Abstract
Background
Remission of Type 2 Diabetes Mellitus (DM) has been observed throughout the last few years, yet factors associated with remission through non-surgical approaches are still unclear. So, the factors associated with type 2 DM remission were investigated.
Methods
Out 670 patients, 63 patients gained non-surgical remission of type 2 DM (defined according to ADA criteria), and 396 patients served as control matched for age, sex, and BMI. The records of patients who attended Alexandria University Students Hospital between the years 2015 and 2018 were reviewed retrospectively. The collected data at first visit and 1 year after remission were history, examination, HbA1c %, oral glucose tolerance test & fasting blood glucose and lipid profile and type of treatment.
Results
75% of patients were females with mean age 51.5 ± 11.34 years. The mean duration of treatment till remission was 26.4 ± 33.1 months. One year after remission HbA1c & BMI were significantly decreased (P = 0.001, 0.03; respectively). However, cox proportional hazards model & ROC curve analysis showed that age < 50 years, female sex, short duration of diabetes < 5.2 years, intial HbA1c < 8.5%, HDL > 45.6 mg/dl, and initial intervention with lifestyle modification, 2000 mg metformin and 100 mg vildagliptin are the factors associated with remission.
Conclusion
Our mission in type 2 DM female patients < 50 years with short duration of disease < 5.2 years, initial HbA1c < 8.5% and HDL > 45.6 mg/dl, is to achieve diabetes remission by intensive life style modification with daily metformin and vildagliptin.
Keywords: Diabetes Mellitus, Remission, Vildagliptin
Introduction
Diabetes Mellitus (DM) is a major public health problem which is associated with serious complications that can be life threatening. Even prediabetes has shown to be associated with various complications including increased cardiovascular risk [1].
Traditionally DM has been considered a progressive incurable condition and the best targets for management were tight glycemic & metabolic control to prevent cardiovascular and other complications [2].
Studies to date have focused largely on DM remission after bariatric surgery, specifically gastric bypass and biliopancreatic diversion as more effective than conventional medical therapy in controlling hyperglycemia in severely obese patients with type 2 diabetes [3], [4]. Yet, few studies demonstrated remission of type 2 DM using nonsurgical approaches. The Look AHEAD (Action for Health for Diabetes) study is perhaps the largest randomized controlled trial of an intensive lifestyle intervention among adults with type 2 DM. Although designed principally to examine the effect of weight loss on cardiovascular disease incidence, it also determined the association of an intensive lifestyle intervention with the frequency of partial and complete type 2 DM remission [5].
Patients and methods
We conducted a retrospective cohort study on type 2 DM patients attending Endocrinology clinic at Alexandria University Students’ Hospital (AUSH) from the year 2015 till the year 2018 to describe the variables associated with remission among patients with type 2 DM who received the standards of care according to updated guidelines.
We excluded patients based on the following criteria: 1) Type 1 DM, 2) History of bariatric surgery, 3) Long-term use (>60 days) of steroids or other hyperglycemic drugs in the year prior to baseline, 4) Organ failure (heart, renal, or liver), 5) Patients who did not complete one year after remission; or 6) Patients who missed more than 2 visits during follow-up.
Definition of remission was based on the 2009 ADA consensus statement; Partial remission defined as having two or more consecutive subdiabetic HbA1c measurements, all of which were in the range of 5.7–6.4% over a period of at least 12 months and complete remission defined as having two or more consecutive normoglycemic HbA1c measurements, all of which were <5.7% over a period of at least 12 months. Each definition of remission requires the absence of pharmacologic treatment during the defined observation period [6].
All patients around the age of 30 years were subjected to antibodies screening and C-peptide level testing to exclude type 1 DM.
We collected baseline covariates from records at the first visit including; demographic characteristics, history including history of DM (time of diagnosis and duration of treatment), and physical examination. Patients were followed up every 3 months till the end of one year after remission. The laboratory work up related to glycemic control (fasting blood sugar, oral glucose tolerance test, and HbA1c), lipid profile (LDL, HDL, VLDL, and total cholesterol) and biochemical assays (estimated glomerular filtration rate [eGFR]) were done every visit.
