Abstract
Background
Metabolic syndrome (MetS) is a known predictor of diabetes mellitus (DM), but whether longitudinal changes in MetS status modify the risk for DM remains unclear. We investigated whether changes in MetS status over 2 years modify the 10-year risk of incident DM.
Methods
We analyzed data from 7,317 participants aged 40 to 70 years without DM at baseline, who took part in 2001 to 2011 Korean Genome Epidemiology Study. Subjects were categorized into four groups based on repeated longitudinal assessment of MetS status over 2 years: non-MetS, resolved MetS, incident MetS, and persistent MetS. The hazard ratio (HR) of new-onset DM during 10 years was calculated in each group using Cox models.
Results
During the 10-year follow-up, 1,099 participants (15.0%) developed DM. Compared to the non-MetS group, the fully adjusted HRs for new-onset DM were 1.28 (95% confidence interval [CI], 0.92 to 1.79) in the resolved MetS group, 1.75 (95% CI, 1.30 to 2.37) in the incident MetS group, and 1.98 (95% CI, 1.50 to 2.61) in the persistent MetS group (P for trend <0.001). The risk of DM in subjects with resolved MetS was significantly attenuated compared to those with persistent MetS over 2 years. In addition, the adjusted HR for 10-year developing DM gradually increased as the number of MetS components increased 2 years later.
Conclusion
We found that discrete longitudinal changes pattern in MetS status over 2 years associated with 10-year risk of DM. These findings suggest that monitoring change of MetS status and controlling it in individuals may be important for risk prediction of DM.
Keywords: Diabetes mellitus, Life style, Metabolic syndrome
INTRODUCTION
Metabolic syndrome (MetS) refers to a clustering of specific cardiovascular disease risk factors whose underlying pathophysiology is thought to be related to insulin resistance; these factors include central obesity, dyslipidemia, impaired glucose tolerance, and hypertension [1]. MetS is very common globally, and its prevalence is increasing together with the rapidly increasing prevalence of obesity [2,3,4]. Subjects with MetS are approximately two times more likely to develop cardiovascular disease [5,6] and 3.5 to 5 times more likely to develop type 2 diabetes mellitus (DM) [7]. However, in the majority of previous studies which investigated the impact of MetS on chronic disease, MetS was assessed only once at baseline. It is worth noting that the majority of published studies on this topic were based on a single assessment of MetS, failing to take into account the potential effect of change in MetS status over time.
Considering that MetS itself is not a frank disease but a cluster of metabolic abnormalities, MetS status in individuals is likely not fixed but variable over time [8,9]. Indeed, recent study demonstrated that a considerable number of participants in a Japanese population (27.2%) showed changes in their MetS status over a 10-year period [10]. Walden et al. [11] also presented that even short-term (6-month) lifestyle interventions significantly improve overall MetS status and reduce the number of MetS components. Moreover, one recent cohort study presented that persistent MetS over a 10-year follow-up, rather than MetS at a given moment, was associated with lower cognitive performance in late midlife [12]. From these findings, we speculate that changes in MetS status could be an independent risk factor for chronic metabolic disease.
Although many previous studies have shown that MetS at baseline is closely associated with incident DM, the relationship between changes in MetS status over mid-term periods of time and future risk of DM remains poorly characterized. Thus, we aimed to investigate the potential impact of longitudinal changes in MetS status, based on repeated two assessments of MetS status over 2 years, on the 10-year risk of developing DM.
METHODS
Study population and design
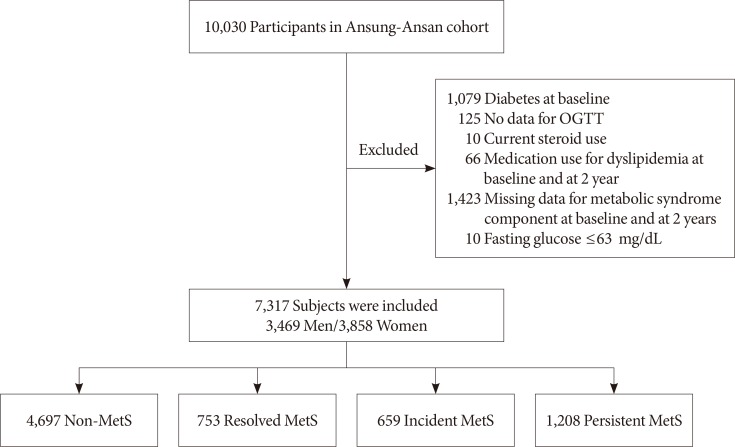
We recruited participants from the Ansung-Ansan cohort study, an ongoing prospective study from 2001 embedded within the Korean Genome Epidemiology Study (KoGES). This cohort consists of a population sample of Korean males and females aged 40 to 69 years with the same ethnic background. The study participants were re-examined at 2-year intervals, and they participated in the sixth follow-up survey. Further details regarding KoGES and detailed methods have been published elsewhere [13,14]. The baseline survey, carried out from 2001 to 2002, included 10,030 adults aged 40 to 70 years. All study participants were invited to the follow-up survey and 6,238 (62.1%) attended. Among them, 1,079 subjects were excluded for having DM at baseline examination and 125 subjects with no data for the 75-g oral glucose tolerance test (OGTT) were also excluded. We also excluded current users of steroids (n=10) and subjects who were taking medication for dyslipidemia at baseline and at 2 years (n=66), those with missing data for MetS components at baseline and at 2 years (n=36), and those having a low level of fasting glucose (≤63 mg/dL) (n=10). After excluding ineligible subjects, the final sample size for the present analysis was 7,317 individuals (3,469 male and 3,858 female) without DM at baseline and at the 2-year follow-up. According to the changes in MetS status between baseline and the follow-up visit over 2 years, participants were divided into four groups: a non-MetS to non-MetS group (non-MetS group), a non-MetS to MetS group (incident MetS group), a MetS to non-MetS group (resolved MetS group), and a MetS to MetS group (persistent MetS group) (Fig. 1). At each visit, informed written consent was obtained from all participants. The study protocol was approved by the Ethics Committee of the Korean Center for Disease Control and the Institutional Review Board of Wonju Severance Christian Hospital (CR318317).
