Abstract
Background
The sequential activation of immediate early (IE), early (E) and late (L) genes is required to allow productive herpes simplex virus type 1 (HSV-1) infection. Several evidences suggest that, together with inflammation, an immunological response incapable to counteract HSV-1 reactivation plays a role in the pathogenesis of Alzheimer’s (AD) and Parkinson’s (PD) diseases. IFN-lambda (IFN-λ), a cytokine endowed with a robust antiviral activity, contains HSV-1 reactivation. HSV-1-induced IFN-λ, IL-10 and IL-1β as well as the expression of viral IE, E and L genes were analyzed in vitro in peripheral blood mononuclear cells (PBMC) of AD and PD patients as well as of healthy controls (HC).
Methods
PBMC of AD, PD and HC were in vitro infected with one multiplicity of infection (1 MOI) HSV-1. IE, E, and L viral genes transcription as well as IFN-λ, IL-10 and IL-1β production were analyzed.
Results
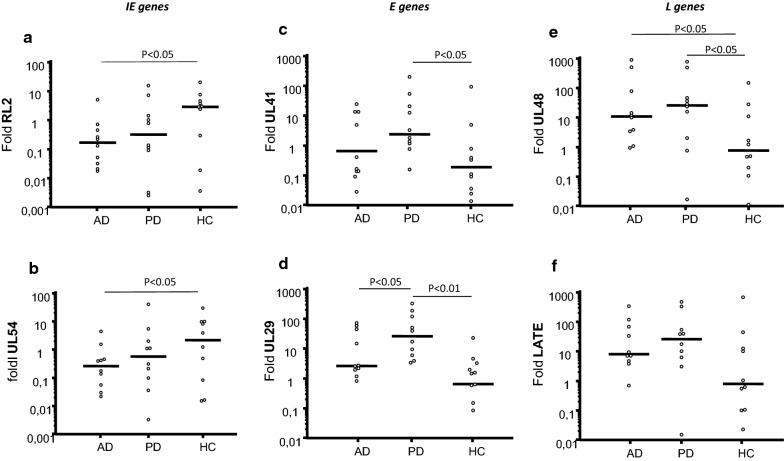
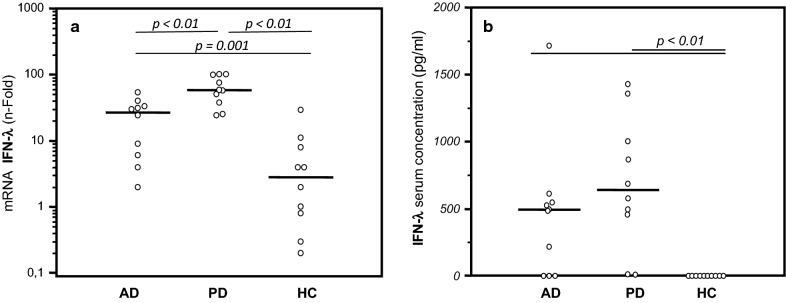
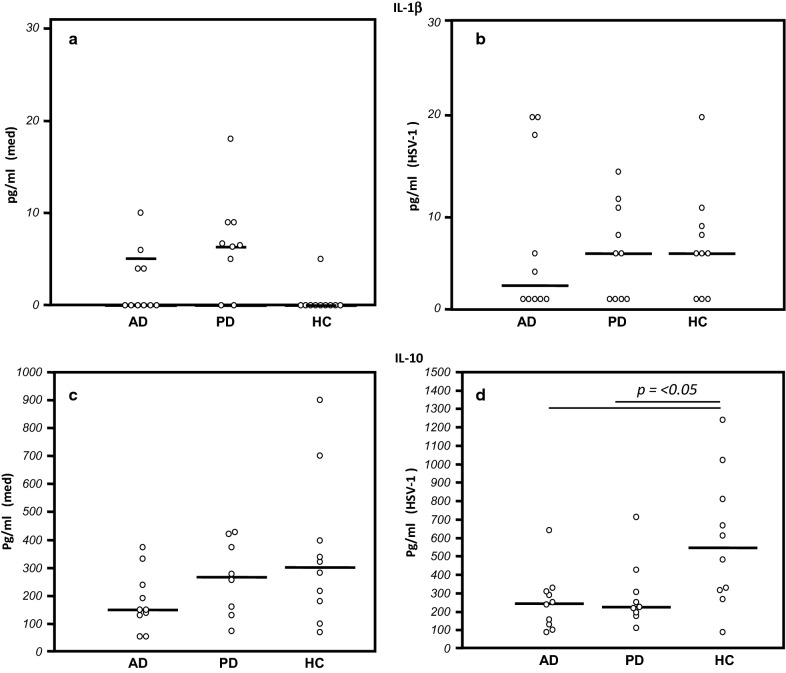
In HSV-1-infected cells of AD and PD patients compared to HC: (1) transcription of IE (ICP0, ICP27) genes was reduced whereas that of E (UL41, UL29) and L (UL48, LAT) genes was increased; (2) IFN-λ mRNA expression was increased. IL-1β was augmented and IL-10 was reduced in unstimulated cells of AD and PD compared to HC; HSV-1 infection significantly increased IL-10 production in HC alone.
Conclusions
Data herein show that a proinflammatory condition is present in AD and PD, in whom attempts to obstacle viral replication via an initial, possibly more potent IFN-λ-mediated control of IE viral genes is unsuccessful.
Keywords: Alzheimer’s disease, HSV-1, Immune response, IFN-λ, Parkinson’s disease
Background
Alzheimer’s disease (AD) and Parkinson’s disease (PD) are neurodegenerative disorders characterized by cognitive and behavioral alterations that lead to personality changes and to a decline in cognitive abilities combined with loss of mental function [1, 2]. Both pathologies are characterized by the accumulation in the brain of misfolded proteins [3, 4]: amyloid-beta (Aβ) in AD and alpha-synuclein (α-syn) in PD, as well as by neuroinflammation, which is driven both by microglial cells and by peripheral monocytes which cross the blood brain barrier (BBB) following a gradient of inflammatory cytokines [5]. This is supported both by PET imaging, showing an increased permeability of the BBB, and by the elevated levels of proinflammatory cytokines in the peripheral blood of PD and AD patients [6–8]: the pathogenesis of these pathologies is only scarcely understood but it is known to include genetic [9–11] and environmental factors [12, 13]. Several pathogens are also hypothesized to be involved in the pathogenesis of AD and PD [14–21]; herpes simplex virus type 1 (HSV-1), in particular, is suspected to play a role in these diseases [16, 22–24].
