Abstract
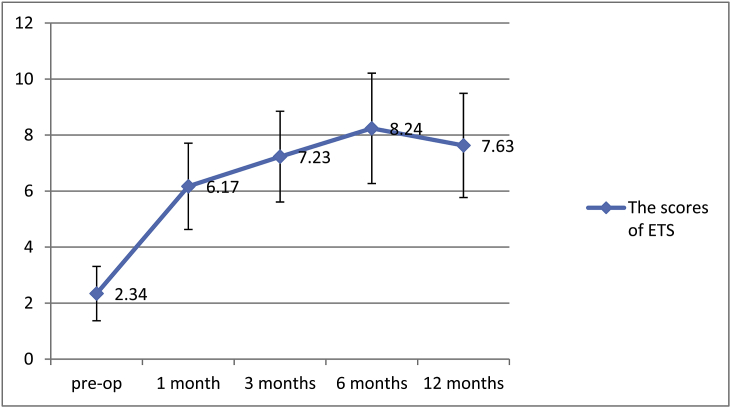
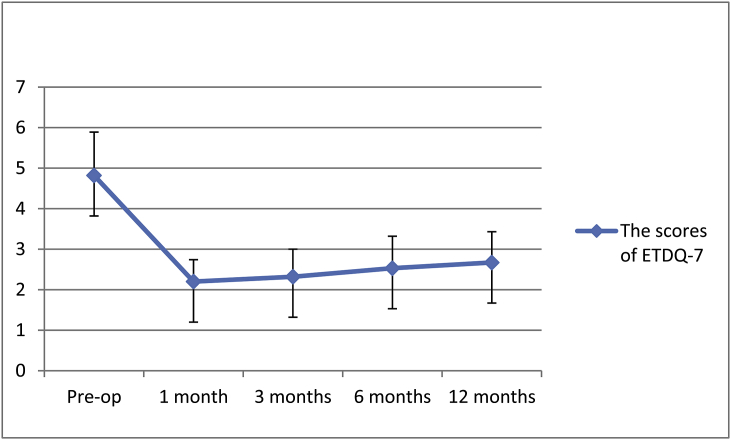
Objective to report outcomes of balloon dilation Eustachian tuboplasty combined with tympanostomy tube insertion and middle ear pressure equalization therapy in treatment of recurrent secretory otitis media. Methods Fifty one patients with recurrent secretory otitis media (62 ears) underwent balloon dilation of Eustachian tube and tympanic tube insertion under general anesthesia, followed by long term middle ear pressure equalization therapies. The Eustachian tube score (ETS) and Eustachian tube function questionnaire (ETDQ-7) were used for pre- and postoperative (up to 12 months) evaluation of Eustachian tube functions. Results The mean ETS score was 2.34 ± 0.97 preoperatively, and 6.17 ± 1.54, 7.23 ± 1.62, 8.24 ± 1.97, and 7.63 ± 1.86 at 1, 3, 6 and 12 months postoperatively, respectively (P < 0.05). The ETDQ-7 score was 4.82 ± 1.07 preoperatively, and 2.20 ± 0.54, 2.32 ± 0.68, 2.53 ± 0.79, and 2.67 ± 0.76 at 1, 3, 6 and 12 months postoperatively, respectively (P < 0.05). Conclusion Balloon dilation of Eustachian tube combined with tympanostomy and catheterization resulted in significant improvement of subjective symptoms and objective evaluation of Eustachian tube functions in most patients with recurrent secretory otitis media, as indicated by the ETS and ETDQ-7 scores, demonstrating high levels of efficacy and patient satisfaction.
