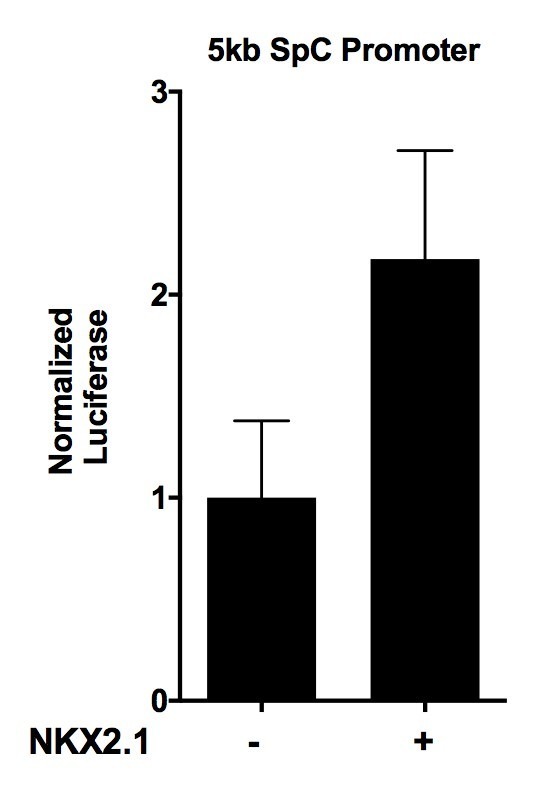
PGC1α cooperates with NKX2-1 and FOXA1 to transactivate AT2 promoters
We next sought to test if the role of PGC1α in AT2 pneumocyte identity maintenance could be through direct action on the promoters of AT2 pneumocyte specific genes. As PGC1α generally co-activates nuclear receptors such as PPARγ, we sought to discover its potential binding partner relevant to AT2 pneumocyte gene regulation. To this end we performed a motif discovery analysis using Multiple Em for Motif Elicitation (MEME) (Bailey and Elkan, 1994; Bailey et al., 2009) algorithm and scanning the promoter regions of the AT2-100. The most enriched novel motif (Figure 7—figure supplement 1B–C) bears significant similarity to the known binding motif of the nuclear receptor, NR5A2 (JASPAR: MA0505.1), also known as Liver Receptor Homolog (LRH) 1 (Gupta et al., 2007a).
To functionally test whether PGC1α can act at promoter sequences to regulate key markers of AT2 identity, we generated reporter constructs in which ~ 5 kb upstream of the transcription start site (TSS) of the genes encoding surfactant proteins A, B, or C (Sftpa/b/c) was inserted into a luciferase reporter plasmid. Transfection of individual expression constructs for NR5A2, PGC1α, NKX2-1, or FOXA1 showed modest promoter induction of up to four fold over mock-transfected cells (Figure 7D). However, co-transfection of these four factors together showed a dramatic 25–100 fold induction of the SFTPA, SFTPB, and SFTPC promoters. Importantly, the absence of PGC1α severely hampered the ability of NKX2-1 and FOXA1 to transactivate the surfactant A and B promoters, suggesting a functional role of PGC1α in the transcriptional transactivation of AT2 promoters.
PGC1α is found in complex with NKX2-1 in surfactant expressing cells
Based on the discovery that NR5A2 and PGC1α can cooperate with NKX2-1 and FOXA1 to transactivate AT2 pneumocyte promoters, we hypothesized that these proteins may exist in a biochemical complex. To test this directly, we used the immortalized mouse lung epithelial line MLE-12 (Wikenheiser et al., 1993). We first verified that these cells indeed express the pertinent proteins and maintain surfactant expression (Figure 7—figure supplement 1D). We next performed co-immunoprecipitation assays from MLE-12 cell extracts. While magnetic beads conjugated to mouse IgG did not enrich eluates for NKX2-1, magnetic beads conjugated to a mouse monoclonal antibody directed against PGC1α readily co-immunoprecipitated NKX2-1 (Figure 7E). To confirm this result, we showed that, while magnetic beads conjugated to rabbit IgG did not enrich eluates for PGC1α, magnetic beads conjugated to a rabbit monoclonal antibody directed against NKX2-1 also co-immunoprecipitated PGC1α (Figure 7F). Thus, PGC1α and NKX2-1 appear to co-exist in a complex in cells that express genes encoding AT2 expressed surfactant proteins.
Discussion
Genetically engineered mouse models have proven to be invaluable tools that complement the significant advances being made in the genetic and biochemical characterization of the initiation, progression and maintenance of human cancers. As genome sequencing efforts catalog clinically actionable mutations and their correlations with the cancer’s observed phenotypes, directly testing how these mutations affect disease initiation, progression, and response to novel therapeutics becomes a high priority. Here we describe a new GEM model that has allowed a deeper dissection of the stages of BRAFV600E-driven lung cancer, a disease that kills ~4000 patients per year in the U.S.A. (Siegel et al., 2016). To engineer this mouse we employed a strategy in which the previously targeted CRE-activated BrafCA allele was re-targeted to allow for the expression of both BRAFV600E and tdTomato from a single bicistronic mRNA following CRE-mediated recombination. Consequently, all BRAFV600E expressing cells are predicted to be red fluorescent by virtue of co-expression of tdTomato. This is an alternative approach to the more widely employed method of using a fluorophore expressed in trans from a different promoter (e.g. Rosa26) the expression of which is co-activated by CRE recombinase (Livet et al., 2007; Madisen et al., 2010; Muzumdar et al., 2007; Snippert et al., 2010). The approach described here has both advantages and disadvantages compared to the use of a fluorophore expressed in trans approach. The main disadvantage of our approach appears to be the modest fluorescence emission of tdTomato when expressed downstream of a P2A element from the mutationally activated BrafT1910A mRNA. Many LSL-XFP alleles have been designed for very high levels of expression by the incorporation of enhancers and strong promoters, whereas our model is driven by the endogenous Braf enhancer/promoter sequences. Hence, although the level of tdTomato fluorescence in lung tumors arising in BrafCAT mice is readily detected by flow cytometry, detection of tdTomato expression by immunohistochemistry in FFPE tissue sections is problematic. However, we have developed protocols that allow for detection of native tdTomato fluorescence in frozen sections (Figure 1D) or by a ligation proximity assay in FFPE sections (Daphne Pringle, unpublished). By contrast, the use of a fluorophore expressed in trans approach inherently relies on the simultaneous activity of CRE at distinct regions of the genome. Thus it is possible for the proto-oncogenic BrafCA locus to be subject to CRE-mediated recombination without recombination of the reporter, or vice-versa. While this is acceptable for some applications, it adds confounding noise that may be amplified under conditions when tumor cells have been specifically depleted by the application of pathway targeted or immunomodulatory therapy that has negligible effect on normal cells. Our approach avoids this noise entirely and results in a level of fluorescence that is directly correlated with expression of BRAFV600E on a cell-by-cell basis (van Veen et al., 2016). Importantly, our approach is especially compatible with the emerging technology of single cell RNA sequencing (scRNA-Seq), in which it is desirable to isolate single BRAFV600E oncoprotein kinase expressing cells for analysis.
Our studies were aided greatly by recent characterizations of the gene expression changes accompanying development of the mouse distal lung epithelium (Treutlein et al., 2014) and KRASG12D-mediated oncogenic transformation of AT2 cells (Desai et al., 2014). Using scRNA-Seq, the authors reconstructed the lineage hierarchies of AT1, AT2, club and ciliated cells, as well as provided a new list of markers useful in identifying these major cell types of the distal lung epithelium. We used these marker lists extensively and without bias or selection for most of our analyses. Importantly, we constructed gene sets for the GSEA analyses that showed widespread decreased AT2 marker expression in BRAFV600E/PIK3CAH1047R-driven lung tumors. Analysis of the full complement of AT2 markers paints a dramatic picture; nearly every AT2 identity marker is diminished in expression in BRAFV600E/PIK3CAH1047R-driven tumors as compared to BRAFV600E-driven tumors, as early as two weeks p.i. Importantly we noted a similar early and consistent repression of PGC1α expression in BRAFV600E/PIK3CAH1047R-driven tumors. Here our data support previous findings that indicate that PGC1α expression is repressed by the PI3K→AKT signaling axis via three insulin response sequences found in the PGC1α promoter shown to bind to the AKT-regulated FOXO1 transcription factor (Daitoku et al., 2003; Kemper et al., 2014). It has also been suggested that BRAFV600E signaling can suppress PGC1α expression via the MITF transcription factor in melanoma, further demonstrating the complicated interplay between growth factor signaling and oxidative phosphorylation (Haq et al., 2013), though this study did not examine any potential connection of PGC1α to tumor cell differentiation status.
