Abstract
Adolescents with sickle cell disease (SCD), a chronic condition primarily impacting African Americans, experience challenges graduating high school. Understanding demographic, educational, and community-level correlates of disease is critical to creating effective interventions for these youth. This study aimed to examine 1) educational attainment for adolescents with SCD, 2) neighborhood correlates of their education, and 3) feasibility of a pilot to increase General Education Diploma (GED) class enrollment. Findings suggest demographic characteristics influence educational attainment. Improving educational attainment in adolescents with SCD requires understanding risk beyond disease severity. Identifying risk and protective neighborhood level factors can inform interventions to improve educational attainment. Feasibility of programming to increase GED enrollment should be further investigated.
Keywords: Adolescent, Academic Attainment, Sickle Cell Disease
Introduction
Adolescents with sickle cell disease (SCD) frequently experience challenges graduating high school which impacts future participation in the labor market as well as other positive life opportunities. SCD is a chronic condition with debilitating effects altering quality of life, academic attainment, and outcomes in adulthood (McCavit, 2012; Schatz J, Brown RT, Pascual JM, Hsu L, & DeBaun MR, 2001; Schwartz, Radcliffe, & Barakat, 2009). SCD disproportionately impacts African American youth, particularly those in or near poverty. Understanding demographic, educational, and community-level correlates of disease is critical to creating effective interventions for youth with SCD.
Sickle Cell Disease
Sickle cell disease (SCD) is a chronic illness affecting approximately 100,000 Americans. SCD primarily affects individuals of African or Caribbean descent. Within the United States 1 in 400 African Americans has SCD, and 1 in 12 carries the recessive trait (Hassell, 2010; Prevention, 2018). There are four common disease genotypes found in the United States:1) Hemoglobin (Hb) SS, 2) HbSC, 3) HbS-beta plus thalassemia (HbSβ+), and 4) HbS beta null-thalassemia (HbSβ°). All four genotypes are considered SCD and have a profound impact on the health and daily life of affected individuals, while sickle cell anemia (SCA) refers only to the two most clinically severe genotypes: HbSS and HbSβ°.
SCD is a recessive, inherited disorder causing red blood cells to assume a crescent or ‘sickled’ shape in their deoxygenated state. Carrying the recessive trait conferred an adaptive advantage against malaria, and consequently disease genotypes evolved in regions of the world where malaria was common (Luzzatto, 2012). Pain, stroke, bone damage, and organ failure are common among individuals with SCD (Darbari et al., 2006; Junior, Daher & da Rocha, 2012; Ohene-Frempong et al., 1998; Pegelow et al., 2002). Without stroke screening and prevention, 11% of children with SCA genotypes experience an overt stroke by age 20. Almost 40% of those with SCA experience a silent stroke by age 18 (DeBaun et al., 2012; Ohene-Frempong et al., 1998; Pegelow et al., 2002). Overt strokes produce signs of neurological damage on physical examination, whereas silent strokes have no physical findings that correlate with the brain lesion(s). While not evident upon physical examination, silent strokes result in significant cognitive deficits and are thus particularly relevant to academic outcomes for youth with SCD. Not only are the effects of silent stroke not readily apparent upon examination, the deficits are not obvious to teachers or classmates. The high prevalence of anemia and neurological damage makes SCD an invisible disability, characterized by increased cognitive deficits and reduced academic achievement, limiting life opportunity for youth (Schatz 2001, Author 2014).
Academic achievement, attainment, & cognition in SCD
Academic achievement, or grades and scores on standardized measures, and attainment, or years of school completed, are lower for children and adolescents with SCD than for their siblings and matched peers (Schatz et al., 2001; Schatz, 2004; Wang et al., 2001). Children with SCD also have higher rates of grade retention, a measure of both achievement and attainment, and often require special education services due to inadequate academic progress (Schatz et al., 2001). In the author’s center, 28% of 14–18 year-olds who had a history of a SCD-related stroke or three or more hospitalizations in a year had been retained a grade; only 33% of 14–18 year-olds were on track to graduate high school in four years (Author, 2003). Students who are not on track to graduate in four years due to absence, grade retention, or academic course failure are at greater risk of dropping out of high school (Burrus & Roberts, 2012; Hammond, Linton, Smink, & Drew, 2007).
Children and adolescents with SCD score lower on tests of reading and math ability and experience higher rates of cognitive deficits when compared to their healthy siblings and peers (Schatz et al., 2001; Bernaudin et al., 2000; Schatz, Brown, Pascual, Hsu & DeBaun, 2001; Schatz, Finke, Kellett & Kramer, 2002). Intelligence quotient (IQ), attention, linguistic abilities, working memory, and processing speed are commonly impaired in children with SCD, particularly in children with severe anemia or strokes (Bernaudin et al., 2000; Hijmans et al., 2011a; Hijmans et al., 2011b; Hogan, Pit-ten Cate, Vargha-Khadem, Prengler & Kirkham, 2006; Schatz et al., 2001; Schatz et al., 2002; Schatz, Finke, & Roberts, 2004; Steen et al., 2005). Mean IQ in children with SCD has been found to be nearly 12 points (11.97) lower than for those without SCD (Schatz et al., 2002; Steen et al. 2005). Studies show that IQ declines at the rate of approximately one point per year (Author, 2013; Schatz et al., 2002; Wang et al., 2001). Decline of IQ with age is not typical in a healthy population, and worsening performance suggests that the cognitive burden of SCD may increase as children age. As a result of these disparities, adolescents with SCD experience cognitive challenges that may hinder academic success, well-being and life opportunity into and throughout adulthood. Improving our understanding of risk factors beyond disease severity variables alone is critical to improving educational achievement and attainment among adolescents with SCD.
Objectives
The objectives of this study were to 1) examine educational attainment for adolescents with SCD in the St. Louis region, 2) examine neighborhood and social correlates of low educational attainment, and 3) assess the feasibility of a pilot program to increase General Education Diploma (GED) participation among adolescents with SCD and their parents. This study builds upon previous studies which have not used high school graduation as an indicator of attainment for youth with SCD, but have instead used grade retention as an indicator of risk for students with SCD (King et al., 2014; Ou & Reynolds, 2010; Schatz J et al., 2001). We hypothesize that 1) high school graduation rate for youth with SCD would be ≥10% lower than the rate for African American students attending St. Louis City public schools, 2) SCA genotypes (HbSS and HbSβ°), a history of overt or silent stroke, low IQ, being a parent, and having public insurance would correlate with lower educational attainment, and 3) a program designed to enroll youth with SCD and their parents in a GED program would be feasible and likely increase educational attainment for youth with SCD.
