Abstract
Purpose
To report an atypical case of vitreoretinal lymphoma, secondary to non-central nervous system (non-CNS) systemic lymphoma, masquerading as an infectious retinitis.
Observations
A 76-year-old female with a history of cecal diffuse large B-cell lymphoma with two prior occurrences of posterior segment ocular involvement presented with a complaint of blurry vision in the right eye. Exam findings were significant for large areas of retinal whitening and retinal hemorrhages in the absence of choroidal lesions or significant vitritis. The clinical suspicion of an infectious retinitis, was supported by a presumptive immunosuppressive state secondary to her recent treatment (within 1 month) with both intravitreal and systemic rituximab plus high-dose methotrexate. Aggressive treatment with intravitreal and systemic antivirals and antibiotics was initiated. However, polymerase chain reaction (PCR) testing of aqueous fluid was negative for cytomegalovirus (CMV), herpes simplex virus, herpes zoster virus and toxoplasma, and her condition continued to worsen, so suspicion was raised for a masquerading recurrent malignancy. She was treated empirically with serial intravitreal injections of methotrexate and showed dramatic clinical improvement. A subsequent relapse occurred that responded rapidly to intravitreal methotrexate in the absence of antiviral/antibiotics.
Conclusion
It is important for clinicians to be aware of atypical presentations of vitreoretinal lymphoma. This case emphasizes the fact that secondary ocular lymphoma after systemic lymphoma can have a vitreoretinal presentation rather than the more common choroidal involvement. Furthermore, it shows that recurrences of this disease in the same patient can have very different manifestations, including an appearance indistinguishable from a viral retinitis.
Keywords: Lymphoma, Vitreoretinal lymphoma, Masquerade, Cytomegalovirus, Retinitis
1. Introduction
Intraocular lymphoma is a rare malignancy, representing fewer than 1% of all intraocular tumors, 1% of all intracranial tumors, and 1% of non-Hodgkin's lymphomas.1 Posterior segment ocular lymphoma is often sub-classified by the tissue involved into two entities, namely vitreoretinal lymphoma or choroidal lymphoma.2,3 These can be primary or secondary. The term “secondary” implies that the disease follows a prior presentation of extraocular lymphoma. Vitreoretinal lymphoma is often associated with CNS lymphoma.2,3 Conversely, the vast majority of ocular involvement following systemic lymphoma outside the CNS affects the choroid and not the retina.2,3 Vitreoretinal lymphoma most often presents with vitreous infiltration and with sub-RPE “nodular” to amorphous infiltrates with overlying RPE pigmentation changes. Choroidal lymphoma, particularly secondary lymphoma, often presents with multifocal, raised, creamy-yellow infiltrates at the level of choroid, sometimes with overlying subretinal fluid.2,4 The diagnosis of intraocular lymphoma may be challenging due to its ability to masquerade as a uveitis. Here we report a patient with a history of systemic diffuse large B-cell lymphoma (DLBCL), who presented with multiple episodes of vitreoretinal lymphoma with different clinical manifestations, the last of which was masquerading as an infectious retinitis.
2. Findings
A 76-year-old female with a history of DLBCL, with previous ocular involvement, presented with a complaint of blurry vision in the right eye for several days in November 2017. She was initially diagnosed with systemic lymphoma in 2013, when a cecal biopsy was found to be positive for DLBCL. Subsequent workup, including bone marrow biopsy, lumbar puncture, and brain MRI, was negative for malignancy. After a full PET scan, she was found to have stage IIIb disease. She underwent six cycles of R-CHOP chemotherapy (rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone) and was considered to be in remission after four cycles.
