Abstract
Chronic acromioclavicular joint dislocations (ACJDs) develop when there is failure of conservative treatment, failed surgical treatment of acute ACJD, or simply missing the treatment in the acute healing phase. There is wide agreement that mechanical fixation alone in chronic ACJD is not sufficient and biological augmentation is necessary. Various arthroscopic techniques for reconstruction of the coracoclavicular ligament have been described, but allografts are expensive, are not available in all centers, carry the risk of disease transmission, and are “dead tissue” with a poor capacity for healing. Autografts are associated with donor-site morbidity and avascular structures. Moreover, these grafts are associated with a high risk of clavicular or coracoid fractures owing to large tunnels. We present an arthroscopic technique to transfer the coracoacromial ligament to the inferior surface of the lateral part of the clavicle in chronic ACJD, augmented with 2 clavicular buttons and a single coracoid button in a V-shaped configuration. The technique has various advantages including better stabilization, anatomic reconstruction, and a minimal risk of fracture of the coracoid and clavicle with small tunnels, using a vascularized graft with arthroscopic control of reduction.
Chronic acromioclavicular joint (ACJ) instability is considered when resorption and progressive retraction of the coracoclavicular (CC) and acromioclavicular (AC) ligaments are present such that spontaneous healing becomes impossible and biological augmentation becomes mandatory.1, 2 Most authors have reported that ACJ injuries with a duration of more than 3 weeks should be considered chronic; however, others have minimized this time interval to only 10 days from injury.1, 2, 3 Failure of conservative or surgical treatment in the acute phase results in chronic ACJ instability; periscapular muscle fatigue, scapular dyskinesia, a subjective sensation of heaviness of the injured upper limb, painful horizontal adduction, and failure to return to high-level sports or manual work develop in about 15% to 40% of patients with complete acromioclavicular joint dislocations (ACJDs).1, 4, 5
Surgical treatment of chronic ACJ instability is challenging, and to date, no gold-standard technique has been determined. One of the most popular techniques described is the Weaver-Dunn procedure. Recently, arthroscopic techniques have been shown to offer the advantages of treating associated intra-articular pathology (SLAP lesions), requiring less soft-tissue dissection, being more cosmetic, providing better visualization of the inferior surface of the coracoid process, having less risk of infection, and allowing earlier rehabilitation.6, 7
Arthroscopic Weaver-Dunn procedures have been described by multiple authors, but these techniques have included a non-augmented coracoacromial (CA) ligament transfer, which caused high stress on the graft; used large tunnels (4.5 mm) with a high risk of fracture and button migration; or tried to reconstruct the obliquely oriented ligaments with a vertically oriented ligament.8, 9, 10 We present a fully arthroscopic technique augmented by a suspensory fixation construct with double–clavicular button fixation and a single subcoracoid button in a V-shaped orientation.
Surgical Technique and Indications
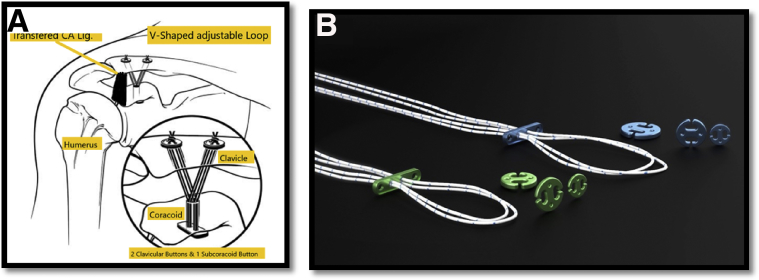
The described technique is considered for chronic cases (>3 weeks) of Rockwood type III, IV, or V ACJD with failed conservative treatment. The principle is to reduce the ACJ by releasing any soft-tissue interposition and then stabilize it with a suspensory loop constructed in a V-shaped orientation with 2 clavicular buttons and 1 button beneath the coracoid base augmented with the CA ligament transferred to the lateral clavicle in a fully arthroscopic manner (Fig 1).
Fig 1.
(A, B) The technique for the Weaver-Dunn procedure is shown with the suspensory fixation system with 2 clavicular buttons and a single subcoracoid button. (CA lig, coracoacromial ligament.)