Fig. 1. Flow chart. OGTT, oral glucose tolerance test; MetS, metabolic syndrome.
Data collection
Study participants in KoGES are examined as frequently as biannually, and at this time are asked to complete self-reported questionnaires on their personal and family medical histories, smoking habits, alcohol consumption, exercise status, and use of medication. For the present study, participants were categorized according to smoking status (never, past, or current smoker) and exercise status (none, ≤3 times per week or regular exercise, or ≥4 times per week). Height, body weight, and waist and hip circumference were measured using standard methods. Waist circumference was measured at the narrowest point between the upper iliac crest and lowest rib after normal expiration. Blood pressure was measured by averaging three recordings taken in the morning after at least 10 minutes of rest in a sitting position. Laboratory samples were obtained after a 12-hour fast. Plasma total cholesterol, triglycerides, high density lipoprotein cholesterol (HDL-C), creatinine, and alanine and aspartate aminotransferases (ALT and AST, respectively) were measured using a Hitachi 747 chemistry analyzer (Hitachi Ltd., Tokyo, Japan). Low density lipoprotein cholesterol was assessed by the Friedewald equation. Plasma samples were taken at 0 and 120 minutes during a 75-g OGTT and assessed for plasma glucose and insulin concentrations using the hexokinase method and a radioimmunoassay kit (LINCO Research, St. Charles, MO, USA), respectively. Glycosylated hemoglobin (HbA1c) levels were measured using high-performance liquid chromatography (Variant II; Bio-Rad, Hercules, CA, USA). The homeostasis model assessment of insulin resistance (HOMA-IR) and β-cell function (HOMA-β) indices were calculated using the following respective formulas: [fasting plasma insulin (µIU/mL)×fasting plasma glucose (mg/dL)/405] and [fasting insulin (µIU/mL)×20/fasting glucose (mg/dL)×0.05551−3.5] [15].
Definition of MetS and incident DM
Based on the modified National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATP III) criteria [16], MetS was defined as the presence of three or more of the following components: (1) abdominal obesity, defined as a waist circumference ≥90 cm for males or ≥85 cm for females (following Korean specific cutoffs for abdominal obesity defined by the Korean Society of Obesity); (2) hypertriglyceridemia, defined as a serum triglyceride concentration ≥150 mg/dL; (3) low HDL-C, defined as a serum HDL-C concentration <40 mg/dL for males or <50 mg/dL for females; (4) high blood pressure, defined as systolic blood pressure (SBP) ≥130 mm Hg, diastolic blood pressure (DBP) ≥85 mm Hg, or treatment with antihypertensive agents; and (5) high fasting glucose, defined as a fasting serum glucose ≥100 mg/dL. In the present study, incident diabetes was defined as the current use of oral diabetes medication or insulin injections, a fasting glucose level ≥126 mg/dL, or a post-load glucose level ≥200 mg/dL during the 2-hour 75-g OGTT, performed biannually as per the 1997 American Diabetes Association criteria [17].
Statistial analysis
Continuous variables are presented as mean±standard deviation, and categorical variables are expressed as numbers and percentages (%). Differences among groups were analyzed using analysis of variance (ANOVA) with Scheffe's post hoc analysis method for continuous variables and chi-square tests for categorical variables. Cumulative rates of the incidence of DM were estimated by Kaplan-Meier survival curves, and equality was compared by log-rank tests. Cox proportional-hazards analyses were conducted to estimate the hazard ratio (HR) and 95% confidence interval (CI) for investigating the association between changes in MetS over 2 years and the development of DM. We used three models with progressive degrees of adjustment. First, we performed an age-adjusted (continuous variable) and sex (categorical variable) analysis. Second, we adjusted for family history of DM (yes/no), smoking (never/past/current smoker), alcohol intake (continuous variable), regular exercise (none, ≤3 times per week or regular exercise, or ≥4 times per week), and SBP (continuous variable). Finally, we further adjusted for body mass index (continuous variable), 2-hour glucose (continuous variable), ALT (continuous variable), total cholesterol (continuous variable), and baseline levels of HOMA-IR (log-transformed continuous variable). A cubic spline regression model was used to assess continuous changes in the number of MetS components over 2 years and the adjusted HR for 10-year incident DM. A P<0.05 was significant. All statistical analyses were conducted using SAS version 9.2 (SAS, Cary, NC, USA).
