Abstract
Background
Expanding public health insurance seeks to attain several desirable objectives, including increasing access to healthcare services, reducing the risk of catastrophic healthcare expenditures, and improving health outcomes. The extent to which these objectives are met in a real-world policy context remains an empirical question of increasing research and policy interest in recent years.
Methods
We reviewed systematically empirical studies published from July 2010 to September 2016 using Medline, Embase, Econlit, CINAHL Plus via EBSCO, and Web of Science and grey literature databases. No language restrictions were applied. Our focus was on both randomised and observational studies, particularly those including explicitly attempts to tackle selection bias in estimating the treatment effect of health insurance. The main outcomes are: (1) utilisation of health services, (2) financial protection for the target population, and (3) changes in health status.
Findings
8755 abstracts and 118 full-text articles were assessed. Sixty-eight studies met the inclusion criteria including six randomised studies, reflecting a substantial increase in the quantity and quality of research output compared to the time period before 2010. Overall, health insurance schemes in low- and middle-income countries (LMICs) have been found to improve access to health care as measured by increased utilisation of health care facilities (32 out of 40 studies). There also appeared to be a favourable effect on financial protection (26 out of 46 studies), although several studies indicated otherwise. There is moderate evidence that health insurance schemes improve the health of the insured (9 out of 12 studies).
Interpretation
Increased health insurance coverage generally appears to increase access to health care facilities, improve financial protection and improve health status, although findings are not totally consistent. Understanding the drivers of differences in the outcomes of insurance reforms is critical to inform future implementations of publicly funded health insurance to achieve the broader goal of universal health coverage.
Introduction
In recent decades, achieving universal health coverage (UHC) has been a major health policy focus globally.[1–3] UHC entitles all people to access healthcare services through publicly organised risk pooling,[4] safeguarding against the risk of catastrophic healthcare expenditures.[5] Low- and middle-income countries (LMICs) face particular challenges in achieving UHC due to particularly limited public resources for health care, inefficient allocation, over-reliance on out-of-pocket payments, and often large population size.[5] As a result, access to health care and the burden of financial cost in LMICs tends to be worse for the poor, often resulting in forgone care.[6–8]
Introducing and increasing the coverage of publicly organised and financed health insurance is widely seen as the most promising way of achieving UHC,[9,10] since private insurance is mostly unaffordable for the poor.[11] Historically, social health insurance, tax-based insurance, or a mix of the two have been the dominant health insurance models amongst high income countries and some LMICs, including Brazil, Colombia, Costa Rica, Mexico, and Thailand.[12] This is partly influenced by the size of the formal sector economy from which taxes and payroll contributions can be collected. In recent decades, community-based health insurance (CBHI) or “mutual health organizations” have become increasingly popular among LMICs, particularly in Sub-Saharan Africa (e.g. Burkina Faso,[13] Senegal[14] and Rwanda[15]) as well as Asia (e.g. China[16] and India[17]). CBHI has emerged as an alternative health financing strategy, particularly in cases where the public sector has failed to provide adequate access to health care.[18]
We searched for existing systematic reviews on health insurance in the Cochrane Database for Systematic Reviews, Medline, Embase, and Econlit. Search terms “health insurance”, “low-middle income countries”, and “utilisation” were used alongside methodological search strategy to locate reviews. Seven systematic reviews were identified of varying levels of quality, [19–26] with Acharya et al.[27] being the most comprehensive. The majority of existing reviews has suggested that publicly-funded health insurance has typically shown a positive impact on access to care, while the picture for financial protection was mixed, and evidence of the impact on health status was very sparse.
This study reviews systematically the recent fast-growing evidence on the impact of health insurance on health care utilisation, financial protection and health status in LMICs. Since the publication of Acharya et al. (which conducted literature searches in July 2010), the empirical evidence on the impact of health insurance has expanded significantly in terms of quantity and quality, with growing use of sophisticated techniques to account for statistical challenges[28] (particularly insurance selection bias). This study makes an important contribution towards our understanding of the impact of health insurance in LMICs, taking particular care in appraising the quality of studies. We recognise the heterogeneity of insurance schemes implemented in LMICs and therefore do not attempt to generalise findings, but we aim to explore the pattern emerging from various studies and to extract common factors that may affect the effectiveness of health insurance, that should be the focus of future policy and research. Furthermore, we explore evidence of moral hazard in insurance membership, an aspect that was not addressed in the Acharya et al review.[27]
Methods
This review was planned, conducted, and reported in adherence with PRISMA standards of quality for reporting systematic reviews.[29]
Participants
Studies focusing on LMICs are included, as measured by per capita gross national income (GNI) estimated using the World Bank Atlas method per July 2016.[30]
Intervention
Classification of health insurance can be complicated due to the many characteristics defining its structure, including the mode of participation (compulsory or voluntary), benefit entitlement, level of membership (individual or household), methods for raising funds (taxes, flat premium, or income-based premium) and the mechanism and extent of risk pooling [31]. For the purpose of this review, we included all health insurance schemes organised by government, comprising social health insurance and tax-based health insurance. Private health insurance was excluded from our review, but we recognise the presence of community-based health insurance (CBHI) in many LMICs, especially in Africa and Asia [18]. We also therefore included CBHI if it was scaled up nationally or was actively promoted by national government. Primary studies that included both public and private health insurance were also considered for inclusion if a clear distinction between the two was made in the primary paper. Studies examining other types of financial incentives to increase the demand for healthcare services, such as voucher schemes or cash transfers, were excluded.
Control group
In order to provide robust evidence on the effect on insurance, it is necessary to compare an insured group with an appropriate control group. In this review, we selected studies that used an uninsured population as the control group. Multiple comparison groups were allowed, but an uninsured group had to be one of them.
Outcome measures
We focus on three main outcomes:
Utilisation of health care facilities or services (e.g. immunisation coverage, number of visits, rates of hospitalisation).
Financial protection, as measured by changes in out-of-pocket (OOP) health expenditure at household or individual level, and also catastrophic health expenditure or impoverishment from medical expenses.
Health status, as measured by morbidity and mortality rates, indicators of risk factors (e.g. nutritional status), and self-reported health status.
The scope of this review is not restricted to any level of healthcare delivery (i.e. primary or secondary care). All types of health services were considered in this review.
Types of studies
The review includes randomized controlled trials, quasi-experimental studies (or “natural experiments”[32]), and observational studies that account for selection bias due to insurance endogeneity (i.e. bias caused by insurance decisions that are correlated with the expected level of utilisation and/or OOP expenditure). Observational studies that did not take account of selection bias were excluded.
Databases and search terms
A search for relevant articles was conducted on 6 September 2016 using peer-reviewed databases (Medline, Embase, Econlit, CINAHL Plus via EBSCO and Web of Science) and grey literatures (WHO, World Bank, and PAHO). Our search was restricted to studies published since July 2010, immediately after the period covered by the earlier Acharya et al. (2012) review. No language restrictions were applied. Full details of our search strategy are available in the supporting information (S1 Table).
Screening and data extraction
Two independent reviewers (DE and MS) screened all titles and abstracts of the initially identified studies to determine whether they satisfied the inclusion criteria. Any disagreement was resolved through mutual consensus. Full texts were retrieved for the studies that met the inclusion criteria. A data collection form was used to extract the relevant information from the included studies.
Assessment of study quality
We used the Grades of Assessment, Development and Evaluation (GRADE) system checklist[33,34] which is commonly used for quality assessment in systematic reviews. However, GRADE does not rate observational studies based on whether they controlled for selection bias. Therefore, we supplemented the GRADE score with the ‘Quality of Effectiveness Estimates from Non-randomised Studies’ (QuEENS) checklist.[35]
cRandomised studies were considered to have low risk of bias. Non-randomised studies that account for selection on observable variables, such as propensity score matching (PSM), were categorised as high risk of bias unless they provided adequate assumption checks or compared the results to those from other methods, in which case they may be classed as medium risk. Non-randomised studies that account for selection on both observables and unobservables, such as regression with difference-in-differences (DiD) or Heckman sample selection models, were considered to have medium risk of bias–some of these studies were graded as high or low risk depending on sufficiency of assumption checks and comparison with results from other methods.
Heterogeneity of health insurance programmes across countries and variability in empirical methods used across studies precluded a formal meta-analysis. We therefore conducted a narrative synthesis of the literature and did not report the effect size. Throughout this review, we only considered three possible effects: positive outcome, negative outcome, or no statistically significant effect (here defined as p-value > 0.1).