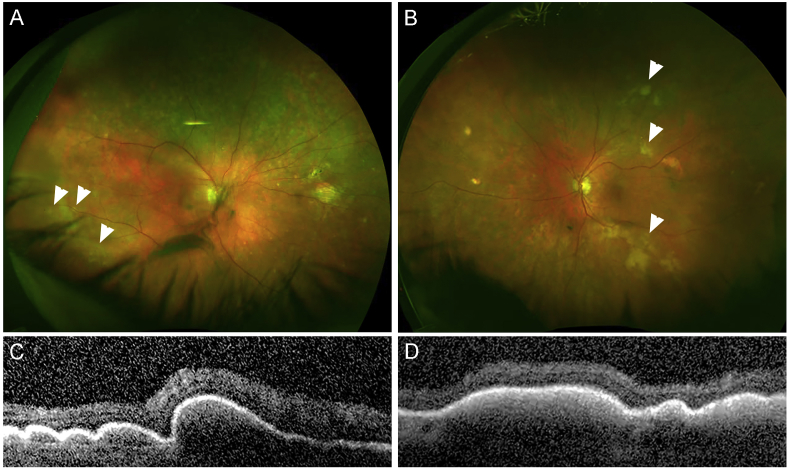
Her history of ocular involvement began in early 2016, when she presented to our clinic with decreased vision in the setting of bilateral multiple new creamy sub-RPE lesions (Fig. 1 and Supplemental Fig. S1). There was no significant vitreous infiltration. She underwent a workup for systemic and CNS lymphoma, which included lumbar puncture, MRI of brain and orbits and PET CT. There was no evidence of extraocular involvement. She was diagnosed with an atypical secondary vitreoretinal lymphoma. After a careful discussion with the patient, it was decided to proceed with systemic therapy, partly due to the bilateral involvement. The patient was treated with four cycles of systemic methotrexate, rituximab, and hydrocortisone. There was rapid resolution of all the creamy sub-RPE lesions, and the patient was considered to be in remission after the second cycle.
Fig. 1.
Fundus photos and OCT images from first intraocular lymphoma episode in 2016. A. Fundus photos were obtained showing sub-RPE creamy/yellow lesions (arrowheads) in the right (A) and left (B) eyes. OCT images were also obtained of the sub-RPE lesions inferior to the inferotemporal arcades in the right (C) and left (D) eyes. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Her disease was considered quiescent until she presented to her ophthalmologist in her state of summer residence in June 2017 with decreased vision in the right eye. This was determined to be a recurrence of her lymphoma with creamy sub-RPE lesions. MRI imaging of the brain and spine, as well as a lumbar puncture were unremarkable for CNS disease. She was empirically treated with two intravitreal injections of rituximab. This was followed by three cycles of systemic high-dose methotrexate and rituximab aimed at treating both vitreoretinal and possible microscopic CNS disease, after which she was again considered to be in remission.
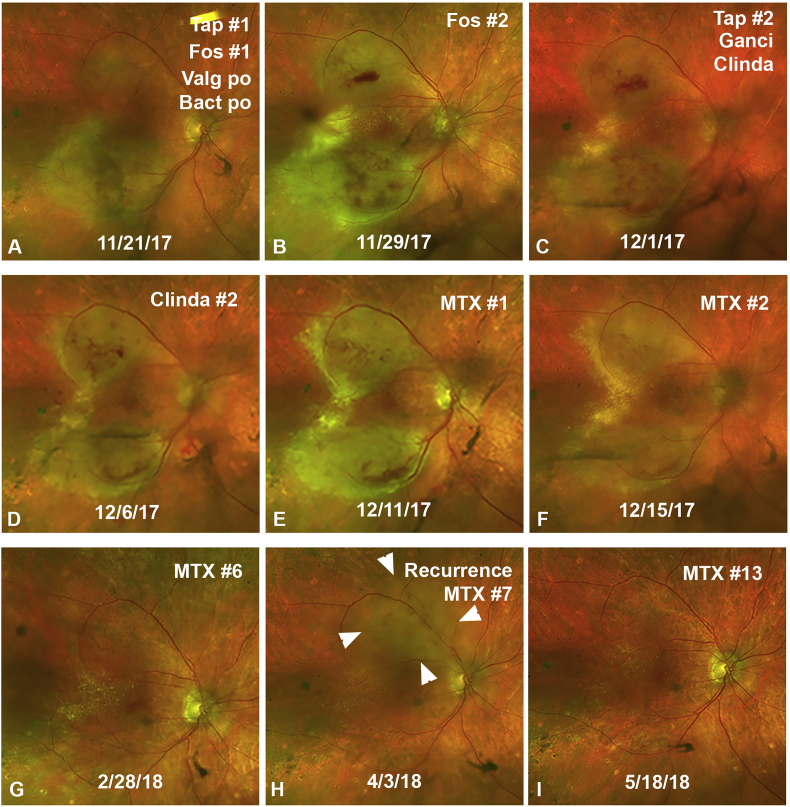
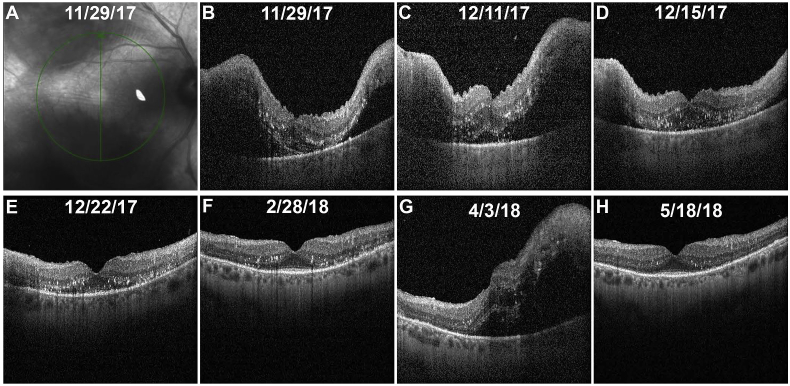
In November 2017, just one month after her chemotherapy was completed, she presented to our clinic (RU), with new onset of decreased vision in her right eye. Her visual acuity was counting fingers at 3 feet in the affected right eye, down from her baseline of 20/30. Her examination in the right eye demonstrated a large area of retinal whitening and overlying retinal hemorrhages along the inferotemporal arcade and inferior macula, with a smaller area of retinal whitening in the superotemporal macula (Fig. 2A). There was no significant vitreous infiltration. Her left eye had no new active lesions. Images were shown to her outside ophthalmologist, who confirmed that these were new lesions. All members of the retina (RU, RW, ZR) and