Anesthesia and Positioning
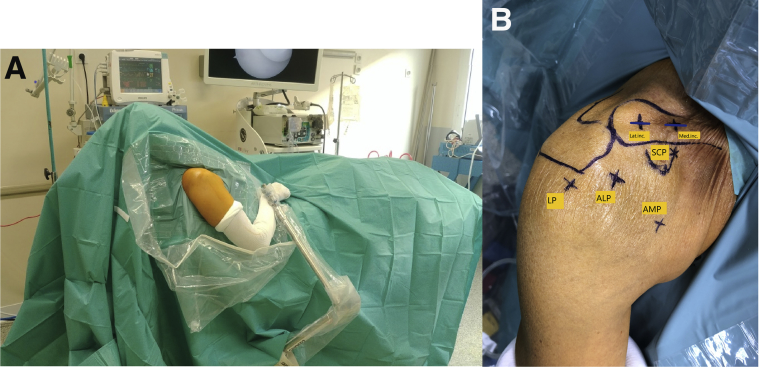
The surgical procedure is performed with the patient under general anesthesia and an interscalene block in the beach-chair position, and a pneumatic arm holder (Smith & Nephew, Andover, MA) is used. Five portals are used—posterior, lateral, anterolateral, anteromedial, and supracoracoid—as well as an incision of about 1 cm on the upper lateral part of the clavicle about 2 cm from the ACJ (Fig 2).
Fig 2.
(A) Outside view of the patient in the beach-chair position with a pneumatic arm holder after surgical sterilization and draping of the right shoulder. (B) The portals and incision are marked in the right shoulder in the beach-chair position, showing the lateral incision (Lat inc) and medial incision (Med inc), lateral portal (LP), anterolateral portal (ALP), anteromedial portal (AMP), and supracoracoid portal (SCP), in addition to the ordinary posterior portal.
Operative Steps
Insertion of 2 Clavicular Guidewires
After a 1-cm incision is performed, just 2 cm lateral to the ACJ, the first clavicular guidewire—a lateral oblique (toward the coracoid process) guidewire—is inserted 2 cm from the ACJ and 1 cm posterior to the anterior edge of the clavicle; the second, medial clavicular guidewire is inserted 4 cm from the ACJ and 1 cm anterior to the posterior edge of the clavicle oblique to the coracoid process (Video 1). It is advisable to mark the 2 clavicular tunnels with guidewires early in the procedure before swelling of the shoulder occurs (Fig 2).
Diagnostic Arthroscopy and Management of Concomitant Pathology
After establishment of the posterior portal, diagnostic arthroscopy is performed for evaluation and management of associated intra-articular shoulder pathology.
Opening of Rotator Interval and Coracoid Visualization
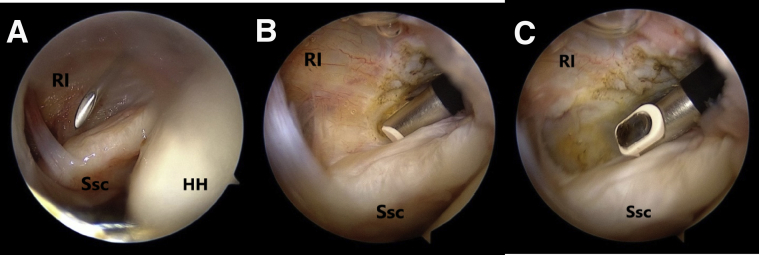
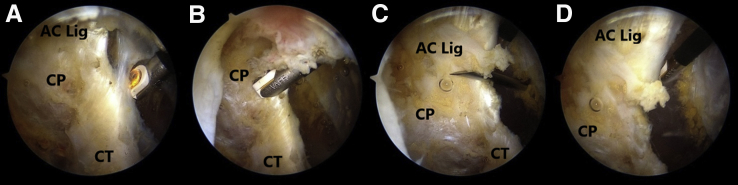
Next, we open the medial part of the rotator interval through an anterior portal using a radiofrequency (RF) device (VAPR; DePuy Mitek, Raynham, MA) (Fig 3). With further dissection, we expose the coracoid process medially with the conjoint tendon attached to its tip and the CA ligament attached to its lateral border, forming a Y-shaped structure (Fig 4).
