Abstract
Internalized stigma undermines health among people diagnosed with HIV and other sexually transmitted infections (STI), yet limited research has examined how internalized stigma develops. Black gay and bisexual men (n = 151) reported their race and sexual orientation internalized stigma once before HIV/STI diagnosis and their HIV/STI internalized stigma monthly for 1 year after HIV/STI diagnosis. Multilevel analyses demonstrated that race and sexual orientation internalized stigma before diagnosis were associated with greater HIV/STI internalized stigma after diagnosis. More research is needed to understand how internalized stigma develops, including within the context of other identities and broader environmental characteristics to inform intervention efforts.
Keywords: African American, HIV, LGBTQ, sexually transmitted infection, stigma
Introduction
Internalized stigma undermines mental, behavioral, and physical health outcomes among people living with a wide range of socially devalued identities (Herek et al., 2009; Lee et al., 2002; Livingston and Boyd, 2010; Mak et al., 2007). Internalized stigma involves endorsing negative beliefs and feelings about people living with a stigmatized identity and applying those beliefs and feelings to the self (Earnshaw and Chaudoir, 2009; Link, 1987). Both people living with HIV and other sexually transmitted infections (STIs), such as gonorrhea, chlamydia, and syphilis, internalize stigma associated with HIV/STI (East et al., 2011; Lee et al., 2002; Newton and Mccabe, 2008). HIV internalized stigma is associated with greater depressive symptoms, longer medical care gaps, and lower likelihoods of medication initiation and adherence (Earnshaw et al., 2013c; Logie et al., 2018; Turan et al., 2016). Although internalized stigma is less studied in the context of other STIs, evidence suggests that STI stigma similarly undermines mental health and treatment-seeking behavior (Hood and Friedman, 2011; Lichtenstein, 2003).
Research that identifies risk factors for HIV/STI internalized stigma can inform intervention efforts to address HIV/STI internalized stigma and ultimately enhance health outcomes among people diagnosed with HIV/STI. The weeks and months after an HIV/STI diagnosis are often critical windows for engagement in care and initiation of treatment (Workowski and Bolan, 2015), and emerging evidence suggests that HIV/STI internalized stigma is heightened immediately after acquiring an HIV/STI diagnosis (Eaton et al., 2018; Tsai et al., 2013). Yet, few studies have focused on internalized stigma among people who have recently been diagnosed with HIV/STI. This study is guided by intersectionality theory, which highlights that people live with multiple interconnected identities representing both marginalization and privilege (Cole, 2009; Crenshaw, 1991; hooks, 1990; Jones and McEwen, 2000; Rosenthal, 2016), and examines the extent to which internalized stigma associated with identities before HIV/STI diagnosis (i.e. race, sexual orientation) are associated with HIV/STI internalized stigma in the year following HIV/STI diagnosis. This study focuses on Black gay and bisexual men, as well as other men who have sex with men, which is the group most affected by HIV and other STIs in the United States (Centers for Disease Control and Prevention, 2017a, 2017b).
Stigmatized identity development
Most Black gay and bisexual men living with HIV/STI are diagnosed during adolescence and/or adulthood, and therefore gain the stigmatized identity of HIV/STI during their lives. For example, 98 percent of individuals newly diagnosed with HIV in the United States in 2016 acquired HIV through sexual contact and/or drug use during adolescence or adulthood, and only 2 percent were born with HIV (Centers for Disease Control and Prevention, 2017a). Similarly, people living with many other stigmatized health conditions and identities (e.g. cancer, substance use disorder, tuberculosis, incarceration, sex work) gain their stigmatized identity after birth. Early stigma theory acknowledged variability in the course of stigma, including that the nature of stigma may change over time (Jones et al., 1984). Yet, limited research to date has been conducted on the process of developing an identity associated with a stigmatized health condition such as HIV/STI.
Theory and research from the literatures on racial and sexual orientation identity development provide insight into how stigma becomes internalized. Much of this work suggests that racial and sexual orientation identity occurs in stages, with individuals at greater risk of internalizing stigma at the beginning stages (Cass, 1984; Vandiver, 2001; Worrell et al., 2001). Individuals absorb stigma from the world around them, including stereotypes (i.e. group-based beliefs) and prejudice (i.e. negative feelings and attitudes) about their stigmatized identity. Knowledge of stereotypes and awareness of prejudice may come from media representations such as television shows; comments from others such as family, friends, and co-workers; as well as other sources (Quinn and Earnshaw, 2011). Early on in the formation of a stigmatized identity, individuals apply stereotypes and prejudice to the self and others with the stigmatized identity (Cass, 1984; Vandiver, 2001; Worrell et al., 2001). With time, individuals may move through additional stages of identity formation involving the development of more positive self-perceptions and the reduction of internalized stigma. There is some evidence to suggest that this process may generalize to developing a stigmatized identity associated with a health condition. For example, Black gay and bisexual men who endorse greater prejudice toward people living with HIV/STI before their HIV/STI diagnosis report greater HIV/STI internalized stigma after their HIV/STI diagnosis (Eaton et al., 2018). The process of gaining a new stigmatized identity additionally occurs in the context of an individual’s existing identities, and these existing identities may further influence the development of the stigmatized identity (Jones and McEwen, 2000).
