Abstract
Adolescents’ media use represents a normative need for information, communication, recreation and functionality, yet problematic Internet use has increased. Given the arguably alarming prevalence rates worldwide and the increasingly problematic use of gaming and social media, the need for an integration of prevention efforts appears to be timely. The aim of this systematic literature review is (i) to identify school-based prevention programmes or protocols for Internet Addiction targeting adolescents within the school context and to examine the programmes’ effectiveness, and (ii) to highlight strengths, limitations, and best practices to inform the design of new initiatives, by capitalizing on these studies’ recommendations. The findings of the reviewed studies to date presented mixed outcomes and are in need of further empirical evidence. The current review identified the following needs to be addressed in future designs to: (i) define the clinical status of Internet Addiction (IA) more precisely, (ii) use more current psychometrically robust assessment tools for the measurement of effectiveness (based on the most recent empirical developments), (iii) reconsider the main outcome of Internet time reduction as it appears to be problematic, (iv) build methodologically sound evidence-based prevention programmes, (v) focus on skill enhancement and the use of protective and harm-reducing factors, and (vi) include IA as one of the risk behaviours in multi-risk behaviour interventions. These appear to be crucial factors in addressing future research designs and the formulation of new prevention initiatives. Validated findings could then inform promising strategies for IA and gaming prevention in public policy and edu-cation.
Keywords: Internet addiction, Social media, Gaming, Addiction prevention, Schools, Adolescents
1. INTRODUCTION
Adolescents’ media use represents a normative need for information, communication, recreation and functionality [1, 2]. In spite of the many beneficial aspects of Internet use [3], problematic Internet use has increased [4, 5], and has been associated with less physical activity and diverse negative neurophysiological and psychosocial consequences in adolescents [6, 7]. Heavy use can potentially lead to addiction in vulnerable adolescents [8], and is a growing public health concern with variability in prevalence rates (from 0.8% in Italy to 26.7% in Hong Kong) [4].
Internet addiction (IA) is a complex disorder in terms of its conceptualization, clinical manifestation, and measurement. For the purposes of the present review, IA is operationally defined as a consistent and potentially pathological behavioural pattern, characterized by salience (preoccupation with online activities), tolerance (seeking increasing time to achieve satisfaction), withdrawal symptoms (when unable to use the Internet), using online activities to modify mood, conflict (within oneself, in relationships, or with academic/occupational activities because of online engagement) and relapse (unsuccessful attempts to control the behaviour) [9]. Specific online activities, such as gaming and using social networking sites (SNSs), are particularly relevant to adolescents and constitute a popular form of entertainment [10-12]. However, both are increasingly recognized as having addictive qualities [9, 13], with many common but also some idiosyncratic characteristics [11, 12, 14, 15]. IA and gaming addiction have been well evidenced for their negative impacts, and social media addiction is increasingly associated with negative consequences on academic achievement [16] and related problems (i.e., procrastination, distraction, poor time management; [17], less physical activity, and greater unhappiness [6]. Given the academic and psychosocial burden, both for gaming and social media use, any recognition of a dysfunctional Internet use pattern needs addressing at the crucial developmental stage of adolescence [18, 19].
1.1. Adolescence and IA
Adolescence, operationally defined as the developmental period between the ages of 10 to 18 years [20], represents a vulnerable period for engagement in risky behaviours (i.e., alcohol drinking, drug taking and engaging in violence) [21], and the development of addictions [11, 22]. It is also a critical period of value formation, personality, and rapid psychological development, characterized by the adoption of various lifestyle, health behaviour and educational choices, which hold a defining role in adulthood [18, 23]. Need satisfaction (e.g., peer communication, self-expression, desire for recognition) [24-26] and peer group pressures [27] may offer a partial explanation for adolescents’ high online media use frequency and high engagement in potentially addictive online behaviours [19, 28]. Considerable research has focused on treatment for affected individuals [29-35]. However, researchers in this field are increasingly discussing prevention and health promotion as a method of positively impacting youth engagement with the online environment [5, 36, 37]. According to the American Psychological Association (APA) guidelines for prevention [38], the prevention field has documented its effectiveness and is progressively acknowledged as a crucial component of practice, research and training, bridging research and public policy. Evidence based prevention practices are therefore encouraged to be viewed as complementary to treatment and crisis intervention with numerous benefits (i.e. reduction of illness and problem behaviours, enhancement of human functioning and reduced health care costs) for policy making, health and well being promotion.
1.2. Prevention, Health Promotion, and Addiction
Prevention is a broad term encompassing a wide array of interventions aimed at reducing the incidence of disease and disability, or slowing the progression and exacerbation of a condition, with health promotion serving as a component of prevention [39]. Prevention approaches mostly encountered in the literature have been categorized according to two definitional frameworks [40, 41]. Caplan’s [40] framework comprises: primary (prevent onset of a disease), secondary (reduce the incidence of a disease) and tertiary (reduce the impact of a persistent health issue) prevention, emphasizing a public health perspective. Gordon’s [41] framework comprises three levels: universal (targeting a wide population), selective (targeting subpopulations) and indicated prevention (targeting at risk or vulnerable individuals) [42]. Health promotion refers to the combined educational and environmental resources driving health [43]. Prevention programmes to address risky adolescent lifestyles have historically been aimed toward non-users (primary prevention), screening for potential problems (secondary prevention), and treatment (tertiary prevention) for adolescents who exhibit problematic behaviours, such as substance abuse or problem gambling [44]. Recent findings suggest more evidence-based, multi-system approaches, involving parents, schools, the community and other relevant stakeholders in guiding prevention efforts [45].
1.3. Need for Evidence-based Health Promoting Prevention Programmes for IA
There is therefore, current scientific consensus for the need to develop well-controlled, methodologically robust interventions for IAs that are grounded in empirical evidence and theory [43, 46]. Evidence-based policy provision needs to be informed by reliable research findings and appropriate dissemination by the media [47], proper evaluation of school-based intervention programmes, and more randomised controlled trials (RCTs) with embedded evaluation standards to inform evidence-based recommendations [48-50]. These initiatives should target specific populations (i.e., adolescents) and specific online activities, such as problematic social media use [51] or gaming [52], should reflect the current state of knowledge, be theory-driven, and have the aim of enhancing skills and competencies associated with risk and protective factors [53, 54]. This could then justify funding and development of public health policy that could lead to a decrease in the incidence and prevalence of IA [6, 55]. Yeun and Han [56], who conducted a meta-analytic review on psychosocial treatment interventions that included prevention initiatives, found large effects for reducing IA and improving self-control and self-esteem, especially where parent-involved counselling, self-control training programmes or where a specific (theory-based) form of therapy was applied.
Detailed protocols to guide the development of theory-driven health promotion interventions are now available. One influential approach, “Intervention Mapping” [43] divides intervention development into six processes: (i) needs assessment based on the PRECEDE-PROCEED Model (PRECEDE: health, behavioural, environmental factors and determinants – PROCEED: development, implementation and evaluation of intervention); (ii) the setting of proximal programme or ‘performance’ objectives (i.e., what needs to be learned or changed that may be linked to individual, organizational or community level change) and its determinants (personal or external); (iii) the selection of theoretical methods (i.e., modelling) and practical strategies to apply it (i.e., video with peer models); (iv) the actual design into one comprehensive programme that supports the theoretical basis; (v) a plan for its systematic implementation by the programme users; and (vi) a process and effect evaluation to assess effects. However, the authors emphasize careful application of theory to avoid risk of undesirable outcomes (i.e., they offer the example of how using ex-drug addicts as role models in school-based programmes has led to increase in drug use – due to implicit messages that drug use can still lead to socially acceptable actions [ex-drug addicts as lecturers] and focusing on the dangers of use, rather than decision-making skills, social resistance skills, and self-efficacy [43].
1.4. School-based Prevention of IA in Adolescence
The school system is increasingly used as a venue to drive prevention efforts and to address health promotion and public health concerns [57]. This can take the form of teacher and parent training, student education, and awareness raising, may enhance protective factors and reinforce positive behaviours or aspects of the environment that reduce the likelihood of negative occurrences [57]. School-based efforts are efficient in that they offer access to large numbers of students in a cost-effective way [53, 58]. Programme benefits have been estimated to exceed programme costs, with cumulative benefits, potentially in more areas than the intended ones (i.e., academic achievement or other health promoting behaviours; [58]), as assessed in school-based addiction prevention programmes (i.e. drugs, alcohol, gambling [59, 60]). Given the similarities between behavioural and non-behavioural addictions [61-63], examining the evidence from school-based initiatives in substance addictions, eating disorders and gambling could fortify the approaches in IA prevention [44, 64-66]. Findings for the effectiveness of universal school based prevention programmes appear to be positive [67, 68], whereas the effectiveness of targeting specific mental health issues is still conflictual [69, 70].
1.5. The Present Study
IA as a phenomenon has been addressed differently in various parts of the world in terms of prevention. Over the past 20 years, the increased risk of IA in South East Asia has prompted respective governments to initiate comprehensive national prevention and intervention plans as well as considerable investment in academic research into the behaviour [56, 71]. For example, in South Korea, with 7% of the population being at risk for IA according to the National Survey on Internet Addiction (2013 [72]), IA prevention education has become compulsory by law (Article 30, item 8 National Information Basic Act) [72], with all levels of education undergoing age-appropriate IA prevention training with the support of local and central government. Such initiatives have only been sporadically introduced in recent years in Western countries and are still in an emerging phase in terms of prevention [36].
King and colleagues [73], who conducted a systematic literature review on worldwide prevention strategies for disordered and hazardous gaming and Internet use, concluded that: (i) formal recognition and definitional confusion remains a challenge in order to develop robust prevention programmes, and (ii) the prevalence of the phenomenon in a global context and the geographically dispersed prevention programmes point to the importance of integrating prevention efforts and successful practices across countries, with attention to cultural differences. Additionally, studies and other reviews report a lack of evidence-based prevention programmes and RCTs – considered the “gold standard” in evaluating intervention outcomes [74] and effectiveness in educational interventions [75] - to guide clinicians, educators, community centres and other important stakeholders with these types of behavioural addictions [50, 71, 76].
Building further on the aforementioned findings and the documented benefits of school interventions in the addiction field [53, 58], it is timely to focus on school-based initiatives for IA prevention. More specifically, the aim of this systematic literature review is to (i) identify relevant prevention programmes or protocols within the school context and to examine the programmes’ effectiveness, and to (ii) highlight strengths, limitations, and best practices to inform the design of new initiatives, by capitalizing on these studies’ recommendations. To the authors’ knowledge, this review extends general reviews on prevention of IA [50, 73] that only partially covered school-based IA programmes as part of the overall prevention initiatives and will focus exclusively on the effectiveness of school based prevention programmes for adolescents providing recommendations that could be useful in informing future designs.
2. METHOD
A systematic literature review was conducted on adolescent school-based prevention interventions for IA and gaming addiction. Inclusion criteria for the present review were the following: (i) all journal papers – referring to published protocols of preventive interventions, even if not accompanied by an evaluation, as well as any type of quantitative and qualitative evaluation of effectiveness; (ii) studies targeting adolescents, aged 11-17 years in a school environment; (iii) studies with publication dates between 2007-2017, since IA prevention approaches are a relatively nascent field within literature; (iv) full-text studies published in English, German, Spanish and Greek language (the native languages of the co-authors); and (iv) studies targeting multiple risk behaviours (i.e., drugs, alcohol), where IA was included as one of the targeted behaviours.
Excluded from the review were: (i) studies referring to IA and general prevention; (ii) East Asian countries’ studies with the main text not published in English language or with small sample sizes, that risk poor transferability of findings due to low ecological validity; (iii) studies that evaluated Internet safety exclusively or school-based interventions focusing on screen time, as this construct is operationally different from IA and refers to sedentary behaviours that encompass a variety of behaviours that are not necessarily Internet-related (i.e., television watching); (iv) studies on the use of the Internet as a medium for other prevention purposes; and (v) cyberbullying and gambling prevention studies, as these do not have IA or gaming as their primary preventive focus.
The systematic literature search consisted of selecting papers from the following electronic databases: Web of Science, PsycINFO, PubMed, Science Direct, and Google Scholar and was conducted using the following broad search terms: prevent*, intervention, program*, adolescent*, school*, gam*, addict*, “internet addiction”, “social media”, “social networking sites”, “digital media”, “internet use”. These database search parameters yielded a total of 1,597 hits, which included the following results in each database: Web of Science (388 results), PubMed (481 results), PsycINFO (243 results), Science Direct (186 results), Google Scholar (249 results), and articles identified from other sources (50 results). A flow chart process for the present review is presented in Fig. (1). Table 1 presents an outline of all the reviewed studies. The interventions and outcomes evaluated in the studies reviewed were too diverse and not reported in all of the studies to allow a quantitative synthesis of the findings. A narrative synthesis of type of interventions, outcomes and effectiveness - where applicable - has therefore been provided.
Fig. (1).
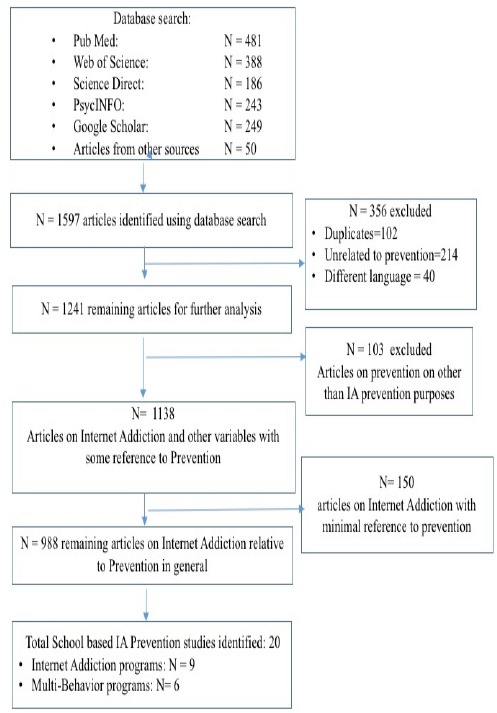
The flow diagram of the selection process.