Results
Results of the search
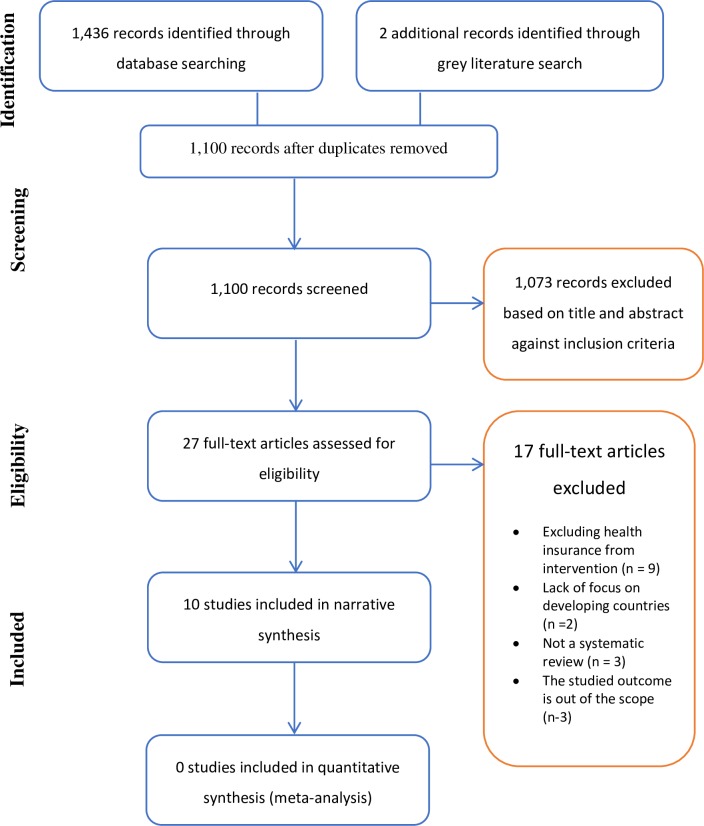
Our database search identified 8,755 studies. Five additional studies were retrieved from grey literature. After screening of titles and abstracts, 118 studies were identified as potentially relevant. After reviewing the full-texts, 68 studies were included in the systematic review (see Fig 1 for the PRISMA diagram). A full description of the included studies is presented in the supporting information (S2 Table). Of the 68 included studies, 40 studies examined the effect on utilisation, 46 studies on financial protection, and only 12 studies on health status (see Table 1).
Fig 1. PRISMA flow diagram for included and excluded studies.
Table 1. Summary of the impact of health insurance on utilisation, financial protection, and health outcomes.
| QUEENS* score and GRADE | Utilisation (N = 40) | Financial protection† (N = 46) | Health status (N = 12) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Positive effect | No effect | Negative effect | Total | Positive effect | No effect | Negative effect | Total | Positive effect | No effect | Negative effect | Total | |
| 3 and Moderate | 1 | 1 | 0 | 2 | 3 | 1 | 0 | 4 | 2 | 0 | 1 | 3 |
| 3 and Low | 6 | 0 | 1 | 7 | 3 | 4 | 1 | 8 | 2 | 0 | 0 | 2 |
| 2 and Low | 15 | 3 | 0 | 18 | 15 | 8 | 1 | 24 | 3 | 2 | 0 | 5 |
| 1 and Low | 10 | 3 | 0 | 13 | 4 | 4 | 2 | 10 | 2 | 0 | 0 | 2 |
| Total | 32 | 7 | 1 | 40 | 25 | 17 | 4 | 46 | 9 | 2 | 1 | 12 |
* QUEENS score: 1 = high risk of bias; 2 = moderate risk; 3 = low risk; GRADE score: Low = low quality; Moderate = moderate quality; High = high quality
† Positive effect for financial protection means that health insurance decreases out-of-pocket health expenditure or reduces the event of catastrophic health expenditure
Utilisation of health care
Table 2 collates evidence on the effects of health insurance on utilisation of healthcare services. Three main findings were observed:
Table 2. Summary of studies reporting utilisation of health care (N = 40), by countries and year.
| Study | Year | Country/Area | Type/name of insurance* | Effect | QUEENS** | GRADE† |
|---|---|---|---|---|---|---|
| Robyn et al[13] | 2012 | Burkina Faso, Nouna district | CBHI | 0 | 3 | Moderate |
| Robyn et al[38] | 2012 | Burkina Faso, Nouna district | CBHI | + | 1 | Low |
| Levine, Polimeni, and Ramage[39] |
2016 | Cambodia | CBHI | + | 3 | Moderate |
| Babiarz et al[40] | 2010 | China | NCMS (Voluntary) | 0 | 2 | Low |
| Lu, Liu, and Shen[41] | 2012 | China | NCMS (Voluntary) | + | 2 | Low |
| Chen et al[42] | 2014 | China | URBMI (Voluntary) | + | 2 | Low |
| Hou et al[43] | 2014 | China | NCMS (Voluntary) | + | 2 | Low |
| Liu and Zhao[44] | 2014 | China | URBMI (Voluntary) | + | 2 | Low |
| Cheng et al[45] | 2015 | China | NCMS (Voluntary) | + | 2 | Low |
| Liao, Gilmour, and Shibuya[46] |
2016 | China | All public insurance | + | 1 | Low |
| Trujillo et al[47] | 2010 | Colombia | Voluntary and subsidised scheme | + | 2 | Low |
| Hassan et al[48] | 2013 | Colombia | Subsidised scheme | + | 1 | Low |
| Miller et al[49] | 2013 | Colombia | Subsidised scheme | + | 3 | Low |
| Hou and Chao[50] | 2011 | Georgia | MIP (Subsidised scheme) | + | 3 | Low |
| Zoidze et al[51] | 2013 | Georgia | MIP (Subsidised scheme) | 0 | 1 | Low |
| Gotsadze et al[52] | 2015 | Georgia | MIP (Subsidised scheme) | 0 | 1 | Low |
| Blanchet et al[53] | 2012 | Ghana | NHIS (Voluntary scheme) | + | 1 | Low |
| Yilma et al[54] | 2012 | Ghana | NHIS (Voluntary scheme) | + | 3 | Low |
| Abrokwah et al[55] | 2014 | Ghana | NHIS (Voluntary scheme) | + | 1 | Low |
| Brugiavini and Pace[56] | 2015 | Ghana | NHIS (Voluntary scheme) | + | 2 | Low |
| Fenny et al[57] | 2015 | Ghana | NHIS (Voluntary scheme) | + | 1 | Low |
| Sheth[37] | 2014 | India (Maharashtra) | CBHI | - | 3 | Low |
| Sood et al[58] | 2014 | India (Karnataka) | Subsidised scheme | 0 | 2 | Low |
| Raza et al[36] | 2016 | India (Uttar Pradesh and Bihar) | CBHI | 0 | 3 | Moderate |
| Sparrow et al[59] | 2013 | Indonesia | JKN (Voluntary and subsidised) | + | 2 | Low |
| Alkenrack and Lindelow[60] | 2015 | Lao PDR | CBHI | + | 2 | Low |
| Rivera-Hernandez et al[61] | 2016 | Mexico | Seguro Popular (Voluntary scheme) | 0 | 2 | Low |
| Bernal et al[62] | 2014 | Peru | SIS (Subsidised scheme) | + | 3 | Low |
| Dhillon et al[63] | 2012 | Rwanda (Mayange, Mwogo and Mareba) | CBHI | + | 1 | Low |
| Lu et al[64] | 2012 | Rwanda (all rural area) | CBHI | + | 2 | Low |
| Panpiemras et al[65] | 2011 | Thailand | UCS (subsidised scheme) | + | 1 | Low |
| Ghislandi, Manachotphong, and Perego[66] |
2015 | Thailand | UCS (subsidised scheme) | + | 2 | Low |
| Limwattananon et al[67] | 2015 | Thailand | UCS (subsidised scheme) | + | 2 | Low |
| Makhloufi et al[68] | 2015 | Tunisia | MHI (Contributory) and MAS (Subsidised) | + | 1 | Low |
| Nguyen[69] | 2012 | Vietnam | All public insurance | + | 3 | Low |
| Nguyen and Wang[70] | 2013 | Vietnam | Subsidised scheme for children | + | 2 | Low |
| Guindon[71] | 2014 | Vietnam | Subsidised scheme | + | 2 | Low |
| Nguyen[72] | 2014 | Vietnam | Contributory (compulsory and voluntary) scheme | + | 1 | Low |
| Palmer et al[73] | 2015 | Vietnam | Subsidised scheme for children | + | 3 | Low |
| Nguyen[74] | 2016 | Vietnam | Voluntary and subsidised scheme (children) | + | 2 | Low |
* SHI = Social Health Insurance; CBHI = Community-based Health Insurance
** Queens score: 1 = high risk of bias; 2 = moderate risk; 3 = low risk
† Grade score: Low = low quality; Moderate = moderate quality; High = high quality
Evidence on utilisation of curative care generally suggested a positive effect, with 30 out of 38 studies reporting a statistically significant positive effect.
Evidence on preventive care is less clear with 4 out of 7 studies reporting a positive effect, two studies finding a negative effect and one study reporting no effect.
Among the higher quality studies, i.e. those that suitably controlled for selection bias reflected by moderate or low GRADE score and low risk of bias (score = 3) on QuEENS, seven studies reported a positive relationship between insurance and utilisation. One study[36] reported no statistically significant effect, and another study found a statistically significant negative effect.[37]
Financial protection
Overall, evidence on the impact of health insurance on financial protection is less clear than that for utilisation (see Table 3). 34 of the 46 studies reported the impact of health insurance on the level of out-of-pocket health expenditure. Among those 34 studies, 17 found a positive effect (i.e. a reduction in out-of-pocket expenditure), 15 studies found no statistically significant effect, and two studies–from Indonesia[59] and Peru[62]–reported a negative effect (i.e. an increase in out-of-pocket expenditure).
