Abstract
Background
Heavy menstrual bleeding (HMB) is an important cause of ill health in women of reproductive age, causing them physical problems, social disruption and reducing their quality of life. Medical therapy has traditionally been first‐line therapy. Surgical treatment of HMB often follows failed or ineffective medical therapy. The definitive treatment is hysterectomy, but this is a major surgical procedure with significant physical and emotional complications, as well as social and economic costs. Less invasive surgical techniques, such as endometrial resection and ablation, have been developed with the purpose of improving menstrual symptoms by removing or ablating the entire thickness of the endometrium.
Objectives
To compare the effectiveness, acceptability and safety of techniques of endometrial destruction by any means versus hysterectomy by any means for the treatment of heavy menstrual bleeding.
Search methods
Electronic searches for relevant randomised controlled trials (RCTs) targeted—but were not limited to—the following: the Cochrane Gynaecology and Fertility Group's specialised register, CENTRAL via the Cochrane Register of Studies Online (CRSO), MEDLINE, Embase, PsycINFO, and the ongoing trial registries. We made attempts to identify trials by examining citation lists of review articles and guidelines and by performing handsearching. Searches were performed in 1999, 2007, 2008, 2013 and on 10 December 2018.
Selection criteria
Any RCTs that compared techniques of endometrial resection or ablation (by any means) with hysterectomy (by any technique) for the treatment of heavy menstrual bleeding in premenopausal women.
Data collection and analysis
Two review authors independently selected trials for inclusion, extracted data and assessed trials for risk of bias.
Main results
We identified nine RCTs that fulfilled our inclusion criteria for this review. For two trials, the review authors identified multiple publications that assessed different outcomes at different postoperative time points for the same women. No included trials used third generation techniques.
Clinical measures of improved bleeding symptoms and satisfaction rates were observed in women who had undergone hysterectomy compared to endometrial ablation. A slightly lower proportion of women who underwent endometrial ablation perceived improvement in bleeding symptoms at one year (risk ratio (RR) 0.89, 95% confidence interval (CI) 0.85 to 0.93; 4 studies, 650 women, I² = 31%; low‐quality evidence), at two years (RR 0.92, 95% CI 0.86 to 0.99; 2 studies, 292 women, I² = 53%) and at four years (RR 0.93, 95% CI 0.88 to 0.99; 2 studies, 237 women, I² = 79%). Women in the endometrial ablation group also showed improvement in pictorial blood loss assessment chart compared to their baseline (PBAC) score at one year (MD 24.40, 95% CI 16.01 to 32.79; 1 study, 68 women; moderate‐quality evidence) and at two years (MD 44.00, 95% CI 36.09 to 51.91; 1 study, 68 women). Repeat surgery resulting from failure of the initial treatment was more likely to be needed after endometrial ablation than after hysterectomy at one year (RR 16.17, 95% CI 5.53 to 47.24; 927 women; 7 studies; I2 = 0%), at two years (RR 34.06, 95% CI 9.86 to 117.65; 930 women; 6 studies; I2 = 0%), at three years (RR 22.90, 95% CI 1.42 to 370.26; 172 women; 1 study) and at four years (RR 36.32, 95% CI 5.09 to 259.21;197 women; 1 study). The satisfaction rate was lower amongst those who had endometrial ablation at two years after surgery (RR 0.87, 95% CI 0.80 to 0.95; 4 studies, 567 women, I² = 0%; moderate‐quality evidence), and no evidence of clear difference was reported between post‐treatment satisfaction rates in groups at other follow‐up times (1 and 4 years).
Most adverse events, both major and minor, were more likely after hysterectomy during hospital stay. Women who had an endometrial ablation were less likely to experience sepsis (RR 0.19, 95% CI 0.12 to 0.31; participants = 621; studies = 4; I2 = 62%), blood transfusion (RR 0.20, 95% CI 0.07 to 0.59; 791 women; 5 studies; I2 = 0%), pyrexia (RR 0.17, 95% CI 0.09 to 0.35; 605 women; 3 studies; I2 = 66%), vault haematoma (RR 0.11, 95% CI 0.04 to 0.34; 858 women; 5 studies; I2 = 0%) and wound haematoma (RR 0.03, 95% CI 0.00 to 0.53; 202 women; 1 study) before hospital discharge. After discharge from hospital, the only difference that was reported for this group was a higher rate of infection (RR 0.27, 95% CI 0.13 to 0.58; 172 women; 1 study).
