Abstract
We report standards (95th, 50th, and 5th centiles) in Prader-Willi syndrome for weight, height, sitting height, head circumference, head length, head breadth, hand length, middle finger length, palm length, hand breadth, foot length, foot breadth, triceps skinfold, and subscapular skinfold. For comparison with Prader-Willi syndrome standardized curves, normal control data from the literature were plotted similarly and standard curves were produced. We encourage the use of these standards with the examination of patients who have Prader-Willi syndrome and in the comparison of the patient who has Prader-Willi syndrome with other similarly affected individuals. The standards may also be useful for assisting in the diagnosis of Prader-Willi syndrome, particularly in younger individuals.
The Prader-Willi syndrome (PWS), generally sporadic in occurrence, is characterized by infantile hypotonia, early childhood obesity, mental deficiency, hypopigmentation, small hands and feet, short stature, hypogonadism, and a characteristic facial appearance.1–6 The incidence of PWS is estimated at 1 in 16 000 live births7 and is the most common dysmorphic form of obesity.6 The cause of this syndrome is not clear, although a chromosome deletion has been found with high-resolution chromosome studies in 60% of individuals who have PWS.6–10 The chromosome deletion is paternal in origin, although parental chromosomes are normal.5,6,11 Nicholls et al12 reported on two patients who had PWS without a recognizable chromosome 15q deletion, but with maternal disomy of chromosome 15 identified with the use of informative DNA markers from the proximal 15q chromosome region. Several additional patients who have PWS without a chromosome deletion have been reported on with either maternal disomy or heterodisomy of chromosome 15 which strongly supports a role for genetic imprinting in the expression of PWS phenotype.13
Recently, Butler et al14 reported the effects of age, sex, and chromosome status on individuals who have PWS with emphasis on hand and foot measurements. However, only a few studies have been reported on the linear growth patterns in individuals who have PWS.4,14–18 There is a paucity of anthropometric standards in PWS.
In this paper, we report standardized curves for 71 male and female patients who have PWS on 14 physical parameters, including weight, height, sitting height, three head dimensions, four hand and two foot measurements, and two skinfold measurements. These standardized curves should be useful in the clinical setting in the examination of patients who have PWS and their comparison with other similarly affected individuals.
MATERIALS AND METHODS
PWS was diagnosed in the 71 white subjects (42 males and 29 females) between the ages of 0 to 24 years included in this study on the basis of infantile hypotonia, hypogonadism, delayed psychomotor development and/or mental deficiency, early childhood obesity, small hands and feet, and short stature. Approximately one half of the patients were on a calorie-restricted diet at the time of the examination. Longitudinal data were collected on several individuals for a period of 6 years.
The anthropometric measurements were made by the authors according to standard techniques as presented by Weiner and Lourie.19 The measurements consisted of the following: weight, length, sitting height, head circumference, head breadth, head length, total hand length, middle finger length, palm length, hand breadth, total foot length, foot breadth, triceps skinfold thickness, and subscapular skinfold thickness. Up to 2 years of age, length was measured in a supine position using a horizontal calibrated board; thereafter height measurements were taken. Head circumference was measured to the nearest millimeter with a steel tape. Weight and height were taken with a balanced beam scale and anthropometer, respectively. Hand and foot measurements were obtained with sliding calipers, and head breadth and length with spreading calipers. Skinfold measurements were obtained to the nearest half-millimeter with a Lange skinfold caliper.
High-resolution chromosome analysis was performed on the 71 patients who had PWS. Thirty-seven (52%) individuals who had PWS were identified with an apparent deletion of the proximal long arm of chromosome 15. Normal chromosome findings were observed in 26 individuals, and the chromosome status was unknown in the remaining 8 individuals.
No significant differences were reported in anthropometric data between individuals with the 15q deletion and those with normal chromosomes,5,17,20–22 but significant anthropometric differences were reported in male and female patients who had PWS (eg, palm length was smaller in female patients).14 Therefore, separate standardized curves were developed for both male and female patients, but deletion and nondeletion individuals who had PWS were combined.
Curves for PWS were developed according to standards of reliability and precision previously described.23,24 The first criterion is a sample size of five or more per age interval. To meet this criterion for our study, male and female patients who had PWS were grouped at either 3- or 4-year age intervals. The second criterion states that the coefficient of variation, ie, the standard deviation expressed as a percentage of the mean, should be less than 25%. The means and standard deviations were calculated for each age interval (eg, 0 to 4 years, 4 to 8 years, 8 to 12 years, 12 to 16 years, 16 to 20 years, and 20 to 24 years) and standardized curves from 2 to 22 years of age were produced after meeting the above two criteria by plotting the mean (or 50th centile), 5th, and 95th centiles for each age interval for the male and female patients who have PWS. For comparison with PWS standardized curves, normal control anthropometric data were collected similarly,25,26 plotted, and standards (95th, 50th, and 5th centiles) produced.
RESULTS
Figures 1 through 14 show standardized curves of anthropometric variables for male and female patients who have PWS and for healthy individuals. For weight in both male and female patients who have PWS, the 50th centile approximates the normal 95th centile (Fig 1). For height in female patients who have PWS, the 50th centile closely approximates the normal 5th centile, and by 12 years of age the 50th centile falls below the normal 5th centile and continues to drop off relative to the normal curve. Similarly, in male patients who have PWS, the 50th centile falls below the normal 5th centile by 14 years of age but with a steeper dropoff than in female patients (Fig 2). For sitting height in female patients who have PWS, the 50th centile approximates but remains below the normal 5th centile for all ages, while in male patients who have PWS, the 50th centile approximates the normal 5th centile, but falls below the 5th centile by 15 years of age (Fig 3).
Fig 1.