All patients were motivated to intensive lifestyle intervention according to ADA guidelines. The intensive intervention included caloric restriction (under supervision of a registered dietitian), moderate-intensity aerobic physical activity (goal 175 min weekly), and smoking cessation [7]. Monitoring of lifestyle adherence was assessed every visit through structured self-reporting diaries & structured personal interviews.
Descriptive statistics were used to summarize the baseline demographic and clinical data, disease characteristics and treatment options. Differences in baseline characteristics between remission and control groups were tested by independent t test (normally distributed data) or Mann– Whitney test (non-normally distributed data).
We examined unadjusted and adjusted models based on a complete case–only analysis. The adjusted model included demographic data (age at cohort entry and sex), baseline factors (BMI, eGFR, HbA1c level), comorbidities (cardiovascular disease, hypertension, dyslipidemia), and diabetes factors (oral or insulin use, drugs categories, and years since diabetes diagnosis).
We calculated the cumulative incidence of remission using the Kaplan-Meier method of estimating the cumulative probability of an event. Cox proportional hazards models were specified to identify significant factors associated with the time of remission. Receiver operating characteristic curve (ROC) was plotted to analyze a recommend cut off value of significant continuous variables.
All analyses were conducted using SPSS version 22 (SPSS Inc., an IBM company; Chicago, Ill) and MedCalc® 13.3.3.0 statistical software (MedCalc Software; Mariakerke, Belgium) packages. All statistical tests were two sided; the level of significance was <0.05.
Collection and analysis of the data in this study were ethically approved by local Institutional Review Board.
Results
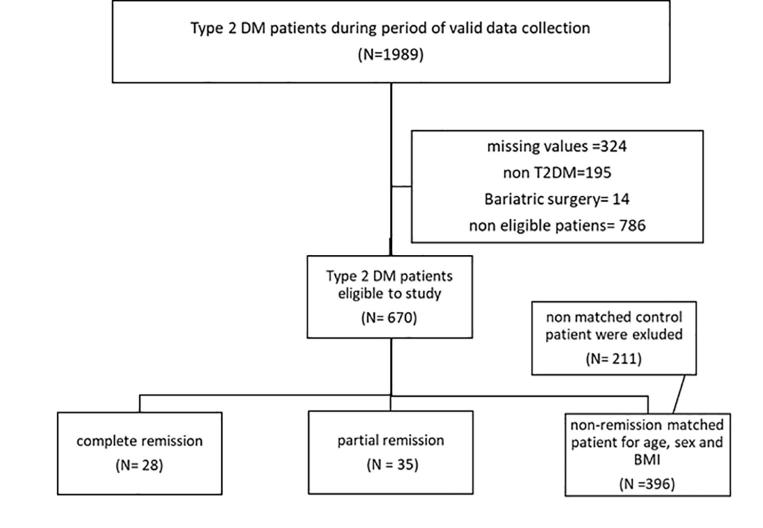
Medical records evaluated retrospectively showed that; out of 670 patients with type 2 DM, 63 patients showed DM remission; around 44% of patients developed complete remission and 56% developed partial remission (Fig. 1).
Fig. 1.
Flow chart of patients enrolled in the study.
At the first visit the demographic data were included in Table 1 10% suffered from ischemic heart disease, and 20% had dyslipidemia.
Table 1.
Demographic data of enrolled patients.