Intersectionality of identities
Intersectionality theory emphasizes that people live with multiple interconnected identities representing both marginalization and privilege (Cole, 2009; Crenshaw, 1991; hooks, 1990; Jones and McEwen, 2000; Rosenthal, 2016). The interconnectedness means that each identity depends on and reflects the other identities, making it impossible to understand one identity without understanding how it relates to other identities (Jones and McEwen, 2000). Prior to being diagnosed with HIV/STI, Black gay and bisexual men have typically formed an identity incorporating their race and sexual orientation, and may have internalized stigma associated with these identities. Indeed, previous research suggests that some Black adolescents and young adults internalize racism (Williams and Williams-Morris, 2000), and that some young lesbian, gay, bisexual, and queer youth internalize sexual orientation stigma (Balaji et al., 2012; Meyer, 2003). Due to the interconnectedness of identities, the development of HIV/STI internalized stigma may be shaped, or influenced, by existing race and/or sexual orientation internalized stigma. Indeed, among Black gay and bisexual men who have been living with HIV, research suggests that experiences of race, sexual orientation, and HIV stigma are interrelated (Bowleg, 2013).
Hypotheses
To date, little known research has examined the process of how stigmatized identities develop after they are gained, including how HIV/STI internalized stigma develops after diagnosis. Guided by intersectionality theory, we hypothesize that race and sexual orientation internalized stigma pre-diagnosis are associated with HIV/STI internalized stigma post-diagnosis. We collapsed across HIV/STI diagnoses given theory and research suggesting that stigma has similar effects across stigmatized health conditions (Earnshaw et al., 2013a; Van Brakel, 2006), but explored whether the effects of race and sexual orientation stigma on HIV/STI internalized stigma were moderated by HIV versus STI diagnosis.
Methods
Procedures and participants
Participants were recruited from a longitudinal study of HIV/STI testing in the Atlanta, GA metropolitan area between April 2014 and February 2016. Participants of this parent study were recruited using online advertisements (e.g. dating apps, Craigslist, BGClive.com) and infield recruitment at gay-identified bars, clubs, parks, and sex parties. In total, 351 Black gay and bisexual men were tested for HIV and 271 were tested for STI (i.e. gonorrhea, chlamydia, syphilis) at four time points over the course of 1 year. Of these, 48 participants were newly diagnosed with HIV and 103 were newly diagnosed with gonorrhea, chlamydia, and/or syphilis. Participants who tested positive for HIV or STI were invited to participate in this study, wherein they were followed for 1 year postdiagnosis. Participants completed 14 assessments in total using audio computer-assisted self-interview software (ACASI), with one occurring pre-diagnosis, one occurring one week post-diagnosis, and 12 occurring each month post-diagnosis for 1 year. Participants were compensated US$45 for their first assessment, including the pre-diagnosis assessment and HIV/STI testing, and US$25 for each follow-up assessment.
Participants who tested positive for HIV/STI were paired with a project staff member, who helped them to identify and coordinate HIV/STI-related healthcare with a local health department, clinic, or private practice provider that best suited the needs of the participant. Project staff therefore coordinated linkage to participants’ initial treatment appointment. All participants provided written informed consent and all study procedures received ethics approval from the University of Connecticut Institutional Review Board (Protocol #H16-130).
Materials
At the baseline assessment, which occurred prediagnosis, participants self-reported socio-demographic information, depressive symptoms, and internalized race and sexual orientation stigma. Depressive symptoms were controlled for given previous research that suggests that depressive symptoms may play a role in leading to internalized stigma (Pantelic et al., 2015; Takada et al., 2014; Tsai et al., 2013). After the baseline assessment, HIV/STI testing was conducted. During follow-up assessments, which occurred postdiagnosis, participants self-reported internalized HIV/STI stigma.
Socio-demographics and depressive symptoms.