Fig 3.
(A) Arthroscopic view of the right shoulder in the beach-chair position from the posterior viewing portal showing the spinal needle in the rotator interval (RI) during creation of the anterior portal. (B, C) Arthroscopic views showing opening of the RI using a radiofrequency device. (HH, humeral head; Ssc, subscapularis.)
Fig 4.
(A-D) Arthroscopic views of the right shoulder in the beach-chair position during dissection and exposure of the coracoid process (CP), conjoint tendon (CT), and coracoacromial ligament (AC Lig), forming a Y-shaped structure.
Visualization of Subacromial Space and Undersurface of Clavicle
First, by use of the posterior portal as the viewing portal and the lateral portal (1 cm distal to the lateral acromial edge in line with the posterior aspect of the ACJ) as the working portal, a shaver and RF device (VAPR) are used to expose the undersurface of the acromion and clavicle and to release the undersurface of the anterior deltoid from the CA ligament. Then, with the lateral portal used as the viewing portal and the anterosuperolateral (ASL) portal used as the working portal, complete exposure of the undersurface of the clavicle is performed (Fig 5A).
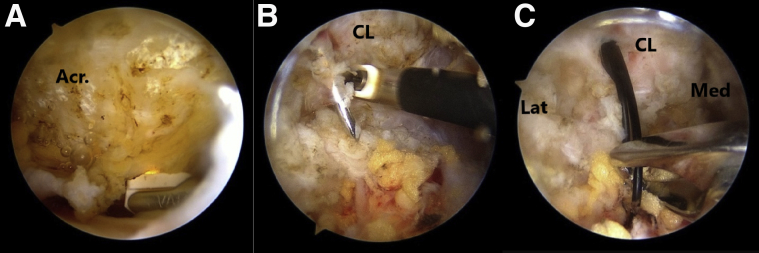
Fig 5.
Arthroscopic views of the right shoulder in the beach-chair position. (A) Preparation of the subacromial space (Acr). (B) Preparation of the undersurface of the clavicle (CL) and the 2.4-mm guidewires. (C) Retrieval of shuttle sutures from the undersurface of the clavicle (CL) in the 2 clavicular tunnels. (Lat, lateral; Med, medial.)
Distal Clavicular Debridement
We do not prefer to abrade the distal part of the clavicle except when severe arthritis is present or it is impossible to gain reduction; instead, we recommend only releasing the interposed soft tissue to facilitate reduction.
Drilling of 2 Clavicular Tunnels
A 2.4-mm drill bit is used to create the 2 clavicular tunnels over the previously positioned guidewires. While performing visualization through the lateral portal, the surgeon inserts a suture retrieval to pass 2 shuttle relays (No. 2 looped polyester suture) through the 2 tunnels. One advantage of this technique is that creation of the clavicular and coracoid tunnels is performed in an independent manner under direct arthroscopic visualization of the inferior surface of the clavicle, thus minimizing the risk of tunnel blowout (Fig 5 B and C).
Dissection of CA Ligament
Continuing visualization through the posterior portal and using the anterior or ASL portal as a working portal, the surgeon uses the VAPR RF device to complete the exposure of the CA ligament. The CA ligament is then dissected from its insertion at the undersurface of the acromion to the coracoid and conjoint tendon, preserving the arterial supply. The ligament is mobilized from the deltoid and released from both the deep and superficial surfaces.
Preparation of CA Ligament
A shuttle relay is used to make a triple Krackow suture to whipstitch the CA ligament, starting near the coracoid process, until reaching its insertion in the acromion using a Fiber Force (No. 2 nonabsorbable suture) (VIMS, Toulouse, France) (Fig 6). Through the subacromial space, while viewing from the posterior portal, the surgeon detaches the proximal attachment of the CA ligament from the undersurface of the acromion without incorporating any bony fragments from the acromion using the RF device through the lateral portal.
