Abstract
Studies on the relationships between marijuana use and quality of life have reported mixed findings. Based on a survey of 123 marijuana users conducted in Los Angeles during 2017-2018, we investigated the relationships between marijuana use frequency, severity of marijuana-related problems, and health-related quality of life (HRQoL). Results indicated that (1) marijuana use frequency was positively related to severity of marijuana-related problems; (2) severity of marijuana-related problems was negatively related to mental domain of HRQoL but was not significantly related to physical domain of HRQoL; and (3) marijuana use frequency was positively associated with mental health symptoms and physical health conditions, and both in turn were negatively linked to mental and physical domains of HRQoL, respectively. Reduction of marijuana-related problems and mitigation of mental and physical health problems may improve HRQoL among marijuana users. The study findings may contribute to developing treatment interventions for marijuana use that simultaneously address marijuana-related problems and associated mental and physical issues.
Keywords: Marijuana use, Quality of life, Severity of marijuana-related problem, Mental health, Physical health
1. Introduction
Marijuana is one of the most widely used psychoactive substances, with an estimated annual prevalence of 3.8% (range 2.7% to 4.9%) of the global population age 15-65 who reported marijuana use in the past year (United Nations Office on Drugs Crime, 2017). In the United States, there were 23.9 million current marijuana users (8.9% of people age 12 or older) in 2016 (Center for Behavioral Health Statistics and Quality, 2017), and epidemiological trends show an increase of marijuana use in recent years (Hasin, 2018).
Marijuana use often co-occurs with mental health problems. A national survey showed that anxiety, depression, and paranoia were associated with the use of marijuana (Cougle et al., 2015). Stress is also a common problem reported by marijuana users (Meil et al., 2016; Passarotti et al., 2015). Moreover, these co-occurring problems may be interrelated. For example, a study by Ketcherside and Filbey (2015) indicated that among heavy marijuana users, perceived stress is associated with depression and anxiety symptoms, which in turn affected problematic marijuana use.
Marijuana users have more adverse physical conditions than non-users. For example, sleep disturbance and poor appetite are frequently observed among individuals experiencing marijuana withdrawal symptoms (Budney and Hughes, 2006). Impairment in respiratory function, as seen with tobacco smoking, is also associated with marijuana use (Hancox et al., 2009; Ribeiro and Ind, 2016), but a causal relationship is not clear (Hall, 2015). Additionally, pain is a common physical problem among marijuana users, and potential analgesic properties of marijuana have been explored in prior studies. A nationally representative survey demonstrated that chronic pain was significantly associated with an increased risk of marijuana use (Zvolensky et al., 2011), which may be related to pain-relieving compounds in marijuana (Cohen, et al., 2016).
Quality of life assessments are important in evaluating treatment for substance use disorders as they focus on perceived functioning and well-being (Smith and Larson, 2003). Health-related quality of life (HRQoL) focuses on perceived satisfaction and functioning in both mental and physical health domains (Karimi and Brazier, 2016). A previous study suggested improved HRQoL with abstinence and lower marijuana use frequency (Brezing et al., 2018). In contrast, a longitudinal study demonstrated that reduction in marijuana use was not associated with improvement in HRQoL (Hser et al., 2017). In a recent meta-analysis, it was reported that heavy marijuana use was linked with poorer HRQoL, but the association was inconsistent across studies and the quality of included studies was determined to be low (Goldenberg et al., 2017). Furthermore, a prospective epidemiological survey revealed that marijuana use significantly affected mental, but not physical domains of HRQoL (Cougle et al., 2015). In sum, findings regarding the relationship between marijuana use and HRQoL are mixed, and this relationship may be different for the mental versus physical domains of HRQoL.
The inconsistent relationship between marijuana use frequency and HRQoL could be due to several reasons. First, factors influencing mental and physical domains of HRQoL could be different, so separate analyses may be preferable to explore the relationships. Second, marijuana use affects HRQoL via the severity of problems experienced by users. Frequent marijuana use increases the likelihood of developing marijuana-associated problems. Some users will subsequently develop related problems, such as diminished life satisfaction and achievement (Volkow et al., 2014) and problems with social activities (Lev-Ran et al., 2012). However, others may use marijuana without similar harms (Hasin, 2018) because problems do not occur immediately and may develop over time. Assessments of the relationship between marijuana use frequency and HRQoL may need to consider marijuana-related problems as perceived by the users, as well as separately consider the impacts of mental health symptoms and physical health conditions on HRQoL. It is important for treatment to not only target marijuana use reduction or abstinence, but to also address problems associated with marijuana and assess changes in perceived problems over time in order to fully evaluate the effectiveness of treatment. This knowledge may contribute to more tailored interventions provided by clinicians when treating problematic marijuana use.
The present study investigates if marijuana-related problems mediates the relationship between marijuana use and HRQoL separately for mental and physical domains. Additionally, mental and physical symptoms were separately controlled for in the respective analyses due to the aforementioned issue that marijuana use often co-occurs with mental health symptoms and worse physical conditions, both of which could influence the respective HRQoL (e.g., Lev-Ran et al., 2012 ; Aspis et al., 2015). We hypothesized that:
H1a: Marijuana use frequency will be negatively associated with mental HRQoL domain.
H1b: Marijuana use frequency will be negatively associated with physical HRQoL domain.
H1c. Marijuana use frequency will be positively associated with severity of marijuana-related problems.