Methods & Results
Participants
A retrospective cohort design was used to examine educational attainment among adolescents with SCD. A waiver of informed consent was obtained through the Institutional Review Board (IRB). A clinical database of active patients was used to generate a list of adolescents treated for SCD at the author’s center. Electronic medical records were reviewed to ensure inclusion and exclusion criteria were met and to complete data collection. Table 1 presents inclusion and exclusion criteria. No compensation was provided to patients included in the review.
Table 1.
Participant inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
|
|
Educational Attainment for Youth with SCD
Analytic Approach
Chart review using a standardized procedure was conducted by a research assistant (RA). Data was entered into the Statistical Package for the Social Sciences (SPSS). Electronic medical records were reviewed for patient demographic information. Stroke history was confirmed via magnetic resonance imaging (MRI) report or hematologist note. Patients were classified as having had an overt stroke, a silent stroke, a negative MRI (which confirmed no stroke) or no available scan/history. Insurance status was recorded, with public insurance (Medicaid and Medicare) serving as a proxy for low socioeconomic status. Educational information was also compiled from a clinical database based upon patient and parental responses on education status during prior clinic evaluation or initial hospital evaluation. Phone calls were made to patients with missing educational information or information entered prior to April 1, 2012. Table 2 presents medical and educational variables collected from patients or patient records and variable descriptions. Statistical analyses including correlation and bivariate logistic regression were completed in SPSS. Kendal’s Tau non-parametric test was used to determine significance (p<.05).
Table 2.
Educational Attainment for Youth with SCD Variables
| Variable | Variable Description |
|---|---|
| Age | Patient age |
| Gender | Patient gender |
| Marital Status | Patient marital status |
| Number of Children | Patient’s number of children |
| Insurance Type | Patient’s insurance type (public, private, or combination) |
| Zip Code | Patient’s zip code |
| SCD Genotype | Patient’s SCD genotype |
| Disease Severity | Patient’s disease severity HbSS/HbSβ° or HbSC/HbSβ+ |
| Stroke History | Patients were classified as having had 1) an overt stroke, 2) a silent stroke, 3) a negative MRI (which confirmed no stroke) or 4) no available scan/history. |
| Intelligence Quotient (IQ) | Patient IQ. Due to a small amount of IQ data, IQ was classified as greater than or equal to the median of 95 points, or <95. |
| Educational Status | Last grade that the patient completed |
| Education Attainment | Patient educational attainment was categorized as 1) graduated high school, 2) in high school and not struggling, 3) in high school and struggling, 4) earned GED, 5) currently enrolled in GED classes, or 6) no GED and not enrolled in GED classes. Lower scores indicated higher educational attainment (e.g. graduated high school=1). |
| Struggling to pass | Patients currently enrolled in high school were queried on recent grades. A grade of D or F on his/her most recent report card was an indicator of struggling to pass. |
| GED Status | Patients who had withdrawn from high school were called and queried on their GED status. |
| Dropped out of high school | Patients who had withdrawn from high school and those who were not in and had not graduated from high school were categorized as having ‘dropped out’ of high school. |
Results
One hundred and twenty-four 16–25 year-old patients were identified, and 108 (87%) met inclusion criteria. All patients resided within St. Louis City, County or East St. Louis and received SCD treatment within the authors’ academic medical center. Ten patients were excluded due to inability to be reached for updated educational data, four had clinically diagnosed psychiatric conditions, and two had severe developmental delays. Of those included in the cohort, mean participant age was 20.2 years, 69% had HbSS or HbSβ°-thalassemia genotypes, 35% had a history of overt or silent stroke, 69% were enrolled in public insurance programs, and 16% were a mother or father (Table 4).
Table 4.
Description of cohort participants
| n (%) | |
|---|---|
| Age | 20.2 years |
| Female | 59 (55) |
| Public insurance | 74 (69) |
| Disease genotype | |
| HbSS | 67 (62) |
| HbSβ0-thalassemia | 7 (7) |
| HbSC | 29 (27) |
| HbSβ+ thalassemia | 5 (5) |
| Cerebrovascular injury | |
| Overt stroke | 9 (8) |
| Silent stroke | 29 (27) |
| Negative MRIs | 52 (48) |
| Are a parent | 17 (16) |
| IQ (n=25) | 93.3 points |
n=108
Fifty-seven percent of the cohort (62 of 108) had graduated high school, 21% (23 of 108) had withdrawn from high school and 21% (23 of 108) were currently enrolled in high school. Of those enrolled in high school, 48% (11 of 23) were struggling to pass. Of those who had withdrawn from high school, 37% (7 of 23) had earned their GED diploma, 26% (6 of 23) were currently enrolled in GED classes, and 44% (10 of 23) had not earned their GED diploma and were not enrolled in GED classes. Public insurance was common. Seventy percent (43 of 62) of patients who graduated high school and 83% (19 of 23) of patients who did not graduate high school had Medicaid. Tables 3–5 present cohort descriptive and demographic characteristics.
Table 3.
Educational Attainment Descriptive Statistics
| N | Minimum | Maximum | Mean | Standard Deviation | |
|---|---|---|---|---|---|
| Gender | 108 | 1.00 | 2.00 | 1.45 | 0.50 |
| Age | 108 | 16.00 | 25.00 | 20.15 | 2.50 |
| IQ | 25 | 71.00 | 123.00 | 93.32 | 13.95 |
Table 5.
Education status of cohort participants
| Reported education status | Number (% of cohort) |
|---|---|
| Graduated high school | 62 (57) |
| In high school | 23 (21) |
| Struggling to pass | 11 (48) |
| Dropped out of high school | 23 (21) |
| Earned GED | 7 (30) |
| Currently Enrolled in GED Class | 6 (26) |
| No earned GED/Not enrolled | 10 (44) |
n=108
Patients currently enrolled in high school were excluded to determine a high school graduation vs. dropout rate for comparison to same-race peers in St. Louis City and St. Louis County. Sixty-three percent (17 of 27) of patients residing within St. Louis City graduated high school and 37% (10 of 27) had withdrawn or dropped out. Seventy-six percent of St. Louis County patients graduated high school (39 of 51), and 24% (12 of 51) had withdrawn. Surprisingly, patient graduation rate was higher than the mean graduation rate for African Americans in the St. Louis City Public School District from 2008–2011, which was 57% (Missouri Department of Elementary and Secondary Education, 2012). It is important to note that the St. Louis City Public School District lost accreditation due to poor performance in 2007 and remained unaccredited throughout the study period.
