Abstract
Background
Workload from electronic health record (EHR) inbox notifications leads to information overload and contributes to job dissatisfaction and physician burnout. Better understanding of physicians’ inbox requirements and workflows could optimize inbox designs, enhance efficiency, and reduce safety risks from information overload.
Design
We conducted a mixed-methods study to identify strategies to enhance EHR inbox design and workflow. First, we performed a secondary analysis of national survey data of all Department of Veterans Affairs (VA) primary care practitioners (PCP) to identify major themes in responses to a free-text question soliciting suggestions to improve EHR inbox design and workflows. We then conducted expert interviews of clinicians at five health care systems (1 VA and 4 non-VA settings using 4 different EHRs) to understand existing optimal strategies to improve efficiency and situational awareness related to EHR inbox use. Themes from survey data were cross-validated with interview findings.
Results
We analyzed responses from 2104 PCPs who completed the free-text inbox question (of 5001 PCPs who responded to survey) and used an inductive approach to identify five themes: (1) Inbox notification content should be actionable for patient care and relevant to recipient clinician, (2) Inboxes should reduce risk of losing messages, (3) Inbox functionality should be optimized to improve efficiency of processing notifications, (4) Team support should be leveraged to help with EHR inbox notification burden, (5) Sufficient time should be provided to all clinicians to process EHR inbox notifications. We subsequently interviewed 15 VA and non-VA clinicians and identified 11 unique strategies, each corresponding directly with one of these five themes.
Conclusion
Feedback from practicing end-user clinicians provides robust evidence to improve content and design of the EHR inbox and related clinical workflows and organizational policies. Several strategies we identified could improve clinicians’ EHR efficiency and satisfaction as well as empower them to work with their local administrators, health IT personnel, and EHR developers to improve these systems.
KEY WORDS: electronic health records, health information technology, medical informatics, burnout, situational awareness, efficiency
INTRODUCTION
The prevalence of physician burnout is increasing.1–3 Burnout affects job satisfaction and productivity,4,5 and can negatively impact patient satisfaction and clinical outcomes.6,7 While several factors have been identified as causes for burnout, excessive workload related to electronic health records (EHRs) is a frequently cited contributor.8–10 Among all EHR-related activities, the burden of managing EHR inbox messages has emerged as a specific source of physician dissatisfaction,11,12 particularly in primary care where physicians spend approximately one hour each day managing inbox-delivered notifications.11,13 EHR inboxes are common in modern EHRs and act similarly to email systems. They are the most frequent vehicles of communicating test results, referral-related information, refill requests, and messages from other clinicians, staff, and patients.13
Poor EHR inbox design and inappropriate message content make processing messages more onerous and inefficient.14,15 An excessive number of steps needed to process messages creates inefficiencies that add to physician workload but provide little benefit to care. Additionally, EHRs make creation of new message types easy. When done thoughtfully, this provides one of the most useful ways to communicate important patient information to physicians. However, unnecessary and excessive notification, such as “For-Your-Information-Only” messages or automated messages that alert physicians of every scheduled referral, can quickly overload physicians and provide little extra benefit to patient care.13,16 Improving inbox management requires an understanding of EHR inbox designs and the message content they relay.
Excessive inbox messages can also lead to loss of situational awareness (SA),17 an aviation concept which has been recently applied to medicine to better understand decision-making in dynamic clinical settings, including decision-making related to EHR-based notifications.18 SA involves four levels: (1) perception of elements in the environment, (2) comprehension of their meaning, (3) projection of their status in the near future, and (4) awareness of best path to follow.19,20,18 EHR information overload, inadequate inbox design, and poor clinician message management processes could lead to a paradoxical reduction in SA due to difficulty in focusing on relevant messages among those that do not impact care (SA level 1), understanding the meaning of messages (SA level 2), developing appropriate expectations based on message information (SA level 3), and taking appropriate action in response (SA level 4). Higher SA levels cannot be reached until lower levels are satisfied. Thus, work to address the EHR inbox and its management must address both efficiency and SA.
Few studies have sought to understand and address inefficiencies and safety implications of EHR inbox designs and workflow management. Our study objective was to identify clinician-recommended strategies to enhance EHR inbox design and workflow. This knowledge can be useful to inform future initiatives to improve efficiency and SA related to EHR inbox management and thus improve patient safety and reduce burnout.
