Abstract
Objectives: To assess contacts with general practitioners (GPs), both regular GPs and out-of-hours GP services (OOH) during the year before an emergency hospital admission.
Design: Longitudinal design with register-based information on somatic health care contacts and use of municipality health care services.
Setting: Four municipalities in central Norway, 2012–2013.
Subjects: Inhabitants aged 50 and older admitted to hospital for acute myocardial infarction, hip fracture, stroke, heart failure, or pneumonia.
Main outcome measures: GP contact during the year and month before an emergency hospital admission.
Results: Among 66,952 identified participants, 720 were admitted to hospital for acute myocardial infarction, 645 for hip fracture, 740 for stroke, 399 for heart failure, and 853 for pneumonia in the two-year study period. The majority of these acutely admitted patients had contact with general practitioners each month before the emergency hospital admission, especially contacts with a regular GP. A general increase in GP contact was observed towards the time of hospital admission, but development differed between the patient groups. Patients admitted with heart failure had the steepest increase of monthly GP contact. A sizable percentage did not contact the regular GP or OOH services the last month before admission, in particular men aged 50–64 admitted with myocardial infarction or stroke.
Conclusion: The majority of patients acutely admitted to hospital for different common severe emergency diagnoses have been in contact with GPs during the month and year before the admission. This points towards general practitioners having an important role in these patients’ health care.
KEY MESSAGES
There is scarce knowledge about primary health care contact before an emergency hospital admission.
The percentage of patients with contacts differed between patient groups, and increased towards hospital admission for most diagnoses, particularly heart failure.
More than 50% having monthly general practitioner contact before admission underscores the general practitioners’ role in these patients’ health care.
Our results underscore the need to consider medical diagnosis when talking about the role of general practitioners in preventing emergency hospital admissions.
Keywords: General practice, primary care physicians, health care, health services research, hospitalization, aged, Norway
Introduction
General practitioners (GPs) play an important role in the management of patients with chronic conditions [1]. GPs are coordinators in the line of treatment, responsible for adequate preventive health care, referral of patients to secondary health care when needed, follow-up and monitoring after secondary health care treatment [2]. Adequate access to GP services and continuity of care from GPs have been suggested to prevent deterioration of several medical conditions [1,3–5] and decrease visits to emergency departments in both children [6,7] and the general population [8–10] across different healthcare systems [11].
In Norway, all inhabitants are provided with a regular GP within a list-based system introduced in 2001, and by the start of 2018 almost the whole population participated in this system [12]. Even though Northern European countries organise their primary health care sectors differently, they all emphasise the importance of general practice and primary care when discussing the public health challenges of an ageing population [13]. There is scarce knowledge on the use of primary health care before an emergency hospital admission. This study aims to explore the extent and timing of contacts with GPs (both regular and out-of-hours (OOH)) among adults 50 years and older during the year before emergency hospital admission for five common acute diagnoses (acute myocardial infarction; hip fracture; stroke; heart failure; and pneumonia).
We expected a gradual increase in contacts as patients got closer to the time of hospital admission, but that the extent and timing would differ according to diagnosis and type of GP contact (regular GP vs. OOH services). We wanted to explore whether an increase in GP contact could be observed over a longer period (e.g. several months), indicating a gradual health deterioration culminating in the acute or sub-acute situation causing the emergency hospital admission. This could point to both a preventive potential but also to the role of close monitoring of vulnerable patients in primary care. For acute myocardial infarction and stroke, we also wanted to explore whether these groups had a more stable level of GP contacts over time before an acute incident leading to their admission, or if there was any indication of increased contact in the weeks or months before admission – indicating a potential for prevention or early detection in primary care.
Methods
This study used a longitudinal design with data from Norwegian national- and municipal registers. We applied register-based information on all somatic health care contacts for the inhabitants in four municipalities (one municipality containing a city (Trondheim) and three neighbouring, more rural municipalities) in central Norway in a two-year period from 2012 to 2013, covering a population of 214,722 persons. The data included routine patient administrative data on inpatient and outpatient somatic health care use from St. Olav’s University Hospital, and information on contacts with regular GPs and OOH services from the Norwegian Health Economics Administration database (Helfo). We linked the registers using a project ID based on the national ID number unique to each Norwegian citizen. We also included information regarding municipality health care services from the four municipalities. All data was de-identified before the analysis.
Inclusion criteria for the analysis were age 50 years or older by the end of 2012, having at least one emergency hospital admission in 2012 or 2013 for one of five diagnoses specified below, and having at least one month of observation time before admission (excluding emergency admissions before 1 February 2012).
The age of each participant in 2012 was categorised into age groups (50–64 years, 65–79 years, and 80+). We also included sex and municipality of residence (dichotomised into living in a city or not). Hospital stay (for other causes than the specific diagnosis) and use of municipal services such as home nursing care, home aid, and long- and short-term stay in institution was also recorded (dichotomised into use or no use) each month during the year before an emergency hospital admission, and each three-day period during the month before admission.
Acute admission to hospital
We identified dates of acute admission to hospital for the following common diagnosis (with corresponding diagnosis codes used from International Classification of Diseases, ICD-10 [14]):
Myocardial infarction (I21), heart failure (I50), stroke (I61, I63 and I64), fracture of hip/femur (S7) and pneumonia excl. COPD (J12-18, excl. those with COPD (J41-44 or J47) as a secondary diagnosis). Diagnoses were based on the primary diagnosis as recorded by the hospital. To make the pneumonia group of more homogenous we excluded all admissions with chronic obstructive pulmonary disease (COPD) as secondary diagnosis. For each patient, only the first admission for each specific diagnosis during the study period was included.