Disease genotype was related to educational attainment and dropping out of high school (p<.05). Disease genotype HbSS and HbSβ° (p<.01) was significantly associated with increased risk of central nervous system (CNS) damage. In patients with HbSS, a lower IQ score was associated with dropping out of high school and lower educational attainment (p<.05). Adolescents with Hemoglobin SS had the lowest graduation rate, followed by Sβ+-thalassemia and HbSC. Patients with hemoglobin Sβ°-thalassemia had the highest graduation rate.
A history of stroke was not related to lower educational attainment in individuals who had brain imaging. Seventy-eight percent (7 of 9) of individuals with a history of overt stroke had graduated high school or were on track to graduate, compared to 69% (20 of 29) of those with silent strokes, 67% (35 of 52) of those with negative scans, and 67% (12 of 18) of those with no MRI. Although a greater percentage of males experienced an overt stroke (10% vs 7%), more females had experienced a silent infarct (37% vs. 14%) and overall, more females experienced CNS damage (51% vs 31%).
Seventy percent of those who graduated from high school had public insurance compared to 83% of those who did not graduate high school. Private insurance coverage was associated with having an IQ over 95 (p<.05, n=25). In patients without a history of silent or overt strokes (n=70), public insurance was associated with lower IQ (IQ≤95) (n=19, p<.01).
Being a parent was significantly associated with lower educational attainment (p<.01, r=−286, n=108) and dropping out of high school (p<.001, correlation=−.443, n=85). Among males, having children was significantly associated with dropping out of high school (p<.05, n=34), and males with HbSS (n=28), followed by HbSC (n=15) were at the greatest risk for lower attainment. For females, being a parent was strongly associated with dropping out of high school (p<.0001). Among patients with HbSS, being a parent was significantly associated with dropping out of high school (p<.01). When controlling for children, males had significantly lower educational attainment than females (p<.05), severe disease genotype was significantly associated with not completing high school (p<.05), and enrollment in a public insurance program was associated with IQ ≤ 95 (p<.05, n=24).
Environmental Correlates of Attainment
While low neighborhood and school district socioeconomic status are often associated with decreased educational attainment among youth, especially African American youth, in urban areas, there is limited research examining the relationship between community or neighborhood-level factors and educational attainment among youth with SCD (Sirin, 2005; Fowler & Walberg, 1991). Identifying community or neighborhood-level risk factors is essential for developing interventions and determining high-risk geographic areas for intervention.
Analytic Approach
Geographic information systems (GIS) is a methodology uniquely suited for an examination of this cohort’s geographic distribution, community environment, and access to GED classes. We hypothesized that 1) lower educational attainment would be associated with zip codes with a) lower median household incomes, b) higher frequencies of teenage parenthood, and c) more patients with SCD, and 2) 40% of patients with SCD would not have access to GED class (no classes within their zip code).
Patients who lived in St. Louis City or St. Louis County were included in this analysis. Patients living in East St. Louis, Illinois, were excluded to eliminate the effect of differing state policies. Table 6 presents a list of zip code level variables included and their sources. Four GIS maps were created (Figures 1–4). Patient and zip code data were compiled and entered into ArcGIS (ERSI, 2011). Data were mapped by zip code. Patient and zip code data were input into SPSS for analysis. To increase sample size and examine the impact of varying environments, variables were grouped for comparison. Groups included 1) the patient concentration in a zip code (0–3, 4–6, or 7–9 patients with SCD per zip code), 2) median zip code income <$40,000 or ≥$40,000, and 3) residence within St. Louis City versus St. Louis County. The Mann-Whitney non-parametric independent samples correlation test was used to assess significance (p<.05).
Table 6.
Environmental Correlates of Attainment Variables.
| Variable | Variable Description (Source) |
|---|---|
| Number live births | Number of live births to mothers 10–19 years old (Missouri State Department of Health and Senior Services) |
| Number births by Age | Number of births stratified by maternal age (10–14 years old, 15–17 years old, and 15–19 years old) was also collected (Missouri State Department of Health and Senior Services). |
| Number and location of schools | Number of unaccredited schools per zip code was determined for 2011 (Missouri Department of Elementary and Secondary Education). |
| Median annual household income | Median annual household income by zip code (United States Census American Community Survey 5-Year Estimates, 2010). |
| GED Classes | A list of active GED classes in St. Louis City, County, and East St. Louis was compiled through a systematic internet search using the terms “GED” or “GED classes” combined with “St. Louis City,” “St. Louis County,” or “[municipality name].” Exclusion criteria were GED study groups or privately held groups. Forty-eight classes were identified and mapped. |
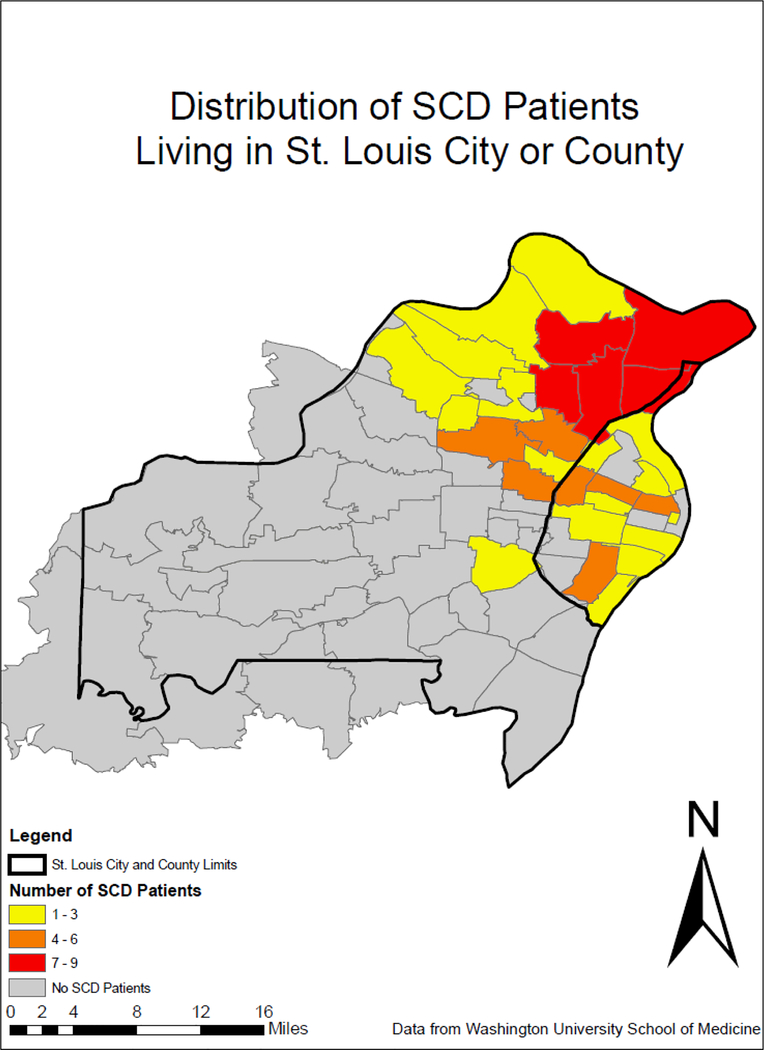
Figure 1.