METHODS
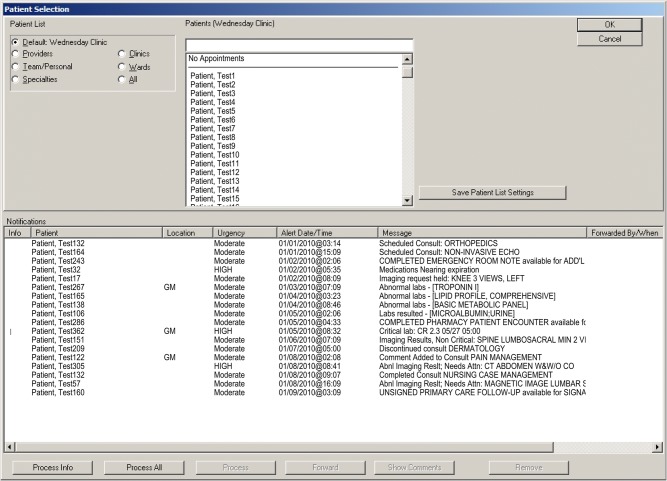
We performed a mixed-methods study using explanatory sequential design.21,22 Using results from a 2013 nationwide Department of Veterans Affairs (VA) survey of primary care practitioners (PCPs; including physicians, physician assistants, and nurse practitioners), we first performed a quantitative analysis of PCP-recommended improvements to EHR inbox design.23 The VA’s EHR inbox functions similarly to those of other commercial EHRs, providing an initial interface where notifications are listed, allowing certain limited actions within the inbox, and linking physicians to the relevant portion of the full medical record (Fig. 1). We then performed separate interviews with practitioners at five health systems (1 VA and 4 private) to identify strategies related to improving SA and efficiency of inbox management. We compared results from the two methods to understand strategies that could potentially address issues with current inbox management SA and efficiency. We also mapped findings to a previously developed socio-technical model for health information technology (HIT) to account for contextual factors in complex adaptive systems.24 Because this model describes both social and technical dimensions related to hardware/software, clinical content, user interface, people, workflow/communication, organizational policies/culture, external regulations, and measurement/monitoring, it has potential to guide where resources are needed to implement recommendations. The study was approved by the local IRB.
Figure 1.
Screenshot of VistA/CPRS inbox used at the Department of Veteran Affairs EHR.
Primary Care Survey
We performed a secondary analysis of data previously collected during a survey of all 5001 VA PCPs (51% response rate).23 Survey questions focused on inbox design and PCP’s inbox message management strategies. Details about survey development and administration are described elsewhere.23 We analyzed free-text responses to the question “If you could change one thing about [your inbox], what would that be?” which was answered by 2104 participants. To provide an assessment of inter-rater reliability, two coders (DRM and TS) with expertise in clinical medicine, informatics, and human factors engineering used Atlas.ti 7.5.16 (Atlas.ti GmBH, Berlin, Germany) to initially code 20% of all responses. Coding was performed independently and identified and categorized clinician-recommended changes. Both coders met weekly to discuss and reconcile codes into a single codebook, which was then used for subsequent coding. Responses could receive multiple codes if more than one recommendation was identified. Cohen’s kappa was then calculated to evaluate inter-rater agreement across this subset. Differences were subsequently reconciled and the remaining responses were coded by a single reviewer (TS). Once all responses were coded, reviewers met to combine individual codes into overarching themes.
Expert Clinician Interviews
We conducted interviews to understand current inbox management techniques across several sites and EHRs as well as to discover alternative inbox design-related solutions and connect these findings to survey results. A team member (DRM) conducted interviews with primary and specialty care clinicians (physicians and physician assistants) at five large multispecialty clinics, including 1 VA and 4 non-VA sites, between April and September 2016. Interviews were conducted as part of a larger study to understand test results management workflows and included questions regarding strategies for improving inbox management efficiency and SA. Medical directors at each site identified practicing clinicians they considered proficient in EHR inbox management to serve as experts in this study. The study team contacted each clinician via email inviting participation. All recommended experts agreed to participate.
After obtaining informed consent, clinicians were asked “what EHR inbox features or inbox-related processes do you use to improve message processing efficiency or prevent from missing important information?” Later in the interview, experts were provided with the previously identified responses from other clinicians to generate richer context. Responses were audio recorded and subsequently transcribed and coded by two reviewers (TS and DRM). Statements about specific workflows or EHR features to improve efficiency or SA were individually identified. Reviewers discussed and developed a list of unique codes by combining similar responses, and each code was categorized as impacting either efficiency or its highest impact among the four SA levels. In order to inform interventions and to better understand resources needed to implement recommendations, the list was then mapped to the 8-dimensional socio-technical model (Table 1).24 A multidisciplinary team with expertise in medicine, informatics, human factors, sociology, and information technology then reviewed the list and evaluated by consensus each item based on its expected impact on efficiency and SA. Identified themes were compared with those from the survey.