uveitis (JC) services at our institution, as well as the outside ophthalmologist agreed that the clinical picture was most consistent with an infectious retinitis, which could be partially explained by her recent immunosuppression. The patient underwent an anterior chamber paracentesis for viral and toxoplasma PCR, followed by an intravitreal injection of foscarnet (2.4 mg/0.1 ml). She was initiated on oral valgancyclovir (900 mg BID) and trimethoprim-sulfamethoxazole (Bactrim DS BID). Eight days after presentation (Fig. 2, Fig. 3B) the patient underwent a second anterior chamber paracentesis and a second injection of foscarnet (2.4 mg/0.1 ml). Both paracentesis samples (sent to two different laboratories), were negative for toxoplasma, cytomegalovirus, herpes simplex virus 1/2, and varicella zoster virus by PCR. Serum tests for toxoplasma, cytomegalovirus, syphilis, and herpes simplex virus were also negative. Given the lack of clinical improvement, the patient received over the next 9 days two intravitreal injections of clindamycin (0.5 mg/0.05 ml), an injection of ganciclovir (2 mg/0.05 ml), and a third injection of foscarnet (see Fig. 2C and D). Yet, three weeks after starting this treatment regimen, the clinical picture was still slowly worsening. Because of the negative test results for infectious agents and the worsening clinical picture despite antiviral/antibiotic treatment, we suspected an atypical presentation of vitreoretinal lymphoma. Retinal and vitreous biopsy were considered, but taking into account the paucity of vitreous cells, the proximity of the retinal lesions to the fovea, and the preference of the patient to avoid surgical intervention, we made the decision to defer biopsy and initiate empiric therapy for lymphoma with intravitreal methotrexate injections (0.4 mg/0.1 ml formulation). Using this time point as a reference (Fig. 2, Fig. 3C), she received injections on days 0, 4, 11, 25, 53 and 81. Clinical improvement was suspected two days after her first injection and was undeniable by day 4 (Fig. 2, Fig. 3D). Her right eye visual acuity with spectacle correction improved to 20/40, with pinhole improvement to 20/25 (Fig. 2G). She was scheduled to have monthly injections, but due to travel issues her seventh injection was delayed by one week. During that week the patient experienced a decrease in vision to 20/80 and a recurrence of the retinal opacification and hemorrhages (Fig. 2H, arrowheads), and subretinal fluid (Fig. 3G). This time she was treated with intravitreal methotrexate without any antivirals/antibacterials, and again responded rapidly with improvement in vision to 20/25 and resolution of the retinal opacification, hemorrhages, and subretinal fluid (Fig. 2, Fig. 3H).