All included diagnoses are well-defined common causes of emergency hospital admissions in adults 50 years and older. Heart failure, hip-fracture and pneumonia are also ambulatory care sensitive conditions (ACSC). According to Ansari (2007): "ACSCs are conditions for which hospitalisation is thought to be avoidable with the application of preventive care and early disease management, usually delivered in the ambulatory setting" [15]. ACSCs are studied internationally with framework and definitions [15], and adapted to the Norwegian context [16].
General practice contacts before an emergency hospital admission
We included all contacts with general practitioners working in a regular GP and/or OOH setting, defined by claims of reimbursement generated by each practitioner after each contact and sent to The Norwegian Health Economics Administration (Helfo). The Helfo-data provided information on whether the claim was made in a regular GP or OOH setting. We coded contact with a regular GP (GP contact) and with the OOH services (OOH contact) into contact or no contact each month during one year before hospital admission and in three-day intervals during the month before admission. We omitted contacts on both the day of admission and the day before (i.e. day 0–1) to avoid registration of the contact directly leading to the emergency hospital admission.
Statistics
We used binomial generalised estimation equation models with a logit function (GEE [17]) to investigate GP/OOH contacts before the hospital admission. First, we estimated the percentage with contact per month during the year before the event. Secondly, we estimated the percentage with contact per triplets of days (2–4, 5–7, …., 29–31 days) before the admission. We performed the analysis separately for each of the selected patient groups.
For the analyses of GP and OOH contacts the year before hospital admission, we included time in the models as a categorical variable with 12 monthly intervals (each in a different temporal distance from the date of the admission). We adjusted for calendar month, age, sex, and whether the patient lived in a city or not. Analyses of GP contacts were also adjusted for whether the patient was institutionalised or not (including long- and short-term stay in municipal institution), as institutionalised patients usually are provided with municipal primary health care physicians not included in the GP scheme (but they still use the OOH services).
For the analyses of GP and OOH three-day contact the month before hospital admission, we grouped time as a categorical variable with 10 three-day intervals (each in a different temporal distance from the date of the event). We adjusted for the same variables as for the year before with the exception that we adjusted for weekday of admission event. We also adjusted for whether the patient was an inpatient (acute or elective) during the last month before admission, as they would see neither their GP nor OOH when in hospital.
We used the estimates from these analyses to produce graphical presentations of GP and OOH contacts during the year and month before hospital admission for each of the five patient groups. To make results more comparable between the patient groups, we chose to show the estimated percentages for a "standard" patient. We selected a woman aged 75 not in institution.
We repeated the analyses described above using conditional logistic regression models to calculate odds ratios of GP and OOH contacts at different time points during the year and month before admission (compared to six months before and the tree-day interval 31–29 days before the admission, respectively). In these analyses, patients are compared with themselves, automatically adjusting for all characteristics that are stable within person (e.g. sex, age and municipality of residence, as well as more difficult to measure variables such as stable co- or multimorbidities).
We explored the association between patient characteristics (sex, age group, institution) and having no GP or OOH contact in the month before an emergency hospital admission (no contact vs. contact) using logistic regression. These analyses included a statistical interaction term between age group and sex, and adjustment for institutional stay and living in a city. For each patient group we estimated the percentage with no contact for each of the subgroups according to age and sex, with predictions made for those not in institutions.
We performed all analyses with STATA version 15.1, and we present all precision levels with 95% confidence intervals (CI).
Results
Among 66,952 identified participants, between 0.6% (heart failure) and 1.3% (pneumonia) of the participants were admitted at least once for each of the five selected diagnosis.
Table 1 provides an overview of the patient groups analysed in the study. The groups differed in composition according to sex, age, living in a city and in the use of municipality and GP services during the month before the hospital admission.
Table 1.
Characteristics of each patient group in the study, based on first-time emergency hospital admission for each patient group (1 January 2012–31 December 2013).
| Myocardial Infarction | Heart failure | Stroke | Pneumonia (excl. COPD) | Hip fracture | |
|---|---|---|---|---|---|
| n (% of total study populationa) | 720 (1.1%) | 399 (0.6%) | 740 (1.1%) | 853 (1.3%) | 645 (1.0%) |
| Female | 31.8% | 61.4% | 49.6% | 48.2% | 71.9% |
| Age, mean (sd) | 71.8 (12.1) | 80.1 (10.3) | 75.8 (11.0) | 76.5 (11.7) | 80.8 (10.7) |
| 50–64 years | 230 (31.9%) | 39 (9.8%) | 132 (17.8%) | 162 (19.0%) | 62 (9.6%) |
| 65–79 years | 264 (36.7%) | 118 (29.6%) | 284 (38.4%) | 288 (33.8%) | 169 (26.2%) |
| 80+ years | 226 (31.4%) | 242 (60.7%) | 324 (43.8%) | 403 (47.2%) | 414 (64.2%) |
| Living in a city | 556 (77%) | 330 (83%) | 575 (78%) | 692 (81%) | 530 (82%) |
| Municipality services the month before emergency hospital admission | |||||
| Home careb,c | 21.0% | 46.4% | 27.4% | 43.7% | 40.2% |
| Living in a nursing homeb,d | 6.6% | 17.3% | 9.2% | 18.3% | 29.6% |
| Having municipality services at allb | 30.9% | 63.7% | 43.0% | 61.4% | 71.8% |
| Contacts with general practitioner, both regular GP (GP) and out-of-hours services (OOH) the month before emergency hospital admission | |||||
| GP and OOH | 4.6% | 14.5% | 7.0% | 12.3% | 7.9% |
| Only GP | 46.0% | 59.6% | 45.1% | 47.4% | 38.8% |
| Only OOH | 2.5% | 5.3% | 2.3% | 6.0% | 3.1% |
| No contact | 46.9% | 20.6% | 45.5% | 34.3% | 50.2% |
All age ≥50 in 2012, receiving somatic health care service in the two-year period 2012 to 2013; each patient can be registered in more than one group, but not more than once in each group since we counted only the first hospital admission for the respective diagnosis.