Table 1.
Eight Dimensions of the Socio-Technical Model for Health Information Technology
| Dimension | Description |
|---|---|
| Hardware and software | The computing infrastructure used to power, support, and operate clinical applications and devices |
| Clinical content | The text, numeric data, and images that constitute the “language” of clinical applications |
| Human-computer interface | All aspects of technology that users can see, touch, or hear as they interact with it |
| People | All individuals who interact with technology, including developers, users, IT personnel, and informaticians |
| Workflow and communication | Processes used to provide patient care |
| Organizational policies and workflows | Policies, procedures, work-environment, and culture |
| External rules and regulation | Federal or state rules that facilitate or constrain organizational activities |
| Measurement and monitoring | Processes to evaluate both intended and unintended consequences of health informational technology implementation and use |
RESULTS
Of 5001 PCPs, 2104 provided free-text information on recommended changes to the VA’s EHR inbox system. Two reviewers identified 37 unique codes based on the responses. Similar codes were iteratively discussed by both reviewers and categorized into 5 major themes. Unique recommendations are listed by theme in Table 4. We calculated a Cohen’s kappa of 0.77 for coding of themes (Table 2), indicating good reliability.
Table 4.
Clinician-Recommended Changes to Inbox Design and Workflows
| Theme: Inbox content should be actionable for patient care and relevant to recipient clinician | |
|
• Remove duplicate and redundant messages • Remove messages not actually intended for the clinician • Remove for-your-information-only messages from other clinicians that do not require any action by the recipient and do not impact patient care • Remove messages for normal test results • Add features to enable sorting, filtering, and flagging of messages to enable focusing on relevant and high-priority messages • Ensure that all key test results generate messages (e.g., electrocardiograms or echocardiograms) | |
| Theme: Inboxes should reduce risk of losing of messages | |
|
• To prevent inadvertent loss of information, messages should only be intentionally removed such as with a “Done” or “Delete” button. • Allow messages to be undeleted via an Undo button, or a repository where previously processed messages can be viewed, searched, and potentially returned to the main inbox • Add a “reminder” or “To-Do” feature to the inbox that can be used to store messages or notes as a reference for future follow-up actions | |
| Theme: Inbox functionality should be optimized to improve efficiency of processing notifications | |
|
• Reduce the number of mouse clicks necessary to process messages • Add features to automate generation of test result letters • Simplify placing of test and refill orders from the message window • Streamline methods of accessing digital films of imaging results • Allow contextual information for messages to be visible from the inbox, such as prior lab, current medication and problem lists, and patient contact information | |
| Theme: Team support should be leveraged to help with EHR inbox notification burden | |
|
• Support staff should triage messages prior to transmitting to clinician and act on certain messages without the need of the clinician • EHR inboxes should allow forwarding of messages to team members and allow the addition of comments to provide instruction or context • Inboxes should incorporate a secure messaging system similar to email to communicate with other physicians | |
| Theme: Sufficient time should be provided to all clinicians to process EHR inbox notifications | |
|
• Provide sufficient administrative time dedicated to processing messages • Allow remote access to the EHR to allow message processing even when not located at the clinic |
Table 2.
Major Themes for Inbox Design Change Recommendations from Survey Responses
| Grounded (n = 2104 responses) | ||
|---|---|---|
| Theme | No. | (%) |
| Inbox content should be actionable for patient care and relevant to recipient clinician | 1450 | (68.9) |
| Inboxes should reduce risk of losing of messages | 318 | (15.1) |
| Inbox functionality should be optimized to improve efficiency of processing notifications | 266 | (12.6) |
| Team support should be leveraged to help with EHR inbox notification burden | 143 | (6.8) |
| Sufficient time should be provided to all clinicians to process EHR inbox notifications | 89 | (4.2) |
For interviews, we recruited from five sites using four different EHRs (Epic 2012 and 2014, GE Centricity, AllScripts, and VA CPRS). Medical directors identified fifteen clinicians who agreed to participate, including nine primary care practitioners and six specialists (Table 3). We received 17 responses about strategies used to improve efficiency of SA of inbox management. Three strategies were unrelated to inbox efficiency or SA and were excluded. After consolidating similar strategies, 11 unique strategies remained and are described below (Table 5).