Table 1. School-based internet addiction/gaming prevention programmes.
| Authors/Study Title | Objectives | Brief Description/Methods | Sample | Scales used | Results | Country | |
|---|---|---|---|---|---|---|---|
| Lindenberg, Halasy & Schoenmaekers (2017) - A randomized efficacy trial of a cognitive-behavioural group intervention to prevent Internet Use Disorder onset in adolescents: The PROTECT study protocol [77]. | Primary outcome: the 12- months incidence rate of IUD. Secondary outcomes: the reduction of IUD and comorbid symptoms and the promotion of problem solving, cognitive restructuring and emotion regulation skills. |
Study protocol: An indicated theory-led, evidence-based, systemic intervention study protocol of a two armed randomized controlled trial to measure the efficacy of a 4 week cognitive-behavioural prevention intervention for adolescents with high risk of IUD. assessments at baseline, and follow-up at 1, 4 and 12 months. 4 weekly sessions (of 90 minutes) by trained professionals. intervention consists of 4 modules addressing: (1) boredom and motivational problems, (2) procrastination and performance anxiety, (3) social interaction and (4) emotion regulation based on empirical findings of IUD risk factors. Cognitive Behavioural focus: (i) psychoeducation, (ii) cognitive restructuring (dysfunctional beliefs), (iii) behaviour modification (problem solving skills, contingency management, 4) emotion regulation training |
Total sample for screening N=3,240 to obtain a total N=340 of high risk adolescents, 12-18 years, approx. 170 classes in 43 schools | Self-report questionnaire (sociodemographic data, usage etc.), screening for risk of IUD: baseline, the German version of the Compulsive Internet Use Scale (CIUS) [91,92] + clinical interviews to assess IGD based on DSM-5 [88] criteria, at 12 month follow up (primary outcome), assessment at baseline and follow-ups of IUD, potential risk factors, comorbid psychopathology + school related consequences (grades + truancy). Other assessment tools: the German Computer Gaming Addiction Scale (CSAS) [93], the German Depression Inventory for Children and Adolescents (DIKJ) [97], the Strength and Difficulties Questionnaire (SDQ) [98], the 7th scale of the German adaption of the Fear Survey Schedule for Children – Revised (PHOKI) [99], the German version of the Social Interaction Anxiety Scale (SIAS) [100,101], the German Interaction Anxiety Scale (SIAS) [100,101], the German Questionnaire for Assessment of Emotion Regulation in Children and Adolescents (FEEL-KJ) [102], the German Questionnaire for Procrastination (APROF) [103], the German Student Assessment List for Social and Learning Behaviour (SSL) [104], the German Self-Efficacy Scale (SWE) [105], and the WHO-5 Well-Being Index [106] User evaluation (acceptance and satisfaction with the intervention). |
N/A | Germany | |
| Walther, Hanewinkel & Morgenstern (2014) - Effects of a Brief School-Based Media Literacy Intervention on Digital Media Use in Adolescents: Cluster Randomized Controlled Trial [79] | Primary outcomes: 1.computer gaming 2. Internet use: days per month, hours per day, and addictive use patterns. Secondary outcomes: 3. Parental media monitoring 4. rules at home | Cluster randomized controlled trial of a 4 week media literacy program on adolescent gaming and Internet Use behavior (Vernetzte www.Welten - Connected www.Worlds), 3 assessment periods (baseline/posttest/follow-up), delivered by trained teachers. | Students (10 -14 years) 2,303 students initially - 1, 843 final sample- in all 3 assessment periods, 27 schools, 102 classes. |
the German Internet Addiction Scale (ISS) [95] + additional questions on use, the German Computer Gaming Addiction Scale (KFN-CSAS-II) [94] | Mixed outcomes: signficant intervention effects only for gaming but not for Internet use: lower increase in self-reported gaming frequency (b= -1.10[95% CI - 2.06, - 0.13]), gaming time (b = - 0.27 [95% CI - 0.40, - 0.14]), and proportion of excessive gamers (AOR = 0.21 [95% CI 0.08, 0.57]) (vs the control group). No intervention effects for frequency and duration of Internet use or for students’ reports of parental monitoring or rules about media behavior at home, the number of internet users doubled during the intervention. | Germany | |
| Dreier, Wölfling, Beutel & Muller (2015) - Prevention of Internet Addiction. Digitally supported workshops for children and adolescents [1] | To enhance students' awareness of potential dangers from excessive media use, initiate discussion, encourage the use of critical thinking and recognition of early signs and counter measures for internet gaming disorder and behavioural addictions. | A prevention program consisting of 3 digital workshops for children and adolescents, discussing internet addiction, internet gaming disorder and diagnostic criteria and structural characteristics of games, employing a peer approach. Three types of Workshops were provided i) to raise awareness for potential IA dangers ii) of Internet Gaming Disorder and its diagnostic criteria iii) and free to play games. Students were asked to create their own free to play game and to evaluate its structural characteristics, the game mechanics and other related factors. | N/A | N/A | N/A | Germany | |
| de Leeuw, de Bruijn, de Weert-van Oene & Schrijvers (2010) - Internet and game behaviour at a secondary school and a newly developed health promotion program: a prospective study [6] | Internet use (hours/day), game use, compulsiveness of use and relationship with other health behaviour outcomes (alcohol use, physical activity, psychosocial wellbeing and body mass index) | Multi-behaviour, pre-post design, pilot project for case-control study. Duration: 2 hours/week for a year by trained teachers, assisted by expert local health agencies and addiction centres. Media Education on: Internet use (digital communication), online bullying, online image, online sexuality, distorted beauty ideal and Internet advertisements. | N=475 initially- N=367 final sample, students 11-16 years at a secondary school | The Compulsive Internet Use Scale (CIUS) [91], an adapted version, the Compulsive Game Use Scale (CGUS), the Strengths and Difficulties Questionnaire (SDQ) [98] | Heavy internet users presented with more behavioural problems (higher SDQ scores [98], 13.8% vs. 1.4% of non-heavy users) as well as game users (14.3% vs. 4.3 of non-heavy users). Girls were heavier users (24.3% vs. 17.4% boys) and children of the lower general secondary education group (33.9% vs. 7.1% non-heavy users). Boys were heavier game users than girls (29.5% vs. 7.7%) and with higher CGUS score with more play time. Heavy game users were less happy at school and scored higher on CIUS [91] than non-heavy game users. Post-intervention effects: the time spent on Internet (hours/day) and the number of pathological Internet users increased (2.22 vs. 1.44) and (97.6% vs. 95.5% respectively), during the study. Heavy game use increased (4.3 vs. 3.24) but number of game users decreased (64.1% vs. 72.5%). Heavy internet use was associated with psychosocial problems. Heavy game use was associated with both psychosocial problems and less physical activity. | Netherlands | |
| Ma, Chu & Chan (2011) - Construction of a teaching package on promoting prosocial internet use and preventing antisocial internet use [83] |
Learning targets: social skills and abilities, self-concept and self-management, social values and social relationships | Protocol description of the new P.A.T.H.S. teaching package for internet use consisting of 9 units on Internet Use: cheating, privacy issues, effects of excessive use on life and study, on-line shopping, online pornographic materials, copyright infringements, impacts on health, negative consequences | N/A | N/A | N/A | Hong Kong | |
| Andrisano-Ruggieri, Santoro, De Caro, Palmieri, Capunzo, Venuleo & Boccia (2016) - Internet addiction: a prevention action-research intervention [82] |
Objectives were promotion of awareness of subjective relationship with technologies and healthy lifestyles among peers | Pre-experimental research design model for the evaluation of a prevention intervention program in schools: a 1 year peer education programme. Use of active methods (e.g., brainstorming, circle time, role playing, tutoring, peer action) | A total of 90 young subjects (45 males and 45 females) | The Internet Addiction Test (IAT) [89,90] | Results reported significant positive difference in the post-treatment values for both males and females: a significant decrease in post-intervention IAT scores (i.e., for the severe level, from 4% to 2.2%, and for the moderate level from 62% to 42.3%). However, there was an observed increase for the mild level from 34% to 55.5%. Researchers did not provide any possible justification for this occurrence. | Italy | |
| Korkmaz & Kiran-Esen (2012) - The Effects of Peer-Training about Secure Internet Use on Adolescents [78] | examine the effects of peer training for secure internet use on adolescents in Turkey. | 10-session peer-education program: 12 Peer trainers received a 10 x 90 session and delivered 2 x 40 minute -sessions | 825 students, 13-15 years, at two elementary schools, N=410 were in the experimental group and N=415 were in the control group. | The Internet Use Habits Scale (IUHS) (Yılmazhan-Gültutan 2007 in [78]) | Findings: i) statistically significant positive difference (Z=-3.267, p<0.05) in the experimental groups in Internet Use Habit Scale total scores; no baseline differences between experimental and control group ii) statistically significant difference in IUHS post-test scores (U=40350.5, p<0.05). | Turkey | |
| Shek & Leung (2013) - Development of an integrated intervention model for internet addiction in Hong Kong [49] | Description of the development of the “Youngster Internet addiction prevention and counselling service” for young people with Internet Addiction problems. Includes: provision of preventive services at the community, school, family and individual provision. peer and family levels, and use of both case and group approaches. | Focus of the counselling model is: controlled and healthy use of the Internet, understanding the change process in adolescents with Internet addiction problem, use of motivational interview methods, adoption of a family perspective, multi-level counselling at the individual, peer and family levels, and use of both case and group approaches. | N/A | N/A | Evaluation findings provide support for the model; use of both objective and subjective outcome evaluation methods. | Hong Kong | |
| Hswen,Rubenzahl & Bickham (2014) - “Cyberhero Mobile Safety”: Feasibility of an online and mobile videogame curriculum for teaching children safe and healthy cellphone and Internet behaviors [85] | To transfer knowledge and skills for safe and balanced mobile (cellphone and mobile internet) behaviours | A videogame-based education program consisting of six educational concepts focusing on social responsibility and citizenship to address risk and protective factors and to build on competencies relevant to healthy online usage. | N=108 | Measured the number of gameplays for each game, the proportion of gameplays where game-specific success criteria were achieved and the length of time required to successfully complete the game. | Positive student perceptions for usability, feasibility, appeal, and perceived impact.: Videogame usability of 82.7 percent of the students’ gameplays. Mean ratings were 4.09 (standard deviation [SD] = 1.28) for likeability, 3.54 (SD = 1.61) for acceptability, and 4.16 (SD = 1.33) for perceived message usefulness. | USA | |
| Multi-behavioural studies | |||||||
| Busch, de Leeuw & Schrijvers (2013) - Results of a Multibehavioural Health-Promoting School Pilot Intervention in a Dutch Secondary School [48] | Evaluation of the multi-behavioural health promoting intervention | Results of a pilot study of a secondary school based, health- promoting intervention (3 year curriculum) that simultaneously targeted a range of adolescent health behaviours that appear to be interrelated and interacting synergistically with common determinants: alcohol use, cannabis, compulsive internet and gaming, and bully victimization. pre-post intervention design. | N=336, 15-16 years | Most survey items were from the Dutch Health Behavior in School-aged Children (HBSC) questionnaire [48], Family Affluence Scale (FAS) [148], Strengths and Difficulties Questionnaire (SDQ) [98], the Olweus Bully/Victim Questionnaire [149], the Compulsive Internet Use Scale (CIUS) [91], and the Videogame Addiction Test (VAT) [96], scales on other risk behaviours (alcohol consumption, drug use etc) | The intervention brought significant behavioural changes for weekly screen time (computer and television), only for boys. CIUS [91] scores were significantly different only for girls (1.37 in 2010 vs. 1.50 in 2007) and VAT [96] scores (1.49 in 2010 vs. to 1.10 in 2007). No differences in weekly hours of gaming for boys (still playing for 3 hours/week vs. half hour for girls). Only one intervention school, without a control group. Comparing participant students results with trends over the same period of time (2007 vs. 2010) with peers participating in the Dutch HBSC (2009 vs. 2010) a significant reduction was observed on all health behaviour measures. | Netherlands | |
| Shek, Ma & Sun (2011) - Development of a new curriculum in a positive youth development program: The Project P.A.T.H.S. in Hong Kong [81] | Protocol study: curriculum design of the Project P.A.T.H.S. universal positive youth development program | The design of a 4-year project, with a curriculum for a positive youth development program (Project P.A.T.H.S.) targeting substance abuse, sexuality issue, Internet addiction, bullying, and money and success issues. Collaboration of the Research Team, the Hong Kong Social Welfare Department and Education Bureau - 20 hour curriculum - with 10 hours for core units and another 10 hours for elective units, 40 units/grade x 30 minutes | Since 2005-2006: 280 secondary schools, 212,000 students, 10-13 years | N/A | Description of the curriculum and its rationale: Program P.A.T.H.S. (Positive Adolescent Training through Holistic Social Program), is a curriculum, in both Chinese and English versions, tailored for each secondary school grade, 120 teaching units are designed with reference to 15 positive youth development constructs. The extension phase of the project (3 more years) involves: 60 teaching units with specific reference to five major adolescent developmental issues (substance abuse, sexuality issue, Internet addiction, bullying, and money and success issues) | Hong Kong | |