Distribution of patients with SCD living in St. Louis City or County. Note: Patients were highly concentrated in St. Louis City and northern St. Louis County.
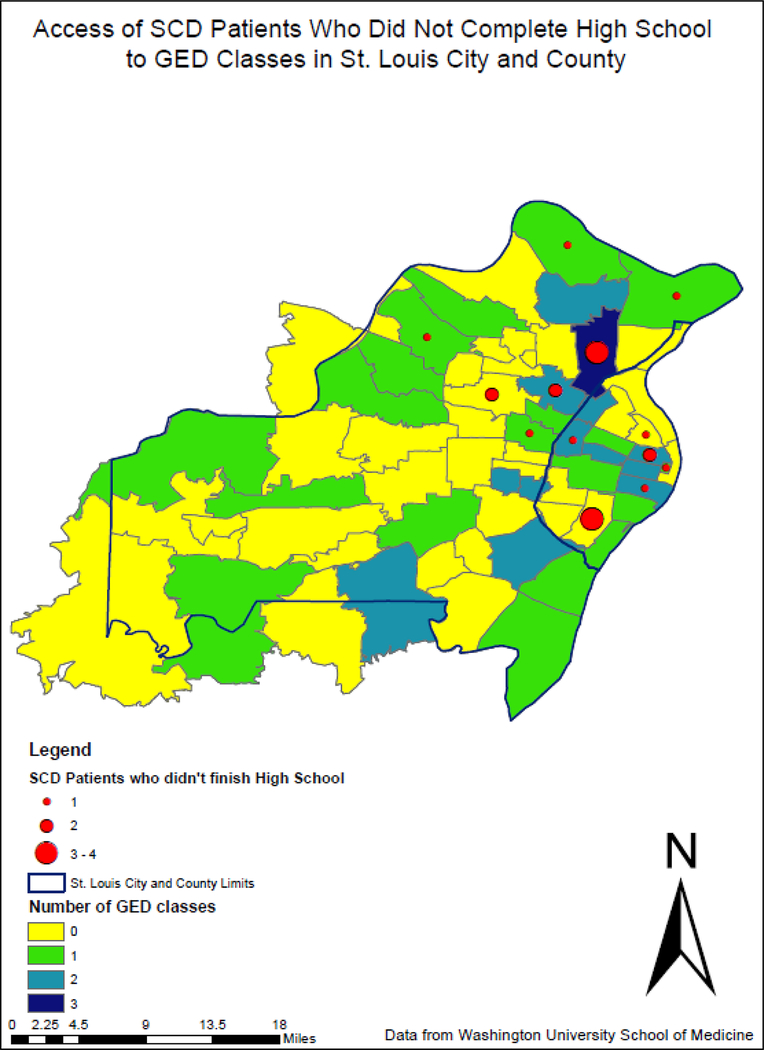
Figure 4.
Access to GED classes for youth with SCD who did not graduate from high school.
Results
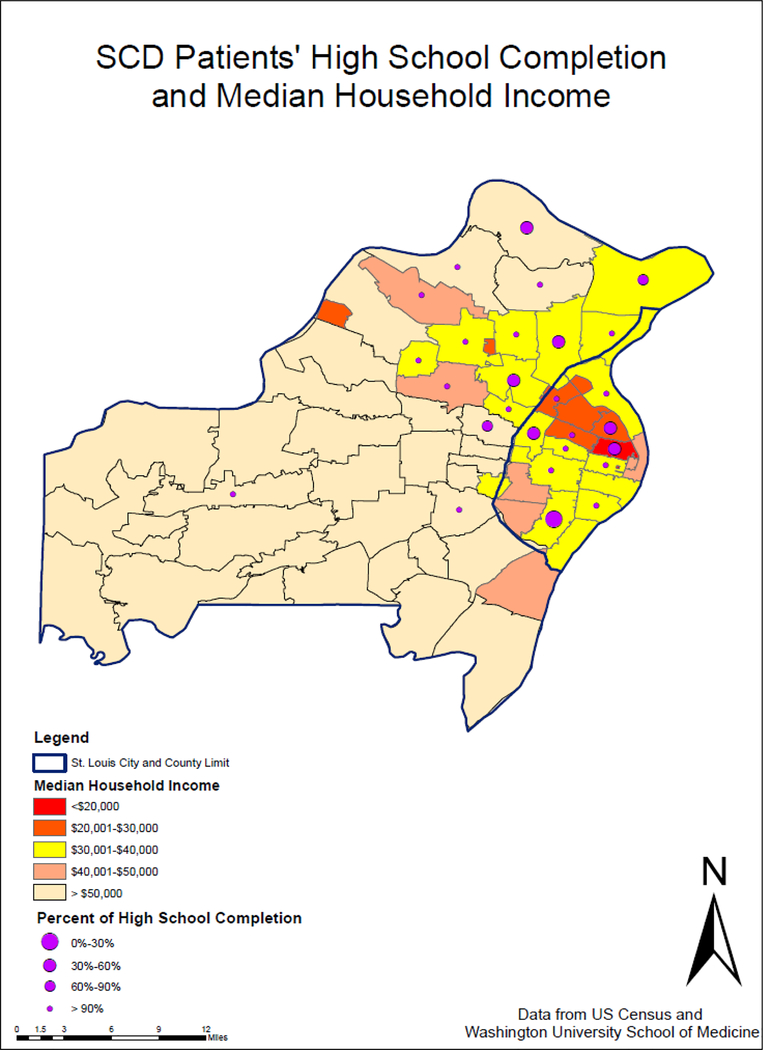
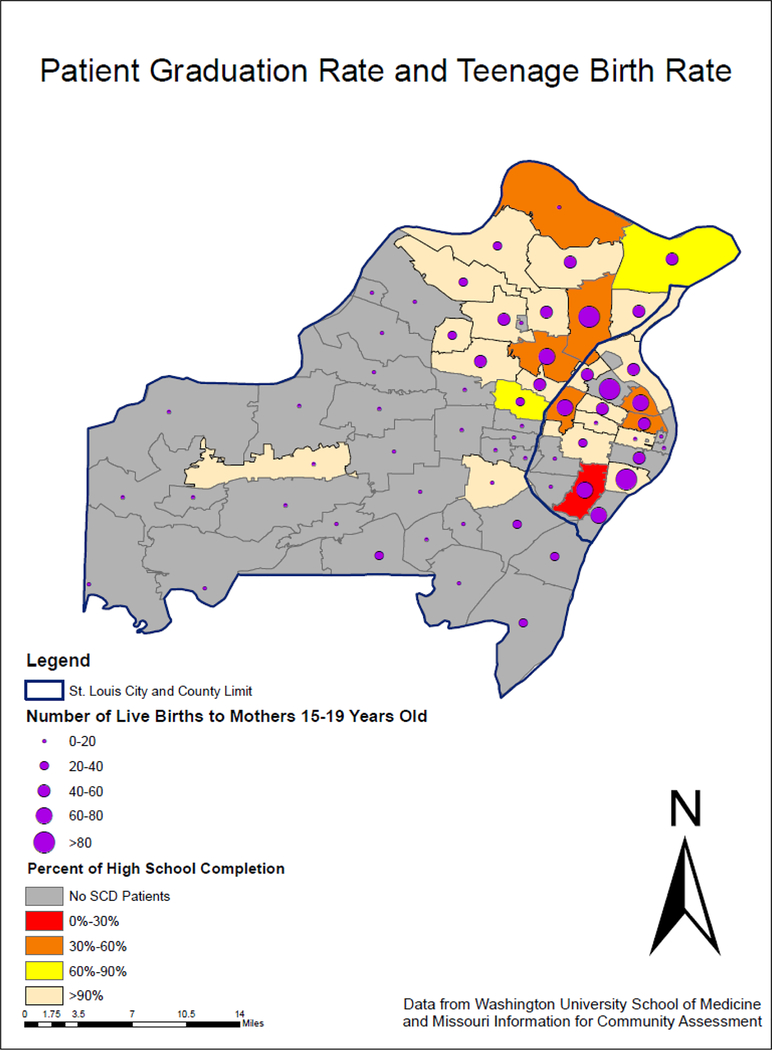
Ninety-nine patients met criteria for inclusion (Figures 1–4). Due to unavailable data, one patient was removed from analysis utilizing census data. Patients were concentrated in St. Louis City and northern St. Louis County zip codes (Figure 1). Most patients lived in zip codes with a median household income <$40,000, and 6 of 7 zip codes with graduation rates at or below 60% were in zip codes with a median household income of <$40,000 (Figure 2). Areas with a lower number of births to 15–19 year old females had higher percentages of patients graduating high school (Figure 3).
Figure 2.
High school completion for youth with SCD and neighborhood income. Patients lived in low income areas compared to peers in other parts of St. Louis County. Income appears lower in the St. Louis City.
Figure 3.
Zip code birth rate to 15–19 year olds and patient graduation rate Note. Areas with a higher number of births (larger dots) were more often located in areas with fewer patients graduating (warmer colors).
Higher educational attainment was found for patients living in high patient concentration areas (7+ patients per zip code, n=38) versus medium patient concentration areas (4–6 patients per zip code, n=34). Mean rank was 41.7 for medium versus 31.1 for high patient concentration areas (where lower scores indicate higher attainment; p<.05). High patient concentration areas were more likely to be located in St. Louis County, and to have a greater percentage of residents identifying as African-American (p<.05). Adolescents in high concentration areas were more likely to graduate high school than those in low patient concentration areas (high patient concentration area mean rank = 25.1, low patient concentration areas mean rank = 33.7; p<.05). Educational outcomes did not significantly differ for patients residing in high versus low (0–3 patients per zip code, n=27) patient concentration areas.
As expected patients who had children as teenagers more commonly lived in zip codes with more births among 10–14 year olds (p<.01), and being a parent and living in a zip code with a higher teenage birth rate was associated with dropping out of high school (p<.001 and p<.05 respectively). High school dropout among patients was higher in zip codes with 60–80 live births to adolescents per year, versus 30–50 (p<.05). Median household income was significantly lower in St. Louis City vs. County (p<.001), and was not significantly related to patient graduation outcomes.