Recovery time was shorter in the endometrial ablation group, considering hospital stay, time to return to normal activities and time to return to work; we did not, however, pool these data owing to high heterogeneity. Some outcomes (such as a woman’s perception of bleeding and proportion of women requiring further surgery for HMB), generated a low GRADE score, suggesting that further research in these areas is likely to change the estimates.
Authors' conclusions
Endometrial resection and ablation offers an alternative to hysterectomy as a surgical treatment for heavy menstrual bleeding. Both procedures are effective, and satisfaction rates are high. Although hysterectomy offers permanent and immediate relief from heavy menstrual bleeding, it is associated with a longer operating time and recovery period. Hysterectomy also has higher rates of postoperative complications such as sepsis, blood transfusion and haematoma (vault and wound). The initial cost of endometrial destruction is lower than that of hysterectomy but, because retreatment is often necessary, the cost difference narrows over time.
Plain language summary
A comparison of the effectiveness and safety of two different surgical treatments for heavy menstrual bleeding
Review question
Heavy menstrual bleeding (HMB) is menstrual blood loss that interferes with women's quality of life. Cochrane researchers compared two surgical treatments for women with HMB. The main factors (thought to be of greatest importance) were how well each operation was able to treat the symptoms of HMB, how women felt about undergoing each operation and what the complication rates were. Additional factors studied were how long each operation took to perform, how long women took to recover from the operation and how much the operation cost the hospital and the woman herself.
Background
Surgical treatments for HMB include removal or destruction of the inside lining (endometrium) of the womb (endometrial resection or ablation) and surgical removal of the whole womb (hysterectomy). Both methods are commonly offered by gynaecologists, usually after a non‐surgical treatment has failed to correct the problem. Endometrial resection/ablation is performed via the entrance to the womb, without the need for a surgical cut. During a hysterectomy, the uterus can be removed via a surgical cut to the abdomen, via the vagina, or via 'keyhole' surgery that involves very small surgical cuts to the abdomen (laparoscopy). Hysterectomy is effective in permanently stopping HMB, but it halts fertility and is associated with all the risks of major surgery, including infection and blood loss. These risks are smaller with endometrial resection/ablation.
Search date
A systematic review of the research comparing endometrial resection and ablation versus hysterectomy for the treatment of heavy menstrual bleeding was most recently updated in December 2018 by Cochrane researchers. After searching for all relevant studies, review authors included nine studies involving a total of 1300 women.
Study characteristics
Only randomised controlled trials (RCTs) are included: these are studies in which participants are randomly allocated to one of two groups, each receiving a different intervention. The two groups are then compared. This review included RCTs that compared endometrial ablation or resection and hysterectomy as treatment for heavy menstrual bleeding. The studies did not include women who had gone through menopause or had cancer (or precancer) of the uterus.
Key results and conclusions
The review of studies revealed that endometrial ablation/resection is an effective and possibly cheaper alternative to hysterectomy, with faster recovery, although retreatment with additional surgery is sometimes needed. Hysterectomy is associated with more definitive resolution of symptoms but there are longer operating times and greater potential for surgical complications. For both operations, women generally reported that undergoing the procedure was acceptable and that they were satisfied with their experience.
Laparoscopic hysterectomy has become more widely used and some outcomes such as duration of hospital stay, time to return to work and time to return to normal activities have become more comparable with those of endometrial ablation. However, laparoscopic hysterectomy is frequently associated with longer operating time than other modes of hysterectomy and requires specific surgical expertise and equipment.
Identifying harms
Both surgical treatments are considered to be generally safe, with low complication rates. Hysterectomy, however, is associated with higher rates of infection, requirement for blood transfusion, and haematoma (collection of blood in soft tissues after surgery).
Quality of the evidence
Evidence reported in this review was of moderate to low quality, suggesting that further research may change the result. This was the case for outcomes such as a woman’s perception of bleeding and proportion of women requiring further surgery for HMB.