Standardized curves for weight of Prader-Willi syndrome (PWS) male and female patients (solid line) and healthy individuals (broken line).
Fig 2.
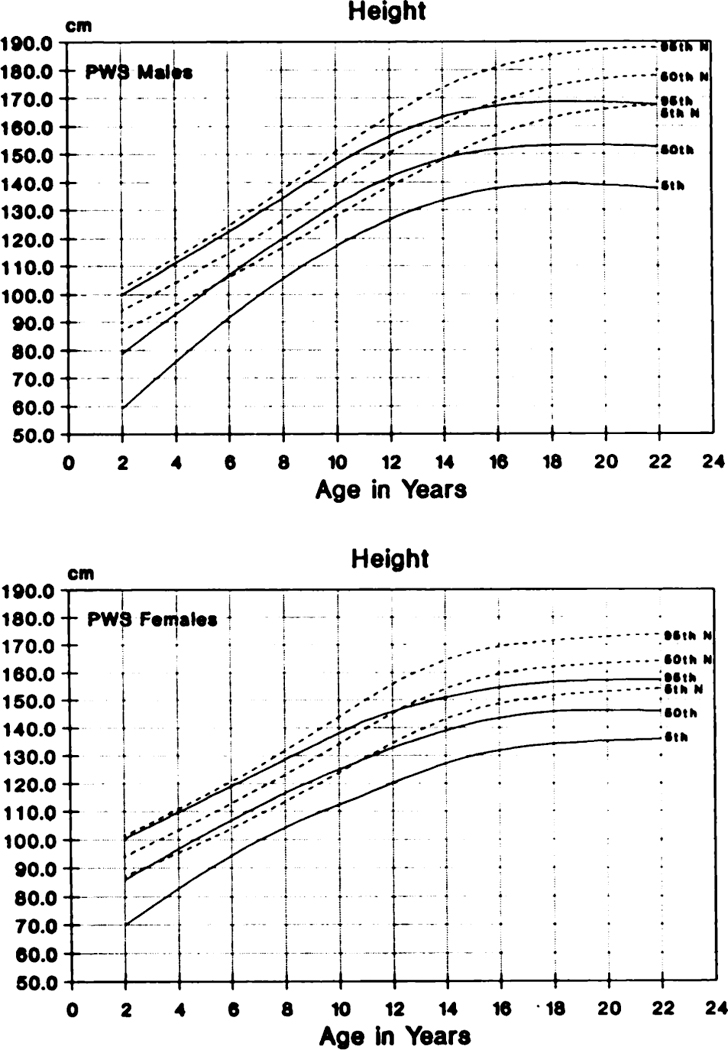
Standardized curves for height of Prader-Willi syndrome (PWS) male and female patients (solid line) and healthy individuals (broken line).
Fig 3.