| Range (mean ± SD) |
p-Value | ||
|---|---|---|---|
| Remission | No remission | ||
| Female sex (%) | 75 | 73 | 0.90 |
| Age (years) | 25–60 (51.5 ± 11.34) | 28.5–63.5 (50.0 ± 12.5) | 0.19 |
| Duration of DM (years) | 0.5–9.5 (4.20 ± 4.13) | 4.5–21 (12.20 ± 7.63) | 0.02 |
| Initial body mass index (kg/m2) | 25.9–41.5 (34.22 ± 7.31) | 27.11–46 (35.8 ± 8.69) | 0.50 |
| Smoker (%) | 6.7 | 71 | 0.00 |
| Comorbidities (%) | 0.01 | ||
| Hypertension | 30 | 42 | |
| Coronary heart disease | 10 | 31 | |
| Dyslipidemia | 20 | 54 | |
| Peripheral neuropathy | 10 | 27 | |
| Nephropathy | 2 | 11 | |
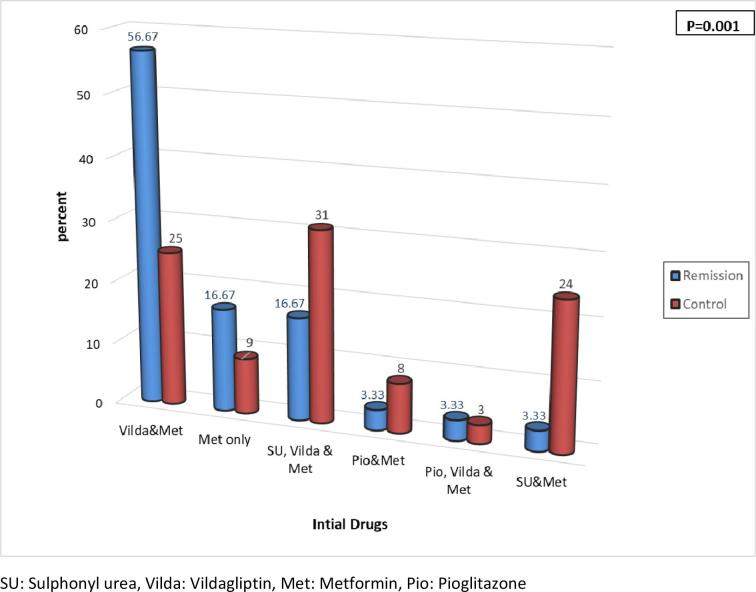
In the first visit, all patients who showed remission were adherent to lifestyle modification and to the prescribed oral antidiabetic drugs; the most frequently prescribed drugs in remission group were vildagliptin + metformin, versus sulphonyl urea + vildagliptin + metformin in control; group (56.67%, 31%, respectively) (Fig. 2). Only 26% of those patients were maintained on statin.
Fig. 2.
Drug category of patients who showed remission at the start of the study.
The mean duration of treatment till complete remission was 12.5 ± 6.95 months, which was significantly lower than mean duration of treatment in partial remission (74 ± 14.29 months, p < 0.001) and also in non-remission patients (84 ± 24.98 months, p < 0.019).
In comparison to first visit, patients after 1 year of remission their body weight & BMI were significantly decreased; mean 94.72 ± 19.35 kg Vs 89.12 ± 16.99 kg (P = 0.003), and 34.22 ± 7.31 kg/m2 Vs 32.16 ± 6.25 kg/m2 (P = 0.027), respectively. Study findings were adjusted for baseline BMI. Also, there was a significant decrease in Hb A1c, fasting plasma glucose (FPG), and oral glucose tolerance test; 8.87 ± 1.49% Vs 5.55 ± 0.53% (P = 0.0001), 185.77 ± 74.58 mg/dl Vs 101.1 ± 11.24 mg/dl (P = 0.0001), and 263.97 ± 95.19 mg/dl Vs 116.6 ± 25.2 mg/dl (P = 0.0001), respectively (Table 1).
Moreover, lipid profile of the patients 1 year after remission has changed dramatically.
Compared to first visit, there was a significant increase in HDL; 42.93 ± 8.63 mg/dl Vs 96.97 ± 45.19 mg/dl (P = 0.0001), whereas there was a significant decrease in LDL and triglycerides (TG); 143.13 ± 39.98 mg/dl Vs 48.44 ± 10.82 mg/dl (P = 0.006) and 146.13 ± 94.19 mg/dl Vs 91.82 ± 71.23 mg/dl (P = 0.002), respectively (Table 2).
Table 2.