Table 3.
Interview Site and Participant Characteristics
| Site | Participants | EHR installed | Primary care | Specialty care | Male | Female |
|---|---|---|---|---|---|---|
| A | 5 | Epic 2012 | 1 | 4 | 1 | 4 |
| B | 5 | Epic 2014 | 5 | 0 | 3 | 2 |
| C | 1 | GE Centricity | 1 | 0 | 0 | 1 |
| D | 3 | Allscripts | 1 | 2 | 3 | 0 |
| E | 1 | VistA CPRS | 1 | 0 | 0 | 1 |
| Total | 15 | 9 | 6 | 7 | 8 |
Table 5.
Clinician-Recommended Strategies to Improve Situational Awareness and Efficiency Grouped by Survey Theme
| Practice | Example | Socio-technical dimension | Efficiency and SA impact* |
|---|---|---|---|
| Inbox content should be actionable for patient care and relevant to recipient clinician | |||
| Leadership and IT reviews the types of messages sent, and only transmit those likely to influence patient care. | • Remove automated for-your-information-only messages that do not impact care, like “height and weight collected.” | Content | Efficiency and SA level 1 |
| Inboxes should reduce risk of losing of messages | |||
| When future action is needed, use reminder features to de-clutter inbox. | • Set future reminder to follow-up on repeat chest imaging results. | Hardware and software | SA levels 1–3 |
| Inbox functionality should be optimized to improve efficiency of processing notifications | |||
| Use macros to increase the efficiency of repetitive actions. | • Macro to automatically route appropriate messages to nursing staff. | Content | Efficiency |
| Use templated text (or voice recognition software) to quickly populate frequently used messages. | • Templated text to describe abnormal cholesterol results and need to improve exercise and diet. | Content | Efficiency |
| Customize and use order preference lists. | • Preference list item for metformin 500 mg with “BID,” “180 tablets,” and “3 refills” preset. | Content | Efficiency |
| Set up your quick routing list for recipients who commonly receive messages. | • Button to automatically add the clinic’s nursing pool to the “To:” field of a message. | Content | Efficiency |
| Actively sign patients up for a portal to facilitate test result release. | • Process to release non-urgent test results to portal is more efficient than generating letters or phone calls. | Workflow | Efficiency |
| When unable to process message immediately, add message comments as reminders of message content. | • Adding “Waiting for forms” comment to a telephone message. | User interface | SA level 1 |
| Develop inbox views that reveal information that is commonly required for decision-making, but prevent the need to open the patient’s full chart. | • EHR features displaying the current medication list when processing refill requests. | Hardware/software and user interface | Efficiency and SA levels 1–3 |
| Team support should be leveraged to help with EHR inbox notification burden | |||
| Allow staff to pre-load orders when patients call requesting refills, test orders, or referrals. | • Allow staff to pre-load referral order when patient calls requesting referral. Physician can approve or cancel referral quicker than entering de novo. | Workflow | Efficiency |
| Sufficient time should be provided to all clinicians to process EHR inbox notifications | |||
| Allow sufficient and distraction-free time for non-face-to-face activities. | • Scheduling designated distraction-free inbox management time. | Organizational policies and workflows | Efficiency and SA levels 1–4 |
*Situational awareness (SA) level 1 = perception of information in the environment; SA level 2 = comprehension of their meaning; SA level 3 = projection of their status in the near future; SA level 4 = awareness of the best path to follow
Recommended Changes and Associated Strategy by Theme
Inbox Content Should Be Actionable for Patient Care and Relevant to Recipient Clinician (n = 1450; 68.9%)
PCPs most commonly (68.9% of responses) recommended that inboxes receive only messages with content relevant to the care they provide to their patients. Excessive message content reduced processing efficiency from information overload and reduced SA level 1 due to the inability to distinguish urgent from routine messages. Recommendations included removal of messages containing duplicate or redundant information (e.g., separate messages for abnormal blood panels and a specific result within the same panel); messages not actually intended for the PCP (e.g., carbon copied on communication between specialists and their support staff and in test results of hospitalized patients intended for inpatient-care team); and “for-your-information-only” messages from other clinicians and staff that required review and signature but neither required action by the recipient nor impacted patient care. While most respondents recommended eliminating irrelevant messages, 257 (12.2%) recommend adding features to enable better sorting, filtering, and flagging of these messages to help focus on messages of higher relevance and priority.
