Abstract
Background
Probable benign paroxysmal positional vertigo, spontaneously resolved (pBPPVsr), is a variant of benign paroxysmal positional vertigo (BPPV) in which there is no observable nystagmus and no vertigo with any positional maneuver.
Objectives
To calculate the incidence pBPPVsr, compare the characteristics of the patients with pBPPVsr and BPPV not spontaneously resolved and describe the spontaneous resolution in the natural course of BPPV.
Methods
Multicenter prospective descriptive study. During a one-year period, all patients with suspected BPPV that presented to the Neurotology Units of five participating centers were recruited. The incidence of pBPPVsr was calculated as a percentage of the total number of patients with BPPV. The prevalence of several variables was compared between pBPPVsr and BPPV not spontaneously resolved. The timing of spontaneous resolution was estimated using Kaplan-Meier curves.
Results
457 patients met the inclusion criteria. The incidence of pBPPVsr was 33.5%. It was significantly higher in males, in patients with normal bone mass and in patients who were not taking sulpiride. A rate of 18% of spontaneous resolution after the first month and 51% after the first year was found. This percentage did not change in a significant way after this moment. The curves for males, patients under 50 and patients with normal blood pressure decreased significantly faster.
Conclusions
In our serie, BPPV spontaneously resolved in half of the patients with BPPV during the first year. This seemed to occur more commonly in males and could have been hindered by sulpiride intake, osteoporosis, advanced age and high blood pressure.
Keywords: Benign paroxysmal positional vertigo; Probable benign paroxysmal positional vertigo, spontaneously resolved; Osteoporosis; Sulpiride; Hypertension
1. Introduction
According to a widely accepted theory, benign paroxysmal positional vertigo (BPPV) is usually caused by otoconia that are dislodged from the otoconia macula beds and are trapped in a semicircular canal (von Brevern et al., 2015). There are two different types of migration: canalolithiasis, where otoconia enter the canal through its non-ampullar end and freely move into the canal (Hall et al., 1979), or less frequently, cupulolithiasis, where otoconia adhere to the cupula (Schuknecht, 1960). BPPV is diagnosed and treated using canalith repositioning procedures (CRP).
Although CRP are simple, BPPV-related expenses are disproportionately high. Often, this is due to the collection of large amounts of diagnostic data, that in many cases do not help to make a conclusive diagnosis (Li et al., 2000) and also due to the use of non-resolutive treatments (Pérez et al., 2008). As we have observed in clinical practice, one of the reasons why diagnostic expenses increase is the spontaneous resolution of BPPV. This phenomenon is a variant of BPPV, which can be difficult to differentiate from any other cause of episodic vestibular syndrome as positional testing is negative and, if the doctor does not suspect this, unnecessary diagnostic tests may be ordered.
Nowadays, it is accepted that spontaneous resolution of BPPV can occur with no treatment other than observation in 35–50% of patients (Burton et al., 2012). The Consensus document of the Committee for the Classification of Vestibular Disorders of the Bárány Society defines this variant of BPPV as “Probable benign paroxysmal positional vertigo, spontaneously resolved” (pBPPVsr). pBPPVsr is defined as recurrent attacks of positional vertigo or positional dizziness, with a duration of less than a minute, provoked by lying down or turning over in the supine position without any observable nystagmus or vertigo during any positional maneuver and this vertigo or dizziness cannot be attributed to another disorder (von Brevern et al., 2015).
pBPPVsr is a time-consuming process with a great interference of the patient's daily life activity (Bhattacharyya et al., 2017). Therefore, it is necessary to carry out studies to calculate its incidence, find out the types of patients who are most likely to experience spontaneous resolution of BPPV and determine the role of spontaneous resolution in the natural course of BPPV.
2. Objectives
-
1.
Calculate the incidence in medical practice of pBPPVsr as a proportion of the total number of patients with BPPV with or without spontaneous resolution.
-
2.
Compare the characteristics of patients with pBPPVsr with patients whose BPPV has not spontaneously resolved.