Summary of findings
Summary of findings for the main comparison. Endometrial resection or ablation compared to hysterectomy for heavy menstrual bleeding.
| Endometrial resection‐ablation compared to hysterectomy for heavy menstrual bleeding. | ||||||
| Patient or population: heavy menstrual bleeding Setting: Intervention: endometrial resection/ablation Comparison: hysterectomy | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with hysterectomy | Risk with endometrial resection/ablation | |||||
| Woman's perception (proportion with improvement in bleeding symptoms) ‐ within 1 year of follow‐up | 978 per 1000 | 871 per 1000 (832 to 910) | RR 0.89 (0.85 to 0.93) | 650 (4 RCTs) | ⊕⊕⊝⊝ LOW 1 2 | |
| PBAC score (continuous data) ‐ at 1 year of follow‐up | The mean PBAC score (continuous data) was 29.6 | The mean PBAC score (continuous data) was 54 24.4 higher than the hysterectomy group (16.01 higher to 32.79 higher) |
‐ | 68 (1 RCT) | ⊕⊕⊕⊝ MODERATE 1 | |
| Proportion requiring further surgery for HMB ‐ within 1 year after surgery | 0 per 1000 | 121 per 1000** | RR 16.17 (5.53 to 47.24) | 927 (7 RCTs) | ⊕⊕⊝⊝ LOW 1 3 | |
| Proportion satisfied with treatment ‐ at 1 year of follow‐up | 820 per 1000 | 771 per 1000 (721 to 820) | RR 0.94 (0.88 to 1.00) | 739 (4 RCTs) | ⊕⊕⊕⊝ MODERATE 1 | |
| Adverse events—short term (intraoperative and immediate postoperative) ‐ Sepsis | 319 per 1000 | 61 per 1000 (38 to 99) | RR 0.19 (0.12 to 0.31) | 621 (4 RCTs) | ⊕⊕⊝⊝ LOW 1 2 | |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
** We are unable to anticipate the absolute risk of further surgery with Endometrial resection or ablation as the number of further surgery, at 1 year follow up, in the hysterectomy group was 0. This number represents the risk in the endometrial resection group from trial data. CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 Downgraded 1 level for risk of bias; lack of blinding (although unfeasible) is likely to bias women's responses
2 Downgraded 1 level for inconsistency; considerable heterogeneity
3 Downgraded 1 level for imprecision; wide confidence interval
Background
Description of the condition
Heavy menstrual bleeding (HMB) is excessive blood loss that interferes with women's quality of life, either physical, psychological, material or social (Munro 2011; NICE 2018). Many other terms are used as HMB synonyms, including menorrhagia, abnormal menstrual bleeding, abnormal uterine bleeding and disordered uterine bleeding. These terms have not always been universally defined, and considerable overlap and confusion between them have been noted in the existing literature (Woolcock 2008). In response to this confusion, the International Federation of Gynaecology and Obstetrics (FIGO) formally defined HMB as "the woman's perspective of increased menstrual volume, regardless of regularity, frequency, or duration" (Munro 2011).
HMB is a common presenting complaint for primary care services and a frequent reason for secondary referral, with 5% of women between 30 and 49 years of age seeking medical attention for the problem (Vessey 1992; Cooper 2011).
Personal perception is often what determines the need for treatment and assessment of outcomes afterwards.
Intervention for HMB should be aimed at correction of identified underlying causes, control of bleeding, amelioration of anaemia and improvement in quality of life measures, with the woman’s contraceptive requirements or desire for future fertility taken into account, along with individual preferences for treatment.
Description of the intervention
Many well‐established treatment options for HMB are available, including hormonal and non‐hormonal medications, but among women who do not desire future fertility or for whom medical treatment may be problematic, inconvenient or prolonged, surgical management may be preferred.
Until the mid‐1980s, hysterectomy was the only option for such women, and 60% of women presenting with HMB during this time underwent hysterectomy as a first‐line treatment (NICE 2007). Hysterectomy continues to be performed via the more traditional abdominal and vaginal routes, but minimally invasive techniques have been introduced for women with benign disease, and these techniques continue to be developed. Such approaches include the introduction of laparoscopic hysterectomy (total laparoscopic hysterectomy and laparoscopically assisted vaginal hysterectomy) in 1989 (Reich 1989); and single‐port laparoscopic hysterectomy in 2009 (Li 2012).
Considerable differences between types of approach have been noted with regard to intraoperative complications, duration of hospital stay, length of recovery and cost. However, as this review aims to compare hysterectomy with endometrial resection and ablation, we have pooled the results for hysterectomy by all approaches.