Comparison between the first visit and one year after remission regarding weight and metabolic profile of patients.
| Mean (min–max) | First visit | Last visit | *P (2-tailed) |
|---|---|---|---|
| BWT (Kg) | 94.72 ± 19.35 (57–150) | 89.12 ± 16.99 (60–145) | 0.003 |
| BMI (Kg/m2) | 34.22 ± 7.31 (23–55) | 30.16 ± 6.25 (24.2–53.2) | 0.027 |
| A1C (%) | 8.87 ± 1.49 (7–12.4) | 5.55 ± 0.53 (4–7) | 0.0001 |
| FPS (mg/dl) | 185.77 ± 74.58 (102–415) | 101.1 ± 11.24 (76–122) | 0.0001 |
| PPS (mg/dl) | 263.97 ± 95.19 (144–476) | 116.6 ± 25.2 (70–167) | 0.0001 |
| HDL (mg/dl) | 42.93 ± 8.63 (25–66) | 96.97 ± 45.19 (31–229) | 0.0001 |
| LDL (mg/dl) | 143.13 ± 39.98 (100–246) | 48.44 ± 10.82 (31–68) | 0.006 |
| TG (mg/dl) | 146.13 ± 94.19 (22–479) | 91.82 ± 71.23 (26–331) | 0.002 |
Data are mean ± standard deviation. BWT: body weight; BMI: body mass index; A1C: hemoglobin A1c, FPS: fasting plasma glucose, PPS: post prandial plasma glucose, HDL: high density lipoprotein, LDL: low density lipoprotein, TG: triglycerides.
Statistically significant at p ≤ 0.05.
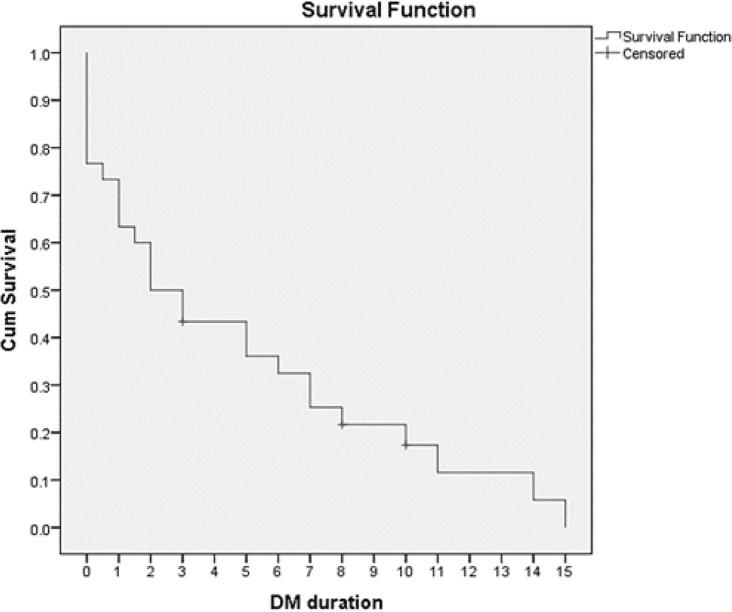
As shown in Fig. 3; the median cumulative incidences of partial and complete remission were 1.4% (95% CI 1.1–1.5%) and 1.17% (95% CI 0.940–2.54%), respectively. The cumulative incidence of remission was 3.47%. Patients with DM duration less than 2.5 years showed a high incidence of remission; 4.6% (95% CI 4.1–5.3%) whereas a low incidence of remission; 0.67% (95% CI 0.4–0.8%) was found in patients with DM duration more than 9 years.
Fig. 3.
Kaplan-Meier curve for cumulative incidence of type 2 DM remission.
After univariate analysis of variables associated with remission (partial & complete), the cox proportional hazards models were performed which showed that in a younger age, female patients, with shorter duration of diabetes and without history of smoking or IHD, especially with lower baseline HbA1c level and higher HDL have the highest probability for diabetes remission. And they will have 7 times the chance for diabetes remission if they were initially treated with 2000 mg metformin and 100 mg vildagliptin but did not start with insulin therapy after adjusting for the effects of other factors, (Table 3).