-
3.
Describe the natural course of BPPV when the phenomenon of spontaneous resolution is considered.
3. Material and methods
A multicenter prospective and descriptive study was designed. The protocol of this research study was accepted by the ethics committee of the main participating center. All patients with suspected BPPV that presented to the Neurotology Units of the five participating centers were prospectively recruited between April 1st, 2015 and March 31st, 2016.
The procedure started with an anamnesis, which contained items related to the development of BPPV (Table 1). After that, the patients underwent a full neurotological exploration including bilateral head thrust tests (Halmagyi and Curthoys, 1988). Spontaneous nystagmus was evaluated without Frenzel glasses and patients with spontaneous nystagmus were excluded in order to avoid including patients who would be difficult to categorize.
Table 1.
Variables related to the development of BPPV, incidence of pBPPVsr in each category and p-values of χ2 and log-rank tests.
| Variable | Description | Categories | pBPPVsr percentage | χ2 test p-value | Log-rank test p-value |
|---|---|---|---|---|---|
| Demographic variables | |||||
| Sex | Man or woman | Man | 42.3% | 0.0060 | 0.0005 |
| Woman | 29.2% | ||||
| Age | Age in years | 0–49 | 38.2% | 0.1780 | 0.0190 |
| >50 | 31.6% | ||||
| Cardiovascular risk factors | |||||
| Hypertension | Diagnosis after periodic screening studies in primary healthcare | No | 36.5% | 0.1020 | 0.0130 |
| Yes | 29.1% | ||||
| Diabetes | Diagnosis after periodic screening studies in primary healthcare | No | 33.3% | 0.8490 | 0.9660 |
| Yes | 34.7% | ||||
| Hyperlipidemia | Diagnosis after periodic screening studies in primary healthcare | No | 33.2% | 0.8650 | 0.5150 |
| Yes | 34.0% | ||||
| Smoking habit | Active or non-active smoker | Non-active | 33.3% | 0.8270 | 0.6100 |
| Active | 34.6% | ||||
| Alcohol consumption | Any alcohol intake within 24 h period prior to medical consultation | No | 33.7% | 0.7940 | 0.4530 |
| Yes | 32.3% | ||||
| Factors related to development of BPPV | |||||
| Migraine | A migraine attack in the last few weeks | No | 34.6% | 0.4160 | 0.6880 |
| Yes | 30.5% | ||||
| Osteoporosis | Osteoporosis diagnosed through densitometry within the previous two years | No | 35.2% | 0.0067 | 0.2080 |
| Yes | 12.1% | ||||
| Traumatic brain injury | Traumatic brain injury within a maximum of 90 days before the start of the current vertigo attack | No | 33.4% | 0.9000 | 0.9000 |
| Yes | 32.4% | ||||
| Traffic accident | Sudden head deceleration or whiplash-like cervical injury within a maximum of 90 days before the start of the current vertigo attack | No | 33.5% | 0.6140 | 0.3970 |
| Yes | 25.0% | ||||
| Prolonged head extension | Prolonged head extension the day before the start of the current vertigo attack | No | 34.9% | 0.0650 | 0.4470 |
| Yes | 23.0% | ||||
| BPPV characteristics | |||||
| First episode | First episode of BPPV | No | 29.2% | 0.0610 | 0.2160 |
| Yes | 37.6% | ||||
| Previous ipsilateral BPPV | Previous BPPV of the same semicircular canal was considered positive, provided that BPPV had been treated with a repositioning maneuver and loss of nystagmus had been verified at least 90 days before the start of the symptoms of the current vertigo attack | No | 34.6% | 0.1880 | 0.2720 |
| Yes | 25.9% | ||||
| Sulpiride intake | Sulpiride intake in the 24 h prior to the medical consultation | No | 36.2% | 0.0007 | 0.1860 |
| Yes | 13.0% | ||||