Keywords: Balloon dilation eustachian tuboplasty, Positive and negative auricular pressure therapy, Chronic recurrent secretory otitis media, Eustachian tube function score, Eustachian tube function questionnaire-7
1. Introduction
The prevalence of chronic recurrent secretory otitis media (SOM) is relatively high, ranging from 1% to 5% among adults (Huisman et al., 2018). Patients experience recurrent symptoms, and a cure for the condition is difficult. SOM has a considerable impact on the quality of life for patients, making it one of the most common intractable diseases encountered in otolaryngology offices. The leading cause is Eustachian tube dysfunction, which can be treated by puncturing the tympanic membrane, pumping out the fluid and inserting a tympanostomy tube in the tympanic membrane. However, if puncture tympanostomy closes and the tympanostomy tube is lost while Eustachian tube dysfunction still exists, hearing loss, bad-smelling discharge and middle ear effusion frequently follow. In such situations, the fear of disease recurrence can be a heavy burden on patients, and the cost of repeated treatments can create an economic burden. Therefore, focus should be placed on improving Eustachian tube function before tympanostomy and catheterization orifices are closed. This will help effectively relieve ear discomforts caused by SOM and reduce the mental and economic pressure on patients.
Balloon dilation Eustachian tuboplasty (BDET) is a procedure for the treatment of Eustachian tube dysfunction, which has been used in the clinic for almost 10 years. International clinical observations of over 1000 patients found it to be more than 80% effective, with patients reporting a high degree of satisfaction. In addition, several researchers have used a middle ear alternating pressure treatment device to treat SOM, with proven efficacy (Silman et al., 2005). Therefore, we included the use of a middle ear alternating pressure treatment device for maintaining Eustachian tube opening following BDET to see whether the combined treatment can improve outcomes compared with previous reports. To our knowledge, no similar studies with the use of this device have been published.
2. Patients and methods
2.1. Clinical data
Patients diagnosed with recurrent SOM between August 2014 and March 2017 at the Third Affiliated Hospital, Sun Yat-Sen University, were enrolled in this prospective study. The study was approved by the medical ethics committee of the university, and all patients enrolled in the study read and signed informed consent forms. Inclusion criteria were 18 years of age or older; SOM confirmed by symptoms, signs, and audiology tests (Rosenfeld et al., 2016); having failed conservative drug treatment of 3 or more months; and two or more tympanic tube implantations in the past. Exclusion criteria were head or neck surgery in the previous 3 months; a history of head or neck area radiotherapy; suspected nasopharyngeal cancers; clinical signs of upper respiratory tract infection, such as sinusitis or acute rhinitis; adenoid hypertrophy, nasal polyp, or any other space-occupying lesion; cleft lip or palate; congenital ciliary dysfunction; and systemic immune deficiency. Patients who failed to complete the daily Eustachian tube function therapy with the alternating pressure treatment device were also withdrawn from the study.
Sixty-two ears (30 on left and 32 on right; 41 from males and 21 from females) from 51 patients were included. Patient age ranged from 18 to 63 years (average 41.2 years). Preoperative endoscopic examination showed fluid in the middle ear with type B tympanogram in all patients. BDET and tympanostomy were performed simultaneously. Preoperative examination excluded the presence of major diseases, and preoperative high-resolution temporal bone spiral computed tomography excluded the presence of internal carotid artery canal fractures or space-occupying lesions around the Eustachian tube.
2.2. Assessment of Eustachian tube function
Eustachian tube function was evaluated using the Eustachian tube function score (ETS) (Schröder et al., 2015a) and the Eustachian tube dysfunction questionnaire-7 (ETDQ-7) (McCoul et al., 2012) before and at 1, 3, 6, 9 and 12 months after surgery. Treatment efficacy was evaluated by combining results of these tests and patient subjective reports. The ETS covers symptoms, signs and acoustic impedance test results (Table 1), and contain five items for which the highest possible score for each item is 2. The left and right ear in patients with bilateral lesions was scored separately. The ETDQ-7 measures seven Eustachian tube dysfunction symptoms. Although it is a subjective evaluation tool, patients’ extreme sensitivity to painful symptoms means that the ETDQ-7 is an effective measure of the obstructive effects of Eustachian tube dysfunction and of treatment efficacy (Table 2).
Table 1.