RESULTS
Characteristics of participants
Clinical and biochemical characteristics of the study subjects according to 2-year changes in MetS status are shown in Table 1. Overall, 19.3% (n=1,412) of participants showed changes in their MetS status from baseline to 2 years. Specifically, 10.3% (n=753) of the total subjects were classified into the resolved MetS group and 9.0% (n=659) were in the incident MetS group. Furthermore, 70.2% (n=4,697) of the participants were in the non-MetS group and 16.5% (n=1,208) of the total subjects had persistent MetS. Compared with non-MetS individuals, the other three groups were more likely to be older, never smokers, and to have a less favorable metabolic risk profiles (Table 1). Waist circumference, body mass index, SBP, DBP, levels of fasting glucose concentration, HbA1c, and HOMA-IR were significantly lower in the resolved MetS group compared with the persistent MetS group. In contrast HDL-C levels were higher in the resolved MetS group compared with those in the persistent MetS group. There was no difference in the proportion of individuals engaging in ‘regular exercise’ or alcohol intake among the four groups.
Table 1. Baseline characteristics of study participants according to changes in metabolic syndrome status over 2 years.
| Variable | Non-MetS | Resolved MetS | Incident MetS | Persistent MetS | P value |
|---|---|---|---|---|---|
| Number (%) | 4,697 (64.2) | 753 (10.3) | 659 (9.0) | 1,208 (16.5) | |
| Age, yr | 50.4±8.6a,b,c | 54.0±8.6c,d | 53.2±8.7c,d | 55.2±8.5a,b,d | <0.0001 |
| Male sex | 2,377 (50.5) | 323 (42.8) | 309 (46.8) | 460 (38.1) | <0.0001 |
| SBP, mm Hg | 118.5±16.3a,b,c | 132.5±16.6b,c,d | 126.7±18.4a,c,d | 136.8±16.9a,b,d | <0.0001 |
| DBP, mm Hg | 79.4±10.7a,b,c | 88.0±10.2b,c,d | 83.8±11.4a,c,d | 90.4±10.4a,b,d | <0.0001 |
| BMI, kg/m2 | 23.6±2.7a,b,c | 25.8±2.7c,d | 25.6±2.8c,d | 27.0±2.8a,b,d | <0.0001 |
| Delta BMI, kg/m2 | 0.0±1.0a,b,c | -0.4±1.1b,c,d | 0.3±1.0a,c,d | 0.1±1.0a,b,d | <0.0001 |
| Waist circumference, cm | 78.9±7.4a,b,c | 87.6±7.6b,c,d | 85.5±6.6a,c,d | 90.9±6.8a,b,d | <0.0001 |
| Total cholesterol, mg/dL | 186.8±33.4a,b,c | 195.5±33.5c,d | 191.4±35.7c,d | 196.3±33.3a,b,d | <0.0001 |
| Triglyceride, mg/dL | 128.9±73.5a,b,c | 213.8±112.2b,d | 153.3±80.7a,c,d | 221.5±110.2b,d | <0.0001 |
| HDL-C, mg/dL | 47.4±10.0a,b,c | 39.7±7.5b,c,d | 43.8±8.8a,c,d | 38.4±6.9a,b,d | <0.0001 |
| LDL-C, mg/dL | 113.6±31.0 | 113.0±33.8 | 117.0±34.8 | 113.6±33.1 | 0.0693 |
| Fasting glucose, mg/dL | 81.9±7.9a,b,c | 83.9±10.0b,c,d | 85.2±8.4a,d | 85.7±10.0a,d | <0.0001 |
| Post-load glucose, mg/dL | 110.1±29.0a,b,c | 123.0±33.3b,d | 118.2±30.5a,c,d | 123.6±30.8b,d | <0.0001 |
| Fasting insulin, μIU/mL | 6.9±4.0a,b,c | 8.4±5.3b,d | 8.2±6.4a,c,d | 9.5±5.6b,d | <0.0001 |
| Post-load insulin, μIU/mL | 24.3±22.2a,b,c | 34.5±30.3b,c,d | 28.8±23.2a,c,d | 39.0±37.3a,d | <0.0001 |
| HbA1c, % | 5.5±0.4a,b,c | 5.7±0.4c,d | 5.7±0.4c,d | 5.7±0.4a,b,d | <0.0001 |
| HOMA-IR | 1.4±0.8a,b,c | 1.8±1.1c,d | 1.7±1.3c,d | 2.0±1.2a,b,d | <0.0001 |
| Delta HOMA-IR | 0.2±1.0a | 0.0±1.4b,d | 0.3±1.6a | 0.1±1.5 | 0.0001 |
| HOMA-β | 160.8±152.6a,c | 182.0±154.0b,d | 156.7±156.3a,c | 185.1±174.9b,d | <0.0001 |
| AST, IU/L | 28.7±17.0 | 30.4±21.1 | 29.4±15.9 | 30.0±13.3 | 0.0084 |
| ALT, IU/L | 25.2±20.9c | 29.8±20.7d | 28.5±18.7c,d | 31.6±20.9d | <0.0001 |
| GGT, IU/L | 28.2±43.4a,b,c | 37.2±70.9d | 43.2±114.2d | 37.8±62.6d | <0.0001 |
| Family history of diabetes | 506 (10.8) | 78 (10.3) | 80 (12.1) | 113 (9.4) | 0.2926 |
| Regular exercise | 674 (14.3) | 104 (13.8) | 79 (12.0) | 155 (12.8) | 0.2668 |
| Alcohol intake, g/day | 9.2±20.2 | 7.9±18.9 | 10.3±22.1 | 8.4±21.5 | 0.1097 |
| Smoking status | 0.0003 | ||||
| Never smoker | 2,705 (58.1) | 465 (62.6) | 372 (57.6) | 771 (64.7) | |
| Ex-smoker | 724 (15.6) | 118 (15.9) | 100 (15.5) | 171 (14.4) | |
| Current smoker | 1,228 (26.4) | 160 (21.5) | 174 (26.9) | 250 (21.0) |
Values are presented as number (%) or mean±standard deviation.