| Betahistine intake | Betahistine intake in the 24 h prior to the medical consultation | No | 33.4% | 0.9480 | 0.9650 |
| Yes | 33.8% | ||||
| Ipsilateral inner ear characteristics | |||||
| Head thrust test | Positive ipsilateral head thrust test. In the case of pBPPVsr, if either test was positive, this was considered a positive result | No | 33.8% | 0.9720 | 0.6910 |
| Yes | 34.1% | ||||
| Inner ear disease | Ipsilateral defined Ménière's disease, vestibular neuritis, sudden hearing loss or vestibular migraine were considered positive | No | 34.0% | 0.1580 | 0.0640 |
| Yes | 18.8% | ||||
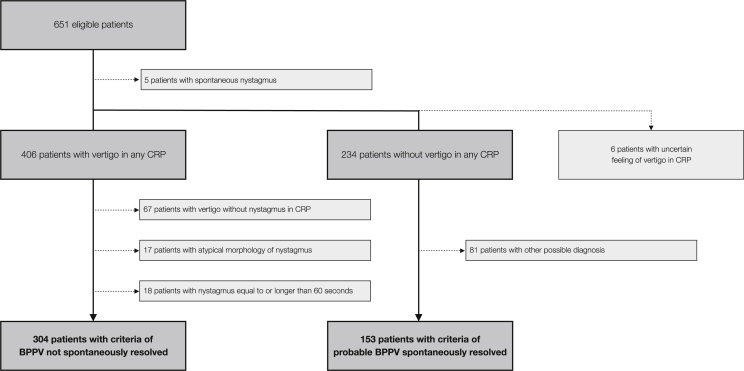
Then, all patients underwent Pagnini-McClure (Pagnini et al., 1989; McClure, 1985) and Dix-Hallpike (Dix and Hallpike, 1952) tests and were divided into three groups depending on the symptoms elicited by these maneuvers. The first group consisted of patients who felt vertigo provoked by any of the maneuvers; the second group consisted of those who did not feel vertigo in any of the maneuvers; and the third group consisted of those who were unable to describe if they were feeling vertigo or not. Within the first group, only the patients who met the criteria for canalolithiasis of the posterior canal, or canalolithisis or cupulolithiasis of the horizontal canal (von Brevern et al., 2015) were included. Therefore, patients lacking nystagmus during the CRP when observed without Frenzel glasses and those showing an atypical morphology or duration of nystagmus were excluded as they did not met these criteria. Within the second group, only those patients who complained of recurrent attacks of positional vertigo provoked by lying down or turning over in the supine position and who met the criteria for pBPPVsr as set out by the Bárány Society (von Brevern et al., 2015) were included. Hence, the patients of the second group whose main complaint was prolonged mild unsteadiness were not included as other diagnosis was possible. All patients in the third group were excluded from this study. Fig. 1 sketches the selection process.
Fig. 1.
Screening of potential candidates to participate in the study to determine the two groups of patients.
The patients in the first group, BPPV not spontaneously resolved (BPPVnsr), were compared with those in the second group (pBPPVsr) in three different ways. Firstly, the incidence in medical practice of pBPPVsr was calculated as a proportion of the total number of patients with any variant of BPPV (canalolithiasis of the posterior canal, canalolithisis or cupulolithiasis of the horizontal canal or probable BPPV spontaneously resolved). The average number of days from when the appointment was requested until the patient was seen of the participating centers was taken into account when doing these calculations. Secondly, the percentages of pBPPVsr over the total of patients with BPPV were compared between the categories of the factors in Table 1 using the χ2 test. Thirdly, the occurrence in time of the spontaneous resolution of BPPV was modeled using a Kaplan-Meier plot and the influence of the variables in Table 1 during this period was analyzed using log-rank tests and Cox regression in order to find factors which help in the spontaneous resolution of BPPV.
4. Results
457 patients met the criteria for inclusion in the study. The median age was 61 and the male-to-female ratio was 149–308. The group with BPPVnsr included 304 patients and the pBPPVsr group included 153 patients. Therefore, in our medical practice the incidence of pBPPVsr as a proportion of the total number of patients with BPPV was 33.5%.
