Abstract
OBJECTIVE:
First-time offending court-involved, non-incarcerated (i.e., community-supervised) youth have high rates of substance use and psychiatric disorders. However, little is known about their use of psychiatric (i.e., mental health and/or substance use) services nor about factors associated with services use. This study examined the prevalence, determinants, and barriers to psychiatric services use among community-supervised youth.
METHODS:
Data are from a longitudinal study of drug use, HIV/STI risk behavior and psychiatric symptoms among adolescents aged 12–18 years from a Northeastern family court, in which caregivers and youth completed assessments (N=423). The Behavior Assessment System for Children, Second Edition assessed youth’s psychiatric symptoms. The Child and Adolescent Services Assessment assessed services use and barriers to use. Family functioning and caregiver-adolescent communication were assessed using the McMaster Family Assessment Device and the Parent-Adolescent Communication Scale, respectively. Multivariable regression was performed to examine the cross-sectional relationship between community-supervised youth’s services use and determinants of use at baseline.
RESULTS:
Nearly 49% of youth experienced psychiatric symptoms and 36% used psychiatric services. The highest adjusted odds of services use were associated with youth psychiatric symptoms and caregiver history of psychopathology. The lowest odds of services use were associated with caregivers identifying as racial and ethnic minorities. Caregiver-reported barriers to youth’s services use differed according to prior services use and by caregiver race/ethnicity.
CONCLUSIONS:
Study results suggest a need for interventions to increase access to and engagement in psychiatric services for community-supervised youth and the importance of accounting for caregiver factors when designing such interventions.
Introduction
In 2015, an estimated 921,580 U.S. youth ≤18 years old were arrested (1) and more than 31 million were under juvenile court jurisdiction (2). Justice-involved youth suffer from significant health problems compared to non-justice involved youth, including psychiatric disorders (i.e., mental health and substance use disorders) (3–7). Between 50%−70% of justice-involved youth meet DSM–IV–TR diagnostic criteria for ≥1 psychiatric disorder (4, 8), 3 – 4 times higher than rates in general-population samples.
Despite experiencing higher rates of psychiatric disorders, justice-involved youth are less likely to receive treatment compared to general-population samples (9). Approximately 25%−30% of justice-involved youth receive treatment while in detention (10, 11). Even fewer receive treatment after being released (8.0%−16.4%) (10, 12, 13). Untreated disorders increase the likelihood of adverse outcomes including suicidality (14) and continued contact with the justice system (15, 16). Untreated disorders can also prevent justice-involved youth from responding to interventions to decrease criminal behavior (17) or increase risk of engaging in illicit behaviors, such as substance use (18), which in turn increases youths’ propensity for future criminal behavior (19).
These findings highlight the importance of early detection and linkage to psychiatric (including substance use) services for justice-involved youth. Multiple youth-, caregiver-, family-, and system-level factors have been associated with psychiatric services use among detained adolescents (10, 13). Teplin and colleagues found lower rates of mental health services use among juvenile detainees who were racial/ethnic minorities, male, and >14 years of age (10). Rawal and colleagues found that Black justice-involved youth had greater mental health needs, but were less likely to receive mental health treatment than White justice-involved youth (20). Few studies have examined how caregiver factors affect justice-involved youth’s services use, however one study among first-time juvenile offenders reported an association between higher levels of family communication problems and mental health services use (21). In a general sample of adolescents, family poverty, caregiver and family stress, effectiveness of parental discipline, and family cohesion significantly predicted mental health treatment engagement (22).
Little is known about the prevalence and determinants of psychiatric services use among justice-involved youth who are community-supervised. This knowledge is important given that 75% of delinquent juveniles are diverted from detention and supervised in the community (2). Understanding the determinants of psychiatric services use among this subgroup of justice-involved youth, particularly first-time offenders, could inform efforts to ensure identification of mental health needs and linkage to appropriate services at one of the earliest points of justice involvement.
The study purpose was to identify: (1) psychiatric treatment need among first-time offending community-supervised youth, (2) prevalence and determinants of psychiatric services use, and (3) barriers to services use. We hypothesized that youth, caregiver and family factors, such as minority status, greater psychiatric symptoms (of youth and/or caregiver) and worse family functioning would be associated with lower rates of psychiatric service use based on prior studies among justice-involved and general youth populations.
Methods
Data Source and Study Population
This cross-sectional study uses baseline data collected from 2014–2016 as part of Project EPICC (Epidemiological Project Involving Children in the Court), a two-year longitudinal study of 423 community-supervised youth-caregiver dyads. As detailed elsewhere (23) youth-caregiver dyads were recruited from a large, Northeastern juvenile court. The sampling frame included all youth aged 12–18 years with a first-time offense. Girls with a delinquent first-time offense were oversampled to ensure sufficient power to conduct sex-based subgroup analyses.
Caregivers were notified about the study through a letter sent prior to the first court-related appointment. Prospective youth and families were approached in the court by a trained research assistant, and those who expressed interest in participating were screened for eligibility. Eligible youth were between 12 and 18 years of age at the time of initial court contact and had an involved caregiver willing to participate in the study. Following informed consent and assent, youth-caregiver dyads completed baseline assessments via an audio computer-assisted self-interview (ACASI). All participants received a $50 gift card for their participation. Study protocols were approved by the Institutional Review Board at the PI and site PI’s institutions.