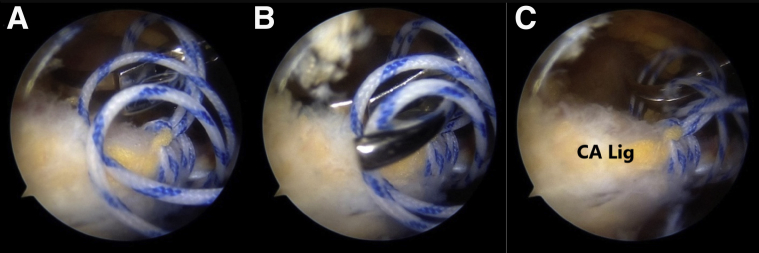
Fig 6.
(A-C) Arthroscopic views of the right shoulder in the beach-chair position showing the technique for the lasso-loop stitch for whipstitching the coracoacromial ligament (CA lig) using a Clever Hook (DePuy Mitek) and BirdBeak device (Arthrex) with No. 2 fiber force suture (VIMS).
Drilling of Coracoid Bone Tunnel
A supracoracoid portal is used to insert a guidewire in the central part of the base of the coracoid process as posteriorly as possible to respect the native CC ligament insertion points, with visualization through the ASL portal. A 2.4-mm drill is used to create the coracoid tunnel under direct arthroscopic control of both the superior and inferior surfaces of the coracoid (Fig 7).
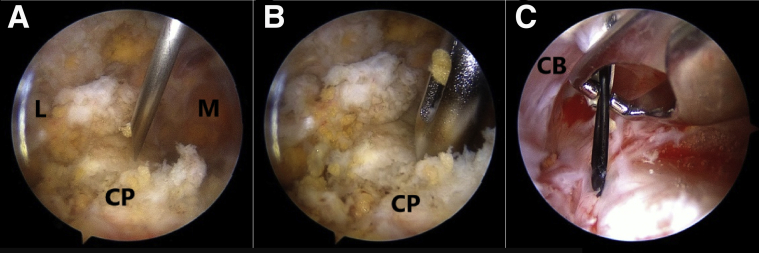
Fig 7.
(A-C) Arthroscopic views of the right shoulder in the beach-chair position during creation of the clavicular bone tunnel and retrieval of the shuttle suture from the undersurface of the coracoid process. (CB, undersurface of coracoid base; CP, top view of coracoid process; L, lateral; M, medial.)
Placement of Suspensory Loop Construct and Fixation of CA Ligament
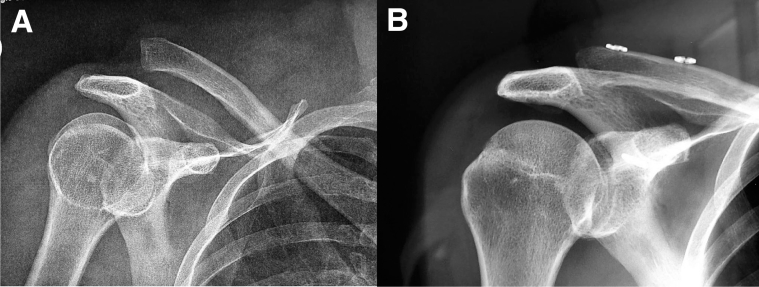
Using the shuttle sutures, we pull the suspensory adjustable-loop ligament construct (VIMS) from the undersurface of the coracoid through the anterior portal while visualizing through the ASL portal. The Oblong button is now settled beneath the coracoid base (Fig 8). Then, the 2 loops of the construct are shuttled through the clavicular tunnels, and the medial loop is tied over the medial button (VIMS) whereas the lateral loop is tied over a round button with 4 holes (VIMS). Pushing the elbow from inferior to superior and manipulating the scapula help to reduce the ACJD under arthroscopic control of reduction. The Fiber Force suture of the CA ligament is also tied over this lateral clavicular button (Fig 9). Radiographic control of the reduction is checked postoperatively (Fig 10).