HSV-1 is a double-stranded DNA virus that belongs to the alphaherpesvirinae subfamily; HSV-1 infection is widespread as more than 70–90% of the world population are believed to be infected by this virus [25]. After the initial infection of epithelial cells, HSV-1 can spread to central nervous system (CNS) and establish a life-long latent infection in the peripheral nervous system [26]. HSV-1 latent infection is characterized by periodical bursts of reactivation that can be asymptomatic, can cause herpes labialis, or, in rare circumstances, if they take place in the central nervous system, can result in meningitis or encephalitis [27, 28]. HSV-1 reactivations are controlled by the immune response; it is hypothesized that if this equilibrium is lost, excessive HSV-1 replication together with neuroinflammation can become an important factor in the pathogenesis of AD and PD [23, 24, 29, 30].
The production of viral particles observed during viral reactivation depends on the coordinated expression of three classes of viral genes: the immediate early (IE), early (E), and late (L) genes [31]. IE and E proteins along with DNA replication are required for the efficient transcription of L genes [32]. Although HSV-1 uses many strategies of immunoevasion [33], innate and adaptive immune responses are activated to control virus replication and infection: IFN-lambda (λ) in particular plays a key role in containing HSV-1 reactivation [34–39].
To analyze whether HSV-1 replication and innate immune defences differ in AD and PD compared to healthy controls (HC) we used an in vitro model of HSV-1 infection. Results herein indicate that both viral replication and innate immune responses are indeed different when AD and PD cells are compared to those of HC.
Methods
Patients and controls
Ten AD and ten PD HSV-1 seropositive patients that fulfilled inclusion criteria for a clinical diagnosis of AD and PD were enrolled from the Rehabilitative Neurology Unit at the Don Carlo Gnocchi Foundation in Milano, Italy. All patients underwent a clinical interview, neurological and neuropsychological examination, laboratory analysis, CT scan or MRI, and other investigations (e.g., EEG, SPET scan, CSF examination, etc.) to exclude reversible causes of dementia. The clinical diagnosis of AD was performed according to the NINCDS-ADRDA work group criteria [40] and the DMS IV–R [41]. Neuropsychological evaluation and psychometric assessment were performed with a Neuropsychological Battery that included: MiniMental State Examination (MMSE), Digit Span Forward and Backward, Logical Memory and Paired Associated Words Tests, Token Test, supra Span Corsi Block Tapping Test, Verbal Fluency Tasks, Raven Colored Matrices, the Rey Complex Figure, Clinical Dementia Rating Scale (CDR) [42, 43].
Diagnosis of PD was based on the Queen Square Brain Bank Criteria [44]. Disease stage has been defined for all the PD according to modified Hoehn and Yahr (HYR) criteria [45]. All but one PD subjects received dopaminergic treatment at the moment of sampling. The study conformed to the ethical principles of the Helsinki Declaration.
Ten sex- and age-matched HSV-1 seropositive healthy controls (HC) as well as six HSV-1 seronegative individuals were also enrolled in the study.
These individuals were selected according to the SENIEUR protocol for immuno-gerontological studies of European Community’s Control Action Program on Aging [46] and were without a family history of dementia or evidence of acute or chronic neurologic diseases at the time of enrollment. The cognitive status of HC was assessed by MMSE (score for inclusion as normal control subjects ≥ 30). Finally, 6 HSV-1-seronegative individuals (3AD, 3HC) were also enrolled in the study.
Informed consent was obtained from all of the blood donors; the ethics committee of the Don Carlo Gnocchi Foundation in Milano, Italy approved the study.
Analysis HSV-1 seropositivity
Sera that had been banked at − 80 °C were used for serological analysis; serum HSV1-IgG titers were measured using commercially available enzyme immunoassays (ELISA) (IBL International, Hamburg, Germany) in accordance with the manufactures instructions. The assay sensitivity was 98.7%, whereas the specificity was 100%. Subjects with antibody index (AI) > 1.1 were considered seropositive, in accordance with the manufactures instructions.
Sample preparation
Whole blood was collected in vacutainer tubes containing ethylenediaminetetraacetic acid (EDTA) (Becton–Dickinson & Co., Rutherford, NJ, USA). Peripheral blood mononuclear cells (PBMC) were separated on lympholyte separation medium (Cedarlane, Hornby, Ontario, CA) and washed twice in PBS at 1000 g for 10 min; viable leukocytes were determined using a TC20 Automated Cell Counter (Biorad Hercules, CA, USA).
Virus preparation
HSV-1 (clinical isolate) was amplified and titred in Vero cells (African Green monkey kidney cells, ATCC CCL81) grown in Dulbecco’s modified Eagle medium (DMEM) containing 2 mM l-glutamine, 1% penicillin (Euroclone, Pero, Milan, Italy) and 10% fetal bovine serum (FBS), and maintained in an incubator with CO2 at 5% and 37 °C. For virus amplification, monolayers of Vero cells were infected with 0.01 multiplicity of infection (MOI)(1 plaque formation units (PFU) per 100 cells) of HSV-1 and incubated at 37 °C with CO2 at 5%. Seventy-two hours later infected cells were submitted to freeze–thaw and the viral suspension was aliquoted and stored at − 80 °C. Virus titation was performed in duplicate using six wells plates. Virus was submitted to limiting dilution (10−1 to 10−6) and 400 µL of each dilution were inoculated on Vero cells and incubated at 37 °C in 5% CO2 for 1 h and 30 min. The inoculum was then removed and 3 mL of DMEM plus 2% low-melting point agarose were added to each well. After 72 h, viral titers were calculated using the plaque-forming unit/ml (PFU/mL) method [47].
Virus-infection
PBMC were cultured overnight in RPMI 1640 supplemented with 10% human serum, 2 mM l-glutamine, and 1% penicillin (medium)(Euroclone). 1.3/106 cells/well plated in 96-wells plates were incubated for 1 h at 37 °C in 5% CO2 with serum-free RPMI alone (Medium) or with 1 MOI HSV-1 [36, 48].
Cells culture
After infection, PBMC were washed with phosphate-buffered saline (PBS) and were cultured in 6-wells plate with RPMI 1640 supplemented with 2 mM l-glutamine, 1% penicillin and 2% human serum. One, 4, and 6 h (see Additional file 1) post infection (p.i.) cells were collected for RNA extraction; 24 h p.i. supernatants were recovered used for cytokines quantification.
HSV-1 DNA extraction
HSV-1 DNA was extracted from supernatants of culture cells using the spin-columns technique (Nucleospin Tissue, Macherey–Nagel, Duren, Germany) according to the manufacturer instructions. DNA concentration was measured using a spectrophotometer (OD: 260 nm).
ApoE and IFN-λ genotyping
Genomic DNA was isolated from whole blood by phenol–chloroform extraction. Customer-design Taqman probes for the 112 and 158 codons were used to determine the genotype of Apolipoprotein E gene (ApoE) [49].