PIK3CA mutation is found in ~4% of human LUAD (Campbell et al., 2016) that, although quite rare, still represents a significant patient population due to the high prevalence of lung cancer in our society. Previous studies have demonstrated that the ability of mutationally-activated KRASG12D to bind and activate PI3Kα is critical for its tumor promoting activities, as well as tumor maintenance (Castellano et al., 2013; Gupta et al., 2007b; Molina-Arcas et al., 2013; Murillo et al., 2018). Despite this, activation of PI3’-lipid signaling remains rate limiting with respect to tumor initiation and growth in KRASG12D-driven lung tumors as evidenced by the strong cooperation between KRASG12D and PIK3CAH1047R in promoting lung tumorigenesis in a GEM model (Green et al., 2015). This cooperation likely reflects the fact that the initial expression of KRASG12D is a relatively weak activator of both PI3’-lipid signaling and the RAF→MEK→ERK pathways (Cicchini et al., 2017). Indeed, whereas KRASG12D derived lung cancer cells show little phosphorylation of AKT at a key activating amino acid (S473), KRASG12D/PIK3CAH1047R derived cells show strong pS473-AKT phosphorylation (Green et al., 2015). Our results suggest that the lack of PI3’-lipid signaling in KRASG12D-driven lung tumors is not only limiting in tumor growth, but in propensity for AT2 pneumocyte de-differentiation. Intriguingly, recent studies have shown that stromally derived IGF-1 promotes a cancer stem cell like phenotype in Kras mutated cell lines (Chen et al., 2014), via the PI3K→AKT signaling axis. It will be interesting to examine in future studies how various tumor genotypes and tumor microenvironments converge upon the initiation and evolution of LUAD de-differentiation.
Lung adenocarcinoma differentiation status, as judged by pathological criteria, remains a critically important prognostic factor in predicting patient survival (Yoshizawa et al., 2011). However, only in recent years have we begun to understand the genetic aberrations that can directly promote loss of differentiation status. The protein most directly demonstrated to influence both lung adenocarcinoma differentiation status and progression is NKX2-1, a homeodomain transcription factor. Indeed, in the KrasLSL-G12D GEM model of KRASG12D-driven lung adenocarcinoma, NKX2-1 expression is diminished or silenced in the most poorly differentiated tumors. Moreover, shRNA-mediated inhibition of NKX2-1 expression is reported to enhance the metastatic potential of KRASG12D/TP53Null-driven lung cancer cells (Winslow et al., 2011). Interestingly, concomitant expression of KRASG12D with genetic silencing of NKX2-1 expression has qualitatively different effects, promoting trans-differentiation of tumor cells into a gastric fate resembling de-differentiated mucinous adenocarcinoma (Snyder et al., 2013), an effect that requires the activity of FOXA1/FOXA2 (Camolotto et al., 2018). Intriguingly, while even haploinsufficiency of NKX2-1 promoted the appearance of mucinous adenocarcinoma in the KrasLSL-G12D GEM model of lung adenocarcinoma, the same was not true in a lung adenocarcinoma model driven by expression of a mutationally-activated form of the EGF receptor (Maeda et al., 2012). In this model, haploinsufficiency of NKX2-1 slowed tumor progression rather than enhancing it. Importantly, loss-of-function mutations or silencing of NKX2-1 is a relatively infrequent event in lung adenocarcinoma. Instead NKX2-1 is often found as the most significantly focally amplified locus (Campbell et al., 2016). Further, in human NSCLC cell lines in which NKX2-1 is amplified, RNAi-mediated inhibition of NKX2-1 expression elicited decreased cell division and apoptosis (Kwei et al., 2008). Hence, the role of NKX2-1 in LUAD progression is thus simultaneously critically important and also complicated. In this case, GEM models provide an ideal system in which to study the contribution of individual mutations to each step of tumor initiation and progression without the complications of mutagen-induced genome hypermutation as is common in KRAS-mutated human lung cancer cells (Chalmers et al., 2017). While a wealth of literature has shown the direct effect of NKX2-1 on AT2 promoters (Bruno et al., 1995), and the importance of NKX2-1 in normal lung development (DeFelice et al., 2003), it has also been shown that transcriptional co-activators are critical for NKX2-1 function (Cassel et al., 2002; Di Palma et al., 2003; Park et al., 2004; Yi et al., 2002). Here we have shown that the binding motif of the nuclear receptor, NR5A2 is highly enriched in the promoters of AT2 specific genes. We also demonstrate that NR5A2, and its known co-factor PGC1α (Yazawa et al., 2010), can potently enhance the activity of NKX2-1 at the promoters for surfactant proteins A and B. Interestingly, while NR5A2 and PGC1α can activate the promoter of SFTPC alone, the added presence of NKX2-1 and FOXA1 does not further co-activate this promoter. It may be the case that PGC1α and NKX2-1 act independently at this promoter, or it may be that there are additional or alternative transcriptional regulators not present in 293 T cells which, when present, allow PGC1α and NKX2-1 to cooperate. In vivo, in BRAFV600E/PIK3CAH1047R-driven tumors, we observed an early decrease of PGC1α mRNA expression, and importantly, a correlation between decreased PGC1α and SFTPA on a cell-by-cell basis within tumors. Combined with functional data in GEM models in which PGC1α expression was genetically silenced, these data argue that mutational-activation of PI3’-lipid signaling in BRAFV600E-driven LUAD leads to diminished PGC1α expression, and that this reduced expression compromises the ability of NKX2-1/FOXA1 to maintain AT2 pneumocyte identity (Figure 7—figure supplement 2A). It is important to note that while genetic silencing of PGC1α recapitulated some aspects of PI3K activation in BRAFV600E-driven driven lung tumors, there were interesting differences, including an increase in markers of club and ciliated cell identity, and no significant effect on AT1 marker expression. It is therefore highly likely that amongst the pleiotropic effects of PI3’-lipid signaling, inhibition of PGC1α-mediated signaling represents one of many important effector pathways. This novel mechanism of lung identity regulation is made more important by the observation that it can be induced by mutational-activation of PI3Kα in both KRASG12D- and BRAFV600E-driven driven lung adenocarcinomas. Since the best characterized role of PGC1α is in the regulation of mitochondrial biogenesis, we were initially surprised to discover the cooperativity that PGC1α shows in the regulation of AT2 cell identity. However, it has recently emerged that crippling mitochondrial function via loss of the critical pyruvate transporter, MPC1, potently drives cells into a de-differentiated stem cell fate in drosophila and mouse intestinal cells (Schell et al., 2017). These studies, and the data presented here, suggest exciting future studies to examine the role of PGC1α to act as a pleiotropic effector of tumor cell growth and differentiation state downstream of PI3’-lipid signaling.
Materials and methods
Key resources table.
| Reagent type (species) or resource |
Designation | Source or reference |
Identifiers | Additional information |
|---|---|---|---|---|
| Gene (Mus musculus) | Braf | Ensembl: ENSMUSG00000002413 |
||
| Gene (Mus musculus) | Pik3ca | Ensembl: ENSMUSG00000027665 |
||
| Genetic reagent (Mus musculus) | BrafCA | McMahon lab stock | MGI:Braftm1Mmcm
JAX:017837 RRID:IMSR_JAX:017837 |
|
| Genetic reagent (Mus musculus) | Pik3caH1047R | Wayne Phillips | MGI:Pik3catm1.1Waph
RRID:MGI:5427584 |
|
| Genetic reagent (Mus musculus) | BrafCAT | This paper | N/A | New genetically engineered mouse reported in this paper |
| Genetic reagent (Mus musculus) | KrasLSL | The Jackson Lab | MGI:Krastm4Tyj
JAX:008179 RRID:IMSR_JAX:008179 |
|
| Cell line (Mus musculus) | MLE-12 | ATCC | CRL-2110 RRID:CVCL_3751 |
|
| Cell line (Homo sapiens) | 293T | Lab Stock | RRID:CVCL_0063 | |
| Antibody | Mouse monoclonal PGC1α | Millipore | Cat# 1F3.9 RRID:AB_10806332 |
Co-IP, 10 ug WB, 1:500 |
| Antibody | Rabbit polyclonal PGC1α | Millipore | Cat# AB3242 RRID:AB_2268462 |
IHC, 1:50 WB, 1:500 |
| Antibody | Rabbit monoclonal NKX2-1 | Abcam | Cat# AB76013 RRID:AB_1310784 |
Co-IP, 10 ug IHC, 1:250 WB, 1:1000 |
| Antibody | Rabbit polyclonal Phospho-S327-NKX2-1 | CST | Cat# 13608 RRID:AB_2798273 |
IHC, 1:250 |
| Antibody | Rabbit monoclonal FOXA1 | Abcam | Cat# AB23738 RRID:AB_2104842 |
IHC, 1:250 |
| Antibody | Rabbit monoclonal FOXA1 | CST | Cat# 58613 RRID:AB_2799548 |
WB, 1:2500 |
| Antibody | Rabbit monoclonal FOXA2 | CST | Cat# D56D6 RRID:AB_10891055 |
IHC, 1:250 WB, 1:1000 |
| Antibody | Rabbit monoclonal SFTPA1 + 2 | Abcam | Cat# AB206299 RRID:AB_2810211 |
IHC, 1:250 WB, 1:1000 |
| Antibody | Goat polyclonal SFTPA | Santa Cruz | Cat# SC-7699 RRID:AB_661292 |
IHC, 1:100 WB, 1:1000 |
| Antibody | Goat polyclonal SFTPA | Santa Cruz | Cat# SC-7700 RRID:AB_661293 |
IHC, 1:100 WB, 1:1000 |
| Antibody | Rabbit polyclonal SFTPA | Santa Cruz | Cat# SC-13977 RRID:AB_661294 |
WB, 1:1000 |
| Antibody | Rabbit monoclonal Lysozyme | Abcam | Cat# AB108508 RRID:AB_10861277 |
IHC, 1:250 WB, 1:1000 |
| Antibody | Goat polyclonal SFTPC | Santa Cruz | Cat# SC-7705 RRID:AB_2185505 |
IHC, 1:250 WB, 1:1000 |
| Antibody | Rabbit polyclonal SFTPC | Santa Cruz | Cat# SC-13979 RRID:AB_2185502 |
WB, 1:1000 |
| Antibody | Goat polyclonal CCA | Santa Cruz | Cat# SC-9772 RRID:AB_2238819 |
IHC, 1:1000 |
| Antibody | Goat polyclonal AQP5 | Santa Cruz | Cat# SC-9890 RRID:AB_2059877 |