The incidence of pBPPVsr varied between the participating centers in the study and it ranged from 19.5% to 60.3%. The incidence rate was 25.5% in centers with a waiting list of less than one month and this rose to 47.3% when the waiting list was longer. In centers with a waiting list of less than one month, 2.4% of patients presented canalithiasis or cupulolithiasis of the horizontal semicircular canal. This rose to 3.6% when the waiting list was longer.
Next, the patients were categorized according to the variables in Table 1 and the incidence rate of pBPPVsr was compared between categories. This table shows these incidence rates and the p-values obtained in the χ2 test results. Three variables were found to be statistically significant: sex, osteoporosis and sulpiride intake the day before testing. pBPPVsr was found to occur more frequently in males, patients with normal bone mass and in those who were not taking sulpiride. However, when the Bonferroni correction for multiple comparisons was applied, the only one of these found to be statistically significant was sulpiride intake.
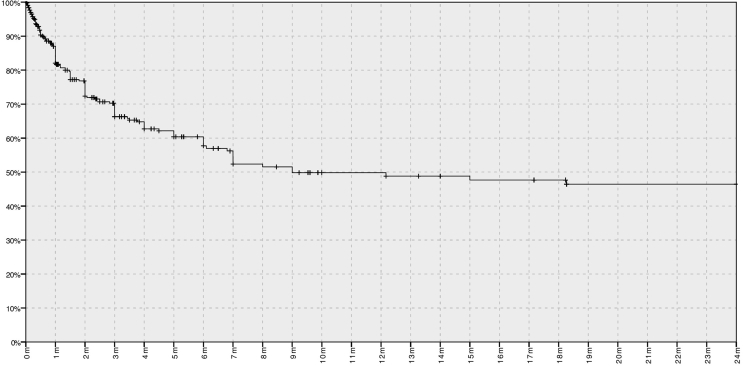
Finally, the Kaplan-Meier curve in Fig. 2 shows the occurrence in time of the spontaneous resolution of BPPV. The x-axis represents the time from the development of the first symptoms of BPPV to the moment of CRP. This figure shows that spontaneous resolution occurred in 4% of patients 1 week after the onset of symptoms; it occurred in 18% of patients after 1 month; 42% after 6 months; and 51% after 1 year. From this moment, this percentage did not increase significantly and after 2 years spontaneous resolution had occurred in 60% of patients.
Fig. 2.
Kaplan-Meier curve showing the occurrence in time of the spontaneous resolution of BPPV. The duration of the current episode of BPPV is represented in the x-axis and the percentage of patients remaining with BPPVnsr in the y-axis. Vertical segments occur when spontaneous resolution takes place and tick-marks indicate censored data produced by patients with BPPVnsr, both detected in the moment of CRP.
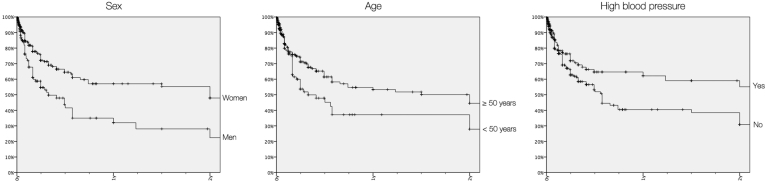
Table 1 shows the log-rank test p-values obtained when the Kaplan-Meier curves for the groups, categorized according to the variables in this table, were compared. Three variables were found to be statistically significant: sex, age and hypertension. Spontaneous resolution occurred sooner in males, in patients under the age of 50 and in those not suffering from hypertension. When the Bonferroni correction was applied, only sex remained statistically significant. The multivariate analysis using Cox regression found dependence between age and hypertension.
5. Discussion
The first cases of spontaneous resolution of BPPV were reported as a collateral finding two decades ago when the results of CRP were still being tested. Spontaneous resolution occurred in some patients in the control groups, who received no treatment (Blakley, 1994; Lynn et al., 1995). At that time, BPPV was even described as a transient benign phenomenon that, as a rule, would resolve spontaneously in about 2–6 weeks (Zucca et al., 1998). The data from our study rejects this idea.