Standardized curves for sitting height of Prader-Willi syndrome (PWS) male and female patients (solid line) and healthy individuals (broken line).
Several differences were observed in the comparison of standardized curves for head dimensions in individuals who have PWS and healthy individuals. For example, for head circumference in both male and female patients who have PWS and in healthy patients, the 50th centile is generally between the normal 50th and 5th centiles, approaching the normal 5th centile by 18 years of age (Fig 4). For head length in both male and female patients who have PWS, the 50th centile is generally between the normal 50th and 5th centiles as with head circumference (Fig 5). For head breadth in female patients who have PWS, the 50th centile is consistently below the normal 5th centile for all ages. For male patients who have PWS, the 50th centile approximates the normal 5th centile, but falls below the normal 5th centile by 14 years of age and continues to drop off at older ages (Fig 6).
Fig 4.

Standardized curves for head circumference of Prader-Willi syndrome (PWS) male and female patients (solid line) and healthy individuals (broken line).
Fig 5.

Standardized curves for head length of Prader-Willi syndrome (PWS) male and female patients (solid line) and healthy individuals (broken line).
Fig 6.

Standardized curves for head breadth of Prader-Willi syndrome (PWS) male and female patients (solid line) and healthy individuals (broken line).
For hand and foot measurements, the following differences were observed when comparing male and female patients who have PWS with control standards. For hand length in female patients who have PWS, the 50th centile approximates the normal 5th centile for all ages. In male patients who have PWS, the 50th centile is between the normal 50th and 5th centiles until 15 years of age when it begins to drop off relative to the normal 5th centile as observed in height and sitting height (Fig 7). For middle finger length and palm length curves in general are similar to those plotted for hand length (Figs 8 and 9). The results for hand breadth are similar to those in the linear hand dimensions (Fig 10). However, in male patients who have PWS, there appears to be a sharper drop-off of the 50th centile after 15 years of age as observed for middle finger length (compare Figs 8 and 10). For foot length in female patients who have PWS, the 50th centile is consistently below the normal 5th centile. In male patients who have PWS, the 50th centile approximates the normal 5th centile until 12 years of age when the 50th centile falls below the normal 5th centile and appears to drop off relative to the normal 5th centile with increasing age (Fig 11). The results for foot breadth are similar to those observed for foot length (Fig 12). Interestingly, hand and foot length measurements when adjusted for height age for the individuals who have PWS were also short (ie, consistently below the 50th centile) for height age with the adjusted foot length being shorter than adjusted hand length in both male and female patients.
Fig 7.

Standardized curves for hand length of Prader-Willi syndrome (PWS) male and female patients (solid line) and healthy individuals (broken line).
Fig 8.

Standardized curves for middle finger length of Prader-Willi syndrome (PWS) male and female patients (solid line) and healthy individuals (broken line).
Fig 9.

Standardized curves for palm length of Prader-Willi syndrome (PWS) male and female patients (solid line) and healthy individuals (broken line).
Fig 10.

Standardized curves for hand breath of Prader-Willi syndrome (PWS) male and female patients (solid line) and healthy individuals (broken line).
Fig 11.

Standardized curves for foot length of Prader-Willi syndrome (PWS) male and female patients (solid line) and healthy individuals (broken line).
Fig 12.

Standardized curves for foot breadth of Prader-Willi syndrome (PWS) male and female patients (solid line) and healthy individuals (broken line).
For the remaining two anthropometric variables, triceps and subscapular skinfolds, several differences were observed between male and female patients who had PWS. For example, with triceps skinfold in female patients who have PWS, the 50th centile approximates the normal 95th centile; whereas in male patients who have PWS, the 50th centile is consistently above the normal 95th centile for all ages (Fig 13). Results for subscapular skinfold are similar to those with triceps skinfold (Fig 14).
Fig 13.

Standardized curves for triceps skinfold of Prader-Willi syndrome (PWS) male and female patients (solid line) and healthy individuals (broken line).
Fig 14.