Participants reported their age, education, income, and sexual orientation. In regression analyses, education was dichotomized to represent some college or more (1) versus high school degree or less (0), and income was dichotomized to represent >US$21,000 annually (1) versus. Two dummy variables were used to represent sexual orientation, including bisexual (1) versus all other sexual orientations (0) and heterosexual (1) versus all other sexual orientations (0). Depressive symptoms were measured using the Center for Epidemiologic Studies Short Depression Scale (CESD-10; Andresen et al., 1994). Participants responded to 10 items regarding the frequency with which they experienced several symptoms within the past week, such as “In the past week, I was bothered by things that don’t usually bother me.” Responses were measured on a 4-point scale ranging from less than 1 day (0) to 5–7 days (3). The scale had adequate internal reliability (Cronbach’s alpha = 0.81), and was summed to create a composite score. A cutoff for screening positive on depressive symptomology was created (score >10).
Internalized race stigma.
Internalized race stigma was measured using items adapted from the Nadanolitization Scale (Taylor and Grundy, 1996). Participants responded to six items describing their feelings about their race, such as “I sometimes struggle with negative feelings about my race” and “I am proud of my race.” Responses were measured on a 6-point scale ranging from strongly disagree (1) to strongly agree (6). Positively worded items were reverse-scored so that higher scores indicated greater internalized stigma. Preliminary analyses suggested that the scale had poor internal reliability. The positively worded items were deleted from the scale, resulting in a three-item measure with acceptable internal reliability (Cronbach’s alpha = 0.70). These items were averaged to create a composite score.
Internalized sexual orientation stigma.
Internalized sexual orientation stigma was measured using items adapted from the Revised Internalized Homophobia Scale (Herek et al., 2009). Participants responded to four items describing their feelings about being attracted to men, such as “I try not to be attracted to men in general.” Responses were measured on a 6-point scale ranging from strongly disagree (1) to strongly agree (6). The scale had acceptable internal reliability (Cronbach’s alpha = 0.80), and items were averaged to create a composite score.
Internalized HIV/STI stigma.
Internalized HIV/STI stigma was measured using items from the HIV Stigma Mechanisms Scale (Earnshaw et al., 2013c), which were adapted for the target population based on formative work. Participants responded to four items describing their feelings about screening positive for HIV or another STI. Responses were measured on a six-point scale ranging from strongly disagree (1) to strongly agree (6). One positively worded item was reverse-scored so that higher scores indicated greater internalized stigma (“Screening positive for HIV (an STI) doesn’t really bother me”). Preliminary analyses suggested that the internal reliability could be strengthened by deleting this positively worded item. The resulting three-item measure had acceptable internal reliability (Cronbach’s alpha = 0.68), and items were averaged to create a composite score. Items included: “Screening positive for HIV (an STI) makes me feel like I’m a bad person,” “I feel I’m not as good as others because I screened positive for HIV (an STI),” and “I feel ashamed of having screened positive for HIV (an STI).”
Data analyses
All analyses were conducted in IBM SPSS Statistics version 24.0. Participant baseline characteristics, including socio-demographics, HIV/STI diagnosis, depressive symptoms, and race and sexual orientation internalized stigma were analyzed using descriptive analyses. Next, multilevel models (i.e. general linear mixed models) were conducted wherein repeated assessments were nested within participants (Hoffman, 2015). First, the effect of time (i.e. weeks since diagnosis) was modeled to describe within-person change in HIV/STI internalized stigma over the first year post-diagnosis. In addition, a scatterplot of the association between time and HIV/STI internalized stigma with a fitted LOESS curve was created to visualize changes in HIV/STI internalized stigma scores over the first year post-diagnosis. Second, race internalized stigma, sexual orientation internalized stigma, and HIV/STI diagnosis were examined as time-invariant predictors of HIV/STI internalized stigma in three separate multilevel models. Each model included one of these variables (race internalized stigma, sexual orientation internalized stigma, or HIV/STI diagnosis) as a predictor of the intercept of HIV/STI internalized stigma (i.e. HIV/STI internalized stigma 1 week after diagnosis) as well as moderators of the linear and quadratic effects (i.e. time squared) of time. Third, control variables were added and a multivariable analysis was performed including all variables as predictors that were significantly associated with HIV/STI internalized stigma in previous analyses. Finally, a moderation analysis was conducted to explore possible interactions between HIV/STI diagnosis, race internalized stigma, and/or sexual orientation internalized stigma. Continuous variables were centered for these analyses, and products were created to represent interactions.