GED Class Matching Pilot
The GED is a 5-subject competency test that is an alternative for students who did not graduate high school and would like to earn an equivalent diploma (“About GED Testing,” 2012). Recipients of the GED can apply to most jobs and educational programs open to high school graduates. Free classes are available to help students prepare for the exam. Classes vary in size, structure, and teaching methods. Providing information about classes to adolescents with SCD may facilitate their enrollment in preferred learning environments. Healthy People 2020, a U.S. government initiative, declared a goal of improving high school and GED outcomes for those with hemoglobinopathies (United States Department of Health and Human Services, Healthy People 2020, 2011). The proposed intervention will provide adolescents with SCD with the knowledge and support to enroll in GED classes. A multi-faceted intervention pilot was proposed to address the educational needs of those patients affected by SCD who did not complete high school, and assess the acceptance and feasibility of a GED class-matching program.
Approach
GED class environments (e.g. amount of auditory distraction, class size) and services (tutoring, free child care, bus passes etc.) were assessed via a standardized phone survey. The program aided youth in selecting and enrolling in a GED class and in generating compensatory strategies for self-identified deficits. Feasibility was defined as 1) >40% of those approached participating in the study, 2) ≥66% of participants enrolled in GED classes at 2 month follow-up, and 3) < 4 hours of in-person support per student. Knowledge about the GED exam and classes was expected to increase by ≥25% at 2 month follow-up. Structuring the class enrollment process for adolescents with SCD increase educational attainment.
Participants recruited by phone were adolescents identified in the retrospective review (ages 16–25 years) who were 1) diagnosed with SCD, 2) had withdrawn from high school and had a minimum of 8th grade completion or 3) were the parent of a child diagnosed with SCD (referred by SCD clinic providers). Meetings took place in a private room at the author’s center, or a public library. Participants were compensated for study-related travel expenses with a one-time $10 gas card or the requisite number of bus tickets. Parents of young children with SCD were provided the additional option of meeting within the home to reduce the cost of transporting the family and the lack of appropriate childcare facilities. The initial meeting followed a standardized structure (see Appendix - Table 8), with phone or in person as requested, an additional 2 month follow-up session, and an optional additional session to navigate public transportation to and from the selected GED class.