Table 3.
The cox proportional hazards models of included type 2 diabetic patients to identify significant factors associated with remission.
| B | S.E | *Adjusted p | HR | 95% CI |
||
|---|---|---|---|---|---|---|
| LL | UL | |||||
| Age | −0.099 | 0.01 | 0.039 | 4.41 | 1.080 | 18.060 |
| Female sex | 0.004 | 0.26 | 0.048 | 1.004 | 0.974 | 1.030 |
| nonsmoking | 0.228 | 0.3 | 0.003 | 1.26 | 1.010 | 1.560 |
| Diabetes duration | −0.03 | 0.022 | 0.003 | 6.00 | 0.999 | 8.002 |
| History of IHD | −2.06 | 0.9 | 0.023 | 5.2 | 0.022 | 0.748 |
| Initial HbA1c | −2.347 | 0.763 | 0.002 | 10.45 | 2.340 | 16.570 |
| Initial HDL | 0.259 | 0.166 | 0.011 | 0.77 | 0.557 | 1.069 |
| 2000 mg Metformin and Vildagliptin | 0.185 | 0.12 | 0.012 | 7.204 | 0.951 | 9.523 |
| Insulin therapy | −0.08 | 0.05 | 0.008 | 7.008 | 0.940 | 10.080 |
CI: Confidence interval; LL: Lower limit; UL: Upper limit; HR: Hazards ratio.
Adjusted P is significant if < 0.05.
As shown in Fig. 4, receiver operating characteristic (ROC) curve was constructed for determining the best cut off value for prediction of type 2 DM remission detected by Youden index. The cut off and predictive values were age < 50 years (sensitivity 71.5% & specificity 61.5%), duration of DM < 5.2 years (sensitivity 89.5% & specificity 59.5%), baseline HbA1c level < 8.5% (sensitivity 58.7% & specificity 55.2%) and HDL > 45.6 mg/dl (sensitivity 62% & specificity 69%). ROC curve for the prediction of remission of DM showed that highest sensitivity was found with short duration of DM while highest specificity was found with HDL.
Fig. 4.
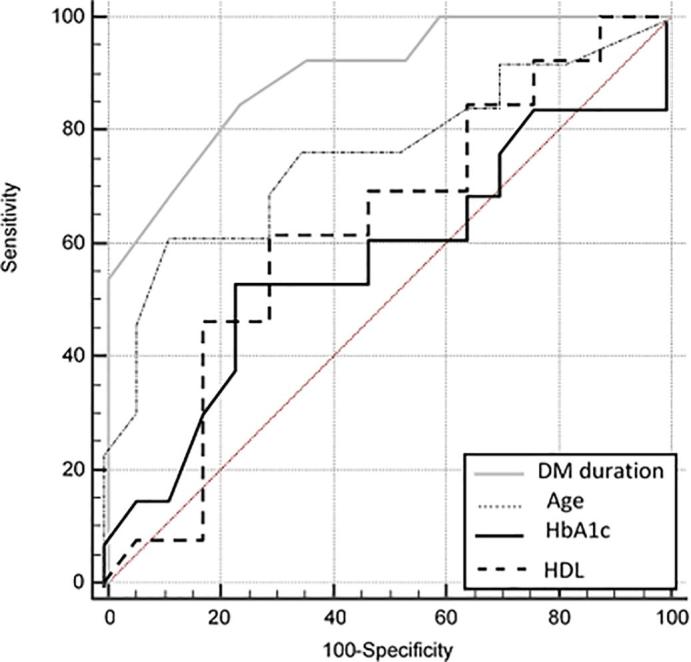
Receiver operating characteristic (ROC) curve determining the best cut off value for predictors of type 2 DM remission.
Discussion
Type 2 DM has been regarded as a progressive lifelong disease with long term dangerous complications. Yet, a growing body of evidence from clinical research has reported the remission of type 2 DM mostly after bariatric surgery. However, recently remission of type 2 DM can be achieved using non surgical approaches.