Variables
Anderson’s behavioral model of health services utilization guided the selection of factors that are potentially associated with community-supervised youth’s psychiatric services use, the dependent variable in this study (24, 25). Although not specific to justice-involved populations, this model includes the broadest range of individual and systems-level factors potentially associated with health services use. Factors are categorized as either (1) predisposing (e.g., demographics and health beliefs), (2) enabling (e.g., income, insurance coverage, availability of and access to health services) or (3) need-based (e.g., psychiatric symptoms). A recently developed model that is specific to justice-involved youth is the Juvenile Justice Behavioral Health Services Cascade (26), however this model only focuses on substance use treatment services and does not incorporate individual or family factors (only organizational/systems-level factors).
Data for all study variables are from caregiver self-report.
Youth Characteristics
Variables included age, sex, race (white; black, African, Haitian; Asian; American Indian; Native Hawaiian or Pacific Islander; other; multiracial), ethnicity (Hispanic/Latinx), father and/or mother figure, insurance coverage, primary care provider, and academic functioning (special education classes and individualized education plan [IEP]). Consistent with prior research (27), race and ethnicity were combined to create a single variable with the following categories: non-Hispanic black, non-Hispanic white, non-Hispanic other (‘other’ includes Asian, American Indian, Native Hawaiian or other Pacific Islander, or other non-specified race) non-Hispanic multi-racial, and Hispanic.
Psychiatric symptoms were assessed using the Behavior Assessment System for Children Second Edition, Parent Rating Scale-Adolescent (BASC-2 PRS-A)(28), a standardized tool for assessing risk of behavioral and emotional problems in youth aged 12–17 years. T-scores are provided for 9 clinical and 6 adaptive scales (median α= .85; range of .72–88). The BASC-2 PRS-A also includes composite scales for Externalizing Problems (Hyperactivity, Aggression, Conduct Problems) and Internalizing Problems (Anxiety, Depression, and Somatization). For these scales, T-scores of 20–60 suggest a “normal” level of risk, scores of 61–70 suggest an “elevated” level of risk, and scores of 71 or higher suggest an “extremely elevated” or “clinically significant” level of risk (29). For this study, T scores of ≥70 on the Externalizing and/or Internalizing Problems scale indicate clinically significant psychiatric symptoms.
Caregiver Characteristics
Variables included age, sex, education level, marital status, employment status, disability status, receipt of public assistance, country of birth, race (same categories as for youth), and Hispanic/Latinx ethnicity. As described for youth, race and ethnicity variables were combined to create 1 variable with the following categories: non-Hispanic black, non-Hispanic white, non-Hispanic other, non-Hispanic multi-racial, and Hispanic.
Caregiver history of a psychiatric diagnosis was assessed using the following items: 1) Have you ever been told by a doctor that you have a psychiatric diagnosis, and/or 2) Have you ever received treatment for drug and/or alcohol problems.
Caregiver-adolescent communication was assessed using the 25-item Parent-Adolescent General Communication Scale (PAC) (30). The PAC scale consists of two subscales: Positive Aspects and Negative Aspects of Communication. Items are scored on a 5-point Likert-type scale ranging from ‘strongly disagree’ to ‘strongly agree’. Higher Positive
Aspects scores indicate more positive communication, and higher Negative Aspects scores indicate more negative communication. In the current sample, each subscale demonstrated moderate internal consistency (Negative Aspects, α= .76; Positive Aspects, α= .81).
Family Characteristics
Variables included annual household income, family size, and family functioning. Caregivers’ perception of family functioning was assessed using the general family functioning scale of the McMaster Family Assessment Device (FAD) (31). This scale consists of 12 items about family communication and support. Each item is rated on a 4-point scale with responses ranging from 1 = strongly agree to 4 = strongly disagree. Higher mean scores indicate better family functioning. Adequate reliability (α = 0.88) has been established in prior studies of community-supervised justice-involved youth (32). For the current sample, internal consistency for the FAD General Functioning scale was α = .90.
Youth’s Psychiatric Services Use
The Child and Adolescent Services Assessment (CASA) was used to assess psychiatric services use by youth ages 8 to 18 years (33). Using criteria established by Burke et al (21), psychiatric services use includes endorsement of any of the following items in the past 4 months: (1) use of psychiatric medications, and/or receipt of care from the following settings and providers: (2) psychiatric inpatient unit, (3) inpatient alcohol/drug treatment unit or detoxification unit, (4) day hospital or partial hospitalization, (5) outpatient drug or alcohol clinic, (6) mental health center for psychiatric or mental health problems, or (7) private professional help from a psychiatrist or psychologist, or (8) social worker or psychiatric nurse.
Barriers to Youth’s Psychiatric Services Use
Barriers to youth’s psychiatric services use were assessed using items from the CASA (33). Caregivers were asked about 12 different barriers to obtaining services for their child in the past 4 months, ranging from stigma (e.g., anticipation of negative reaction by family, friends, or others); to concerns about cost, transportation, or language; to agency hurdles. Agency hurdles include obstacles such as bureaucratic delay (waiting lists, paperwork), refusal to treat, or non-availability of the desired treatment.
Statistical Analyses
Descriptive statistics, including means and percentages, were used to describe youth, caregiver, and family characteristics for the total sample. Bivariate analyses, including t tests and chi square tests, were conducted to compare these characteristics among youth with and without psychiatric services use in the past 4 months. The relationship between services use and characteristics was assessed using multivariable logistic regression. Characteristics that were significantly associated (p<0.05) with services use in the bivariate analyses, nor highly correlated (p<0.5) with other characteristics were included in the multivariable model. All analyses were conducted using Stata, version 15.