Results
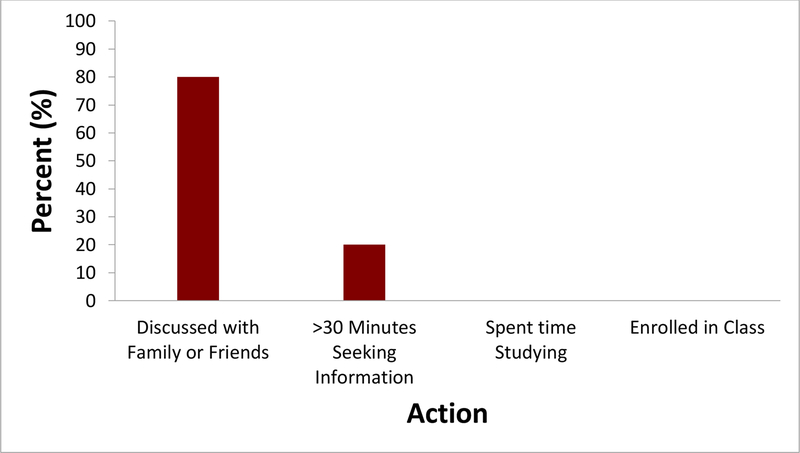
Five of 12 participants who were approached consented to participate (41%). Table 7 presents participant demographics. All five participants indicated that they were planning to enroll in GED classes during the next 2 months. Despite high interest, only 1 of 5 participants indicated that she had spent >30 minutes in the past 2 months seeking information about the GED and GED classes, and zero of 5 had spent time studying or enrolled in a class. All adolescents identified career goals, and all participants had 3 or more GED classes to choose from within 30 minutes via car or public transit.
Table 7.
Demographic information of GED protocol participants.
| Participant # |
Gender | Age | Insurance | SCD genotype |
Stroke | Last grade completed |
Employed |
|---|---|---|---|---|---|---|---|
| 1 | F | 19 | Public | HbSS | Silent | 11 | No |
| 2 | F | 21 | Private | NO SCD | No MRI | 10 | Part-time |
| 3 | F | 24 | Public | HbS-β+ | Negative MRI | 8 | No |
| 4 | F | 18 | Public | HbSS | Silent | 8 | No |
| 5 | F | 20 | Public | HbSS | No MRI | 10 | No |
Participants self-identified the following perceived limitations: memory (80%), procrastination (60%) and attention (40%). Sixty percent of the participants independently stated a need to improve learning and study strategies. Participants also indicated concerns specific to SCD: 75% stated that SCD had contributed to not completing high school, 75% reported worrying about managing SCD while in GED classes.
Adolescents requested varying degrees of support and one-on-one attention. GED knowledge increased from 71% to 84%, from pre-test to post-test during the initial session. Two participants requested an additional visit to navigate transportation to GED class. Two participants completed 2-month follow-up. Both had enrolled in and consistently attended GED classes and rated person-class fit as 10/10 (perfect). A third participant was unable to meet for formal post-testing during the required time-frame at 2 months, but contacted the research team at 2 months to state that she had continued attending the class with a friend. Two participants were lost to follow-up due to disconnected phone lines. The average amount of in-person contact per person was < 2 hours per participant, which met feasibility criteria.
Discussion
Adolescents with SCD served by our local center are now graduating high school at a similar rate as their peers. While this finding is inconsistent with previous literature on educational attainment among youth with SCD, it may be in part explained by the overall low graduation rates in the St. Louis area (several school districts in the area were also unaccredited at the time of this study). This finding may also be in part due to the increased support in the classroom provided by our center. After the initial findings in 2003, our children’s hospital supported a social worker to serve as a school liaison who screened for educational risk factors, facilitated referral for cognitive assessments, and advocated for school support such as 504 Plans or IEPs. Other factors impacted by SCD were associated with lower educational attainment. HbSS and an IQ <95 were associated with not completing high school. In addition, demographic characteristics, such as male gender, being a parent, and public insurance were associated with not completing high school. This suggests that our center’s practice of identifying patients at-risk for lower attainment primarily by stroke history or disease severity may be an incomplete assessment of risk. Gender and inconsistent contraceptive practices among sexually active adolescents may provide additional indicators of risk for lower academic attainment and grounds for targeted intervention.
Educational attainment was not worse among adolescents who had a history of SCD-related strokes. Information on special academic service utilization and medical interventions (e.g. chronic transfusion therapy, hydroxyurea) were not measured, therefore we are unable to determine whether success is due to no difference in risk or due to special education services and medical treatment factors. Current medical and educational services offered at our center do appear effective in facilitating high school graduation in adolescents who have experienced a stroke.
High patient population areas appear to have relatively higher patient graduation rates, however seven of 12 medium to high patient population areas have graduation rates below 60%. Schools within these areas, which have a higher percentage of black students, may have more experience or policies in place to meet the needs of patients with SCD. Greater community support or ethnic identity may also facilitate higher attainment. Students in medium patient concentration zip codes, were at the greatest risk for not completing high school. Schools in moderately saturated areas may benefit from education on SCD and successful accommodations to increase adolescents’ success. Focusing educational in-services may have the greatest impact in zip codes with 4–6 patients. Zip code birth rates were related to patient birth rates and high school graduation. Providing sexual education resources to adolescents and/or parents, particularly to those living in zip codes with a high number of adolescent births, may reduce patient pregnancy-related withdrawals from school.
Together these data support the need to consider community-level factors to identify adolescents at heightened risk for not graduating high school, in addition to disease-related factors. Nearly a quarter of the cohort did not complete high school, and nearly half of those (10 of 23) could be served by a GED matching program. Almost half of currently enrolled high school students were struggling to pass and are at-risk for not graduating on time. Current and future patients may benefit from a program that facilitates GED enrollment, and we attempted to pilot this to intervene as opposed to only assessing the educational performance and related factors.
Over 40% of patients who had not completed high school were willing to meet with a research assistant to discuss the GED. Despite high baseline interest in enrolling in a GED class, few adolescents had taken steps towards enrolling in the preceding 2 months. The disparity between desire and action suggests that adolescents may benefit from information and additional support. Due to accessibility of multiple GED classes to patients, having information about classes proved useful in adolescents’ selecting their best-fit class.
Learning challenges that patients most often selected from a list of twelve (memory and attention) are consistent with executive functioning deficits that occur at a higher rate in adolescents with SCD (Schatz, Brown, Pascual, Hsu & DeBaun, 2001). With facilitation, adolescents were able to co-generate several strategies for areas or adapt suggested strategies. By providing a structured information session, follow up, and targeted strategies tailored to the participants’ life and learning styles, initiation towards GED class enrollment increased.