H2a: Severity of marijuana-related problems will be negatively associated with mental HRQoL domain.
H2b: Severity of marijuana-related problems will be negatively associated with physical HRQoL domain.
H3a: Mental health symptoms will be negatively associated with mental HRQoL domain.
H3b: Physical health conditions will be negatively associated with physical HRQoL domain.
2. Methods
2.1. Participants and procedures
A cross-sectional survey was designed to explore functional outcomes associated with reduction in marijuana use. This survey was conducted among participants with a history of marijuana use recruited from substance use disorder (SUD) treatment programs and the general community (e.g., Marijuana Anonymous meetings, Craigslist) in Los Angeles between April 2017 and February 2018. Study inclusion criteria were (1) currently or formerly in treatment for marijuana use or, alternatively, having used marijuana heavily in the past year and reduced the marijuana use since then, and (2) able to provide informed consent. To reduce recall bias and selection bias, we excluded participants who received any treatment for substances other than marijuana, had used marijuana heavily more than one year ago, and had been decreasing marijuana use for less than a month. Given the lack of a standard definition for heavy cannabis use (Becker et al., 2015; Liebregts et al. 2015; Cousijn et al. 2014), in part due to variability in amount, frequency, and methods of cannabis use, heavy use and reduction were self-defined by the participant.
Participants were recruited through flyers and advertisements in local substance use treatment clinics and other sources (e.g., Marijuana Anonymous meetings, Craigslist). Research assistants explained detailed information regarding this study and confirmed study eligibility. A total of 123 interested individuals answered open-ended questions that required them to self-identify as eligible to participate the study. All respondents were eligible to participate. After prospective participants gave informed consent, small groups of approximately 10 eligible participants were provided instructions on how to complete questionnaires regarding marijuana use patterns and other functional outcomes. Research assistants provided assistance to the groups to facilitate self-administration of assessments. The group sessions lasted about two hours, and participants were compensated for their time. All responses were anonymous. The study was approved by the Institutional Review Boards (IRBs) at the University of California, Los Angeles.
2.2. Measures
Study measures included demographic characteristics, marijuana use frequency, severity of marijuana-related problems, mental health symptoms (anxiety, depression, stress, and paranoia), physical health conditions (sleep disturbance, respiratory function, pain intensity, and appetite problem), and HRQoL for mental and physical domains. Several variables, including anxiety, depression, sleep disturbance, pain intensity, and HRQoL, were measured by standardized scales that provided norms (relative to the general population in the United States) by converting the total raw score to a T-score metric ranging from 0 to 100, with a mean of 50 and a standard deviation fixed at 10. See Table 1 for a summary of study assessments.
Table 1.
Summary of measures
| Variable | Instrument/ scale (Reference) | Number of items |
Description |
|---|---|---|---|
| Marijuana use frequency | |||
| Days of use | N/A | 1 | Scores range from 0-6; higher scores indicate more use. |
| Daily use frequency | N/A | 1 | Scores range from 0-5; higher scores indicate more use. |
| Severity of marijuana-related problems | Marijuana Problem Scale (MPS; Stephens et al., 1994) | 19 | Scores range from 0-19; higher scores indicate more problems. |
| Mental health symptoms | |||
| Anxiety | Hospital Anxiety and Depression Scale (HADS; Zigmond and Snaith 1983) | 7 | Scores range from 0-21; higher scores indicate more anxiety. |
| Depression | Hospital Anxiety and Depression Scale (HADS; Zigmond and Snaith 1983) | 7 | Scores range from 0-21; higher scores indicate more depression. |
| Stress | Perceived Stress Scale (PSS; Cohen et al., 1994) | 4 | Scores range from 0-16; higher scores indicate more stress |
| Paranoia | Specific Psychotic Experiences Questionnaire – Paranoia Subscale (SPEQ; Ronald et al., 2013) | 15 | Scores range from 0-75; higher scores indicate worse symptoms. |
| Physical health conditions | |||
| Sleep disturbance | PROMIS Sleep Disturbance (Buysse et al., 2010) | 8 | T-score metric ranging from 0-100; higher scores indicate worse conditions. |
| Respiratory function | Part I of St. George’s Respiratory Questionnaire (SGRQ; Jones, Quirk, & Baveystock, 1991) | 5 | Recoded and summed with weights; Higher scores indicate poor respiratory function. |
| Pain intensity | PROMIS Pain Intensity (PROMIS Health Organization and PROMIS Cooperative Group, 2016) | 3 | T-score metric ranging from 0-100; higher scores indicate worse pain. |
| Appetite problems | Simplified Nutritional Appetite Questionnaire (SNAQ; Wilson et al., 2005) | 4 | Scores range from 4-20; higher scores indicate poor appetite |
| HRQoL | |||
| Mental health domain | Short Form 12 (SF-12; Ware Jr et al., 1996) | 12 | T-score metric ranging from 0-100; higher scores indicate better mental HRQoL. |
| Physical health domain | T-score metric ranging from 0-100; higher scores indicate better physical HRQoL. |
N/A=non-applicable
2.2.1. Marijuana use frequency.
Two items were used to measure marijuana use frequency in the past 30 days prior to the survey. One was the number of self-reported days using marijuana in the past 30 days. We scored it as: 0 = 0 days, 1 = 1–5 days, 2 = 6–10 days, 3 = 11–15 days, 4 = 16–20 days, 5 = 21–25 days, 6 = 26–30 days. Another was the daily use frequency that asked participants to score the average times of marijuana use per day on the days they used during the past 30 days: 0 = none, 1 = once a day, 2 = 2–3 times a day, 3 = 4–5 times a day, 4 = 6–7 times a day, 5 = more than 7 times a day.