The phenomenon of the spontaneous resolution of BPPV has been linked to the fact that the endolymph, which is a low calcium content fluid, is able to dissolve otoconia. The endolymph can rapidly dissolve large otoconia in about 20 h under experimental conditions; however, one can assume that, in physiological conditions, the rate at which otoconia dissolve is much slower as they may become attached or trapped in the cupula, and also due to the presence of diffusion barriers (cupula or clots) or to the small volume of the endolymph (Zucca et al., 1998). These facts explain why BPPV does not resolve spontaneously in most cases.
BPPV of the horizontal canal has been described as having a higher rate of spontaneous resolution than other types of BPPV (Moon et al., 2006; Sekine et al., 2006) because free-floating debris in this canal would tend to float back out into the utricle as a result of natural head movements (Parnes et al., 2003). However, in our sample, after comparing the percentage of horizontal BPPV with other types of BPPV across the participating centers and taking into account the different waiting list times of these centers, no significant differences were found.
5.1. Incidence in medical practice of pBPPVsr
In our sample, incidence in medical practice of pBPPVsr as a proportion of the total number of patients with BPPV was 33.5%. This incidence rate varied a lot between the participating centers. This variability can be attributed to two causes. First, the patients' pathway through the healthcare system varied depending on the center. In most of the centers, a medical appointment had to be requested by the general practitioners; in one center, however, the pathway was simpler and the appointment could be requested directly by the patient; and in another one the pathway was longer because the appointment had to be requested by an otolaryngologist. Each physician in the patient's pathway could have acted to filter out mild cases, depending on his abilities to recognize pBPPVsr, to distinguish it from other causes of episodic vestibular syndrome and to treat BPPV. Secondly, the waiting list time varied between centers, ranging from three days to six weeks. Fig. 2 shows that spontaneous resolution is more common in the first days after the onset of symptoms and therefore a longer waiting list time will lead to a higher incidence of pBPPVsr.
The incidence rate found must be interpreted as an approximation to the real value as sometimes the diagnosis of pBPPVsr is not easy, even for trained neurotologists. In order to make this diagnosis, the patient has to have suffered recurrent attacks of positional vertigo or positional dizziness; however, some patients with BPPV may have prolonged mild unsteadiness as well as attacks of positional vertigo (von Brevern et al., 2015). If this unsteadiness is more annoying than the vertigo, differential diagnosis becomes trickier. On the other hand, CRP are not 100% sensitive in BPPVnsr patients as otoliths may move close to the canal wall, which prevents the relevant endolymph shifts (Bronstein and Lempert, 2007); therefore, in these cases, patients would be incorrectly classified as pBPPVsr.
5.2. Characteristics of patients suffering from pBPPVsr
A preliminary analysis of our data showed three significant differences between the pBPPVsr group and the BPPVnsr group: there were more males in the pBPPVsr group, and patients in the pBPPVsr group had a better bone mass and a lower sulpiride intake than those in the BPPVnsr group. When the Bonferroni correction was applied, only sulpiride intake remained significant. Despite the statistical significance of the differences, their magnitudes do not seem relevant for clinical practice; thus, it was not possible to model a pBPPVsr prototype patient using the data collected.
A higher incidence of pBPPVsr was found in males, whereas BPPV has been described as more common in females (Bronstein and Lempert, 2007). Two hypotheses can explain this fact. The first one assumes that BPPV is equally common in both genders, but that spontaneous resolution is a less common occurrence in women, who thus have to seek medical care more often. In this sense, other studies show that there is a similar recurrence rate of BPPV in both genders (Pérez et al., 2012). The second hypothesis postulates that, due to sociocultural factors, an episode of pBPPVsr causes symptoms that are more unexpected in males, who thus demand more medical attention.