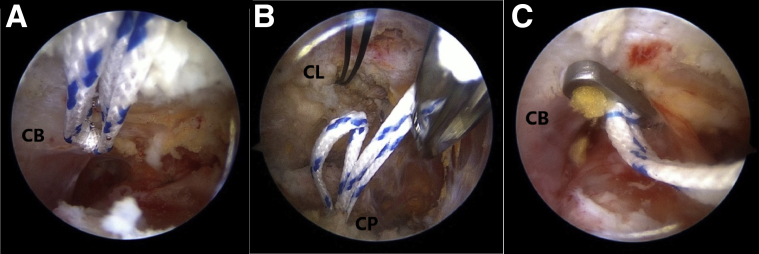
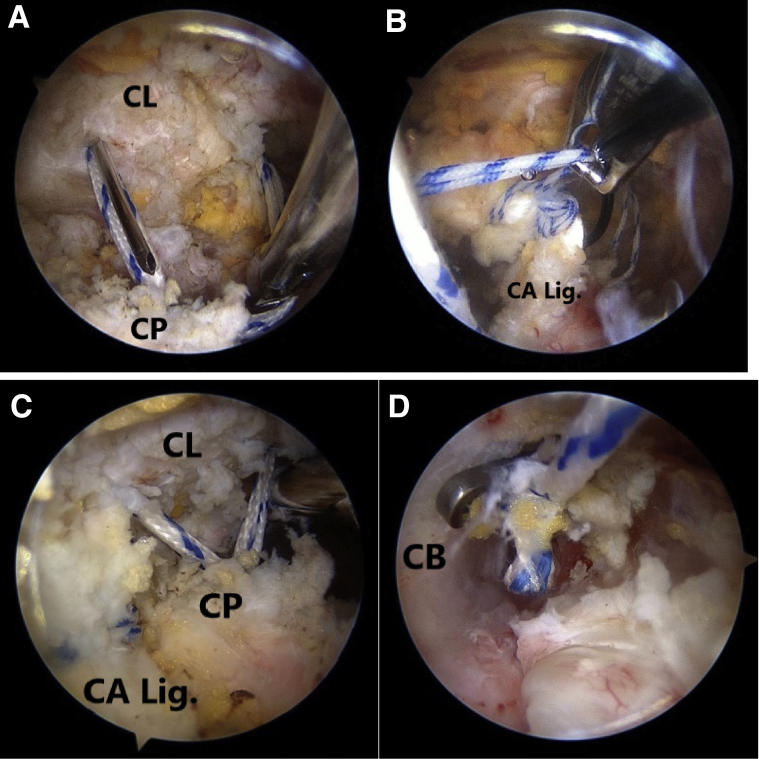
Fig 8.
Arthroscopic views of the right shoulder in the beach-chair position during shuttling of the suspensory fixation system (VIMS adjustable loop). (A) Loop passing in the tunnel in the coracoid base (CB). (B) Two clavicular loops pointing from the dorsal surface of the coracoid to be shuttled in the previously prepared 2.4-mm clavicular tunnels. (CL, clavicular undersurface; CP, coracoid process.) (C) Oblong button under the coracoid base (CB).
Fig 9.
Arthroscopic views of the right shoulder in the beach-chair position. (A) Undersurface of the clavicle (CL) with the 2 loops of the suspensory fixation system in the tunnels reconstructing the conoid and trapezoid and a spinal needle in the lateral tunnel to fix the coracoacromial ligament to the lateral clavicular tunnel. (CP, coracoid process.) (B) Passage of the fiber force of the coracoacromial ligament (CA Lig) in the lateral clavicular tunnel. (C) Final construct showing the V-shaped limbs of the suspensory fixation system exiting from the coracoid process (CP) to the clavicular undersurface and coracoacromial ligament (CA lig) also attached to the lateral limb to the clavicle (CL). (D) Oblong button under the coracoid base (CB).
Fig 10.
(A) Preoperative radiograph of the right shoulder (anteroposterior view) showing a Rockwood type V acromioclavicular joint dislocation. (B) Postoperative radiograph of the same patient (anteroposterior view) showing acromioclavicular joint reduction, 2 coracoid buttons, and a single subcoracoid button.