MetS, metabolic syndrome; SBP, systolic blood pressure; DBP, diastolic blood pressure; BMI, body mass index; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; HbA1c, glycosylated hemoglobin; HOMA-IR, homeostasis model assessment of insulin resistance; HOMA-β, homeostasis model assessment of β-cell function; AST, aspartate aminotransferase; ALT, alanine aminotransferase; GGT, gamma-glutamyl transferase.
aP<0.05 vs. resolved MetS after analysis of variance (ANOVA) followed by Scheffé post hoc comparison, bP<0.05 vs. incident MetS after ANOVA followed by Scheffé post hoc comparison, cP<0.05 vs. persistent MetS after ANOVA followed by Scheffé post hoc comparison, dP<0.05 vs. non-MetS after ANOVA followed by Scheffé post hoc comparison.
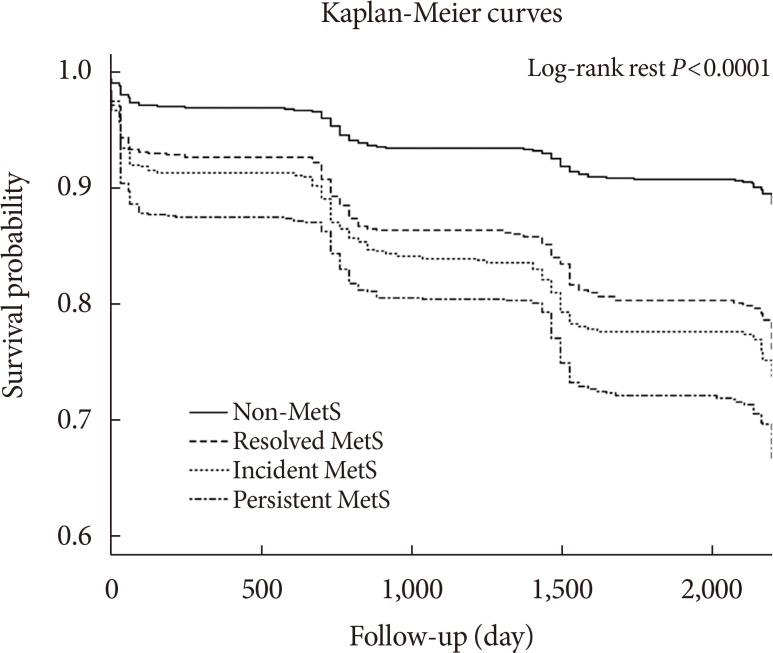
Kaplan-Meier plot of time to disease according to the 2-year changes in MetS status
Of the 7,317 participants analyzed in our study, 1,099 (15.0%) developed DM during the 10-year follow-up. The Kaplan-Meier survival curves for cumulative survival free from DM during the 10-year follow-up period based on two repeated longitudinal assessments of MetS status over 2 years are shown in Fig. 2. Compared with the non-MetS group, the other three groups (that is, resolved MetS, incident MetS, and persistent MetS groups) had higher probabilities of developing incident DM. Cumulative incidence of DM significantly decreased to the greatest degree for the resolved MetS group, followed by the incident MetS group, and then the persistent MetS group (log-rank test, P<0.05 for all three comparisons). Although the survival curves between resolved MetS and incident MetS groups were not significantly different (log-rank test, P=0.156), differences between the resolved MetS and persistent MetS groups were significant (log-rank test, P<0.001). It suggests that people in the resolved MetS had significantly lower risk of incident DM compared to people in the persistent MetS group.
Fig. 2. Diabetes-free survival duration according to change in metabolic syndrome (MetS) status from baseline to 2 years by Kaplan-Meier analysis.