2.2.2. Severity of marijuana-related problems.
The Marijuana Problem Scale (MPS, form AS5) (Stephens et al., 1994), a self-report 19-item instrument, was used to assess negative effects of marijuana on social relationships, self-esteem, motivation and productivity, work and finances, physical health, memory impairment, and legal problems. Participants were asked to rate experienced problems related to marijuana use in the past 30 days on the range from 0 (not a problem) to 2 (a serious problem). It was calculated with the number of items scored “minor” or “serious” problems, and total scores ranged from 0-19.
2.2.3. Anxiety and depression.
The Hospital Anxiety and Depression Scale (HADS) (Zigmond and Snaith 1983) was used. HADS is a brief (7 items each), validated self-assessment of anxiety and depression severity (Bjelland et al. 2002). Each item was rated on a four-point (0–3) response category with scores ranging from 0 to 21 for both anxiety and depression.
2.2.4. Stress.
The Perceived Stress Scale (PSS) was used to measure the degree to which situations in a participant’s life were appraised as stressful in the past month (Cohen et al., 1994). Four items (Cohen and Williamson, 1988) were rated on a Likert scale ranging from never (0) to very often (4). Higher scores indicate higher perceived stress.
2.2.5. Paranoia.
We selected the “Paranoia subscale” from the Specific Psychotic Experiences Questionnaire (SPEQ) (Ronald et al., 2013) that included five self-report subscales (paranoia, hallucinations, cognitive disorganization, grandiosity, and anhedonia). The 15 items were adapted from the Paranoia Checklist, rating on a Likert scale that ranges from “not at all” (0) to “daily” (5). Higher scores indicate worse symptoms.
2.2.6. Sleep Disturbance.
The Patient-Reported Outcomes Measurement Information System (PROMIS; PROMIS Health Organization and PROMIS Cooperative Group, 2016) Sleep Disturbance measure was used to assess sleep disturbance using eight items from the PROMIS Sleep Disturbance instrument, which assessed conditions with sleep, difficulty falling asleep, whether sleep was refreshing, and sleep quality over the past 7 days (Buysse et al., 2010). The eight items were rated on a Likert scale, ranging from never (1) to always (5). Higher scores indicate worse conditions.
2.2.7. Respiratory function.
We selected the first 5 items in Part I of St. George's Respiratory Questionnaire (SGRQ, version 2.3) (Jones, Quirk, & Baveystock, 1991) to assess lung/respiratory symptoms in the past 4 weeks. The first four items were rated on a Likert scale, ranging from almost every day (1) to not at all (5), and the fifth item asked about unpleasant episodes of lung/respiratory problems, ranging from more than three episodes (1) to no episodes (5). These 5 items were recoded and summed with weights (Jones, 2009). Higher scores indicate poor respiratory function.
2.2.8. Pain intensity.
The PROMIS Pain Intensity instrument was used to assess how much a participant hurt in the past 7 days (PROMIS Health Organization and PROMIS Cooperative Group, 2016). The first two items within the short form assess pain intensity over the past seven days while the last item asks the participants to rate their pain intensity “right now.” The three items were rated on a Likert scale, ranging from no pain (1) to very severe (5). Higher scores indicate worse pain.
2.2.9. Appetite problems.
The Simplified Nutritional Appetite Questionnaire (SNAQ), a 4-item single-domain questionnaire (Wilson et al., 2005), was used to measure a participant’s appetite problems. We reversed a Likert scale in each item, ranging from 1 to 5 with higher scores indicating poor appetite.
2.2.10. HRQoL for mental and physical domains.
The Short-Form Health Survey (SF-12) (Ware Jr et al., 1996) was used to ask about participants’ health status and assessed HRQoL in the past 4 weeks. The SF-12 consists of 12 items that are scored in two dimensions (Maruish. 2012): the mental health and physical health. The physical QoL score includes items on general health perception, physical functioning, reduction in physical activities as compared with the subjectively expected, and pain, whereas the mental QoL score includes questions on general health perception, mood, energy level and reduction in social activities, work ability or general function explained by emotional factors. Higher scores indicate better HRQoL.
2.3. Analysis
Relationships between marijuana use frequency, severity of marijuana-related problems. and HRQoL were analyzed, controlling for mental health symptoms and physical health conditions for the respective outcome measures. Multiple imputations were used due to missing data. We used the structural equation model (SEM) for the analyses. SEM is a multivariate method that combines factor analysis and path analysis, which allows relationships among multiple measures or constructs to be tested simultaneously (Ullman & Bentler, 2012). A latent construct is a factor indicated by multiple indicators (observed measures) and therefore is free of random error. A path analysis allows the evaluation of causal relationships in which an independent variable produces both direct and indirect effects on a dependent variable (Ullman & Bentler, 2012), in our case, we are testing if marijuana use produces direct effects on HRQoL and indirect effects on HRQoL via the marijuana-related problems as a mediator.
