Abstract
Background:
The probability of returning to competition for injured baseball pitchers is similar after ulnar collateral ligament (UCL) repair as after UCL reconstruction, but the time to return is significantly quicker after UCL repair. Previous research has found no differences in pitching biomechanics between pitchers with and without a history of UCL reconstruction, but pitching biomechanics after UCL repair has not been studied.
Hypothesis:
There will be significant differences in pitching biomechanics between pitchers returning to play after UCL repair and pitchers with no injury history.
Study Design:
Controlled laboratory study.
Methods:
A total of 33 pitchers were tested shortly after UCL repair (9.8 ± 2.6 months) and compared with a matched group of 33 uninjured pitchers. Each group comprised 14 college pitchers and 19 high school pitchers. Shoulder and elbow passive ranges of motion were measured. The biomechanics of 10 fastballs was then collected using a 12-camera automated motion capture system. Ball velocity was measured using a separate 3-camera optical tracking system. Data were compared between the UCL repair group and the control group using the Student t test (significance set at P < .05).
Results:
There were no differences in passive range of motion or fastball velocity between the 2 groups. There were no differences in joint kinetics during pitching, but 3 kinematic variables showed significant differences. Specifically, the UCL repair group produced less elbow extension (flexion: 27° ± 6° vs 24° ± 4°, respectively; P = .03), less elbow extension velocity (2442 ± 367 vs 2631 ± 292 deg/s, respectively; P = .02), and less shoulder internal rotation velocity (6273 ± 1093 vs 6771 ± 914 deg/s, respectively; P = .049 ) compared with the control group.
Conclusion:
Elbow extension, elbow velocity, and shoulder velocity differed between pitchers with a recent history of UCL repair and a matched control group, but it is unclear whether this has clinical significance, as there were no differences in ball velocity and passive range of motion. Furthermore, it is unknown whether these few differences in pitching biomechanics resolve with time.
Clinical Relevance:
Elbow and shoulder kinematics during pitching might not be completely regained within the first year after UCL repair, although passive range of motion and pitch velocity show no difference in comparison to other healthy pitchers.
Keywords: elbow, Tommy John surgery, kinematics, kinetics, shoulder
In the past decade, there has been a marked rise in the number of ulnar collateral ligament (UCL) surgeries in baseball.4,20 From 2000 to 2017, the number of UCL surgeries in Major League Baseball approximately doubled, from about 20 per year to about 40 per year.4 During that same time period, the number of UCL surgeries in Minor League Baseball increased from 10 per year to 140 per year.4 There is also growing concern in amateur baseball, as the vast majority of UCL surgeries are now performed on high school and college baseball players.9,10,20 The incidence of UCL surgeries in National Collegiate Athletic Association baseball (including Divisions I, II, and III) is nearly 1 procedure per team each year (0.86/team/year).25 Mahure and colleagues20 projected that in 10 years, the annual incidence of UCL surgeries in the 15- to 24-year-old population would increase by more than 50%. Since Dr Frank Jobe first performed UCL surgery on Tommy John in 1974, the standard approach for surgical treatment of UCL injuries has remained reconstruction of the UCL with an autologous palmaris longus graft.3,9,23,26 Between 70% and 90% of baseball players successfully return to play at the same or higher level,3,4,23,26 with an average time to return to play at that level reported between 12 and 17 months.4,26
UCL repair was also considered an option through the 1990s but lost favor because of inferior outcomes compared with UCL reconstruction.1,5 Conway and colleagues5 reported that the percentage of patients who returned to the same or higher level of competition for at least 12 months was 68% for UCL reconstruction and 50% for UCL repair. Azar et al1 reported that the percentage of patients who returned to their previous or higher level was 81% for UCL reconstruction and 63% for UCL repair. However, the introduction of new technology and techniques has led some surgeons to re-evaluate UCL repair. In vitro studies have shown initial strength after UCL repair with internal brace augmentation to be similar to the strength after UCL reconstruction.8,18 Savoie et al27 published findings on a series of UCL repairs for 60 high school and college athletes, reporting 93% with good-to-excellent outcomes and return to play within 6 months of surgery. More recently, Dugas et al7 found similar outcomes in 111 high school and college athletes, reporting that 92% returned to the same or higher level of competition at an average of 7 months after UCL repair with internal brace augmentation.