Table 3. Summary of studies reporting financial protection outcome (N = 46).
| Study | Year | Country | Insurance* | Cost sharing | Effect | QUEENS** | GRADE† |
|---|---|---|---|---|---|---|---|
| Parmar et al[81] | 2012 | Burkina Faso, Nouna district | CBHI | Yes | + | 2 | Low |
| Fink et al[75] | 2013 | Burkina Faso, Nouna district | CBHI | Yes | + | 3 | Moderate |
| Levine, Polimeni, and Ramage[39] | 2016 | Cambodia | CBHI | No | + | 3 | Moderate |
| Babiarz et al[40] | 2010 | China | NCMS (Voluntary) | Yes | + | 2 | Low |
| Lu, Liu, and Shen[41] | 2012 | China | NCMS (Voluntary) | Yes | 0 | 2 | Low |
| Cheung and Padieu[80] | 2013 | China | NCMS (Voluntary) | Yes | + | 2 | Low |
| Jing et al[82] | 2013 | China | NCMS (Voluntary) | Yes | 0 | 1 | Low |
| Bai and Wu[79] | 2014 | China | NCMS (Voluntary) | Yes | + | 3 | Low |
| Hou et al[43] | 2014 | China | NCMS (Voluntary) | Yes | 0 | 2 | Low |
| Liu and Zhao[44] | 2014 | China | URBMI (Voluntary) | Yes | 0 | 2 | Low |
| Liu, Wu, and Liu[83] | 2014 | China | All public insurance | Yes | 0 | 1 | Low |
| Yuan et al[84] | 2014 | China | All public insurance | Yes | 0 | 2 | Low |
| Atella, Brugiavini, and Pace[85] | 2015 | China | All public insurance | Yes | + | 1 | Low |
| Cheng et al[86] | 2015 | China | NCMS (Voluntary) | Yes | 0 | 2 | Low |
| Jung and Streeter[87] | 2015 | China | All public insurance | Yes | + | 2 | Low |
| Yang and Wu[88] | 2015 | China | NCMS | Yes | 0 | 2 | Low |
| Camacho and Conover[89] | 2013 | Colombia | Subsidised scheme | No | 0 | 3 | Low |
| Miller et al[49] | 2013 | Colombia | Subsidised scheme | No | 0 | 3 | Low |
| Yilma et al[90] | 2015 | Ethiopia | CBHI | Yes | + | 1 | Low |
| Zoidze et al[51] | 2013 | Georgia | MIP (Subsidised scheme) | Yes | - | 1 | Low |
| Gotsadze et al[52] | 2015 | Georgia | MIP (Subsidised scheme) | Yes | 0 | 1 | Low |
| Abrokwah et al[55] | 2014 | Ghana | NHIS (Voluntary scheme) | Yes | + | 1 | Low |
| Brugiavini and Pace[56] | 2015 | Ghana | NHIS (Voluntary scheme) | Yes | 0 | 2 | Low |
| Aryeetey et al[78] | 2016 | Ghana | NHIS (Voluntary scheme) | Yes | + | 2 | Low |
| Fan et al[77] | 2012 | India (Andrha Pradesh) | Subsidised scheme | No | + | 3 | Low |
| Sheth[37] | 2014 | India (Maharashtra) | CBHI | Yes | + | 3 | Low |
| Sood et al[58] | 2014 | India (Karnataka) | Subsidised scheme | No | + | 2 | Low |
| Raza et al[36] | 2016 | India (Uttar Pradesh and Bihar) | CBHI | Yes | 0 | 3 | Moderate |
| Aji et al[91] | 2013 | Indonesia | Askeskin (Subsidised scheme) | No | + | 2 | Low |
| Sparrow et al[59] | 2013 | Indonesia | Askeskin (Subsidised scheme) | No | - | 2 | Low |
| Alkenbrack and Lindelow[60] | 2015 | Lao | CBHI | Yes | 0 | 2 | Low |
| Galarraga et al[92] | 2010 | Mexico | Seguro Popular (Voluntary scheme) | Yes | + | 2 | Low |
| Sosa-Rubi, Salinas-Rodriguez, and Galarraga[93] | 2011 | Mexico | Seguro Popular (Voluntary scheme) | Yes | + | 2 | Low |
| Wirtz et al[94] | 2012 | Mexico | Seguro Popular (Voluntary scheme) | Yes | + | 2 | Low |
| Avilla-Burgos et al[95] | 2013 | Mexico | Seguro Popular (Voluntary scheme) | Yes | + | 1 | Low |
| Grogger et al[76] | 2015 | Mexico | All public insurance | Yes | + | 3 | Moderate |
| Bernal et al[62] | 2014 | Peru | SIS (Subsidised scheme) | No | - | 3 | Low |
| Lu et al[64] | 2012 | Rwanda | CBHI | Yes | + | 2 | Low |
| Koch and Alaba[96] | 2010 | South Africa | Contributory scheme | yes | - | 1 | Low |
| Limwattananon et al[67] | 2015 | Thailand | UCS (subsidised scheme) | No | + | 2 | Low |
| Makhloufi et al[68] | 2015 | Tunisia | MHI (Contributory) and MAS (Subsidised) | Yes | 0 | 1 | Low |
| Sepehri et al[97] | 2011 | Vietnam | Contributory, voluntary, and subsidised schemes | No | + | 2 | Low |
| Nguyen[69] | 2012 | Vietnam | All public insurance | Yes | 0 | 3 | Low |
| Nguyen and Wang[70] | 2013 | Vietnam | Subsidised scheme for children | No | + | 2 | Low |
| Palmer et al[73] | 2015 | Vietnam | Subsidised scheme for children | No | 0 | 3 | Low |
| Nguyen[74] | 2016 | Vietnam | Voluntary and subsidised scheme (children) | No | + | 2 | Low |
* SHI = Social Health Insurance; CBHI = Community-based Health Insurance
** Queens score: 1 = high risk; 2 = moderate risk; 3 = low risk
† Grade score: Low = low quality; Moderate = moderate quality; High = high quality
Another financial protection measure is the probability of incurring catastrophic health expenditure defined as OOP exceeding a certain threshold percentage of total expenditure or income. Of the 14 studies reporting this measure, nine reported reduction in the risk of catastrophic expenditure, three found no statistically significant difference, and two found a negative effect of health insurance. Only four studies reported sensitivity analysis varying changes in the threshold level,[59,62,75,76] though this did not materially affect the findings.
Two studies used a different measure of financial protection, the probability of impoverishment due to catastrophic health expenditure, reporting conflicting findings.[77,78] Finally, four studies evaluated the effect on financial protection by assessing the impact of insurance on non-healthcare consumption or saving behaviour, such as non-medical related consumption[79], probability of financing medical bills via asset sales or borrowing[40], and household saving[80]. No clear pattern can be observed from those four studies.
Health status
Improving health is one of the main objectives of health insurance, yet very few studies thus far have attempted to evaluate health outcomes. We identified 12 studies, with considerable variation in the precise health measure considered (see Table 4). There was some evidence of positive impact on health status: nine studies found a positive effect, one study reported a negative effect, and two studies reported no effect.
Table 4. Summary of studies reporting health status (N = 12).
| Study | Year | Country | Insurance* | Effect | QUEENS** | GRADE† | Chosen outcomes |
|---|---|---|---|---|---|---|---|
| Fink et al[75] | 2013 | Burkina Faso, Nouna district | CBHI | - | 3 | Moderate | Child and adult mortality |
| Levine, Polimeni, and Ramage[39] | 2016 | Cambodia | CBHI | + | 3 | Moderate | Health index |
| Chen and Jin[98] | 2012 | China | NCMS (Voluntary) | 0 | 2 | Low | Child and maternal mortality |
| Cheng et al[45] | 2015 | China | NCMS (Voluntary) | 0 | 2 | Low | Adult mortality |
| Peng and Conley[99] | 2015 | China | NCMS (Voluntary) | + | 2 | Low | Malnutrition and food consumption |
| Camacho and Conover[89] | 2013 | Colombia | Subsidised scheme | + | 3 | Low | Low birth weight and newborn health status |
| Miller et al[49] | 2013 | Colombia | Subsidised scheme | + | 3 | Low | Acute illness |
| Sood et al[58] | 2014 | India (Karnataka) | Subsidised scheme | + | 2 | Low | Adult mortality |
| Pfutze[100] | 2014 | Mexico | Seguro Popular (Voluntary scheme) | + | 2 | Low | Child mortality |
| Pfutze[101] | 2015 | Mexico | Seguro Popular (Voluntary scheme) | + | 1 | Low | Miscarriages prevalence |
| Hendriks et al[102] | 2014 | Nigeria | CBHI | + | 1 | Low | Blood pressure |
| Quimbo et al[103] | 2011 | Philippines | PhilHealth (Voluntary scheme) | + | 3 | Moderate | CRP-positive level and wasting |
* SHI = Social Health Insurance; CBHI = Community-based Health Insurance
** Queens score: 1 = high risk; 2 = moderate risk; 3 = low risk
† Grade score: Low = low quality; Moderate = moderate quality; High = high quality
Type of insurance and countries
Considering the heterogeneity of insurance schemes among different countries, we attempted to explore the aggregate results by the type of insurance scheme and by country. Table 5 provides a summary of results classified by three type of insurance scheme: community-based health insurance, voluntary health insurance (non-CBHI), and compulsory health insurance. This division is based on the mode of participation (compulsory vs voluntary), which may affect the presence of adverse selection and moral hazard. Premiums are typically community-rated in CBHI, risk-rated in voluntary schemes and income-rated in compulsory schemes.