Single nucleotide polymorphism (SNP) rs12979860 IFN-λ was typed as previously described [50].
RNA-extraction
Total mRNA was extracted from unstimulated PBMC as well as from PBMC 1, 4 and 6 h after HSV-1 infection using the RNA easy Mini extraction kit (Qiagen, Hilden, Germany) and was eluted in RNAse-Free water. Total RNA concentration was determined by spectrophotometer (OD: 260 nm). Purity was determined as the 260 nm/280 nm OD ratio with expected values between 1.8 and 2.0. RNA was treated with TURBO DNA free DNAse (Ambion INC, Austin, TX, USA) and retro transcribed with High-capacity cDNA Reverse Transcription Kit (Applied Biosystems, Foster City, CA, USA), as specified by manufacturers. cDNA samples were stored at – 20 °C until use.
Analysis of gene expression by reverse transcription-polymerase chain reaction (RT-PCR)
Quantitative RT-PCR was performed using the RT2 SYBR Green qPCR mastermix (Qiagen, Hilden, Germany); glyceraldehyde 3-phosphate dehydrogenase (GAPDH), IFN-λ expression was analyzed 4 h p.i. Primers (Qiagen, Hilden, Germany) were cDNA specific; after calculation of 2ΔΔCt (where Ct is the cycle threshold) between the target gene and GAPDH housekeeping mRNA, results were expressed as ratios between stimulated and unstimulated (medium) cells (n-Fold). Experiments were individually run on each one of the individuals included in the study.
qPCR using TaqMan universal master mix (Life Technologies, Carlsbad, CA, US) was used to quantify exogenous HSV-1 copies and viral genes. The HSV-1 DNA polymerase gene (UL30) was amplified to estimate the amount of viral DNA in each supernatant (copies/ml). Immediate early RL2/ICP0 and UL54/ICP27 (RNA extracted 1 h p.i.), early UL29/ICP8 and UL41 (RNA extracted 4 h p.i.), and late UL48/VP16 and LAT genes (RNA extracted 6 h p.i.) were amplified from cDNA. The YWHAZ gene (ID: Hs03044281_g1, Life Technologies) was used as reference. qPCR amplifications were performed by Biorad CFX Real-Time PCR instrument (Biorad, Hercules, California, USA); all experiments were performed in triplicate. For primers and probe sequences, see Table 1; the primers used for HSV-1 genes were selected on the base of previous published works [51–55], but a cross-reactivity with other endogenous viruses, most specifically with the closely related HSV-2, cannot be excluded.
Table 1.
Primers and probes used for quantification of HSV-1 viral genes
| Gene name | Protein name | Primer/probe | Sequence | References |
|---|---|---|---|---|
| RL2 | ICP0 | Primer F | 5′-AACTCGTGGGTGCTGATTGAC-3′ | [51] |
| Primer R | 5′-CAGGTCTCGGTCGCAGGGAAAC-3′ | |||
| Probe | 5′FAM-AGCCCGCCCCGGATGTCTGGG-TAMRA 3′ | |||
| UL29 | ICP8 | Primer F | 5′-CACCAGGTTGCGCATCAG-3′ | [53] |
| PRIMER R | 5′-CTGCATACGGTGGTGAACAAC-3′ | |||
| Probe | 5′FAM-ACCTCGCGGTCCACG-TAMRA-3′ | |||
| UL54 | ICP27 | Primer F | 5′-CGCCAAGAAAATTTCATCGAG-3′ | [49] |
| Primer R | 5′-ACATCTTGCACCACGCCAG-3′ | |||
| Probe | 5′FAM-CTGGCCTCCGCCGACGAGAC-TAMRA 3′ | |||
| UL30 | HSV pol | Primer F | 5′-CATCAGCGACCCGGAGAGGGAC-3′ | [50] |
| Primer R | 5′-GGGCCAGGCGCTTGTTGGTGTA-3′ | |||
| Probe | 5′FAM-CCGCCGAACTGAGCAGACACCCGCGC-TAMRA3′ | |||
| UL48 | VP16 | Primer F | 5′-CCGGGTCCGGGATTTACC-3′ | [52] |
| Primer R | 5′-CTCGAAGTCGGCCATATCCA-3′ | |||
| Probe | 5′FAM-CCCCACGACTCCGCC-TAMRA 3′ | |||
| UL41 | UL41 | Primer F | 5′-GGACATCCGCGACGAAAAC-3′ | [52] |
| Primer R | 5′-AGAAACCTGTCGGCGATATCAG-3′ | |||
| Probe | 5′FAM-CTGGCGCGATCTATC-TAMRA 3′ | |||
| LAT | LAT | Primer F | 5′-GCATAGAGAGCCAGGCACAAAA-3′ | [52] |
| Primer R | 5′-ACGTACTCCAAGAAGGCATGTG-3′ | |||
| Probe | 5′FAM-TCCCACCCCGCCTGTG-TAMRA 3′ |
ELISA
IL-1β, IFN-lambda (λ) (IL-29) and IL-10 concentration in the supernatants of PBMC that were or were not HSV-1 infected analyzed by ELISA immunoassays according to the manufacturer’s instructions (ThermoFisher, Waltham, MA, USA). A plate reader (Sunrise, Tecan, Mannedorf, Switzerland) was used and optical densities (OD) were determined at 450/620 nm. IFN-lambda (λ) serum concentration was measured using the same immunoassay.
Statistical analysis
Quantitative data distribution was analyzed by Shapiro–Wilk test. Normally distributed data were summarized as mean and standard deviation (SD), and comparison among groups were analyzed by ANOVA test and Student t test. Not-normally distributed data were summarized as median and interquartile range (IQR: 25th and 75th percentile), and comparisons were analyzed by Kruskal–Wallis test and Mann–Whitney U test, as appropriate. Data analysis was performed using the MedCalc statistical package (MedCalc Software bvba, Mariakerke Belgium). p-values < 0.05 were considered statistically significant.
Results
Demographic and clinical characterization
The demographic and clinical characterization of the individuals enrolled in the study is shown in Table 2. Gender and age were comparable in the three groups examined. ApoE e4 was 2.5-fold elevated in AD and 2.0-fold in PD compared to HC although without reaching statistical differences probably due to the small number of subjects of the our cohort.
Table 2.