The analysis was conducted in three steps. First, a preliminary analysis and Pearson’s r correlation coefficients for all variables were computed and reported. Second, confirmatory factor analysis (CFA) was conducted to assess the associations between latent variables and factors to support the subsequent assessment of the SEM. There are three latent variables in the model. One was marijuana use frequency with two indicators: number of days of marijuana use and number of times marijuana was used per day. The second was mental health symptoms (anxiety, depression, stress, and paranoia). The third construct was physical health conditions, with indicators including sleep disturbance, respiratory function, pain intensity, and appetite. Finally, SEM was performed with SAS version 9.4 PROC PATH by the maximum likelihood estimation.
Model fit was assessed by the chi-square (χ2) test statistic and the values in the following goodness-of-fit indices: comparative fit index (CFI) of equal to or greater than 0.95, root mean square error of approximation (RMSEA) of less than or equal to 0.08, standardized root mean square residual (SRMR) of < 0.09, and Adjusted Goodness of Fit Index (AGFI) of equal to or greater than 0.90, in accordance with the recommendations (Iacobucci, 2010; Kline, 2015).
3. Results
3.1. Participant characteristics
A total of 123 participants comprised of 80.5% males and 19.5% females provided survey data for the present analysis. The average age was 35.0 ±12.4 years old. 28.5% of them were Hispanics, followed by African Americans (27.6%), whites (23.6%), and other races/ethnicities (20.3%) (Table 1). Among marijuana-related problems (measured by the MPS), the most common problems cited included financial difficulties (39.0%), procrastination (38.2%), and poor relationships with family (36.6%) and partner (36.6%).
3.2. Pearson’s correlation and CFA
Table 3 shows the intercorrelations between observed variables. Results revealed that variables were correlated with one another in a way that supported the hypothesized interrelationships among the factors. The HRQoL (SF-12) mental health domain score was correlated with days of marijuana use (r = −0.40, p < 0.001), severity of marijuana-related problems (r = −0.20, p < 0.05), anxiety (r = −0.63, p < 0.001), depression (r = −0.57, p < 0.001), stress (r = −0.54, p < 0.001), and paranoia (r = −0.40, p < 0.001). The HRQoL (SF-12) physical domain score was correlated with daily use frequency (r = −0.20, p < 0.05), severity of marijuana-related problems (r = −0.21, p < 0.05), and respiratory function (r = −0.22, p < 0.05). Moreover, days of use and daily use frequency were associated with each other so that we combined both as a latent variable named “marijuana use frequency.” Anxiety, depression, stress, and paranoia had some significant relationships with each other, so the four were combined as a latent variable named “mental health symptoms.” Sleep disturbance, respiratory function, pain intensity, and appetite problems had some significant relationships with each other, so the four were combined as a latent variable named “physical health conditions.”
Table 3.
The intercorrelations among variables
| Mental health | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. |
|---|---|---|---|---|---|---|---|---|
| 1. Days of use | 1 | 0.69*** | 0.20* | 0.14 | 0.18 | 0.16 | 0.08 | −0.40*** |
| 2. Daily use frequency | 1 | 0.27** | 0.24** | 0.27** | 0.22* | 0.14 | −0.16 | |
| 3. Severity of marijuana-related problems | 1 | 0.30*** | 0.32*** | 0.29** | 0.18* | −0.20* | ||
| 4. Anxiety | 1 | 0.80*** | 0.52*** | 0.46*** | −0.63*** | |||
| 5. Depression | 1 | 0.50*** | 0.34*** | −0.57*** | ||||
| 6. Stress | 1 | 0.38*** | −0.54*** | |||||
| 7. Paranoia | 1 | −0.40*** | ||||||
| 8. SF-12 mental health domain | 1 | |||||||
| Physical health | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. |
| 1. Days of use | 1 | 0.69*** | 0.20* | 0.26** | 0.13 | 0.21* | 0.27** | −0.14 |
| 2. Daily use frequency | 1 | 0.27** | 0.28** | 0.22* | 0.16 | 0.24** | −0.20* | |
| 3. Severity of marijuana-related problems | 1 | 0.22* | 0.19* | 0.09 | 0.27** | −0.21* | ||
| 4. Sleep disturbance | 1 | 0.34*** | 0.35*** | 0.11 | −0.17 | |||
| 5. Respiratory function | 1 | 0.13 | 0.12 | −0.22* | ||||
| 6. Pain intensity | 1 | 0.12 | −0.16 | |||||
| 7. Appetite problems | 1 | −0.18 | ||||||
| 8. SF-12 physical health domain | 1 |
Note. Days of use and Daily use frequency for marijuana use present the mean category.
P < 0.05
P < 0.01
P < 0.001
The results of CFA revealed that both measurement models, one with marijuana use frequency and mental health symptoms and the other with marijuana use frequency and physical health conditions, had adequate fit with the data (mental: χ2 = 6.60, p = 0.580, CFI = 1.00, RMSEA = 0.00, SRMR = 0.03, AGFI = 0.95; physical: χ2 = 10.12, p = 0.257, CFI = 0.98, RMSEA = 0.05, SRMR = 0.06, AGFI= 0.93).