Thus, for injured amateur baseball pitchers, UCL repair offers similar outcomes as UCL reconstruction, with a considerably shorter time needed to return to play. However, it is unknown whether pitching biomechanics is different after returning from UCL repair. The purpose of this study was to quantify the biomechanics of pitchers shortly after returning from UCL repair and to compare them to the biomechanics of a healthy control group.
Four hypotheses were tested based on hypotheses in a previous biomechanical study comparing professional pitchers with a history of UCL reconstruction to a control group with no history of UCL injuries.15 Two of the hypotheses tested whether pitchers in the UCL repair group exhibited mechanics previously associated with an increased UCL load and injury risk:
Hypothesis 1: Shoulder external rotation at the instant of lead-foot contact will differ between the UCL repair group and control group.
Hypothesis 2: The UCL repair and control groups will have different arm and trunk angles in the frontal plane at the instant of ball release.
The other 2 hypotheses concerned whether pitching biomechanics after UCL repair is altered or compromised:
Hypothesis 3: The UCL repair group will display a shortened stride, insufficient trunk forward tilt, and excessive shoulder horizontal adduction, all characteristics associated with “holding back” or being tentative.
Hypothesis 4: Elbow and shoulder kinematics and kinetics will differ between the UCL repair and control groups.
Methods
This study was approved by Sterling IRB. Baseball pitchers who had undergone UCL repair by the coauthors of this study (J.R.D., E.L.C., B.A.E.) were contacted and invited to participate. It was explained to each patient that he would receive a free evaluation of his pitching biomechanics and that his deidentified data would also be used in a scientific assessment of pitching after UCL repair. Furthermore, it was explained that participation in the biomechanics study was completely voluntary and that the decision would have no effect on future medical treatment at our clinic. An a priori power analysis was performed based on biomechanical results of a previous study comparing pitchers undergoing UCL reconstruction to a control group.15 It was determined that at least 16 participants in each group would be needed to find clinically meaningful differences. A total of 33 qualified patients volunteered to participate and were included in the UCL repair group of the study. All patients were male.
All patients in the UCL repair group had been diagnosed and treated in our clinic as previously described.7 Briefly, conservative treatment was the first approach in most patients. Conservative treatment varied between patients based on many factors, including injury onset, timing of the season, and their career aspirations. Typically, the nonoperative approach included rest and physical therapy; in some patients, bracing and/or platelet-rich plasma injections were also used. When nonoperative treatment failed, UCL repair and UCL reconstruction options were discussed with the patient. The decision between UCL repair and UCL reconstruction was determined intraoperatively based on the quality of the ligamentous tissue. All patients who were enrolled in the current study underwent UCL repair augmented with an internal brace system (Arthrex). With this system, a 3.5-mm anchor was placed in the location of the tear and was loaded with collagen-dipped FiberTape and 0 FiberWire (both Arthrex). A second anchor was placed at the opposing attachment site with collagen-dipped FiberTape loosely tensioned. Rehabilitation after UCL repair was an accelerated version of the program used for UCL reconstruction. Patients began an interval throwing program about 11 weeks after UCL repair.
As soon as available after returning to competition, each pitcher in the treatment group was tested in the James R. Andrews, MD, Biomechanics Laboratory at the American Sports Medicine Institute. Upon arrival, participants were provided details of the study and testing procedure, and each signed a consent form. If the athlete was younger than 19 years, he signed an assent form, and a parent signed a consent form.
Each participant was free of elbow pain at the time of biomechanical testing. The participant wore only athletic shoes, socks, and tight-fitting shorts during testing. Passive range of motion was measured bilaterally with a handheld goniometer and a digital inclinometer (Baseline Evaluation Instruments; Fabrication Enterprises) using previously established methods.24,29 The participant laid in the supine position on an examination table. Shoulder external rotation and internal rotation were measured with the arm abducted 90°. When measuring internal rotation, the scapula was manually stabilized with the investigator’s thumb against the coracoid process. Elbow extension was measured and defined as 0° with full extension, a positive value with flexion contracture, and a negative value with hyperextension.