| Shek, Yu, Leung, Wu & Law (2016) - Development, implementation, and evaluation of a multi-addiction prevention program for primary school students in Hong Kong: the B.E.S.T. Teen Program [86] | i) objective outcome evaluation with a pretest–posttest experimental-control group design: 1. addictive behaviours 2. behavioural intentions 3. psychosocial competencies 4. knowledge about addiction, and 5. beliefs about addiction. ii) subjective outcome evaluation: students’ perceptions of the program | The B.E.S.T. Teen Program aimed to promote behavioural, emotional, social, and thinking competencies to prevent multiple-addictions | N=679 students 10-11 years, 10 schools (5 experimental and 5 control) in Hong Kong | The measures were: i) an objective outcome evaluation questionnaire (based on IAT [89,90], expert views and intended learning outcomes) that was developed and validated by the research team, and assessed: addictive behaviour, behavioural intention, psychosocial competencies, knowledge about addiction, beliefs about addiction ii) a subjective outcome evaluation measured program attributes, implementer attributes and program effectiveness. | Partial support for program effectiveness, the experimental group reported less intention by 45% for excessive Internet use (β = −0.61, S.E. = 0.19, OR = 0.55, p < .002),group significantly predicted participants’ intention to use Internet excessively in the coming 2 years (β = −.07, p = .02) experimental group scored higher on psychosocial skills, knowledge and beliefs compared to control. No significant effects for the other outcome indicators (i.e. intention for smoking). High positive views expressed for the curriculum content and high program satisfaction. | Hong Kong | |
| Shek & Ma (2014) - Effectiveness of a Chinese positive youth development program: the Project P.A.T.H.S in Hong Kong [80] | To examine the effectiveness of Project P.A.T.H.S. 4 months post intervention and provide supplementary research findings on its effectiveness | Social survey data - use of a static-group comparison design (pre-experimental design) | 3,328 students were recruited from 28 secondary schools for the wave 1 data (4 months post-intervention), with 16 schools intervention group and 12 schools controls | The modified version of the Chinese Positive Youth Development Scale (CPYDS) [80] with 15 subscales: (1) bonding, (2) resilience, (3) social competence, (4) recognition for positive behaviour, (5) emotional competence, (6) cognitive competence, (7) behavioural competence, (8) moral competence, (9) self-determination, (10) self-efficacy, (11) clear and positive identity, (12) beliefs in the future, (13) prosocial involvement, (14) prosocial norms and (15) spirituality. 10 item Internet Addiction Test (IAT) (Chinese version) [150] and other measures of adolescent psychological symptoms and risk behaviour (Substance Use, Deliberate Self-Harm Behavior, Hopelessness, Exposure to pornographic materials etc.) | This study examined the effectiveness of Project P.A.T.H.S. The data collection took place 4 months after the inception of Project P.A.T.H.S. Compared with students in the nonparticipating schools, students participating in the Project P.A.T.H.S. had better positive youth development and displayed less adolescent risk behaviour. | Hong Kong | |
| Shek & Yu (2011) - Prevention of adolescent problem behavior: Longitudinal impact of the Project P.A.T.H.S. in Hong Kong [108] | Examine the longitudinal impact of project P.A.T.H.S. | A longitudinal randomized group design with six waves of data, collected from 19 experimental schools and 24 control schools analysed with individual growth curve (IGC) modelling | Experimental group: n = 3,797 at Wave 1, control group: (n = 4,049 at Wave 1) | Chinese Positive Youth Development Scale (CPYDS) [80] | Results demonstrated that adolescents receiving the program exhibited significantly increases in self-control over Internet use. The control group showed a gradual deteriorating trend, while the experimental group first showed a slower rate of decrease and then changed to a tendency of increase, offering evidence for long-term effects in preventing adolescent problem behaviour through promoting positive youth development. | Hong Kong | |
| Busiol & Lee (2015) - Prevention of Internet Addiction: The P.A.T.H.S. Program [107] | The developmental issues underpinning the P.A.T.H.S programme and how these are addressed | commentary based on findings of the P.A.T.H.S program | N/A | N/A | The impacts and consequences of Internet addiction might be less easily recognized or ignored. Project P.A.T.H.S against Internet addiction, advocates that positive youth development promotion in adolescence is key to an effective prevention programme. Results indicated improvement in psychosocial competencies and decrease in problem behaviour vs. control group. Authors discussed the extension phase of Project P.A.T.H.S. on Internet addiction. | Hong Kong | |
3. RESULTS
All studies that met the inclusion criteria were universal prevention studies, targeting general adolescent student populations, except for one indicated prevention study [77], which was a protocol for a study targeting high risk adolescents for IA. These high risk adolescents were identified through an initial screening based on the protocol’s inclusion (adolescents aged 12-18 years at risk for IUD) and exclusion criteria (meeting DSM-5 criteria for Internet Gaming Disorder (IGD), comorbid depression and anxiety disorders – social phobia or performance anxiety). Interventions varied from digitally supported workshops (1) and peer to peer training [78] to more complex designs: media literacy intervention on digital media use [79], multi-behaviour health promotion programmes with internet use and gaming included as a target behaviour [6, 48] to cognitive behavioural group intervention protocols (77) and integrated intervention models for IA [49] that embedded preventive/psychoeduca-tional and therapeutic elements in their approach to target at risk and affected adolescents. Multi-behaviour programmes were: health education programmes that were part of an integrated school health promotion programme (as described by the European Network of Health Promoting Schools in Europe [SHE] in the case of de Leeuw and colleagues [6]; the Utrecht Healthy School (UHS) [48]; and large multi-addiction and positive youth development programmes [80, 81]. These involved a range of high risk behaviours rather than targeting a single mental health promoting intervention [68]. Seven such programmes were reviewed, where IA and gaming were part of the targeted behaviours, but five papers referred to the same programme (the Hong Kong P.A.T.H.S. Programme - The Project Positive Adolescent Training through Holistic Social Programs) [79].
With regards to study designs in papers reporting programme evaluations, two studies were randomized controlled trials (RCTs); one used three assessment points (baseline, post-test, and 12-month follow-up) [79], and the other used assessments at one, four and 12 months after admission [77]. Four used pre-post intervention pre-experimental pilot designs [6, 48, 78, 82]. Three studies were protocols of studies
with no accompanying evaluation [1, 77, 83]. An analysis of objectives, methods and respective effectiveness of interventions is presented below and key challenges will be highlighted that can be taken into account when addressing future designs.
Lindenberg and colleagues [77] designed a cluster prospective randomised controlled two-armed registered trial protocol (intervention vs. assessment only), using strict clinical criteria accounting for RCT methodological elements (randomisation, allocation concealment, blinding, measuring compliance, controlling for co-interventions, and accounting for dropout). Walther and colleagues [79] designed a two-wave (baseline, post-intervention) RCT with two arms (intervention vs. control group). Cluster randomisation, in both studies, was stratified according to school type (based on the German education system). In Walther and colleagues’ study [79], the blockwise randomisation led to unequal sample sizes and different types of schools in the two groups, whereas in the Lindenberg and colleagues’ study [77], each school was considered a unit of randomisation.
Risks of biases were acknowledged in the studies where an intervention was assessed. The following were identified: selection bias (allocation generation) [6, 48, 79] for baseline differences between groups, potentially compromising the studies’ validity, performance bias (blinding procedures of participants) in all studies, attrition bias (non-completion) [6, 48, 78], detection biases (blinding process of outcome assessors), reporting bias (self-reporting or partial accounting of results), as all of the measures were self-reports, and social desirability biases (providing socially acceptable answers) [82]. Biases may potentially lead to faulty reporting of either beneficial or harmful or incorrect conclusions of intervention effects, such as lack of proper randomization that may be associated with more positive intervention outcomes [84]. No protocols were pre-registered with the exception of Lindenberg and colleagues’ [77] that is a registered pre-clinical trial.
The programmes targeted adolescents (of various ages between 8-18 years with the majority targeting middle adolescence: 12-18 years [77]; 10-14 years [79]; 15-16 years [48]; 11-16 years [6)] 13-15 years [78]; 8-12 years [85]; and 12-15 years [81], spanning eight countries (Germany, The Netherlands, Italy, Australia, Korea, Hong Kong, USA, and Turkey). These programmes were delivered by a combination of either trained school teachers (with the guidance of expert health agencies) during class time [79, 85], trained professionals (psychologists, social workers, and researchers) and public health teams [77, 82, 86], a research team comprising scholars in various disciplines [80], or by peer training [1, 78].
Intervention sample sizes ranged considerably from 90 adolescents [78] to 1,843 adolescents in all three assessment periods [79] with the exception of the Project P.A.T.H.S., that used exceptionally large sample sizes (250 schools) across the different phases of its implementation [81]. The duration of interventions varied from two forty minute sessions and ten peer training sessions [78] to a three year curriculum [48]. The programmes predominantly targeted Internet use and gaming, with the multi-behavioural programmes targeting a variety of adolescent risk behaviours (i.e. alcohol, drugs, and bullying), and aiming for holistic adolescent growth [81]. Few studies included some degree of parental involvement and evidence-based parts that were customized based on school priorities [48]: parental recommendations and encouragement of media-related communication with children [79], or made reference to parental engagement in the programme [6]. Consequently, the programmes featured variability in the objectives, methods, the assessment tools, and the outcomes they aimed to achieve.
3.1. IA and Gaming-related Outcomes
Problematic internet use was assessed as a function of the following variables: internet use disorder (IUD) and gaming addiction [77], IA [82], internet use habits [78], internet use and gaming frequency, proportion of excessive gamers [79], compulsive Internet use and gaming [6, 48]. This demonstrates a wide range in outcomes assessing problematic Internet use and gaming, and reflects the diverse conceptualizations of the disorder and the conceptual confusion that characterizes research in the IA field.
3.2. Protective and Risk Factors
Further to IA symptomatology, the prevention programmes evaluated in the present review aimed to enhance protective factors and minimize risk variables of IA, reduce comorbid symptoms and negative psychosocial consequences related to IA. These variables were measured as secondary outcomes in the majority of the studies. Protective factors encountered were individual (rather than systemic) factors, related to skill enhancement, knowledge imparting and attitude changing, as well as reducing symptoms of comorbidities. These were related to increase of knowledge of IA risks and impacts, and promotion of psychosocial competencies: critical evaluation skills, social skills, problem solving skills, emotion regulation and self-control skills, cognitive restructuring skills, reduction of impulsiveness, self-concept, self-management, promotion of healthy social relationships, promotion of awareness of subjective relationship (personal relevance) with technologies, and social learning (peer training).
Overall, the following outcomes were assessed to determine whether these prevention interventions for IA (i) reduce symptoms or severity, or (ii) confer a change in attitudes in psychosocial functioning compared to baseline measures. Usage outcomes included Internet use and gaming duration/frequency (days per month, hours per day, and addictive use patterns) [6, 48, 77-79, 82], the 12-month incidence rate of IUD and reduction of IUD [77]. Knowledge and Attitude shifting outcomes included attitude/perception or awareness change towards Internet use [78, 82, 86]; behavioural intention, knowledge and shifting of misconceptions regarding addictions [86]. Skill enhancement outcomes included enhanced problem-solving, self-control, critical thinking, cognitive restructuring, self-reflection and emotion regulation skills [77, 86, 87], and media literacy [79]. Symptom reduction outcomes included comorbid symptoms and negative school-related outcomes [77], cognitive, emotional, social, and behavioural competence. Process evaluation outcomes included usability, likeability, knowledge, and attitude change [81, 85, 86]. Multiple-risk behaviour outcomes related to substance abuse and alcohol use [48], addictive behaviours, psychosocial competencies, and knowledge about addiction. Qualitative outcomes included parental media monitoring and rules at home [79]. These outcomes were assessed with a variety of assessment tools.
3.3. Assessment Tools for IA/gaming Addiction
A wide variability was also observed in terms of the diagnostic tools used to assess the outcomes of the programmes with respective differences in the cut-off points that address clinical symptom severity, as well as those utilized to assess psychosocial symptom severity and improvement. All studies relied on use of self-report data with the exception of the study by Lindenberg and colleagues [77], which included clinical diagnostic interviews according to the DSM-5 [88] IGD criteria to assess gaming addiction (used as exclusion criterion) in the 12 month follow-up of the PROTECT Study. Two of the programmes [80, 82] used Young’s Internet Addiction Test (IAT) [89, 90, 150]; the Compulsive Internet Use Scale (CIUS) [91, 92] was utilized in three studies [6, 48, 77]; Walther and colleagues [79] and Korkmaz and Kiran-Esen [78] used the Internet Use Habits Scale (IUHS) (Yılmazhan-Gültutan 2007 in [78]). Other scales used were the German Computer Gaming Addiction Scale (CSAS and KFN-CSAS-II) [93, 94]; and the German Internet Addiction Scale (ISS) [95] were utilized in 2 studies [77, 79]. The Compulsive Game Use Scale (CGUS) used in the de Leeuw and colleagues study [6] was a non-validated version adapted for gaming based on the CIUS [91]. Similarly, Busch and colleagues [48] used the Videogame Addiction Test (VAT) [96] to assess video game addiction. In Shek and colleagues [86], IA was measured with a single item question, therefore addictive behaviour may not be accurately represented in their results.