Results
Sample Characteristics
The sample consisted of 423 youth-caregiver dyads. As shown in Table 1, slightly more than half of youth were male (53%) and the mean age was 14.6 years. Thirty percent were non-Hispanic White, 8% non-Hispanic black, 4% non-Hispanic other, 15% non-Hispanic-multiracial, and 43% Hispanic. The majority (94%) were insured (Medicaid) and had a primary care provider (91%). In the past 4 months, nearly half of youth (49%) experienced clinically significant psychiatric symptoms.
Table 1.
Baseline characteristics of 423 community-supervised youths ages 12–18 and their caregivers and families.
| Characteristic | N | % |
|---|---|---|
| Youth | ||
| Age | ||
| Mean±SD | 423 | 14.6±.1.5 |
| Psychiatric Symptoms | ||
| No | 217 | 51 |
| Yes | 206 | 49 |
| Sex | ||
| Male | 226 | 53 |
| Female | 193 | 46 |
| Other (nonbinary) | 4 | 1 |
| Race/Ethnicity | ||
| non-Hispanic White | 127 | 30 |
| non-Hispanic Black, African | ||
| American, or Hattian | 33 | 8 |
| non-Hispanic Othera | 17 | 4 |
| non-Hispanic Mixed or Multi-Racial | 65 | 15 |
| Hispanic | 181 | 43 |
| Mother Figure in House | ||
| No | 34 | 8 |
| Yes | 389 | 92 |
| Father Figure in House | ||
| No | 214 | 51 |
| Yes | 209 | 49 |
| Attends Special Education Classes | ||
| No | 311 | 74 |
| Yes | 112 | 27 |
| Has an Individualized Education Plan | ||
| No | 281 | 66 |
| Yes | 142 | 34 |
| Has Health Insurance | ||
| No | 25 | 6 |
| Yes | 398 | 94 |
| Has a Primary Care Provider | ||
| No | 37 | 9 |
| Yes | 386 | 91 |
| Caregiver | ||
| Age | ||
| Mean±SD | 423 | 41.1±7.2 |
| Sex | ||
| Male | 56 | 13 |
| Female | 367 | 87 |
| Race/Ethnicity | ||
| non-Hispanic White | 176 | 42 |
| non-Hispanic Black, African | ||
| American, or Hattian | 36 | 9 |
| non-Hispanic Othera | 26 | 6 |
| non-Hispanic Mixed or Multi-Racial | 38 | 9 |
| Hispanic | 147 | 35 |
| US Born | ||
| No | 131 | 31 |
| Yes | 292 | 69 |
| Education level | ||
| some high school | 123 | 29 |
| high school grad | 81 | 19 |
| some college | 125 | 30 |
| college grad or higher | 94 | 22 |
| Marital status | ||
| not married | 306 | 72 |
| married | 116 | 27 |
| Employment status | ||
| Not employed | 220 | 52 |
| Employed | 203 | 48 |
| Receives public assistance | ||
| No | 149 | 35 |
| Yes | 274 | 65 |
| Receives disability funds | ||
| No | 337 | 80 |
| Yes | 86 | 20 |
| History of a Psychiatric Disorder | ||
| No | 289 | 68 |
| Yes | 134 | 32 |
| Positive Caregiver-Adolescent Communication Score | ||
| Mean±SDb | 422 | 37.7±8.0 |
| Negative Caregiver-Adolescent Communication Score | ||
| Mean±SDb | 421 | 26.6±8.0 |
| Family | ||
| Family size (N of children) | ||
| 1 | 109 | 26 |
| 2 | 125 | 30 |
| >=3 | 189 | 45 |
| Household income | ||
| <= 10,000 | 86 | 20 |
| 10,000 – 49,999 | 271 | 64 |
| >=50,000 | 66 | 16 |
| General Family Functioning Score | ||
| Mean±SDc | 406 | 3.3 ±.55 |
| Youths’ use of psychiatric services in past 4 monthsd | ||
| No | 272 | 64 |
| Yes | 151 | 36 |
| # Barriers to Youth’s Psychiatric Servicesa Use | ||
| 0 | 336 | 79 |
| 1 | 53 | 13 |
| >= 2 | 34 | 8 |
Includes Asian, American Indian, Native Hawaiian or other Pacific Islander, or other nonspecified race.
Possible scores range from 10 to 50, with higher scores indicating more positive or more negative communication. Results were missing for 1 youth on the positive scale and 2 youths on the negative scale.
Assessed with the general family functioning scale of the McMaster Family Assessment Device. Possible scores range from 0 to 4, with higher scores indicating better functioning. Results were missing for 17 youths.
Use of psychiatric medications or receipt of care from any of the following: psychiatric inpatient unit, inpatient alcohol or drug treatment unit or detoxification unit, day hospital or partial hospitalization, outpatient drug or alcohol clinic, mental health center for psychiatric or mental health problems, private professional help from a psychiatrist or psychologist, or private professional help from a social worker or psychiatric nurse.
Caregivers were predominantly female (87%) and on average 41.1 years old. Forty-two percent were non-Hispanic white and 35% were Hispanic. Forty-five percent had 3 or more children, 65% were receiving public assistance, and 71% completed at least high school. Almost one-third (32%) reported a history of a psychiatric diagnosis.
Prevalence and Determinants of Youth’s Psychiatric Services Use
Table 2 displays rates of psychiatric services use by youth, caregiver, and family characteristics. In the past 4 months, 36% of youth had received psychiatric services. A significantly higher proportion of youth with psychiatric symptoms used services compared to those without symptoms (54% vs. 18%, p<.001). Youth whose caregiver reported a history of psychiatric diagnosis were also more likely to use services (59% vs. 25%, p<.001). Non-Hispanic black and non-Hispanic-other caregiver race/ethnicity were associated with the lowest rates of youth’s service use (14% and 12%, respectively); however the number of caregivers from these racial/ethnic groups was small (n=5 and n=3, respectively). A higher percentage of youth from families with 1 child used services relative to youth from larger families. Youth from families with lower family functioning (mean score <3) were significantly more likely to use services relative to youth from higher functioning families. Poor caregiver-adolescent communication (i.e., higher negative communication and lower positive communication subscale scores) was associated with greater services use.