The current study showed that the median incidences of partial and complete remission among 670 patients with type 2 DM throughout 3 years were 1.4% (95% CI 1.1–1.5%) and 1.17% (95% CI 0.940–2.54%), respectively. In accordance with our finding, Karter et al, found that the incidences of remissions per 1000 person-years of partial, complete, or prolonged remission were 2.8 (2.6–2.9), 0.24 (0.20–0.28), and 0.04 (0.01–0.06), respectively [8]. Also, Uusitupa showed that remission of type 2 DM can be achieved and the most important factor affecting remssion is weight loss which improves insulin sensitivity and on the long run may help to preserve β-cell mass [9].
The largest trial to date; the Look AHEAD multicenter randomized controlled trial, compared intensive lifestyle intervention (ILI) with diabetes support and education (DSE) among 4503 overweight & obese patients with type 2 DM across 4 years. Results showed that ILI group was more likely to experience remission (partial or complete), with prevalence of 11.5% (95% CI, 10.1%–12.8%) during the first year and 7.3% (95% CI, 6.2%–8.4%) at 4 years, compared with 2% for the DSE group at both time points (95% CIs, 1.4%–2.6% at year 1 and 1.5%–2.7% at year 4) (P < 0.001 for each). In agreement with our findings, DM remission occurred particularly in those whose diabetes is of short duration, who have lower HbA1c levels, and who do not require insulin therapy. Also, in line with our results, baseline BMI was not associated with remission in the Look AHEAD study, which found that only a change in BMI predicted remission [10].
Contrary to our results, Karter et al found that older age is associated with higher rates of remission. Their results are consistent with evidence from the Diabetes Prevention Program demonstrating that older adults over 65 years experienced the greatest risk reduction in diabetes from lifestyle modification [8].
In accordance with our results, Lean et al showed in the DiRECT trial that type 2 DM remission can occur without surgery and the most potent predictor of remission is weight loss > 15 kg and that sustained remission was linked to the extent of sustained weight loss [11].
The majority of patients who showed remission in our study were initially prescribed vildagliptin + metformin. After occurrence of remission, patients stopped all drugs and were maintained only on lifestyle programs. Vellanki et al, in their 4-year placebo-controlled study found that remission of type 2 DM is maintained by metformin + sitagliptin. Maintenance of remission was significantly higher in sitagliptin + metformin group compared with placebo (P = 0.015), and mean time to relapse was significantly prolonged in the metformin + sitagliptin group compared with the placebo group (P = 0.004) [12]. However, the proposed mechanisms for remission of T2DM were related to weight loss, this could not be explained by modest effect of vildagliptin and metformin on weight. We matched the cases and control for BMI and adjusted all factors against BMI in cox regression analysis. This could be explained by activation of hematopoietic stem cells in response to DPP4 inhibitors which control inflammatory and immune response pathogenesis of T2DM [13], in association with β-cell regeneration [14].
The limitation of the study is that diabetic patients receiving new therapeutic agents such as sodium glucose transporter 2 inhibitors (SGLT2 inhibitors) and glucagon like peptide 1 agonists (GLP1 agonists) were not discussed in our study. This is due to lack of availability during the study period as these agents have become part of standard of care only recently in Egypt after we have started the study. Moreover most of the Egyptian diabetic patients are poor and can’t afford such expensive drugs.
Conclusion
Type 2 DM remission is possible without surgical intervention. Factors influencing medical remission include; female sex, young age < 50 years, short duration since diagnosis of DM < 5.2 years, baseline HbA1c < 8.5% and HDL > 45.6 mg/dl. Therefore, our mission in type 2 DM patients with such criteria is to achieve diabetes remission as a treatment target by intensive life style modification in association with daily metformin and vildagliptin.
Recommendation
A double blinded clinical trial is needed to assess factors associated with remission of T2DM using more data including new therapeutic agents for diabetes such as SGLT2 inhibitors and GLP1 agonists.
Author disclosures
Dr. Magdy Allam: I declare that no funding source for this work.
Dr. Hanaa El-Zawawy: I declare that no funding source for this work.