3.4. Assessment Tools for Psychosocial Impacts and Comorbid Symptomatology
A number of assessment instruments were utilized to assess psychosocial symptom severity and improvement reflecting a variability in socio-emotional impacts and potential comorbid conditions. The German Depression Inventory for Children (DIKJ) [97], the Strengths and Difficulties Questionnaire (SDQ) (emotional symptoms, hyperactivity, peer problems, conduct problems and prosocial behaviour) [98] was used in three studies [6, 77, 80]. Lindenberg and colleagues [77] used the seventh scale of the German adaptation of the Fear Survey Schedule for Children – Revised (PHOKI) [99] the German Interaction Anxiety Scale (SIAS) [100, 101], the German Questionnaire for Assessment of Emotion Regulation in Children and Adolescents (FEEL-KJ) [102], the German Questionnaire for Procrastination (APROF) [103], the German Student Assessment List for Social and Learning Behaviour (SSL) [104], the German Self-Efficacy Scale (SWE) [105], and the World Health Organization-Well-Being Index (The WHO-5 Well-Being Index) [106]. The Chinese Positive Youth Development Scale (CPYDS) was used in one study [80]. In the case of the multi-behavioural studies, scales regarding other risk behaviours (alcohol consumption, drug use, bullying behaviours etc) were also administered.
3.5. Intervention Methods
The reviewed prevention programmes embraced a range of intervention methods used unilaterally or in combination: (i) peer-to-peer approach [1, 6]; (ii) skill-based, competency enhancement strategy, psychosocial competencies to promote adolescent strengths, encouraging critical thinking, self-monitoring, self-reflection, critical perception and discussion about own use or media literacy enhancement [1, 48, 86]; (iii) reduction of comorbid symptoms and negative psychosocial consequences: anxiety, depression negative school-related outcomes (i.e., procrastination) [77]; (iv) awareness-raising/information imparting about the negative consequences and potential risks of IA (all studies), and (v) emphasis on positive psychology (the Positive Adolescent Training through Holistic Social Programs (Project P.A.T.H.S) [80, 81, 86, 87, 107-109].
3.6. Effectiveness
Effectiveness measures were reported by seven studies (the remaining being protocol studies), with the majority reporting mixed outcomes as to Internet or gaming use. Effect sizes (Cohen’s d) were calculated by the authors of this review, where applicable, for the RCTs and the pre-experimental designs, in order to employ a common method of measuring effectiveness across studies. De Leeuw and colleagues [6] presented small to medium effect sizes, ranging from d = 0.112 (Cohen’s d) in gaming use duration scores to d = 0.401 for internet use duration. In third year students only, a higher effect size was observed for compulsive Internet use scores (d = 0.563). The results indicated an increase in time spent on the Internet (hours/day), in heavy game use and an increase in the number of pathological Internet users contrary to expectations, but managed to achieve a decrease in numbers of game users, suggesting that the intervention partially managed to influence adolescents’ intention to change Internet and game use. The study also confirmed the association between Internet use and psychosocial problems and between game use and less physical activity.
In the study by Walther and colleagues [79], findings suggested mixed effects for computer gaming – a decrease in self-reported gaming frequency from baseline (Time 1) to post-test (Time 2) only for the intervention group, but an increase was reported from post-test (Time 2) to follow-up (Time 3) for both the intervention and the control groups. No intervention effects were found for frequency or duration of students’ Internet use. On the contrary, Internet use increased during the study duration (15 months), while the number of Internet users doubled. Students’ reports of parental monitoring or rules about media behaviour at home (secondary outcomes) were unaffected by the intervention.
Similarly, Andrisano-Ruggieri and colleagues’ [82] intervention had a medium effect size (Cohen’s d = 0,579 for males and d = 0,409 for females) and exhibited a significant decrease in post-intervention IAT [89, 90] scores in the severe and moderate level, but an increase in IAT [89, 90] scores for the mild level. Statistically significant positive differences in the post-intervention findings (Z=-3.267, p<0.05) were observed for the intervention group vs. the control group in Korkmaz and Kiran-Esen’s study [78], as measured by the Internet Use Habit Scale pre- and post-test total scores.
The multi-behaviour intervention of Busch and colleagues [48] also presented mixed findings. The intervention brought significant behavioural changes for weekly screen time (computer and television) only for boys, but no differences were observed for boys in weekly hours of gaming. Gender differences were observed in the results. CIUS [91] scores were significantly different only for girls as VAT [96] scores. Comparing participating students’ results with trends over the same period of time (2007 vs. 2010) with peers participating in the Dutch Health Behaviour in School-aged Children (HBSC) study (2009 vs. 2010 – Trimbos Institute in Busch and colleagues [48]), a significant reduction was observed on all health behaviour measures. No change was observed for time of use or compulsiveness for boys, but boys presented significantly fewer psychosocial problems in the post-intervention condition compared to the girls.
Positive results were observed in the multi-risk behaviour programmes. The P.A.T.H.S Project (the largest positive youth development programme implemented in Asia) [87] led to a reduction of IA and increased self-control over Internet use. It employed various assessment periods. In the initial phase, RCT data were collected over eight occasions. In year 1, pre-test and post-test scores were collected. In year 2, four waves of data were analysed with individual growth curve models, suggesting better performance and less risk in the experimental group on various outcomes. In years three and four, six and seven, respectively, results were similarly positive [80]. However, an exhaustive appraisal of this large scale project is beyond the scope of this review that has been analysed in over 120 papers [87].
The B.E.S.T. Teen Program [86] presented preliminary objective and subjective outcome evaluations based on pre-intervention scores, and predicted a 45% decreased likelihood of the intervention group to exhibit uncontrollable Internet use, significantly lower intention to use excessively, and higher scoring on psychosocial skills, knowledge and beliefs about addiction, and correction of misconceptions. Programme participants held high positive views of the curriculum content and programme satisfaction. However, results were based on single item scores for each addictive behaviour measured, including IA, that presented low reliability (Cronbach’s a ranging from .24 to .31 pre-to-post-test).
In the US, the study of Hswen, Rubenzahl and Bichman [85] provided a qualitative evaluation by assessing in-game measures of usability and student perceptions of likeability, acceptability and perceived usefulness of educational videogame content. These were evaluated at post-intervention via questionnaires and demonstrated that this educational platform appears feasible and effective in increasing knowledge of healthy and safe smartphone use in school aged children.
Shek and Leung’s study [49] presented the development of a pioneering integrated IA prevention and intervention model in Hong Kong (the Youngster Internet Addiction Prevention and Counselling Service). However, the authors did not provide any analysis of effectiveness findings in this paper [49]. Studies in South East Asian countries identified in the literature (mainly South Korean) reported positive changes for their outcome variables [110-115], but were excluded from this review because they were published in languages unknown to the authors (see exclusion criteria). Their findings should be interpreted with caution as with very small sample sizes it is inherently more difficult to find the true effects of the interventions and applicability and transferability of programmes in other cultural contexts should be carefully examined. However, lack of wider dissemination of research findings limits the evidence base that is essential to identify best practices [73], and to warrant an understanding for prevention approaches conducted in countries where IA constitutes a priority in public health policy and where prevention has already been established on a national level [116].
4. DISCUSSION
Heterogeneity was observed in the scope, content, outcome evaluation (i.e., IA, screen time, frequency, attitudes, habits, etc.), and assessment tools used in the reviewed studies. This partially reflects the versatile conceptualization for IA, its complexity, and the different rationales on priorities that an IA prevention programme should focus on. The majority of programmes targeted reduction of IA. However, studies presented mixed outcomes with regards to Internet use and gaming, and it appears that setting reduced Internet use time as an outcome is rather problematic, similar to problems with the assessment tools for its measurement. Increasing knowledge for impacts and risks, promotion of protective factors and the enhancement of skills and competencies, and using peer–to-peer training were the main strategies used by the prevention programmes. The study designs varied from complex RCTs to assess the effectiveness of an intervention that uses CBT techniques for at-risk individuals [77, 79] to pilot pre-experimental designs delivered and measured within one school without the use of a control group [6, 48, 82]. Seven studies in this review were identified in support of a more integrated approach (multi-behaviour risk) for promoting healthier lifestyles in prevention efforts [6, 48, 80, 81, 86, 87, 107, 108]. However, five of the multi-behaviour prevention studies referred to the same programme and its extension period (Project P.A.T.H.S.) [80, 81, 86, 108, 109], suggesting that only three programmes addressing multiple risk behaviours to date have included IA as an outcome among other risk behaviours. This could be attributed to different aetiology, such as substance addictions (tobacco, alcohol and illicit drug use) traditionally being considered as the main risk behaviours in adolescents [117], the current scientific debate and lack of consensus for the clinical status of the disorder and its classification [4, 7, 118-120], and potentially the different prevalence rates amongst different countries that do not signal the same degree of risk for adolescents across countries.
4.1. Effectiveness of Interventions
Three major issues may be critical in terms of intervention effectiveness that appear to be compromising intervention results and need to be further addressed: i) the diversity of IA/gaming assessment tools used and the absence of diagnostic criteria and clinical status; ii) various methodological limitations encountered in the programmes’ designs, and iii) the use of Internet and gaming time reduction as main outcome variables in IA prevention studies.
The heterogeneity in assessment tools and cut-off points, the absence of diagnostic criteria and clinical status, and the use of self-reported data remain critical issues in empirical research in IA. The contested nature of IA is reflected in the wide use of measurement tools assessing IA and gaming and in the dimensional structure of these instruments [121], presenting methodological shortcomings that have an impact in the assessment of programmes’ effectiveness. Thus, deciphering the diagnostic/clinical status of IA is closely related to assessment and to serving prevention and clinical purposes. For example, the construct validity of the CIUS [91] presents sound psychometric qualities, but factor loadings are invariant between heavy and non-heavy use [122] and the measurement neglects other crucial dimensions of the construct (of withdrawal, tolerance or motives of escapism and social motivation) [121, 122]. Similarly, the Internet Addiction Test (IAT) used in two of the studies uses cut-off points that are arbitrary, not reflecting clinical disorder severity based on symptom evaluation, and does not present a temporal assessment of symptom presence [4].
More recent assessment tools base their factorial analysis on the DSM-5’s [88] IGD criteria, whereas older instruments do not reflect this development. New intervention designs should then cautiously adopt measures that are concurrent to scientific developments. Lindenberg and colleagues [77] used the only protocol in this review that applied DSM-5 criteria for IGD in a clinical interview, excluding gaming disorder and drawing a distinction between Internet Use Disorder (IUD) and gaming. This is the first prevention protocol that treats IA as a separate clinical entity from gaming addiction and uses assessment methods other than self-report data.
Other methodological design limitations that were encountered in the reviewed studies were: the pre-experimental designs, implemented with only one school (i.e., with students of higher socioeconomic background with higher levels of education), the lack of a control group to assess between-group differences [6, 82], the absence of evidence-based recommendations, critical in current addiction intervention directives [123] - with the exception of one programme [48] - and of follow-up assessments to estimate whether programme benefits are maintained over the long term [86], and small geographically restricted sample sizes (n=104) [85] indicate the need for further empirical evidence. All studies relied on self-report data and self-selection processes at a school level [79], posing a threat to representative sampling and the generalizability of the results. De Leeuw and colleagues [6] reflect on the inability to address which specific components of their intervention are driving the changes observed in the post-intervention with certainty, and whether these reflect knowledge benefits or extend to actual behavioural changes. Similarly, it was uncertain why gender differences in the results were observed in Busch and colleagues’ study [48], and it is crucial that research on gender differences be considered in the design of IA and gaming prevention and intervention programmes, attending to different gender needs [124].
An equally important omission is a post-intervention process evaluation for the assessment of Type III errors [48] or other biases for the identification of other methodological shortcomings, and for a further account of effectiveness [86]. Process evaluations are considered an essential component of an intervention, proposed by the new Medical Research Council guidance [125] and the APA guidelines for prevention [38], as they provide information about replication in the same context or about the reproducibility of outcomes that are relevant to policy makers who cannot only rely on effect sizes. Employing multiple evaluation strategies to allow for triangulation of data has also been recommended as an optimum approach to measure effectiveness [126].
The present review has highlighted the diversity in programme scope and outcomes and the mixed results in reducing Internet and/or gaming use. This partial influence on adolescents’ online behaviour was attributed by some of the authors to: (i) the difficulty in assessing Internet use vs. gaming, and ii) the developmental trajectory that presents variability in use (increase and change in use with age increase). However, setting Internet time reduction as outcome appears to be particularly problematic for many reasons, although less so for gaming, as highlighted in the studies reviewed [6, 79, 82]. In de Leeuw’s [43] study, although Internet use increased, this was not reflected in the CIUS [91] scores, adding to evidence that time that individuals spend online is contextual and not generalized may not be the defining variable in problematic use as has been argued by others [12, 127, 128]. The Internet is an essential tool in modern education and recreation, but determining the optimal use limit is paradoxical and a general all-encompassing concept (browsing, various types of recreation and social interaction, etc.) in need of further specification. This can be easier to achieve for gaming, but is substantially more difficult for general Internet use since it is an integral part of adolescents’ daily lives. Internet time reduction as an outcome in prevention studies has an inherent assumption that Internet use is negative. However, contrary to substance addictions, many beneficial effects have been evidenced for Internet use and gaming [129, 130]. Therefore, what needs to be addressed is determining exactly what is required to be limited when designing an IA and gaming intervention. Complete abstinence is not proposed as a viable solution to any intervention [49, 79], but in addition to contextual factors in adolescent life, examining motivational and harm-reduction factors (i.e., education, attention switching, and dissuasion) have been proposed to reduce game playing time and addiction levels [55].