Endometrial ablation is a minimally invasive hysteroscopic surgical intervention for HMB involving removal or destruction of the endometrium. Since it was introduced in the 1990s, its popularity as an alternative to hysterectomy has grown (Fernandez 2011). An examination of the UK National Health Service (NHS) statistics in 2005 revealed that endometrial destruction was being performed more frequently than hysterectomy for benign HMB in the UK (Reid 2007). In a long‐term study with up to 25 years' follow‐up in the UK, only 25% of the woman with an endometrial resection or ablation underwent a subsequent hysterectomy; and 75% of the surgeries were in the first five years of follow‐up (Kalampolas 2017), suggesting endometrial ablation may have a role in limiting the number of hysterectomies performed. This, however, may also reflect progression through menopause for many of these women.
Endometrial resection and ablation techniques are classically divided, according to the requirement of hysteroscopy to perform the ablation, in first‐ and second‐generation techniques. First‐generation techniques require direct hysteroscopic vision throughout the procedure and include desiccation of the endometrium by way of rollerball endometrial ablation (REA) and transcervical resection of the endometrium with loop electrode. This can be useful to identify and remove other endometrial pathology such as polyps and fibroids. A potential complication of endometrial resection is systemic fluid overload due to absorption of hysteroscopic fluid; therefore careful intraoperative input/output fluid balance requires attention and documentation. The efficacy and safety of first‐generation techniques are often operator dependent.
Newer technologies were subsequently introduced; second‐ and third‐generation techniques are non‐hysteroscopic, are considered easier to perform, equally effective and safe (Madhu 2009), reporting lower complication rates of around 1% for bipolar ablation (Athanatos 2015; Laberge 2016). All of these techniques, with the exception of hydrothermal ablation and endometrial laser intrauterine thermal therapy, involve performing surgery with a hysteroscope, i.e. without direct visualisation. The second‐generation techniques have allowed widespread use of endometrial ablation, as they require less advanced hysteroscopic skill and do not necessitate intraoperative fluid balance. However, these procedures depend heavily on the surgical equipment itself for efficacy and safety. The difference between the second and third generation is that third‐generation techniques have replaced latex with silicone in the balloon and have active fluid circulation, which enables the total endometrial surface to receive equal heat distribution (Kumar 2016).
How the intervention might work
Hysterectomy is regarded as ‘definitive’ treatment for HMB with guaranteed amenorrhoea and cessation of fertility and little need for future treatment. However, hysterectomy by any route is associated with all the complications of major surgery, including intraoperative bleeding, infection and venous thromboembolism. Other reported complications include urinary incontinence and dyspareunia. Urinary tract injuries are an unusual hysterectomy complication, having an overall incidence in laparoscopic hysterectomy of 0.73% (bladder 0.05% to 0.66%, ureter 0.02% to 0.4%) (Adelman 2014).
Endometrial ablation is a less invasive surgical option for women with HMB, although a successful outcome after endometrial ablation is not guaranteed and further surgery is occasionally required (Nagele 1998; Bourdrez 2004). Endometrial resection/ablation is often chosen because of perceived short hospitalisation, quick return to normal functioning and avoidance of major surgery (Nagele 1998). Vaginal discharge and increased period pain are common complications following endometrial resection/ablation. Uncommon complications include intraoperative uterine perforation and associated pelvic organ injury from direct perforation or electrosurgical burns. Pregnancies occurring after endometrial ablation have been reported to be at higher risk of ectopic pregnancy, preterm birth and abnormality of placentation (Sharp 2012).
Why it is important to do this review
HMB is a common reason for women to seek treatment, and many choose a surgical option as first‐ or second‐line management. Surgical methods for treatment of HMB show a trend in favour of endometrial resection/ablation and towards newer endometrial resection/ablation techniques. In the late 1980s and early 1990s, 60% of women with HMB who were referred to a gynaecologist in the UK were treated with hysterectomy (Coulter 1991), but an examination of NHS statistics in 2005 revealed that endometrial destruction was being performed more frequently than hysterectomy for benign HMB in the UK (Reid 2007).
Despite this trend, many women still express a preference for first‐line hysterectomy (Kennedy 2002), and rates of different methods of hysterectomy are evolving.
As surgical techniques for both hysterectomy and endometrial resection/ablation continue to evolve, corresponding changes in success rates, outcomes and complications will be noted, necessitating regular comparison and review.
Objectives
To compare the effectiveness, acceptability and safety of techniques of endometrial destruction by any means versus hysterectomy by any means for the treatment of heavy menstrual bleeding.