Demographic, clinical and genetic characteristics of the individuals enrolled in the study
| Alzheimer’s disease patients (AD) | Parkinson disease patients (PD) |
Healthy controls (HC) |
|
|---|---|---|---|
| N | 10 | 10 | 10 |
| Gender (M:F) | 5:5 | 7:3 | 4:6 |
| Age (years) | 78.50 ± 5.44 | 80.22 ± 5.21 | 78.90 ± 5.95 |
| MMSE | 19.07 ± 2.51 | – | 30 |
| Y&H | – | 2.72 ± 0.94 | – |
| ApoE ε-4 carriers (%) | 50 | 40 | 20 |
Data are expressed as mean ± standard deviation
MMSE: Mini-Mental State Examination
Y&H: Hoehn and Yahr Scale
HSV-1 viral load and gene expression
HSV-1 viral load in supernatants 24 h post-infection was comparable among the three groups, with the highest values being observed in PD patients (AD: 4.83 × 106 ± 1.98 × 106 copies/ml; PD: 5.31 × 106 ± 1.57 × 106 copies/ml; HC: 5.16 × 106 ± 1.94 × 106 copies/ml). No significant differences were observed in the HSV-1 seronegative group (see Additional file 2).
The expression of immediate early, early and late HSV-1 genes was analyzed next. Results showed that expression of immediate early genes ICP0 and UL54 was decreased in AD and PD compared to HC; these differences reached statistical significance in the case of AD cells (RL2: p = 0.02 vs. HC. UL54: p = 0.04 vs. HC) (Fig. 1).
Fig. 1.
HSV-1 genes expression: Left panels. HSV-1 RL2 (a) and UL54 (b) immediate early (IE) genes. Central panels. HSV-1 UL41 (c) and UL29 (d) early (E) genes. Right panels. HSV-1 UL48 (e) and LATE (f) late (L) genes. HSV-1-infected PBMC of AD and PD patients and Healthy Control (HC) were used to generate the results. Data are expressed as median; statistical significance is shown
The pattern of expression of early and late genes was totally different. Thus, all the four analyzed early and late viral genes were over-expressed upon HSV-1 infection of cells of AD and PD patients compared to HC. In particular, in PD, the expression of the UL41 (p = 0.02) and UL29 (p = 0.003) early genes as well as that of the UL48 (p = 0.04) late gene was significantly increased compared to HC. In AD, expression of the UL48 late gene was significantly increased in comparison with HC (p = 0.04). Interestingly, expression of all early and late genes was higher in PD compared to AD patients, reaching statistical significance for the UL29 early gene (p = 0.04) (Fig. 1). Unormalized qPCR data were summarized in additional file (see Additional file 3). A similar pattern of gene expression observed in HSV-1—uninfected individuals.
IFN-λ mRNA expression and serum concentration
IFN-λ (IL-29) is a cytokine that is part of the innate immune response and is endowed with a potent antiviral activity. IFN-λ (IL-29) mRNA was measured in PBMC that were infected or not with HSV-1,as well as serum concentration was detected in all subjects enrolled. Results showed that IFN-λ mRNA expression was significantly increased in PD and AD patients compared to HC (p = 0.001 and p = 0.003, respectively), and in AD compared to PD (p = 0.005) (Fig. 2). Similar results were obtained when serum concentration of IFN-λ (IL-29) was measured. Thus, IFN-λ (IL-29) serum concentration was significantly increased in AD and PD patients compared to HC (p < 0.01 in both cases) (Fig. 2). When IFN-λ production was measured in supernatant by unstimulated and by HSV-1 stimulated PBMC, this cytokine could not be detected in any sample, possibly because of the low sensitivity of the method used (data not shown). A similar pattern of IFN-λ mRNA expression and serum concentration was observed in HSV-1–uninfected individuals. These results indicate that a much more prompt and potent IFN-λ (IL-29)-mediated antiviral innate immune response is elicited in AD and PD compared to what is observed in HC.
Fig. 2.
IFN-λ mRNA-expression and serum concentration. a IFN-λ mRNA expression in HSV-1-infected cells of HSV-1-infected PBMC from AD and PD patients and Healthy Control (HC). b IFN-λ serum concentration in AD and PD patients and Healthy Control (HC). Data are expressed as median, each dot represents IFN-λ gene or protein production by single individual. Statistical significance is shown
IL-1β and IL-10 production
Cytokines production was evaluated by immunoassay (ELISA) in supernatants of PBMC that were either cultured in medium alone or infected with HSV-1. Results showed that IL-1β production was already increased in unstimulated cells of AD and PD patients compared to HC, even if these differences were not statistically significant.
HSV-1 stimulation induced IL-1β production by cells of HC but did not modify the production of this cytokine by cells of AD and PD. IL-10 production, on the other hand, was slightly increased in HC compared to AD and PD in unstimulated conditions and was significantly increased by HSV-1 infection in HC alone (AD and PD vs. HC p < 0.05) (Fig. 3).
Fig. 3.
Cytokines production: IL-1β (upper panels) and IL-10 (lower panels) production by PBMC of AD and PD patients and Healthy Control (HC) that were cultured in medium alone (med) (a, c) or were stimulated with HSV-1 (b, d). Data are expressed as median, each dot represents IL-1β or IL-10 protein production by single individual. Statistical significance is shown
Finally, possibly because of the small number of individuals examined, no correlation was found between the examined immunological and virological parameters and either ApoE or IFN-λ genotypes in any of the groups enrolled in the study. Again similar pattern of cytokine production was observed in HSV-1–uninfected individuals.
Discussion
Viral infections, and in particular infection with HSV-1, have long been suspected to play a pathogenic role in AD; more recently a possible role for this virus has also been suggested in the pathogenesis of PD. HSV-1 infection remains latent in the nervous system after primary infection;
the hypothesis is supported by research data implicating brain infections by HSV-1 [16, 30]. Viruses are prevalent in AD brains and can evade the host immune system forming latent or chronic infections, interact with genetic and environmental factors to initiate accumulation and/or formation of Aβ, hyperphosphorylation of tau proteins, and inflammation in the brain [21].
Periodic reactivations are hypothesized to be associated with AD and PD, as suggested by a number of results. Thus, in AD: (1) HSV-1 encephalitis involves the hippocampus as well as the temporal and frontal lobes, these are the same brain area that are affected in AD; (2) HSV-1 genome is found in the hippocampus and in the temporal and frontal lobes brains of sporadic AD patients; (3) the combination of ApoE 4 allele, a genetic risk factor for AD, and HSV-1 infection, greatly augments the risk of developing AD; (4) HSV-1 DNA colocalizes with Aβ; (5) the phosphorylation of tau, which is characteristically seen in AD, is enhanced by HSV-1 infection in in vitro and in animal models [16, 19, 20, 56, 57]; and (6) Aβ and HSV-1 cross-reactive antobodies can be observed in patients [19, 58, 59]. In the case of PD, a possible HSV-1 pathogenetic role is suggested by results indicating that cross reactivity between HSV-1 and α-synuclein stimulates autoimmune responses targetting neurons of the substantia nigra [23]. Taken together these results support the hypothesis that periodic HSV-1 reactivation in the CNS could facilitate the onset of AD and PD, possibly as an effect of direct neuronal damage and of the neuroinflammatory milieu which is driven by viral reactivations [5, 19, 20, 37, 59–61].