Due to lack of appropriate follow-up, we cannot determine whether the feasibility criteria of >66% enrollment in GED classes at 2-month follow-up was met. The census demonstrated that 40–50% of people living at 150% of the poverty level or less move over five years (Ihrke, David K., and Carol S. Faber. 2012. Geographical Mobility: 2005 to 2010. Current Population Reports, P20–567. U.S. Census Bureau, Washington, DC.) Given the prevalence of poverty in the SCD population, a second, reliable method or person of contact should be obtained at the initial session to prevent attrition due to a disconnected phone line in future interventions. Expansion of the program to more diagnostic groups may increase feasibility of a hospital-based GED program while continuing to offer the structured support to a high-risk group. Interest in our program extended twice to members of participants’ families who likewise hadn’t completed high school.
A strength of the GED pilot study was that multiple possible barriers to enrollment were addressed in the program, including information access, transportation, childcare, finances, cognitive challenges, guidance, learning strategies and disease self-management. The semi-structured format was easily replicable. Weaknesses were the small sample size, the lack of representation from males, and the attrition rate. In addition, the GED knowledge and behavior measures were not validated. Although enrollment in GED classes does not guarantee earning a degree, enrollment was able to be assessed during the study time frame and is often the first step to earning the GED.
Overall study limitations include limited generalizability due to the single-center, retrospective, and correlational design, and inability to control for all confounders. However, we are able to interpret the results in the context of system support over the past 15 years at our institution. The relationship between public insurance and IQ may be poverty-related, nutrition-related, or related to the school and home environment. At a minimum, these results reinforce the need to assess for the environment to interpret cognitive assessments and educational attainment in this population. Screening measures for undiagnosed psychological conditions were also not conducted. Though limited, the current study broadened understanding of factors related to educational attainment in a sample of urban dwelling, African-American adolescents with SCD. Further exploration is needed to infer causation, the mechanism(s) of impact, and areas for development of targeted interventions.
Demographic characteristics do influence educational attainment. Identifying risk and protective environmental factors and their characteristics can assist in the development and implementation of interventions. Improving educational attainment in adolescents with SCD requires understanding risk beyond disease severity variables alone. A future multi-site prospective study could provide accurate measurements and sequencing of educational services received, neurological insult, anemia severity, and the impact of hospitalizations. In addition, psychosocial variables, achievement test scores, home environment, and the impact of parenthood can be assessed in a larger group of patients. Accurate assessment of factors that impact educational attainment will enable educators, social workers and allied health professionals to design targeted, evidence-based interventions that consider psychosocial and disease-related factors.
Figure 5.
GED behaviours in previous 2 months. Note. n=5. Despite high interest, patients appear to require additional support and resources to translate interest into behaviour.
Acknowledgments
We would like to acknowledge members of the Washington University Child Health and Education Lab, who supported the completion of this project and manuscript.
Appendix A –. GED Class Matching Pilot
Materials
Materials included 1) completed phone surveys by GED classes, 2) a St. Louis- and SCD-specific GED manual written by the authors, 3) google maps depicting transportation options from the patient’s address to nearby GED classes, and 4) pens. In addition, the authors created a 9-item multiple choice test to assess knowledge about the GED (e.g. subject areas tested), and a 7-item survey that queried actions and behaviors taken in the past 2 months that supported GED class enrollment (e.g. studying for more than 30 minutes). Use of an audio recorder was optional.
Table 8.
Initial meeting standardized structure:
| Component | Description |
|---|---|
| Pre-tests | 9-item pre-test and 7-item baseline survey of GED knowledge and behaviors were completed. The tester was blind to the participant’s performance in order to minimize experimenter bias. |
| GED manual | The participant was oriented to the seven section manual created by the authors, which contained information about the GED, St. Louis areas resources, “Your Student Style” questionnaires, and lists of compensatory/learning strategies. Participants were provided with a short overview of the GED. Patients identified individual preferences, strengths and weaknesses. |
|
Compensatory
Strategies co-generation |
Adolescents generated three strategies to overcome or compensate for each weakness. |
| GED class-matching | If the participant remained interested in GED classes, he or she was provided information on GED classes within a 30-minute bus ride, including the class structure and environment and maps depicting the transit route(s). Participants selected a class that fit their needs. Childcare and SCD-related concerns were addressed. |
| Goal setting | Adolescents set goals for dates by which to complete desired steps towards enrollment. |
| Post-test | Adolescents completed a 9-item post-test and 7-item survey on GED knowledge and behaviors. The post-test was identical to the pre-test. |
Contributor Information
Kelly M. Harris, Program in Occupational Therapy, Washington University in St. Louis, School of Medicine.
Joyce N. Dadekian, Program in Occupational Therapy, Washington University in St. Louis School of Medicine.
Regina A. Abel, Program in Occupational Therapy, Washington University in St. Louis School of Medicine.
Brittni Jones, Department of Education, Washington University in St. Louis.
Ashley Housten, Program in Occupational Therapy and Department of Surgery, Washington University in St. Louis School of Medicine.
Barbara Ddamulira, George Warren Brown School of Social Work, Washington University in St. Louis.
Kelly Chadwick-Mansker, Program in Occupational Therapy, Washington University in St. Louis School of Medicine, Division of Pediatric Hematology/Oncology, St. Louis Children’s Hospital, St. Louis, MO..
Allison A. King, Program in Occupational Therapy, Washington University in St. Louis School of Medicine, Division of Pediatric Hematology/Oncology, St. Louis Children’s Hospital, St. Louis, MO..