4.2. Time Reduction as a Primary Outcome Variable
Focusing only on time spent online is also limiting in the conceptualization of gaming. First, in the context of gaming, the criterion of tolerance, which according to the DSM-5 [88] relates to increased time involvement, has increasingly been challenged [131] as not sufficiently representing the individual’s experience, with time in IGD not being the equivalent of dosage in substance-related addictions. Conversely, it appears that tolerance reflects more than just the need to increase time involvement, and taps into powerful structural game characteristics associated with key gaming motivations: inadequacy, a perception of no satisfaction from any game duration; achievement, overcoming challenges and progressing, and wealth, the increasing need to acquire valuable game artefacts [131]. Second, there is an increasing convergence in activities on the Internet that complicate the traditional divisions between activities, rendering prevention and intervention objectives more difficult to operationally define. Recent research evidence challenges the traditional definitional boundaries between gaming and social networking [19] and emphasizes the increased social networking activity observed in gaming contexts and vice versa [15], or between gaming and gambling activities [132]. These appear to share many common characteristics with diffused boundaries, including structural differences (in gaming the elements of interactivity, skill-based play, indicators of progress and success; in gambling: betting and wagering components, chance outcomes, and monetary characteristics with risk involvement) [19, 132]. This issue highlights the complexity in the assessment of online activities and poses further challenges in the design of prevention initiatives.
4.3. Protective, Risk and Harm-reducing Factors in IA Prevention Programmes
An emphasis on protective factors – characteristics that reduce the likelihood of IA occurrence – were encountered in the studies reviewed [83, 87]. These were intrapersonal protective factors (i.e., related to genetic predispositions, personality traits and mental disorders), rather than systemic (family or community wide). Specifically, the studies highlighted the promotion of positive psychology variables (i.e., self-esteem, self-efficacy), [133] the enhancement of skills and competencies to prevent IA (i.e. self-control, emotion regulation, and social interaction) [86], and stressed the need for further assessment of mediating and moderating factors that may influence programme effects [79]. In line with the reviewed studies, the evidence suggests that risk and protective factors have a higher association with IA in young age groups and supports the need to address intrapersonal variables when designing interventions: escapism, self-identity, attention, control and emotion regulation variables, temperamental characteristics (anger, aggression, addictive proclivity) and negative stress coping [134]; resilience, socio-emotional adjustment and positive developmental transitions (i.e., from adolescence to adulthood) [117]; positive psychology approaches (that increase positive emotions and enhance social competencies [105]; active observation and awareness (facets of mindfulness) [135].
Additional evidence from treatment studies of IA support the approach of strengthening protective factors [136], and minimizing harm-reducing factors [55]: with the use of various techniques such as attention switching (distracting the individual’s attention with other meaningful activities), dissuasion (perception of others as attempting to prevent playing with coaxing, argumentation, etc.), rationalization/education (training to understand impacts of problematic behaviour), parental monitoring (how an individual perceives parental attention on their life - active or passive), resource restriction (the extent to which an individual has been restricted to play in terms of resources, i.e., money or equipment), perceived cost (perception of financial cost involved in the activity) or refraining from engaging [7]. Overall, supporting positive mental health (comprising of both emotional wellbeing and social functioning) in school-based settings, and stressing agency, autonomy and optimism has been a positive proposition [68].
Apart from intrapersonal factors, capitalizing on interpersonal protective factors in IA prevention, such as family involvement and school relations [117] in the design and implementation of interventions, is recommended as being a more effective approach than interventions that focus solely on adolescents [37, 50, 57]. Health promotion is increasingly perceived in an ecological context, related to an individual’s environment, family, social networks, communities and public policies [43]. However, prevention efforts examined in this review are characterized by a lack of this multi-level involvement of stakeholders and have not tapped into family dynamics or the impact of parental monitoring and parental closeness, which has been found to be a protective factor and a major inhibitor of IA [137, 138] and to reduce game playing [55]. On the contrary, poor adolescent–parent relationships have been associated with IA [26]. Evidence from the treatment context demonstrates that multilevel counselling (including counselling, motivational interviewing, family involvement, individual and group therapy) and multi-modal efficacy treatment (employing a variety of therapeutic approaches with the use of family training and/or teacher education) have been found to hold promise for individuals with IA [136]. Therefore, the family has been proposed to be the focus of prevention strategies [139], by utilizing family-centered approaches, parental education, initiatives to improve communication skills with adolescents, promotion of healthy interaction, and helping the family reduce maladaptive family behaviours [140].
Further to protective factors, the studies reviewed aimed at reducing psychosocial difficulties (i.e., motivational levels and social interaction) and comorbid symptoms (i.e. performance anxiety, depression, and procrastination). This is in accordance to IA literature, which emphasizes the strong comorbidity of IA with various disorders (attention deficit hyperactivity disorder, anxiety, and depression) [141] and the association with psychosocial problems. The prospective study of Lindenberg [77] utilizes therapeutic techniques, such as cognitive-behavioural approaches to address cognitive biases (i.e., the vicious cycle of Internet use reinforced by operant conditioning) and behaviour modification (i.e., problem solving and contingency management). Cognitive mechanisms (i.e., stonewalling, minimizing, blaming, excusing, and rationalizing) have been suggested to be implicated in IA [89], and CBT has been proposed as the most effective form of treatment for IA [29, 142], therefore applying therapeutic techniques for at-risk individuals may be a promising approach.
4.4. Multi-behaviour, Health-promoting Focus
The shared underlying determinants, the protective and harm-reducing factors of risk behaviours in young people and the ensuing clustering of risk behaviours has driven the prevention field to integrate practices employing a more holistic, multi-behavioural approach in prevention. Risk behaviours appear to be interrelated and according to de Leeuw and colleagues [6] and other authors [48], heavy Internet and game use and the respective psychosocial problems are not separate concerns, but are concomitant with other health issues interacting synergistically, indicating that prevention programmes should address related health problems. Sharing common goals (e.g., developing refusal skills, coping with emotions and inhibitions, considering long-term consequences, and increasing awareness) relevant risk areas (i.e., risk behaviours such as drug and alcohol use, gambling, and gaming) can be thematically integrated [117, 143] and delivered as a broader prevention curriculum that also bears academic performance benefits. This rationale was adopted by the school-based multi-risk behaviour Project P.A.T.H.S. [81] and the multi-addiction programme B.E.S.T. [86].
Treatment and prevention strategies that target both problematic Internet use (PIU) and other problem behaviours, such as problem gambling [144], have been suggested to synergistically improve multiple health outcomes, leading to a reduction of risk-taking behaviours in adolescence [50, 145].
An inherent limitation of school-based programmes is the lack of assessment/screening data at a school level [82, 146] and the practical difficulty in promoting selective prevention for at-risk and/or addicted adolescents [50]. Also, there is a lack of systematic prevention curricula in Western societies, aiming to endorse an understanding for IA impacts and potential risks, despite the arguably alarming prevalence rates worldwide. Therefore, an interesting challenge is for researchers to assess the role that the school could play in the future as part of an overall systemic approach towards IA, co-attending to the specific prevention or therapeutic needs for at-risk adolescents and addressing challenges presented in methodology and implementation [147, 150].
CONCLUSION
With an ever-growing reliance on technological media for information, work, leisure, shopping, and communication, the online environment is increasingly meeting adolescent needs, and the need to balance technology use from an early age is growing. The present review provided insights on current evidence of school-based prevention initiatives for IA, the variety of the approaches employed, and their respective effectiveness. Findings emphasize the scarcity of prevention research. Future research should include RCTs using rigorous methodological designs to provide evidence-based recommendations. Such studies add to a growing body of evidence, which may have a considerable impact on the formulation of health and education policies, as well as on guidelines for schools and parental monitoring. More specifically, future research is needed to provide further insight into mediating and moderating variables, protective and harm-reducing factors, and focus on the needs of the stakeholders to formulate the design of interventions.
Additionally, reaching a consensus regarding the definition, clinical status and assessment of IA, gaming addiction and social media addiction would upgrade prevention efforts targeting adolescents significantly as it will allow comparisons between intervention studies and the identification of factors that are critical in such interventions. Validated findings could then inform promising strategies for IA prevention. Researchers and mental health professionals are increasingly acknowledging the necessity of developing and using prevention approaches, and it is timely that IA is recognized as a problematic condition for a minority of users and addressed within public health and education policy.
ACKNOWLEDGEMENTS
Declared none.
CONSENT FOR PUBLICATION
Not applicable.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
REFERENCES
- 1.Dreier M., Wölfling K., Beutel M.E., Müller K.W. Prävention der internetsucht: Workshops für kinder und jugendliche mit digitalen methodenkoffern. Padiatr. Padol. 2015;50(5):200–205. [http://dx.doi.org/10.1007/s00608-015-0308-x]. [Google Scholar]
- 2.Kuss D.J., Griffiths M.D. Online social networking and addiction--a review of the psychological literature. Int. J. Environ. Res. Public Health. 2011;8(9):3528–3552. doi: 10.3390/ijerph8093528. [http://dx.doi.org/10.3390/ ijerph8093528]. [PMID: 22016701]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boyd D. It’s complicated: the social lives of networked teens. Yale, CT, USA: Yale University Press; 2014. [Google Scholar]
- 4.Kuss D.J., Griffiths M.D., Karila L., Billieux J. Internet addiction: a systematic review of epidemiological research for the last decade. Curr. Pharm. Des. 2014;20(25):4026–4052. doi: 10.2174/13816128113199990617. [http://dx. doi.org/10.2174/13816128113199990617]. [PMID: 24001297]. [DOI] [PubMed] [Google Scholar]
- 5.Kaess M., Parzer P., Brunner R., Koenig J., Durkee T., Carli V., Wasserman C., Hoven C.W., Sarchiapone M., Bobes J., Cosman D., Värnik A., Resch F., Wasserman D. Pathological internet use is on the rise among european adolescents. J. Adolesc. Health. 2016;59(2):236–239. doi: 10.1016/j.jadohealth.2016.04.009. [http://dx.doi.org/10.1016/j.jadohealth. 2016.04.009]. [PMID: 27267140]. [DOI] [PubMed] [Google Scholar]