Osteoporosis has been described as a risk factor for the development of BPPV due to a vitamin D deficiency and higher bone turnover rates at a systemic level, which could disturb local Ca2+ homeostasis in the inner ear (Lee et al., 2017). In our sample, spontaneous resolution was three times more common in the normal bone mass group. The fact that the p-value for this variable did not reach statistical significance could be due to the fact that there were not many patients in these categories (20 in the pBPPVsr group and 75 in the BPPVnsr group) as a densitometry performed within the two years prior to the medical interview was required for patients to be included in these categories.
The lower sulpiride intake in the pBPPVsr group was attributed to the fact that patients suffering from pBPPVsr should be asymptomatic and should not feel the need to take medication.
5.3. The natural course of BPPV
The Kaplan-Meier curve shows that spontaneous resolution is more frequent when less time has passed since the onset of the symptoms (Fig. 2). The curve has a hyperbolic shape, thus indicating that the spontaneous resolution does not significantly affect the number of patients with BPPVnsr after one year and it does not occur in 100% of patients after two years.
There are few studies about the natural course of BPPV. Imai et al., in a prospective study with 108 patients with BPPV, found that the average period of time from the onset of BPPV to its remission was 39 ± 47 days for posterior canal BPPV and 16 ± 19 days for horizontal canal BPPV. Vertigo lasted for more than 1 month in 36% of patients with posterior canal BPPV and in 11% of those with horizontal canal BPPV (Imai et al., 2005). Our data differed significantly from the data collected for this study: after 1 month, 82% of our patients remained symptomatic and this fact can be attributed to the different inclusion criteria of these two studies: all patients recruited by Imai et al. needed to have nystagmus in the diagnostic maneuvers of BPPV to be included.
The data presented in Fig. 1 can be biased due to three factors: the way in which patients are filtered, the moment when resolution takes place and the reliability of long-term symptoms. Firstly, patients suffering from short-term BPPV with spontaneous resolution would not have been considered seriously ill by general practitioners and thus specialized medical care would not have been requested; this fact could have underestimated the found timing of spontaneous resolution. In fact, despite the Kaplan-Meier curve always having a hyperbolic shape, log-rank tests showed significant differences between the participating centers. Secondly, when the patients were asked about the moment when resolution had taken place, most of them were unable to remember the exact date. Some of them had developed avoidant positional strategies and therefore had not even realized that the symptoms had resolved. Due to these uncertainties, the date of resolution was defined as the moment when CRP were performed and these were negative. Thirdly, long-term BPPV symptoms could be misinterpreted and might not really be unresolved cases of BPPV, but rather cases of relapsing-remitting BPPV. 5.6% of the patients said that they had suffered continuously for over 2 years and 0.9% of the patients said that they had had continuous symptoms for over 25 years. These cases were excluded from the Kaplan-Meier curve to avoid this bias.
Because of these biases, we think that the real population curve must be hyperbolic, but that its slope must be higher in its initial segments and that its horizontal asymptote must have a lower ordinate. Carrying out a study with members of the general population could solve the biases; however, this kind of study is expensive, especially in the case of a benign condition like pBPPVsr.
Fig. 3 compares the Kaplan-Meier curves for patients categorized into groups based on the variables that showed significant differences in the log-rank tests: sex, age and hypertension. In males, the curve has steeper slopes and a lower ordinate at the two-year point than in females. This finding fits well with the higher incidence rate of pBPPVsr found in males. The Cox regression found dependence between age and hypertension. No previous references about pBPPVsr and these variables have been reported yet. Nevertheless, if one considers the absence of spontaneous resolution and the recurrence of BPPV to be related phenomena (they can be confused in long-term BPPV), both age and hypertension have been linked to a higher risk of recurrence (Rashad, 2009; Tan et al., 2017).
Fig. 3.
Kaplan-Meier curves for the categories of variables with significant differences in log-rank test.