Discussion
Many techniques have been described for the treatment of chronic ACJDs. For many years, the modified Weaver-Dunn procedure was considered the gold standard in ACJ reconstruction, especially for chronic cases.2 Our arthroscopic Weaver-Dunn technique offers 3 main advantages: anatomic reconstruction, small tunnels, and possible revision with the Mumford procedure if needed in case of secondary ACJ arthritis.
Semitendinosus tendon graft for CC ligament reconstruction is associated with superior clinical results compared with a modified Weaver-Dunn procedure augmented with CC wire only and not titanium buttons, but there is a risk of coracoid or clavicular fracture; in addition, autogenous semitendinosus tendon grafting requires a second surgical procedure with associated morbidity for the patient. Allograft is not composed of living tissue, is expensive, is not available in all centers, and is associated with disease transmission.5, 6
Lafosse et al.8 described an all-arthroscopic technique for CC ligament reconstruction for acute or chronic ACJD in which they augmented the transfer with a transarticular K-wire, which was problematic and thus was discarded. They subsequently used an unaugmented CA ligament transfer technique, which may increase the stresses on the transferred ligament.8
Zooker et al.11 reported on the biomechanical properties of the double-button augmentation method for the Weaver-Dunn procedure, which showed greater stability over tape cerclage in both the superoinferior and anteroposterior directions. In addition, they compared translation between intact and reconstructed specimens and showed better superior stability after a Weaver-Dunn reconstruction with double-button augmentation than in the intact group. Boileau et al.10 described an arthroscopic technique for CC ligament reconstruction that consisted of (1) resecting the distal clavicle and creating a socket in its medullary canal, (2) rerouting the CA ligament with a bone block harvested from the tip of the acromion in a socket created in the distal clavicle (Chuinard's modification of the Weaver-Dunn procedure), and (3) augmenting the reconstruction with 2 titanium buttons.
Nevertheless, some cases of chronic ACJD are not arthritic. Distal clavicular excision is known to increase the instability of the ACJ, so there is no value in performing distal clavicular excision and obtaining the bony fragment from the acromion tip, which increases the operative time and risk of bleeding, as well as bony nonunion. Moreover, the AC ligament is attached to the apex of the acromion with many variations; it can be difficult to harvest it with a bone block from the tip of a type D acromion according to the Gagey classification (proximal CA ligament insertion at the inferior aspect of the acromion away from its apex), which represents 22.2% of the cases. It is impossible to revise this technique without resecting the graft.12
We reported a high rate of failure after using a U-shaped ligament around the coracoid to reconstruct the CC ligaments owing to friction and rupture of the ligament.13 Thus, we developed the described technique, which offers the advantages of arthroscopic techniques for management of associated pathology, better cosmetic results, less soft-tissue dissection, better visualization of both surfaces of the coracoid, and control of reduction in both the horizontal and vertical planes under direct arthroscopic visualization, with less risk of coracoid and clavicular fractures owing to the use of small 2.4-mm tunnels and CC tunnels being made in a staged fashion at the center of both the clavicle and coracoid, which we consider unfeasible when using the AC guide.
We consider it impossible to position an aiming device perfectly onto the clavicle and under the coracoid while trying to reduce the ACJ perfectly. Our technique takes advantage of the loop ligament, first, to perfectly drill the clavicle (2 oblique tunnels); second, to perfectly drill the coracoid process (1 tunnel); and third, to reduce the dislocated ACJ with the tensioning of the flexible and adjustable-loop ligament (3 stages in this procedure). Moreover, there is wide variation in the shape of the coracoid process, and it seems difficult to consider an aiming guide as universal.14 This technique offers better biomechanical properties of the suspensory fixation system used. The CA ligament retains its vascularity, which enhances the healing potential without any risk of donor-site morbidity or disease transmission (Table 1).
Table 1.