References
- Bernaudin F, Verlhac S, Freard F, Roudot-Thorraval F, Benkerrou M, Thuret I…Brugieres P. (2000). Multicenter prospective study of children with sickle cell disease: Radiographic and psychometric correlation. Journal of Child Neurology, 15(5), 333–343. [DOI] [PubMed] [Google Scholar]
- Brittain JE, Han J, Ataga KI, Orringer EP, & Parise LV (2004). Mechanism of CD47-induced alpha4beta1 integrin activation and adhesion in sickle reticulocytes. The Journal of Biological Chemistry, 279, 42393–42402. [DOI] [PubMed] [Google Scholar]
- Burrus J, & Roberts RD (2012). Dropping Out of High School: Prevalence, Risk Factors, and Remediation Strategies. R&D Connections. No.18 Retrieved from https://www.ets.org/research/policy_research_reports/rdc-18 [Google Scholar]
- Centers for Disease Control and Prevention. (2018). Data & Statistics on Sickle Cell Disease | CDC. Retrieved from https://www.cdc.gov/ncbddd/sicklecell/data.html. [Google Scholar]
- Darbari DS, Kple-Faget P, Kwagyan J, Rana S, Gordeuk VR & Castro O (2006). Circumstances of death in adult sickle cell disease patients. American Journal of Hematology, 81(11), 858–863. [DOI] [PubMed] [Google Scholar]
- Da Silva Junior GB, Daher EDF, & da Rocha FAC (2012). Osteoarticular involvement in sickle cell disease. Revista Brasileira de Hematologia e Hemoterapia, 34(2), 156–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeBaun MR, Sarnaik SA, Rodeghier MJ, Minniti CP, Howard TH, Iyer RV…Casella JF (2012). Associated risk factors for silent cerebral infarcts in sickle cell anemia: low baseline hemoglobin, sex, and relative high systolic blood pressure. Blood, 119(16), 3684–3690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ESRI (2011) ArcGIS Desktop: Realease 10. Redlands, CA: Environmental Systems Research Institute. [Google Scholar]
- Fowler WJ, & Walberg HJ (1991). School Size, characteristics, and outcomes. Educational Evaluation and Policy Analysis, 13 (2), 189–202. [Google Scholar]
- Hammond C, Linton D, Smink J, & Drew S (2007). Dropout Risk Factors And Exemplary Programs. Clemson, SC: National Dropout Prevention Center, Communities in Schools, Inc. [Google Scholar]
- Hassell KL (2010). Population estimates of sickle cell disease in the U.S. American Journal of Preventive Medicine, 38(Supplement 4), S512–521. doi: 10.1016/j.amepre.2009.12.022 [DOI] [PubMed] [Google Scholar]
- Hassell KL (2010). Population estimates of sickle cell disease in the US. [Article]. American Journal of Preventive Medicine, 38(4), S512–S521. doi: 10.1016/j.amepre.2009.12.022 [DOI] [PubMed] [Google Scholar]
- Hijmans CT, Fijnvandraat K, Grootenhuis MA, van Geloven N, Heijboer H, Peters M, & Oosterlaan J (2011). Neurocognitive deficits in children with sickle cell disease: a comprehensive profile. Pediatric Blood & Cancer, 56(5), 783–788. [DOI] [PubMed] [Google Scholar]
- Hijmans CT, Grootenhuis MA, Oosterlaan J, Heijboer H, Peters M, & Fijnvandraat K (2011). Neurocognitive deficits in children with sickle cell disease are associated with the severity of anemia. Pediatric Blood & Cancer, 57(2), 297–302. [DOI] [PubMed] [Google Scholar]
- Hogan AM, Pit-ten Cate IM, Vargha-Khadem F, Prengler M, & Kirkham FJ (2006). Physiological correlates of intellectual function in children with sickle cell disease: hypoxaemia, hyperaemia and brain infarction. Developmental Science, 9(4), 379–387. [DOI] [PubMed] [Google Scholar]
- Luzzatto L (2012). Sickle cell anaemia and malaria. The Mediterranean Journal of Hematology and Infectious Diseases, 4(1). Retrieved November 21, 2013 from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3499995/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCavit TL (2012). Sickle cell disease. Pediatrics in review / American Academy of Pediatrics, 33(5), 195–204; quiz 205–196. doi: 10.1542/pir.33-5-195 [DOI] [PubMed] [Google Scholar]
- Missouri Department of Elementary and Secondary Education (2012). About GED Testing. Retrieved on November 25, 2012 from [http://dese.mo.gov/divcareered/ged_about.htm]
- Missouri Department of Elementary and Secondary Education (2012). Guided inquiry: District graduation rates. Retrieved February 17, 2012 from https://apps.dese.mo.gov/MCDS/home. [Google Scholar]
- National Heart, Lung and Blood Institute, Disease and conditions index. (2009). Sickle cell anemia: who is at risk? Retrieved September 10, 2011 from [Google Scholar]
- Ohene-Frempong K, Weiner SJ, Sleeper LA, Miller ST, Embury S, Moohr JW…Gill FM (1998). Cerebrovascular accidents in sickle cell disease: rates and risk factors. Blood, 91(1), 288–294. [PubMed] [Google Scholar]
- Ohnishi ST, & Ohnishi T (1994). Membrane abnormalities in sickle cell disease and in other red blood cell disorders. Boca Raton, FL: CRC Press. [Google Scholar]
- Ou S-R, & Reynolds AJ (2010). Grade Retention, Postsecondary Education, and Public Aid Receipt. Educational Evaluation and Policy Analysis, 32(1), 118–139. doi: 10.3102/0162373709354334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pegelow CH, Macklin EA, Moser FG, Wang WC Bello JA, Miller ST…Kinney TR (2002). Longitudinal changes in brain magnetic resonance imaging findings in children with sickle cell disease. Blood, 99(8), 3014–3018. [DOI] [PubMed] [Google Scholar]
- Schatz J, Brown RT, Pascual JM, Hus L, & DeBaun MR (2001). Poor school and cognitive functioning with silent cerebral infarcts and sickle cell disease. Neurology, 56(8), 1109–1111. [DOI] [PubMed] [Google Scholar]
- Schatz J, Finke RL, Kellett JM, & Kramer JH (2002). Cognitive functioning in children with sickle cell disease: a meta-analysis. Journal of Pediatric Psychology, 27(8), 739–748. [DOI] [PubMed] [Google Scholar]
- Schatz J, Finke R, & Roberts CW (2004). Interactions of biomedical and environmental risk factors for cognitive development: a preliminary study of sickle cell disease. Journal of Developmental & Behavioral Pediatrics, 25(5), 303–310. [DOI] [PubMed] [Google Scholar]
- Schatz J (2004). Brief report: Academic attainment in children with sickle cell disease. Journal of Pediatric Psychology, 29(8), 627–633. [DOI] [PubMed] [Google Scholar]
- Schwartz LA, Radcliffe J, & Barakat LP (2009). Associates of school absenteeism in adolescents with sickle cell disease. Pediatric blood & cancer, 52(1), 92–96. doi: 10.1002/pbc.21819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirin SR (2005). Socioeconomic status and academic achievement: A meta-analytic review of research. Review of Educational Research 75(3), 417–453. [Google Scholar]
- Steen RG, Fineberg-Buchner C, Hankins G, Weiss L, Prifitera A, & Mulhern RK (2005). Cognitive deficits in children with sickle cell disease. Journal of Child Neurology, 20(2), 102–107. [DOI] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy People 2020 (2013, June 5). Blood disorders and blood safety. Retrieved from http://healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=4 [Google Scholar]
- Census Bureau US. (2010). Selected characteristics in the United States. 2010 American Community Survey 5-Year Estimates. Retrieved from http://factfinder2.census.gov [Google Scholar]
- Wang W, Enos L, Gallagher D, Thompson R, Guarini L, Vichinsky E…Armstrong FD (2001). Neuropsychologic performance in school-aged children with sickle cell disease: a report from the Cooperative Study of Sickle Cell Disease. The Journal of Pediatrics, 139(3), 391–397. [DOI] [PubMed] [Google Scholar]