Results
Participant characteristics at baseline are included in Table 1. The 151 participants ranged in age from 18 to 53 years (M(SD) = 26.45(6.39)). Most participants (70.2%) had some college education or more, including a college degree and some graduate education. Approximately half (47.7%) of participants earned less than US$10,000 per year, and 15.8 percent earned greater than US$31,000 per year. Regarding sexual orientation, 40.4 percent of participants identified as gay or homosexual, 39.1 percent identified as bisexual, 12.6 percent identified as heterosexual, and 7.3 percent identified as same gender loving. Most participants (68.2%) were diagnosed with an STI other than HIV, with the remainder (31.8%) diagnosed with HIV. Average depressive symptoms were 8.64 (SD = 6.19), and 31.3 percent (n = 47) of participants met the cutoff for depressive symptomatology. Average race internalized stigma was 2.07 (SD = 1.29) and average sexual orientation stigma was 2.66 (SD = 1.45), indicating low internalized stigma among participants overall.
Table 1.
Participant characteristics at baseline (n = 151).
| M (SD) | % (n) | |
|---|---|---|
| Socio-demographic characteristics | ||
| Age | 26.45 (6.39) | |
| Education | ||
| High-school degree or less | 29.8 (45) | |
| Some college | 47.7 (72) | |
| College degree or more | 22.5 (34) | |
| Income | ||
| <US$10,000 | 47.7 (72) | |
| US$11,000–30,000 | 36.4 (55) | |
| >US$31,000 | 15.8 (24) | |
| Sexual orientation | ||
| Gay/homosexual | 40.4 (61) | |
| Bisexual | 39.1 (59) | |
| Heterosexual | 12.6 (19) | |
| Same gender loving | 7.3 (11) | |
| Diagnosis | ||
| STI | 68.2 (103) | |
| HIV | 31.8 (48) | |
| Depressive symptoms | 8.64 (6.19) | |
| Intersecting internalized stigma | ||
| Race | 2.07 (1.29) | |
| Sexual orientation | 2.66 (1.45) | |
Percentages may not total to 100 due to missing data; age ranged 18–53; depressive symptoms ranged 0–27; internalized race and sexual orientation stigma ranged 1–6.
The effect of time was modeled to describe within-person change in HIV/STI internalized stigma over the first year post-diagnosis. The best-fitting model included the effects of time and time squared, with the intercept included as a random effect. The intercept indicated that participants scored an average of 2.65 (standard error (SE) = 0.11; p < 0.01) on HIV/STI internalized stigma 1 week after diagnosis. The effect of time (B(SE) = −0.03(0.01), p < 0.01) and time squared (B(SE) = 0.01(0.01), p < 0.01) were statistically significant, demonstrating that HIV/STI internalized stigma proceeded to decrease over the first year post-diagnosis and that this decrease decelerated over time. The scatterplot of the association between time and HIV/STI internalized stigma over the first year after diagnosis including the LOESS curve is included in Figure 1.
Figure 1.
Scatterplot of association between time and HIV/STI internalized stigma in first year after diagnosis, with fitted LOESS curve.
Race internalized stigma, sexual orientation internalized stigma, and HIV/STI diagnosis were included as time-invariant predictors of HIV/STI internalized stigma in three separate multilevel models. Race internalized stigma (B(SE) = 0.33(0.08), p < 0.01) and sexual orientation internalized stigma (B(SE) = 0.17(0.07), p < 0.01) were statistically significant predictors of the intercept of HIV/STI internalized stigma, indicating that participants who had higher race or sexual orientation internalized stigma before HIV/STI diagnosis had higher HIV/STI internalized stigma immediately after diagnosis. HIV/STI diagnosis did not predict the intercept of HIV/STI internalized stigma, suggesting that participants with HIV and STI diagnoses had similar levels of HIV/STI internalized stigma immediately after HIV/STI diagnosis. Neither race internalized stigma, sexual orientation internalized stigma, nor HIV/STI diagnosis moderated the linear or quadratic effects of time on HIV/STI internalized stigma, indicating that the rate of change in HIV/STI internalized stigma over the first year post-diagnosis was not affected by these characteristics.
A multivariable model was conducted including all statistically significant predictors of HIV/STI internalized stigma (Table 2). Education (B(SE) = −0.52(0.22), p = 0.02) and depressive symptomatology (B(SE) = 0.33(0.08), p < 0.01) were the only participant characteristics at baseline that were associated with HIV/STI internalized stigma, and so were included in the analysis. In the multivariable model, the linear and quadratic effects of time remained associated with HIV/STI internalized stigma. In addition, race and sexual orientation internalized stigma remained associated with HIV/STI internalized stigma. Depressive symptomatology was associated with HIV/STI internalized stigma, indicating that participants who had depressive symptomatology before HIV/STI diagnosis reported more HIV/STI internalized stigma after diagnosis. Education became marginally statistically significantly associated with HIV/STI internalized stigma after controlling for the effects of the other variables.
Table 2.