Standardized curves for subscapular skinfold of Prader-Willi syndrome (PWS) male and female patients (solid line) and healthy individuals (broken line).
DISCUSSION
Standardized curves were produced for 14 anthropometric variables of both male and female patients who had PWS as well as healthy control individuals from the literature. So far, no significant differences have been reported for anthropometric data between individuals who have PWS with the 15q deletion and those with normal chromosomes.5,17,21,22 However, significant anthropometric differences recently have been reported in male and female patients who have PWS.14 These data are supported by the current analysis of the standard curves based on this clinical population of individuals with PWS. Particularly, smaller hand and foot measurements (eg, palm length) were observed in female patients who have PWS than in male patients who have PWS.
There are several additional abnormal physical parameters in individuals who have PWS, particularly weight, height, skinfold measurements as well as hand and foot measurements, even though approximately one half of the patients who have PWS were on a calorie-restricted diet. These abnormal parameters can be appreciated readily after comparing these PWS standards with the standardized curves developed from measurements on sample populations of unaffected individuals.
We previously have reported negative correlations of Z scores for linear body dimensions with age in individuals who have PWS14,22 and suggested that these data reflect a deceleration in linear growth in PWS relative to normal individuals. The drop-off of the 50th centile for such linear dimensions as height, sitting height, and hand length observed in individuals who have PWS relative to the 50th centile in healthy individuals further demonstrates this slowing down in growth. The fall-off in linear growth generally occurs after 12 years of age in female patients and after 14 years of age in male patients; it probably reflects the lack of a pubertal growth spurt in individuals who have PWS. The fall-off in values is particularly apparent in male patients. Interestingly, in PWS male patients who have PWS, this phenomenon is also observed in breadth dimensions, including breadths of the head, hand, and foot.
Anthropometric standards have been developed for several syndromes27,28 and have been used successfully in the medical management of patients. The use of standards have become routine in most clinical genetics centers for monitoring growth and development of patients with certain syndromes (eg, Down syndrome). Medical care of patients who have PWS is complex, particularly monitoring abnormal growth parameters (eg, weight, height). There is recent evidence for growth hormone deficiency in patients who have PWS and favorable responses reported in several patients who have PWS undergoing growth hormone therapy.4,6,29 The use of our anthropometric standards may be helpful in those patients who have PWS being treated with growth hormone. Therefore, the use of PWS standards should assist the clinician in monitoring the various abnormal physical parameters in patients affected with this syndrome. The standards reported herein may also be useful for assisting in the diagnosis of PWS, particularly in the younger individuals. We would encourage the use of these standards in the examination of patients who have PWS and in the comparison of the patient who has PWS with other similarly affected individuals.
ACKNOWLEDGMENTS
This research was supported in part by a grant from the March of Dimes Birth Defects Foundation.
We thank Pamela Grimm for expert preparation of the manuscript and Tim Mangrum and Judy Haynes for their technical assistance.
REFERENCES
- 1.Prader A, Labhart A, Willi H. Ein Syndrome von Adipositas, Kleinwuchs, Kryptochismus and Oligophrenie nach myatonieartigem Zustand in Neugeborenenalter. Schweiz Med Wochenschr. 1956;86:1260–1261 [Google Scholar]
- 2.Hall BD, Smith DW. Prader-Willi syndrome. J Pediatr. 1972;81:286–293 [DOI] [PubMed] [Google Scholar]
- 3.Cassidy SB. Prader-Willi syndrome. Curr Probl Pediatr. 1984;14:1–55 [DOI] [PubMed] [Google Scholar]
- 4.Bray GA, Dahms WT, Swerdloff RS, Fiser RH, Atkinson RL, Carrel RE. The Prader-Willi syndrome. Medicine. 1983;62:59–80 [PubMed] [Google Scholar]
- 5.Butler MG, Meaney FJ, Palmer CG. Clinical and cytogenetic survey of 39 individuals with Prader-Labhart-Willi syndrome. Am J Med Genet. 1986;23:793–809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Butler MG. Prader-Willi syndrome: current understanding of cause and diagnosis. Am J Med Genet. 1990;35:319–332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burd L, Vesely B, Martsolf J, Korbeshian J. Prevalence study of Prader-Willi syndrome in North Dakota. Am J Med Genet. 1990;37:97–99 [DOI] [PubMed] [Google Scholar]