Evaluation of Eustachian tube function by the Eustachian tube function score (ETS).
| Item (symptom or examination finding) | 0 points | 1 point | 2 points |
|---|---|---|---|
| Fullness | Always | Infrequent | None |
| Hearing loss | Severe | Medium | Mild or none |
| Clicking noise during swallowing | No clicking | Infrequent, slim | Always, obvious |
| Clicking noise during Valsalva maneuver | No clicking | Infrequent, slim | Always, obvious |
| Change of pressure tympanometry (calm, Valsalva maneuver, swallowing) | No change | Change between 5 and 10 daPa | Change over 10 daPa |
Table 2.
Evaluation of Eustachian tube function by the Eustachian tube dysfunction questionnaire-7 (ETDQ-7).
| Symptom | No problem | Moderate problem | Severe problem |
|---|---|---|---|
| Pressure in the ears? | 1, 2 | 3, 4, 5 | 6, 7 |
| Pain in the ears? | 1, 2 | 3, 4, 5 | 6, 7 |
| A feeling that your ears are clogged? | 1, 2 | 3, 4, 5 | 6, 7 |
| Ear symptoms when you have a cold or sinusitis? | 1, 2 | 3, 4, 5 | 6, 7 |
| Cracking or popping sounds in the ears? | 1, 2 | 3, 4, 5 | 6, 7 |
| Ringing in the ears? | 1, 2 | 3, 4, 5 | 6, 7 |
| A feeling that your hearing is muffled? | 1, 2 | 3, 4, 5 | 6, 7 |
2.3. Surgical protocols
All operations were performed under general anesthesia. An incision was made in the inferoanterior quadrant of the tympanic membrane under fiber endoscopy. Secretions were cleared from the middle ear space, and a mixture of dexamethasone (2 mg) and chymotrypsin (4000 U) injected, which was removed before the tympanic tube was inserted. BDET was performed under a 0° endoscope with an adrenaline-soaked (0.9% saline 30 mL and adrenaline 3 mg) cotton ball via the nasal cavity. Once the Eustachian tube was located in the nasopharynx, a dilator catheter was placed in the Eustachian tube and a balloon was inserted through the catheter. Saline solution was injected to increase the pressure inside the balloon to 10 bar for duration and kept for 120 s before the balloon was de-pressurized and removed. Mucus drainage from the Eustachian tube could be seen before the endoscope was withdrawn.
2.4. Postoperative middle ear alternating pressure therapy
Patients were trained in Eustachian tube alternating pressure therapy using a middle ear pressure equalizer (Model NW-5100) after surgery. The therapy was performed once every morning and once every night for 1 year postoperatively.
2.5. Statistical analysis
Data were analyzed with the Statistical Package for the Social Sciences version 16.0. Measurement data were expressed as mean ± standard deviation, and Student's t-test was used to assess statistical significance. P < 0.05 was considered to indicate statistical significance.
3. Results
3.1. General information
Between August 2014 and March 2017, 51 patients (62 ears) were diagnosed with recurrent SOM and received BDET and TTI followed by 12 months of middle ear alternating pressure therapy. At 12 months follow up, the tympanic tube was lost with the tympanic membrane healed without infection in 6 patients (8 ears). Two patients failed to complete follow-ups and continue middle ear alternating pressure therapy, and therefore withdrawn from the study.
The mean ETS score was 2.34 ± 0.97, 6.17 ± 1.54, 7.23 ± 1.62, 8.24 ± 1.97 and 7.63 ± 1.86 preoperatively and at 1, 3, 6 and 12 months postoperatively, respectively (P < 0.05), indicating efficacy of the treatment. At 12 months, treatment remained effective in 90.3% of the ears (Fig. 1).
Fig. 1.
Pre- and postoperative Eustachian tube function scores (ETS).
The mean ETDQ-7 score was 4.82 ± 1.07, 2.20 ± 0.54, 2.32 ± 0.68, 2.53 ± 0.79 and 2.67 ± 0.76 preoperatively and at 1, 3, 6 and 12 months postoperatively, respectively (P < 0.05), paralleling ETS scores and confirming treatment efficacy. At 12 months, ETDQ-7 remained improved in 93.5% of the ears (Fig. 2).