Methods
Criteria for considering studies for this review
Types of studies
Published and non‐published randomised controlled trials (RCTs) were eligible for inclusion. We excluded quasi‐randomised trials.
Types of participants
Source of recruitment
Primary care, family planning and specialist clinics.
Inclusion criterion
Women of reproductive years with heavy menstrual bleeding (including both heavy regular periods (menorrhagia) and heavy irregular periods (metrorrhagia)), measured objectively or subjectively.
Exclusion criteria
Postmenopausal bleeding (> 1 year from the last period).
HMB caused by uterine malignancy or endometrial hyperplasia.
Iatrogenic causes of HMB (e.g. intrauterine coil devices).
Types of interventions
Endometrial resection and ablation (including first‐generation techniques, such as transcervical resection of the endometrium with loop electrode or rollerball; second‐generation techniques, such as endometrial ablation by thermal balloon, microwave, thermal free‐fluid, radiofrequency and cryotherapy); and third‐generation endometrial ablation techniques that are similar to the second‐generation techniques but have replaced latex with silicone in the balloon and have active fluid circulation.
Hysterectomy (by abdominal, vaginal and laparoscopic/laparoscopically assisted routes).
Types of outcome measures
Primary outcomes
Effectiveness (improvement in bleeding)
Woman's perception (proportion with improvement in bleeding symptoms).
PBAC (Pictorial Blood Loss Assessment Chart) score: a visual measure of amount of blood loss (clinically significant HMB correlates with a score > 100).*
Requirement for further surgery.
Acceptability
Proportion satisfied with treatment.
Safety (adverse outcomes)
Adverse events: short term (intraoperative and immediately postoperative).
Adverse events: long term (after hospital discharge).
Secondary outcomes
Quality of life scores (continuous data).
Quality of life (proportion with improvement).
Duration of surgery.
Duration of hospital stay.
Time to return to normal activity.
Time to return to work.
Total health service cost per woman.
Total individual cost per woman.
*PBAC score: a score over 100 suggests significantly heavy menstrual bleeding. A reduction from over 100 to under 100 would be clinically significant at an individual level.
Search methods for identification of studies
We searched all publications that would potentially describe RCTs comparing surgical techniques to resect or ablate the endometrium versus hysterectomy for the treatment of heavy menstrual bleeding. We consulted with the Cochrane Gynaecology and Fertility Group Information Specialist regarding our search strategies for identifying potential studies for inclusion.
Electronic searches
The original search was performed in 1999. Updated searches were performed in 2008, 2013 and 2018.
The two review authors searched the Gynaecology and Fertility Group's specialised register, ProCite platform (searched 10 December 2018; Appendix 1); CENTRAL via the Cochrane Register of Studies Online (CRSO), Web platform (searched 10 December 2018; Appendix 2); MEDLINE, OVID platform (searched from 1946 to 10 December 2018; Appendix 3); Embase, OVID platform (searched from 1980 to 10 December 2018; Appendix 4); PsycINFO, OVID platform (searched from 1806 to 10 December 2018; Appendix 5).
Searching other resources
The principal review author searched the following trial registers for ongoing trials: ClinicalTrials.gov (a service of the US National Institutes of Health); and the World Health Organization International Trials Registry Platform search portal (www.who.int/trialsearch/Default.aspx) in December 2018 (Appendix 6).
We also searched citation lists of all studies that appeared to meet the inclusion criteria of the review, studies found in the literature review stage of the introduction, other relevant studies and evidence‐based guidelines on the management of abnormal bleeding.
Data collection and analysis
We performed statistical analysis in accordance with guidelines described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). When possible, we pooled outcomes statistically.
Selection of studies
Trials for inclusion in the review were selected by two of the review authors (AL and IC or AL and SS in 2008, RJF and AL in 2013, RJF and MBR in 2019) after the search strategy described previously was employed. This task was undertaken independently, and the final list of included studies reflected consensus between the two review authors. Details of the screening and selection process are shown in Figure 1.
1.