A set of 38 reflective markers were attached to the participant on bony landmarks as previously described.11,13,17 The participant performed his normal warm-up routine for pitching in a game and then pitched 10 full-effort fastballs from a regulation portable mound to a strike-zone target located above home plate 60.5 ft (18.44 m) away. Three-dimensional motion of the reflective markers was computed at 240 Hz with a 12-camera automated motion capture system (Motion Analysis Corp). Ball velocity was measured with a separate 3-camera optical tracking system (PITCHf/x; SMT).
For each pitcher in the UCL repair group, a matched control pitcher was identified from the database of pitchers previously tested at the American Sports Medicine Institute with a similar testing protocol. All control pitchers were healthy at the time of biomechanical testing and had no injury for the previous 12 months. Control pitchers were selected to match the level (high school or college), height, and weight of the pitchers in the UCL repair group. The characteristics of the UCL repair group and control group are shown in Table 1. There were no significant differences between groups. Each group was composed of 14 college pitchers and 19 high school pitchers.
TABLE 1.
Comparison of the Characteristics Between UCL Repair and Control Groupsa
| UCL Repair Group (n = 33) | Control Group (n = 33) | P | |
|---|---|---|---|
| Time from surgery to testing, mo | 9.8 ± 2.6 | — | — |
| Age at testing, y | 18.0 ± 2.0 | 17.7 ± 1.6 | .50 |
| Height, cm | 184 ± 6 | 184 ± 7 | ≥.99 |
| Weight, kg | 85.4 ± 13.7 | 84.0 ± 9.3 | .64 |
| Ball velocity, mph | 78.4 ± 7.3 | 77.2 ± 5.4 | .45 |
aData are expressed as mean ± SD. UCL, ulnar collateral ligament.
For each pitcher in the UCL repair group and control group, kinematics and kinetics were computed with BioPitch software (American Sports Medicine Institute) as previously described.11,22 Mean values were computed for the 10 fastballs thrown by each pitcher. Data were compared between the UCL repair group and control group using the Student t test (statistical significance was set at P < .05).
Results
Passive range of motion data are shown in Table 2. There were no statistical differences between groups regarding the dominant arm. However, shoulder external rotation of the nondominant arm was greater for the control group (P = .04).
TABLE 2.
Passive Range of Motion Comparison Between UCL Repair and Control Groupsa
| UCL Repair Group (n = 33) | Control Group (n = 33) | P | |
|---|---|---|---|
| Dominant shoulder external rotation, deg | 119 ± 10 | 117 ± 9 | .28 |
| Nondominant shoulder external rotation, deg | 108 ± 11 | 116 ± 9 | .04b |
| Dominant shoulder internal rotation, deg | 48 ± 9 | 49 ± 9 | .52 |
| Nondominant shoulder internal rotation, deg | 60 ± 8 | 60 ± 9 | .68 |
| Dominant elbow extension, deg | 4 ± 8 | 1 ± 8 | .08 |
| Nondominant elbow extension,c deg | –1 ± 4 | –1 ± 8 | .78 |
aData are expressed as mean ± SD. UCL, ulnar collateral ligament.
bSignificant difference (P < .05) between the 2 groups.
cNegative elbow extension signifies hyperextension.
Results of the biomechanical comparison between the UCL repair group and control group are shown in Table 3. There were no differences between the 2 groups related to arm timing at foot contact or frontal plane at ball release. Similarly, there were no significant differences in biomechanical variables related to “holding back.” There were 3 significant differences in arm biomechanics between the groups. Specifically, shoulder internal rotation velocity (Figure 1) and elbow extension velocity (Figure 2) were significantly less for the UCL repair group than the control group (internal rotation velocity: 6273 ± 1093 vs 6771 ± 914 deg/s, respectively [P = .049]; elbow extension velocity: 2442 ± 367 vs 2631 ± 292 deg/s, respectively [P = .02]). After ball release, the control group had greater elbow extension (ie, less elbow flexion [defined in Figure 2]) than the UCL repair group (flexion: 24° ± 4° vs 27° ± 6°, respectively; P = .03).
TABLE 3.