Fig. 2.
Pre- and postoperative Eustachian tube dysfunction questionnaire-7 (ETDQ-7) scores.
4. Discussion
Eustachian tube dysfunction is the most common cause for recurrent SOM. Chronic nasal diseases can lead to swelling of Eustachian tube mucosa and inflammation can cause Eustachian tube mucosal remodeling and fibrosis, significantly affecting drainage via the Eustachian tube and resulting in negative pressure in the middle ear, often creating a vicious cycle. In addition to conservative pharmaceutical treatments, Eustachian tube dilation, tympanostomy and catheterization are often used to treat SOM in the clinic. However, in some patients symptoms continue to repeat despite these treatments.
A great deal of research has focused on modifying treatments to eliminate Eustachian tube obstruction and improve its function, including Eustachian tube dilation. In 1983, Yamashita (1983) reported Eustachian tube dilation using a flexible fiberscope combined with slight tearing and repositioning of cartilage and connective tissues around the tube to lower the minimum pressure required for tube opening and facilitate tube opening by surrounding muscles. This technique permits observation of the inside of the entire cartilaginous portion up to the isthmus for evaluating tubal dysfunction conditions in cases such as SOM, as well as pre- and postoperative tubal conditions in tympanoplasty. After balloon expansion techniques were used to treat aortic stenosis by cardiovascular specialists, in 2010 Ockermann (Ockermann et al., 2010) used the technique for dilation of the Eustachian tube in eight patients (13 ears) and evaluated Eustachian tube function at 1, 2 and 8 weeks. At 8 weeks, Eustachian tube function remained significantly improved compared with preoperative data. Subsequently, Eustachian tube balloon dilation has been widely used in various countries. In 2012, Catalano et al. (2012) performed BDET on 70 patients (100 ears) and followed up the patients for 6 months. Relief of ear fullness and negative pressure was reported in 71% of the patients, and most patients were satisfied with the treatment. Luukkainen et al. (2018) followed up 34 patients (52 ears) after BDET from 1.8 to 4.6 years. They found reduced ear pain, ear pressure and ear stuffiness in 75% of the patients compared to before surgery, and 82% of patients indicated willingness to undergo BDET again if symptoms reappeared. The overall postoperative patient satisfaction was high. All these studies found that patients experienced significant improvement following BDET with high rates of patient satisfaction.
Hou et al. studied the use of BDET plus TTI in the treatment of recurrent SOM and found that the efficacy rate was 83.9% assessed by the ETS and 84.3% assessed by the ETDQ-7. We used the same evaluation methods in our study and found postoperative rates of efficacy of over 90%. The reason for this difference may be related to the continuous use of middle ear alternating pressure therapy after surgery in our study. The middle ear alternating pressure treatment instrument is a portable device that can introduce stable airflow for 5 s. When the Eustachian tube is open during swallowing, the continuous airflow into the Eustachian tube can promote continuous and stable tube expansion. The instructions given to patients in this study for using of the device meant that the Eustachian tube on each side received passive expansion at least six times a day. This likely contributed to the maintenance of treatment efficacy after initial surgery, although specific mechanisms behind this result requires further research.
Following standard survey methodology, McCoul et al. (2012) in 2012 developed the ETDQ-7 scale for evaluating Eustachian-tube-related symptoms. When tested by Cronbach's alpha coefficient and the receiver operating characteristic curve analysis, the scale showed good reliability and diagnostic values. The reliability of the Chinese version of the scale has also been verified (Chen et al., 2016). Hu et al. (2016) used the ETDQ-7 to evaluate patients after BDET plus TTI treatment and showed significant improvement of the ETDQ-7 scores at 1, 3 and 6 months compared with the scores before surgery. Reporting a rate of efficacy of 84.3% after BDET using the ETDQ-7,Hou et al. (2016) believed that this scale was worthy of clinical application. In our study, the ETDQ-7 score significantly decreased after surgery at each following up time point compared before treatment (P < 0.05). Singh et al. (2017) observed 11 patients (13 ears) after BDET surgery and found that although the ETDQ-7 showed subjective symptoms improvement, there was no improvement in tympanogram data.