5.4. Advice for dealing with pBPPVsr
In the differential diagnosis of episodic vestibular syndrome, pBPPVsr must be included in order to avoid wasting large amounts of money collecting diagnostic data. This entity was present in all of the Neurotology Units participating in this study, but the incidence rate varied depending on the patients’ pathway through the healthcare system.
Spontaneous resolution is more likely in the first days after the onset of the symptoms and it is unlikely to occur after one year has passed. Spontaneous resolution may also be more common in males.
However, when dealing with pBPPVsr, one should carry out a differential diagnosis with vestibular migraine as it can also cause episodic positional vertigo. Unlike BPPV, episodes of positional vertigo in vestibular migraine tend to be of shorter duration, to recur frequently, and to occur at an earlier age, and they are often accompanied by migraine symptoms (von Brevern et al., 2004).
6. Conclusion
Spontaneous resolution of BPPV occurs in 18% of patients during the first month after the appearance of the first symptoms of the disease and in 51% after the first year, but it is unusual for spontaneous resolution to occur after this point. Spontaneous resolution of BPPV is more common in males and could be hindered by sulpiride intake, osteoporosis, advanced age and high blood pressure.
Compliance with ethical standards
-
•
This study was not funded.
-
•
None of the author had conflict of interest in relation with the study.
-
•
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
-
•
Informed consent was obtained from all individual participants included in the study.
Footnotes
Peer review under responsibility of PLA General Hospital Department of Otolaryngology Head and Neck Surgery.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.joto.2019.04.002.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Bhattacharyya N., Gubbels S.P., Schwartz S.R. Clinical practice guideline: benign paroxysmal positional vertigo (update) Otolaryngol--Head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg. 2017 Mar;156(3_Suppl. l):S1–S47. doi: 10.1177/0194599816689667. [DOI] [PubMed] [Google Scholar]
- Blakley B.W. A randomized, controlled assessment of the canalith repositioning maneuver. Otolaryngol--Head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg. 1994 Apr;110(4):391–396. doi: 10.1177/019459989411000407. [DOI] [PubMed] [Google Scholar]
- Bronstein A., Lempert T. Dizziness: A Practical Approach to Diagnosis and Management. first ed. Cambridge University Press; 2007. Positional vertigo. [Google Scholar]
- Burton M.J., Eby T.L., Rosenfeld R.M. Extracts from the Cochrane Library: modifications of the Epley (canalith repositioning) maneuver for posterior canal benign paroxysmal positional vertigo. Otolaryngol--Head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg. 2012 Sep;147(3):407–411. doi: 10.1177/0194599812457134. [DOI] [PubMed] [Google Scholar]
- Dix M.R., Hallpike C.S. The pathology, symptomatology and diagnosis of certain common disorders of the vestibular system. Ann. Otol. Rhinol. Laryngol. 1952 Dec;61(4):987–1016. doi: 10.1177/000348945206100403. [DOI] [PubMed] [Google Scholar]
- Hall S.F., Ruby R.R., McClure J.A. The mechanics of benign paroxysmal vertigo. J. Otolaryngol. 1979 Apr;8(2):151–158. [PubMed] [Google Scholar]
- Halmagyi G.M., Curthoys I.S. A clinical sign of canal paresis. Arch. Neurol. 1988 Jul;45(7):737–739. doi: 10.1001/archneur.1988.00520310043015. [DOI] [PubMed] [Google Scholar]
- Imai T., Ito M., Takeda N. Natural course of the remission of vertigo in patients with benign paroxysmal positional vertigo. Neurology. 2005 Mar 8;64(5):920–921. doi: 10.1212/01.WNL.0000152890.00170.DA. [DOI] [PubMed] [Google Scholar]