Herein we report results obtained in an in vitro system in which peripheral blood immune cells of AD and PD patients as well as of HC were infected with HSV-1. All the individuals enrolled in the study were HSV-1 seropositive, thus, in this in vitro model we evaluated virus-specific secondary immune responses. Results showed that both HSV-1 gene expression and HSV-1-stimulated immune responses are different in patients compared to controls. Thus, the expression of IE (ICP0 and ICP27) genes was reduced in AD and PD, compared to controls. IE genes products activate the transcription of early genes, which are expressed prior to DNA replication, and, subsequently, that of late genes. In contrast to what was observed with IE genes, the expression of both early (UL41, UL29) and late (UL48, LAT) genes was higher in both groups of patients compared to HC.
Viral replication is initially contained by innate immunity; IFN-λ plays a pivotal role in this process. Recent results showing that IFN-λ production is significantly augmented in patients with a diagnosis of Mild Cognitive Impairment who do not convert into AD over a 24 months period reinforce the idea that that innate immunity and IFN-λ in particular, are important players in protection against AD [8]. The observation herein upon IFN-λ mRNA and serum concentration were significantly increased in both groups of patients suggest that the initial reduction of IE genes transcription is an immune-mediated attempt to obstacle HSV-1 replication, an attempt that is clearly ineffective, as indicated by the augmented transcription rates of E and L viral genes.
Because HSV-1 reactivations is tightly linked to neuroinflammation we analyzed pro- and anti-inflammatory cytokines in our system as well. Results indicated that unstimulated IL-1β production was slightly increased in AD and PD compared to HC whereas that of the anti-inflammatory cytokine IL-10 was reduced in patients compared to controls. Notably, IL-10 production upon in vitro HSV-1 infection was significantly increased in HC alone. IL-10 reduces antigen-stimulation proliferation and dampens immune responses by down modulating the generation of pro-inflammatory cytokines [62–64]. That IL-10 production is reduced in chronic neurodegenerative diseases is known [63, 65]. The results obtained in this in vitro infection system reinforce the observation that inflammation characterizes AD and PD, suggesting that the ability of immune cells of these individuals to secrete IL-10 in response to a viral insult is defective or exhausted. A small group of HSV-1 seronegative AD and HC was also included in the study and interestingly after in vitro infection, immunological and virological results obtained in these individuals overlapped those obtained in HSV-seropositive subjects.
Overall, these results confirm previously published data [8, 65, 66] and support the idea that a constitutive proinflammatory milieu is present in chronic neurodegenerative diseases, including AD and PD.
Notably, ApoE was shown to play a role in the modulation of innate immunity. In humans there are three well-described major isoforms of ApoE: ApoE-ε4, ApoE-ε3 and ApoE-ε2, which are encoded by allelic variants of the ApoE gene on chromosome 19. ApoE-ε4 was observed to be more frequent in diseases in which innate immunity plays a role, including AD, and, more recently, viral infection [67, 68]. The presence of single copy apoε4 was also shown to associate with increased production of IL-1β, IL-6, and IFN-λ by TLR-2 and TLR-4 agonists-stimulated cells [69]. Possibly because of the limited number of individuals analyzed in this study, no association between ApoE genotype and immunological data was observed; further investigations in larger cohorts of subjects will be needed to verify possible associations between ApoE isofoms and the virological and immunological parameters examined herein. Moreover, although virus-induced pathology is modulated by ApoE-ε4, it has been reported that ApoE does not modulate HSV shedding [70] so that similar viral loads are to be expected independently of ApoE genotype.
Herein, because IL-1β is also endowed with direct antiviral properties it is nevertheless tempting to speculate that a constitutive production of this cytokine by cells of AD and PD patients could be an additional attempt to prevent viral reactivation.
Conclusion
Although further studies will be necessary to confirm these findings, results herein indicate that, at least in our in vitro system, HSV-1-specific immune responses differ when healthy controls are compared to AD and PD. In these patients such responses could be geared toward a ineffective control of viral replication through innate immunity-mediated mechanisms.
Supplementary information
Additional file 1. Experiment performed in THP-1 cell line to determine the best timing of HSV-1 gene expression.
Additional file 2. Summary statistics table of HSV-1 genes and IFN-lambda mRNA expression, and cytokines concentration.
Additional file 3. Raw data of HSV-1 gene expression.
Acknowledgements
The authors thank all the subjects enrolled in the study; we are particularly grateful to Prof. Nemni and all the staff of the AD and PD Rehabilitative Neurology Unit of Don Carlo Gnocchi Foundation in Milano and the unit of Day Hospital of IRCCS S. Maria Nascente for taking care of our patients.
Abbreviations
- Aβ
amyloid-beta
- AD
Alzheimer’s disease
- α-syn
alpha-synuclein
- ANOVA
analysis of variance
- BBB
blood brain barrier
- CNS
central nervous system
- CDR
Clinical Dementia Rating Scale
- DMEM
Dulbecco’s modified Eagle medium
- E
early genes
- FBS
fetal bovine serum
- HC
healthy control
- HSV-1
herpes simplex virus type 1
- IFN-λ
IFN-lambda
- IE
immediate early
- IL-1β
Interleukin-beta
- IL-10
interleukin-10
- L
late genes
- MMSE
MiniMental State Examination
- MOI
multiplicity of infection
- MRI
magnetic resonance imaging
- PBMC
peripheral blood mononuclear cells
- PD
Parkinson’s disease
Authors’ contributions
Conceived and designed experiments: FLR, SA, MS, MC. Recruited patients and collected clinical data: AB, RN; Performed the virological experiments: SA; Performed immonological experiments: FP and IM; Performed analysis: SA, FLR. Wrote the paper: FLR, AS, MC. All authors read and approved the final manuscript.
Funding
This work was supported by 2017–2018 Ricerca Corrente (Italian Ministry of Healthy).
Availability of data and materials
The data that support the findings of this study are available on request from the corresponding author [FLR]. The dataset supporting the conclusions of this article is included within the article and its additional file.
Ethics approval and consent to participate
The research protocol was approved by the ethics committees of Don C. Gnocchi Foundation, IRCCS S. Maria Nascente in Milan, Italy.
Consent for publication
All participant gave informed consent before taking part in this study.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Francesca La Rosa and Simone Agostini are Co-Authors
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12967-019-2034-9.