To address inbox content-related issues, interviewed clinicians at one site reported a close working relationship with clinic administrators and information technology (IT). This allowed them to initiate discussions with administrators and IT representatives about the lack of clinical benefit of certain messages and disable those where no unintended consequences were expected. For example, one participant cited an automated “height and weight collected” message that was previously sent to clinicians each time their staff collected heights and weights. During discussion with administrators and IT, this was identified to have no meaningful impact on patient care and was disabled.
Inboxes Should Reduce Risk of Losing of Messages (n = 318; 15.1%)
Fifteen percent of survey respondents recommended changes to prevent inadvertent loss of important information from the inbox (SA level 1). Survey participants reported that inboxes immediately removed messages once clicked on, regardless of whether processing was complete. Others indicated that messages were removed after 30 days whether reviewed or not. Several reported that this lack of control over message removal led them to fear losing important and actionable information about their patients. Recommended changes include modification of inbox functionality so that messages could only be intentionally removed, such as by clicking on a “delete” or “done” button. Alternatively, respondents indicated that functionality to look back at recently removed messages would provide a safety net. Methods to do so included implementation of an “undo” button or a repository where previously processed messages could be viewed and returned to the main inbox, similar to email “trash” folders. Additionally, 84 respondents (4%) recommend adding a “reminder” or “to do” feature to the inbox to allow storage of messages or notes as references for future follow-up actions (supporting SA level 3).
Interviewed clinicians reported frequent use of self-reminder messages in other EHRs that could be sent to themselves at a pre-specified date in the future. The “remind me” feature accepted input of a send date, free-text message, and an optional patient record number (or pre-populated from the currently open chart). For example, a reminder could prompt a clinician to investigate in two weeks whether a test had been completed by the patient. Participants indicated that this allowed temporary removal of important but non-urgent messages that cluttered their inboxes.
Inbox Functionality Should Be Optimized to Improve Efficiency of Processing Notifications (n = 266; 12.6%)
PCPs reported excessive steps were needed to process messages and recommended features to streamline inbox management. While most responses requested non-specific improvements to inbox usability, 94 (4.5%) responses specifically recommended reducing the number of mouse clicks necessary to process messages. Examples included addition of features to automate generation of letters that notify patients of test results and simplified methods to order reflex tests and medication refills from the inbox. Similarly, 11 respondents recommended allowing contextual information for messages to be visible from the inbox, including prior lab results to enable trending of new results, current medication and problem lists, and patient contact information.
Seven strategies identified during interviews fit into this theme. Of these, four involved using EHR features to improve message processing efficiency by automating frequently performed actions with macros (to automate documentation and routing of messages), templated text (to automate commonly used documentation), preference lists (to quickly place orders), and routing lists (to quickly choose message recipients). Another strategy involved adding comments to previously reviewed messages to enable context without the need to reopen the message, such as “waiting for fax.” Clinicians also reported that actively signing up patients to the patient portal improved efficiency because releasing results to the portal was more efficient than generating letters. The final strategy involved reliance on inbox features that provided key contextual information needed for decision-making, facilitating SA levels 1–3. For example, clinicians often accessed screens within the inbox that displayed current medications and allergies for processing refill requests and prior labs of the same type when processing test results. This allowed clinicians to process messages more efficiently by eliminating the additional steps needed to open and navigate to the same information in patients’ records. However, not all EHR inboxes offered such capabilities.
Team Support Should Be Leveraged to Help with EHR Inbox Notification Burden (n = 143; 6.8%)
Surveyed PCPs reported that message management processes should include team members, and inbox designs should facilitate team-based care coordination. Ninety-one (4.3%) respondents indicated that support staff should triage messages prior to sending them to clinicians and act on messages within their scope of practice (e.g., directly scheduling patients). Additionally, 30 respondents indicated that the inbox should facilitate both inter- and intra-team communication, with some suggesting the inbox integrate a secure messaging system that allowed clinicians and staff to communicate with each other.
To streamline inbox message management processes, interviewed clinicians also recommended having non-physician staff serve as initial reviewers for all messages. Clinicians reported that inbox message requests for refills, referrals, or pre-visit labs could be reviewed by non-physician staff who could then enter but not sign relevant orders. Clinicians’ inbox management time can thus be reduced if they mostly approve, modify, or decline certain orders, rather than routinely place these orders themselves.