Relationship between 2-year changes in MetS status and 10-year incident DM
Cox proportional-hazards analysis was used to investigate the risk of 10-year incident DM according to the changes in MetS status from baseline to 2 years (Table 2). The crude HRs of DM were 2.21 (95% CI, 1.84 to 2.66) in the resolved MetS group, 2.60 (95% CI, 2.17 to 3.13) in the incident MetS group, and 3.28 (95% CI, 2.85 to 3.78) in the persistent MetS group compared with the non-MetS group (P for trend <0.001). Compared to the non-MetS group, the incident MetS and persistent MetS groups had a significantly higher risk of 10-year incident DM even after adjustment for multiple risk factors for diabetes. While, risk of developing diabetes in resolved MetS group was attenuated with insignificant HR 1.28 (95% CI, 0.92 to 1.79) in fully adjusted model (Model 4 in Table 2). Among the four groups, participants with persistent MetS showed the highest incidence risk of DM (HR, 1.98; 95% CI, 1.50 to 2.61), and participants with resolved MetS showed attenuated risk of developing DM (HR, 1.28; 95% CI, 0.92 to 1.79). The difference was statistically significant (P<0.0001).
Table 2. Association between 2-year metabolic syndrome status change and incidence of diabetes (Cox models).
| Variable | Non-MetS | Resolved MetS | Incident MetS | Persistent MetS | P value |
|---|---|---|---|---|---|
| Incident DM case | 459 (9.8) | 151 (20.1) | 152 (23.1) | 337 (27.9) | >0.001 |
| Crude hazard ratio | Reference | 2.21 (1.84–2.66) | 2.60 (2.17–3.13) | 3.28 (2.85–3.78) | <0.001 |
| Model 1 | Reference | 2.20 (1.83–2.65) | 2.54 (2.11–3.05) | 3.27 (2.83–3.77) | <0.001 |
| Model 2 | Reference | 1.94 (1.59–2.37) | 2.39 (1.98–2.90) | 2.91 (2.48–3.42) | <0.001 |
| Model 3 | Reference | 1.28 (1.01–1.61) | 1.78 (1.43–2.22) | 1.85 (1.52–2.26) | <0.001 |
| Model 4 | Reference | 1.28 (0.92–1.79) | 1.75 (1.30–2.37) | 1.98 (1.50–2.61) | <0.001 |
Values are presented as number (%). Model 1: adjusted for sex, age; Model 2: Model 1+family history of diabetes, smoking, alcohol intake, regular exercise, energy intake, and systolic blood pressure; Model 3: Model 2+body mass index (BMI), post-load glucose, alanine aminotransferase, total cholesterol, estimated glomerular filtration rate, and homeostasis model assessment of insulin resistance (HOMA-IR); Model 4: Model 3+delta BMI, regular exercise (follow-up) and delta HOMA-IR.
MetS, metabolic syndrome; DM, diabetes mellitus.
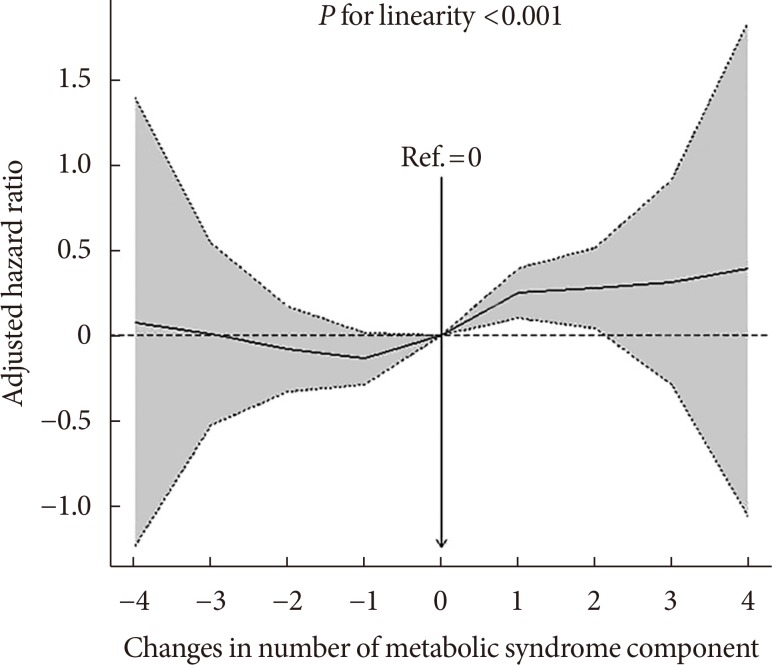
Relationship between 2-year changes in the number of MetS components and incident DM
Changes in the number of MetS components over 2 years as a continuous variable showed a strong association with the likelihood of developing DM after 10 years, even after adjustment for confounding factors (Fig. 3). In addition, a positive curve-linear relationship was found between the adjusted HR for incident diabetes and changes in the number of MetS components based on the Cox proportional-hazards model fitted in a cubic spline (P<0.001 for linearity) (Model 3 at Table 2, Fig. 3).