Table 5. Summary of results based on type of insurance, only 18 studies with high quality and low risk of bias.
| Country and type of insurance scheme | Summary |
|---|---|
| Community-based health insurance/CBHI (N = 5 studies) | Overall: positive effect on utilisation but two studies from India shows no positive effect. Positive effect on financial protection but not in India. Contentious effect on health status |
| 1. Burkina Faso | Positive effect on utilisation [38], reduced catastrophic health expenditure events, but negative effect on elderly’s health, ≥ 65 years old.[75] No effect among adults < 65 years old and children.[75] |
| 2. Cambodia | Positive effect on utilisation, reduced OOP health expenditure, but no effect on health status [39] |
| 3. India | Reduced consumption of health care but the author argued it could be that the enrolees were becoming healthier reducing their need to seek care.[37] Another paper shows no effect on utilisation and OOP health expenditure [36] |
| Voluntary health insurance, non-CBHI (N = 7 studies) | Overall: positive effect on utilisation. Inconclusive on financial protection, but there is an indication it is affected by rurality and proximity to adequately-staffed health facilities. Positive effect on specific health status, but not mortality rate. |
| 1. Ghana | Positive effect on utilisation [54] |
| 2. Vietnam | Positive effect on utilisation but no effect on OOP health expenditure [69] |
| 3. Mexico | Reduced health expenditure among enrolees living in rural area and proximate to large health facilities. Similar effect among the enrolees living in urban area [76] |
| 4. Philippines | Positive effect on health status measured by wasting and C-reactive protein level [103] |
| 5. China | Positive effect on utilisation among the elderly enrolees (>65 years old) [45]; no effect on OOP health expenditure [45] but reduced non-medical consumption among the enrolees[79]; No effect on mortality rate [45,98] |
| Compulsory health insurance, non-CBHI (N = 6 studies) |
Overall: positive effect on utilisation. Inconclusive evidence on financial protection, positive effect on specific health status. |
| 1. India | Reduced OOP health expenditure for inpatient care [77] |
| 2. Vietnam | Positive effect on utilisation but not on OOP health expenditure [73] |
| 3. Georgia | Positive effect on utilisation [50] |
| 4. Peru | Positive effect on utilisation of preventive and curative care, but negative effect on OOP health expenditure [62] |
| 5. Colombia | Positive effect on utilisation and reduced OOP health expenditure [49]Positive effect on newborn health measured by incidence of low birth weight and several indicators of preterm baby [89] |
In principle, CBHI is also considered a voluntary scheme, but we separated it to explore whether the larger size of pooling from non-CBHI schemes may affect the outcomes. Social health insurance is theoretically a mandatory scheme that requires contribution from the enrolees. However, in the context of LMICs, the mandatory element is hard to enforce, and in practice the scheme adopts a voluntary enrolment. Additionally, the government may also want to subsidise the premium for poor people. Therefore, in this review SHI schemes can fall into either the voluntary health insurance (non-CBHI) or compulsory health insurance (non-CBHI), depending on the target population defined in the evaluation study. Lastly, we chose studies with high quality/low risk only to provide more robust results.
Based on the summary in Table 5, the effect on utilisation overall does not differ based on type of insurance, with most evidence suggesting an overall increase in utilisation by the insured. The two studies showing no effect or reduced consumption of care were conducted in two different areas of India, which may–somewhat tentatively–suggest a common factor unique to India’s health system that may compromise the effectiveness of health insurance in increasing utilisation.
Regarding financial protection, the evidence for both CBHI and non-CBHI voluntary health insurance is inconclusive. Furthermore, there is an indication of heterogeneity by supply side factors captured by proximity to health facilities. Evidence from studies exploring subsidised schemes suggests no effect on financial protection, even a negative effect among the insured in Peru.
Lastly, evidence for health status may be influenced by how health outcomes are measured. Studies exploring specific health status, (examples included health indexes, wasting, C-reactive protein, and low birth weight), show a positive effect, whereas studies using mortality rates tends to show no effect or even negative effects. Studies exploring CBHI scheme did not find any evidence of positive effect on health status, as measured either by mortality rate or specific health status.
Discussion
This review synthesises the recent, burgeoning empirical literature on the impact of health insurance in LMICs. We identified a total of 68 eligible studies over a period of six years–double the amount identified by the previous review by Acharya et al. over an approximately 60-year time horizon (1950—July 2010). We used two quality assessment checklists to scrutinise the study methodology, taking more explicit account of the methodological robustness of non-experimental designs.
Programme evaluation has been of interest to many researchers for reporting on the effectiveness of a public policy to policymakers. In theory, the gold standard for a programme evaluation is the randomised control trial, in which the treatment is randomly assigned to the participants. The treatment assignment process has to be exogenous to ensure that any observed effect between the treated and control groups can only be caused by the difference in the treatment assignment. Unfortunately, this ideal scenario is often not feasible in a public policy setting. Our findings showed that only three papers between 2010 and 2016 were able to conduct a randomised study to evaluate the impact of health insurance programmes in developing countries, particularly CBHI [38,75,103]. Policymakers may believe in the value of an intervention regardless of its actual evidence base, or they may believe that the intervention is beneficial and that no one in need should be denied it. In addition, policymakers are inclined to demonstrate the effectiveness of an intervention that they want implemented in the most promising contexts, as opposed to random allocation [104].
Consequently, programme evaluators often have to deal with a non-randomised treatment assignment which may result in selection bias problems. Selection bias is defined as a spurious relationship between the treatment and the outcome of interest due to the systematic differences between the treated and the control groups [105]. In the case of health insurance, an individual who chooses to enrol in the scheme may have different characteristics to an individual who chooses not to enrol. When those important characteristics are unobservable, the analyst needs to apply more advanced techniques and, sometimes, stronger assumptions. Based on our findings, we noted several popular methods, including propensity score matching (N = 8), difference-in-difference (N = 10), fixed or random effects of panel data (N = 6), instrumental variables (N = 12) and regression discontinuity (N = 6). Those methods have varying degree of success in controlling the unobserved selection bias and analysts should explore the robustness of their findings by comparing initial findings with other methods by testing important assumptions. We noted some papers combining two common methods, such as difference-in-difference with propensity score matching (N = 10) and fixed effects with instrumental variables (N = 8), in order to obtain more robust results.
Overall effect
Compared with the earlier review, our study has found stronger and more consistent evidence of positive effects of health insurance on health care utilisation, but less clear evidence on financial protection. Restricting the evidence base to the small subset of randomised studies, the effects on financial protection appear more consistently positive, i.e. three cluster randomised studies[39,75,76] showed a decline in OOP expenditure and one randomised study[36] found no significant effect.
Besides the impact on utilisation and financial protection, this review identified a number of good quality studies measuring the impact of health insurance on health outcomes. Twelve studies were identified (i.e. twice as many as those published before 2010), nine of which showed a beneficial health effect. This holds for the subset of papers with stronger methodology for tackling selection bias.[39,49,89,103] In cases where a health insurance programme does not have a positive effect on either utilisation, financial protection, and health status, it is particularly important to understand the underlying reasons.
Possible explanation of heterogeneity
Payment system
Heterogeneity of the impact of health insurance may be explained by differences in health systems and/or health insurance programmes. Robyn et al. (2012) and Fink et al (2013) argued that the lack of significant effect of insurance in Burkina Faso may have been partially influenced by the capitation payment system. As the health workers relied heavily on user fees for their income, the change of payment system from fee-for-services to capitation may have discouraged provision of high quality services. If enrolees perceive the quality of contracted providers as bad, they might delay seeking treatment, which in turn could impact negatively on health.
Several studies from China found the utilisation of expensive treatment and higher-level health care facilities to have increased following the introduction of the insurance scheme.[41,44,45,88] A fee-for-service payment system may have incentivised providers to include more expensive treatments.[43,83,88] Recent systematic reviews suggested that payment systems might play a key role in determining the success of insurance schemes,[23,106] but this evidence is still weak, as most of the included studies were observational studies that did not control sufficiently for selection bias.
Uncovered essential items
Sood et al. (2014) found no statistically significant effect of community-based health insurance on utilisation in India. They argued that this could be caused by their inability to specify the medical conditions covered by the insurance, causing dilution of a potential true effect. In other countries, transportation costs[69] and treatments that were not covered by the insurance[59,60] may explain the absence of a reduction in out-of-pocket health expenditures.