Sufficient Time Should Be Provided to All Clinicians to Process EHR Inbox Notifications (n = 89; 4.2%)
Finally, PCPs requested sufficient time and resources to address inbox messages, including “protected” time for inbox message processing and remote access to their inboxes. PCPs reported the current amount of non-face-to-face time to process messages was insufficient to allow thoughtful consideration of inbox messages, and that clinic/organizational policies must ensure that protected non-face-to-face time corresponds with the time necessary to process messages.
Interviewed clinicians reported using various methods to create or make best use of non-face-to-face time to process messages. One participant closed the office door and sent all phone calls to voicemail to allow processing of messages in an interruption-free environment. Another checked messages throughout the day to prevent the compulsion to rush through messages after clinic. Such strategies facilitate efficiency by reducing interruptions and enhancing all SA levels by allowing clinicians perceive and comprehend message content and make projections in an unhurried manner, allowing them to take the most appropriate action.
DISCUSSION
Using a mixed-methods approach, we identified priorities to address emerging concerns related to safety and burnout from EHR inbox notification workload. High-priority themes included adjusting message content to make it more actionable for patient care and relevant to recipient clinician, designing EHR inboxes to reduce risk of losing message information, optimizing inbox functionality to improve processing efficiency, increasing integration of non-clinician staff in message processing workflows, and providing sufficient time and resources for clinicians to process messages. In subsequent interviews, clinicians validated the importance of these themes by describing current strategies to improve efficiency and SA related to each one.
Of the strategies identified during interviews, most involved efficiency. This is not unexpected given clinicians’ focus on reducing their workloads. Two impacted SA level 1 (perception of information): making key clinical information more salient by eliminating clutter unrelated to patient care and allowing a focus on more urgent messages and adding comments to messages to allow them to discern urgent from non-urgent messages on subsequent review. Three strategies, providing sufficient and uninterrupted time and resources for message processing, using reminders to ensure future action, and providing contextual information to improve interpretation of inbox messages, could potentially enable higher SA levels and improve safety. For example, clinicians who have sufficient time to thoughtfully consider clinical information, comprehend its meaning, project future status, and take appropriate actions in response (SA levels 1–4) will achieve better outcomes for their patients.
The overlap in themes between inbox recommendations from surveyed PCPs and current strategies of interviewed clinicians confirms the importance of these themes to inbox-related efficiency and situational awareness. For example, surveyed PCPs requested quick access to specific patient-related information to streamline processing efficiency, while interviewed clinicians indicated use of similar EHR features that make such information readily available within the inbox to improve efficiency and SA. This also suggests significant variations in implementation, inbox designs, and message processing workflows at different sites leading to variable efficiency and SA. Such variations are quite likely given the proprietary nature of most modern EHRs and the lack of systematic sharing of inbox management best practices across organizations and between clinicians. Additional research in this area should inform the understanding of efficiency and SA outcomes of different inbox designs and clinician workflows, informing guidance to EHR vendors to improve their inbox designs. This evidence should also lead health care organizations to improve clinical workflows and help develop better vendor-organization partnerships to ensure that clinicians are properly trained to use the EHR inbox (Table 4).
The themes identified were associated with six of the eight socio-technical dimensions24 (Table 5), ranging from changes in software features, user interface changes, and inbox workflows. This suggests that neither vendors that design EHRs nor health systems that implement and use them can fully optimize efficiency and SA independently. They both must work together and share the responsibility to achieve these goals.25 For example, the most common change recommended by PCPs was to ensure that message content was relevant to patient care provided by the message recipient. To reduce information-only messages commonly cited as contributing to unnecessary inbox workload, health systems can create clinician-led committees to determine which automated inbox messages are truly pertinent to patient care and establish relationships with information technology departments to remove those that are not. Similarly, organizations must provide training and guidance to users to limit their sending of for-your-information-only messages that clutter inboxes. Conversely, PCP recommendations for addition of new features to improve processing efficiency, such as automating recurrently performed actions (e.g., generating lab result letters for mailing or patient portal release), suggest the need for EHR vendors to design, develop, and implement such features.
There are few current efforts to improve inbox content and design. The American Medical Association’s STEPS Forward program26,27 emphasizes education and tools for practice restructuring to improve efficiency of inbox management. However, additional efforts in this area are needed. Evening and weekend time on EHRs, particularly in primary care where brunt of information load is higher,11 suggests that current inbox-related workloads are not sustainable in the long term. We identified several strategies to improve clinicians’ EHR efficiency and satisfaction and empower them to work with their local administrators, health IT personnel, and EHR developers to improve these systems. All of these recommendations from practicing frontline clinicians should help address safety and efficiency problems related to EHR inbox notifications.