Fig. 3. Adjusted hazard ratio (HR) for incident diabetes according to changes in number of metabolic syndrome component for 2 years follow-up. The data shown are from cubic splines and the 95% confidence intervals. Adjusted HRs are from Cox proportional-hazards models after adjusting for age, sex, family history of diabetes, smoking, alcohol intake, regular exercise, energy intake, body mass index, alanine aminotransferases, and post-load glucose at baseline.
DISCUSSION
In this large prospective cohort study in a general Asian population, we observed changes in MetS status during a 2-year period as well as the presence of MetS at baseline were independent predictors for the future 10-year DM risk. This study has three main findings. First, incident MetS and persistent MetS over 2 years were significantly associated with 10-year incident DM even after adjustment for confounding factors and resolved MetS over 2 years did not significantly increase the risk of diabetes after adjustment for confounding factors. Second, the risk of DM was the highest in the persistent MetS (approximate two-fold higher risk of incident DM), followed by the incident MetS, and resolved MetS, in that order. Third, the 10-year risk of DM was attenuated in subjects who had resolved their MetS status over 2 years compared to those who had persistent MetS status. To the best of our knowledge, this is the first largest community-based longitudinal cohort study to report the late effect of temporal changes in MetS over a short-term period on the further occurrence of diabetes. The prospective design, the strength of the associations, and the graded dose-response relationships of MetS status suggest that longitudinal changes in MetS status and its components may play a key role in the development of DM.
MetS is a traditionally well-known independent risk factor for DM. Although each individual MetS component—high fasting glucose, dyslipidemia, high blood pressure, etc.—is a strong predictor for DM, MetS-related pathophysiologic processes (i.e., adipocyte dysfunction, systemic inflammation, and oxidative stress) also may contribute to the development of DM. For this reason, beyond the predictive ability of each MetS component, MetS itself has been considered a strong predictor for incident DM. Similarly, our study demonstrates that an increased number of MetS components over time also increases long-term risk of future DM regardless of MetS components. Given the importance of lifestyle modification for improvement of MetS and MetS-related disease risk, a recent study showed that a 6-month lifestyle change program reduced the number of MetS components with a decreased level of HOMA-IR as a measure of insulin resistance, and high-sensitivity C-reactive protein as a measure of systemic inflammation [11]. Furthermore, incident MetS and maintenance of the MetS status during a 10-year period were strong risk factors for DM [10]. However, this study evaluated the changes in MetS and occurrence of DM at the same time point, which is different from our study. Regarding the fact that motivation for lifestyle changes cannot be usually maintained for a long time in a clinical setting, our study aimed to evaluate whether early temporal metabolic control influences long-term clinical outcomes.
A major result of this study was that resolution of MetS during a short-term period attenuated future 10-year DM risk, especially compared to those with persistent MetS during the same time. It should be noted that even after adjustment for individual MetS components at baseline (i.e., glucose and SBP), subjects with resolved MetS status showed significantly attenuated future DM risk. The mechanism as to why changes in MetS status during a short-term period might modify risk of developing DM 10 years later is not clear; however, ‘cardiometabolic memory’ can be one of plausible mechanism for this phenomenon [18,19]. Cardiometabolic memory has been suggested based on clinical evidence to explain how, even after the cessation of a clinical trial, the superiority of one treatment over the outcome persists [20]. Recent studies demonstrated that transient intensive glucose lowering induces memory for the suppression of diabetic microangiopathies and transient intensive blood pressure and cholesterol lowering were also resulted in the formation of memory for the suppression of cardiovascular events in the long term follow-up period [21,22,23]. In line with these observations, several clinical trials demonstrated that lifestyle modification aimed at glucose lowering was very effective in the suppression of new onset diabetes even after the termination of clinical trials [24,25]. This concept provides evidence for the proper interventions for patients with metabolic abnormalities and cardiovascular risks as early as possible for prevention of diabetes in the long run.
This study has some limitations. First, there may be a selection bias because we included participants who received examinations at both baseline and the second visit. Because these patients might be more concerned with their health than those who did not attend one or both visits, we may have underestimated the impact of changes of MetS status on incident DM. However, we tried to avoid this bias before selecting. Second, we could not assess the presence of cardiometabolic abnormalities in 37.9% of the sample that did not complete the follow-up visit. Finally, there may be racial/ethnic differences in MetS that limit translating these results to other countries [26,27,28], so our findings should be applied to other ethnic groups with caution.
Collectively, our study demonstrated that not only the presence of MetS at baseline but also changes in MetS status may influence the risk of future incident DM in a 10-year longitudinal study. Although MetS at baseline increases future DM risk, this risk was attenuated by resolution of MetS status from baseline to 2 years compared to those with persistent MetS status. These findings suggest monitoring status change of MetS may provide an important approach to identify a population with higher risk of DM and help to prevent DM in clinical practice. Further studies with different racial and ethnic compositions are also warranted to replicate our findings.
ACKNOWLEDGMENTS
This study was partly supported by the Korean Society of Cardiometabolic Syndrome and Gangwon branch of Korean Endocrine Society.