References
- 1.de Lau LM, Breteler MM. Epidemiology of Parkinson’s disease. Lancet Neurol. 2006;5(6):525–535. doi: 10.1016/S1474-4422(06)70471-9. [DOI] [PubMed] [Google Scholar]
- 2.Blennow K, Zetterberg H. Biomarkers for Alzheimer’s disease: current status and prospects for the future. J Intern Med. 2018;284(6):643–663. doi: 10.1111/joim.12816. [DOI] [PubMed] [Google Scholar]
- 3.Ross CA, Poirier MA. Protein aggregation and neurodegenerative disease. Nat Med. 2004;10(Suppl):S10–S17. doi: 10.1038/nm1066. [DOI] [PubMed] [Google Scholar]
- 4.Wang X, Huang T, Bu G, Xu H. Dysregulation of protein trafficking in neurodegeneration. Mol Neurodegener. 2014;9:31. doi: 10.1186/1750-1326-9-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caggiu E, Paulusb K, Gallerib G, Arrub G, Manettib R, Sechib GP, et al. Homologous HSV1 and alpha-synuclein peptides stimulate a T cell response in Parkinson’s disease. J Neuroimmunol. 2017;310:26–33. doi: 10.1016/j.jneuroim.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 6.Moura KC, Campos JM, de Rosso AL, Nicaretta DH, Pereira JS, Silva DJ, et al. Genetic analysis of PARK2 and PINK1 genes in Brazilian patients with early-onset Parkinson’s disease. Dis Markers. 2013;35(3):181–185. doi: 10.1155/2013/597158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saresella M, La Rosa F, Piancone F, Zoppis M, Marventano I, Calabrese E, Rainone V, Nemni R, Mancuso R, Clerici M. The NLRP3 and NLRP1 inflammasomes are activated in Alzheimer’s disease. Mol Neurodegener. 2016;11:23. doi: 10.1186/s13024-016-0088-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.La Rosa F, Saresella M, Piancone F, Marventano I, Calabrese E, Nemni R, et al. Increased TLR8 and 9 expression correlates with preserved hippocampal volumes and lack of progression to AD in mild cognitive impairment individuals. J Alzheimers Dis. 2016;53:S34. [Google Scholar]
- 9.Castellano JM, Kim J, Stewart FR, Jiang H, DeMattos RB, Patterson BW, et al. Human apoE isoforms differentially regulate brain amyloid-beta peptide clearance. Sci Transl Med. 2011;3(89):89ra57. doi: 10.1126/scitranslmed.3002156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spratt DE, Martinez-Torres RJ, Noh JY, Mercier P, Manczyk N, Barber JR, et al. A molecular explanation for the recessive nature of parkin-linked Parkinson’s disease. Nat Commun. 2013;4:1983. doi: 10.1038/ncomms2983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barrett MJ, Koeppel AF, Flanigan JL, Turner SD, Worrall BB. Investigation of genetic variants associated with Alzheimer disease in Parkinson disease cognition. J Parkinsons Dis. 2016;6(1):119–124. doi: 10.3233/JPD-150706. [DOI] [PubMed] [Google Scholar]
- 12.Allen MT, Levy LS. Parkinson’s disease and pesticide exposure a new assessment. Crit Rev Toxicol. 2013;43:515–534. doi: 10.3109/10408444.2013.798719. [DOI] [PubMed] [Google Scholar]
- 13.Alegre-Abarrategui J, Brimblecombe KR, Roberts RF, Velentza-Almpani E, Tilley BS, Bengoa-Vergniory N. Selective vulnerability in α-synucleinopathies. Acta Neuropathologica. 2019 doi: 10.1007/s00401-019-02010-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marttila RJ, Arstila P, Nikoskelainen J, Halonen PE, Rinne UK. Viral antibodies in the sera from patients with Parkinson disease. Eur Neurol. 1977;15:25–33. doi: 10.1159/000114785. [DOI] [PubMed] [Google Scholar]
- 15.Takahashi M, Yamada T. Viral etiology for Parkinson’s disease a possible role of influenza A virus infection. Jpn J Infect Dis. 1999;52:89–98. [PubMed] [Google Scholar]
- 16.Itzhaki RF. Herpes and Alzheimer’s disease: subversion in the central nervous system and how it might be halted. J Alzheimers Dis. 2016;54(4):1273–1281. doi: 10.3233/JAD-160607. [DOI] [PubMed] [Google Scholar]
- 17.Jang H, Boltz DA, Webster RG, Smeyne RJ. Viral parkinsonism. Biochim Biophys Acta. 2009;1792(7):714–721. doi: 10.1016/j.bbadis.2008.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wozniak MA, Shipley SJ, Combrinck M, Wilcock GK, Itzhaki RF. Productive herpes simplex virus in brain of elderly normal subjects and Alzheimer’s disease patients. J Med Virol. 2005;75:300–306. doi: 10.1002/jmv.20271. [DOI] [PubMed] [Google Scholar]
- 19.Wozniak MA, Itzhaki RF, Shipley SJ, Dobson CB. Herpes simplex virus infection causes cellular beta-amyloid accumulation and secretase upregulation. Neurosci Lett. 2007;429:95–100. doi: 10.1016/j.neulet.2007.09.077. [DOI] [PubMed] [Google Scholar]
- 20.Wozniak MA, Mee AP, Itzhaki RF. Herpes simplex virus type 1 DNA is located within Alzheimer’s disease amyloid plaques. J Pathol. 2009;217:131–138. doi: 10.1002/path.2449. [DOI] [PubMed] [Google Scholar]
- 21.Harris SA, Harris EA. Molecular Mechanisms for Herpes Simplex Virus Type 1 Pathogenesis in Alzheimer’s Disease. Front Aging Neurosci. 2018;10:48. doi: 10.3389/fnagi.2018.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lam MM, Mapletoft JP, Miller MS. Abnormal regulation of the antiviral response in neurological/neurodegenerative diseases. Cytokine. 2016;88:251–258. doi: 10.1016/j.cyto.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 23.Caggiu E, Paulus K, Arru G, Piredda R, Sechi GP, Sechi A. Humoral cross reactivity between α-synuclein and herpes simplex-1 epitope in Parkinson’s disease, a triggering role in the disease? J Neuroimmunol. 2016;291:110–114. doi: 10.1016/j.jneuroim.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 24.Caggiu E, Arru G, Hosseini S, Niegowska M, Sechi G, Zarbo IR, Sechi LA. Inflammation, infectious triggers, and Parkinson’s disease. Front Neurol. 2019;10:122. doi: 10.3389/fneur.2019.00122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang J, Liu H, Wei B. Immune response of T cells during herpes simplex virus type 1 (HSV-1) infection. J Zhejiang Univ Sci B. 2017;18(4):277–288. doi: 10.1631/jzus.B1600460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mitchell BM, Bloom DC, Cohrs RJ, Gilden DH, Kennedy PG. Herpes simplex virus-1 and varicella-zoster virus latency in ganglia. J Neurvirol. 2003;9:194–204. doi: 10.1080/13550280390194000. [DOI] [PubMed] [Google Scholar]