IHC, 1:50 |
| Antibody | Rabbit polyclonal NR5A2 | Abcam | Cat# AB153944 RRID:AB_2810212 |
WB, 1:1000 |
| Recombinant DNA reagent | M50 Super 8x TOPFlash | Addgene | Plasmid #12456 RRID:Addgene_12456 |
Vector used to build SFTP Luciferase reporters |
| Recombinant DNA reagent | pCDNA3-mLRH1 | Holly Ingraham | Ms NR5A2 expression vector | |
| Recombinant DNA reagent | pDTA-TK | Addgene | Plasmid #22677 RRID:Addgene_22677 |
Empty targeting vector for mouse production |
| Recombinant DNA reagent | MSCV-NKX2.1 | Addgene | Plasmid #31271 RRID:Addgene_31271 |
NKX2.1 expression vector |
| Recombinant DNA reagent | PCDH-FOXA1 | Eric Snyder | FOXA1 expression vector | |
| Recombinant DNA reagent | FUW-mKate | This paper | Fluorescent protein mKate expression vector used for assaying transfection efficiency | |
| Recombinant DNA reagent | GFP-PGC1 | Addgene | Plasmid #4 RRID:Addgene_4 |
PGC1α expression vector |
| Recombinant DNA reagent | pWZL-Hygro | Addgene | Plasmid #18750 RRID:Addgene_18750 |
Empty vector used to normalize amount of DNA transfected |
| Recombinant DNA reagent | SFTPA-LUC | This paper | 5 kb SFTPA promoter in luciferase reporter | |
| Recombinant DNA reagent | SFTPB-LUC | This paper | 5 kb SFTPB promoter in luciferase reporter | |
| Recombinant DNA reagent | SFTPC-LUC | This paper | 5 kb SFTPC promoter in luciferase reporter | |
| Peptide, recombinant protein | TAT-CRE | Excellgen | Cat# Eg-1001 | Cell permeant CRE protein |
| Commercial assay or kit | Dynabeads protein G IP kit. | Thermo | Cat# 10007D | |
| Commercial assay or kit | Pierce firefly luc one step glow assay kit | Thermo | Cat# 16196 | |
| Software, algorithm | MEME | http://meme-suite.org | Multiple Em Motif Elucidation | |
| Software, algorithm | FIMO | http://meme-suite.org | Find Individual MOtifs | |
| Software, algorithm | GSEA | http://gsea.org | Gene Set Enrichment Analysis | |
| Software, algorithm | R | http://rstudio.com | R programming language | |
| Software, algorithm | Custom R scripts |
github.com/jevanveen
/vanveen-elife |
Referenced scripts hosted at GitHub | |
| Other | Antigen Retrieval | Syrbu and Cohen, 2011 | Antigen Retrieval Method for Immunostaining of Paraffin Sections | Method greatly aiding in immunostaining |
Contact for reagent and resource sharing
Further information and requests for reagents should be directed to and will be fulfilled by the Lead Contact, Martin McMahon (martin.mcmahon@hci.utah.edu).
Biological vs technical replication
Individual animals, tumors, and different cell lines comprise independent biological replicates. Repeated testing on the same cell line is considered technical replication.
Experimental model: Mice
All mouse work was done with the approval of either the University of California IACUC under approval #AN089594 or the University of Utah IACUC under approval #15-11014. Mice were housed in microisolator cages on ventilated racks in AAALAC accredited vivaria. Mice were housed in groups, as possible, and were provided bedding enrichment. Animals were provided standard laboratory rodent chow or Capecchi’s breeder diet when appropriate. Cages were supplied with water via a lixit system built into the housing rack or with a water bottle placed in the microisolator cage. Institute husbandry staff performed twice daily health checks. For breeding purposes, FVB/N and C57BL/6J mice were obtained from the Jackson Laboratory. In all animal experiments, animals were age matched to within 4 weeks of one another, all being between 3 to 4 months old. A power analysis was conducted in R to determine the number of animals to include based on RNA-Seq data of Sftpa from a previous experiment (power.t.test(delta = 2895.4, sd = 918, sig.level = 0.05, power = 0.8)) indicating 3.4 mice per group would be sufficient to see a 2-fold difference. This was rounded up and four mice were initiated for each time point and genotype. Equal numbers of male and female mice were selected for each time point and genotype. Mice were then randomized within sex and genotype and assigned to groups for harvest at different time points such that at each time point, 2 females and two males were euthanized for analysis. All mice used in these experiments were completely drug naïve and had never undergone other experimental procedures. Mice were on a mixed background of C57BL/6, 129, and FVB. Tumor initiation was performed by experimenters blinded to genotype.
Experimental model: Cell lines
MLE-12 immortalized lung cells were newly obtained from ATCC and therefore assumed to be of the correct identity and to be free of mycoplasma contamination. MLE-12 cells were cultured in HITES medium supplemented with 2% FBS (HyClone) and penicillin/streptomycin. 293 T cells were from a frozen lab stock, whose identity was confirmed by STR profiling at the Huntsman Cancer Institute DNA sequencing core, and whose mycoplasma contamination status was confirmed to be negative by PCR. 293 T cells were maintained in DMEM (Life Technologies) supplemented with 10% FBS (HyClone) and supplemented with 5 mM glutamine and penicillin/streptomycin.
Vector construction
All PCR steps were performed with CloneAmp (Clontech) high-fidelity polymerase premix and all newly constructed vectors were verified by Sanger sequencing. The targeting vector used to produce the BRafCAT mouse strain was built by the cloning of three fragments into the dual selection targeting vector pDTA-TK. Two fragments, comprising 4.8 kb and 3.8 kb targeting homology arms were amplified from a C57BL/6J BAC containing the mouse BRaf locus. A third fragment comprising the entirety of the genetically engineered module was assembled by gene synthesis (Genewiz). The three fragments were cloned into the AGEI site of pDTA-TK using In-Fusion (Clontech).
New luciferase reporter constructs for the promoters of mouse surfactant proteins A, B, and C were created by amplification of mouse genomic DNA from a tail biopsy. Primer blast (NCBI) was used to create primers which captured 4500–5500 base pairs of promoter sequence beginning with the bases found immediately before the first annotated transcribed exon (ensembl.org). The TCF/LEF sites found in the M50 Super Top Flash construct were removed by digestion with KPNI and XHOI and In-Fusion was used to clone the SFTPA, B, or C promoters in their place. The FUW-Kate plasmid was constructed by gene synthesis (IDT) of sequence encoding the mKate2 red fluorophore with ends compatible for In-Fusion cloning into the EcoRI and BamHI sites of FUW.
ES cell targeting and screening
The BRafCAT targeting construct was linearized by restriction enzyme digestion with the rare cutting enzyme I-CeuI and electroporated into 2H1 BrafCA/+ ES cells, which were selected for construct integration using puromycin. Three 96-well plates of resistant clones were screened via PCR using one primer specific to the targeting construct and one primer found in the mouse genome, outside of the construct homology arms, such that a 4.8 kb product would be the result of homologous targeting construct integration, whereas integration by NHEJ would yield no product. Cell permeant TAT-CRE was added directly to culture media at a final concentration of 1 uM to test for functionality and CRE dependence of the fluorophore. Purified TAT-CRE was obtained from Excellgen (Rockville, MD).
Tumor induction
Mice were euthanized for analysis of lung tumor cell fluorescence at 2, 6, or 12 weeks p.i. Mice destined for lung harvest at either 2 or 6 weeks were initiated with 107 pfu of Ad5-Sftpc-CRE (Fasbender et al., 1998; Sutherland et al., 2014). Mice destined for lung harvest at 12 weeks were initiated with a lower titer (106 pfu) of Ad5-Sftpc-CRE to avoid encountering premature endpoints due to tumor burden.
Tissue harvest
At euthanasia, mice were perfused by first cutting the vena cava caudalis underneath the liver and then injection of DEPC treated PBS into the right ventricle of the heart until lungs turned white (Arlt et al., 2012). The cranial, medial and caudal lobes of the right lung were first taken and placed into ice cold PBS and placed on ice. A new syringe and needle containing 10% neutral buffered formalin (NBF) was inserted into the larynx of mice and 10 ml was slowly infused to initiate fixation of the remaining lung lobes. The two remaining partially fixed lung lobes were placed into 25 ml of NBF and incubated for 24 hr before being processed into paraffin and sectioned.
Tissue dissociation and FACS
Tumor bearing lungs were minced using fine scissors in a 0.5 mg/ml solution of Liberase TM (Roche). Minced tissue was incubated in a 37°C degree water bath for 15 min before being dissociated by pipetting up and down with a 1 ml pipette tip. Red blood cell lysis was performed by the addition of BD PharmLyse to 1x concentration and samples were incubated for an additional 10 min. Samples were passed through a 100 um filter fitted on a 50 ml conical tube. Filters were rinsed with 9 ml of ice cold Hanks Balanced Salt Solution (HBSS) and flow through was pelleted by centrifugation. From this point on, cells were kept on ice until lysis. Pellets were resuspended in 10 ml ice cold HBSS and passed through a 70 um filter affixed to the same 50 ml conical tube. Finally, dissociated cells were resuspended in 1 ml HBSS and passed through 35 um cell strainer cap into 5 mL round bottom polystyrene tubes. FACS was performed on a Becton-Dickinson ARIA III fitted with 100 uM nozzle, using gates as shown in the figures. tdTomato positive cells were sorted into RLT lysis buffer, homogenized and stored at −80°C until RNA purification.