3.3. Structural equation modeling
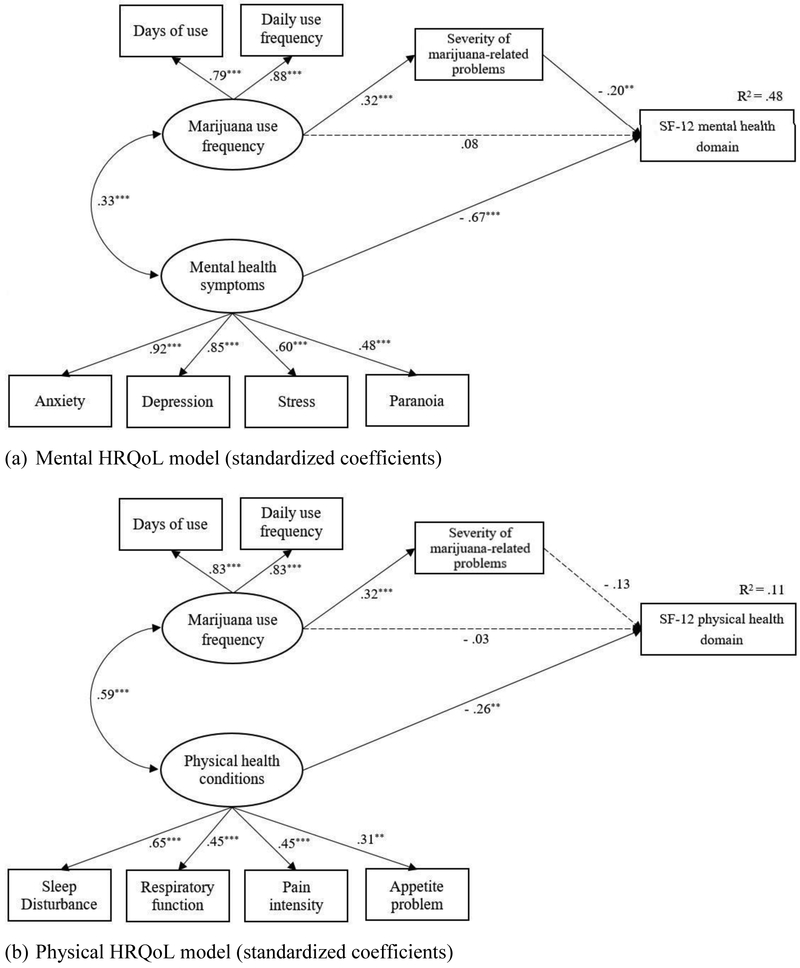
The model of mental HRQoL (Fig. 1a) had a good fit (χ2 = 27.64, p = 0.052, CFI = 0.97, RMSEA = 0.07, SRMR = 0.08, AGFI = 0.90) and accounted for 48% of the variance on the mental health domain score. Marijuana use frequency was significantly related to greater severity of perceived problems (H1c: β = 0.32, p < 0.001), which was associated with poorer HRQoL for mental health (H2a: β = −0.20, p < 0.01). Mental health symptoms were positively associated with marijuana use frequency and negatively linked to HRQoL for mental domain (H3a: β = −0.67, p < 0.001). Among mental health symptoms, anxiety was the most significantly related observed indicator (β = 0.92, p < 0.001), followed by depression (β = 0.85, p < 0.001).
Fig. 1.
Relationships between marijuana use, severity of marijuana-related problems, and HRQoL for mental and physical health domains, controlling for the effects of mental health syptoms and physical health conditions.
* P < 0.05 ** P < 0.01 *** P < 0.00.
Note. The dotted line presents a non-significant relationship.
The model of physical HRQoL (Fig. 1b) was a good fit (χ2 = 21.70, p = 0.203, CFI = 0.97, RMSEA = 0.05, SRMR = 0.06, AGFI = 0.91) and accounted for 11% of the variance on the physical health domain score. The results revealed that marijuana use frequency was significantly related to more severe marijuana problems, but was not significantly associated with HRQoL for physical health (H2b: β = −0.13, p > 0.05). Physical health conditions were positively associated with marijuana use frequency and negatively affected HRQoL for physical domain (H3b: β = −0.26, p < 0.01). Among physical health conditions, sleep disturbance was the most significantly related observed indicator (β = 0.65, p < 0.001), followed by respiratory function (β = 0.45, p < 0.001) and pain intensity (β = 0.45, p < 0.001).
4. Discussion
The study findings are mostly consistent with our hypotheses. Using SEM to examine the relationships between marijuana use frequency, severity of marijuana-related problems, and the physical and mental HRQoL domains, separately, we found that marijuana use frequency was positively associated with severity of marijuana-related problems, which in turn had negative effects on mental HRQoL but non-significant relationship with physical HRQoL. The relationship between marijuana use frequency and either mental or physical HRQoL domains was not significant. Overall, the hypothesized model explained 48% of the variance on the mental HRQoL measure, while it explained only 11% of the variance on the physical HRQoL.
A prior study reported an effect of marijuana use frequency on mental HRQoL but not physical HRQoL (Cougle et al., 2015). However, our study did not support the direct association between marijuana use frequency and either mental HRQoL or physical HRQoL. Instead, we found that marijuana use frequency was associated with severity of marijuana-related problems, which affected mental HRQoL. This finding suggests that individuals who frequently use marijuana subsequently had more marijuana-related problems, and this relationship further affected their mental HRQoL. The present study results suggest a new insight that reducing problems associated with marijuana use may be an important clinical target for patients to improve their HRQoL and attain better treatment outcomes. Our findings suggest that reductions in marijuana use alone may not affect mental health-related quality of life if perceived problems are still active.