- 27.Reske A, Pollara G, Krummenacher C, Chain BM, Katz DR. Understanding HSV-1 entry glycoproteins. Rev Med Virol. 2007;17:205–215. doi: 10.1002/rmv.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Heldwein EE, Krummenacher C. Entry of herpesviruses into mammalian cells. Cell Mol Life Sci. 2008;65(11):1653–1668. doi: 10.1007/s00018-008-7570-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Agostini S, Mancuso R, Baglio F, Clerici M. A protective role for herpes simplex virus type-1-specific humoral immunity in Alzheimer’s disease. Expert Rev Anti Infect Ther. 2017;15(2):89–91. doi: 10.1080/14787210.2017.1264271. [DOI] [PubMed] [Google Scholar]
- 30.Itzhaki RF. Herpes simplex virus type 1 and Alzheimer’s disease: possible mechanisms and signposts. FASEB. 2017;31:3216–3226. doi: 10.1096/fj.201700360. [DOI] [PubMed] [Google Scholar]
- 31.Roizman B, Zhou G. The 3 facets of regulation of herpes simplex virus gene expression: a critical inquiry. Virology. 2015;479–480:562–567. doi: 10.1016/j.virol.2015.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Koelle DM, Corey L. Recent progress in herpes simplex virus immunobiology and vaccine research. Clin Microbiol Rev. 2003;16:96–113. doi: 10.1128/CMR.16.1.96-113.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Su C, Zhan G, Zheng C. Evasion of host antiviral innate immunity by HSV-1, an update. Virol J. 2016;13:38. doi: 10.1186/s12985-016-0495-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Donnelly RP, Kotenko SV. Interferon-lambda: a new addition to an old family. J Interferon Cytokine Res. 2010;30:555–564. doi: 10.1089/jir.2010.0078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li J, Ye L, Wang X, Hu S, Ho W. Induction of IFN-lambda contributes to TLR3-mediated HSV-1 inhibition in astrocytes. J Neurosci Res. 2012;90(2):399–406. doi: 10.1002/jnr.22758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gosselin J, Flamand L, D’Addario M, Hiscott J, Stefanescu I, Ablashi DV. Modulatory effects of Epstein-Barr, herpes simplex, and human herpes-6 viral infections and co-infections on cytokine synthesis: a comparative study. J Immunol. 1992;149:181–187. [PubMed] [Google Scholar]
- 37.Gosselin J, Flamand L, D’Addario M, Hiscott J, Menezes J. Infection of peripheral blood mononuclear cells by herpes simplex and Epstein-Barr viruses: differential induction of interleukin 6 and tumor necrosis factor-a. J Clin Invest. 1992;89:1849–1856. doi: 10.1172/JCI115789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ahmad A, Sharif-Askari E, Fawaz L, Menezes J. Innate immune response of the human host to exposure with herpes simplex virus type 1: in vitro control of the virus infection by enhanced natural killer activity via interleukin-15 induction. J Virol. 2000;74:7196–7203. doi: 10.1128/JVI.74.16.7196-7203.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Akpek G, Joseph R, Gunay C, Kessler II, Shvartsbeyn M, Bhatnagar B, et al. Frequent detection of herpes simplex virus antigen in skin and peripheral blood CD34 + mononuclear cells from patients with graft-versus-host disease. Biol Blood Marrow Transplant. 2013;19:529–537. doi: 10.1016/j.bbmt.2012.12.021. [DOI] [PubMed] [Google Scholar]
- 40.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s Disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Service Task Force on Alzheimer’s Disease. Neurology. 1984;34(7):939–944. doi: 10.1212/WNL.34.7.939. [DOI] [PubMed] [Google Scholar]
- 41.American Psychiatric Association . Diagnostic and statistical manual of mental disorders DSM-IV-R. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 42.Folstein MF, Folstein SE, McHugh PR. Mini-mental state. A practical method for grading the cognitive state of patients for the clinicians. J Psychiat Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 43.Hughes CP, Berg L, Danziger WL, Coben LA, Martin RL. A new clinical scale for staging of dementia. Br J Psychiatry. 1982;140:566–572. doi: 10.1192/bjp.140.6.566. [DOI] [PubMed] [Google Scholar]
- 44.Gelb DJ, Oliver E, Gilman S. Diagnostic criteria for Parkinson disease. Arch Neurol. 1999;56:33–39. doi: 10.1001/archneur.56.1.33. [DOI] [PubMed] [Google Scholar]
- 45.Hoehn MM, Yahr MD. Parkinsonism: onset, progression, and mortality. Neurology. 1967;17(5):427–442. doi: 10.1212/WNL.17.5.427. [DOI] [PubMed] [Google Scholar]
- 46.Ligthart GJ, Corberand JX, Fournier C, Galanaud P, Hijmans W, Kennes B, et al. Admission criteria for immunogerontological studies in man: the SENIEUR protocol. Mech Ageing Dev. 1984;28:47–55. doi: 10.1016/0047-6374(84)90152-0. [DOI] [PubMed] [Google Scholar]
- 47.Spear PG, Roizman B. Proteins specified by herpes simplex virus. V. Purification and structural proteins of the herpesvirion. J Virol. 1972;9:143–159. doi: 10.1128/jvi.9.1.143-159.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Larcher C, Gasser A, Hattmannstorfer R, Obexer P, Furhapter C, Fritsch P, Sepp N. Interaction of HSV-1 infected peripheral blood mononuclear cells with cultured dermal microvascular endothelial cells: a potential model for the pathogenesis of HSV-1 induced erythema multiforme. J Invest Dermatol. 2001;116(1):150–156. doi: 10.1046/j.1523-1747.2001.00235.x. [DOI] [PubMed] [Google Scholar]
- 49.Mancuso R, Baglio F, Agostini S, Cabinio M, Laganà MM, Hernis A, et al. Relationship between herpes simplex virus-1-specific antibody titers and cortical brain damage in Alzheimer’s disease and amnestic mild cognitive impairment. Front Aging Neurosci. 2014;6:285. doi: 10.3389/fnagi.2014.00285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Costa AS, Agostini S, Guerini FR, Mancuso R, Zanzottera M, Ripamonti E, et al. Modulation of Immune Responses to Herpes Simplex Virus Type 1 by IFNL3 and IRF7 Polymorphisms: a Study in Alzheimer’s Disease. J Alzheimers Dis. 2017;60(3):1055–1063. doi: 10.3233/JAD-170520. [DOI] [PubMed] [Google Scholar]