Advantages and Disadvantages of Technique
| Advantages |
| The transferred CA ligament retains its vascularity unlike free grafts. |
| There is no risk of associated morbidity from the use of autogenous graft. |
| There is no risk of disease transmission and no additional cost, in contrast to the use of allografts. |
| There is no need to harvest the acromion. |
| A double–clavicular button construct is biomechanically superior to a single–clavicular button construct. |
| There is less risk of fracture of the clavicle and coracoid. |
| The surgeon can judge the quality of the reduction by direct arthroscopic visualization. |
| There is no need for hardware removal. |
| The technique enables management of concomitant pathology. |
| Excellent cosmesis is achieved. |
| There is less risk of adhesions. |
| Disadvantages |
| Disturbance of shoulder kinematics and/or the CA arch has been claimed, but AC joint dislocations are more frequent in the young population in whom massive rotator cuff tears are not common. |
| The original CA ligament transfer without augmentation is biomechanically inferior to free grafts. |
| Evaluation of horizontal instability after use of this construct is lacking; future studies should focus on this point. |
AC, acromioclavicular; CA, coracoacromial.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.K. is a consultant for VIMS and DePuy Mitek and receives royalties from FH Orthopedics (Arrow shoulder prosthesis). Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Technique of arthroscopic coracoacromial (CA) ligament transfer augmented with V-shaped suspensory fixation system for chronic acromioclavicular (AC) joint dislocation. The patient is a 45-year-old man with a chronic right-sided type V AC joint dislocation. Besides the ordinary posterior portal, we use the marked portals and 2 skin incisions about 2 cm and 4 cm from the AC joint; 2 wires are inserted in the distal clavicle. Diagnostic arthroscopy is performed, followed by opening of the rotator interval and coracoid visualization with the conjoint tendon and CA ligament attached. After exposure of the subacromial space and undersurface of the distal clavicle, 2 shuttle relays are inserted into the 2 clavicular tunnels. After full dissection of the CA ligament, we use a shuttle relay to make a triple Krackow stitch to the CA ligament starting near the coracoid process until reaching its insertion in the acromion using a fiber force. Using a radiofrequency device, we detach the proximal attachment of the CA ligament from the undersurface of the acromion. Then, we use a supracoracoid portal to insert a guidewire in the central part of the base of the coracoid process. Next, we shuttle the suspensory loop construct from the undersurface of the coracoid; after that, we shuttle the 2 loops, with each loop in a separate clavicular tunnel. Finally, we stabilize the fiber force in the CA ligament through the lateral clavicular tunnel to the circular clavicular button over the clavicle with the lateral loop. After full reduction of the AC joint under arthroscopic control, we can tie and secure each loop. Postoperative radiographs are shown, in addition to range of motion after 1 month.
References
- 1.Barth J., Duparc F., Baverel L. Prognostic factors to succeed in surgical treatment of chronic acromioclavicular dislocations. Orthop Traumatol Surg Res. 2015;101(suppl 8):S305–S311. doi: 10.1016/j.otsr.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 2.Martetshläger F., Tauber M., Habermeyer P., Hawi N. Arthroscopically assisted acromioclavicular and coracoclavicular ligament reconstruction for chronic acromioclavicular joint instability. Arthrosc Tech. 2016;5:e1239–e1246. doi: 10.1016/j.eats.2016.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Le Hanneur M., Thoreson A., Delgrande D. Biomechanical comparison of anatomic and extra-anatomic reconstruction techniques using local grafts for chronic instability of the acromioclavicular joint. Am J Sports Med. 2018;46:1927–1935. doi: 10.1177/0363546518770603. [DOI] [PubMed] [Google Scholar]
- 4.Tauber M., Valler D., Lichtenberg S., Magosch P., Moroder P., Habermeyer P. Arthroscopic stabilization of chronic acromioclavicular joint dislocations: Triple- versus single-bundle reconstruction. Am J Sports Med. 2016;44:482–489. doi: 10.1177/0363546515615583. [DOI] [PubMed] [Google Scholar]