Based on the participants’ responses, the most common marijuana-related problems included financial difficulties, procrastination, and poor relationships with family or partner. These problems may more directly affect mental health and have less impact on physical health-related quality of life. The primary problems reported in this study were similar (but not identical) to those observed in prior studies among college students (e.g. procrastination, reduced productivity, and memory loss) (Buckner et al., 2010). Marijuana-related problems may be diverse among adolescent and adult populations, warranting more research to clarify their relationships with HRQoL.
The hypothesis that mental health symptoms was negatively associated with mental HRQoL was supported by the present study. Prior research demonstrated similar findings that marijuana use was associated with poorer mental HRQoL among patients with anxiety and depression who were already at risk for low mental HRQoL (Aspis et al., 2015; Lev-Ran et al., 2012). Our study has found that anxiety and depression were significant mental health symptoms affecting mental HRQoL. Additionally, our study findings suggest that stress and paranoia are also important mental health symptoms among marijuana users, but these symptoms have not been well examined in prior marijuana-focused studies. More research regarding stress and paranoia as well as other mental health symptoms are needed to further examine their relationship to mental HRQoL among marijuana users.
It is not surprising that the study also showed that severity of physical health conditions was negatively associated with physical HRQoL. A positive relationship between marijuana use and poor physical health conditions was found in this study, which is consistent with prior studies (Budney and Hughes, 2006; Hancox et al., 2009; Ribeiro and Ind, 2016; Zvolensky et al., 2011). In the past, there has been limited research to evaluate the relationship between physical health problems and physical HRQoL among marijuana users. In the present study, we found that marijuana users who reported these physical symptoms or conditions had poor HRQoL for physical domain. It is worth noting that sleep disturbance and respiratory function were two of the greatest health problem contributors to physical HRQoL as indicated by high factor loadings on physical health conditions. Nevertheless, our study findings reveal that neither the marijuana use frequency nor the marijuana-related problems were significantly associated with physical HRQoL domain. A prior longitudinal study of stimulant users reported similar results, suggesting that reductions in use over time contributed to only minor improvements in physical HRQoL (Borders et al., 2009). Still, given the limited research examining marijuana use and physical HRQoL, additional research efforts are needed to shed light on relevant physical health problems in relation to marijuana use and HRQoL.
There were several limitations in the present study. First, the causal relationships between marijuana use frequency, severity of marijuana-related problems, and mental and physical HRQoL cannot be determined because the study is based on data from a cross-sectional survey. Longitudinal studies would be needed to reveal temporal relationships between marijuana use frequency and mental health problems and to confirm the findings. Second, selection biases might exist because this study involved a cross-sectional survey of participants who were recruited by flyers and advertisements. Third, functional assessments were collected by self-report, without verification by objective measurements. However, scales used had been tested in other studies with good validity and reliability. Also, past-month marijuana use patterns were based on participants’ self-report, which may be influenced by recall bias. Finally, the sample size was too small to investigate more complex relationships between variables using additional potential constructs and covariates (e.g., use of other substances).
Despite these limitations, this study provides better understanding of the relationships between marijuana use frequency, severity of problems related to marijuana use, and HRQoL, controlling for mental and physical symptoms. Our findings suggest that to improve marijuana users’ HRQoL, treatment should incorporate interventions that address not only marijuana use reduction but also problems caused by marijuana use that may take additional time to address even after use levels have been reduced. For example, interventions could be designed to enhance and optimize skills related to time management, coping with stress, and improving family relationships. Also, severity of marijuana-related problems could be used as an indicator for efficacy of treatments (Babor, 2004), as individuals with more severe problems related to marijuana use are generally more likely to seek treatment for marijuana use (Buckner et al., 2010). Additionally, our findings show that more frequent marijuana users have concurrent mental health symptoms and worse physical health conditions that may negatively impact their HRQoL. Integrated treatment models simultaneously addressing marijuana use and mental health symptoms (e.g., anxiety and depression) have been recommended (National Institute on Drug Abuse, 2018). In conclusion, this study extends previous research and improves the understanding of the relationships among marijuana use, marijuana-related problems, and HRQoL.
Table 2.
Demographics of participants and descriptive information in variables (n = 123)
| Mean ± SD/ % | |
|---|---|
| Age | 35.0 ± 12.4 |
| Gender | |
| Male | 80.5 |
| Female | 19.5 |
| Race/ethnicity | |
| African American | 27.6 |
| Asian | 4.1 |
| Hispanic | 28.5 |
| White | 23.6 |
| Multi-race/Multi-ethnic | 13.8 |
| Other | 2.4 |
| Educational degree | |
| High school or lower | 76.4 |
| College degree or higher | 23.6 |
| Employment status | |
| Employed | 25.2 |
| Unemployed | 74.8 |
| Marijuana use | |
| Days of use | 1.2 ± 1.9 |
| Daily use frequency | 1.1 ± 1.5 |
| Severity of marijuana-related problems | 5.1 ± 5.4 |
| Mental health symptoms | |
| Anxiety | 6.5 ± 4.3 |
| Depression | 6.1 ± 4.2 |
| Stress | 6.2 ± 3.1 |
| Paranoia | 22.4 ± 25.4 |
| Physical health conditions | |
| Sleep disturbance | 52.4 ± 10.3 |
| Respiratory function | 26.0 ± 28.1 |
| Pain intensity | 41.7 ± 11.0 |
| Appetite problems | 8.6 ± 2.8 |
| HRQoL | |
| SF-12 mental health domain | 46.1 ± 10.4 |
| SF-12 physical health domain | 48.4 ± 8.8 |
Highlights.