- Lee S.B., Lee C.H., Kim Y.J. Biochemical markers of bone turnover in benign paroxysmal positional vertigo. PLoS One. 2017;12(5):e0176011. doi: 10.1371/journal.pone.0176011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J.C., Li C.J., Epley J. Cost-effective management of benign positional vertigo using canalith repositioning. Otolaryngol--Head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg. 2000 Mar;122(3):334–339. doi: 10.1016/S0194-5998(00)70043-X. [DOI] [PubMed] [Google Scholar]
- Lynn S., Pool A., Rose D. Randomized trial of the canalith repositioning procedure. Otolaryngol--Head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg. 1995 Dec;113(6):712–720. doi: 10.1016/S0194-59989570010-2. [DOI] [PubMed] [Google Scholar]
- McClure J.A. Horizontal canal BPV. J. Otolaryngol. 1985 Feb;14(1):30–35. [PubMed] [Google Scholar]
- Moon S.Y., Kim J.S., Kim B.K. Clinical characteristics of benign paroxysmal positional vertigo in Korea: a multicenter study. J. Korean Med. Sci. 2006 Jun;21(3):539–543. doi: 10.3346/jkms.2006.21.3.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagnini P., Nuti D., Vannucchi P. Benign paroxysmal vertigo of the horizontal canal. ORL J Oto-Rhino-Laryngol Its Relat Spec. 1989;51(3):161–170. doi: 10.1159/000276052. [DOI] [PubMed] [Google Scholar]
- Parnes L.S., Agrawal S.K., Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV) CMAJ Can Med Assoc J J Assoc Medicale Can. 2003 Sep 30;169(7):681–693. [PMC free article] [PubMed] [Google Scholar]
- Pérez P., Manrique C., Alvarez M.J., Aldama P. [Evaluation of benign paroxysmal positional vertigo in primary health-care and first level specialist care] Acta Otorrinolaringol. Esp. 2008 Jul;59(6):277–282. [PubMed] [Google Scholar]
- Pérez P., Franco V., Cuesta P. Recurrence of benign paroxysmal positional vertigo. Otol Neurotol Off Publ Am Otol Soc Am Neurotol Soc Eur Acad Otol Neurotol. 2012 Apr;33(3):437–443. doi: 10.1097/MAO.0b013e3182487f78. [DOI] [PubMed] [Google Scholar]
- Rashad U.M. Long-term follow up after Epley's manoeuvre in patients with benign paroxysmal positional vertigo. J. Laryngol. Otol. 2009 Jan;123(1):69–74. doi: 10.1017/S0022215108002430. [DOI] [PubMed] [Google Scholar]
- Schuknecht H.F. Cupulolithiasis. Arch Otolaryngol Chic Ill. 1960;90(6):765–778. doi: 10.1001/archotol.1969.00770030767020. 1969 Dec. [DOI] [PubMed] [Google Scholar]
- Sekine K., Imai T., Sato G. Natural history of benign paroxysmal positional vertigo and efficacy of Epley and Lempert maneuvers. Otolaryngol--Head Neck Surg Off J Am Acad Otolaryngol-Head Neck Surg. 2006 Oct;135(4):529–533. doi: 10.1016/j.otohns.2005.09.021. [DOI] [PubMed] [Google Scholar]
- Tan J., Deng Y., Zhang T. Clinical characteristics and treatment outcomes for benign paroxysmal positional vertigo comorbid with hypertension. Acta Otolaryngol. 2017 May;137(5):482–484. doi: 10.1080/00016489.2016.1247985. [DOI] [PubMed] [Google Scholar]
- von Brevern M., Radtke A., Clarke A.H. Migrainous vertigo presenting as episodic positional vertigo. Neurology. 2004 Feb 10;62(3):469–472. doi: 10.1212/01.wnl.0000106949.55346.cd. [DOI] [PubMed] [Google Scholar]
- von Brevern M., Bertholon P., Brandt T. Benign paroxysmal positional vertigo: diagnostic criteria. J Vestib Res Equilib Orientat. 2015;25(3–4):105–117. doi: 10.3233/VES-150553. [DOI] [PubMed] [Google Scholar]
- Zucca G., Valli S., Valli P. Why do benign paroxysmal positional vertigo episodes recover spontaneously? J Vestib Res Equilib Orientat. 1998 Aug;8(4):325–329. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.