- 6.de Leeuw J.R.J., de Bruijn M., de Weert-van Oene G.H., Schrijvers A.J. Internet and game behaviour at a secondary school and a newly developed health promotion programme: a prospective study. BMC Public Health. 2010;10:544. doi: 10.1186/1471-2458-10-544. [http://dx.doi.org/10. 1186/1471-2458-10-544]. [PMID: 20828394]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pontes H.M., Kuss D.J., Griffiths M.D. Clinical psychology of Internet addiction: a review of its conceptualization, prevalence, neuronal processes, and implications for treatment. Neurosci. Neuroecon. 2015;4:11–23. [Google Scholar]
- 8.Kuss D.J., van Rooij A.J., Shorter G.W., Griffiths M.D., van de Mheen D. Internet addiction in adolescents: Prevalence and risk factors. Comput. Human Behav. 2013;29(5):1987–1996. [http:// dx.doi.org/10.1016/j.chb.2013.04.002]. [Google Scholar]
- 9.Kuss D.J., Shorter G.W., van Rooij A.J., van de Mheen D., Griffiths M.D. The Internet addiction components model and personality: Establishing construct validity via a nomological network. Comput. Human Behav. 2014;39:312–321. [http://dx.doi.org/10. 1016/j.chb.2014.07.031]. [Google Scholar]
- 10.Griffiths M.D., Davies M.N.O., Chappell D. Online computer gaming: A comparison of adolescent and adult gamers. J. Adolesc. 2004;27(1):87–96. doi: 10.1016/j.adolescence.2003.10.007. [http://dx.doi.org/10.1016/j.adolescence.2003. 10.007]. [PMID: 15013262]. [DOI] [PubMed] [Google Scholar]
- 11.Griffiths M.D., Kuss D.J. Adolescent social networking: should parents and teachers be worried? Educ. Health. 2011;29(2):23–25. [Google Scholar]
- 12.Kuss D.J., Griffiths M.D. Online gaming addiction in children and adolescents: A review of empirical research. J. Behav. Addict. 2012;1(1):3–22. doi: 10.1556/JBA.1.2012.1.1. [http://dx.doi.org/10.1556/JBA.1.2012.1.1]. [PMID: 26166826]. [DOI] [PubMed] [Google Scholar]
- 13.Gámez-Guadix M. Depressive symptoms and problematic internet use among adolescents: Analysis of the longitudinal relationships from the cognitive-behavioral model. Cyberpsychol. Behav. Soc. Netw. 2014;17(11):714–719. doi: 10.1089/cyber.2014.0226. [http://dx.doi.org/10.1089/cyber. 2014.0226]. [PMID: 25405784]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schou Andreassen C., Billieux J., Griffiths M.D., Kuss D.J., Demetrovics Z., Mazzoni E., Pallesen S. The relationship between addictive use of social media and video games and symptoms of psychiatric disorders: A large-scale cross-sectional study. Psychol. Addict. Behav. 2016;30(2):252–262. doi: 10.1037/adb0000160. [http://dx.doi.org/ 10.1037/adb0000160]. [PMID: 26999354]. [DOI] [PubMed] [Google Scholar]
- 15.Kuss D.J., Griffiths M.D. Social networking sites and addiction: Ten lessons learned. Int. J. Environ. Res. Public Health. 2017;14(3):311–327. doi: 10.3390/ijerph14030311. [http://dx.doi.org/10.3390/ijerph14030311]. [PMID: 28304359]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seo D.G., Park Y., Kim M.K., Park J. Mobile phone dependency and its impacts on adolescents’ social and academic behaviors. Comput. Human Behav. 2016;63:282–292. [http://dx.doi.org/10. 1016/j.chb.2016.05.026]. [Google Scholar]
- 17.Kirschner P.A., Karpinski A.C. Facebook® and academic performance. Online Interactivity: Role Technol. Behav. Change. 2010;26(6):1237–1245. [Google Scholar]
- 18.Kaltiala-Heino R., Lintonen T., Rimpelä A. Internet addiction? Potentially problematic use of the Internet in a population of 12–18 year-old adolescents. Addict. Res. Theory. 2004;12(1):89–96. [http://dx.doi.org/10.1080/1606635031000098796]. [Google Scholar]
- 19.Kuss D.J., Griffiths M.D. Adolescent online gaming addiction. Educ. Health. 2012;30(1):15–17. doi: 10.1556/JBA.1.2012.1.1. [DOI] [PubMed] [Google Scholar]
- 20.Developing adolescents: A reference for professionals. Washington, D.C.: American Psychological Association; 2002. [Google Scholar]
- 21.Leather N.C. Risk-taking behaviour in adolescence: a literature review. J. Child Health Care. 2009;13(3):295–304. doi: 10.1177/1367493509337443. [http://dx.doi. org/10.1177/1367493509337443]. [PMID: 19713410]. [DOI] [PubMed] [Google Scholar]
- 22.Chambers R.A., Taylor J.R., Potenza M.N. Developmental neurocircuitry of motivation in adolescence: A critical period of addiction vulnerability. Am. J. Psychiatry. 2003;160(6):1041–1052. doi: 10.1176/appi.ajp.160.6.1041. [http://dx.doi.org/10.1176/appi.ajp.160.6.1041]. [PMID: 12777258]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pavis S., Cunningham-Burley S., Amos A. Health related behavioural change in context: Young people in transition. Soc. Sci. Med. 1998;47(10):1407–1418. doi: 10.1016/s0277-9536(98)00257-3. [http://dx.doi.org/10.1016/S0277-9536(98)00257-3]. [PMID: 9823037]. [DOI] [PubMed] [Google Scholar]
- 24.Liu Q-X., Fang X-Y., Wan J-J., Zhou Z-K. Need satisfaction and adolescent pathological internet use: Comparison of satisfaction perceived online and offline. Comput. Human Behav. 2016;55:695–700. [http://dx.doi.org/10.1016/j.chb.2015.09.048]. [Google Scholar]
- 25.Liu Y., Liu R-D., Ding Y., Wang J., Zhen R., Xu L. How online basic psychological need satisfaction influences self-disclosure online among chinese adolescents: Moderated mediation effect of exhibitionism and narcissism. Front. Psychol. 2016;7:1279. doi: 10.3389/fpsyg.2016.01279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Soh P.C-H., Charlton J.P., Chew K-W. The influence of parental and peer attachment on internet usage motives and addiction. First Monday. 2014;19(7) http://firstmonday.org/ojs/index.php/fm/article/ view/5099 [Online]. [http://dx.doi.org/10.5210/fm.v19i7.5099]. [Google Scholar]
- 27.Esen B.K. Adolescents’ internet addiction is predicted by peer pressure and perceived social support. Educ. Sci. 2009;4(4):1331–1340. [Google Scholar]
- 28.Berdibayeva S., Garber A., Ivanov D., Massalimova A., Kukubayeva A., Berdibayev S. Psychological Prevention of older Adolescents’ Interpersonal Relationships, Who are Prone to Internet Addiction. Procedia Soc. Behav. Sci. 2016;217:984–989. [http:// dx.doi.org/10.1016/j.sbspro.2016.02.081]. [Google Scholar]
- 29.King D.L., Delfabbro P.H., Griffiths M.D. Clinical interventions for technology-based problems: Excessive internet and video game use. J. Cogn. Psychother. 2012;26(1):43–56. [http://dx.doi.org/10. 1891/0889-8391.26.1.43]. [Google Scholar]
- 30.Chun J., Shim H., Kim S. A meta-analysis of treatment interventions for internet addiction among Korean adolescents. Cyberpsychology Behav. Soc. Netw. 2017;20(4):225–231. doi: 10.1089/cyber.2016.0188. Available from: http://online.liebertpub.com/doi/10. [DOI] [PubMed] [Google Scholar]
- 31.Khazaal Y., Xirossavidou C., Khan R., Edel Y., Zebouni F., Zullino D. Cognitive-behavioral treatments for internet addiction. Open Addict. J. 2012;5(1):30–35. [http://dx.doi.org/10.2174/ 1874941001205010030]. [Google Scholar]
- 32.King D.L., Delfabbro P.H. Internet gaming disorder treatment: A review of definitions of diagnosis and treatment outcome. J. Clin. Psychol. 2014;70(10):942–955. doi: 10.1002/jclp.22097. [http://dx.doi.org/10.1002/ jclp.22097]. [PMID: 24752874]. [DOI] [PubMed] [Google Scholar]
- 33.Day I. A family systems approach to the understanding and treatment of internet gaming disorder. Fam. J. (Alex. Va.) 2017;25(3):264–270. [http://dx.doi.org/10.1177/1066480717711108]. [Google Scholar]
- 34.Young K.S. CBT-IA: The first treatment model for internet addiction. J. Cogn. Psychother. 2011;25(4):304–312. [http://dx. doi.org/10.1891/0889-8391.25.4.304]. [Google Scholar]
- 35.King D.L., Delfabbro P.H., Griffiths M.D., Gradisar M. Assessing clinical trials of Internet addiction treatment: A systematic review and CONSORT evaluation. Clin. Psychol. Rev. 2011;31(7):1110–1116. doi: 10.1016/j.cpr.2011.06.009. [http://dx.doi.org/10.1016/j.cpr.2011.06.009]. [PMID: 21820990]. [DOI] [PubMed] [Google Scholar]
- 36.Turel O., Mouttapa M., Donato E. Preventing problematic Internet use through video-based interventions: A theoretical model and empirical test. Behav. Inf. Technol. 2015;34(4):349–362. [http:// dx.doi.org/10.1080/0144929X.2014.936041]. [Google Scholar]
- 37.Tsitsika A., Janikian M., Greydanus D.E., Omar H.A., Merrick J. A new millennium: A new age of behavioral disorders? Intl. J. Child Adolesc. Health. 2013;6(4):363–366. [Google Scholar]
- 38.Guidelines for prevention in psychology. Am. Psychol. 2014;69(3):285–296. doi: 10.1037/a0034569. [http://dx.doi.org/10.1037/a0034569]. [PMID: 24188360]. [DOI] [PubMed] [Google Scholar]
- 39.Defining the scope of prevention.O’Connell, M.E.; Boat, T.; Warner, K.E., Eds.; Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities; National Academies Press: US. 2009 https://www.ncbi.nlm.nih.gov/books/ NBK32789/ online. [PubMed]
- 40.Caplan G. Principles of preventive psychiatry. New York: Basic Books; 1964. [Google Scholar]
- 41.Gordon R.S., Jr An operational classification of disease prevention. Public Health Rep. 1983;98(2):107–109. [PMID: 6856733]. [PMC free article] [PubMed] [Google Scholar]
- 42.Prevention and promotion in mental health: evidence and research; Geneva, 2002. pp. 1–46. [Google Scholar]
- 43.Kok G., Schaalma H., Ruiter R.A.C., van Empelen P., Brug J. Intervention mapping: protocol for applying health psychology theory to prevention programmes. J. Health Psychol. 2004;9(1):85–98. doi: 10.1177/1359105304038379. [http://dx.doi.org/10.1177/1359105304038379]. [PMID: 14683571]. [DOI] [PubMed] [Google Scholar]
- 44.Gupta R., Derevensky J.L. An empirical examinination of Jacobs’ general theory of addictions: Do adolescent gamblers fit the theory? J. Gambl. Stud. 1998;14(1):17–49. doi: 10.1023/a:1023046509031. [http://dx.doi.org/10. 1023/A:1023046509031]. [PMID: 12766433]. [DOI] [PubMed] [Google Scholar]
- 45.Rutter H., Glonti K. Towards a new model of evidence for public health. Lancet. 2016;388(2):S7. [http://dx.doi.org/10.1016/S0140-6736(16)32243-7]. [Google Scholar]
- 46.Craig P., Dieppe P., Macintryre S., Michie S., Nazareth I., Petticrew M. Developing and evaluating complex interventions: New guidance. Med. Res. Counc. 2008:1–39. doi: 10.1136/bmj.a1655. Available from https://www.mrc.ac.uk/documents/pdf/complex-interventions-guidance/ [ cited Oct 15, 2016] [DOI] [PMC free article] [PubMed]
- 47.Livingstone S., Haddon L., Görzig A., Ólafsson K. Risks and safety on the internet: The perspective of European children. Full Findings. LSE. London: EU Kids Online; 2011. pp. 9–16. [Google Scholar]
- 48.Busch V., De Leeuw R.J.J., Schrijvers A.J.P. Results of a multibehavioral health-promoting school pilot intervention in a Dutch secondary school. J. Adolesc. Health. 2013;52(4):400–406. doi: 10.1016/j.jadohealth.2012.07.008. [http:// dx.doi.org/10.1016/j.jadohealth.2012.07.008]. [PMID: 23299009]. [DOI] [PubMed] [Google Scholar]
- 49.Shek D.T.L., Leung H. Development of an integrated intervention model for Internet addiction in Hong Kong. Intl. J. Child Adolesc. Health. 2013;6(4):475–486. [Google Scholar]
- 50.Vondráčková P., Gabrhelík R. Prevention of Internet addiction: A systematic review. J. Behav. Addict. 2016;5(4):568–579. doi: 10.1556/2006.5.2016.085. [http://dx.doi.org/10.1556/2006.5.2016.085]. [PMID: 27998173]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bányai F., Zsila Á., Király O., Maraz A., Elekes Z., Griffiths M.D., Andreassen C.S., Demetrovics Z. Problematic social media use: Results from a large-scale nationally representative adolescent sample. PLoS One. 2017;12(1):e0169839. doi: 10.1371/journal.pone.0169839. [http://dx.doi.org/10. 1371/journal.pone.0169839]. [PMID: 28068404]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wartberg L., Kriston L., Kramer M., Schwedler A., Lincoln T.M., Kammerl R. Internet gaming disorder in early adolescence: Associations with parental and adolescent mental health. Eur. Psychiatry. 2017;43:14–18. doi: 10.1016/j.eurpsy.2016.12.013. [Online]. [http://dx.doi.org/10.1016/j. eurpsy.2016.12.013]. [PMID: 28365463]. [DOI] [PubMed] [Google Scholar]
- 53.Griffin K.W., Botvin G.J. Evidence-based interventions for preventing substance use disorders in adolescents. Child Adolesc. Psychiatr. Clin. N. Am. 2010;19(3):505–526. doi: 10.1016/j.chc.2010.03.005. [http://dx.doi.org/ 10.1016/j.chc.2010.03.005]. [PMID: 20682218]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hagger M.S., Wong G.G., Davey S.R. A theory-based behavior-change intervention to reduce alcohol consumption in undergraduate students: Trial protocol. BMC Public Health. 2015;15:306. doi: 10.1186/s12889-015-1648-y. [http://dx.doi.org/10.1186/s12889-015-1648-y]. [PMID: 25886281]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Xu Z., Turel O., Yuan Y. Online game addiction among adolescents: motivation and prevention factors. Eur. J. Inf. Syst. 2012;21:321–340. [http://dx.doi.org/10.1057/ejis.2011.56]. [Google Scholar]