Library Construction and Sequencing cDNA libraries for RNA-Sequencing experiments were produced by the High Throughput Genomics Core at the Huntsman Cancer Center. RNA was purified using the Qiagen RNeasy micro system. RNA integrity was assayed using the Agilent TapeStation 2200 and High Sensitivity RNA ScreenTapes. RNA data was included in final analyses if RINe values were above 6. No other exclusion of samples was done. For all samples, libraries were prepared using the Nugen Ovation Ultralow Library System V2. Libraries were sequenced using an Illumina HiSeq 2000 device with 50 single end cycles and v4 chemistry.
Bioinformatics
For RNA sequencing analysis, RNA transcript abundance was estimated using Salmon with default parameters on the main instance of the Galaxy webserver (https://usegalaxy.org). Differentially expressed genes were then determined by use of DESeq2 using default parameters on the main instance of the Galaxy webserver (https://usegalaxy.org), resulting in the datasets Figure 2—source data 1, Figure 7—source data 1. Gene set enrichment analysis was next performed using the R-package ‘fgsea’ with default parameters using the scripts provided as Figure 2—source code 1, Figure 3—source code 1, Figure 7—source code 1. Gene correlation network analysis was performed in the R-package ‘WGCNA’ with the following parameters: To decrease noise, genes were filtered for minimal expression (R-norm >40), leaving 14207 genes to be clustered. These genes were clustered in a single block with a soft-thresholding power of ‘3’ as recommended in the WGCNA documentation based on the scale free topology fit index of our data. WGCNA R script provided as Figure 6—source code 1, data provided as Figure 6—source data 1. For motif discovery, the promoter regions from the top 100 most specific AT2 marker genes were defined as 5 kb upstream of the transcriptional start site, and downloaded from biomart (https://www.ensembl.org/biomart). This list of sequences was filtered by repeat masker to remove low complexity DNA (repeatmasker.org). The filtered list was analyzed for enriched novel motifs using MEME (http://meme-suite.org) with default settings less the following parameters: Find 25 motifs of width between 6 and 25 nucleotides. Novel motifs were matched to known transcription factor motifs from human and mouse (HOCOMOCO v11 full) using TomTom (http://meme-suite.org) with default settings. To determine if PI3’-lipid signaling strength affects Ppargc1a transcript levels in human tumors, lung adenocarcinoma data were downloaded from the NCI Genomic Data Commons Data Portal and segregated into those cases predicted to have strong or weak activation of PI3’-lipid signaling (Figure 6—figure supplement 1—source data 1). The groups were defined as such: ‘Strong activation’ due to mutation in at least one of the following genes: Pik3ca, Pten, Pik3r1, and Akt1, ‘Unknown PI3K activation status’ due to none of these mutations being detectable. FPKM values for Ppargc1a were then compared between these two groups. This resulted in n = 211 control samples and n = 19 mutant samples with predicted strong activation of PI3K signaling. All R scripts written for this study are available at GitHub (van Veen, 2019; copy archived at https://github.com/elifesciences-publications/vanveen-elife).
Tissue processing and antibody staining
Harvested tissues were processed and embedded in paraffin, and sectioned at 4 uM. After deparaffinization in Citra-Clear (Stat Lab, McKinney, TX), sections were re-hydrated in an ethanol series and antigens were unmasked using heated incubation in Tris-EDTA-SDS (Syrbu and Cohen, 2011). Sections were blocked for non-specific interaction in 10% Normal Donkey Serum in PBS and antibody staining was performed using the following primary antibody concentrations: PGC1α (AB3242) 1:50. NKX2-1 (AB76013) 1:250. Phospho-S327-NKX2-1 (13608) 1:250. FOXA1 (AB23738) 1:250. FOXA2 (D56D6) 1:250. SFTPA (SC-7699) 1:250. Lysozyme (AB108508) 1:250. SFTPC (SC-7705) 1:250. CCA (SC-9772) 1:1000. AQP5 (SC-9890) 1:50. Primary antibody incubation was performed overnight at four degrees. After washing, alexa-488 and alexa-594 conjugated donkey anti mouse and donkey anti rabbit secondary antibodies were diluted 1:250, and incubated on sections for 2 hr at room temperature. Stained sections were counterstained in DAPI and mounted in fluoromount G.
Microscopy and quantitation of immunofluorescent images
For overview see Figure 3—figure supplement 1. Fluorescent imaging in Figure 6d was performed on a Zeiss Apotome. Fluorescent imaging in Figure 5 was performed on a Leica DM1000. All other fluorescent imaging was performed on a Nikon Ti-E inverted microscope employing a high sensitivity Andor Clara CCD camera. All images being compared in figures and in quantification were captured at exactly the same parameters for light and exposure. Acquisition settings were set such that pixel intensities were below saturation within regions of interest. When image intensity scales were adjusted for clarity, the intensity scales of images compared were set at exactly the same input and output levels. Intensity scales were never modified before quantitation. Images of tumor bearing lungs were imported into NIH ImageJ, where individual tumors were traced, and matched TIFF files were exported for each available fluorescent channel. A custom pipeline was built in CellProfiler to identify tumor cells based first upon identifying tumor nuclei using NKX2-1 immunoreactivity, when available, or DAPI staining when NKX2-1 immunostaining had not been performed. Tumor cells were defined based on propagation from identified nuclei, and tumor cytoplasm was defined as tumor cell minus tumor nucleus. For tumors analyzed in Kras based models, tumors were more diffuse and intermingled with surrounding parenchyma and so identifying tumor cells based on propagation from nuclei led to poor performance, and so tumor cells were defined as a three pixel ring around the tumor nucleus. Measurements were taken from pertinent TIFF files within individual nuclear, cellular, and cytoplasmic objects. Data were exported into comma separated value files and imported into R Studio using a custom script. For the purposes of graphing, individual tumor cell points were graphed using a custom script employing the R function ggplot(). For all measurements, median fluorescence within each cellular object was the primary data output. For the purposes of quantification, tumor cells were not treated as independent, but whole tumor averages were considered (mean of median fluorescence values), and each tumor was treated as independent. Fluorescence was not assumed to fit a normal distribution, and as such two factor comparisons were done using Wilcoxon Rank Sum test to generate p values using the R function wilcoxon.test(). For comparisons of more than two conditions, one way ANOVA was performed using aov() followed by Tukey’s honest significant difference using TukeyHSD(). Chi-Squared tests were performed in R with the function chisq.test(). When quadrants were drawn defining ‘negative’ and ‘positive’ staining: BRAFV600E driven tumors were noted to have relatively uniform positive expression of markers studied, and so ‘negative’ was defined as any tumor cell with median fluorescence less than one standard deviation below the mean of median fluorescence in BRAFV600E driven tumor cells. For all imaging and quantification, images were captured from 2 to 4 separate animals bearing tumors per group. Specific scripts and data for figures as follows: Figure 3: CellProfiler pipeline (Figure 3—source code 3) used with raw images to produce Figure 3—source data 1, 2 and 3. Figure 3—source data 1, 2 and 3 then used with Figure 3—source code 2 to perform statistics and produce graphs. Figure 4: CellProfiler pipeline (Figure 4—source code 2 and Figure 4—source code 3) used with raw images to produce Figure 4—source data 1 and Figure 4—source data 2. Figure 4—source data 1 and 2 then used with Figure 4—source code 1 to perform statistics and produce graphs. Figure 5: Cellprofiler pipeline (Figure 5—source code 2) used with raw images to produce Figure 5—source data 1. Figure 5—source data 1 then used with Figure 5—source code 1 to perform statistics and produce graphs. Figure 7: CellProfiler pipeline (Figure 3—source code 3) used with raw images to produce Figure 7—source data 1. Figure 7—source data 1 then used with Figure 7—source code 2 to perform statistics and produce graphs.
Luciferase assays
Using Fugene 6, HEK293 cells were co-transfected with luciferase reporter constructs, candidate transcriptional regulators, a fluorescent reporter construct to measure transfection efficiency (FUW-Kate), and empty vector (pUC19) to standardize total amount of DNA transfected across conditions to 100 ng/well of 96 well plate. Transfection efficiency was measured by fluorescence on an Incucyte ZOOM automated microscopy system (https://www.essenbioscience.com/). Luciferase production was measured with the Pierce Firefly Luc One-Step Glow Assay Kit, normalized to transfection efficiency, and represented as fold change over cells transfected with no candidate transcriptional regulators. All assays were performed in triplicate. Data provided as Figure 7—source data 3.