Fig. 2.
Ultra-widefield fundus photos of the right eye demonstrating the clinical course during the most recent presentation. The arrowheads (H) demarcate the main area of recurrence. Abbreviations: Tap = anterior chamber paracentesis for PCR testing, Fos = intravitreal foscarnet, Valg = oral valganciclovir, Bact = oral Bactrim DS, Ganci = intravitreal ganciclovir, Clinda = intravitreal clindamycin, MTX = intravitreal methotrexate.
Fig. 3.
Optical Coherence Tomography (OCT) of the right eye during the most recent presentation. An infrared photo (A) shows the location at which the OCT cuts were obtained. Vertical cuts through the central macula demonstrate the initial lack of response to anti-infectious therapy (B, C), response to intravitreal methotrexate (D, E, F), recurrence of disease after increasing the methotrexate injection interval (G), and eventual resolution after re-treatment with frequent intravitreal methotrexate injections without antivirals or antibiotics (H).
3. Discussion
This case presents with several unique features. First, the ocular tissue that was most prominently involved was the retina; i.e. there were sub-RPE lesions, but no choroidal lesions and minimal vitreous cells. Given her prior history of systemic lymphoma involving the cecum, and the fact that she never had any evidence of CNS infiltration, one would expect ocular involvement to present in the form of secondary choroidal lymphoma, rather than vitreoretinal lymphoma. This association has been described by many,2, 3, 4 but a recent report by Salomão et al.5 has shown that there are exceptions to this rule, with rare cases of vitreoretinal lymphoma presenting after systemic lymphoma.
Another interesting aspect of this case is that it emphasizes that recurrences of vitreoretinal lymphoma can have very different clinical presentations even in the same patient. Third, this case highlights the fact that vitreoretinal lymphoma can present as large areas of prominent retinal whitening and retinal hemorrhages indistinguishable from infectious retinitis. We could only find two other case reports of vitreoretinal lymphoma masquerading as retinitis.6,7 In contrast to our case, both of these cases presented with significant vitreous infiltration. But interestingly, one of these cases was similar to our case in that it combined the two atypical features of having a retinitis-like appearance, and of being a secondary vitreoretinal lymphoma in a patient that had previously had systemic lymphoma.7
Our case also demonstrates that vitreoretinal lymphoma can lead to severe recurrences even shortly after completion of an intensive and “clinically effective” treatment. Just 1 month after an aggressive local and systemic treatment, one would expect a low risk for lymphoma recurrence, and would be more concerned about some level of immunosuppression. Yet, while it is important to consider opportunistic infections, lymphoma recurrence must remain in the differential.
Finally, it should be noted that there is a great deal of variability with regards to treatment protocols, when dealing with intravitreal injections for intraocular lymphoma.8, 9, 10, 11, 12 However, even with intense protocols requiring a total of 25 injections in 1 year, it is possible for patients to have recurrences after stopping treatment (Dr. J. William Harbour, personal communication). Thus, we may need better parameters13 to decide how to tailor, and in particular, when to stop treatment.
4. Conclusions
This case illustrates the complex clinical nature of ocular lymphoma. The clinical presentation may be indistinguishable from an infectious retinitis. Also, it can have a vitreoretinal presentation (rather than choroidal) even when it follows a systemic (non-CNS) lymphoma. Recurrences can occur very quickly after a “successful” clinical response to systemic and/or local treatment. Furthermore, the clinical appearance of recurrences of vitreoretinal lymphoma may be diverse, even in the same patient. Finally, there is a need for better parameters to help assess subclinical activity, which will be instrumental in guiding therapeutic decisions.
Patient consent
As no identifying information is disclosed, patient consent was not obtained.
Conflicts of interest
There are no conflicts of interest to report.
Financial support
This work was supported by an unrestricted grant from Research to Prevent Blindness.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajoc.2019.100545.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
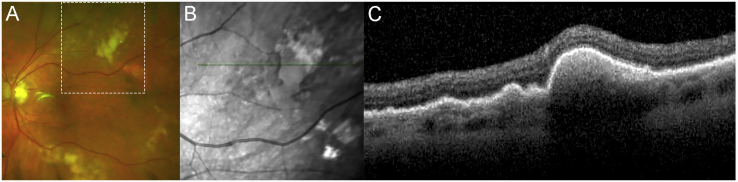
Supplemental Fig. S1.