Predictors of HIV/STI internalized stigma in first year after diagnosis.
| B | SE | p value | |
|---|---|---|---|
| Intercept | 2.66 | 0.20 | <0.01 |
| Time | −0.03 | 0.01 | <0.01 |
| Time*Time | 0.01 | 0.01 | <0.01 |
| Race internalized stigma | 0.21 | 0.07 | <0.01 |
| Sexual orientation internalized stigma | 0.11 | 0.06 | 0.05 |
| Education | −0.33 | 0.17 | 0.06 |
| Depressive symptomatology | 0.03 | 0.01 | 0.05 |
Race internalized stigma and sexual orientation internalized stigma were centered. Education (0 = high school or less, 1 = some college or more) and depressive symptomatology (0 = no depressive symptomatology, 1 = depressive symptomatology) were dummy coded. Other socio-demographic characteristics and HIV/STI diagnosis were not associated with HIV/STI internalized stigma in preliminary analyses.
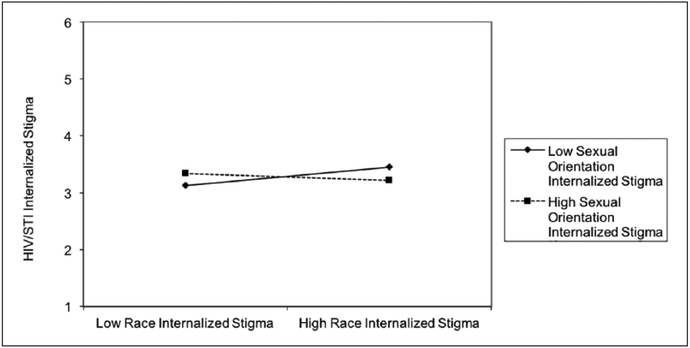
The moderation analysis included the same variables as the multivariable analysis, as well as two-way interactions between race internalized stigma with sexual orientation internalized stigma, race internalized stigma with HIV/STI diagnosis, and sexual orientation internalized stigma with HIV/STI diagnosis, and a three-way interaction between race internalized stigma, sexual orientation internalized stigma, and HIV/STI diagnosis. The two-way interaction between race internalized stigma with sexual orientation internalized stigma was approaching statistical significance (B(SE) = −0.09(0.05), p = 0.08). All other interaction terms were nonstatistically significant (ps > 0.38). Figure 2 includes a graph of the interaction of the effect of race and sexual orientation internalized stigma on HIV/STI internalized stigma. Post hoc tests were performed to test the association between race internalized stigma and HIV/STI internalized stigma among participants with below average (i.e. below the mean) and above average (i.e. above the mean) sexual orientation internalized stigma. Among participants with below average sexual orientation internalized stigma, greater race internalized stigma was associated with greater HIV/STI internalized stigma (B(SE) = 0.33(0.09), p < 0.001). Yet, among participants with above average sexual orientation internalized stigma, race internalized stigma was not associated with greater HIV/STI internalized stigma (B(SE) = 0.10(0.09), p = 0.28).
Figure 2.
Interaction between effect of race and sexual orientation internalized stigma on HIV/STI internalized stigma in first year after diagnosis.
Discussion
To date, research on the process of how internalized stigma associated with a health condition develops is very limited. No known quantitative studies have examined the extent to which internalized stigma associated with identities existing before HIV/STI diagnosis is associated with HIV/STI internalized stigma after HIV/STI diagnosis. Previous research guided by intersectionality theory suggests that experiences of race, sexual orientation, and HIV stigma are interrelated among Black gay and bisexual men who have been living with HIV (Bowleg, 2013). Results of this study extend this research and suggest that internalized stigma associated with race, sexual orientation, and HIV/STI stigma are interconnected across the span of HIV/STI diagnosis. More specifically, Black gay and bisexual men who internalized more race and sexual orientation stigma before HIV/STI diagnosis internalized more HIV/STI stigma after HIV/STI diagnosis. These associations were not moderated by HIV/STI diagnosis, suggesting that effects were similar for Black gay and bisexual men diagnosed with HIV versus another STI. Moreover, a marginally significant interaction was found between race and sexual orientation stigma, indicating that the association between race internalized stigma and HIV/STI internalized stigma may be stronger among participants with lower sexual orientation stigma. This may be due to a ceiling effect, wherein race internalized stigma has a smaller effect on HIV/STI internalized stigma among individuals who have internalized sexual orientation to a greater extent. This result should be interpreted with caution, however, given that the interaction was only approaching statistical significance. Future research is needed to replicate this finding and explore its meaning.