Authors’ contributions
Authors have an equal contribution in this research.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Magdy M. Allam, Email: m_mohamed0902@alexmed.edu.eg.
Hanaa T. El-Zawawy, Email: hanaaelzawawy@yahoo.com.
References
- 1.El-Zawawy H.T. Serum leptin in male hypothyroid prediabetic patients: Association with cardiovascular risk. Cardiovasc Endocrinol Metab. 2018;7(4):84–87. doi: 10.1097/XCE.0000000000000157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holman R.R., Paul S.K., Bethel M.A., Matthews D.R., Neil H.A. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359:1577–1589. doi: 10.1056/NEJMoa0806470. [DOI] [PubMed] [Google Scholar]
- 3.Mingrone G., Panunzi S., De Gaetano A. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366:1577–1585. doi: 10.1056/NEJMoa1200111. [DOI] [PubMed] [Google Scholar]
- 4.Robert M., Ferrand-Gaillard C., Disse E., Espalieu P., Simon C., Laville M. Predictive factors of type 2 diabetes remission 1 year after bariatric surgery: impact of surgical techniques. Obes Surg. 2013;23(6):770–775. doi: 10.1007/s11695-013-0868-4. [DOI] [PubMed] [Google Scholar]
- 5.Gregg E.W., Chen H., Wagenknecht L.E., Clark J.M., Delahanty L.M., Bantle J. Association of an intensive lifestyle intervention with remission of type 2 diabetes. JAMA. 2012;308(23):2489–2496. doi: 10.1001/jama.2012.67929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buse J.B., Caprio S., Cefalu W.T., Ceriello A., Del Prato S., Inzucchi S.E. How do we define cure of diabetes? Diabetes Care. 2009;32(11):2133–2135. doi: 10.2337/dc09-9036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Diabetes Association 5. Lifestyle management: standards of medical care in diabetes—2019. Diabetes Care. 2019;42(Supplement 1):S46–S60. doi: 10.2337/dc19-S005. [DOI] [PubMed] [Google Scholar]
- 8.Karter A.J., Nundy S., Parker M.M., Moffet H.H., Huang E.S. Incidence of remission in adults with type 2 diabetes: the diabetes & aging study. Diabetes Care. 2014;37(12):3188–3195. doi: 10.2337/dc14-0874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Uusitupa M. Remission of type 2 diabetes: mission not impossible. Lancet. 2018;391(10120):515–516. doi: 10.1016/S0140-6736(17)33100-8. [DOI] [PubMed] [Google Scholar]
- 10.Gregg E.W., Chen H., Wagenknecht L.E., Clark J.M., Delahanty L.M., Bantle J. Association of an intensive lifestyle intervention with remission of type 2 diabetes. JAMA. 2012;308(23):2489–2496. doi: 10.1001/jama.2012.67929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lean M.E.J., Leslie W.S., Barnes A.C., Brosnahan N., Thom G., McCombie L. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol. 2019;7(5):344–355. doi: 10.1016/S2213-8587(19)30068-3. [DOI] [PubMed] [Google Scholar]
- 12.Vellanki P., Smiley D.D., Stefanovski D., Anzola I., Duan W., Hudson M. Randomized controlled study of metformin and sitagliptin on long-term normoglycemia remission in African american patients with hyperglycemic crises. Diabetes Care. 2016;39(11):1948–1955. doi: 10.2337/dc16-0406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhu E., Hu L., Wu H., Piao L., Zhao G., Inoue A. Dipeptidyl peptidase-4 regulates hematopoietic stem cell activation in response to chronic stress. J Am Heart Assoc. 2017;6(7) doi: 10.1161/JAHA.117.006394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li C.J., Sun B., Fang Q.H., Ding M., Xing Y.Z., Chen L.M. Saxagliptin induces β-cell proliferation through increasing stromal cell-derived factor-1α in vivo and in vitro. Front Endocrinol. 2017 Nov;27(8):326. doi: 10.3389/fendo.2017.00326. [DOI] [PMC free article] [PubMed] [Google Scholar]