Biomechanical Comparison Between UCL Repair and Control Groupsa
| UCL Repair Group (n = 33) | Control Group (n = 33) | P | |
|---|---|---|---|
| Hypothesis 1: arm timing | |||
| Shoulder external rotation at foot contact, deg | 60 ± 27 | 55 ± 25 | .43 |
| Hypothesis 2: frontal plane at ball release | |||
| Shoulder abduction at ball release, deg | 88 ± 8 | 88 ± 8 | .69 |
| Trunk lateral tilt at ball release, deg | 26 ± 12 | 19 ± 17 | .08 |
| Hypothesis 3: “holding back” | |||
| Stride length, % height | 81 ± 6.7 | 79 ± 5.8 | .33 |
| Maximum shoulder horizontal adduction, deg | 21 ± 5 | 21 ± 6 | .78 |
| Trunk forward tilt at ball release, deg | 33 ± 9 | 34 ± 8 | .63 |
| Hypothesis 4: arm biomechanics | |||
| Maximum elbow flexion, deg | 104 ± 11 | 107 ± 11 | .23 |
| Maximum shoulder external rotation, deg | 158 ± 8 | 161 ± 11 | .20 |
| Maximum elbow varus torque, N·m | 82.7 ± 21.0 | 82.1 ± 19.4 | .90 |
| Maximum shoulder internal rotation torque, N·m | 84.1 ± 20.9 | 83.0 ± 19.3 | .83 |
| Maximum shoulder horizontal adduction torque, N·m | 95.5 ± 29.2 | 89.7 ± 16.5 | .32 |
| Maximum elbow extension velocity, deg/s | 2442 ± 367 | 2631 ± 292 | .02b |
| Maximum shoulder internal rotation velocity, deg/s | 6273 ± 1093 | 6771 ± 914 | .049b |
| Maximum shoulder proximal force, N | 967 ± 245 | 947 ± 175 | .71 |
| Maximum elbow extension after ball release,c deg | 27 ± 6 | 24 ± 4 | .03b |
aData are expressed as mean ± SD. UCL, ulnar collateral ligament.
bSignificant difference (P < .05) between the 2 groups.
cMeasured as minimum elbow flexion.
Figure 1.
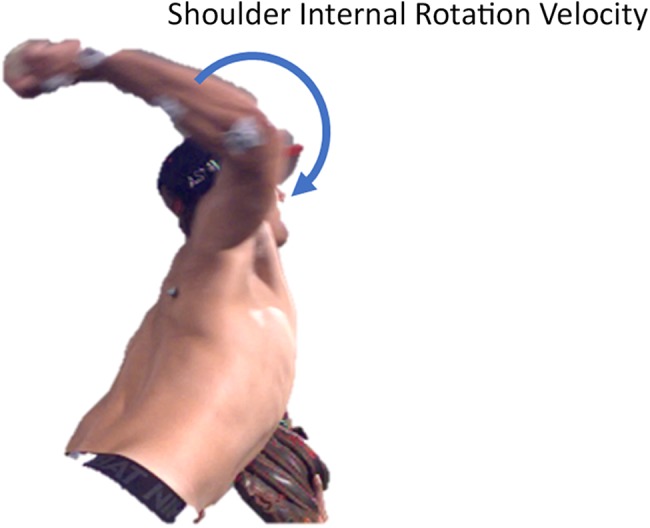
Shoulder internal rotation velocity.
Figure 2.
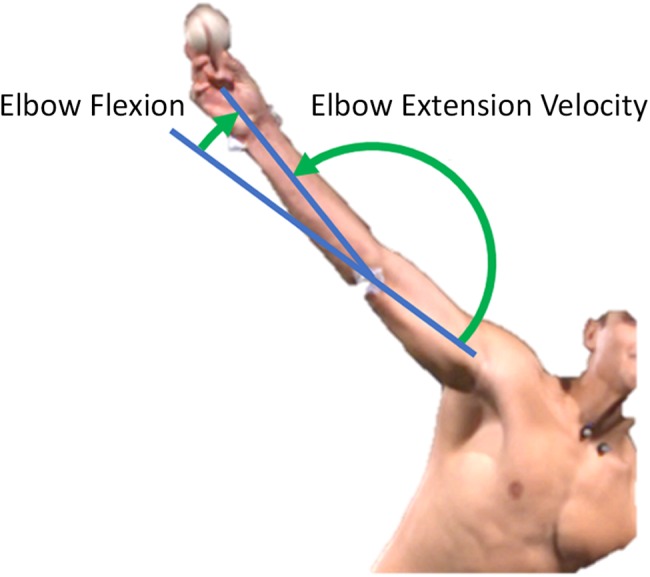
Elbow extension velocity and elbow flexion angle.