This work contributes to understanding of the process of stigmatized identity development. Past theory and research has suggested that internalized stigma stems largely from absorbing stigma, including stereotypes and prejudice, from the world surrounding individuals (Cass, 1984; Quinn and Earnshaw, 2011; Vandiver, 2001; Worrell et al., 2001). Individuals may learn about HIV/STI stereotypes from and observe HIV/STI prejudice in negative media representations of people living with HIV/STI, negative comments from other individuals about people living with HIV/STI, and other sources long before they are diagnosed with HIV/STI. These stereotypes and prejudice may become the foundations of internalized stigma once HIV/STI has been diagnosed. Indeed, recent research has confirmed that Black gay and bisexual men who endorse greater prejudice toward people living with HIV/STI before they are diagnosed with HIV/STI internalize greater HIV/STI stigma after they are diagnosed (Eaton et al., 2018).
Yet, these results highlight an additional risk factor for internalized stigma among people newly diagnosed with HIV/STI: internalized stigma associated with other identities. This is consistent with intersectionality theory, which suggests that people’s identities are interconnected and therefore may shape, or influence, each other. Thus, individuals’ experiences of stigma associated with pre-existing identities may shape their experiences of stigma associated with new identities. Greater research employing an intersectionality lens is needed to understand how new identities associated with health conditions develop in the context of pre-existing stigmatized identities including race, sexual orientation, and others. This is particularly important given that the time immediately after gaining a health condition may be a vulnerable period. For example, as shown in this study and others, internalized stigma appears to be heightened immediately after being diagnosed with HIV/STI (Tsai et al., 2013). Moreover, the time immediately after being diagnosed with a health condition is often a critical window for engagement in care and initiation of treatment.
Strengths, limitations, and future directions
This study drew on prospective, longitudinal data spanning immediately before and the first year following HIV/STI diagnosis. It is the first known study to quantitatively examine the extent to which internalized stigma associated with identities before HIV/STI diagnosis is associated with HIV/STI internalized stigma after HIV/STI diagnosis. Yet, a relatively small sample of Black gay and bisexual men in the Atlanta, GA metropolitan area of the United States was included in this study. Future research is needed to determine the extent to which findings generalize to more diverse samples and geographic locations. We collapsed across HIV and several other STIs and examined internalized stigma among Black gay and bisexual men diagnosed with HIV or another STI. This is consistent with theory and previous research suggesting that stigma has similar effects across stigmatized health conditions (Earnshaw et al., 2013b; Van Brakel, 2006). Moreover, results of this study suggest that diagnosis of HIV versus STI did not moderate the associations between race and/or sexual orientation internalized stigma with HIV/STI internalized stigma. There are several similarities in stigma associated with HIV and other STIs (e.g. both are perceived to be controllable, gained during one’s lifetime, and concealable). Yet, there are also key differences in stigma associated with HIV versus other STIs that may be curable or not perceived to be as great of a threat to others. Future researchers may continue to examine similarities and differences in internalized stigma among Black gay and bisexual men newly diagnosed with HIV versus other STIs.
Future research may continue to examine other risk factors for HIV/STI internalized stigma among Black gay and bisexual men and other people living with HIV/STI, including internalized stigma associated with other identities (e.g. drug use, sex work, incarceration) to build a more comprehensive understanding of risk factors for internalizing HIV/STI stigma. Research may also explore the magnitude, or importance, of the new stigmatized identity, and how this relates to wellbeing. Such research can contribute to greater understanding of the process of stigmatized identity development.
Conclusions and implications
This study suggests that internalized stigma prior to HIV/STI diagnosis is associated with HIV/STI internalized stigma after diagnosis among Black gay and bisexual men. Interventions that address internalized stigma among Black gay and bisexual men may therefore prevent, or attenuate, HIV/STI internalized stigma among Black gay and bisexual men who are diagnosed with HIV/STI during their lifetime. Given that the majority of Black gay and bisexual men living with HIV are diagnosed between 13 and 34 years old (Centers for Disease Control and Prevention, 2017a), and STIs show similar trends, interventions to address other forms of internalized stigma should be introduced during childhood and adolescence. Some evidence suggests that interventions that foster pride, empowerment, and self-esteem may reduce internalized stigma (Corrigan et al., 2013; Earnshaw et al., 2013a). It may be possible to deliver these interventions within familial settings, by involving parents, and schools, by involving teachers and other school staff (Earnshaw et al., 2013a; Earnshaw et al., 2018). Clinicians may also play a role in screening youth for internalized stigma and its negative consequences (e.g. depressive symptoms), and referring them to mental healthcare. Cognitive-behavioral stress management appears to be effective for addressing stigma among young adults experiencing sexual minority stigma and may be adapted for youth (Pachankis et al., 2015). It is critical to address race and sexual orientation internalized stigma among young Black gay and bisexual men to promote their wellbeing across the lifespan.