Methodological differences
Two studies in Georgia evaluated the same programme but with different conclusions.[50,51] This discrepancy may be explained by the difference in the estimated treatment effect: one used average treatment effect (ATE), finding no effect, and another used average treatment effect on the treated (ATT), reporting a positive effect. ATE is of prime interest when policymakers are interested in scaling up the programme, whereas ATT is useful to measure the effect on people who were actually exposed to insurance.[107]
Duration of health insurance
We also found that the longer an insurance programme has been in place prior to the timing of the evaluation, the higher the odds of improved health outcomes. It is plausible that health insurance would not change the health status of population instantly upon implementation.[21] While there may be an appetite among policymakers to obtain favourable short term assessments, it is important to compare the impact over time, where feasible.
Moral hazard
Acharya et al (2012) raised an important question about the possibility of a moral hazard effect as an unintended consequence of introducing (or expanding) health insurance in LMICs. We found seven studies exploring ex-ante moral hazard by estimating the effect on preventive care. If uninsured individuals expect to be covered in the future, they may reduce the consumption of preventive care or invest less in healthy behaviours.[108,109] Current overall evidence cannot suggest a definite conclusion considering the heterogeneity in chosen outcomes. One study found that the use of a self-treated bed nets to prevent malaria declined among the insured group in Ghana[54] while two studies reported an increase in vaccination rates[62] and the number of prenatal care visits[55,62]among the insured group. Another study reported no evidence that health insurance encouraged unhealthy behaviour or reduction of preventive efforts in Thailand.[66]
Two studies from Colombia found that the insured group is more likely to increase their demand for preventive treatment.[47,49] As preventive treatment is free for all, both authors attributed this increased demand to the scheme’s capitation system, incentivising providers to promote preventive care to avoid future costly treatments.[110] Another study of a different health insurance programme in Colombia found an opposite effect.[48]
Study limitations
This review includes a large variety of study designs and indicators for assessing the multiple potential impacts of health insurance, making it hard to directly compare and aggregate findings. For those studies that used a control group, the use of self-selected controls in many cases creates potential bias. Studies of the effect of CBHI are often better at establishing the counterfactual by allowing the use of randomisation in a small area, whereas government schemes or social health insurance covering larger populations have limited opportunity to use randomisation. Non-randomised studies are more susceptible to confounding factors unobserved by the analysts. For a better understanding of the links between health insurance and relevant outcomes, there is also a need to go beyond quantitative evidence alone and combine the quantitative findings with qualitative insights. This is particularly important when trying to interpret some of the counterintuitive results encountered in some studies.
Conclusion
The impact of different health insurance schemes in many countries on utilisation generally shows a positive effect. This is aligned with the supply-demand theory in whichhealth insurance decreases the price of health care services resulting in increased demand. It is difficult to draw an overall conclusion about the impact of health insurance on financial protection, most likely because of differences in health insurance programmes. The impact of health insurance on health status suggests a promising positive effect, but more studies from different countries is required.
The interest in achieving UHC via publicly funded health insurance is likely to increase even further in the coming years, and it is one of the United Nation’s Sustainable Development Goals (SDGs) for 2030[111]. As public health insurance is still being widely implemented in many LMICs, the findings from this review should be of interest to health experts and policy-makers at the national and the international level.
Supporting information
(DOCX)
(DOCX)
(DOCX)
Data Availability
The search strategy for this review is available in Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.UN Economic and Social Council. Progress towards the Sustainable Development Goals: Report of the Secretary-General. Geneva; 2016. [Google Scholar]
- 2.Marten R, Mcintyre D, Travassos C, Shishkin S, Longde W, Reddy S, et al. An assessment of progress towards universal health coverage in Brazil, Russia, India, China, and South Africa (BRICS). Lancet. 2014;384: 2164–2171. 10.1016/S0140-6736(14)60075-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Savedoff WD, Savedoff WD, De Ferranti D, Smith AL, Fan V. Universal Health Coverage 2 Political and economic aspects of the transition to universal health coverage. Lancet. 2012;380: 924–932. 10.1016/S0140-6736(12)61083-6 [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Research for universal health coverage: World health report 2013. WHO. Geneva: World Health Organization; 2014. [Google Scholar]
- 5.World Health Organization. The world health report 2010 Health systems financing: the path to universal coverage. World Health Organization; 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stevens P. Diseases of poverty and the 10/90 Gap. London; 2004. [Google Scholar]
- 7.ILO. Social Health Protection. An ILO strategy towards universal access to health care. Geneva; 2008. [Google Scholar]
- 8.Kankeu HT, Saksena P, Xu K, Evans DB. The financial burden from non-communicable diseases in low- and middle-income countries: a literature review. Heal Res Policy Syst. BioMed Central; 2013;11: 31 10.1186/1478-4505-11-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maeda A, Araujo E, Cashin C, Harris J, Ikegami N, Reich MR. Universal Health Coverage for Inclusive and Sustainable Development: A Synthesis of 11 Country Case Studies. The World Bank; 2014. 10.1596/978-1-4648-0297-3 [DOI] [Google Scholar]
- 10.Jowett M, Kutzin J. Raising revenues for health in support of UHC: strategic issues for policy makers. world Health Organization. Geneva; 2015. Report No.: 1. 10.1080/13545701.2015.1088658 [DOI]
- 11.Kutzin J. Anything goes on the path to universal coverage? No. Bull World Health Organ. World Health Organization; 2012;90: 867–868. 10.2471/BLT.12.113654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang H, Switlick K, Ortiz C, Zurita B, Connor C. Health Insurance Handbook. The World Bank; 2011. 10.1596/978-0-8213-8982-9 [DOI] [Google Scholar]
- 13.Robyn PJ, et al. Econometric Analysis to Evaluate the Effect of Community-Based Health Insurance on Reducing Informal Self-Care in Burkina Faso. Health Policy Plan. 2012;27: 156–165. 10.1093/heapol/czr019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jütting JP. Do community-based health insurance schemes improve poor people’s access to health care? Evidence from rural senegal. World Dev. 2004;32: 273–288. 10.1016/j.worlddev.2003.10.001 [DOI] [Google Scholar]
- 15.Saksena ଝ Priyanka, Antunes AF, Xu K, Musango L, Carrin G. Mutual health insurance in Rwanda: Evidence on access to care and financial risk protection. Health Policy (New York). 2010;99: 203–209. 10.1016/j.healthpol.2010.09.009 [DOI] [PubMed] [Google Scholar]
- 16.Wang H, Yip W, Zhang L, Wang L, Hsiao W. Community-based health insurance in poor rural China: the distribution of net benefits. Health Policy Plan. Oxford University Press; 2005;20: 366–374. 10.1093/heapol/czi045 [DOI] [PubMed] [Google Scholar]
- 17.Devadasan N, Kent R, Van Damme K, Criel B. Community Health Insurance in India: An Overview. Econ Polit Wkly. Economic and Political Weekly; 2004;39: 3179–3183. 10.2307/4415264 [DOI] [Google Scholar]
- 18.Carrin G, Waelkens M-P, Criel B. Community-based health insurance in developing countries: a study of its contribution to the performance of health financing systems. Trop Med Int Heal. Blackwell Science Ltd; 2005;10: 799–811. 10.1111/j.1365-3156.2005.01455.x [DOI] [PubMed] [Google Scholar]
- 19.Comfort AB, Peterson LA, Hatt LE. Effect of health insurance on the use and provision of maternal health services and maternal and neonatal health outcomes: a systematic review. J Heal Popul Nutr. BioMed Central; 2013;31: 81–105 25p. 10.3329/jhpn.v31i4.2361 [DOI] [PubMed] [Google Scholar]