Discussion
The first 2 hypotheses were that pitchers in the UCL repair group would exhibit mechanics that has been previously associated with increased elbow torque and risk of injuries. Ideally, biomechanics of the pitchers in the UCL repair group should have been quantified before their UCL injury to prove causality, but this was not possible. The premise of looking for flaws in mechanics after returning from an injury is based on the assumption that these pitchers have the same mechanics as before their injury. It is unknown how many pitchers change their mechanics after an injury, either intentionally or not. Previous research has shown that even when flaws are identified with a biomechanical evaluation, only about 50% of baseball pitchers correct the flaws.14 The first hypothesis was based on the popular concept in baseball that pitchers who are “late” have greater stress and injury risk at the elbow.2,15,28 Biomechanical research has shown that a “late” arm, quantified as low shoulder external rotation at the instant of lead-foot contact, is associated with increased elbow torque.12,16 The second hypothesis was that at the instant of ball release, shoulder abduction and trunk lateral tilt would differ between the 2 groups. Previous research has shown that these 2 angles as well as “arm slot” (essentially, the position of the upper extremity in the space resulting from these 2 angles) affect elbow and shoulder kinetics.11,21 These 2 hypotheses were rejected by the current study. This is consistent with a previous biomechanical study that also failed to show these mechanical flaws in pitchers with a history of UCL injuries.15
The third hypothesis was that the UCL repair group would pitch with a shortened stride, insufficient trunk forward tilt, and excessive shoulder horizontal adduction. In our experience, these are characteristics that we often see in our biomechanics laboratory when analyzing pitchers who are having difficulties returning from an injury. Previous research did not show pitchers with these mechanical flaws after returning from UCL reconstruction,6 but pitchers who returned after superior labrum anterior-posterior (SLAP) repair of the shoulder demonstrated insufficient trunk forward tilt.19 Data from the current study did not support the hypothesis that pitchers are “holding back” after UCL repair.
There were no differences in passive range of motion of the throwing shoulder between the UCL repair group and control group. On average, the passive range of motion of the throwing elbow was 4° short of full extension for the UCL repair group and 1° for the control group, but this trend was not statistically significant (P = .08). However, during pitching, the UCL repair group had significantly less elbow extension compared with the control group. Less elbow motion during pitching for the UCL repair group (∼77°, from 104° to 27°) than the control group (∼83°, from 107° to 24°) may explain why the UCL repair group generated less elbow extension velocity. Although the observed deficit in shoulder external rotation during pitching for the UCL repair group was not significant (P = .20), this group produced less shoulder internal rotation velocity. Thus, decreased elbow extension, elbow extension velocity, and shoulder internal rotation velocity for the UCL repair group supported the hypothesis that arm biomechanics differed between the 2 groups. Although the study of pitchers undergoing SLAP repair also showed significant differences in shoulder kinematics,19 the study of pitchers undergoing UCL reconstruction did not report any difference in arm biomechanics and passive range of motion.15
There are several possible explanations why there were differences and trends in the current study that were not shown in the previous study15 of pitchers undergoing UCL reconstruction. Pitchers in the current study were tested just 9.8 ± 2.6 months after surgery, whereas the time from surgery to biomechanical testing averaged 30.5 months for the pitchers undergoing UCL reconstruction. Another factor might have been differences in the skill level, as participants were amateur high school and college pitchers in the current study and professional pitchers in the UCL reconstruction study. The biomechanical findings may also be due to random differences between groups, as both the current study and the previous UCL reconstruction study compared pitchers after returning from elbow surgery to a matched control group. An ideal study design would have been to capture data for the surgery group before the injury and then compare them to their own data after returning to play using repeated-measures analysis, but preinjury biomechanical data were not available.
Of course, another possible explanation may be that the type of UCL surgery (repair vs reconstruction) does affect pitching mechanics after returning to play. Our belief is that the timing of testing was the biggest factor; future research testing pitchers with more time between UCL repair and biomechanical analysis (perhaps ≥24 months) could prove whether observed changes in arm kinematics resolve with time. Differences in arm biomechanics were not associated with differences in ball velocity. It is not clear how the UCL repair group achieved equal ball velocity with less joint movement velocity.