Table 2.
Use of psychiatric services in the past 4 months by 423 community-supervised youths ages 12–18, by youth, caregiver, and family characteristicsa
| Characteristic | Used Psychiatrica Services | p-value | |
|---|---|---|---|
| N | % | ||
| Total Sample | 151 | 36 | |
| Youth | |||
| Age | |||
| Mean±SD | 151 | 14.5±1.51 | |
| Psychiatric Symptoms | |||
| No | 39 | 18 | <.001 |
| Yes | 112 | 54 | |
| Sex | |||
| Other (nonbinary) | 1 | 25 | |
| Male | 76 | 34 | .546 |
| Female | 74 | 38 | |
| Race/Ethnicity | |||
| non-Hispanic White | 60 | 47 | <.001 |
| non-Hispanic Black, African American, or Hattian | 4 | 12 | |
| non-Hispanic Othera | 5 | 29 | |
| non-Hispanic Mixed or Multi-Racial | 21 | 32 | |
| Hispanic | 61 | 34 | |
| Mother Figure in House | |||
| No | 19 | 56 | .010 |
| Yes | 132 | 34 | |
| Father Figure in House | |||
| No | 77 | 36 | .902 |
| Yes | 74 | 35 | |
| Attends Special Education Classes | |||
| No | 95 | 31 | <.001 |
| Yes | 56 | 50 | |
| Has an Individualized Education Plan | |||
| No | 80 | 29 | <.001 |
| Yes | 71 | 50 | |
| Has Health Insurance | |||
| No | 8 | 32 | .691 |
| Yes | 143 | 36 | |
| Has a Primary Care Provider | |||
| No | 12 | 32 | .664 |
| Yes | 139 | 36 | |
| Caregiver | |||
| Age | 151 | 42.5±7.9 | |
| Mean±SD | |||
| Sex | |||
| Male | 21 | 38 | .762 |
| Female | 130 | 35 | |
| Race/Ethnicity | |||
| non-Hispanic White | 81 | 46 | <.001 |
| non-Hispanic Black, African American, or Hattian | 5 | 14 | |
| non-Hispanic Othera | 3 | 12 | |
| non-Hispanic Mixed or Multi-Racial | 12 | 32 | |
| Hispanic | 50 | 34 | |
| US Born | |||
| No | 40 | 31 | .138 |
| Yes | 111 | 38 | |
| Education level | |||
| some high school | 35 | 29 | .132 |
| high school grad | 28 | 35 | |
| some college | 47 | 38 | |
| college grad or higher | 41 | 44 | |
| Marital status | |||
| not married | 107 | 35 | .645 |
| married | 44 | 38 | |
| Employment status | |||
| Not employed | 71 | 32 | .126 |
| Employed | 80 | 35 | |
| Receives public assistance | |||
| No | 55 | 37 | .700 |
| Yes | 96 | 35 | |
| Receives disability funds | |||
| No | 113 | 34 | .066 |
| Yes | 38 | 44 | |
| History of a Psychiatric Disorder | |||
| No | 72 | 25 | <.001 |
| Yes | 79 | 59 | |
| Negative Communication Mean Score (N=150) | |||
| <36 (less negative) | 117 | 32 | .001 |
| >=36 (more negative) | 33 | 55 | |
| Positive Communication Mean Score (N=149) | |||
| <36 (less positive) | 62 | 42 | .045 |
| >=36 (more positive) | 88 | 32 | |
| Family | |||
| Family size (#kids) | |||
| 1 | 51 | 47 | .004 |
| 2 | 47 | 38 | |
| >=3 | 83 | 28 | |
| Household income | |||
| <= 10,000 | 31 | 38 | .162 |
| 10,000 – 49,999 | 83 | 32 | |
| > 50,000 | 28 | 44 | |
| General Family Functioning Mean Score (N=143) | |||
| < 3 (lower functioning) | 54 | 51 | <.001 |
| >=3 (higher functioning) | 89 | 30 | |
Use of psychiatric medications or receipt of care from any of the following: psychiatric inpatient unit, inpatient alcohol or drug treatment unit or detoxification unit, day hospital or partial hospitalization, outpatient drug or alcohol clinic, mental health center for psychiatric or mental health problems, private professional help from a psychiatrist or psychologist, or private professional help from a social worker or psychiatric nurse.
Includes Asian, American Indian, Native Hawaiian or other Pacific Islander, or other nonspecified race.
Possible scores range from 10 to 50, with higher scores (>=36) indicating more positive or more negative communication.
Assessed with the general family functioning scale of the McMaster Family Assessment Device. Possible scores range from 0 to 4, with a score of >=3 indicating higher functioning.
Table 3 displays the multivariable associations between youth’s psychiatric services use and sample characteristics. Youth psychiatric symptoms were positively associated with the odds of services use (adjusted (a) OR=3.79; CI=2.17–6.62), as was caregiver history of psychiatric diagnosis (aOR =3.40; CI=2.01–5.55). Youth of caregivers who identified as non-Hispanic-other were significantly less likely to have used services relative to youth of non-Hispanic white caregivers (aOR=0.22; CI=.06-.84). None of the other caregiver race/ethnicity categories were associated with youth’s services use. Neither caregiver-adolescent communication nor general family functioning scores were significantly associated with the odds of youth’s services use after adjusting for potential confounders.