In addition, intersectionality theory emphasizes that social processes are intertwined with individual-level processes. Thus, stigma, which is a social process (Link & Phelan, 2001), is intertwined with individuals’ experiences of internalized stigma. It is therefore critical to develop strategies to eliminate stigma associated with HIV/STI, race, and sexual orientation at the social level to prevent individuals from internalizing stigma associated with HIV/STI, race, and sexual orientation.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institutes of Health, Grants R01MH094230 (LAE), R01NR013865 (LAE), and K01DA042881 (VAE).
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Andresen EM, Malmgren JA, Carter WB, et al. (1994) Screening for depression in well older adults: Evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). American Journal of Preventive Medicine 10(2): 77–84. [PubMed] [Google Scholar]
- Balaji AB, Oster AM, Viall AH, et al. (2012) Role flexing: How community, religion, and family shape the experiences of young black men who have sex with men. AIDS Patient Care and STDs 26(12): 730–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L (2013) “Once you’ve blended the cake, you can’t take the parts back to the main ingredients”: Black gay and bisexual men’s descriptions and experiences of intersectionality. Sex Roles 68: 754–767. [Google Scholar]
- Cass VC (1984) Homosexual identity formation: Testing a theoretical model. The Journal of Sex Research 20(2): 143–167. [Google Scholar]
- Centers for Disease Control and Prevention (2017a) HIV Surveillance Report, 2016. Atlanta, GA: U.S. Department of Health and Human Services; Available at: https://www.cdc.gov/hiv/library/reports/hiv-surveillance.html [Google Scholar]
- Centers for Disease Control and Prevention (2017b) Sexually Transmitted Disease Surveillance Report, 2016. Atlanta, GA: U.S. Department of Health and Human Services; Available at: https://doi.org/https://www.cdc.gov/std/stats14/default.htm [Google Scholar]
- Cole ER (2009) Intersectionality and research in psychology. American Psychologist 64(3): 170–180. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Kosyluk KA and Rusch N (2013) Reducing self-stigma by coming out proud: Roadrunner search discovery service. American Journal of Public Health 103(5): 794–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crenshaw K (1991) Mapping the margins: Intersectionality, identity politics, and violence against women of color. Stanford Law Review 43(6): 1241–1299. [Google Scholar]
- Earnshaw VA and Chaudoir SR (2009) From conceptualizing to measuring HIV stigma: A review of HIV stigma mechanism measures. AIDS and Behavior 13: 1160–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Bogart LM, Dovidio JF, et al. (2013a) Stigma and racial/ethnic HIV disparities: Moving toward resilience. American Psychologist 68(4): 225–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Quinn DM, Kalichman SC, et al. (2013b) Development and psychometric evaluation of the Chronic Illness Anticipated Stigma Scale. Journal of Behavioral Medicine 36(3): 270–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Reisner SL, Menino DD, et al. (2018) Stigma-based bullying interventions: A systematic review. Developmental Review 48(1): 178–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Smith LR, Chaudoir SR, et al. (2013c) HIV stigma mechanisms and well-being among PLWH: A test of the HIV Stigma Framework. AIDS and Behavior 17(5): 1785–1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- East L, Jackson D, O’Brien L, et al. (2011) Stigma and stereotypes: Women and sexually transmitted infections introduction and background. Collegian 19(1): 15–21. [DOI] [PubMed] [Google Scholar]
- Eaton LA, Earnshaw VA, Maksut JL, et al. (2018) Experiences of stigma and health care engagement among Black MSM newly diagnosed with HIV/STI. Journal of Behavioral Medicine 41: 458–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek GM, Gillis JR and Cogan JC (2009) Internalized stigma among sexual minority adults: Insights from a social psychological perspective. Journal of Counseling Psychology 56(1): 32–43. [Google Scholar]
- Hoffman L (2015) Longitudinal Analysis: Modeling Within-Person Fluctuation and Change. New York: Routledge. [Google Scholar]
- Hood JE and Friedman AL (2011) Unveiling the hidden epidemic: A review of stigma associated with sexually transmissible infections. Sexual Health 8(2): 159–170. [DOI] [PubMed] [Google Scholar]
- hooks b (1990) Yearning: Race, Gender, and Cultural Politics. Boston, MA: South End Press. [Google Scholar]
- Jones EE, Farina A, Hastorf AH, et al. (1984) Social Stigma: The Psychology of Marked Relationships. New York: Freeman, W.H. [Google Scholar]