- 20.Ekman B. Community-based health insurance in low-income countries: a systematic review of the evidence. Health Policy Plan. Lund University Centre for Health Economics (LUCHE), Lund University, Lund, Sweden. bjorn.ekman@luche.lu.se: Oxford University Press / USA; 2004;19: 249–270. 10.1093/heapol/czh031 [DOI] [PubMed] [Google Scholar]
- 21.Giedion U, Alfonso EA, Díaz Y, Andrés Alfonso E, Díaz Y. The Impact of Universal Coverage Schemes in the Developing World: A Review of the Existing Evidence. Univers Heal Cover Stud Ser (UNICO), No 25; Washington DC: World; 2013; [Google Scholar]
- 22.Habib SS, Perveen S, Maqbool H, Khuwaja A. The role of micro health insurance in providing financial risk protection in developing countries-a systematic review. BMC Public Health. 2016;16 10.1186/s12889-016-2937-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Robyn PJ, Sauerborn R, Bärnighausen T, Barnighausen T, Bärnighausen T. Provider payment in community-based health insurance schemes in developing countries: a systematic review. Heal Policy Plan. Institute of Public Health, University of Heidelberg, Im Neuenheimer Feld 324, 69120 Heidelberg, Germany. E-mail: jakerobyn@gmail.com: Oxford University Press / USA; 2013;28: 111–122. doi: heapol/czs034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Spaan E, Mathijssen J, Tromp N, McBain F, ten Have A, Baltussen R, et al. The impact of health insurance in Africa and Asia: a systematic review. Bull World Health Organ. Department of Primary and Community Care, Radboud University Nijmegen Medical Centre, PO Box 9101, 6500HB Nijmegen, Netherlands: World Health Organization; 2012;90: 685–692 8p. 10.2471/BLT.12.102301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liang X, Guo H, Jin C, Peng X, Zhang X. The Effect of New Cooperative Medical Scheme on Health Outcomes and Alleviating Catastrophic Health Expenditure in China: A Systematic Review. Baradaran HR, editor. PLoS One. Public Library of Science; 2012;7: e40850 10.1371/journal.pone.0040850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu BB, Gong X, Chu J, Gao J, Gong X, Chu J, et al. Study on the role of financial risk pooling of different health security mechanisms in low and middle income counties [Chinese]. Chinese J Evidence-Based Med. 2008;8: 833–841. [Google Scholar]
- 27.Acharya A, Vellakkal S, Taylor F, Masset E, Satija A, Burke M, et al. The Impact of Health Insurance Schemes for the Informal Sector in Low- and Middle-Income Countries: A Systematic Review. World Bank Res Obs. Oxford University Press; 2013;28: 236–266. 10.1093/wbro/lks009 [DOI] [Google Scholar]
- 28.Cameron DB, Mishra A, Brown AN. The growth of impact evaluation for international development: how much have we learned? J Dev Eff. Routledge; 2016;8: 1–21. 10.1080/19439342.2015.1034156 [DOI] [Google Scholar]
- 29.Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. Public Library of Science; 2009;6: e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Bank. World Bank countries and lending groups (Database) [Internet]. 2016. [cited 1 Sep 2016]. Available: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. [Google Scholar]
- 31.A System of Health Accounts 2011. OECD; 2017. 10.1787/9789264270985-en [DOI] [Google Scholar]
- 32.Craig P, Cooper C, Gunnell D, Haw S, Lawson K, Macintyre S, et al. Using natural experiments to evaluate population health interventions: new Medical Research Council guidance. J Epidemiol Community Health. BMJ Publishing Group Ltd; 2012;66: 1182–6. 10.1136/jech-2011-200375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schünemann HJ, et al. What is "quality of evidence" and why is it important to clinicians? BMJ. British Medical Journal Publishing Group; 2008;336: 995–8. 10.1136/bmj.39490.551019.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cochrane. Cochrane handbook for systematic reviews of interventions. Higgins JPT, Green SE, editors. Wiley-Blackwell; 2008. [Google Scholar]
- 35.Faria R, Hernandez Alava M, Manca A, Wailoo AJ, Uk W, @nice_Dsu T, et al. NICE DSU technical support document 17: the use of observational data to inform estimates of treatment effectiveness in technology appraisal. Sheffield, UK; 2015. [Google Scholar]
- 36.Raza WA, van de Poel E, Bedi A, Rutten F. Impact of Community-Based Health Insurance on Access and Financial Protection: Evidence from Three Randomized Control Trials in Rural India. Health Econ. 2016;25: 675–687. 10.1002/hec.3307 [DOI] [PubMed] [Google Scholar]
- 37.Sheth K. Evaluating Health-Seeking Behavior, Utilization of Care, and Health Risk: Evidence from a Community Based Insurance Model in India. 2014. Report No.: 36.
- 38.Robyn PJ, Fink G, Sie A, Sauerborn R. Health insurance and health-seeking behavior: evidence from a randomized community-based insurance rollout in rural Burkina Faso. Soc Sci Med. England: Robyn,Paul Jacob. University of Heidelberg, Institute of Public Health, Germany.; 2012;75: 595–603. 10.1016/j.socscimed.2011.12.018 [DOI] [PubMed] [Google Scholar]
- 39.Levine D, Polimeni R, Ramage I. Insuring Health or Insuring Wealth? An Experimental Evaluation of Health Insurance in Rural Cambodia. J Dev Econ. 2016;119: 1–15. 10.1016/j.jdeveco.2015.10.008 [DOI] [Google Scholar]
- 40.Babiarz KS, Miller G, Yi HM, Zhang LX, Rozelle S. New evidence on the impact of China’s New Rural Cooperative Medical Scheme and its implications for rural primary healthcare: multivariate difference-in-difference analysis. Br Med J. 2010;341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lu C, Liu Y, Shen J. Does China’s Rural Cooperative Medical System Achieve Its Goals? Evidence from the China Health Surveillance Baseline Survey in 2001. Contemp Econ Policy. 2012;30: 93–112. [Google Scholar]
- 42.Chen G, Liu GG, Xu F. The impact of the urban resident basic medical insurance on health services utilisation in China. Pharmacoeconomics. New Zealand: Chen,Gang. Flinders Health Economics Group, A Block, Level 1, Repatriation General Hospital, School of Medicine, Flinders University, Daws Road, Daw Park, SA, 5041, Australia, Gang.Chen@flinders.edu.au; 2014;32: 277–292. 10.1007/s40273-013-0097-7 [DOI] [PubMed] [Google Scholar]
- 43.Hou Z, Van de Poel E, Van Doorslaer E, Yu B, Meng Q. Effects of NCMS on access to care and financial protection in China. Health Econ. England: Hou,Zhiyuan. Center for Health Management and Policy, Shandong University, China.; 2014;23: 917–934. 10.1002/hec.2965 [DOI] [PubMed] [Google Scholar]
- 44.Liu H, Zhao Z. Does Health Insurance Matter? Evidence from China’s Urban Resident Basic Medical Insurance. J Comp Econ. 2014;42: 1007–1020. [Google Scholar]
- 45.Cheng L, Liu H, Zhang Y, Shen K, Zeng Y. The impact of health insurance on health outcomes and spending of the elderly: Evidence from china’s new cooperative medical scheme. Heal Econ (United Kingdom). United Kingdom: John Wiley and Sons Ltd (Southern Gate, Chichester, West Sussex PO19 8SQ, United Kingdom); 2015;24: 672–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liao Y, Gilmour S, Shibuya K. Health insurance coverage and hypertension control in China: Results from the China health and nutrition survey. PLoS One. 2016;11 (3) (no. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Trujillo AJ, Ortiz AIV, GÃ3mez FR, Steinhardt LC. Health Insurance Doesn’t Seem To Discourage Prevention Among Diabetes Patients In Colombia. Health Aff. 2010;29: 2180–2188. 10.1377/hlthaff.2010.0463 [DOI] [PubMed] [Google Scholar]
- 48.Hassan AR, Jimenez JC, Montoya RC. The Impact of Subsidized Health Insurance on the Poor in Colombia: Evaluating the Case of Medellin. Econ Apl J Appl Econ. 2013;17: 543–556. [Google Scholar]
- 49.Miller G, Pinto D, Vera-Hernandez M. Risk Protection, Service Use, and Health Outcomes under Colombia’s Health Insurance Program for the Poor. Am Econ J Appl Econ. 2013;5: 61–91. 10.1257/app.5.4.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hou X, Chao S. Targeted or untargeted? The initial assessment of a targeted health insurance program for the poor in Georgia. Health Policy. Ireland: Hou,Xiaohui. The World Bank Group, 1818 H. St. NW, Washington, DC 20433, United States. xhou@worldbank.org; 2011;102: 278–285. 10.1016/j.healthpol.2011.06.006 [DOI] [PubMed] [Google Scholar]
- 51.Zoidze A, Rukhazde N, Chkhatarashvili K, Gotsadze G. Promoting universal financial protection: Health insurance for the poor in Georgia—a case study. Heal Res Policy Syst. United Kingdom: BioMed Central Ltd. (Floor 6, 236 Gray’s Inn Road, London WC1X 8HB, United Kingdom); 2013;11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gotsadze G, Zoidze A, Rukhadze N, Shengelia N, Chkhaidze N. An impact evaluation of medical insurance for poor in Georgia: preliminary results and policy implications. Health Policy Plan. 2015;30: i2–i13. 10.1093/heapol/czu095 [DOI] [PubMed] [Google Scholar]