Several limitations merit mention. First, while the survey was national, it was only performed in the VA system, and even though the interviews were performed at four additional non-VA sites using 4 (by 3 different EHR vendors) commercial EHRs, findings may not be generalizable to all sites and all EHRs. However, the EHRs used at these sites represent several commonly used EHRs in the USA. Second, secondary data analysis of survey did not allow an opportunity to clarify responses, suggesting some context for responses might be missed. However, to minimize bias, coders focused only on stated facts and did not attempt to code implied meanings. Third, because the results are based on clinician-reported information and may not represent actual impacts on efficiency and SA, future research should include understanding and evaluating actual workflows, interface designs, and clinician knowledge and use of EHR inbox features. Finally, while survey data was collected in 2012, there have been no subsequent significant changes to VA EHR inbox design and functionality to invalidate study findings.
CONCLUSION
Our study highlights several strategies to improve clinicians’ EHR inbox-related efficiency and provides data to empower clinicians to work with their local administrators, health IT personnel, and EHR developers to address the emerging burden of EHR inbox management. Feedback from frontline clinician end-users should be gathered routinely to inform improvements in EHR inbox content, design, and related organizational workflows and policies. To improve safety and reduce clinician burnout, next steps should include development of standards for inbox designs and clinician workflows as well as systematic sharing of best practices to improve inbox use across organizations and clinicians.
Funding
This project is funded by the Agency for Healthcare Research and Quality (K08-HS022901 and R01HS022087), and partially funded by the Houston VA HSR&D Center for Innovations in Quality, Effectiveness and Safety (CIN 13–413). The original survey was supported by the Department of Veterans Affairs National Center for Patient Safety. Dr. Singh is additionally supported by the VA Health Services Research and Development Service (CRE 12-033; Presidential Early Career Award for Scientists and Engineers USA 14-274). Dr. Giardina is additionally supported by the Agency for Healthcare Research and Quality (K01HS025474). These funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Compliance with Ethical Standards
Conflict of Interest
The authors have no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in Burnout and Satisfaction With Work-Life Balance in Physicians and the General US Working Population Between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–1613. doi: 10.1016/j.mayocp.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 2.Wright AA, Katz IT. Beyond Burnout - Redesigning Care to Restore Meaning and Sanity for Physicians. N Engl J Med. 2018;378(4):309–311. doi: 10.1056/NEJMp1716845. [DOI] [PubMed] [Google Scholar]
- 3.Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among us physicians relative to the general us population. Arch Intern Med. 2012;172(18):1377–1385. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 4.Anagnostopoulos F, Liolios E, Persefonis G, Slater J, Kafetsios K, Niakas D. Physician burnout and patient satisfaction with consultation in primary health care settings: evidence of relationships from a one-with-many design. J Clin Psychol Med Settings. 2012;19(4):401–410. doi: 10.1007/s10880-011-9278-8. [DOI] [PubMed] [Google Scholar]
- 5.Humphries N, Morgan K, Conry MC, McGowan Y, Montgomery A, McGee H. Quality of care and health professional burnout: narrative literature review. Int J Health Care Qual Assur. 2014;27(4):293–307. doi: 10.1108/IJHCQA-08-2012-0087. [DOI] [PubMed] [Google Scholar]
- 6.Halbesleben JRB, Rathert C. Linking physician burnout and patient outcomes: exploring the dyadic relationship between physicians and patients. Health Care Manage Rev. 2008;33(1):29–39. doi: 10.1097/01.HMR.0000304493.87898.72. [DOI] [PubMed] [Google Scholar]
- 7.Panagioti Maria, Geraghty Keith, Johnson Judith, Zhou Anli, Panagopoulou Efharis, Chew-Graham Carolyn, Peters David, Hodkinson Alexander, Riley Ruth, Esmail Aneez. Association Between Physician Burnout and Patient Safety, Professionalism, and Patient Satisfaction. JAMA Internal Medicine. 2018;178(10):1317. doi: 10.1001/jamainternmed.2018.3713. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 8.Guo U, Chen L, Mehta PH. Electronic health record innovations: Helping physicians - One less click at a time. HIM J. 2017;46(3):140–144. doi: 10.1177/1833358316689481. [DOI] [PubMed] [Google Scholar]