- 56.Yeun Y.R., Han S.J. Effects of psychosocial interventions for school-aged children’s internet addiction, self-control and self-esteem: Meta-analysis. Healthc. Inform. Res. 2016;22(3):217–230. doi: 10.4258/hir.2016.22.3.217. [http://dx.doi.org/10.4258/hir.2016.22.3.217]. [PMID: 27525163]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Romano J.L. Prevention in the twenty-first century: promoting health and well-being in education and psychology. Asia Pac. Educ. Rev. 2014;15(3):417–426. [http://dx.doi.org/10.1007/s12564-014-9327-8]. [Google Scholar]
- 58.Caulkins J.P., Pacula R.L., Paddock S., Chiesa J. 2002 https://www.rand.org/pubs/monograph_reports/MR1459.html
- 59.Newton N.C., Andrews G., Teesson M., Vogl L.E. Delivering prevention for alcohol and cannabis using the Internet: A cluster randomised controlled trial. Prev. Med. 2009;48(6):579–584. doi: 10.1016/j.ypmed.2009.04.009. [http://dx.doi.org/10.1016/j.ypmed.2009.04.009]. [PMID: 19389420]. [DOI] [PubMed] [Google Scholar]
- 60.Walther B., Hanewinkel R., Morgenstern M. Short-term effects of a school-based program on gambling prevention in adolescents. J. Adolesc. Health. 2013;52(5):599–605. doi: 10.1016/j.jadohealth.2012.11.009. [http://dx.doi.org/ 10.1016/j.jadohealth.2012.11.009]. [PMID: 23375824]. [DOI] [PubMed] [Google Scholar]
- 61.Alavi S.S., Ferdosi M., Jannatifard F., Eslami M., Alaghemandan H., Setare M. Behavioral addiction versus substance addiction: Correspondence of psychiatric and psychological views. Int. J. Prev. Med. 2012;3(4):290–294. [PMID: 22624087]. [PMC free article] [PubMed] [Google Scholar]
- 62.Kuss D.J., Griffiths M.D. Internet and gaming addiction: a systematic literature review of neuroimaging studies. Brain Sci. 2012;2(3):347–374. doi: 10.3390/brainsci2030347. [http://dx.doi.org/10.3390/brainsci2030347]. [PMID: 24961198]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sussman S., Leventhal A., Bluthenthal R.N., Freimuth M., Forster M., Ames S.L. A framework for the specificity of addictions. Int. J. Environ. Res. Public Health. 2011;8(8):3399–3415. doi: 10.3390/ijerph8083399. [http:// dx.doi.org/10.3390/ijerph8083399]. [PMID: 21909314]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dickson L.M., Derevensky J.L., Gupta R. Harm reduction for the prevention of youth gambling problems: Lessons learned from adolescent high-risk behavior prevention programs. J. Adolesc. Res. 2004;19(2):233–263. [http://dx.doi.org/10.1177/0743558403258272]. [Google Scholar]
- 65.Tobler N.S., Roona M.R., Ochshorn P., Marshall D.G., Streke A.V., Stackpole K.M. School-Based adolescent drug prevention programs: 1998 Meta-Analysis. J. Prim. Prev. 2000;20(4):275–336. [http://dx.doi.org/10.1023/A:1021314704811]. [Google Scholar]
- 66.Todirita I.R., Lupu V. Gambling prevention program among children. J. Gambl. Stud. 2013;29(1):161–169. doi: 10.1007/s10899-012-9293-1. [http://dx.doi.org/ 10.1007/s10899-012-9293-1]. [PMID: 22314758]. [DOI] [PubMed] [Google Scholar]
- 67.Durlak J.A., Wells A.M. Primary prevention mental health programs for children and adolescents: A meta-analytic review. Am. J. Community Psychol. 1997;25(2):115–152. doi: 10.1023/a:1024654026646. [http://dx.doi.org/10. 1023/A:1024654026646]. [PMID: 9226860]. [DOI] [PubMed] [Google Scholar]
- 68.Wells J., Barlow J., Stewart‐Brown S. A systematic review of universal approaches to mental health promotion in schools. Health Educ. 2003;103(4):197–220. [http://dx.doi.org/10.1108/ 09654280310485546]. [Google Scholar]
- 69.Das J.K., Salam R.A., Lassi Z.S., Khan M.N., Mahmood W., Patel V., Bhutta Z.A. Interventions for adolescent mental health: An overview of systematic reviews. J. Adolesc. Health. 2016;59(4S):S49–S60. doi: 10.1016/j.jadohealth.2016.06.020. [http://dx.doi.org/10.1016/j.jadohealth.2016.06. 020]. [PMID: 27664596]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Soole D.W., Mazerolle L., Rombouts S. School-based drug prevention programs: A review of what works. Aust. N. Z. J. Criminol. 2008;41(2):259–286. [http://dx.doi.org/10.1375/acri.41.2.259]. [Google Scholar]
- 71.Young K.S. The evolution of Internet addiction. Addict. Behav. 2017;64:229–230. doi: 10.1016/j.addbeh.2015.05.016. [http://dx.doi.org/10.1016/j.addbeh.2015.05. 016]. [PMID: 26059165]. [DOI] [PubMed] [Google Scholar]
- 72.Cho C. South Korea’s efforts to prevent internet addiction. The Cambridge Handbook of International Prevention Science. Cambridge: Cambridge University Press; 2016. pp. 551–571. [Google Scholar]
- 73.King D.L., Delfabbro P.H., Doh Y.Y., Wu A.M., Kuss D.J., Pallesen S., Mentzoni R., Carragher N., Sakuma H. Policy and prevention approaches for disordered and hazardous gaming and internet use: An international perspective. Prev. Sci. 2018;19(2):233–249. doi: 10.1007/s11121-017-0813-1. [PMID: 28677089]. [DOI] [PubMed] [Google Scholar]
- 74.Saturni S., Bellini F., Braido F., Paggiaro P., Sanduzzi A., Scichilone N., Santus P.A., Morandi L., Papi A. Randomized controlled trials and real life studies. Approaches and methodologies: A clinical point of view. Pulm. Pharmacol. Ther. 2014;27(2):129–138. doi: 10.1016/j.pupt.2014.01.005. [http://dx.doi.org/10.1016/j.pupt.2014.01.005]. [PMID: 24468677]. [DOI] [PubMed] [Google Scholar]
- 75.Torgerson C.J., Torgerson D.J. 2013 https://www.researchgate. net/profile/David_Torgerson/publication/273421357_Randomised_trials_in_education_An_introductory_handbook/links/55d5f3be08 aec156b9a6fe06.pdf
- 76.Shapira N.A., Lessig M.C., Goldsmith T.D., Szabo S.T., Lazoritz M., Gold M.S., Stein D.J. Problematic internet use: proposed classification and diagnostic criteria. Depress. Anxiety. 2003;17(4):207–216. doi: 10.1002/da.10094. [http://dx.doi.org/10.1002/da.10094]. [PMID: 12820176]. [DOI] [PubMed] [Google Scholar]
- 77.Lindenberg K., Halasy K., Schoenmaekers S. A randomized efficacy trial of a cognitive-behavioral group intervention to prevent internet use disorder onset in adolescents: The PROTECT study protocol. Contemp. Clin. Trials Commun. 2017;6:64–71. doi: 10.1016/j.conctc.2017.02.011. [http://dx.doi.org/10.1016/j.conctc.2017.02.011]. [PMID: 29740637]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Korkmaz M., Kiran-Esen B. The effects of peer-training about secure internet use on adolescents.Turk Psychol Couns Guid J [Internet]. 2012;4(38):180–7. Available from: http://dergipark.gov.tr/download/article-file/200072. [Google Scholar]
- 79.Walther B., Hanewinkel R., Morgenstern M. Effects of a brief school-based media literacy intervention on digital media use in adolescents: cluster randomized controlled trial. Cyberpsychol. Behav. Soc. Netw. 2014;17(9):616–623. doi: 10.1089/cyber.2014.0173. [http://dx.doi.org/10.1089/ cyber.2014.0173]. [PMID: 25126888]. [DOI] [PubMed] [Google Scholar]
- 80.Shek D.T.L., Ma C.M.S. Effectiveness of a Chinese positive youth development program: The Project P.A.T.H.S. in Hong Kong. Int. J. Disabil. Hum. Dev. 2014;13(4):489–496. http://www. degruyter.com/view/j/ijdhd.2014.13.issue-4/ijdhd-2014-0346/ijdhd-2014-0346.xml [online]. [http://dx.doi.org/10.1515/ijdhd-2014-0346]. [Google Scholar]
- 81.Shek D.T.L., Ma H.K., Sun R.C.F. Development of a new curriculum in a positive youth development program: the project P.A.T.H.S. in Hong Kong. ScientificWorldJournal. 2011;11:2207–2218. doi: 10.1100/2011/289589. [http://dx.doi.org/10.1100/2011/289589]. [PMID: 22125468]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Andrisano-Ruggieri R., Santoro E., De Caro F., Palmieri L., Capunzo M., Venuleo C., Giovanni B. Internet addiction: a prevention action-research intervention. Epidemiol Biostat Public Health [Internet]. 2016;13(3):1–5. http://ebph.it/article/view/11817 [cited 2017 Mar 6] [Google Scholar]
- 83.Ma H.K., Chu M.K.Y., Chan W.W.Y. Construction of a teaching package on promoting prosocial internet use and preventing antisocial Internet use. ScientificWorldJournal. 2011;11:2136–2146. doi: 10.1100/2011/672898. [http://dx. doi.org/10.1100/2011/672898]. [PMID: 22125462]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gluud L.L. Bias in clinical intervention research. Am. J. Epidemiol. 2006;163(6):493–501. doi: 10.1093/aje/kwj069. [http://dx.doi.org/10.1093/aje/kwj069]. [PMID: 16443796]. [DOI] [PubMed] [Google Scholar]
- 85.Hswen Y., Rubenzahl L., Bickham D.S. Feasibility of an online and mobile videogame curriculum for teaching children safe and healthy cellphone and internet behaviors. Games Health J. 2014;3(4):252–259. doi: 10.1089/g4h.2013.0074. [http://dx.doi.org/10.1089/g4h.2013.0074]. [PMID: 26192373]. [DOI] [PubMed] [Google Scholar]
- 86.Shek D.T.L., Yu L., Leung H., Wu F.K.Y., Law M.Y.M. Development, implementation, and evaluation of a multi-addiction prevention program for primary school students in Hong Kong: the B.E.S.T. Teen program. Asian J. Gambl. Issues Public Health. 2016;6:5. doi: 10.1186/s40405-016-0014-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Shek D.T.L., Yu L. A review of validated youth prevention and positive youth development programs in Asia. Int. J. Adolesc. Med. Health. 2011;23(4):317–324. doi: 10.1515/ijamh.2011.028. [http://dx.doi.org/10.1515/IJAMH. 2011.028]. [PMID: 22416499]. [DOI] [PubMed] [Google Scholar]
- 88.The American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). 5th ed. USA: American Psychiatric Publishing; 2013. [Google Scholar]
- 89.Young K.S. Caught in the net: How to recognize the signs of internet addiction– and a winning strategy for recovery. 1st ed. New York, NY, USA: John Wiley & Sons, Inc; 1998. [Google Scholar]
- 90.Young K.S. Internet addiction: The emergence of a new clinical disorder. Cyberpsychol. Behav. 1998;1(3):237–244. [http://dx.doi. org/10.1089/cpb.1998.1.237]. [Google Scholar]
- 91.Meerkerk G-J., Van Den Eijnden R.J., Vermulst A.A., Garretsen H.F.L. The compulsive internet use scale (CIUS): some psychometric properties. Cyberpsychol. Behav. 2009;12(1):1–6. doi: 10.1089/cpb.2008.0181. [http:// dx.doi.org/10.1089/cpb.2008.0181]. [PMID: 19072079]. [DOI] [PubMed] [Google Scholar]
- 92.Rumpf H.J., Meyer C., John U. Prävalenz der Internetabhängigkeit. Berlin: PINTA; 2011. pp. 1–21. [Google Scholar]
- 93.Rehbein F., Baier D., Kleimann M., Mößle T. Computerspielabhängigkeitsskala (CSAS): Ein Verfahren zur Erfassung der Internet Gaming Disorder nach DSM-5. Göttingen, Bern, Wien: Hogrefe; 2015. [Google Scholar]
- 94.Rehbein F., Kleimann M., Mössle T. Prevalence and risk factors of video game dependency in adolescence: results of a German nationwide survey. Cyberpsychol. Behav. Soc. Netw. 2010;13(3):269–277. doi: 10.1089/cyber.2009.0227. [http://dx.doi.org/10.1089/cyber.2009.0227]. [PMID: 20557246]. [DOI] [PubMed] [Google Scholar]
- 95.Hahn A., Jerusalem M. Internet addiction - reliability and validity in online research.Online-Marktforschung: Beitrage aus Wissenschaft und Praxis. Wiesbaden: Gabler; 2001. pp. 211–234. [http:// dx.doi.org/10.1007/978-3-322-99429-5_15] [Google Scholar]
- 96.Van Rooij A.J. Online video game addiction.Exploring a new phenomenon. Erasmus Universiteit: The Netherlands, May. 2011. [Google Scholar]
- 97.Stiensmeier-Pelster J., Braune-Krickau M., Schürmann M., Duda K. DIKJ: Manual. 3rd ed. Gött Hogrefe; 2014. [Google Scholar]
- 98.Goodman R., Meltzer H., Bailey V. The strengths and difficulties questionnaire: A pilot study on the validity of the self-report version. Eur. Child Adolesc. Psychiatry. 1998;7(3):125–130. doi: 10.1007/s007870050057. [http://dx.doi.org/10.1007/s007870050057]. [PMID: 9826298]. [DOI] [PubMed] [Google Scholar]
- 99.Döpfner M., Schnabel M., Goletz H., Ollendick T. Phobiefragebogen für Kinder und Jugendliche: PHOKI. Gottingen: Hogreffe; 2006. [Google Scholar]
- 100.Mattick R.P., Clarke J.C. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behav. Res. Ther. 1998;36(4):455–470. doi: 10.1016/s0005-7967(97)10031-6. [http://dx.doi.org/10. 1016/S0005-7967(97)10031-6]. [PMID: 9670605]. [DOI] [PubMed] [Google Scholar]
- 101.Stangier U., Heidenreich T., Berardi A., Golbs U., Hoyer J. Die Erfassung sozialer Phobie durch die Social Interaction Anxiety Scale (SIAS) und die Social Phobia Scale (SPS). Z. Klin. Psychol. Psychother. 1999;28(1):28–36. [http://dx.doi.org/10.1026//0084-5345.28.1.28]. [Google Scholar]
- 102.Grob A., Smolenski C. Fragebogen zur erhebung der emotionsregulation bei kindern und jugendlichen: FEEL-KJ. Manual. 2nd ed. Bern: Huber; 2011. [Google Scholar]
- 103.Höcker A., Engberding M., Rist F. Prokrastination: ein manual zur behandlung des pathologischen aufschiebens. Göttingen: Hogrefe Verlag; 2013. [Google Scholar]
- 104.Petermann U., Petermann F., Lohbeck A. Schülereinschätzliste für Sozial und Lernverhalten: SSL, 2014. [Google Scholar]