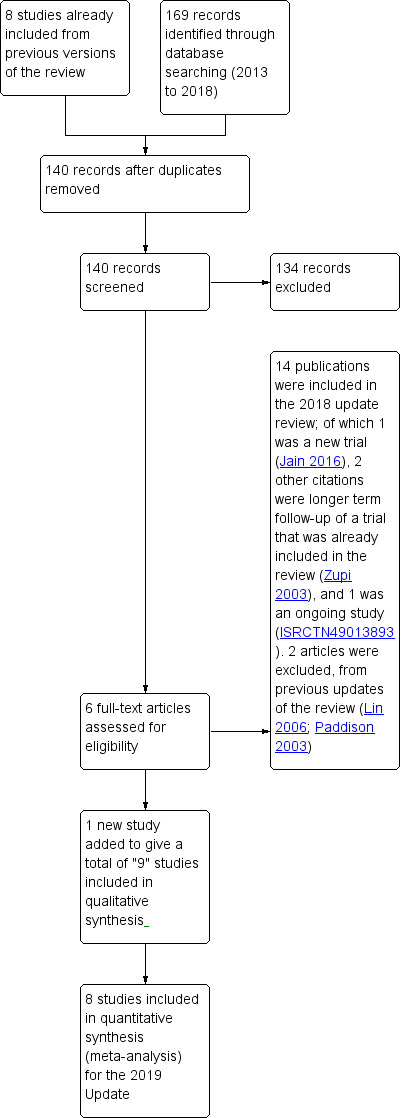
Study screening and selection process (2013 to 2018).
Data extraction and management
All assessments of characteristics of the included studies were performed independently by two review authors (AL and IC in 2008, RJF and AL in 2013, MBR and RJF in 2019) using forms designed according to Cochrane guidelines and described in Higgins 2011.
When necessary, additional information on trial methodology or original trial data were sought from the principal or corresponding author of any trials that appeared to meet the eligibility criteria (see Acknowledgements section for details of the study authors who provided clarification of data beyond that reported in the publications).
Quality criteria and methodological details were extracted from each study as follows.
Trial characteristics
Study design.
Numbers of women randomly assigned, excluded and lost to follow‐up.
Whether an intention‐to‐treat analysis was done.
Whether a power calculation was done.
Duration, timing and location of the study.
Number of centres.
Source of funding.
Characteristics of study participants
Age and any other recorded characteristics of participants in the study.
Other inclusion criteria.
Exclusion criteria.
Type of surgery.
Source of participants.
Proportion participating of those eligible.
Interventions used
Type of endometrial destruction technique used and route of hysterectomy performed.
Outcomes
Methods used to evaluate menstrual symptoms (e.g. PBAC score, woman‐defined 'improvement in symptoms').
Methods used to measure requirement for further surgery for HMB.
Methods used to evaluate participant satisfaction and change in quality of life post surgery.
Methods used to record adverse surgical events.
Methods used to measure resource and individual costs.
Methods used to measure duration of surgery, hospital stay and recovery time.
Assessment of risk of bias in included studies
Included trials were assessed for risk of bias using the 'Risk of bias tool' developed by the Cochrane Collaboration (known simply as 'Cochrane' since February 2015) and described in Higgins 2011.
Sequence generation (whether the allocation sequence was adequately generated to produce comparable groups).
Allocation concealment (whether the allocation was adequately concealed).
Blinding of participants, personnel and outcome assessors (whether knowledge of the allocated intervention was adequately controlled during the study).
Incomplete outcome data (whether incomplete outcome data were adequately addressed).
Selective outcome reporting (whether reports of the study were free of the suggestion of selective outcome reporting).
Other sources of bias (whether the study was apparently free of other problems that could put it at high risk of bias, e.g. baseline imbalance, bias related to study design, early termination of the study).
Details of the risk of bias for each included study are displayed in Characteristics of included studies and are summarised in Figure 2 and Figure 3.
2.
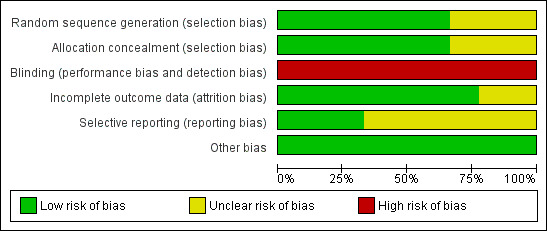
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
3.