- 51.Cohrs RJ, Randall J, Smith J, Gilden DH, Dabrowski C, van Der Keyl H, et al. Analysis of individual human trigeminal ganglia for latent herpes simplex virus type 1 and varicella-zoster virus nucleic acids using real-time PCR. J Virol. 2000;74:11464–11471. doi: 10.1128/JVI.74.24.11464-11471.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kaufman HE, Azcuy AM, Varnell ED, Sloop GD, Thompson HW, Hill JM. HSV-1 DNA in tears and saliva of normal adults. Invest Ophthalmol Vis Sci. 2005;46:241–247. doi: 10.1167/iovs.04-0614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mott KR, Underhill D, Wechsler SL, Town T, Ghiasi H. A role for the JAK-STAT1 pathway in blocking replication of HSV-1 in dendritic cells and macrophages. Virol J. 2019;6:56. doi: 10.1186/1743-422X-6-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Du T, Zhou G, Roizman B. HSV-1 gene expression from reactivated ganlia is disordered and concurrent with suppression of latency-associated transcripts and miRNAs. Proc Natl Acad Sci USA. 2011;108:18820–18824. doi: 10.1073/pnas.1117203108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ma JZ, Russell TA, Spelman T, Carbone FR, Tscharke DC. Lytic gene expression is frequent in HSV-1 latent infection and correlates with the engagement of a cell-intrinsic transcriptional response. PLoS Pathog. 2014;10:e1004237. doi: 10.1371/journal.ppat.1004237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Miklossy J. Emerging roles of pathogens in Alzheimer disease. Expert Rev Mol Med. 2011;3:e30. doi: 10.1017/S1462399411002006. [DOI] [PubMed] [Google Scholar]
- 57.Gema A, Aldudo J, Alonso M, Santana S, Valdivieso F. Herpes simplex virus type 1 induces nuclear accumulation of hyperphosphorylated tau in neuronal cells. J Neurosci Res. 2012;90(5):1020–1029. doi: 10.1002/jnr.23003. [DOI] [PubMed] [Google Scholar]
- 58.Cheng SB, Ferland P, Webster P, Bearer EL. Herpes simplex virus dances with amyloid precursor protein while exiting the cell. PLoS ONE. 2011;6:e17966. doi: 10.1371/journal.pone.0017966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Vojdani A, Vojdani E. Amyloid-Beta1-42 cross-reactive antibody prevalent in human sera may contribute to intraneuronal deposition of A-Beta-P-42. Int J Alzheimers Dis. 2018;2018:1672568. doi: 10.1155/2018/1672568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Itzhaki RF, Lin WR, Shang D, Wilcock GK, Faragher B, Jamieson GA. Herpes simplex virus type 1 in brain and risk of Alzheimer’s disease. Lancet. 1997;349:241–244. doi: 10.1016/S0140-6736(96)10149-5. [DOI] [PubMed] [Google Scholar]
- 61.De Chiara G, Marcocci ME, Civitelli L, Argnani R, Piacentini R, Ripoli C, et al. APP processing induced by herpes simplex virus type 1 (HSV-1) yields several APP fragments in human and rat neuronal cells. PLoS ONE. 2010;5:e13989. doi: 10.1371/journal.pone.0013989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tumpey TM, Cheng H, Yan XT, Oakes JE, Lausch RN. Chemokine synthesis in the HSV-1-infected cornea and its suppression by interleukin-10. J Leukoc Biol. 1998;63(4):486–492. doi: 10.1002/jlb.63.4.486. [DOI] [PubMed] [Google Scholar]
- 63.Yan XT, Zhuang M, Oakes JE, Lausch RNJ. Autocrine action of IL-10 suppresses proinflammatory mediators and inflammation in the HSV-1-infected cornea. J Leukoc Biol. 2001;69(1):149–157. [PubMed] [Google Scholar]
- 64.Azher TN, Yin XT, Stuart PM. Understanding the role of chemokines and cytokines in experimental models of herpes simplex keratitis. J Immunol Res. 2017 doi: 10.1155/2017/7261980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Saresella M, Calabrese E, Marventano I, Piancone F, Gatti A, Farina E, et al. A potential role for the PD1/PD-L1 pathway in the neuroinflammation of Alzheimer’s disease. Neurobiol Aging. 2012;33(3):624.e11–624.e22. doi: 10.1016/j.neurobiolaging.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 66.Dursun E, Gezen-Ak D, Hanağas H, Bilgiç B, Lohmann E, Ertan S, Atasoy IL, et al. The interleukin 1 alpha, interleukin 1 beta, interleukin 6 and alpha-2-macroglobulin serum levels in patients with early or late onset Alzheimer’s disease, mild cognitive impairment or Parkinson’s disease. J Neuroimmunol. 2015;283:50–57. doi: 10.1016/j.jneuroim.2015.04.014. [DOI] [PubMed] [Google Scholar]
- 67.Mahley RW, Rall SC., Jr Apolipoprotein E: far more than a lipid transport protein. Annu Rev Genomics Hum Genet. 2000;1:507–537. doi: 10.1146/annurev.genom.1.1.507. [DOI] [PubMed] [Google Scholar]
- 68.Kuhlmann I, Minihane AM, Huebbe P, Nebel A, Rimbach G. Apolipoprotein E genotype and hepatitis C, HIV and herpes simplex disease risk: a literature review. Lipids Health Dis. 2010;9:8. doi: 10.1186/1476-511X-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gale SC, Gao L, Mikacenic C, Coyle SM, Rafaels N, Murray Dudenkov T, Madenspacher JH, Draper DW, Ge W, Aloor JJ, Azzam KM, Lai L, Blackshear PJ, Calvano SE, Barnes KC, Lowry SF, Corbett S, Wurfel MM, Fessler MB. APOE 4 is associated with enhanced in vivo innate immune responses in human subjects. J Allergy Clin Immunol. 2014;134:127–134. doi: 10.1016/j.jaci.2014.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Koelle DM, Magaret A, Warren T, Schellenberg GD, Wald A. APOE genotype is associated with oral herpetic lesions but not genital or oral herpes simplex virus shedding. Sex Transm Infect. 2010;86(3):202–206. doi: 10.1136/sti.2009.039735. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Experiment performed in THP-1 cell line to determine the best timing of HSV-1 gene expression.
Additional file 2. Summary statistics table of HSV-1 genes and IFN-lambda mRNA expression, and cytokines concentration.
Additional file 3. Raw data of HSV-1 gene expression.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author [FLR]. The dataset supporting the conclusions of this article is included within the article and its additional file.