- 5.Tauber M., Gordon K., Koller H., Fox M., Resch H. Semitendinosus tendon graft versus a modified Weaver-Dunn procedure for acromioclavicular joint reconstruction in chronic cases: A prospective comparative study. Am J Sports Med. 2009;37:181–190. doi: 10.1177/0363546508323255. [DOI] [PubMed] [Google Scholar]
- 6.Beitzel K., Obopilwe E., Chowaniec D.M. Biomechanical comparison of arthroscopic repairs for acromioclavicular joint instability: Suture button systems without biological augmentation. Am J Sports Med. 2011;39:2218–2225. doi: 10.1177/0363546511416784. [DOI] [PubMed] [Google Scholar]
- 7.Menge T.J., Tahal D.S., Katthagen J.C., Millett P.J. Arthroscopic acromioclavicular joint reconstruction using knotless coracoclavicular fixation and soft-tissue anatomic coracoclavicular ligament reconstruction. Arthrosc Tech. 2017;6:e37–e42. doi: 10.1016/j.eats.2016.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lafosse L., Baier G.P., Leuzinger J. Arthroscopic treatment of acute and chronic acromioclavicular joint dislocation. Arthroscopy. 2005;21:1017. doi: 10.1016/j.arthro.2005.05.034. [DOI] [PubMed] [Google Scholar]
- 9.Hosseini H., Friedmann S., Tröger M., Lobenhoffer P., Agneskirchner J.D. Arthroscopic reconstruction of chronic AC joint dislocations by transposition of the coracoacromial ligament augmented by the Tight Rope device: A technical note. Knee Surg Sports Traumatol Arthrosc. 2009;17:92–97. doi: 10.1007/s00167-008-0633-8. [DOI] [PubMed] [Google Scholar]
- 10.Boileau P., Old J., Gastaud O., Brassart N., Roussanne Y. All-arthroscopic Weaver-Dunn-Chuinard procedure with double-button fixation for chronic acromioclavicular joint dislocation. Arthroscopy. 2010;26:149–160. doi: 10.1016/j.arthro.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 11.Zooker C.C., Parks B.G., White K.L., Hinton R.Y. Tight Rope versus fiber mesh tape augmentation of acromioclavicular joint reconstruction: A biomechanical study. Am J Sports Med. 2010;38:1204–1208. doi: 10.1177/0363546509359064. [DOI] [PubMed] [Google Scholar]
- 12.Kany J., Amaravathi R.S., Guinand R., Valenti P. Arthroscopic acromioclavicular joint reconstruction using a synthetic ligament device. Eur J Orthop Surg Traumatol. 2012;22:357–364. [Google Scholar]
- 13.Kany J., Guinand R., Croutzet P. All arthroscopic augmented Vargas procedure: An option after failed acromioclavicular joint dislocation reconstruction. A technical note. Orthop Traumatol Surg Res. 2016;102:669–672. doi: 10.1016/j.otsr.2015.12.022. [DOI] [PubMed] [Google Scholar]
- 14.Manal F., Cheah P.S., Ahmad U. Anatomic variation in morphometry of human coracoid process among Asian population. Biomed Res Int. 2017;2017:6307019. doi: 10.1155/2017/6307019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technique of arthroscopic coracoacromial (CA) ligament transfer augmented with V-shaped suspensory fixation system for chronic acromioclavicular (AC) joint dislocation. The patient is a 45-year-old man with a chronic right-sided type V AC joint dislocation. Besides the ordinary posterior portal, we use the marked portals and 2 skin incisions about 2 cm and 4 cm from the AC joint; 2 wires are inserted in the distal clavicle. Diagnostic arthroscopy is performed, followed by opening of the rotator interval and coracoid visualization with the conjoint tendon and CA ligament attached. After exposure of the subacromial space and undersurface of the distal clavicle, 2 shuttle relays are inserted into the 2 clavicular tunnels. After full dissection of the CA ligament, we use a shuttle relay to make a triple Krackow stitch to the CA ligament starting near the coracoid process until reaching its insertion in the acromion using a fiber force. Using a radiofrequency device, we detach the proximal attachment of the CA ligament from the undersurface of the acromion. Then, we use a supracoracoid portal to insert a guidewire in the central part of the base of the coracoid process. Next, we shuttle the suspensory loop construct from the undersurface of the coracoid; after that, we shuttle the 2 loops, with each loop in a separate clavicular tunnel. Finally, we stabilize the fiber force in the CA ligament through the lateral clavicular tunnel to the circular clavicular button over the clavicle with the lateral loop. After full reduction of the AC joint under arthroscopic control, we can tie and secure each loop. Postoperative radiographs are shown, in addition to range of motion after 1 month.