Severity of marijuana-related problems may play a mediating role between marijuana use and mental HRQoL domain.
Marijuana use was positively associated with mental health symptoms and physical health conditions.
Both mental health symptoms and physical health conditions were negatively associated to mental and physical domains of HRQoL, respectively.
Reduction of marijuana-related problems and mitigation of mental and physical health problems may improve HRQoL among marijuana users.
Acknowledgment
We appreciate the staff at each participating treatment facility in Los Angeles, California: Tarzana Treatment Centers, Los Angeles Centers for Alcohol and Drug Abuse (LA CADA), SHIELDS for Families, Antelope Valley Rehabilitation Centers, UCLA Dual Diagnosis Intensive Outpatient Program, Phoenix House.
Funding sources
This study was supported by the National Institute on Drug Abuse (Dr. Hser and Dr. Mooney, grant numbers DA042280), and in part additionally supported by the Ministry of Science and Technology, Taiwan (Jung-Yu Liao, grant number 106-2917-I-003-005.
Footnotes
Declaration of interest
All authors declare no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aspis I, Feingold D, Weiser M, Rehm J, Shoval G, Lev-Ran S, 2015. Cannabis use and mental health-related quality of life among individuals with depressive disorders. Psychiatry Res. 230(2), 341–349. [DOI] [PubMed] [Google Scholar]
- Babor TF, 2004. Brief treatments for cannabis dependence: findings from a randomized multisite trial. J. Consult. Clin. Psychol 72(3), 455. [DOI] [PubMed] [Google Scholar]
- Becker MP, Collins PF, Lim KO, Muetzel RL, & Luciana M, 2015. Longitudinal changes in white matter microstructure after heavy cannabis use. Dev. Cogn. Neurosci 16, 23–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjelland I, Dahl AA, Haug TT, Neckelmann D, 2002. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J. Psychosom. Res 52(2), 69–77. [DOI] [PubMed] [Google Scholar]
- Borders TF, Booth BM, Falck RS, Leukefeld C, Wang J, Carlson RG, 2009. Longitudinal changes in drug use severity and physical health-related quality of life among untreated stimulant users. Addic. Behav 34(11), 959–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brezing CA, Choi CJ, Pavlicova M, Brooks D, Mahony AL, Mariani JJ, Levin FR, 2018. Abstinence and reduced frequency of use are associated with improvements in quality of life among treatment-seekers with cannabis use disorder. Am. J. Addict 27(2), 101–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Ecker AH, Cohen AS, 2010. Mental health problems and interest in marijuana treatment among marijuana-using college students. Addic. Behav 35(9), 826–833. [DOI] [PubMed] [Google Scholar]
- Budney AJ, Hughes JR, 2006. The cannabis withdrawal syndrome. Curr. Opin. Psychiatr 19(3), 233–238. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Yu L, Moul DE, Germain A, Stover A, Dodds NE, Johnston KL, Shablesky-Cade MA, Pilkonis PA, 2010. Development and validation of patient-reported outcome measures for sleep disturbance and sleep-related impairments. Sleep 33(6), 781–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2017. 2016 National survey on drug use and health: detailed tables. Substance Abuse and Mental Health Services Administration, Rockville, MD: https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2016/NSDUH-DetTabs-2016.pdf. (accessed 20 June 2018) [Google Scholar]
- Cohen NL, Heinz AJ, Ilgen M, Bonn-Miller MO, 2016. Pain, cannabis species, and cannabis use disorders. J. Stud. Alcohol Drugs 77(3), 515–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R, 1994. Perceived stress scale. http://www.mindgarden.com/documents/PerceivedStressScale.pdf. (accessed 14 September 2017) [Google Scholar]
- Cohen S, Williamson G, 1988. Perceived stress in a probability sample of the United States, in: Spacapan S, Oskamp S (Eds.), The Social Psychology of Health. SAGE, Newbury Park, CA, pp. 31–68. [Google Scholar]
- Cougle JR, Hakes JK, Macatee RJ, Chavarria J, Zvolensky MJ, 2015. Quality of life and risk of psychiatric disorders among regular users of alcohol, nicotine, and cannabis: an analysis of the National Epidemiological Survey on Alcohol and Related Conditions (NESARC). J. Psychiatr. Res 66, 135–141. [DOI] [PubMed] [Google Scholar]
- Cousijn J, Wiers RW, Ridderinkhof KR, van den Brink W, Veltman DJ, Goudriaan AE, 2014. Effect of baseline cannabis use and working-memory network function on changes in cannabis use in heavy cannabis users: A prospective fMRI study. Hum. Brain Mapp 35(5), 2470–2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldenberg M, IsHak WW, Danovitch I, 2017. Quality of life and recreational cannabis use. Am. J. Addict 26(1), 8–25. [DOI] [PubMed] [Google Scholar]
- Hall W, 2015. What has research over the past two decades revealed about the adverse health effects of recreational cannabis use? Addiction 110(1), 19–35. [DOI] [PubMed] [Google Scholar]