This study was supported by the Center for Genome Science, Korea National Institute of Health, Korea Centers for Disease Control and Prevention (contract numbers 2001; 2003-348-6111-221, 2004-347-6111-213, and 2005-347-2400-2440-215). The data from the Center for Genome Science, Korea National Institute of Health, Korea Centers for Disease Control and Prevention were provided under the condition that the Korea Centers for Disease Control and Prevention would be given opportunity to comment on the manuscript before submission for publication.
Footnotes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
- Conception or design: S.G.A., J.Y.K.
- Acquisition, analysis, or interpretation of data: J.H.H., Y.I.K., T.G.
- Drafting the work or revising: J.H.H., S.G.A., K.C.S., K.K.K.
- Final approval of the manuscript: J.H.C., K.K.K., J.Y.K.
References
- 1.Kahn R, Buse J, Ferrannini E, Stern M American Diabetes Association; European Association for the Study of Diabetes. The metabolic syndrome: time for a critical appraisal: joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2005;28:2289–2304. doi: 10.2337/diacare.28.9.2289. [DOI] [PubMed] [Google Scholar]
- 2.Aguilar M, Bhuket T, Torres S, Liu B, Wong RJ. Prevalence of the metabolic syndrome in the United States, 2003-2012. JAMA. 2015;313:1973–1974. doi: 10.1001/jama.2015.4260. [DOI] [PubMed] [Google Scholar]
- 3.Zuo H, Shi Z, Hu X, Wu M, Guo Z, Hussain A. Prevalence of metabolic syndrome and factors associated with its components in Chinese adults. Metabolism. 2009;58:1102–1108. doi: 10.1016/j.metabol.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 4.Lim S, Shin H, Song JH, Kwak SH, Kang SM, Won Yoon J, Choi SH, Cho SI, Park KS, Lee HK, Jang HC, Koh KK. Increasing prevalence of metabolic syndrome in Korea: the Korean National Health and Nutrition Examination Survey for 1998-2007. Diabetes Care. 2011;34:1323–1328. doi: 10.2337/dc10-2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dekker JM, Girman C, Rhodes T, Nijpels G, Stehouwer CD, Bouter LM, Heine RJ. Metabolic syndrome and 10-year cardiovascular disease risk in the Hoorn Study. Circulation. 2005;112:666–673. doi: 10.1161/CIRCULATIONAHA.104.516948. [DOI] [PubMed] [Google Scholar]
- 6.Vinluan CM, Zreikat HH, Levy JR, Cheang KI. Comparison of different metabolic syndrome definitions and risks of incident cardiovascular events in the elderly. Metabolism. 2012;61:302–309. doi: 10.1016/j.metabol.2011.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hanley AJ, Karter AJ, Williams K, Festa A, D'Agostino RB, Jr, Wagenknecht LE, Haffner SM. Prediction of type 2 diabetes mellitus with alternative definitions of the metabolic syndrome: the Insulin Resistance Atherosclerosis Study. Circulation. 2005;112:3713–3721. doi: 10.1161/CIRCULATIONAHA.105.559633. [DOI] [PubMed] [Google Scholar]
- 8.Chen W, Srinivasan SR, Li S, Xu J, Berenson GS. Clustering of long-term trends in metabolic syndrome variables from childhood to adulthood in Blacks and Whites: the Bogalusa Heart Study. Am J Epidemiol. 2007;166:527–533. doi: 10.1093/aje/kwm105. [DOI] [PubMed] [Google Scholar]
- 9.Wilson PW, D'Agostino RB, Parise H, Sullivan L, Meigs JB. Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation. 2005;112:3066–3072. doi: 10.1161/CIRCULATIONAHA.105.539528. [DOI] [PubMed] [Google Scholar]
- 10.Ohnishi H, Saitoh S, Akasaka H, Furukawa T, Mori M, Miura T. Impact of longitudinal status change in metabolic syndrome defined by two different criteria on new onset of type 2 diabetes in a general Japanese population: the Tanno-Sobetsu Study. Diabetol Metab Syndr. 2016;8:64. doi: 10.1186/s13098-016-0182-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walden P, Jiang Q, Jackson EA, Oral EA, Weintraub MS, Rubenfire M. Assessing the incremental benefit of an extended duration lifestyle intervention for the components of the metabolic syndrome. Diabetes Metab Syndr Obes. 2016;9:177–184. doi: 10.2147/DMSO.S94772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Akbaraly TN, Kivimaki M, Shipley MJ, Tabak AG, Jokela M, Virtanen M, Marmot MG, Ferrie JE, Singh-Manoux A. Metabolic syndrome over 10 years and cognitive functioning in late midlife: the Whitehall II study. Diabetes Care. 2010;33:84–89. doi: 10.2337/dc09-1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cho YS, Go MJ, Kim YJ, Heo JY, Oh JH, Ban HJ, Yoon D, Lee MH, Kim DJ, Park M, Cha SH, Kim JW, Han BG, Min H, Ahn Y, Park MS, Han HR, Jang HY, Cho EY, Lee JE, Cho NH, Shin C, Park T, Park JW, Lee JK, Cardon L, Clarke G, McCarthy MI, Lee JY, Lee JK, Oh B, Kim HL. A large-scale genome-wide association study of Asian populations uncovers genetic factors influencing eight quantitative traits. Nat Genet. 2009;41:527–534. doi: 10.1038/ng.357. [DOI] [PubMed] [Google Scholar]