Total study population = 66,952 unique individuals.
Measured during the last 30 days before admission to hospital.
Both home nursing care and/or home aid.
Both short-term and/or long-term institution stay.
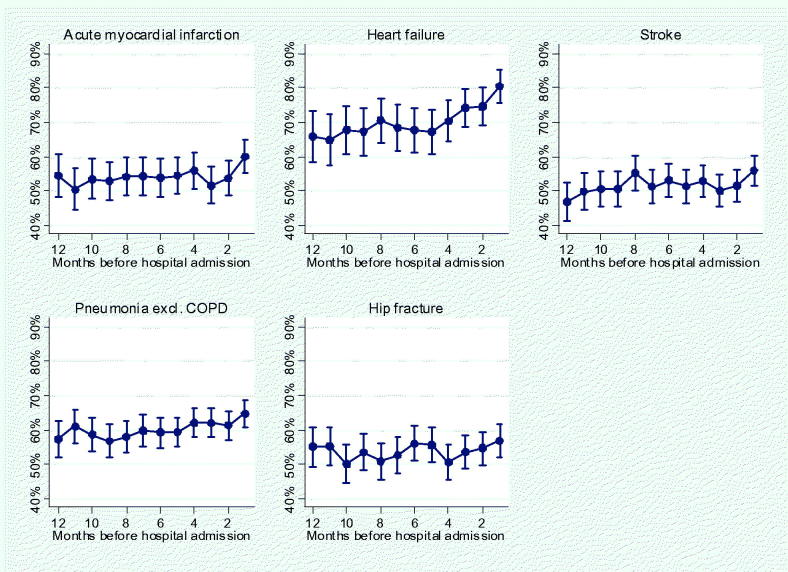
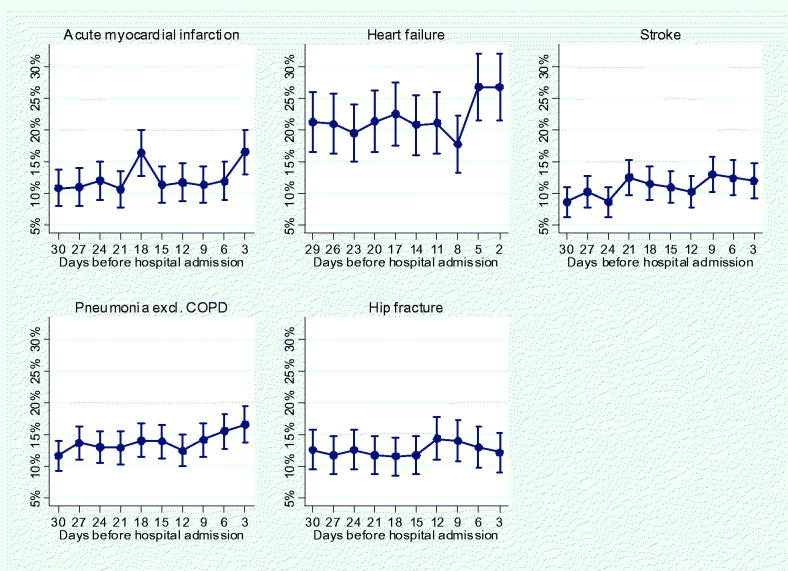
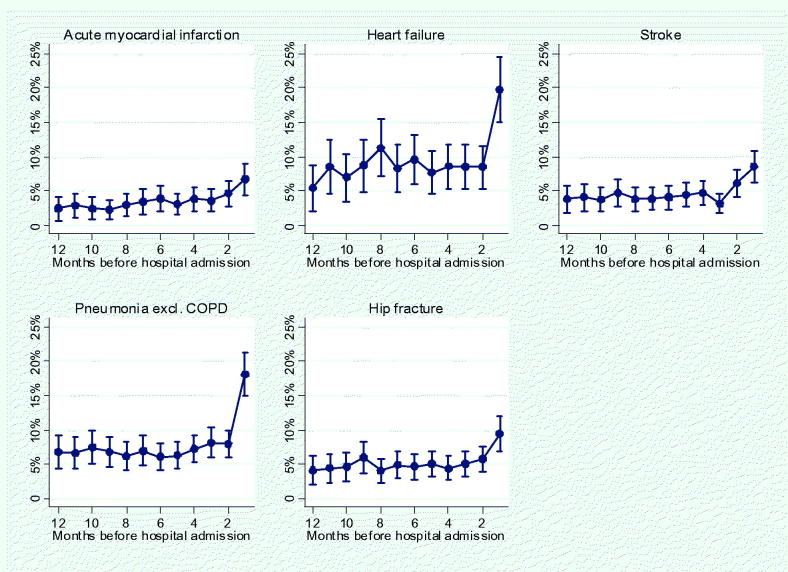
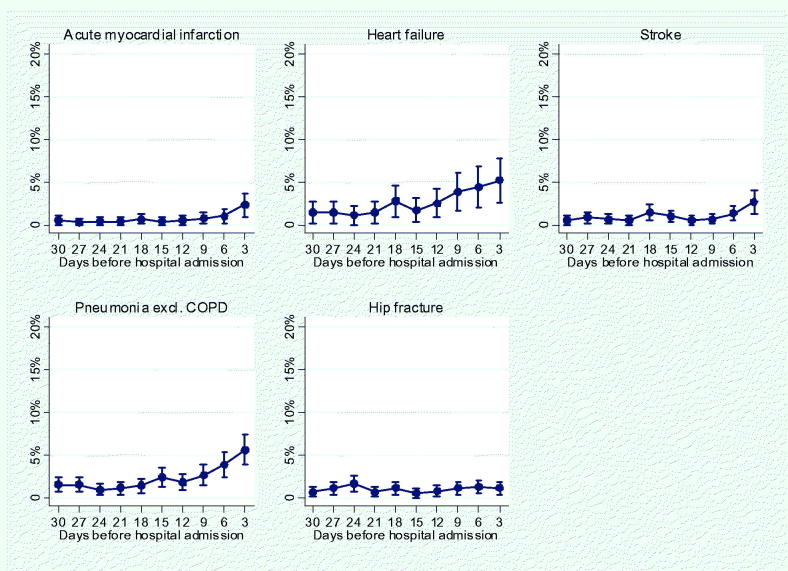
Figures 1–4 show results from the regression analyses as estimated percentages of monthly GP and OOH contact during the last year (Figures 1 and 3) and of three-day GP and OOH contact during the last month (Figures 2 and 4) before an emergency hospital admission. All estimated percentages are reported for our "standard" patient; a woman aged 75 in 2012, not in institution. Results from the conditional logistic regression analyses are presented in Tables A1–A4 (Appendix), comparing each patients’ GP and OOH contacts at different time points with their own contact level 6 months and 31–29 days before hospital admission. The results from these analyses were in line with the results from the main analysis.
Figure 1.
Estimated percentage (vertical axis) with at least one contact with a regular general practitioner (GP contact) per month for a woman aged 75 in 2012 not in institution according to time before an emergency hospital admission. Vertical lines represent 95% CIs. Analysis adjusted for calendar month, age, sex, living in a city and stay in an institution (both short- and long term).
Figure 2.
Estimated percentage (vertical axis) with at least one contact with a regular general practitioner (GP contact) per three-day interval for a woman aged 75 in 2012 not in institution according to time before an emergency hospital admission. Vertical lines represent 95% CIs. Analysis adjusted for weekday of admission, age, sex, living in a city, hospital stay and any stay in an institution (both short- and long term).
Figure 3.
Estimated percentage (vertical axis) with at least one OOH (general practitioner out-of-hours services) contact per month for a woman aged 75 in 2012 not in institution according to time before an emergency hospital admission. Vertical lines represent 95% CIs. Analysis adjusted for calendar month, age, sex, living in a city, and stay in an institution (both short- and long term).
Figure 4.
Estimated percentage (vertical axis) with at least one OOH (general practitioner out-of-hours services) contact per 3-day interval for a woman aged 75 in 2012 not in institution according to time before an emergency hospital admission. Vertical lines represent 95% CIs. Analysis adjusted for weekday of admission, age, sex, living in a city, hospital stay and stay in an institution (both short- and long term).