Considering that the ETDQ-7 reflects only subjective feelings of patients, which may not always be consistent with actual improvement of organ functions, its use has certain limitations. Therefore, to avoid the drawbacks of using subjective evaluation alone, this study adopted a combination of subjective and objective measurements. The ETS contains both subjective and objective indices that allow gauging subjective patients symptoms of otitis media as well as objectively assessing Eustachian tube functioning. The ETS is a simple, practical and comprehensive tool for assessing Eustachian tube functions. It can be used before and after balloon tuboplasty. Schröder (Schröder et al., 2013) used the ETS to evaluate patients undergoing BDET. In a group of 12 patients (20 ears), the ETS score was 1.25 ± 1.83 before treatment, and improved to 6.2 ± 2.61 one year after. In a second group of 66 patients (115 ears), the ETS score was 2.21 ± 2.02 preoperatively and improved to 5.4 ± 2.53 2 months after. In a similar study in 2015, Schröder (Schröder et al., 2015b) increased the sample size and extended the observation time. In 622 patients (1076 ears) undergoing BDET, 1 year follow-up results were available in 188 ears with the ETS score improved from 3.13 before surgery to 5.75 at 1 year after; 2 years follow-up results were available in 34 with the ETS score increased from 2.65 before surgery to 6.26 at 2 years after; and 3 years follow-up results were available in 11 of 119 ears with the ETS score increased from 2.36 before surgery to 5.27 at 3 years after. In our study, the mean ETS score was 2.34 ± 0.97 before surgery and 7.63 ± 1.86 at 12 months after (P < 0.05).
At present, there are several techniques for balloon dilation of the Eustachian tube. The common view (Ockermann et al., 2010) is that after the mucosa of the cartilaginous portion expands under the pressure of the balloon, the submucosa expands and tears, and this damage is repaired by filling in with fibroblasts, new blood vessels, and inflammatory cells, while collagen fibers that are prone to cause scar contracture are less likely to appear and therefore stenosis is less likely. However, where there is damage repair, production of collagen fibers is inevitable. To reduce the risk of restenosis due to local deposition of fibrous collagen and to maintain normal tube functionality, better methods for continued scar expansion are needed. We chose to use a middle ear alternating pressure treatment device for continued tube expansion to reduce the risk of restenosis and improve outcomes. At 12 months of follow-up, substantial treatment effects were demonstrated, indicating that our treatment protocol may be an ideal approach for chronic SOM.
Our study showed that at 12 months, the rate of treatment efficacy was 90.3% by ETS and 93.5% by ETDQ-7. Other studies (Hou et al., 2016; Li et al., 2016) using the ETS and ETDQ-7 to evaluate the efficacy of BDET plus TTI reported efficacy rates of 83.9%–84.6%. The higher rate of efficacy in our study may be attributed to continuous middle ear alternating pressure therapy after BDET and TTI which helped maintain Eustachian tube functions.
Although our study has shown that middle ear alternating pressure therapy following BDET and TTI is effective, because of the small sample size and short follow-up time, it is difficult to accurately explain the mechanisms. Long-term prospective studies with large sample sizes are needed to further evaluate the safety and efficacy of this treatment and determine whether other more effective treatment models exist.
Conflicts of interest
The authors have no conflicts of interest to declare.
Acknowledgments
This study was supported by the Guangzhou Science and Technology Project (Industrial, Academic and Research Collaborative Innovation Project): 201803010093, and the major development projects of sun yat-sen university: 201812281965.