- 8.Ledbetter DH, Mascarello JT, Riccardi VM, Harper VD, Airhart SD, Strobel RJ. Chromosome 15 abnormalities and the Prader-Willi syndrome. Am J Hum Genet. 1982;34:278–285 [PMC free article] [PubMed] [Google Scholar]
- 9.Cassidy SB, Thuline HC, Holm VA. Deletion of chromosome 15 (ql 1–13) in a Prader-Willi syndrome clinic population. Am J Med Genet. 1984;17:485–495 [DOI] [PubMed] [Google Scholar]
- 10.Mattei MG, Souiah N, Mattei JF. Chromosome 15 anomalies and the Prader-Willi syndrome: cytogenetic analysis. Hum Genet. 1984;66:313–334 [DOI] [PubMed] [Google Scholar]
- 11.Butler MG, Palmer CG. Parental origin of chromosome 15 deletion in Prader-Willi syndrome. Lancet. 1983;1:1285–1286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nicholls R, Knoll JHM, Butler MG, Karam S, Lalande M. Genetic imprinting suggested by maternal heterodisomy in nondeletion Prader-Willi syndrome. Nature. 1989;342:281–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mascari MJ, Ladda RL, Butler MG, Gottlieb W, Nicholls RD. Molecular analysis in non-deletion Prader-Willi syndrome. Am J Hum Genet. 1990;47:A228 [Google Scholar]
- 14.Butler MG, Haynes JL, Meaney FJ. Anthropometric study with emphasis on hand and foot measurements in the Prader-Willi syndrome: sex, age and chromosome effects. Clin Genet. 1991;39:39–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nugent JK, Holm VA. Physical growth in Prader-Willi syndrome In: Holm VA, Sulzbacher S, Pipes PL, eds. The Prader-Willi Sydrome. Baltimore: University Park Press; 1981:269–280 [Google Scholar]
- 16.Holm VA, Nugent JK. Growth in the Prader-Willi syndrome. Birth Defects Orig Artie Ser. 1982;18:93–100 [PubMed] [Google Scholar]
- 17.Butler MG, Meaney FJ. An anthropometric study of 38 individuals with Prader-Labhart-Willi syndrome. Am J Med Genet. 1987;26:445–455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Butler MG, Butler RI, Meaney FJ. The use of skinfold measurements to judge obesity during the early phase of Prader-Labhart-Willi syndrome. Int J Obes. 1988;12:417–422 [PMC free article] [PubMed] [Google Scholar]
- 19.Weiner JS, Lourie JA. Human Biology: A Guide to Field Methods International Biological Programme Handbook No. 9. Oxford: Blackwell Scientific Publications; 1969 [Google Scholar]
- 20.Meaney FJ, Butler MG. Craniofacial variation and growth in the Prader-Labhart-Willi syndrome. Am J Phys Anthro-pol. 1987;74:459–464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meaney FJ, Butler MG. Characterization of obesity in Prader-Labhart-Willi syndrome: fatness patterning. Med Anthropol Q. 1988;3:294–305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meaney FJ, Butler MG. The developing role of anthropologists in medical genetics: anthropometric measurement of the Prader-Labhart-Willi syndrome as an illustration. Med Anthropol. 1989;10:247–253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Center for Health Statistics. Selected body measurements of children 6–11 years, United States In: Vital and Health Statistics. Washington, DC: US Public Health Service; 1973. US Dept of Health, Education, and Welfare publication (HSM) 73–1605, Series 11-No. 123 [PubMed] [Google Scholar]
- 24.Brandt JM, Allen GA, Haynes JL, Butler MG. Normative standards and comparison of anthropometric data of white and black newborn infants. Dysmorph Clin Genet. 1990;4:121–137 [PMC free article] [PubMed] [Google Scholar]
- 25.Snyder RG, Schneider LW, Owings CL, Reynolds HM, Gollomb DH, Schork MA, eds. Anthropometry of Infants, Children and Youths to Age 18 for Product Safety Design SP-450. Warrendale, PA: Society of Automobile Engineers, Inc; 1977 [Google Scholar]
- 26.Tanner JM, Whitehouse RH. Revised standards for triceps and subscapular skinfolds in British children. Arch Dis Child. 1975;50:142–145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Meaney FJ, Farrer LA. Clinical anthropometry and medical genetics: a compilation of body measurements in genetic and congenital disorders. Am J Med Genet. 1986;25:343–359 [DOI] [PubMed] [Google Scholar]
- 28.Hall JG, Froster-Iskenius UG, Allanson JE, eds. Handbook of normal physical measurements. Oxford: Oxford University Press; 1989 [Google Scholar]
- 29.Lee PDK, Wilson DM, Rountree L, Hintz RL, Rosenfeld RG. Linear growth response to exogenous growth hormone in Prader-Willi syndrome. Am J Med Genet. 1987;28:865–871 [DOI] [PubMed] [Google Scholar]