As noted above, a limitation of the current study was that preinjury biomechanical data for the UCL repair group were not available. Such data would have allowed for direct analysis of changes in individual pitchers associated with their injury and treatment. Another limitation of the study was the short time period from surgery to the biomechanical evaluation. Also, with data for only 10 pitches recorded, we were unable to look at any effect of fatigue on mechanics in these patients. Future research will investigate pitching biomechanics ≥2 years after UCL repair. Future research is also needed to assess performance after returning from UCL repair, such as level of play, pitching statistics, ball velocity, ball control, length of career, and future injuries.
Conclusion
Amateur pitchers demonstrated reduced elbow extension, elbow extension velocity, and shoulder internal rotation velocity at a mean of 9.8 ± 2.6 months after returning from UCL repair in comparison to a control group with no injury history. However, it is unclear whether these kinematic differences have clinical significance, as there were no differences in ball velocity and passive range of motion. Furthermore, it is unknown whether these few differences in pitching biomechanics resolve with time.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: E.L.C. has received consulting fees and royalties from Arthrex, nonconsulting fees from Smith & Nephew, educational support from Prime Surgical, and hospitality payments from Encore Medical. B.A.E. has received nonconsulting fees from Smith & Nephew and royalties from Arthrex. J.R.D. has received consulting fees and royalties from Arthrex and hospitality payments from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Sterling IRB.
References
- 1. Azar FM, Andrews JR, Wilk KE, Groh D. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med. 2000;28(1):16–23. [DOI] [PubMed] [Google Scholar]
- 2. Boddy K. Strasburg, the inverted W, and pitching mechanics. 2010. Available at: http://www.drivelinebaseball.com/2010/09/04/strasburg-the-inverted-w-and-pitching-mechanics. Accessed December 12, 2018.
- 3. Cain EL, Andrews JR, Dugas JR, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38(12):2426–2434. [DOI] [PubMed] [Google Scholar]
- 4. Camp CL, Conte S, D’Angelo J, Fealy SA. Epidemiology of ulnar collateral ligament reconstruction in Major and Minor League Baseball pitchers: comprehensive report of 1429 cases. J Shoulder Elbow Surg. 2018;27(5):871–878. [DOI] [PubMed] [Google Scholar]
- 5. Conway JE, Jobe FW, Glousman RE, Pink MM. Medial instability of the elbow in throwing athletes: treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am. 1992;74(1):67–83. [PubMed] [Google Scholar]
- 6. Dahm DL, Curriero FC, Camp CL, et al. Epidemiology and impact of knee injuries in Major and Minor League Baseball players. Am J Orthop (Belle Mead NJ). 2016;45(3):E54–E62. [PubMed] [Google Scholar]
- 7. Dugas JR, Looze CA, Capogna B, et al. Ulnar collateral ligament repair with collagen-dipped FiberTape augmentation in overhead throwing athletes. Am J Sports Med. 2019;47(5):1096–1102. [DOI] [PubMed] [Google Scholar]
- 8. Dugas JR, Walters BL, Beason DP, Fleisig GS, Chronister JE. Biomechanical comparison of ulnar collateral ligament repair with internal bracing versus modified Jobe reconstruction. Am J Sports Med. 2016;44(3):735–741. [DOI] [PubMed] [Google Scholar]
- 9. Erickson BJ, Chalmers PN, Bush-Joseph CA, Verma NN, Romeo AA. Ulnar collateral ligament reconstruction of the elbow: a systematic review of the literature. Orthop J Sports Med. 2015;3(12):2325967115618914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Erickson BJ, Nwachukwu BU, Rosas S, et al. Trends in medial ulnar collateral ligament reconstruction in the United States: a retrospective review of a large private-payer database from 2007 to 2011. Am J Sports Med. 2015;43(7):1770–1774. [DOI] [PubMed] [Google Scholar]
- 11. Escamilla RF, Slowik JS, Diffendaffer AZ, Fleisig GS. Differences among overhand, three-quarter, and sidearm pitching biomechanics in professional baseball players. J Appl Biomech. 2018;34(5):377–385. [DOI] [PubMed] [Google Scholar]