- Jones SR and McEwen MK (2000) A conceptual model of multiple dimensions of identity. Journal of College Student Development 41(4): 405–414. [Google Scholar]
- Lee RS, Kochman A and Sikkema KJ (2002) Internalized stigma among people living with HIV/AIDS. AIDS and Behavior 6(4): 309–319. [Google Scholar]
- Lichtenstein B (2003) Stigma as a barrier to treatment of sexually transmitted infection in the American deep south: Issues of race, gender and poverty. Social Science & Medicine 57(12): 2435–2445. [DOI] [PubMed] [Google Scholar]
- Link BG (1987) Understanding labeling effects in the area of mental disorders: An assessment of the effects of expectations of rejection. American Sociological Review 52(96): 96–112. [Google Scholar]
- Link BG and Phelan JC (2001) Conceptualizing Stigma. Annual Review of Sociology 27: 363–385. [Google Scholar]
- Livingston JD and Boyd JE (2010) Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Social Science & Medicine 71(12): 2150–2161. [DOI] [PubMed] [Google Scholar]
- Logie CH, Lacombe-Duncan A, Wang Y, et al. (2018) Pathways from HIV-related stigma to antiretroviral therapy measures in the HIV care cascade for women living with HIV in Canada. Journal of Acquired Immune Deficiency Syndromes 77(2): 144–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak WWS, Poon CYM, Pun LYK, et al. (2007) Meta-analysis of stigma and mental health. Social Science & Medicine 65(2): 245–261. [DOI] [PubMed] [Google Scholar]
- Meyer IH (2003) Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin 129(5): 674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newton DC and Mccabe MP (2008) Sexually transmitted infections impact on individuals and their relationships. Journal of Health Psychology 13(7): 864–869. [DOI] [PubMed] [Google Scholar]
- Pachankis JE, Hatzenbuehler ML, Rendina HJ, et al. (2015) LGB-affirmative cognitive-behavioral therapy for young adult gay and bisexual men: A randomized controlled trial of a transdiagnostic minority stress approach. Journal of Consulting and Clinical Psychology 83(5): 875–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pantelic M, Shenderovich L, Cluver L, et al. (2015) Predictors of internalised HIV-related stigma: A systematic review of studies in sub-Saharan Africa. Health Psychology Review 9(4): 469–490. [DOI] [PubMed] [Google Scholar]
- Quinn DM and Earnshaw VA (2011) Understanding concealable stigmatized identities: The role of identity in psychological, physical, and behavioral outcomes. Social Issues and Policy Review 5(1): 160–190. [Google Scholar]
- Rosenthal L (2016) Incorporating intersectionality into psychology: An opportunity to promote social justice and equity. American Psychologist 71(6): 474–485. [DOI] [PubMed] [Google Scholar]
- Takada S, Weiser SSD, Kumbakumba E, et al. (2014) The dynamic relationship between social support and HIV-related stigma in rural Uganda. Annals of Behavioral Medicine 48(1): 26–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor J and Grundy C (1996) Measuring Black internalization of White stereotypes about African Americans: The Nadanolitization Scale In: Jones RL (ed.) Handbook of Tests and Measures for Black Populations (2ne edn). Hampton, VA: Cobb and Henry, pp. 217–226. [Google Scholar]
- Tsai AC, Bangsberg DR, Bwana M, et al. (2013) How does antiretroviral treatment attenuate the stigma of HIV? Evidence from a cohort study in rural Uganda. AIDS and Behavior 17(8): 2725–2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan B, Smith W, Cohen MH, et al. (2016) Mechanisms for the negative effects of internalized HIV-related stigma on antiretroviral therapy adherence in women: The mediating roles of social isolation and depression. Journal of Acquired Immune Deficiency Syndromes 72(2): 198–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Brakel WH (2006) Measuring health-related stigma–A literature review. Psychology, Health & Medicine 11(3): 307–334. [DOI] [PubMed] [Google Scholar]
- Vandiver BJ (2001) Psychological nigrescence revisited: Introduction and overview. Journal of Multicultural Counseling and Development 29: 165–173. [Google Scholar]
- Williams DR and Williams-Morris R (2000) Racism and mental health: The African American experience. Ethnicity & Health 5: 243–268. [DOI] [PubMed] [Google Scholar]
- Workowski KA and Bolan GA (2015) Sexually transmitted diseases treatment guidelines, 2015. Morbidity and Mortality Weekly Report 64(3): 1–137. Available at: https://www.cdc.gov/std/tg2015/tg-2015-print.pdf [PMC free article] [PubMed] [Google Scholar]
- Worrell FC, Cross WE, and Vandiver BJ. (2001). Nigrescence theory: Current status and challenges for the future. Journal of Multicultural Counseling and Development 29: 201–213. [Google Scholar]