TABLE 3.
Predictors of use of psychiatric services in the past 4 months by 423 community-supervised youths ages 12–18a
| Characteristic | AORb | 95% CI | p |
|---|---|---|---|
| Youth | |||
| Psychiatric Symptoms (reference: no psychiatric symptoms) | 3.79 | 2.17–6.62 | <.001 |
| IEPc (reference: no IEP) | 1.61 | .96–2.71 | .070 |
| Mother Figure at Home (reference: no mother figure at home) | .53 | .22–1.27 | .156 |
| Caregiver | - | ||
| Age | 1.05 | 1.01–1.09 | .012 |
| Race/Ethnicity (reference: non-Hispanic White) | |||
| non-Hispanic Black, African | |||
| American, or Hattian | .38 | .13–1.18 | .079 |
| non-Hispanic Otherc | .22 | .06-.84 | .027 |
| non-Hispanic Mixed or Multi-Racial | .50 | .20–1.24 | .137 |
| Hispanic | .94 | .54–1.64 | .818 |
| Caregiver-adolescent positive communication | 1.01 | .98–1.05 | .513 |
| Caregiver-adolescent negative communication | 1.01 | .98–1.04 | .757 |
| History of a Psychiatric Disorder | |||
| (reference: no history of a psychiatric disorder) | 3.40 | 2.04–5.66 | <.001 |
| Family | |||
| Family Size (reference: 1 child) | |||
| 2 | .75 | .40–1.40 | .293 |
| ≥3 | .58 | .31–1.09 | .089 |
| General Family Functioning | .82 | .48–1.39 | .458 |
Use of psychiatric medications or receipt of care from any of the following: psychiatric inpatient unit, inpatient alcohol or drug treatment unit or detoxification unit, day hospital or partial hospitalization, outpatient drug or alcohol clinic, mental health center for psychiatric or mental health problems, private professional help from a psychiatrist or psychologist, or private professional help from a social worker or psychiatric nurse.
Adjusted odds ratio. Represents the odds of psychiatric service use for each variable of interest, controlling for all other variables in the model.
Includes Asian, American Indian, Native Hawaiian or other Pacific Islander, or other non-specified race.
Barriers to Psychiatric Services Use
Twenty-one percent (n=87) of caregivers encountered one or more barriers to accessing services for their adolescent (Table 1). Each individual barrier was endorsed by less than 10% of the total sample (see Supplemental Table 1). The most commonly reported barrier was transportation issues (6%, n=25), followed by agency/program issues (6%, n=24), time (4%, n=18), and distrust of professionals (4%, n=18).
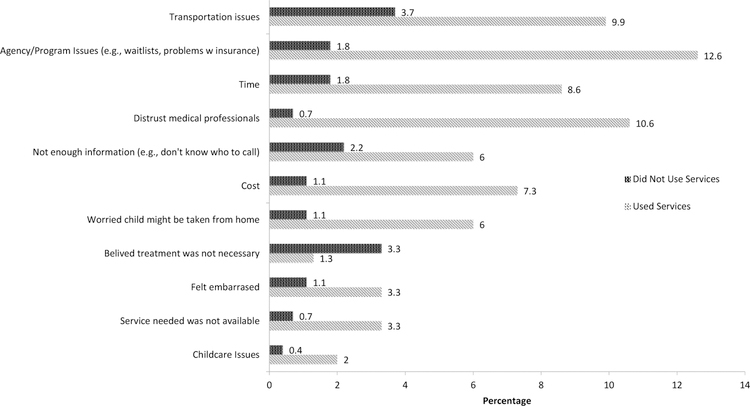
Caregivers of youth who had received psychiatric services were significantly more likely to experience barriers relative to caregivers of youth who had not received services (35% vs. 13%, p<.001). The frequency of each barrier also differed according to whether youth received psychiatric services (Figure 1). The most common barriers reported by caregivers of youth who received services (n=151) were agency/program issues (13%, n=19) and distrust of professionals (11%, n=16). Among youth who hadn’t received services (n=272), the top barriers were transportation issues (4%, n=10) and “did not feel treatment was necessary” (3%, n=9).
Figure 1.
Barriers to accessing psychiatric services reported by 423 caregivers of community-supervised youths, by youths’ use of psychiatric services in the past 4 months
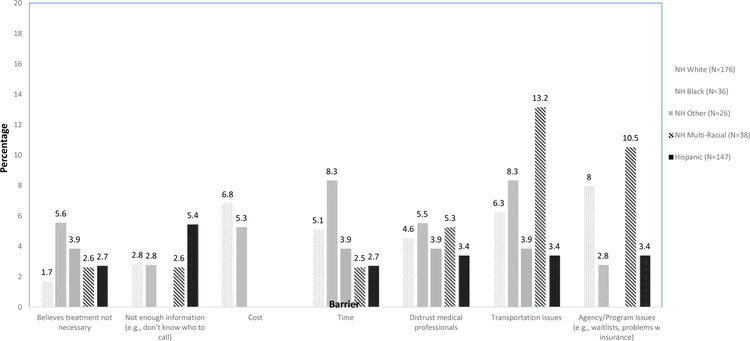
Barriers to youth’s psychiatric services were not significantly related to caregiver race/ethnicity, however racial/ethnic group differences in the frequency of each individual barrier were observed. As shown in Figure 2, the most frequently endorsed barrier among non-Hispanic white caregivers (n=176) was agency/program issues (8%, n=14). Among non-Hispanic black caregivers (n=36) it was transportation issues and time (8%, n=3). Among Hispanic/Latinx caregivers (n=147) it was “not enough information” (5%, n=15).