- 14.Lim S, Jang HC, Lee HK, Kimm KC, Park C, Cho NH. A rural-urban comparison of the characteristics of the metabolic syndrome by gender in Korea: the Korean Health and Genome Study (KHGS) J Endocrinol Invest. 2006;29:313–319. doi: 10.1007/BF03344102. [DOI] [PubMed] [Google Scholar]
- 15.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 16.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC, Jr, Spertus JA, Costa F American Heart Association; National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 17.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37(Suppl 1):S81–S90. doi: 10.2337/dc14-S081. [DOI] [PubMed] [Google Scholar]
- 18.Ceriello A. Hypothesis: the “metabolic memory”, the new challenge of diabetes. Diabetes Res Clin Pract. 2009;86(Suppl 1):S2–S6. doi: 10.1016/S0168-8227(09)70002-6. [DOI] [PubMed] [Google Scholar]
- 19.Ihnat MA, Thorpe JE, Kamat CD, Szabo C, Green DE, Warnke LA, Lacza Z, Cselenyak A, Ross K, Shakir S, Piconi L, Kaltreider RC, Ceriello A. Reactive oxygen species mediate a cellular ‘memory’ of high glucose stress signalling. Diabetologia. 2007;50:1523–1531. doi: 10.1007/s00125-007-0684-2. [DOI] [PubMed] [Google Scholar]
- 20.Itoh H, Kurihara I, Miyashita K, Tanaka M. Clinical significance of ‘cardiometabolic memory’: a systematic review of randomized controlled trials. Hypertens Res. 2017;40:526–534. doi: 10.1038/hr.2016.192. [DOI] [PubMed] [Google Scholar]
- 21.Action to Control Cardiovascular Risk in Diabetes Follow-On (ACCORDION) Eye Study Group and the Action to Control Cardiovascular Risk in Diabetes Follow-On (ACCORDION) Study Group. Persistent effects of intensive glycemic control on retinopathy in type 2 diabetes in the action to control cardiovascular risk in diabetes (ACCORD) follow-on study. Diabetes Care. 2016;39:1089–1100. doi: 10.2337/dc16-0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong MG, Perkovic V, Chalmers J, Woodward M, Li Q, Cooper ME, Hamet P, Harrap S, Heller S, MacMahon S, Mancia G, Marre M, Matthews D, Neal B, Poulter N, Rodgers A, Williams B, Zoungas S ADVANCE-ON Collaborative Group. Long-term benefits of intensive glucose control for preventing end-stage kidney disease: ADVANCE-ON. Diabetes Care. 2016;39:694–700. doi: 10.2337/dc15-2322. [DOI] [PubMed] [Google Scholar]
- 23.Bosch J, Lonn E, Pogue J, Arnold JM, Dagenais GR, Yusuf S HOPE/HOPE-TOO Study Investigators. Long-term effects of ramipril on cardiovascular events and on diabetes: results of the HOPE study extension. Circulation. 2005;112:1339–1346. doi: 10.1161/CIRCULATIONAHA.105.548461. [DOI] [PubMed] [Google Scholar]
- 24.Lindstrom J, Peltonen M, Eriksson JG, Ilanne-Parikka P, Aunola S, Keinänen-Kiukaanniemi S, Uusitupa M, Tuomilehto J Finnish Diabetes Prevention Study (DPS) Improved lifestyle and decreased diabetes risk over 13 years: long-term follow-up of the randomised Finnish Diabetes Prevention Study (DPS) Diabetologia. 2013;56:284–293. doi: 10.1007/s00125-012-2752-5. [DOI] [PubMed] [Google Scholar]
- 25.Li G, Zhang P, Wang J, Gregg EW, Yang W, Gong Q, Li H, Li H, Jiang Y, An Y, Shuai Y, Zhang B, Zhang J, Thompson TJ, Gerzoff RB, Roglic G, Hu Y, Bennett PH. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet. 2008;371:1783–1789. doi: 10.1016/S0140-6736(08)60766-7. [DOI] [PubMed] [Google Scholar]
- 26.Sumner AE, Cowie CC. Ethnic differences in the ability of triglyceride levels to identify insulin resistance. Atherosclerosis. 2008;196:696–703. doi: 10.1016/j.atherosclerosis.2006.12.018. [DOI] [PubMed] [Google Scholar]
- 27.Walker SE, Gurka MJ, Oliver MN, Johns DW, DeBoer MD. Racial/ethnic discrepancies in the metabolic syndrome begin in childhood and persist after adjustment for environmental factors. Nutr Metab Cardiovasc Dis. 2012;22:141–148. doi: 10.1016/j.numecd.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gaillard T, Schuster D, Osei K. Differential impact of serum glucose, triglycerides, and high-density lipoprotein cholesterol on cardiovascular risk factor burden in nondiabetic, obese African American women: implications for the prevalence of metabolic syndrome. Metabolism. 2010;59:1115–1123. doi: 10.1016/j.metabol.2009.09.035. [DOI] [PubMed] [Google Scholar]