Regarding GP contact per month the year before hospital admission (Figure 1), the estimated percentage with GP contact (estimated for our "standard" patient) increased the last three months before hospital admission for heart failure: the percentage with GP contacts increased from 68% six months before admission to 81% one month before admission, an increase of 12%-points (95CI, 7–19%). For acute myocardial infarction and pneumonia, the increase was seen in the last month before hospital admission. Acute myocardial infarction increased from 54% six months before, to 60% one month before admission (increase of 6%-points (95%CI, 1–11%)), and pneumonia increased from 59% six months before, to 65% one month before admission (increase of 5%-points (95%CI, 1–10%)). Compared with their own GP contact 6 months before admission, the odds ratio of GP contact in the month before admission was 2.44 (95% CI, 1.59–3.75), 1.40 (95% CI, 1.06–1.84) and 1.36 (95% CI, 1.04–1.77) for patients admitted for heart failure, myocardial infarction and pneumonia, respectively (see Appendix Table A1).
When investigating GP contact per three-day interval the last month before hospital admission (Figure 2), an increase in contacts occurred during the three-day intervals close to the time of admission for stroke, pneumonia and myocardial infarction. The estimated percentage with GP contact increased during the last three three-day intervals before hospital admission for stroke, increasing from 9% 31–29 days before, to 12% 4–2 days before admission (increase of 3%-points (95%CI, 0–6%)). For pneumonia, the percentage with GP contact increased in the last two three-day intervals before hospital admission, increasing from 12% 31–29 days before, to 17% 4–2 days before admission (increase of 5%-points (95% CI, 2–8%)). For acute myocardial infarction, GP contacts increased day 21–19 and in the last three-day interval before hospital admission, increasing from 11% 31–29 days before, to 16% 4-2 days before admission (an increase of 6%-points (95% CI, 2–9%)). Compared with their own GP contact in the three-day interval 31–29 days before admission, the odds ratio of GP contact in the last three-day interval (4–2 days before) before admission was 1.48 (95% CI, 1.02–2.14), 1.57 (95% CI, 1.16–2.12) and 1.73 (95% CI, 1.20–2.48) for patients admitted for stroke, pneumonia and myocardial infarction, respectively (see Table A2 in Appendix).