Figure 2.
Selected barriers to accessing psychiatric services reported by 423 caregivers of community-supervised youths, by caregiver race-ethnicity
Discussion
Previous psychiatric services research among justice-involved youth has focused predominantly on detained adolescents. This study adds to the literature examining the prevalence and correlates of psychiatric services use among a large sample of community-supervised youth (N=423). The rate of services use was low (35%) among this population despite a high prevalence of clinically significant psychiatric symptoms (48.7%). These results are consistent with prior literature showing that 74% of first-time juvenile offenders had a psychiatric disorder, yet only 20% had received mental health services (21). A study of mental health treatment rates among previously detained adolescents showed that 82.2% of needed treatment, but only 16.4% received it following community re-entry (13).
The strongest predictors of psychiatric services use were youth psychiatric symptoms per the BASC-2 caregiver-report and caregiver history of a psychiatric diagnosis. Findings are consistent with previous research demonstrating that symptom severity (34, 35) and meeting diagnostic threshold criteria (36) are the most significant predictors of adolescent psychiatric services use. Caregiver psychopathology may also positively influence youth’s mental health services use (37, 38). Caregivers who have personally experienced a mental health disorder and/or have used mental health services may be more likely to bring their children for treatment (38, 39).
Caregiver-adolescent communication quality and family functioning were not associated with youth’s service use despite some research demonstrating that youth from families with poor relationship dynamics are more likely to seek out mental health treatment (22, 40). However, prior studies are few and findings are inconsistent (41, 42). Given that youth’s access to psychiatric services is often dependent on caregivers’ support and involvement (e.g., health insurance, transportation), future research should elucidate how family factors positively or negatively impact youth’s engagement in services.
Results suggest that youth whose caregiver identifies as a racial/ethnic minority are potentially less likely to receive psychiatric services relative to non-Hispanic white caregivers. More research is needed among community-supervised youth and families to understand how caregiver race/ethnicity influences youth’s services use in the presence of other factors. Potential explanations are that minority caregivers are less likely than white caregivers to identify when their child’s problem requires treatment and to initiate treatment once identified (43, 44), uncertainty about treatment benefits (45), less knowledge about treatment options (44), and other perceived barriers such as cost, lack of choices in types of services offered, and having to travel too far (46).
Barriers to youth’s services use differed according to whether or not youth had received services. More caregivers of youth who used services reported barriers than caregivers of youth who had not, primarily due to higher endorsement of service-related barriers. Service-related barriers (e.g., agency problems) were more common among youth who had received services, whereas barriers to engagement (e.g., perceived need for treatment, transportation difficulties) were more common among youth who had not received services. These findings suggest that interventions to reduce barriers should be tailored to the stage of services use, such as help-seeking or treatment engagement (26).
There are several limitations worth noting. Data are cross-sectional and thus preclude any causal inferences. This study was also not designed to gather in-depth information about barriers to services use and thus may have missed additional important barriers. The focus on caregiver self-report data may have missed certain factors specific to youth’s perception. However, research suggests that caregivers may be better able to discern psychiatric symptoms and severity than youth (47, 48), and caregiver’s recognition of symptoms and perceived need for treatment are correlated with youth’s services use (21, 49, 50). Additionally, caregiver-perceived burden plays a significant role in youth’s ability to access health services given that youth are often reliant on their parents to get them to their appointments and remain engaged in treatment (22, 51, 52). Caregivers’ own psychological state at the time of reporting (i.e., during youth’s first justice involvement) may have influenced their perception of their adolescent’s psychiatric symptoms; however, the rate of psychiatric symptoms in this sample is comparable to other studies of justice-involved youth. The low rates of substance use service use also precluded separate analysis from mental health service use. Lastly, generalizability to other community-supervised youth and families may be limited by single-state geographic study location, overrepresentation of females, publicly insured, low participation rate (28%), and potential differences between participants and those who declined that were unmeasurable. Despite low participation, the study’s sampling approach likely resulted in a sample that is larger and more representative than other services-related studies including first-time offending youth (<100) (21, 53).
Conclusions
There is a critical need to better understand the factors that influence community-supervised youth’s psychiatric services use given the high rate of unmet treatment need, particularly among youth from racially and ethnically diverse families. Study findings also highlight the importance of considering caregiver factors when designing interventions to community-supervised youth’s engagement in psychiatric services, including their perspectives on barriers to accessing these services for their adolescent. Obtaining this information during initial assessment for treatment needs may help the justice system connect youth to services that match their needs and preferences.
Supplementary Material
HIGHLIGHTS.
Just over one-third of first-time offending youth recently used behavioral health services
Youth psychiatric symptoms and caregiver history of a psychiatric diagnosis were significant predictors of services use.
Youth whose caregivers identify as a racial or ethnic minority were disproportionately less likely to receive behavioral health services.
Youth who had never received services encountered different barriers than youth who had.
Acknowledgements:
Grant Support: All phases of this study were supported by the National Institute on Drug Abuse (Grant #: 3R01DA034538–05S1)
Footnotes
Disclosures
All authors have indicated they have no potential, perceived, or real conflicts of interest to disclose.
Previous Presentation: These data were presented at the American Public Health Association annual meeting on November 8th, 2018 in Atlanta, Georgia.