Protein biochemistry
For immunoblot analysis of protein expression in MLE-12 cells, cells were lysed on ice in RIPA buffer supplemented with Thermo Halt protease inhibitor complex. Lysates were separated by acrylamide electrophoresis on pre-cast Novex 4–12% gradient Bis-Tris gels and transferred onto PVDF membranes using an Invitrogen iblot two transfer device. After blocking of non-specific interactions using Li-Cor blocking reagent, membranes were incubated in PBS containing antibodies at the following concentrations: SFTPC: (sc-13979) 1:1000; SFTPA: (sc-13977), 1:1000; NKX2-1: (ab76013), 1:1000; FOXA1: (58613), 1:2500; PGC1α: (ab3242), 1:500; NR5A2 (ab153944), 1:1000. Protocol was repeated twice for a total of n = 3 with equivalent results.
For co-immunoprecipitation experiments, 10 ug of the following antibodies were bound to Dynabeads magnetic Protein G beads (Ms anti-PGC1α (1F3.9), Rb anti-NKX2-1 (AB76013), Normal Rabbit IgG (CST#2729), Mouse IgG1 (CST#5415)) for 15 min at room temperature. All following steps were performed at four degrees centigrade. MLE-12 cells were lysed by 15 passages through a 25 gauge needle in the following buffer: 20 mM Tris HCl pH 8, 137 mM NaCl, 0.1%(v/v) Nonidet-P40. Lysates were centrifuged for 5 min at 1000xg to remove insoluble fraction. Cleared lysates were divided and incubated with either target antibody or IgG bound magnetic beads for 30 min before proceeding with washing and elution steps following product protocol. Eluates were separated by acrylamide electrophoresis on pre-cast Novex 4–12% gradient Bis-Tris gels and transferred onto PVDF membranes using an Invitrogen iblot two transfer device. After blocking of non-specific interactions using Li-Cor blocking reagent, membranes were incubated in PBS containing antibodies at the following concentrations: NKX2-1: (ab76013), 1:1000; PGC1α: (ab3242), 1:500. Protocol was repeated twice for a total of n = 3 with equivalent results.
Acknowledgements
The authors would like to thank: Tim Mosbruger in the Bioinformatics Core at the Huntsman Cancer Institute (HCI); The Embryonic Stem Cell Core at the University of California, San Francisco (UCSF); The Gladstone Transgenic Gene-Targeting Core at UCSF; The Pathology cores at both UCSF and HCI; Brian Dalley and the the High Throughput Genomics Core at the Huntsman Cancer Center; and The FACS Facility at the Helen Diller Comprehensive Cancer Center at UCSF. We also thank Joseph Juan for assistance in tumor induction, Alex Jones and Eric Snyder for generously sharing the PCDH-FOXA1 construct pre-publication, Eric Snyder for helpful discussions and critical manuscript editing, Stephanie Correa for helpful discussions and equipment usage, and Holly Ingraham for generously sharing the pCDNA3-mLRH1 construct pre-publication. Dr. McMahon and colleagues gratefully acknowledge philanthropic support for this research from Five for the Fight.
Funding Statement
The funders had no role in study design, data collection and interpretation, or the decision to submit the work for publication.
Contributor Information
Martin McMahon, Email: martin.mcmahon@hci.utah.edu.
Jonathan A Cooper, Fred Hutchinson Cancer Research Center, United States.
Maureen Murphy, The Wistar Institute, United States.
Funding Information
This paper was supported by the following grants:
National Cancer Institute NCI R01_CA131261 to Martin McMahon.
SASS Postdoctoral Fellowship to J Edward van Veen, Martin McMahon.
University of California, San Francisco Program for Breakthrough Biomedical Research to J Edward van Veen, Martin McMahon.
National Cancer Institute 5T32CA108462-1 to J Edward van Veen, Martin McMahon.
National Cancer Institute NCI P30_CA042014 to Martin McMahon.
Additional information
Competing interests
Reviewing editor, eLife.
No competing interests declared.
Author contributions
Conceptualization, Data curation, Software, Formal analysis, Supervision, Funding acquisition, Validation, Investigation, Visualization, Methodology, Writing—original draft, Project administration, Writing—review and editing.
Conceptualization, Data curation, Supervision, Investigation, Methodology, Writing—review and editing.
Conceptualization, Investigation, Writing—review and editing.
Conceptualization, Investigation, Writing—review and editing.
Investigation, Writing—review and editing.
Conceptualization, Investigation, Writing—review and editing.
Conceptualization, Investigation, Writing—review and editing.
Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Writing—review and editing.
Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Writing—review and editing.
Ethics
Animal experimentation: All mouse work was done with the approval of the University of California IACUC under approval #AN089594. Mice were housed in microisolator cages on ventilated racks in an AAALAC accredited facility.
Additional files
Data availability
Sequencing data have been deposited in GEO under accession code GSE123126. All R scripts written for this study are available at GitHub (https://github.com/jevanveen/vanveen-elife; copy archived at https://github.com/elifesciences-publications/vanveen-elife).
The following dataset was generated:
van Veen JE, Scherzer M, Boshuizen J, Chu M, Liu A, Landman A, Green S, McMahon M. 2018. Mutationally-activated PI3'-kinase-α promotes de-differentiation of lung tumors initiated by the BRAFV600E oncoprotein kinase. NCBI Gene Expression Omnibus. GSE123126
The following previously published dataset was used:
Joshua D Campbell, Anton Alexandrov, Jaegil Kim, Jeremiah Wala, Alice H Berger, Chandra Sekhar Pedamallu, Sachet A Shukla, Guangwu Guo, Angela N Brooks, Bradley A Murray, Marcin Imielinski, Xin Hu, Shiyun Ling, Rehan Akbani, Mara Rosenberg, Carrie Cibulskis, Aruna Ramachandran, Eric A Collisson, David J Kwiatkowski, Michael S Lawrence, John N Weinstein, Roel G W Verhaak, Catherine J Wu, Peter S Hammerman, Andrew D Cherniack, Gad Getz, Cancer Genome Atlas Research Network, Maxim N Artyomov, Robert Schreiber, Ramaswamy Govindan, Matthew Meyerson. 2016. Distinct patterns of somatic genome alterations in lung adenocarcinomas and squamous cell carcinomas. cBioPortal. nsclc_tcga_broad_2016
References
- Arlt MJ, Born W, Fuchs B. Improved visualization of lung metastases at single cell resolution in mice by combined in-situ perfusion of lung tissue and X-Gal staining of lacZ-tagged tumor cells. Journal of Visualized Experiments. 2012:e4162. doi: 10.3791/4162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey TL, Boden M, Buske FA, Frith M, Grant CE, Clementi L, Ren J, Li WW, Noble WS. MEME SUITE: tools for motif discovery and searching. Nucleic Acids Research. 2009;37:W202–W208. doi: 10.1093/nar/gkp335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey TL, Elkan C. Fitting a mixture model by expectation maximization to discover motifs in biopolymers. Proceedings. International Conference on Intelligent Systems for Molecular Biology. 1994;2:28–36. [PubMed] [Google Scholar]
- Bruno MD, Bohinski RJ, Huelsman KM, Whitsett JA, Korfhagen TR. Lung cell-specific expression of the murine surfactant protein A (SP-A) gene is mediated by interactions between the SP-A promoter and thyroid transcription factor-1. Journal of Biological Chemistry. 1995;270:6531–6536. doi: 10.1074/jbc.270.12.6531. [DOI] [PubMed] [Google Scholar]
- Camolotto SA, Pattabiraman S, Mosbruger TL, Jones A, Belova VK, Orstad G, Streiff M, Salmond L, Stubben C, Kaestner KH, Snyder EL. FoxA1 and FoxA2 drive gastric differentiation and suppress squamous identity in NKX2-1-negative lung Cancer. eLife. 2018;7:e38579. doi: 10.7554/eLife.38579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell JD, Alexandrov A, Kim J, Wala J, Berger AH, Pedamallu CS, Shukla SA, Guo G, Brooks AN, Murray BA, Imielinski M, Hu X, Ling S, Akbani R, Rosenberg M, Cibulskis C, Ramachandran A, Collisson EA, Kwiatkowski DJ, Lawrence MS, Weinstein JN, Verhaak RG, Wu CJ, Hammerman PS, Cherniack AD, Getz G, Artyomov MN, Schreiber R, Govindan R, Meyerson M, Cancer Genome Atlas Research Network Distinct patterns of somatic genome alterations in lung adenocarcinomas and squamous cell carcinomas. Nature Genetics. 2016;48:607–616. doi: 10.1038/ng.3564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cancer Genome Atlas Research Network Comprehensive molecular profiling of lung adenocarcinoma. Nature. 2014;511:543–550. doi: 10.1038/nature13385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capon DJ, Seeburg PH, McGrath JP, Hayflick JS, Edman U, Levinson AD, Goeddel DV. Activation of Ki-ras2 gene in human Colon and lung carcinomas by two different point mutations. Nature. 1983;304:507–513. doi: 10.1038/304507a0. [DOI] [PubMed] [Google Scholar]