- Hancox RJ, Poulton R, Ely M, Welch D, Taylor DR, McLachlan CR, Greene JM, Moffitt TE, Caspi A, Sears MR, 2009. Effects of cannabis on lung function: a population-based cohort study. Eur. Respir. J 35(1), 42–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, 2018. US epidemiology of cannabis use and associated problems. Neuropsychopharmacology 43(1), 195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hser YI, Mooney LJ, Huang D, Zhu Y, Tomko RL, McClure E, Chou CP, Gray KM, 2017. Reductions in cannabis use are associated with improvements in anxiety, depression, and sleep quality, but not quality of life. J. Subst. Abus. Treat 81, 53–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacobucci D, 2010. Structural equations modeling: Fit indices, sample size, and advanced topics. J. Consum. Psychol 20(1), 90–98. [Google Scholar]
- Jones PW 2009. The St George's respiratory questionnaire manual (version 2.3). http://www.healthstatus.sgul.ac.uk/SGRQ_download/SGRQ%20Manual%20June%202009.pdf. (accessed 14 April 2018) [Google Scholar]
- Jones PW, Quirk F, Baveystock C, 1991. The St George's respiratory questionnaire. Respir. Med 85, 25–31. [DOI] [PubMed] [Google Scholar]
- Karimi M, Brazier J, 2016. Health, health-related quality of life, and quality of life: what is the difference? Pharmacoeconomics 34(7), 645–649. [DOI] [PubMed] [Google Scholar]
- Ketcherside A, Filbey FM, 2015. Mediating processes between stress and problematic marijuana use. Addict. Behav 45, 113–118. [DOI] [PubMed] [Google Scholar]
- Kline RB, 2015. Principles and practice of structural equation modeling, Fourth edition. Guilford publications, New York. [Google Scholar]
- Lev-Ran S, Le Foll B, McKenzie K, Rehm J, 2012. Cannabis use and mental health-related quality of life among individuals with anxiety disorders. J. Anxiety Disord 26(8), 799–810. [DOI] [PubMed] [Google Scholar]
- Liebregts N, van der Pol P, de Graaf R, van Laar M, van den Brink W, Korf DJ, 2015. Persistence and desistance in heavy cannabis use: the role of identity, agency, and life events. J. Youth Stud 18(5), 617–633. [Google Scholar]
- Maruish ME, 2012. User’s manual for the SF-12v2 Health Survey, Third edition. QualityMetric Incorporated, Rhode Island. [Google Scholar]
- Meil WM, LaPorte DJ, Mills JA, Sesti A, Collins SM, Stiver AG, 2016. Sensation seeking and executive deficits in relation to alcohol, tobacco, and marijuana use frequency among university students: Value of ecologically based measures. Addic. Behav 62, 135–144. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse (NIDA), revised June 2018. Marijuana. https://www.drugabuse.gov/publications/research-reports/marijuana (accessed 4 August 2018).
- Passarotti A, Crane NA, Hedeker D, Mermelstein RJ, 2015. Longitudinal trajectories of marijuana use from adolescence to young adulthood. Addic. Behav 45, 301–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PROMIS Health Organization and PROMIS Cooperative Group. 2016. PROMIS pain intensity instrument, https://cde.drugabuse.gov/instrument/0a481bfb-a5e6-3c84-e050-bb89ad43314d (accessed 4 March 2017). [Google Scholar]
- Ribeiro LI, Ind PW, 2016. Effect of cannabis smoking on lung function and respiratory symptoms: A structured literature review. npj Prim. Care Respir. Med 26, 16071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronald A, Sieradzka D, Cardno AG, Haworth CM, McGuire P, Freeman D, 2013. Characterization of psychotic experiences in adolescence using the specific psychotic experiences questionnaire: findings from a study of 5000 16-year-old twins. Schizophr. Bull 40(4), 868–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith KW, Larson MJ, 2003. Quality of life assessments by adult substance abusers receiving publicly funded treatment in Massachusetts. Am. J. Drug Alcohol Abuse 29(2), 323–335. [DOI] [PubMed] [Google Scholar]
- Stephens RS, Roffman RA, Simpson EE, 1994. Treating adult marijuana dependence: a test of the relapse prevention model. J. Consult. Clin. Psychol 62(1), 92. [DOI] [PubMed] [Google Scholar]
- Ullman JB, & Bentler PM 2012. Structural equation modeling, in: Irving BW (Eds), Handbook of Psychology, Second Edition. John Wiley & Sons, Inc., New Jersey, pp. 661–690. 10.1002/9781118133880.hop202023 (Accessd 4 June 2017). [DOI] [Google Scholar]
- United Nations Office on Drugs Crime, 2017. World drug report 2017, Booklet 2 Global overview of drug demand and supply. United Nations Publications, Austria. [Google Scholar]
- Volkow ND, Baler RD, Compton WM, Weiss SR, 2014. Adverse health effects of marijuana use. N. Engl. J. Med 370(23), 2219–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware JE Jr, Kosinski M, Keller SD, 1996. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med. Care 34(3), 220–233. [DOI] [PubMed] [Google Scholar]
- Wilson MMG, Thomas DR, Rubenstein LZ, Chibnall JT, Anderson S, Baxi A, Diebold MR, Morley JE, 2005. Appetite assessment: Simple appetite questionnaire predicts weight loss in community-dwelling adults and nursing home residents. Am. J. Clin. Nutr 82(5), 1074–1081. [DOI] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP, 1983. The hospital anxiety and depression scale. Acta Psychiatr. Scand 67(6), 361–370. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Cougle JR, Bonn-Miller MO, Norberg MM, Johnson K, Kosiba J, Asmundson GJ, 2011. Chronic pain and marijuana use among a nationally representative sample of adults. Am. J. Addict 20(6), 538–542. [DOI] [PubMed] [Google Scholar]