References
- 1.OJJDP. Law enforcement and juvenile crime. Juvenile Arrests, 2015 [Google Scholar]
- 2.Hockenberry S, Puzzanchera C: Juvenile Court Statistics 2015 Pittsburgh, PA: National Center for Juvenile Justice., 2018 [Google Scholar]
- 3.Romero EG, Teplin LA, McClelland GM, et al. : A longitudinal study of the prevalence, development, and persistence of HIV/sexually transmitted infection risk behaviors in delinquent youth: Implications for health care in the community. Pediatrics 119:E1126–E41, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Teplin LA, Abram KM, McClelland GM, et al. : Psychiatric disorders in youth in juvenile detention. Arch Gen Psychiatry 59:1133–43, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Teplin LA, Elkington KS, McClelland GM, et al. : Major mental disorders, substance use disorders, comorbidity, and HIV-AIDS risk behaviors in juvenile detainees. Psychiat Serv 56:823–8, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Institute of Justice. Delinquency to adult offending, 2014 [Google Scholar]
- 7.Rosenfeld R, White HR, Finn-Aage E: Special categories of serious and violent offenders: Drug dealers, gang members, homicide offenders, and sex offenders; in From juvenile delinquency to adult crime: Criminal careers, justice policy, and prevention Edited by Loeber R, Farrington DP. New York: Oxford Press, 2012 [Google Scholar]
- 8.Colins O, Vermeiren R, Vreugdenhil C, et al. : Psychiatric disorders in detained male adolescents: a systematic literature review. Can J Psychiatry 55:255–63, 2010 [DOI] [PubMed] [Google Scholar]
- 9.Kenny DT, Lennings CJ, Nelson PK: The Mental Health of Young Offenders Serving Orders in the Community. Journal of Offender Rehabilitation 45:123–48, 2007 [Google Scholar]
- 10.Teplin LA, Abram KM, McClelland GM, et al. : Detecting mental disorder in juvenile detainees: who receives services. Am J Public Health 95:1773–80, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Young DW, Dembo R, Henderson CE: A National Survey of Substance Abuse Treatment for Juvenile Offenders. Journal of substance abuse treatment 32:255–66, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aalsma MC, Tong Y, Lane K, et al. : Use of outpatient care by juvenile detainees upon community reentry: effects of mental health screening and referral. Psychiatr Serv 63:997–1003, 2012 [DOI] [PubMed] [Google Scholar]
- 13.White LM, Lau KS, Aalsma MC: Detained Adolescents: Mental Health Needs, Treatment Use, and Recidivism. The journal of the American Academy of Psychiatry and the Law 44:200–12, 2016 [PubMed] [Google Scholar]
- 14.Abram KM, Paskar LD, Washburn JJ, et al. : Perceived barriers to mental health services among youths in detention. J Am Acad Child Adolesc Psychiatry 47:301–8, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.CASA: Criminal neglect: Substance abuse, juvenile justice, and the children left behind New York: National Center on Addiction and Substance Abuse at Columbia University, 2004 [Google Scholar]
- 16.Cuellar AE, McReynolds LS, Wasserman GA: A cure for crime: can mental health treatment diversion reduce crime among youth? Journal of policy analysis and management : [the journal of the Association for Public Policy Analysis and Management] 25:197–214, 2006 [DOI] [PubMed] [Google Scholar]
- 17.Andrews DA, Bonta J, Wormith JS: The Risk-Need-Responsivity (RNR) Model: Does Adding the Good Lives Model Contribute to Effective Crime Prevention? Criminal Justice and Behavior 38:735–55, 2011 [Google Scholar]
- 18.Garner BR, Belur VK, Dennis ML: The GAIN Short Screener (GSS) as a Predictor of Future Arrest or Incarceration Among Youth Presenting to Substance Use Disorder (SUD) Treatment. Substance abuse : research and treatment 7:199–208, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Skeem JL, Manchak S, Peterson JK: Correctional policy for offenders with mental illness: creating a new paradigm for recidivism reduction. Law and human behavior 35:110–26, 2011 [DOI] [PubMed] [Google Scholar]
- 20.Rawal P, Romansky J, Jenuwine M, et al. : Racial differences in the mental health needs and service utilization of youth in the juvenile justice system. J Behav Health Serv Res 31:242–54, 2004 [DOI] [PubMed] [Google Scholar]
- 21.Burke JD, Mulvey EP, Schubert CA: Prevalence of mental health problems and service use among first-time juvenile offenders. J Child Fam Stud 24:3774–81, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gopalan G, Goldstein L, Klingenstein K, et al. : Engaging families into child mental health treatment: updates and special considerations. Journal of the Canadian Academy of Child and Adolescent Psychiatry = Journal de l’Academie canadienne de psychiatrie de l’enfant et de l’adolescent 19:182–96, 2010 [PMC free article] [PubMed] [Google Scholar]
- 23.Hirschtritt ME, Dauria EF, Marshall BDL, et al. : Sexual Minority, Justice-Involved Youth: A Hidden Population in Need of Integrated Mental Health, Substance Use, and Sexual Health Services. Journal of Adolescent Health 63:421–8, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Andersen R, Newman JF: Societal and individual determinants of medical care utilization in the United States. The Milbank Memorial Fund quarterly Health and society 51:95–124, 1973 [PubMed] [Google Scholar]
- 25.Andersen RM: Revisiting the behavioral model and access to medical care: does it matter? Journal of health and social behavior 36:1–10, 1995 [PubMed] [Google Scholar]
- 26.Belenko S, Knight D, Wasserman GA, et al. : The Juvenile Justice Behavioral Health Services Cascade: A new framework for measuring unmet substance use treatment services needs among adolescent offenders. J Subst Abuse Treat 74:80–91, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Race, Ethnicity, and Language Data: Standardization for Health Care Quality Improvement Edited by Ulmer C, McFadden B, Nerenz DR. Washington, DC: National Academies Press, 2009 [PubMed] [Google Scholar]