- Cassel TN, Berg T, Suske G, Nord M. Synergistic transactivation of the differentiation-dependent lung gene clara cell secretory protein (secretoglobin 1a1) by the basic region leucine zipper factor CCAAT/enhancer-binding protein alpha and the homeodomain factor Nkx2.1/thyroid transcription factor-1. Journal of Biological Chemistry. 2002;277:36970–36977. doi: 10.1074/jbc.M201293200. [DOI] [PubMed] [Google Scholar]
- Castellano E, Sheridan C, Thin MZ, Nye E, Spencer-Dene B, Diefenbacher ME, Moore C, Kumar MS, Murillo MM, Grönroos E, Lassailly F, Stamp G, Downward J. Requirement for interaction of PI3-kinase p110α with RAS in lung tumor maintenance. Cancer Cell. 2013;24:617–630. doi: 10.1016/j.ccr.2013.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalmers ZR, Connelly CF, Fabrizio D, Gay L, Ali SM, Ennis R, Schrock A, Campbell B, Shlien A, Chmielecki J, Huang F, He Y, Sun J, Tabori U, Kennedy M, Lieber DS, Roels S, White J, Otto GA, Ross JS, Garraway L, Miller VA, Stephens PJ, Frampton GM. Analysis of 100,000 human Cancer genomes reveals the landscape of tumor mutational burden. Genome Medicine. 2017;9:34. doi: 10.1186/s13073-017-0424-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles RP, Iezza G, Amendola E, Dankort D, McMahon M. Mutationally activated BRAF(V600E) elicits papillary thyroid Cancer in the adult mouse. Cancer Research. 2011;71:3863–3871. doi: 10.1158/0008-5472.CAN-10-4463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charles RP, Silva J, Iezza G, Phillips WA, McMahon M. Activating BRAF and PIK3CA mutations cooperate to promote anaplastic thyroid carcinogenesis. Molecular Cancer Research. 2014;12:979–986. doi: 10.1158/1541-7786.MCR-14-0158-T. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W-J, Ho C-C, Chang Y-L, Chen H-Y, Lin C-A, Ling T-Y, Yu S-L, Yuan S-S, Louisa Chen Y-J, Lin C-Y, Pan S-H, Elizabeth Chou H-Y, Chen Y-J, Chang G-C, Chu W-C, Lee Y-M, Lee J-Y, Lee P-J, Li K-C, Chen H-W, Yang P-C. Cancer-associated fibroblasts regulate the plasticity of lung Cancer stemness via paracrine signalling. Nature Communications. 2014;5:e3472. doi: 10.1038/ncomms4472. [DOI] [PubMed] [Google Scholar]
- Cicchini M, Buza EL, Sagal KM, Gudiel AA, Durham AC, Feldser DM. Context-Dependent effects of amplified MAPK signaling during lung adenocarcinoma initiation and progression. Cell Reports. 2017;18:1958–1969. doi: 10.1016/j.celrep.2017.01.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daitoku H, Yamagata K, Matsuzaki H, Hatta M, Fukamizu A. Regulation of PGC-1 promoter activity by protein kinase B and the forkhead transcription factor FKHR. Diabetes. 2003;52:642–649. doi: 10.2337/diabetes.52.3.642. [DOI] [PubMed] [Google Scholar]
- Dane KY, Chan LA, Rice JJ, Daugherty PS. Isolation of cell specific peptide ligands using fluorescent bacterial display libraries. Journal of Immunological Methods. 2006;309:120–129. doi: 10.1016/j.jim.2005.11.021. [DOI] [PubMed] [Google Scholar]
- Dankort D, Filenova E, Collado M, Serrano M, Jones K, McMahon M. A new mouse model to explore the initiation, progression, and therapy of BRAFV600E-induced lung tumors. Genes & Development. 2007;21:379–384. doi: 10.1101/gad.1516407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dankort D, Curley DP, Cartlidge RA, Nelson B, Karnezis AN, Damsky WE, You MJ, DePinho RA, McMahon M, Bosenberg M. Braf(V600E) cooperates with pten loss to induce metastatic melanoma. Nature Genetics. 2009;41:544–552. doi: 10.1038/ng.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeFelice M, Silberschmidt D, DiLauro R, Xu Y, Wert SE, Weaver TE, Bachurski CJ, Clark JC, Whitsett JA. TTF-1 phosphorylation is required for peripheral lung morphogenesis, perinatal survival, and tissue-specific gene expression. Journal of Biological Chemistry. 2003;278:35574–35583. doi: 10.1074/jbc.M304885200. [DOI] [PubMed] [Google Scholar]
- Desai TJ, Brownfield DG, Krasnow MA. Alveolar progenitor and stem cells in lung development, renewal and Cancer. Nature. 2014;507:190–194. doi: 10.1038/nature12930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Palma T, Nitsch R, Mascia A, Nitsch L, Di Lauro R, Zannini M. The paired domain-containing factor Pax8 and the homeodomain-containing factor TTF-1 directly interact and synergistically activate transcription. Journal of Biological Chemistry. 2003;278:3395–3402. doi: 10.1074/jbc.M205977200. [DOI] [PubMed] [Google Scholar]
- Drilon A, Laetsch TW, Kummar S, DuBois SG, Lassen UN, Demetri GD, Nathenson M, Doebele RC, Farago AF, Pappo AS, Turpin B, Dowlati A, Brose MS, Mascarenhas L, Federman N, Berlin J, El-Deiry WS, Baik C, Deeken J, Boni V, Nagasubramanian R, Taylor M, Rudzinski ER, Meric-Bernstam F, Sohal DPS, Ma PC, Raez LE, Hechtman JF, Benayed R, Ladanyi M, Tuch BB, Ebata K, Cruickshank S, Ku NC, Cox MC, Hawkins DS, Hong DS, Hyman DM. Efficacy of larotrectinib in TRK Fusion-Positive cancers in adults and children. The New England Journal of Medicine. 2018;378:731–739. doi: 10.1056/NEJMoa1714448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engelman JA, Chen L, Tan X, Crosby K, Guimaraes AR, Upadhyay R, Maira M, McNamara K, Perera SA, Song Y, Chirieac LR, Kaur R, Lightbown A, Simendinger J, Li T, Padera RF, García-Echeverría C, Weissleder R, Mahmood U, Cantley LC, Wong KK. Effective use of PI3K and MEK inhibitors to treat mutant kras G12D and PIK3CA H1047R murine lung cancers. Nature Medicine. 2008;14:1351–1356. doi: 10.1038/nm.1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fasbender A, Lee JH, Walters RW, Moninger TO, Zabner J, Welsh MJ. Incorporation of adenovirus in calcium phosphate precipitates enhances gene transfer to airway epithelia in vitro and in vivo. Journal of Clinical Investigation. 1998;102:184–193. doi: 10.1172/JCI2732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnett S, Dutchak KL, McDonough RV, Dankort D. p53 loss does not permit escape from braf(V600E)-induced senescence in a mouse model of lung Cancer. Oncogene. 2017;511:543. doi: 10.1038/onc.2017.235. [DOI] [PubMed] [Google Scholar]
- Green S, Trejo CL, McMahon M. PIK3CA(H1047R) Accelerates and enhances KRAS(G12D)-Driven lung tumorigenesis. Cancer Research. 2015;75:5378–5391. doi: 10.1158/0008-5472.CAN-15-1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S, Stamatoyannopoulos JA, Bailey TL, Noble WS. Quantifying similarity between motifs. Genome Biology. 2007a;8:R24. doi: 10.1186/gb-2007-8-2-r24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S, Ramjaun AR, Haiko P, Wang Y, Warne PH, Nicke B, Nye E, Stamp G, Alitalo K, Downward J. Binding of ras to phosphoinositide 3-kinase p110alpha is required for ras-driven tumorigenesis in mice. Cell. 2007b;129:957–968. doi: 10.1016/j.cell.2007.03.051. [DOI] [PubMed] [Google Scholar]
- Hamvas A, Deterding RR, Wert SE, White FV, Dishop MK, Alfano DN, Halbower AC, Planer B, Stephan MJ, Uchida DA, Williames LD, Rosenfeld JA, Lebel RR, Young LR, Cole FS, Nogee LM. Heterogeneous pulmonary phenotypes associated with mutations in the thyroid transcription factor gene NKX2-1. Chest. 2013;144:794–804. doi: 10.1378/chest.12-2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han X, Wang R, Zhou Y, Fei L, Sun H, Lai S, Saadatpour A, Zhou Z, Chen H, Ye F, Huang D, Xu Y, Huang W, Jiang M, Jiang X, Mao J, Chen Y, Lu C, Xie J, Fang Q, Wang Y, Yue R, Li T, Huang H, Orkin SH, Yuan GC, Chen M, Guo G. Mapping the mouse cell atlas by Microwell-Seq. Cell. 2018;173:1307. doi: 10.1016/j.cell.2018.05.012. [DOI] [PubMed] [Google Scholar]
- Haq R, Shoag J, Andreu-Perez P, Yokoyama S, Edelman H, Rowe GC, Frederick DT, Hurley AD, Nellore A, Kung AL, Wargo JA, Song JS, Fisher DE, Arany Z, Widlund HR. Oncogenic BRAF regulates oxidative metabolism via PGC1α and MITF. Cancer Cell. 2013;23:302–315. doi: 10.1016/j.ccr.2013.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heist RS, Engelman JA. SnapShot: non-small cell lung Cancer. Cancer Cell. 2012;21:448–448.e2. doi: 10.1016/j.ccr.2012.03.007. [DOI] [PubMed] [Google Scholar]