- 9.Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship Between Clerical Burden and Characteristics of the Electronic Environment With Physician Burnout and Professional Satisfaction. Mayo Clin Proc. 2016;91(7):836–848. doi: 10.1016/j.mayocp.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 10.Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: Primary Care Physician Workload Assessment Using EHR Event Log Data and Time-Motion Observations. Ann Fam Med. 2017;15(5):419–426. doi: 10.1370/afm.2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murphy DR, Meyer AN, Russo E, Sittig DF, Wei L, Singh H. The Burden of Inbox Notifications in Commercial Electronic Health Records. JAMA Intern Med. 2016;176(4):559–560. doi: 10.1001/jamainternmed.2016.0209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gregory ME, Russo E, Singh H. Electronic Health Record Alert-Related Workload as a Predictor of Burnout in Primary Care Providers. Appl Clin Inform. 2017;8(3):686–697. doi: 10.4338/ACI-2017-01-RA-0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murphy DR, Reis B, Sittig DF, Singh H. Notifications received by primary care practitioners in electronic health records: a taxonomy and time analysis. Am J Med. 2012;125(2):209.e1–7. doi: 10.1016/j.amjmed.2011.07.029. [DOI] [PubMed] [Google Scholar]
- 14.Hysong SJ, Sawhney MK, Wilson L, et al. Provider management strategies of abnormal test result alerts: a cognitive task analysis. J Am Med Inform Assoc JAMIA. 2010;17(1):71–77. doi: 10.1197/jamia.M3200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hysong SJ, Sawhney MK, Wilson LA, et al. Understanding the Management of Electronic Test Result Notifications in the Outpatient Setting. BMC Med Inform Decis Mak. 2011;11(1):22. doi: 10.1186/1472-6947-11-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murphy DR, Reis B, Kadiyala H, et al. Electronic Health Record-Based Messages to Primary Care Providers: Valuable Information or Just Noise? Arch Intern Med. 2012;172(3):283. doi: 10.1001/archinternmed.2011.740. [DOI] [PubMed] [Google Scholar]
- 17.Cutrona SL, Fouayzi H, Burns L, et al. Primary Care Providers’ Opening of Time-Sensitive Alerts Sent to Commercial Electronic Health Record InBaskets. J Gen Intern Med. 2017;32(11):1210–1219. doi: 10.1007/s11606-017-4146-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singh H, Giardina TD, Petersen LA, et al. Exploring situational awareness in diagnostic errors in primary care. BMJ Qual Saf. 2012;21(1):30–38. doi: 10.1136/bmjqs-2011-000310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Endsley MR. Toward a theory of situation awareness in dynamic systems. Hum Factors J Hum Factors Ergon Soc. 1995;37(1):32–64. doi: 10.1518/001872095779049543. [DOI] [Google Scholar]
- 20.Singh H, Petersen LA, Thomas EJ. Understanding diagnostic errors in medicine: a lesson from aviation. Qual Saf Health Care. 2006;15(3):159–164. doi: 10.1136/qshc.2005.016444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang W, Creswell J. The use of “mixing” procedure of mixed methods in health services research. Med Care. 2013;51(8):e51–57. doi: 10.1097/MLR.0b013e31824642fd. [DOI] [PubMed] [Google Scholar]
- 22.Tariq Shema, Woodman Jenny. Using mixed methods in health research. JRSM Short Reports. 2013;4(6):204253331347919. doi: 10.1177/2042533313479197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Singh H, Spitzmueller C, Petersen NJ, et al. Primary care practitioners’ views on test result management in EHR-enabled health systems: a national survey. J Am Med Inform Assoc. 2013;20(4):727–735. doi: 10.1136/amiajnl-2012-001267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sittig DF, Singh H. A new sociotechnical model for studying health information technology in complex adaptive healthcare systems. Qual Saf Health Care. 2010;19(s3):i68–74. doi: 10.1136/qshc.2010.042085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sittig DF, Belmont E, Singh H. Improving the safety of health information technology requires shared responsibility: It is time we all step up. Healthc Amst Neth. 2018;6(1):7–12. doi: 10.1016/j.hjdsi.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 26.EHR In-Basket Restructuring for Improved Efficiency - STEPS Forward. STEPSforward.org. https://www.stepsforward.org/modules/ehr-inbasket-management. Accessed July 9, 2018.
- 27.Henry TA. Taming your unruly in-basket is possible with a little teamwork. AMA Wire. https://wire.ama-assn.org/practice-management/taming-your-unruly-basket-possible-little-teamwork. Published January 17, 2018. Accessed July 9, 2018.