- 53.Blanchet NJ, Fink G, Osei-Akoto I. The effect of Ghana’s National Health Insurance Scheme on health care utilisation. Ghana Med J. Ghana: Blanchet,N J. Dept. of Global Health and Population, Harvard School of Public Health, Boston, MA, United States. nblanche@hsph.harvard.edu; 2012;46: 76–84. [PMC free article] [PubMed] [Google Scholar]
- 54.Yilma Z, Van Kempen L, De Hoop T. A perverse “net” effect? Health insurance and ex-ante moral hazard in Ghana. Soc Sci Med. 2012;75: 138–147. 10.1016/j.socscimed.2012.02.035 [DOI] [PubMed] [Google Scholar]
- 55.Abrokwah SO, Moser CM, Norton EC. The effect of social health insurance on prenatal care: the case of Ghana. Int J Health Care Finance Econ. United States: Abrokwah,Stephen O. Swiss Reinsurance America Holding Corp, 175 King st, Armonk, NY, USA, stephen_abrokwah@swissre.com; 2014;14: 385–406. 10.1007/s10754-014-9155-8 [DOI] [PubMed] [Google Scholar]
- 56.Brugiavini A, Pace N. Extending health insurance in Ghana: effects of the National Health Insurance Scheme on maternity care. Health Econ Rev. 2015;6: 1–10. 10.1186/s13561-016-0083-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fenny AP, Asante FA, Enemark U, Hansen KS. Treatment-seeking behaviour and social health insurance in Africa: the case of Ghana under the National Health Insurance Scheme. Glob J Health Sci. Canada: Fenny,Ama P. Aarhus University. amafenny@yahoo.co.uk; 2015;7: 296–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sood N, Bendavid E, Mukherji A, Wagner Z, Nagpal S, Mullen P. Government health insurance for people below poverty line in India: quasi-experimental evaluation of insurance and health outcomes. BMJ. England: Sood,Neeraj. Department of Pharmaceutical Economics and Policy, School of Pharmacy, University of Southern California, Los Angeles, CA, USA Leonard D Schaeffer Center for Health Policy and Economics, University of Southern California, Los Angeles, CA, USA; 2014;349: g5114 10.1136/bmj.g5114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sparrow R, Suryahadi A, Widyanti W. Social health insurance for the poor: targeting and impact of Indonesia’s Askeskin programme. Soc Sci Med. England: Sparrow,Robert. Australian National University, Canberra, Australia. Electronic address: mail@robertsparrow.net; 2013;96: 264–271. 10.1016/j.socscimed.2012.09.043 [DOI] [PubMed] [Google Scholar]
- 60.Alkenbrack S, Lindelow M. The impact of community-based health insurance on utilization and out-of-pocket expenditures in lao people’s democratic republic. Heal Econ (United Kingdom). United Kingdom: John Wiley and Sons Ltd (Southern Gate, Chichester, West Sussex PO19 8SQ, United Kingdom); 2015;24: 379–399. [DOI] [PubMed] [Google Scholar]
- 61.Rivera-Hernandez M, Rahman M, Mor V, Galarraga O. The Impact of Social Health Insurance on Diabetes and Hypertension Process Indicators among Older Adults in Mexico. Health Serv Res. 2016;51: 1323–1346. 10.1111/1475-6773.12404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bernal N, Carpio M, Klein T. The Effects of Access to Health Insurance for The Effects of Access to Health Insurance for Informally Employed Individuals in Peru. 2014. [Google Scholar]
- 63.Dhillon RS, Bonds MH, Fraden M, Ndahiro D, Ruxin J. The impact of reducing financial barriers on utilisation of a primary health care facility in Rwanda. Glob Public Health. England: Dhillon,Ranu S. Earth Institute, Columbia University, New York, NY, USA.; 2012;7: 71–86. 10.1080/17441692.2011.593536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lu C, Chin B, Lewandowski JL, Basinga P, Hirschhorn LR, Hill K, et al. Towards universal health coverage: an evaluation of Rwanda Mutuelles in its first eight years. PLoS One. United States: Lu,Chunling. Department of Global Health and Social Medicine, Harvard Medical School, Boston, Massachusetts, USA. Chunling_Lu@hms.harvard.edu; 2012;7: e39282 10.1371/journal.pone.0039282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Panpiemras J, Puttitanun T, Samphantharak K, Thampanishvong K. Impact of Universal Health Care Coverage on patient demand for health care services in Thailand. Health Policy. Ireland: Panpiemras,Jirawat. Thailand Development Research Institute, Bangkok 10310, Thailand.; 2011;103: 228–235. 10.1016/j.healthpol.2011.08.008 [DOI] [PubMed] [Google Scholar]
- 66.Ghislandi S, Manachotphong W, Perego VME. The impact of Universal Health Coverage on health care consumption and risky behaviours: evidence from Thailand. Heal Econ Policy Law. Cambridge University Press; 2015;10: 251–266. 10.1017/S1744133114000334 [DOI] [PubMed] [Google Scholar]
- 67.Limwattananon S, Neelsen S, O’Donnell O, Prakongsai P, Tangcharoensathien V, van Doorslaer E. Universal Coverage with Supply-Side Reform: The Impact on Medical Expenditure Risk and Utilization in Thailand. J Public Econ. 2015;121: 79–94. [Google Scholar]
- 68.Makhloufi K, Ventelou B, Abu-Zaineh M. Have Health Insurance Reforms in Tunisia Attained Their Intended Objectives? Int J Heal Econ Manag. 2015;15: 29–51. [DOI] [PubMed] [Google Scholar]
- 69.Nguyen CV. The impact of voluntary health insurance on health care utilization and out-of-pocket payments: new evidence for Vietnam. Health Econ. England: Nguyen,Cuong Viet. Indochina Research and Consulting, Hanoi, Vietnam. c_nguyenviet@yahoo.com; 2012;21: 946–966. 10.1002/hec.1768 [DOI] [PubMed] [Google Scholar]
- 70.Nguyen H, Wang W. The effects of free government health insurance among small children-evidence from the free care for children under six policy in Vietnam. Int J Health Plann Manage. United Kingdom: John Wiley and Sons Ltd (Southern Gate, Chichester, West Sussex PO19 8SQ, United Kingdom); 2013;28: 3–15. [DOI] [PubMed] [Google Scholar]
- 71.Guindon GE. The impact of health insurance on health services utilization and health outcomes in Vietnam. Health Econ Policy Law. England: Guindon,G Emmanuel. 1Centre for Health Economics and Policy Analysis,McMaster University,Hamilton,ON,Canada.; 2014;9: 359–382. 10.1017/S174413311400005X [DOI] [PubMed] [Google Scholar]
- 72.Nguyen MT. Moral Hazard and Adverse Selection in Health Insurances, Evidence from a Transitional Economy. Singapore Econ Rev. 2014;59: 1–21. [Google Scholar]
- 73.Palmer M, Mitra S, Mont D, Groce N. The impact of health insurance for children under age 6 in Vietnam: A regression discontinuity approach. Soc Sci Med. 2015;145: (10p). 10.1016/j.socscimed.2014.08.012 [DOI] [PubMed] [Google Scholar]
- 74.Nguyen C. The impact of health insurance programs for children: evidence from Vietnam. Health Econ Rev. 2016;6 (1) (no. 10.1186/s13561-016-0111-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fink G, Robyn PJ, Sie A, Sauerborn R. Does health insurance improve health?: Evidence from a randomized community-based insurance rollout in rural Burkina Faso. J Health Econ. Netherlands: Fink,Gunther. Harvard School of Public Health, United States. Electronic address: gfink@hsph.harvard.edu; 2013;32: 1043–1056. 10.1016/j.jhealeco.2013.08.003 [DOI] [PubMed] [Google Scholar]
- 76.Grogger J, Arnold T, Leon AS, Ome A. Heterogeneity in the effect of public health insurance on catastrophic out-of-pocket health expenditures: the case of Mexico. Health Policy Plan. Oxford University Press; 2015;30: 593–599. 10.1093/heapol/czu037 [DOI] [PubMed] [Google Scholar]
- 77.Fan VY, Karan A, Mahal A. State health insurance and out-of-pocket health expenditures in Andhra Pradesh, India. Int J Health Care Finance Econ. United States: Fan,Victoria Y. Center for Global Development, 1800 Massachusetts Ave NW, Third Floor, Washington, DC 20036, USA. vfan@cgdev.org; 2012;12: 189–215. 10.1007/s10754-012-9110-5 [DOI] [PubMed] [Google Scholar]
- 78.Aryeetey GC, Westeneng J, Spaan E, Jehu-Appiah C, Agyepong IA, Baltussen R. Can health insurance protect against out-of-pocket and catastrophic expenditures and also support poverty reduction? Evidence from Ghana’s National Health Insurance Scheme. Int J Equity Health. 2016;15 10.1186/s12939-016-0401-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bai CE, Wu BZ. Health insurance and consumption: Evidence from China’s New Cooperative Medical Scheme. J Comp Econ. 2014;42: 450–469. [Google Scholar]
- 80.Cheung D, Padieu Y. Heterogeneite de l’impact de l’assurance sante sur les comportements d’epargne en Chine rurale. (Heterogeneity of the Impact of Health Insurance on Saving Behaviours in Rural China. With English summary.). Rev Econ Polit. 2013;123: 641–662. [Google Scholar]