- Huillard E, Hashizume R, Phillips JJ, Griveau A, Ihrie RA, Aoki Y, Nicolaides T, Perry A, Waldman T, McMahon M, Weiss WA, Petritsch C, James CD, Rowitch DH. Cooperative interactions of BRAFV600E kinase and CDKN2A locus deficiency in pediatric malignant astrocytoma as a basis for rational therapy. PNAS. 2012;109:8710–8715. doi: 10.1073/pnas.1117255109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyman DM, Puzanov I, Subbiah V, Faris JE, Chau I, Blay JY, Wolf J, Raje NS, Diamond EL, Hollebecque A, Gervais R, Elez-Fernandez ME, Italiano A, Hofheinz RD, Hidalgo M, Chan E, Schuler M, Lasserre SF, Makrutzki M, Sirzen F, Veronese ML, Tabernero J, Baselga J. Vemurafenib in multiple nonmelanoma cancers with BRAF V600 mutations. The New England Journal of Medicine. 2015;373:726–736. doi: 10.1056/NEJMoa1502309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson EL, Willis N, Mercer K, Bronson RT, Crowley D, Montoya R, Jacks T, Tuveson DA. Analysis of lung tumor initiation and progression using conditional expression of oncogenic K-ras. Genes & Development. 2001;15:3243–3248. doi: 10.1101/gad.943001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juan J, Muraguchi T, Iezza G, Sears RC, McMahon M. Diminished WNT -> β-catenin -> c-MYC signaling is a barrier for malignant progression of BRAFV600E-induced lung tumors. Genes & Development. 2014;28:561–575. doi: 10.1101/gad.233627.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemper MF, Stirone C, Krause DN, Duckles SP, Procaccio V. Genomic and non-genomic regulation of PGC1 isoforms by estrogen to increase cerebral vascular mitochondrial biogenesis and reactive oxygen species protection. European Journal of Pharmacology. 2014;723:322–329. doi: 10.1016/j.ejphar.2013.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim CF, Jackson EL, Woolfenden AE, Lawrence S, Babar I, Vogel S, Crowley D, Bronson RT, Jacks T. Identification of bronchioalveolar stem cells in normal lung and lung Cancer. Cell. 2005;121:823–835. doi: 10.1016/j.cell.2005.03.032. [DOI] [PubMed] [Google Scholar]
- Kinross KM, Montgomery KG, Kleinschmidt M, Waring P, Ivetac I, Tikoo A, Saad M, Hare L, Roh V, Mantamadiotis T, Sheppard KE, Ryland GL, Campbell IG, Gorringe KL, Christensen JG, Cullinane C, Hicks RJ, Pearson RB, Johnstone RW, McArthur GA, Phillips WA. An activating Pik3ca mutation coupled with pten loss is sufficient to initiate ovarian tumorigenesis in mice. Journal of Clinical Investigation. 2012;122:553–557. doi: 10.1172/JCI59309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwei KA, Kim YH, Girard L, Kao J, Pacyna-Gengelbach M, Salari K, Lee J, Choi YL, Sato M, Wang P, Hernandez-Boussard T, Gazdar AF, Petersen I, Minna JD, Pollack JR. Genomic profiling identifies TITF1 as a lineage-specific oncogene amplified in lung Cancer. Oncogene. 2008;27:3635–3640. doi: 10.1038/sj.onc.1211012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langfelder P, Horvath S. WGCNA: an R package for weighted correlation network analysis. BMC Bioinformatics. 2008;9:559. doi: 10.1186/1471-2105-9-559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazzaro D, Price M, de Felice M, Di Lauro R. The transcription factor TTF-1 is expressed at the onset of thyroid and lung morphogenesis and in restricted regions of the foetal brain. Development. 1991;113:1093–1104. doi: 10.1242/dev.113.4.1093. [DOI] [PubMed] [Google Scholar]
- Livet J, Weissman TA, Kang H, Draft RW, Lu J, Bennis RA, Sanes JR, Lichtman JW. Transgenic strategies for combinatorial expression of fluorescent proteins in the nervous system. Nature. 2007;450:56–62. doi: 10.1038/nature06293. [DOI] [PubMed] [Google Scholar]
- Madisen L, Zwingman TA, Sunkin SM, Oh SW, Zariwala HA, Gu H, Ng LL, Palmiter RD, Hawrylycz MJ, Jones AR, Lein ES, Zeng H. A robust and high-throughput cre reporting and characterization system for the whole mouse brain. Nature Neuroscience. 2010;13:133–140. doi: 10.1038/nn.2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maeda Y, Tsuchiya T, Hao H, Tompkins DH, Xu Y, Mucenski ML, Du L, Keiser AR, Fukazawa T, Naomoto Y, Nagayasu T, Whitsett JA. Kras(G12D) and Nkx2-1 haploinsufficiency induce mucinous adenocarcinoma of the lung. Journal of Clinical Investigation. 2012;122:4388–4400. doi: 10.1172/JCI64048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minoo P, Hamdan H, Bu D, Warburton D, Stepanik P, deLemos R. TTF-1 regulates lung epithelial morphogenesis. Developmental Biology. 1995;172:694–698. doi: 10.1006/dbio.1995.8080. [DOI] [PubMed] [Google Scholar]
- Molina-Arcas M, Hancock DC, Sheridan C, Kumar MS, Downward J. Coordinate direct input of both KRAS and IGF1 receptor to activation of PI3 kinase in KRAS-mutant lung Cancer. Cancer Discovery. 2013;3:548–563. doi: 10.1158/2159-8290.CD-12-0446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murillo MM, Rana S, Spencer-Dene B, Nye E, Stamp G, Downward J. Disruption of the interaction of RAS with PI 3-Kinase induces regression of EGFR-Mutant-Driven lung Cancer. Cell Reports. 2018;25:3545–3553. doi: 10.1016/j.celrep.2018.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzumdar MD, Tasic B, Miyamichi K, Li L, Luo L. A global double-fluorescent cre reporter mouse. Genesis. 2007;45:593–605. doi: 10.1002/dvg.20335. [DOI] [PubMed] [Google Scholar]
- Pacheco-Pinedo EC, Durham AC, Stewart KM, Goss AM, Lu MM, Demayo FJ, Morrisey EE. Wnt/β-catenin signaling accelerates mouse lung tumorigenesis by imposing an embryonic distal progenitor phenotype on lung epithelium. Journal of Clinical Investigation. 2011;121:1935–1945. doi: 10.1172/JCI44871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park KS, Whitsett JA, Di Palma T, Hong JH, Yaffe MB, Zannini M. TAZ interacts with TTF-1 and regulates expression of surfactant protein-C. Journal of Biological Chemistry. 2004;279:17384–17390. doi: 10.1074/jbc.M312569200. [DOI] [PubMed] [Google Scholar]
- Revel JP. Identification of glycogen in electron micrographs of thin tissue sections. The Journal of Cell Biology. 1960;8:575–589. doi: 10.1083/jcb.8.3.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Viciana P, Warne PH, Dhand R, Vanhaesebroeck B, Gout I, Fry MJ, Waterfield MD, Downward J. Phosphatidylinositol-3-OH kinase as a direct target of ras. Nature. 1994;370:527–532. doi: 10.1038/370527a0. [DOI] [PubMed] [Google Scholar]
- Rosell R, Carcereny E, Gervais R, Vergnenegre A, Massuti B, Felip E, Palmero R, Garcia-Gomez R, Pallares C, Sanchez JM, Porta R, Cobo M, Garrido P, Longo F, Moran T, Insa A, De Marinis F, Corre R, Bover I, Illiano A, Dansin E, de Castro J, Milella M, Reguart N, Altavilla G, Jimenez U, Provencio M, Moreno MA, Terrasa J, Muñoz-Langa J, Valdivia J, Isla D, Domine M, Molinier O, Mazieres J, Baize N, Garcia-Campelo R, Robinet G, Rodriguez-Abreu D, Lopez-Vivanco G, Gebbia V, Ferrera-Delgado L, Bombaron P, Bernabe R, Bearz A, Artal A, Cortesi E, Rolfo C, Sanchez-Ronco M, Drozdowskyj A, Queralt C, de Aguirre I, Ramirez JL, Sanchez JJ, Molina MA, Taron M, Paz-Ares L, Spanish Lung Cancer Group in collaboration with Groupe Français de Pneumo-Cancérologie and Associazione Italiana Oncologia Toracica Erlotinib versus standard chemotherapy as first-line treatment for european patients with advanced EGFR mutation-positive non-small-cell lung Cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. The Lancet Oncology. 2012;13:239–246. doi: 10.1016/S1470-2045(11)70393-X. [DOI] [PubMed] [Google Scholar]
- Sakamoto N, Feng Y, Stolfi C, Kurosu Y, Green M, Lin J, Green ME, Sentani K, Yasui W, McMahon M, Hardiman KM, Spence JR, Horita N, Greenson JK, Kuick R, Cho KR, Fearon ER. BRAFV600E cooperates with CDX2 inactivation to promote serrated colorectal tumorigenesis. eLife. 2017;6:e20331. doi: 10.7554/eLife.20331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scagliotti G, Novello S, von Pawel J, Reck M, Pereira JR, Thomas M, Abrão Miziara JE, Balint B, De Marinis F, Keller A, Arén O, Csollak M, Albert I, Barrios CH, Grossi F, Krzakowski M, Cupit L, Cihon F, Dimatteo S, Hanna N. Phase III study of carboplatin and paclitaxel alone or with sorafenib in advanced non-small-cell lung Cancer. Journal of Clinical Oncology. 2010;28:1835–1842. doi: 10.1200/JCO.2009.26.1321. [DOI] [PubMed] [Google Scholar]