- 105.Schwarzer R., Jerusalem M. Generalized self-efficacy scale. Measures in health psychology: A user’s portfolio causal and control beliefs. Windsor, UK: NFER-NELSON; 1995. pp. 35–37. [Google Scholar]
- 106.Topp C.W., Østergaard S.D., Søndergaard S., Bech P. The WHO-5 well-being index: A systematic review of the literature. Psychother. Psychosom. 2015;84(3):167–176. doi: 10.1159/000376585. [http://dx.doi.org/ 10.1159/000376585]. [PMID: 25831962]. [DOI] [PubMed] [Google Scholar]
- 107.Busiol D., Lee T.Y. Student Well-Being in Chinese Adolescents in Hong Kong. 2015 http://link.springer.com/chapter/10.1007/978-981-287-582-2_14
- 108.Shek D.T.L., Yu L. Prevention of adolescent problem behavior: longitudinal impact of the Project P.A.T.H.S. in Hong Kong. ScientificWorldJournal. 2011;11:546–567. doi: 10.1100/tsw.2011.33. [http://dx.doi.org/10.1100/tsw.2011.33]. [PMID: 21403974]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Yu L., Shek D.T.L. Internet addiction in Hong Kong adolescents: A three-year longitudinal study. J. Pediatr. Adolesc. Gynecol. 2013;26(3) Suppl.:S10–S17. doi: 10.1016/j.jpag.2013.03.010. [http://dx.doi.org/10.1016/j.jpag. 2013.03.010]. [PMID: 23683821]. [DOI] [PubMed] [Google Scholar]
- 110.Deng L., Fang X., Liu C., Lan J., Zhang J., Liu Q-X. The pilot exploration of psycho-education on adolescent internet addiction prevention. Psychol. Res. 2013:1. [Google Scholar]
- 111.Joo A., Park I. Effects of an empowerment education program in the prevention of internet games addiction in middle school students. J. Korean Acad. Nurs. 2010;40(2):255–263. doi: 10.4040/jkan.2010.40.2.255. http://search. ebscohost.com/login.aspx?direct=true&profile=ehost&scope=site [DOI] [PubMed] [Google Scholar]
- 112.Kim M.S., Choi E.M., Lee S.H., Bae J.H. Development and preliminary outcome study of smartphone overuse prevention education program for adolescents of middle school. J. Korea Soc. IT Serv. 2013;12(4):307–318. [http://dx.doi.org/10.9716/KITS.2013. 12.4.307]. [Google Scholar]
- 113.Kim S.J., Lee C.S., Kweon Y.R., Choi B.S. Effects of online game addiction prevention program for middle school students in South Korean urban ity.Presentation presented at: Children’s Mental Health. 2007. [Google Scholar]
- 114.Mun S.Y., Lee B.S. Effects of an integrated internet addiction prevention program on elementary students’ self-regulation and internet addiction. J. Korean Acad. Nurs. 2015;45(2):251–261. doi: 10.4040/jkan.2015.45.2.251. [http://dx.doi.org/10.4040/jkan.2015.45.2.251]. [PMID: 25947187]. [DOI] [PubMed] [Google Scholar]
- 115.Park G.R., Kim H.S. J. Korean Acad. Nurs. 2011;41(5):694–703. doi: 10.4040/jkan.2011.41.5.694. [Effects of a group counseling integration program on self-determination and Internet addiction in high school students with tendency to Internet addiction]. [http://dx.doi.org/10.4040/jkan.2011. 41.5.694]. [PMID: 22143218]. [DOI] [PubMed] [Google Scholar]
- 116.Lim S.S. Regulatory initiatives for managing online risks and opportunities for youths – the East Asian experience. MWalrave Ed. E-Youth Balanc. Oppor Risks. 2012:271–290. [Google Scholar]
- 117.Jackson C.A., Henderson M., Frank J.W., Haw S.J. An overview of prevention of multiple risk behaviour in adolescence and young adulthood. J. Public Health (Oxf.) 2012;34(Suppl. 1):i31–i40. doi: 10.1093/pubmed/fdr113. [http://dx.doi.org/10.1093/pubmed/fdr113]. [PMID: 22363029]. [DOI] [PubMed] [Google Scholar]
- 118.Grant J.E., Potenza M.N., Weinstein A., Gorelick D.A. Introduction to behavioral addictions. Am. J. Drug Alcohol Abuse. 2010;36(5):233–241. doi: 10.3109/00952990.2010.491884. [http://dx.doi.org/10.3109/00952990.2010.491884]. [PMID: 20560821]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Griffiths M.D., Kuss D.J., Billieux J., Pontes H.M. The evolution of Internet addiction: A global perspective. Addict. Behav. 2016;53:193–195. doi: 10.1016/j.addbeh.2015.11.001. [http://dx.doi.org/10.1016/j.addbeh.2015.11.001]. [PMID: 26562678]. [DOI] [PubMed] [Google Scholar]
- 120.Kuss D.J., Griffiths M.D., Pontes H.M. DSM-5 diagnosis of internet gaming disorder: Some ways forward in overcoming issues and concerns in the gaming studies field. J. Behav. Addict. 2017;6(2):133–141. doi: 10.1556/2006.6.2017.032. [http://dx.doi.org/10.1556/2006.6.2017.032]. [PMID: 28662619]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lortie C.L., Guitton M.J. Internet addiction assessment tools: dimensional structure and methodological status. Addiction. 2013;108(7):1207–1216. doi: 10.1111/add.12202. [http://dx.doi.org/10.1111/add.12202]. [PMID: 23651255]. [DOI] [PubMed] [Google Scholar]
- 122.Kuss D.J., Shorter G.W., van Rooij A.J., Griffiths M.D., Schoenmakers T.M. J. Mental Health Addiction, 2013 http://link.springer.com/10.1007/s11469-013-9459-9
- 123.UK Drug Policy Commission (UKDPC) A fresh approach to drugs: the final report of UK Drug Policy Commission. 2012 www.ukdpc.org.uk
- 124.Ha Y.M., Hwang W.J. Gender differences in internet addiction associated with psychological health indicators among adolescents using a national web-based survey. Int. J. Ment. Health Addict. 2014;12(5):660–669. [http://dx.doi.org/10.1007/s11469-014-9500-7]. [Google Scholar]
- 125.Moore G.F., Audrey S., Barker M., Bond L., Bonell C., Hardeman W., Moore L., O’Cathain A., Tinati T., Wight D., Baird J. Process evaluation of complex interventions: Medical Research Council guidance. BMJ. 2015;350:h1258. doi: 10.1136/bmj.h1258. [http://dx.doi.org/10. 1136/bmj.h1258]. [PMID: 25791983]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Shek D.T.L., Wu F.K.Y. The Project P.A.T.H.S. in Hong Kong: work done and lessons learned in a decade. J. Pediatr. Adolesc. Gynecol. 2016;29(1) Suppl.:S3–S11. doi: 10.1016/j.jpag.2015.10.003. [http://dx.doi.org/10.1016/ j.jpag.2015.10.003]. [PMID: 26461524]. [DOI] [PubMed] [Google Scholar]
- 127.Griffiths M.D., Szabo A. Is excessive online usage a function of medium or activity? An empirical pilot study. J. Behav. Addict. 2014;3(1):74–77. doi: 10.1556/JBA.2.2013.016. [http://dx.doi.org/10.1556/JBA.2.2013.016]. [PMID: 25215216]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Griffiths M.D. The Role of Context in Online Gaming Excess and Addiction: Some Case Study Evidence. Int. J. Ment. Health Addict. 2010;8(1):119–125. [http://dx.doi.org/10.1007/s11469-009-9229-x]. [Google Scholar]
- 129.Colder Carras M., Van Rooij A.J., Van de Mheen D., Musci R., Xue Q-L., Mendelson T. Video gaming in a hyperconnected world: A cross-sectional study of heavy gaming, problematic gaming symptoms, and online socializing in adolescents. Comput. Human Behav. 2017;68:472–479. doi: 10.1016/j.chb.2016.11.060. [http://dx.doi.org/10.1016/j.chb. 2016.11.060]. [PMID: 28260834]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Griffiths M.D., Kuss D.J., Ortiz de Gortari A.B. Videogames as therapy: An updated selective review of the medical and psychological literature. Int. J. Priv. Health Inf. Manage. 2017;5(2):71–96. [http://dx.doi.org/10.4018/IJPHIM.2017070105]. [Google Scholar]
- 131.King D.L., Delfabbro P.H. Defining tolerance in internet gaming disorder: Isn’t it time? Addiction. 2016;111(11):2064–2065. doi: 10.1111/add.13448. [http://dx.doi.org/10.1111/add.13448]. [PMID: 27297731]. [DOI] [PubMed] [Google Scholar]
- 132.King D., Delfabbro P., Griffiths M. The convergence of gambling and digital media: Implications for gambling in young people. J. Gambl. Stud. 2010;26(2):175–187. doi: 10.1007/s10899-009-9153-9. [http://dx.doi.org/10.1007/ s10899-009-9153-9]. [PMID: 19756979]. [DOI] [PubMed] [Google Scholar]
- 133.Koo H.J., Kwon J-H. Risk and protective factors of internet addiction: A meta-analysis of empirical studies in Korea. Yonsei Med. J. 2014;55(6):1691–1711. doi: 10.3349/ymj.2014.55.6.1691. [http://dx.doi.org/10.3349/ymj.2014.55.6. 1691]. [PMID: 25323910]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Khazaei F., Khazaei O., Ghanbari H.B. Positive psychology interventions for internet addiction treatment.Comput Hum Behav [Internet]. 2017;72:304–311. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0747563217301462. [Google Scholar]
- 135.Calvete E., Gámez-Guadix M., Cortazar N. Mindfulness facets and problematic Internet use: A six-month longitudinal study. Addict. Behav [Internet]. 2017;72:57–63. doi: 10.1016/j.addbeh.2017.03.018. http://linkinghub.elsevier.com/retrieve/pii/S0306460317301296 [DOI] [PubMed] [Google Scholar]
- 136.Cash H., Rae C.D., Steel A.H., Winkler A. Internet addiction: A brief summary of research and practice. Curr. Psychiatry Rev. 2012;8(4):292–298. doi: 10.2174/157340012803520513. [http://dx.doi.org/10.2174/157340012803520513]. [PMID: 23125561]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Ding Q., Li D., Zhou Y., Dong H., Luo J. Perceived parental monitoring and adolescent internet addiction: A moderated mediation model. Addict. Behav. 2017;74:48–54. doi: 10.1016/j.addbeh.2017.05.033. [http://dx.doi.org/10. 1016/j.addbeh.2017.05.033]. [PMID: 28575738]. [DOI] [PubMed] [Google Scholar]
- 138.Lin C-H., Lin S-L., Wu C-P. The effects of parental monitoring and leisure boredom on adolescents’ internet addiction. Adolescence. 2009;44(176):993–1004. [PMID: 20432612]. [PubMed] [Google Scholar]
- 139.Flora K. Internet addiction disorder among adolescents and young adults: the picture in Europe and prevention strategies.In: Perspectives on youth: Connections and disconnection [Internet]. Strasburg; 2015:119–32. Available from: https:// hephaestus.nup.ac.cy/handle/11728/82 [cited 2017 Jun 7].
- 140.Yen J-Y., Yen C-F., Chen C-C., Chen S-H., Ko C-H. Family factors of internet addiction and substance use experience in Taiwanese adolescents. Cyberpsychol. Behav. 2007;10(3):323–329. doi: 10.1089/cpb.2006.9948. [http://dx.doi.org/10.1089/cpb.2006.9948]. [PMID: 17594255]. [DOI] [PubMed] [Google Scholar]
- 141.Ho R.C., Zhang M.W., Tsang T.Y., Toh A.H., Pan F., Lu Y., Cheng C., Yip P.S., Lam L.T., Lai C.M., Watanabe H., Mak K.K. The association between internet addiction and psychiatric co-morbidity: A meta-analysis. BMC Psychiatry. 2014;14:183. doi: 10.1186/1471-244X-14-183. [http://dx.doi.org/10.1186/1471-244X-14-183]. [PMID: 24947851]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Kuss D.J., Lopez-Fernandez O. Internet addiction and problematic Internet use: A systematic review of clinical research. World J. Psychiatry. 2016;6(1):143–176. doi: 10.5498/wjp.v6.i1.143. [http://dx.doi.org/10.5498/wjp.v6. i1.143]. [PMID: 27014605]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Hale D.R., Fitzgerald-Yau N., Viner R.M. A systematic review of effective interventions for reducing multiple health risk behaviors in adolescence. Am. J. Public Health. 2014;104(5):e19–e41. doi: 10.2105/AJPH.2014.301874. [http://dx.doi.org/10.2105/AJPH.2014.301874]. [PMID: 24625172]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Yau Y.H.C., Pilver C.E., Steinberg M.A., Rugle L.J., Hoff R.A., Krishnan-Sarin S., Potenza M.N. Relationships between problematic internet use and problem-gambling severity: Findings from a high-school survey. Addict. Behav. 2014;39(1):13–21. doi: 10.1016/j.addbeh.2013.09.003. [http://dx.doi.org/10.1016/j.addbeh.2013.09.003]. [PMID: 24140304]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Šmahel D., Blinka L. 2012. Excessive internet use among European children. [Google Scholar]
- 146.Klaniene L., Jocubaite R. Prevention of the internet abuse of the risk group teenagers (12-14 years). Socio-Pedagog. Technol. Socio-Educ. Work. 2012;19(30):77–87. [Google Scholar]
- 147.Forman S.G., Olin S.S., Hoagwood K.E., Crowe M., Saka N. Evidence-based interventions in schools: Developers’ views of implementation barriers and facilitators. School Ment. Health. 2009;1:26. [http://dx.doi.org/10.1007/s12310-008-9002-5]. [Google Scholar]
- 148.Boyce W., Torsheim T., Currie C., Zambon A. The family affluence scale as a measure of national wealth: Validation of an adolescent self-report measure. Soc. Indic. Res., 2006;78:473e87.. [Google Scholar]
- 149.Wang J., Iannotti R.J., Nansel T.R. School bullying among adolescents in the United States: Physical, verbal, relational, and cyber. J. Adolesc. Health. 2009;45(4):368–375. doi: 10.1016/j.jadohealth.2009.03.021. [http://dx.doi.org/10. 1016/j.jadohealth.2009.03.021]. [PMID: 19766941]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Shek D.T., Tang V.M., Lo C.Y. Internet addiction in Chinese adolescents in Hong Kong: assessment, profiles, and psychosocial correlates. ScientificWorldJournal. 2008;8:776–787. doi: 10.1100/tsw.2008.104. [http://dx.doi.org/10. 1100/tsw.2008.104]. [PMID: 18690381]. [DOI] [PMC free article] [PubMed] [Google Scholar]