Imaging of a sub-RPE lesion. A fundus photo (A), infrared image showing OCT registration line (B) and OCT image (C) showing the sub-RPE location of the clinical infiltrates are shown. The white dashed line in panel A demarcates the area captured in the infrared image.
References
- 1.Mochizuki M., Singh A.D. Epidemiology and clinical features of intraocular lymphoma. Ocul Immunol Inflamm. 2009;17:69–72. doi: 10.1080/09273940902957305. [DOI] [PubMed] [Google Scholar]
- 2.Coupland S.E., Damato B. Understanding intraocular lymphomas. Clin Exp Ophthalmol. 2008;36:564–578. doi: 10.1111/j.1442-9071.2008.01843.x. [DOI] [PubMed] [Google Scholar]
- 3.Chan C.C., Rubenstein J.L., Coupland S.E. Primary vitreoretinal lymphoma: a report from an international primary central nervous system lymphoma collaborative group symposium. The Oncologist. 2011;16:1589–1599. doi: 10.1634/theoncologist.2011-0210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mashayekhi A., Shukla S.Y., Shields J.A., Shields C.L. Choroidal lymphoma: clinical features and association with systemic lymphoma. Ophthalmology. 2014;121:342–351. doi: 10.1016/j.ophtha.2013.06.046. [DOI] [PubMed] [Google Scholar]
- 5.Salomão D.R., Pulido J.S., Johnston P.B., Canal-Fontcuberta I., Feldman A.L. Vitreoretinal presentation of secondary large B-cell lymphoma in patients with systemic lymphoma. JAMA Ophthalmol. 2013;131:1151–1158. doi: 10.1001/jamaophthalmol.2013.334. [DOI] [PubMed] [Google Scholar]
- 6.Zloto O., Elkader A.E., Fabian I.D., Vishnevskia-Dai V. Primary vitreoretinal lymphoma masquerading as refractory retinitis. Case Rep Ophthalmol. 2015;6:345–350. doi: 10.1159/000440762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ryan M.E., Shantha J.G., Grossniklaus H.E., Yeh S. Secondary vitreoretinal lymphoma masquerading as acute retinal necrosis. Ophthalmic Surg Lasers Imaging Retina. 2015;46:1048–1050. doi: 10.3928/23258160-20151027-11. [DOI] [PubMed] [Google Scholar]
- 8.Frenkel S., Hendler K., Siegal T., Shalom E., Pe'er J. Intravitreal methotrexate for treating vitreoretinal lymphoma: 10 years of experience. Br J Ophthalmol. 2008;92:383–388. doi: 10.1136/bjo.2007.127928. [DOI] [PubMed] [Google Scholar]
- 9.Fishburne B.C., Wilson D.J., Rosenbaum J.T., Neuwelt E.A. Intravitreal methotrexate as an adjunctive treatment of intraocular lymphoma. Arch Ophthalmol. 1997;115:1152–1156. doi: 10.1001/archopht.1997.01100160322009. [DOI] [PubMed] [Google Scholar]
- 10.Sou R., Ohguro N., Maeda T., Saishin Y., Tano Y. Treatment of primary intraocular lymphoma with intravitreal methotrexate. Jpn J Ophthalmol. 2008;52:167–174. doi: 10.1007/s10384-008-0519-9. [DOI] [PubMed] [Google Scholar]
- 11.de Smet M.D., Vancs V.S., Kohler D., Solomon D., Chan C.C. Intravitreal chemotherapy for the treatment of recurrent intraocular lymphoma. Br J Ophthalmol. 1999;83:448–451. doi: 10.1136/bjo.83.4.448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hashida N., Ohguro N., Nishida K. Efficacy and complications of intravitreal rituximab injection for treating primary vitreoretinal lymphoma. Transl Vis Sci Technol. 2012;1:1. doi: 10.1167/tvst.1.3.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Raja H., Snyder M.R., Johnston P.B. Effect of intravitreal methotrexate and rituximab on interleukin-10 levels in aqueous humor of treated eyes with vitreoretinal lymphoma. PLoS One. 2013;8 doi: 10.1371/journal.pone.0065627. [DOI] [PMC free article] [PubMed] [Google Scholar]