- 81.Parmar D, Reinhold S, Souares A, Savadogo G, Sauerborn R. Does community-based health insurance protect household assets? Evidence from rural Africa. Health Serv Res. United States: Parmar,Divya. Institute of Public Health, INF 324, Heidelberg University, Heidelberg, Germany. Parmar@uni-heidelberg.de; 2012;47: 819–839. 10.1111/j.1475-6773.2011.01321.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jing SS, Yin AT, Shi LZ, Liu JN. Whether New Cooperative Medical Schemes Reduce the Economic Burden of Chronic Disease in Rural China. PLoS One. 2013;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Liu K, Wu Q, Liu J. Examining the association between social health insurance participation and patients’ out-of-pocket payments in China: the role of institutional arrangement. Soc Sci Med. England: Liu,Kai. Department of Social Work, The Chinese University of Hong Kong, Shatin, N.T., Hong Kong. Electronic address: kevin-liukai@hotmail.comWu,Qiaobing. Department of Social Work, The Chinese University of Hong Kong, Shatin, N.T., Hong Kong.Liu,Junqi; 2014;113: 95–103. 10.1016/j.socscimed.2014.05.011 [DOI] [PubMed] [Google Scholar]
- 84.Yuan S, Liu Y, Li N, Zhang Y, Zhang Z, Tao J, et al. Impacts of Health Insurance Benefit Design on Percutaneous Coronary Intervention Use and Inpatient Costs among Patients with Acute Myocardial Infarction in Shanghai, China. Pharmacoeconomics. Springer International Publishing; 2014;32: 265–275. 10.1007/s40273-013-0079-9 [DOI] [PubMed] [Google Scholar]
- 85.Atella V, Brugiavini A, Pace N. The health care system reform in China: Effects on out-of-pocket expenses and saving. China Econ Rev. 2015;34: 182–195. 10.1016/j.chieco.2015.02.003 [DOI] [Google Scholar]
- 86.Li C, Yu X, Butler JRG, Yiengprugsawan V, Yu M. Moving towards universal health insurance in China: Performance, issues and lessons from Thailand. Soc Sci Med. Department of Health Services, Fourth Military Medical University, PR China; Australian Centre for Economic Research on Health, Australian National University, Australia: Pergamon Press—An Imprint of Elsevier Science; 2011;73: 359–366 8p. 10.1016/j.socscimed.2011.06.002 [DOI] [PubMed] [Google Scholar]
- 87.Jung J, Streeter JL. Does health insurance decrease health expenditure risk in developing countries? The case of China. South Econ J. 2015;82: 361–384. 10.1002/soej.12101 [DOI] [Google Scholar]
- 88.Yang W, Wu X. Paying for outpatient care in rural China: cost escalation under China’s New Co-operative Medical Scheme. Health Policy Plan. 2015;30: 187–196. 10.1093/heapol/czt111 [DOI] [PubMed] [Google Scholar]
- 89.Camacho A, Conover E. Effects of Subsidized Health Insurance on Newborn Health in a Developing Country. Econ Dev Cult Change. 2013;61: 633–658. [Google Scholar]
- 90.Yilma Z, Mebratie A, Sparrow R, Dekker M, Alemu G, Bedi AS. Impact of Ethiopia’s Community Based Health Insurance on Household Economic Welfare. World Bank Econ Rev. Oxford University Press; 2015;29: S164–S173. 10.1093/wber/lhv009 [DOI] [Google Scholar]
- 91.Aji B, De Allegri M, Souares A, Sauerborn R. The impact of health insurance programs on out-of-pocket expenditures in Indonesia: an increase or a decrease? Int J Environ Res Public Health. Multidisciplinary Digital Publishing Institute; 2013;10: 2995–3013. 10.3390/ijerph10072995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Galarraga O, Sosa-Rubi SG, Salinas-Rodriguez A, Sesma-Vazquez S. Health insurance for the poor: impact on catastrophic and out-of-pocket health expenditures in Mexico. Eur J Health Econ. Germany: Galarraga,Omar. Health Economics Unit, Center for Evaluation and Survey Research, Mexican School of Public Health, National Institute of Public Health (INSP), Av. Universidad 655, Cuernavaca 62508, Mexico.; 2010;11: 437–447. 10.1007/s10198-009-0180-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sosa-Rubi SG, Salinas-Rodriguez A, Galarraga O. Impacto del Seguro Popular en el gasto catastrofico y de bolsillo en el Mexico rural y urbano, 2005–2008. Salud Publica Mex. 2011;53 10.1590/S0036-36342011001000006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wirtz VJ, Santa-Ana-Tellez Y, Servan-Mori E, Avila-Burgos L. Heterogeneous effects of health insurance on out-of-pocket expenditure on medicines in Mexico. Value Health. United States: Wirtz,Veronika J. Center for Health Systems Research, National Institute of Public Health, Cuernavaca, Mexico.; 2012;15: 593–603. 10.1016/j.jval.2012.01.006 [DOI] [PubMed] [Google Scholar]
- 95.Avila-Burgos L, Servan-Mori E, Wirtz VJ, Sosa-Rubi SG, Salinas-Rodriguez A. [Effect of Seguro Popular on health expenditure in Mexican households ten years after its implementation]. Efectos del Seguro Pop sobre el gasto en salud en hogares Mex a diez anos su implementacion. Mexico: Avila-Burgos,Leticia. Centro de investigacion en Sistemas de Salud, Instituto Nacional de Salud Publica, Cuernavaca, Morelos, Mexico.Servan-Mori,Edson. Centro de investigacion en Evaluacion y Encuestas, Instituto Nacional de Salud Publica, Cuernavaca, Mo; 2013;55 Suppl 2: S91–9. [PubMed] [Google Scholar]
- 96.Koch S, Alaba O. On health insurance and household decisions: A treatment effect analysis. Soc Sci Med. 2010;70: 175–182. 10.1016/j.socscimed.2009.10.015 [DOI] [PubMed] [Google Scholar]
- 97.Sepehri A, Sarma S, Oguzoglu U. Does the financial protection of health insurance vary across providers? Vietnam’s experience. Soc Sci Med. England: Sepehri,Ardeshir. University of Manitoba, Winnipeg, Man, Canada R3T 5V5. sepehri@cc.umanitoba.ca; 2011;73: 559–567. 10.1016/j.socscimed.2011.06.009 [DOI] [PubMed] [Google Scholar]
- 98.Chen Y, Jin GZ. Does health insurance coverage lead to better health and educational outcomes? Evidence from rural China. J Health Econ. Netherlands: Chen,Yuyu. Guanghua School of Management, Peking University, China.; 2012;31: 1–14. 10.1016/j.jhealeco.2011.11.001 [DOI] [PubMed] [Google Scholar]
- 99.Peng X, Conley D. The implication of health insurance for child development and maternal nutrition: evidence from China. Eur J Heal Econ. 2016;17: (14p). 10.1007/s10198-015-0696-7 [DOI] [PubMed] [Google Scholar]
- 100.Pfutze T. The Effects of Mexico’s Seguro Popular Health Insurance on Infant Mortality: An Estimation with Selection on the Outcome Variable. World Dev. 2014;59: 475–486. [Google Scholar]
- 101.Pfutze T. Does access to health insurance reduce the risk of miscarriages? Evidence from Mexico’s Seguro popular. Lat Am Econ Rev. 2015;24 10.1007/s40503-015-0022-x [DOI] [Google Scholar]
- 102.Hendriks ME, Wit FWNM, Akande TM, Kramer B, Osagbemi GK, Tanovic Z, et al. Effect of Health Insurance and Facility Quality Improvement on Blood Pressure in Adults With Hypertension in Nigeria. JAMA Intern Med. American Medical Association; 2014;174: 555 10.1001/jamainternmed.2013.14458 [DOI] [PubMed] [Google Scholar]
- 103.Quimbo SA, Peabody JW, Shimkhada R, Florentino J, Solon O. Evidence of a causal link between health outcomes, insurance coverage, and a policy to expand access: experimental data from children in the Philippines. Health Econ. England: Quimbo,Stella A. School of Economics, University of the Philippines, Philippines.; 2011;20: 620–630. 10.1002/hec.1621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Bonell CP, Hargreaves J, Cousens S, Ross D, Hayes R, Petticrew M, et al. Alternatives to randomisation in the evaluation of public health interventions: Design challenges and solutions. J Epidemiol Community Health. 2011;65: 582–587. 10.1136/jech.2008.082602 [DOI] [PubMed] [Google Scholar]
- 105.Wooldridge JM. Introductory Econometrics: A Modern Approach. Fifth Inte Mason, Ohio: South-Western Cengage Learning; 2013. [Google Scholar]
- 106.Eijkenaar F, Emmert M, Scheppach M, Schöffski O. Effects of pay for performance in health care: A systematic review of systematic reviews. Health Policy (New York). 2013;110: 115–130. 10.1016/j.healthpol.2013.01.008 [DOI] [PubMed] [Google Scholar]
- 107.Loi M, Rodrigues M. A note on the impact evaluation of public policies: the counterfactual analysis. Luxembourg; 2012. 10.2788/50327 [DOI] [Google Scholar]
- 108.de Preux LB. Anticipatory ex ante moral hazard and the effect of medicare on prevention. Health Econ. John Wiley & Sons, Ltd.; 2011;20: 1056–1072. 10.1002/hec.1778 [DOI] [PubMed] [Google Scholar]
- 109.Dave D, Kaestner R. Health insurance and ex ante moral hazard: evidence from Medicare. Int J Health Care Finance Econ. Springer US; 2009;9: 367–390. 10.1007/s10754-009-9056-4 [DOI] [PubMed] [Google Scholar]
- 110.Peckham S, Disclaimer KG. GP payment schemes review. 2014. [Google Scholar]
- 111.World Health Organization. World Health Statistics 2016: Monitoring health for the SDGs. WHO. Geneva: World Health Organization; 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
The search strategy for this review is available in Supporting Information files.