Regarding OOH contacts the year before hospital admission (Figure 3), all patient groups had increased contact the last month before admission. The estimated percentage with OOH contact the last month before admission varied from 7% (95% CI, 4–9%) for myocardial infarction to 20% (95% CI, 15–25%) for heart failure. Compared with their own OOH contact 6 months before admission the odds ratio of OOH contact in the month before admission varied from 1.96 (95%Ci, 1.11–3.48) for myocardial infarction to 3.68 (95% CI, 2.46–5.50) for pneumonia (see Table A3 in Appendix).
All patient groups had increased OOH contact the last three-day interval before an emergency hospital admission, except hip fracture patients (Figure 4 and Appendix Table A4).
No contacts
For all patient groups, the estimated percentage with no GP or OOH contact during the last month before emergency hospital admission was higher among younger and men (Table A5, Appendix), with larger differences between age groups in men compared to women (p-value for interaction term between age group and sex was <0.05 in all patient groups). The group without contact was highest for men 50–64 years being admitted with stroke (estimated percentage 65% (95% CI, 62–68%)) and acute myocardial infarction (estimated percentage 62% (95% CI, 60–65%)). Few patients among those aged 80+ being admitted to hospital with heart failure did not contact their GP prior to admission, only 10% (95% CI, 08–12%) in men and 17% (95% CI, 15–19%) in women.
Discussion
The majority of patients in the age group 50+ acutely admitted for one of the five selected conditions (myocardial infarction, heart failure, stroke, pneumonia or hip fracture) had contact with primary care physicians each month before the admission, especially with regular GPs. The percentage in contact with GPs often increased close to the time of hospital admission, but the time and extent of this increase varied substantially between groups according to diagnosis, as well as with type of GP service (regular GP and/or OOH services). Those admitted for heart failure stood out with a higher percentage with regular GP and OOH contacts before the hospital admission. A substantial group of patients contacted neither their GP nor OOH the last month before the emergency hospital admission, varying according to diagnosis, sex and age group.
Strengths and limitations
To our knowledge, this is the first study to investigate the contact with GP services before an emergency hospital admission. We based our study on data from a total population regarding contacts with both primary and secondary somatic health care, giving limited risk of selection bias. Our study population comprised both urban and rural municipalities, but since all three rural municipalities were located close to the urban municipality (a large city) we could only partly address possible urban-rural variations in health and help seeking behaviour [18].
The study could have benefitted from more information on clinical characteristics as well as the social situation of the patients. We only had data regarding somatic hospital contacts and did not include psychiatric specialised services. The included patient groups were rather small, not providing precision to present smaller changes in health care contact prior to hospital admission.
The results should be interpreted in the light that health care, and especially primary care, is organised quite differently in different countries. Even in the Nordic countries there are differences in the organisation of GP services [13], though no distinct pattern has been found of GPs in one country providing more diverse services for their patients than in the other Nordic countries [19]. The delineation of responsibilities between primary and secondary health care also differs [20].
Interpretation of results and comparison with existing literature
In this study, we investigated contacts with primary care physicians as regular GPs and the OOH services. While regular GP contacts could indicate planned or proactive care, more frequent GP contact could indicate either poor health or recent deterioration [21]. Contact with the OOH services are indicative of emergency conditions which need to be dealt with immediately, but might also indicate a potential for prevention within the regular GP services [22].
The patient group admitted to hospital with heart failure had the highest contact with the primary physicians, increasing towards the date of admission. Heart failure is a heterogeneous disease due to both aetiology and comorbidity, and despite numerous treatments available, heart failure-patients experience progressively worsening symptoms, frequent admission to hospital, and premature death [23]. Our results indicate that GPs do monitor heart-failure-patients, and that GP contact increases when the condition worsens.
Those admitted to hospital with acute myocardial infarction and stroke had similar patterns: a modest increase in the contact with both regular GP and OOH services immediately before admission. This could mean that some patients contacted the services with symptoms related to the cardiovascular event that happened only days later. Streamlining of specialised services after a serious cardio- or cerebrovascular event is underscored as an important task for improving patient prognosis [24–26]. The extent to which GPs could better capture early signals of these events, and thereby intervene in order to prevent the need for emergency hospital admission has been less scrutinised, although there are several guidelines for the prevention according to risk factors [27,28].
For pneumonia (excl. COPD), the patients increased their GP and OOH contacts the last week the last month before the emergency hospital admission. Patients with pneumonia could be seen as a particularly interesting group, as the condition usually develops sub-acutely, and early detection and intervention (e.g. treatment with antibiotics initiated at an earlier stage) could possibly reduce risk of hospital admission [29]. For the pneumonia group, the increase in contact with the OOH services before admission was particularly prominent. This could be due to community-acquired pneumonia with acute symptoms and need for hospital admission for the most the severely ill [29]. The results do not support that an emergency hospital admission for pneumonia is the final stage of a general health deterioration over time as only a small trend of increased contact over the last months before admission could be observed.
A hip fracture is often regarded a result of a general health decline. Our results did not show any substantial change in contact with GP services as an indicator of such health decline neither the year nor month before the emergency hospital admission. The explanation for this could possibly relate to an under-use of GP services in this group or that the patients are monitored and treated in the municipal services. Hip fracture patients are often elderly, frail and multi-morbid [30], which comply well with the characteristics of our patient group, including the fact that almost 30% were institutionalised and more than 70% had municipal care services.