Footnotes
Peer review under responsibility of PLA General Hospital Department of Otolaryngology Head and Neck Surgery.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.joto.2019.05.003.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Catalano P.J., Jonnalagadda S., Yu V.M. Balloon catheter dilatation of Eustachian tube: a preliminary study. Otol. Neurotol. 2012;33(9):1549–1552. doi: 10.1097/MAO.0b013e31826a50c3. [DOI] [PubMed] [Google Scholar]
- Chen Bin, Yu Chenjie, Shen Xiaohui. Evaluation of the Chinese version of the seven-item eustachian tube dysfunction questionnaire. Chinese Journal of Otology. 2016;14(5):582–585. [Google Scholar]
- Hou Zhaohui, Li Ruixiang, Wu Nan. Outcomes of balloon eustachian tuboplasty for refractory otitis media with effusion. Chinese Journal of Otology. 2016;14(5):560–565. [Google Scholar]
- Hu Yue, Dong Yaodong, Liu Dongliang. Balloon dilation eustachian tuboplasty combined with tympanotomy tube insertion in the treatment of refractory secretory. Chinese Journal of Otology. 2016;14(5):586–590. [Google Scholar]
- Huisman J.M.L., Verdam F.J., Stegeman I. Treatment of Eustachian tube dysfunction with balloon dilation: a systematic review. The Laryngoscope. 2018 Jan;128(1):237–247. doi: 10.1002/lary.26800. [DOI] [PubMed] [Google Scholar]
- Li Yongqi, Chen Yubin, Yin Gendi. Balloon dilation Eustachian tuboplasty in the treatment of chronic recurrent secretory otitis media. Chinese Journal of Otology. 2016;14(5):610–614. [Google Scholar]
- Luukkainen V., Vnencak M., Aarnisalo A.A. Patient satisfaction in the long-term effects of Eustachian tube balloon dilation is encouraging. Acta Otolaryngol. 2018;138(2):122–127. doi: 10.1080/00016489.2017.1384568. [DOI] [PubMed] [Google Scholar]
- McCoul E.D., Anand V.K., Christos P.J. Validating the clinical assessment of eustachia tube dysfunction:The Eustachian TubeDysfunction Questionnaire (ETDQ-7) The Laryngoscope. 2012;122(5):1137–1141. doi: 10.1002/lary.23223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ockermann T., Reineke U., Upile T. Balloon dilatation eustachian tuboplasty: a clinical study. The Laryngoscope. 2010;120(7):1411–1416. doi: 10.1002/lary.20950. [DOI] [PubMed] [Google Scholar]
- Rosenfeld R.M., Shin J.J., Schwartz S.R. Clinical practice guideline: otitis media with effusion (update) Otolaryngol. Head Neck Surg. 2016;154(1):S1–S41. doi: 10.1177/0194599815623467. [DOI] [PubMed] [Google Scholar]
- Schröder S., Reineke U., Lehmann M. Chronic obstructive eustachian tube dysfunction in adults: long-term results of balloon eustachian tuboplasty. HNO. 2013;61(2):142–151. doi: 10.1007/s00106-012-2573-3. [DOI] [PubMed] [Google Scholar]
- Schröder S., Lehmann M., Sauzet O. A novel diagnostic tool for chronic obstructive eustachian tube dysfunction—the eustachian tube score. The Laryngoscope. 2015;125(3):703–708. doi: 10.1002/lary.24922. [DOI] [PubMed] [Google Scholar]
- Schröder S., Lehmann M., Ebmeyer J. Balloon Eustachian tuboplasty: a retrospective cohort study. Clin. Otolaryngol. 2015;40(6):629–638. doi: 10.1111/coa.12429. [DOI] [PubMed] [Google Scholar]
- Silman S., Arick D.S., Emmer M.B. Nonsurgical home treatment of middle ear effusion and associated hearing loss in children. Part II: validation study. Ear Nose Throat J. 2005;84(10):646–654. [PubMed] [Google Scholar]
- Singh T., Taneja V., Kulendra K. Balloon Eustachian tuboplasty treatment of longstanding Eustachian tube dysfunction. J. Laryngol. Otol. 2017;131(7):614–619. doi: 10.1017/S0022215117000974. [DOI] [PubMed] [Google Scholar]
- Yamashita K. Pneumatic endoscopy of the Eustachian tube. Endoscopy. 1983;15(4):257–259. doi: 10.1055/s-2007-1021526. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.