- Schell JC, Wisidagama DR, Bensard C, Zhao H, Wei P, Tanner J, Flores A, Mohlman J, Sorensen LK, Earl CS, Olson KA, Miao R, Waller TC, Delker D, Kanth P, Jiang L, DeBerardinis RJ, Bronner MP, Li DY, Cox JE, Christofk HR, Lowry WE, Thummel CS, Rutter J. Control of intestinal stem cell function and proliferation by mitochondrial pyruvate metabolism. Nature Cell Biology. 2017;19:1027–1036. doi: 10.1038/ncb3593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shai A, Dankort D, Juan J, Green S, McMahon M. TP53 silencing bypasses growth arrest of BRAFV600E-Induced lung tumor cells in a Two-Switch model of lung tumorigenesis. Cancer Research. 2015;75:3167–3180. doi: 10.1158/0008-5472.CAN-14-3701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw AT, Kim DW, Nakagawa K, Seto T, Crinó L, Ahn MJ, De Pas T, Besse B, Solomon BJ, Blackhall F, Wu YL, Thomas M, O'Byrne KJ, Moro-Sibilot D, Camidge DR, Mok T, Hirsh V, Riely GJ, Iyer S, Tassell V, Polli A, Wilner KD, Jänne PA. Crizotinib versus chemotherapy in advanced ALK-positive lung Cancer. The New England Journal of Medicine. 2013;368:2385–2394. doi: 10.1056/NEJMoa1214886. [DOI] [PubMed] [Google Scholar]
- Shaw AT, Ou SH, Bang YJ, Camidge DR, Solomon BJ, Salgia R, Riely GJ, Varella-Garcia M, Shapiro GI, Costa DB, Doebele RC, Le LP, Zheng Z, Tan W, Stephenson P, Shreeve SM, Tye LM, Christensen JG, Wilner KD, Clark JW, Iafrate AJ. Crizotinib in ROS1-rearranged non-small-cell lung Cancer. The New England Journal of Medicine. 2014;371:1963–1971. doi: 10.1056/NEJMoa1406766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA: A Cancer Journal for Clinicians. 2016;66:7–30. doi: 10.3322/caac.21332. [DOI] [PubMed] [Google Scholar]
- Snippert HJ, van der Flier LG, Sato T, van Es JH, van den Born M, Kroon-Veenboer C, Barker N, Klein AM, van Rheenen J, Simons BD, Clevers H. Intestinal crypt homeostasis results from neutral competition between symmetrically dividing Lgr5 stem cells. Cell. 2010;143:134–144. doi: 10.1016/j.cell.2010.09.016. [DOI] [PubMed] [Google Scholar]
- Snyder EL, Watanabe H, Magendantz M, Hoersch S, Chen TA, Wang DG, Crowley D, Whittaker CA, Meyerson M, Kimura S, Jacks T. Nkx2-1 represses a latent gastric differentiation program in lung adenocarcinoma. Molecular Cell. 2013;50:185–199. doi: 10.1016/j.molcel.2013.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srinivas S, Watanabe T, Lin CS, William CM, Tanabe Y, Jessell TM, Costantini F. Cre reporter strains produced by targeted insertion of EYFP and ECFP into the ROSA26 locus. BMC Developmental Biology. 2001;1 doi: 10.1186/1471-213X-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahlman MT, Gray ME, Whitsett JA. Expression of thyroid transcription factor-1(TTF-1) in fetal and neonatal human lung. Journal of Histochemistry & Cytochemistry. 1996;44:673–678. doi: 10.1177/44.7.8675988. [DOI] [PubMed] [Google Scholar]
- Sutherland KD, Song JY, Kwon MC, Proost N, Zevenhoven J, Berns A. Multiple cells-of-origin of mutant K-Ras-induced mouse lung adenocarcinoma. PNAS. 2014;111:4952–4957. doi: 10.1073/pnas.1319963111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syrbu SI, Cohen MB. An enhanced antigen-retrieval protocol for immunohistochemical staining of formalin-fixed, paraffin-embedded tissues. Methods in Molecular Biology. 2011;717:101–110. doi: 10.1007/978-1-61779-024-9_6. [DOI] [PubMed] [Google Scholar]
- Trejo CL, Juan J, Vicent S, Sweet-Cordero A, McMahon M. MEK1/2 inhibition elicits regression of autochthonous lung tumors induced by KRASG12D or BRAFV600E. Cancer Research. 2012;72:3048–3059. doi: 10.1158/0008-5472.CAN-11-3649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trejo CL, Green S, Marsh V, Collisson EA, Iezza G, Phillips WA, McMahon M. Mutationally activated PIK3CA(H1047R) cooperates with BRAF(V600E) to promote lung Cancer progression. Cancer Research. 2013;73:6448–6461. doi: 10.1158/0008-5472.CAN-13-0681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treutlein B, Brownfield DG, Wu AR, Neff NF, Mantalas GL, Espinoza FH, Desai TJ, Krasnow MA, Quake SR. Reconstructing lineage hierarchies of the distal lung epithelium using single-cell RNA-seq. Nature. 2014;509:371–375. doi: 10.1038/nature13173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsao H, Goel V, Wu H, Yang G, Haluska FG. Genetic interaction between NRAS and BRAF mutations and PTEN/MMAC1 inactivation in melanoma. Journal of Investigative Dermatology. 2004;122:337–341. doi: 10.1046/j.0022-202X.2004.22243.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Veen JE, Pringle DR, McMahon M. P2A-Fluorophore tagging of BRAF tightly links expression to fluorescence in vivo. PLOS ONE. 2016;11:e0157661. doi: 10.1371/journal.pone.0157661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Veen JE. vanveen-elife. 64fb003GitHub. 2019 https://github.com/jevanveen/vanveen-elife
- Vivanco I, Sawyers CL. The phosphatidylinositol 3-Kinase AKT pathway in human Cancer. Nature Reviews Cancer. 2002;2:489–501. doi: 10.1038/nrc839. [DOI] [PubMed] [Google Scholar]
- Wang J, Kobayashi T, Floc'h N, Kinkade CW, Aytes A, Dankort D, Lefebvre C, Mitrofanova A, Cardiff RD, McMahon M, Califano A, Shen MM, Abate-Shen C. B-Raf activation cooperates with PTEN loss to drive c-Myc expression in advanced prostate Cancer. Cancer Research. 2012;72:4765–4776. doi: 10.1158/0008-5472.CAN-12-0820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wikenheiser KA, Vorbroker DK, Rice WR, Clark JC, Bachurski CJ, Oie HK, Whitsett JA. Production of immortalized distal respiratory epithelial cell lines from surfactant protein C/simian virus 40 large tumor antigen transgenic mice. PNAS. 1993;90:11029–11033. doi: 10.1073/pnas.90.23.11029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winslow MM, Dayton TL, Verhaak RG, Kim-Kiselak C, Snyder EL, Feldser DM, Hubbard DD, DuPage MJ, Whittaker CA, Hoersch S, Yoon S, Crowley D, Bronson RT, Chiang DY, Meyerson M, Jacks T. Suppression of lung adenocarcinoma progression by Nkx2-1. Nature. 2011;473:101–104. doi: 10.1038/nature09881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yatabe Y, Mitsudomi T, Takahashi T. TTF-1 expression in pulmonary adenocarcinomas. The American Journal of Surgical Pathology. 2002;26:767–773. doi: 10.1097/00000478-200206000-00010. [DOI] [PubMed] [Google Scholar]
- Yazawa T, Inaoka Y, Okada R, Mizutani T, Yamazaki Y, Usami Y, Kuribayashi M, Orisaka M, Umezawa A, Miyamoto K. PPAR-gamma coactivator-1alpha regulates progesterone production in ovarian granulosa cells with SF-1 and LRH-1. Molecular Endocrinology. 2010;24:485–496. doi: 10.1210/me.2009-0352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi M, Tong GX, Murry B, Mendelson CR. Role of CBP/p300 and SRC-1 in transcriptional regulation of the pulmonary surfactant protein-A (SP-A) gene by thyroid transcription factor-1 (TTF-1) Journal of Biological Chemistry. 2002;277:2997–3005. doi: 10.1074/jbc.M109793200. [DOI] [PubMed] [Google Scholar]
- Yoshizawa A, Motoi N, Riely GJ, Sima CS, Gerald WL, Kris MG, Park BJ, Rusch VW, Travis WD. Impact of proposed IASLC/ATS/ERS classification of lung adenocarcinoma: prognostic subgroups and implications for further revision of staging based on analysis of 514 stage I cases. Modern Pathology. 2011;24:653–664. doi: 10.1038/modpathol.2010.232. [DOI] [PubMed] [Google Scholar]
- Yu H, McDaid R, Lee J, Possik P, Li L, Kumar SM, Elder DE, Van Belle P, Gimotty P, Guerra M, Hammond R, Nathanson KL, Dalla Palma M, Herlyn M, Xu X. The role of BRAF mutation and p53 inactivation during transformation of a subpopulation of primary human melanocytes. The American Journal of Pathology. 2009;174:2367–2377. doi: 10.2353/ajpath.2009.081057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan B, Li C, Kimura S, Engelhardt RT, Smith BR, Minoo P. Inhibition of distal lung morphogenesis in Nkx2.1(-/-) embryos. Developmental Dynamics. 2000;217:180–190. doi: 10.1002/(SICI)1097-0177(200002)217:2<180::AID-DVDY5>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- Yuan TL, Cantley LC. PI3K pathway alterations in Cancer: variations on a theme. Oncogene. 2008;27:5497–5510. doi: 10.1038/onc.2008.245. [DOI] [PMC free article] [PubMed] [Google Scholar]