Our study presented results for common diagnoses, three of them (heart failure, pneumonia and hip fracture) regarded as part of potentially avoidable hospitalisations, the ambulatory care sensitive conditions [15], adapted to the Norwegian context [16]. Other studies point to the role of GPs in preventing these hospital admissions [4,31], though Norwegian results have been inconclusive [16,32]. We did not find any striking differences between the contact patterns of the diagnosis regarding whether they were potentially avoidable or not, though our data are limited for any conclusion. Our study might suggest some important targets and relevant areas for further exploration. First, our results point towards the regular GP having an important role to most patients. Second, our results underscore the need to consider patient groups according to the medical diagnosis when talking about the role of primary health care in preventing admission to hospital. Prevention strategies from primary care physicians would be challenging in patient groups where a substantial part did not have any contacts with GP services (e.g. by treating disease/symptoms at a stage so that admission to hospital becomes unnecessary). Groups with high use of OOH services and an increase in OOH services before admission to hospital (as seen with heart failure and pneumonia) could be an interesting target for further exploration of the potential for intervention in the GP services.
Conclusion
The majority of patients with emergency hospital admission for the five selected conditions (myocardial infarction, heart failure, stroke, pneumonia or hip fracture) were regularly in contact with a general practitioner (GP) before admission. This points towards GPs’ having an important role in these patients’ health care. Nevertheless, a substantial percentage of the patients admitted with these severe diagnoses did not see their GPs the month before hospital admission. This group of patients could represent a possible target for prevention, although not easily reached.
Ethics approval
The Regional Committee for Medical and Health Research Ethics in Central Norway approved the study (2011/2047).
Appendix
Table A1.
Odds ratios for GP (regular general practitioner) contact month by month compared to 6 months before an emergency hospital admission for the different diagnoses.
| Myocardial infarction |
Heart failure |
Stroke |
Pneumonia (excl. COPD) |
Hip fracture |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| 12 months before | 1.04 | (0.75–1.44) | 0.86 | (0.53–1.38) | 0.70 | (0.50–0.97) | 0.88 | (0.65–1.20) | 0.95 | (0.66–1.39) |
| 6 months before | 1.00 | (reference) | 1.00 | (reference) | 1.00 | (reference) | 1.00 | (reference) | 1.00 | (reference) |
| 5 months before | 1.04 | (0.78–1.38) | 0.96 | (0.64–1.44) | 0.91 | (0.68–1.20) | 1.00 | (0.76–1.31) | 0.98 | (0.71–1.36) |
| 4 months before | 1.13 | (0.85–1.49) | 1.15 | (0.77–1.73) | 0.99 | (0.75–1.32) | 1.18 | (0.90–1.55) | 0.73 | (0.53–1.01) |
| 3 months before | 0.89 | (0.67–1.17) | 1.51 | (1.00–2.29) | 0.85 | (0.65–1.13) | 1.17 | (0.90–1.53) | 0.87 | (0.63–1.20) |
| 2 months before | 0.99 | (0.75–1.31) | 1.56 | (1.03–2.35) | 0.94 | (0.71–1.23) | 1.13 | (0.87–1.47) | 0.93 | (0.67–1.27) |
| 1 month before | 1.40 | (1.06–1.84) | 2.44 | (1.59–3.75) | 1.18 | (0.89–1.55) | 1.36 | (1.04–1.77) | 1.04 | (0.75–1.43) |
Estimates from conditional logistic regression analyses, comparing contacts within patients.
Table A2.
Odds ratios for GP (regular general practitioner) contact in three-day intervals compared to the three-day interval 31–29 days before an emergency hospital admission for the different diagnoses.
| Myocardial infarction |
Heart failure |
Stroke |
Pneumonia (excl. COPD) |
Hip fracture |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| 31–29 days before | 1.00 | (reference) | 1.00 | (reference) | 1.00 | (reference) | 1.00 | (reference) | 1.00 | (reference) |
| 19–17 days before | 1.70 | (1.19–2.45) | 1.10 | (0.76–1.60) | 1.41 | (0.98–2.04) | 1.26 | (0.92–1.71) | 0.90 | (0.60–1.36) |
| 16–14 days before | 1.07 | (0.73–1.57) | 0.99 | (0.68–1.44) | 1.32 | (0.91–1.92) | 1.24 | (0.91–1.68) | 0.92 | (0.62–1.38) |
| 13–11 days before | 1.11 | (0.75–1.63) | 1.01 | (0.69–1.47) | 1.21 | (0.83–1.77) | 1.08 | (0.79–1.48) | 1.20 | (0.81–1.77) |
| 10–8 days before | 1.07 | (0.73–1.58) | 0.80 | (0.54–1.17) | 1.63 | (1.14–2.35) | 1.27 | (0.94–1.73) | 1.15 | (0.78–1.70) |
| 7–5 days before | 1.13 | (0.77–1.65) | 1.41 | (0.98–2.02) | 1.54 | (1.07–2.23) | 1.44 | (1.06–1.95) | 1.04 | (0.70–1.54) |
| 4–2 days before | 1.73 | (1.20–2.48) | 1.40 | (0.98–2.02) | 1.48 | (1.02–2.14) | 1.57 | (1.16–2.12) | 0.96 | (0.64–1.44) |
Estimates from conditional logistic regression analyses, comparing contacts within patients.
Table A3.