- 12. Fleisig GS. The Biomechanics of Baseball Pitching [dissertation]. Birmingham: University of Alabama; 1994. [Google Scholar]
- 13. Fleisig GS, Diffendaffer AZ, Aune KT, Ivey B, Laughlin WA. Biomechanical analysis of weighted-ball exercises for baseball pitchers. Sports Health. 2017;9(3):210–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fleisig GS, Diffendaffer AZ, Ivey B, Aune KT. Do baseball pitchers improve mechanics after biomechanical evaluations? Sports Biomech. 2018;17(3):314–321. [DOI] [PubMed] [Google Scholar]
- 15. Fleisig GS, Leddon CE, Laughlin WA, et al. Biomechanical performance of baseball pitchers with a history of ulnar collateral ligament reconstruction. Am J Sports Med. 2015;43(5):1045–1050. [DOI] [PubMed] [Google Scholar]
- 16. Fortenbaugh D, Fleisig GS, Andrews JR. Baseball pitching biomechanics in relation to injury risk and performance. Sports Health. 2009;1(4):314–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Glanzer JA, Diffendaffer AZ, Drogosz M, Slowik JS, Lo NJ, Fleisig GS. Comparison of variability in kinematics between baseball pitchers with and without consistent pitch location [published online August 26, 2019]. Sports Biomech. doi:10.1080/14763141.2019.1642378. [Google Scholar]
- 18. Jones CM, Beason DP, Dugas JR. Ulnar collateral ligament reconstruction versus repair with internal bracing: comparison of cyclic fatigue mechanics. Orthop J Sports Med. 2018;6(2):2325967118755991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Laughlin WA, Fleisig GS, Scillia AJ, Aune KT, Cain EL, Dugas JR. Deficiencies in pitching biomechanics in baseball players with a history of superior labrum anterior-posterior repair. Am J Sports Med. 2014;42(12):2837–2841. [DOI] [PubMed] [Google Scholar]
- 20. Mahure SA, Mollon B, Shamah SD, Kwon YW, Rokito AS. Disproportionate trends in ulnar collateral ligament reconstruction: projections through 2025 and a literature review. J Shoulder Elbow Surg. 2016;25(6):1005–1012. [DOI] [PubMed] [Google Scholar]
- 21. Matsuo T, Fleisig GS, Zheng N, Andrews JR. Influence of shoulder abduction and lateral trunk tilt on peak elbow varus torque for college baseball pitchers during simulated pitching. J Appl Biomech. 2006;22:93–102. [DOI] [PubMed] [Google Scholar]
- 22. Oi T, Slowik JS, Diffendaffer AZ, et al. Biomechanical differences between Japanese and American professional baseball pitchers. Orthop J Sports Med. 2019;7(2):2325967119825625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Osbahr DC, Cain EL, Raines BT, Fortenbaugh D, Dugas JR, Andrews JR. Long-term outcomes after ulnar collateral ligament reconstruction in competitive baseball players: minimum 10-year follow-up. Am J Sports Med. 2014;42(6):1333–1342. [DOI] [PubMed] [Google Scholar]
- 24. Reinold MM, Macrina LC, Fleisig GS, Aune K, Andrews JR. Effect of a 6-week weighted baseball throwing program on pitch velocity, pitching arm biomechanics, passive range of motion, and injury rates. Sports Health. 2018;10(4):327–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rothermich MA, Conte SA, Aune KT, Fleisig GS, Cain EL, Dugas JR. Incidence of elbow ulnar collateral ligament surgery in collegiate baseball players. Orthop J Sports Med. 2018;6(4):2325967118764657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Saper M, Pearce S, Shung J, Zondervan R, Ostrander R, Andrews JR. Outcomes and return to sport after revision anterior cruciate ligament reconstruction in adolescent athletes. Orthop J Sports Med. 2018;6(4):2325967118764884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Savoie FH, Trenhaile SW, Roberts J, Field LD, Ramsey JR. Primary repair of ulnar collateral ligament injuries of the elbow in young athletes: a case series of injuries to the proximal and distal ends of the ligament. Am J Sports Med. 2008;36(6):1066–1072. [DOI] [PubMed] [Google Scholar]
- 28. Verducci T. Is Strasburg headed for trouble? One pitching expert thinks so. 2010. Available at: http://www.si.com/more-sports/2010/07/30/strasburg-trades. Accessed December 12, 2018.
- 29. Wilk KE, Reinold MM, Macrina LC, et al. Glenohumeral internal rotation measurements differ depending on stabilization techniques. Sports Health. 2009;1(2):131–136. [DOI] [PMC free article] [PubMed] [Google Scholar]