- 28.Reynolds C, Kamphaus R: Behavior Assessment for Children, (BASC-2) Circle Pines, MN: American Guidance Service, 2004 [Google Scholar]
- 29.Kamphaus R, Reynolds C: Behavior Assessment System for Children — Second Edition (BASC-2): Behavioral and Emotional Screening System (BESS) Bloomington, MN: Pearson, 2007 [Google Scholar]
- 30.Barnes H, Olson DH: Parent adolescent communication and the circumplex model. Child Development 56:438–47, 1985 [Google Scholar]
- 31.Epstein NB, Baldwin LM, Bishop DS: The McMaster family assessment Device. Journal of Marital and Family Therapy 9:171–80, 1983 [Google Scholar]
- 32.Tolou-Shams M, Brogan L, Esposito-Smythers C, et al. : The role of family functioning in parenting practices of court-involved youth. J Adolesc 63:165–74, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.BH Z. Ascher Farmer EM, Burns BJ, et al. : The Child and Adolescent Services Assessment (CASA):Description and Psychometrics. Journal of Emotional and Behavioral Disorders 4:12–20, 1996 [Google Scholar]
- 34.Kataoka SH, Zhang L, Wells KB: Unmet need for mental health care among U.S. children: variation by ethnicity and insurance status. The American journal of psychiatry 159:1548–55, 2002 [DOI] [PubMed] [Google Scholar]
- 35.Merikangas KR, He JP, Burstein M, et al. : Service utilization for lifetime mental disorders in U.S. adolescents: results of the National Comorbidity Survey-Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry 50:32–45, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cheng TC, Lo CC: Mental Health Service and Drug Treatment Utilization: Adolescents with Substance Use/Mental Disorders and Dual Diagnosis. Journal of Child & Adolescent Substance Abuse 19:447–60, 2010 [Google Scholar]
- 37.Breland DJ, McCarty CA, Zhou C, et al. : Determinants of mental health service use among depressed adolescents. Gen Hosp Psychiatry 36:296–301, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Olfson M, Marcus SC, Druss B, et al. : Parental depression, child mental health problems, and health care utilization. Medical care 41:716–21, 2003 [DOI] [PubMed] [Google Scholar]
- 39.Turner EA, Liew J: Children’s adjustment and child mental health service use: the role of parents’ attitudes and personal service use in an upper middle class sample. Community Ment Health J 46:231–40, 2010 [DOI] [PubMed] [Google Scholar]
- 40.Verhulst FC, van der Ende J: Factors associated with child mental health service use in the community. J Am Acad Child Adolesc Psychiatry 36:901–9, 1997 [DOI] [PubMed] [Google Scholar]
- 41.Fisher JH, Lichvar E, Hogue A, et al. : Perceived Need for Treatment and Engagement in Mental Health Services Among Community-Referred Racial/Ethnic Minority Adolescents. Administration and policy in mental health, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ryan SM, Jorm AF, Toumbourou JW, et al. : Parent and family factors associated with service use by young people with mental health problems: a systematic review. Early Interv Psychiatry 9:433–46, 2015 [DOI] [PubMed] [Google Scholar]
- 43.Thurston IB, Phares V, Coates EE, et al. : Child problem recognition and help-seeking intentions among black and white parents. Journal of clinical child and adolescent psychology : the official journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53 44:604–15, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yeh M, McCabe K, Hough RL, et al. : Racial/ethnic differences in parental endorsement of barriers to mental health services for youth. Ment Health Serv Res 5:65–77, 2003 [DOI] [PubMed] [Google Scholar]
- 45.McMiller WP, Weisz JR: Help-seeking preceding mental health clinic intake among African-American, Latino, and Caucasian youths. J Am Acad Child Adolesc Psychiatry 35:1086–94, 1996 [DOI] [PubMed] [Google Scholar]
- 46.Thurston IB, Phares V: Mental health service utilization among African American and Caucasian mothers and fathers. J Consult Clin Psychol 76:1058–67, 2008 [DOI] [PubMed] [Google Scholar]
- 47.Fraser A, Cooper M, Agha SS, et al. : The presentation of depression symptoms in attention-deficit/hyperactivity disorder: comparing child and parent reports. Child Adolesc Ment Health 23:243–50, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kuhn C, Aebi M, Jakobsen H, et al. : Effective Mental Health Screening in Adolescents: Should We Collect Data from Youth, Parents or Both? Child Psychiatry Hum Dev 48:385–92, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reardon T, Harvey K, Baranowska M, et al. : What do parents perceive are the barriers and facilitators to accessing psychological treatment for mental health problems in children and adolescents? A systematic review of qualitative and quantitative studies. Eur Child Adolesc Psychiatry 26:623–47, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Langer DA, Wood JJ, Wood PA, et al. : Mental Health Service Use in Schools and Non-School-Based Outpatient Settings: Comparing Predictors of Service Use. School Ment Health 7:161–73, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Becker KD, Buckingham SL, Brandt NE: Engaging youth and families in school mental health services. Child Adolesc Psychiatr Clin N Am 24:385–98, 2015 [DOI] [PubMed] [Google Scholar]
- 52.Lindsey MA, Brandt NE, Becker KD, et al. : Identifying the common elements of treatment engagement interventions in children’s mental health services. Clinical child and family psychology review 17:283–98, 2014 [DOI] [PubMed] [Google Scholar]
- 53.Zeola MP, Guina J, Nahhas RW: Mental Health Referrals Reduce Recidivism in First-Time Juvenile Offenders, But How Do We Determine Who is Referred? The Psychiatric quarterly 88:167–83, 2017 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.