Odds ratios for OOH (general practitioner out-of-hours service) contact month by month compared to 6 months before an emergency hospital admission for the different diagnoses.
| Myocardial infarction |
Heart failure |
Stroke |
Pneumonia (excl. COPD) |
Hip fracture |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| 12 months before | 0.62 | (0.27–1.43) | 0.49 | (0.23–1.04) | 0.97 | (0.49–1.93) | 1.08 | (0.63–1.85) | 0.85 | (0.44–1.65) |
| 6 months before | 1.00 | (reference) | 1.00 | (reference) | 1.00 | (reference) | 1.00 | (reference) | 1.00 | (reference) |
| 5 months before | 0.78 | (0.40–1.54) | 0.75 | (0.42–1.35) | 1.12 | (0.63–2.00) | 1.03 | (0.64–1.65) | 1.10 | (0.63–1.93) |
| 4 months before | 1.02 | (0.54–1.92) | 0.85 | (0.49–1.49) | 1.26 | (0.72–2.20) | 1.22 | (0.78–1.91) | 0.94 | (0.53–1.65) |
| 3 months before | 0.93 | (0.49–1.76) | 0.86 | (0.49–1.50) | 0.76 | (0.42–1.39) | 1.36 | (0.87–2.11) | 1.11 | (0.64–1.91) |
| 2 months before | 1.31 | (0.72–2.38) | 0.91 | (0.52–1.57) | 1.56 | (0.92–2.65) | 1.30 | (0.84–2.02) | 1.30 | (0.77–2.22) |
| 1 month before | 1.96 | (1.11–3.48) | 2.83 | (1.74–4.61) | 2.42 | (1.45–4.03) | 3.68 | (2.46–5.50) | 2.47 | (1.50–4.06) |
Estimates from conditional logistic regression analyses, comparing contacts within patients.
Table A4.
Odds ratios for OOH (general practitioner out-of-hours service) contact in three-day intervals compared to the three-day interval 31–29 days before an emergency hospital admission for the different diagnoses.
| Myocardial infarction |
Heart failure |
Stroke |
Pneumonia (excl. COPD) |
Hip fracture |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| 31–29 days before | 1.00 | (reference) | 1.00 | (reference) | 1.00 | (reference) | 1.00 | (reference) | 1.00 | (reference) |
| 19–17 days before | 1.82 | (0.42–7.84) | 2.05 | (0.69–6.10) | 3.15 | (0.99–9.97) | 0.91 | (0.40–2.10) | 1.87 | (0.62–5.66) |
| 16–14 days before | 1.08 | (0.21–5.49) | 1.23 | (0.37–4.10) | 2.05 | (0.60–6.94)) | 1.60 | (0.77–3.35) | 0.82 | (0.22–3.09) |
| 13–11 days before | 1.50 | (0.32–6.91) | 1.90 | (0.62–5.78) | 1.00 | (0.25–4.07) | 1.17 | (0.53–2.56) | 1.30 | (0.39–4.35) |
| 10–8 days before | 2.27 | (0.55–9.41) | 3.03 | (1.07–8.59) | 1.26 | (0.33–4.77) | 1.77 | (0.86–3.65) | 2.06 | (0.67–6.27) |
| 7–5 days before | 3.19 | (0.81–12.51) | 3.56 | (1.27–9.93) | 2.90 | (0.90–9.35) | 2.66 | (1.34–5.26) | 2.33 | (0.78–6.97) |
| 4–2 days before | 8.10 | (2.29–28.63) | 4.33 | (1.58–11.88) | 6.16 | (2.07–18.35) | 3.95 | (2.05–7.59) | 2.09 | (0.68–6.36) |
Estimates from conditional logistic regression analyses, comparing contacts within patients.
Table A5.
The estimated percentage (with 95% Confidence intervals) with no contact with general practitioners (regular or out-of-hours service) the last month before an emergency hospital admission for patients not living in an institution, according to age group and sex.
| Myocardial infarction | Heart failure | Stroke | Pneumonia (excl. COPD) | Hip fracture | |
|---|---|---|---|---|---|
| Female | |||||
| 50–64 years | 43% (39–48) | 25% (18–32) | 46% (41–50) | 32% (29–36) | 44% (38–49) |
| 65–79 years | 33% (30–36) | 15% (12–19) | 45% (42–47) | 30% (27–32) | 41% (38–44) |
| 80+ years | 36% (33–39) | 17% (15–19) | 35% (32–37) | 32% (30–34) | 32% (30–34) |
| Male | |||||
| 50–64 years | 62% (60–65) | 33% (27–39) | 65% (62–68) | 42% (39–45) | 52% (46–58) |
| 65–79 years | 51% (49–54) | 13% (11–15) | 47% (45–49) | 29% (27–31) | 47% (42–51) |
| 80+ years | 30% (27–32) | 10% (08–12) | 35% (32–38) | 24% (22–25) | 30% (27–34) |
| p-value for interactiona | <0.001 | 0.002 | <0.001 | <0.001 | 0.024 |
Based on the results from a logistic regression with an interaction between sex and age group, and adjusted for living in an institution (patients who had no days/nights in institution the last month before an emergency hospital admission) and living in a city (patients living in a city when admitted to hospital).
Interaction term between age group and sex.
Funding Statement
This work was supported by the Norwegian University of Science and Technology, and is a part of a larger project ‘Health care services under pressure – Consequences for patient flows, efficiency and patient safety in Norway’ funded by the Norwegian Research Council (grant number 256579). The data used was from a project also funded by the Norwegian Research Council (grant number 220553).
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.Barker I, Steventon A, Deeny SR. Association between continuity of care in general practice and hospital admissions for ambulatory care sensitive conditions: cross sectional study of routinely collected, person level data. BMJ. 2017;356:j84. [DOI] [PubMed] [Google Scholar]
- 2.Helse- og Omsorgsdepartementet [the Norwegian Ministry of Health and Care Services] [Internet]. Forskrift om Fastlegeordning i Kommunene [Ordination of the Municipal Regular General Practitioner Scheme]; 2012. [cited 2019 Nov 28]. Available from: https://lovdata.no/dokument/SF/forskrift/2012-08-29-842#KAPITTEL_3
- 3.Rosano A, Loha CA, Falvo R, et al. . The relationship between avoidable hospitalization and accessibility to primary care: a systematic review. Eur J Public Health. 2013;23:356–360. [DOI] [PubMed] [Google Scholar]
- 4.van Loenen T, van den Berg MJ, Westert GP, et al. . Organizational aspects of primary care related to avoidable hospitalization: a systematic review. Fam Practice. 2014;31:502–516. [DOI] [PubMed] [Google Scholar]
- 5.Dantas I, Santana R, Sarmento J, et al. . The impact of multiple chronic diseases on hospitalizations for ambulatory care sensitive conditions. BMC Health Serv Res. 2016;16:348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cecil E, Bottle A, Cowling TE, et al. . Primary care access, emergency department visits, and unplanned short hospitalizations in the UK. Pediatrics 2016;137:e20151492. [DOI] [PubMed] [Google Scholar]
- 7.Lass M, Tatari CR, Merrild CH, et al. . Contact to the out-of-hours service among Danish parents of small children – a qualitative interview study. Scand J Prim Health Care. 2018;36:216–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cowling TE, Cecil EV, Soljak MA, et al. . Access to primary care and visits to emergency departments in England: a cross-sectional, population-based study. PLoS One. 2013;8:e66699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agarwal S, Banerjee J, Baker R, et al. . Potentially avoidable emergency department attendance: interview study of patients' reasons for attendance. Emerg Med J. 2012;29:e3. [DOI] [PubMed] [Google Scholar]
- 10.Kohnke H, Zielinski A. Association between continuity of care in Swedish primary care and emergency services utilisation: a population-based cross-sectional study. Scand J Prim Health Care. 2017;35:113–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huntley A, Lasserson D, Wye L, et al. . Which features of primary care affect unscheduled secondary care use? A systematic review. BMJ Open. 2014;4:e004746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Helsedirektoratet [Internet] Fastlegestatistikk [Regular General Practitioner Statistics]; 2017. [updated 18 Dec 2018; cited 2019 Jan 8]. Available from: https://helsedirektoratet.no/statistikk-og-analyse/fastlegestatistikk
- 13.Olsen KR, Anell A, Häkkinen U, et al. . General practice in the Nordic countries. Nordic J Health Eco. 2016;4:56–67. [Google Scholar]
- 14.World Health Organisation [Internet] International Classification of Diseases and Related Health Problems, ICD-10 1990/2018 [cited 2018 Jul 1]. Available from: http://www.who.int/classifications/icd/en/
- 15.Ansari Z. The concept and usefulness of ambulatory care sensitive conditions as indicators of quality and access to primary health care. Aust J Prim Health. 2007;13:91–110. [Google Scholar]
- 16.Helsedirektoratet [Internet] Samhandlingsstatistikk 2012–13 [Cooperation statistics 2012–13]. Helsedirektoratet. no; Feb 2014. Report No.: 978-82-8081-313-8 Contract No.: 224. [Google Scholar]
- 17.Twisk JWR. Applied longitudinal data analysis for epidemiology. Cambridge: Cambridge University Press; 2003. [Google Scholar]
- 18.Verheij RA. Explaining urban-rural variations in health: a review of interactions between individual and environment. Soc Sci Med. 1996;42:923–935. [DOI] [PubMed] [Google Scholar]
- 19.Eide TB, Straand J, Björkelund C, et al. . Differences in medical services in Nordic general practice: a comparative survey from the QUALICOPC study. Scand J Primary Health Care. 2017;35:153–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kringos D, Boerma W, Bourgueil Y, et al. . The strength of primary care in Europe: an international comparative study. Br J Gen Pract. 2013;63:e742–e750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Youens D, Harris M, Robinson S, et al. . Regularity of contact with GPs: measurement approaches to improve valid associations with hospitalization. Fam Practice. 2019 Jan 26 [cited 2019 Mar 06] doi: 10.1093/fampra/cmz002 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 22.Sandvik H, Hunskaar S. Frequent attenders at primary care out-of-hours services: a registry-based observational study in Norway. BMC Health Serv Res. 2018;18:492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McMurray JJV, Pfeffer MA. Heart failure. Lancet. 2005;365:1877–1889. [DOI] [PubMed] [Google Scholar]
- 24.Anderson L, Sharp GA, Norton RJ, et al. . Home‐based versus centre‐based cardiac rehabilitation. Cochrane Database Syst Rev. 2017;6:CD007130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith SC Jr, Benjamin EJ, Bonow RO, et al. . AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol. 2011;58:2432–2446. [DOI] [PubMed] [Google Scholar]
- 26.Stroke Unit Trialists’ Collaboration Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev. 2013;9:CD000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Piepoli MF, Hoes AW, Agewall S, et al. . 2016 European Guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37:2315–2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meschia JF, Bushnell C, Boden-Albala B, et al. . Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:3754–3832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prina E, Ranzani OT, Torres A. Community-acquired pneumonia. Lancet. 2015;386:1097–1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Johansen A, Golding D, Brent L, et al. . Using national hip fracture registries and audit databases to develop an international perspective. Injury. 2017;48:2174–2179. [DOI] [PubMed] [Google Scholar]
- 31.Menec VH, Sirski M, Attawar D, et al. . Does continuity of care with a family physician reduce hospitalizations among older adults? J Health Serv Res Policy. 2006;11:196–201. [DOI] [PubMed] [Google Scholar]
- 32.Deraas TS, Berntsen GR, Jones AP, et al. . Associations between primary healthcare and unplanned medical admissions in Norway: a multilevel analysis of the entire elderly population. BMJ Open. 2014;4:e004293. [DOI] [PMC free article] [PubMed] [Google Scholar]