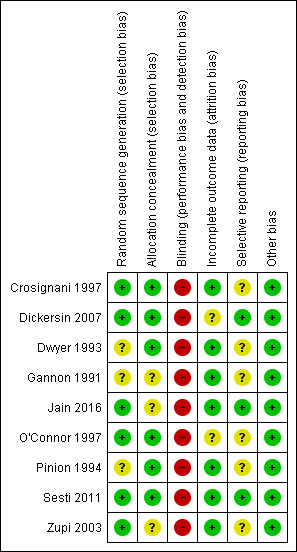
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Measures of treatment effect
For dichotomous data (e.g. number of adverse outcomes), we used the numbers of events in the control and intervention groups of each study to calculate risk ratios (RRs). For continuous data (e.g. PBAC score), if all studies reported exactly the same outcomes, we calculated mean differences (MDs) between treatment groups. If similar outcomes were reported on different scales, we calculated the standardised mean difference (SMD). We reversed the direction of effect of individual studies, if required, to ensure consistency across trials. We treated ordinal data (e.g. quality of life scores) as continuous data. We presented 95% confidence intervals (CIs) for all outcomes. When data needed to calculate RRs or MDs were not available, we utilised the most detailed numerical data available that may facilitate similar analyses of included studies (e.g. test statistics, P values). We compared the magnitude and direction of effect reported by studies versus how they were presented in the review, while taking account of legitimate differences.
For dichotomous data (e.g. proportion of participants satisfied with their treatment), results of each study were expressed as a risk ratio. For some dichotomous outcomes (e.g. proportion of participants requiring further surgery), a higher proportion represented a negative consequence of that treatment, and for other outcomes (e.g. proportion with improvement in menstrual blood loss), a higher proportion was considered a benefit of treatment. This approach to the categorising of outcomes should be noted when summary graphs for the meta‐analysis are viewed for assessment of benefits as opposed to harms of treatment. Thus, for some dichotomous outcomes, treatment benefit has been displayed as risk ratios and confidence intervals to the left of the centre line, but for others, a treatment benefit has been shown to the right of the centre line. Each outcome was labelled for clarification.
For other outcomes for which high values were considered a negative consequence of treatment—for example duration of surgery, length of hospital stay and time to return to work—evaluation of the summary graphs reveals that means and confidence intervals to the left were considered a benefit of endometrial destruction.
With one exception, quality of life scores were entered as continuous data—mean plus standard deviation values post treatment. One study, however, recorded the percentage mean change of EuroQol scores from baseline to four months after treatment. Some scales measured general quality of life summary score; others reported results separately in different categories, representing general quality of life but without a summary score; still others used more specific measurements of aspects of quality of life, such as anxiety, social adjustment and depression.
For some outcomes, women were assessed at different periods of follow‐up after surgery.
Menstrual symptoms were recorded at one, two, three and four years after surgery, PBAC scores at one and two years after surgery, and quality of life at four months and one, two and four years post treatment.
Adverse events were recorded before and after discharge from hospital.
Requirement for further surgery was measured separately within the first year and at two, three and four years after treatment.
Unit of analysis issues
The unit of analysis was the woman with HMB who was randomly assigned to endometrial resection/ablation or to hysterectomy.
Dealing with missing data
We analysed data on an intention‐to‐treat basis as far as possible; otherwise we only analysed available data. When we found that data were missing, we made attempts to obtain this information from the original trial authors.
Assessment of heterogeneity
We examined heterogeneity (variations) between the results of different studies by visual inspection of scatter of data points on the graphs and overlap in their confidence intervals. More formally, we examined the results of the I² statistic (a quantity that describes approximately the proportion of variation in point estimates that is due to heterogeneity rather than sampling error; Higgins 2008). When we found statistical heterogeneity to be very substantial (> 90%), we considered calculation of a summary effect measure to be inappropriate and we did not pool study data. Results of these studies can be viewed in forest plots that portray the range of values for comparison in each study.
Assessment of reporting biases
We aimed to avoid reporting bias by using a robust search strategy with no restrictions on language or publication forum. We identified multiple publications of the same study for several of the included studies and we have referenced them as such. If we had found 10 or more studies to include in the analysis we planned to use funnel plots to explore the possibility of small‐study effects.
Data synthesis
Combination of data was not always possible, as some outcomes were measured differently (e.g. some trials used PBAC score as a measure of improvement in bleeding, whilst others used proportion reporting improvement in bleeding symptoms, proportion with excessive bleeding, etc.). We displayed such data in the forest plots; however, often only one trial contributed data to each plot.
For continuous data (e.g. PBAC score), if all studies reported exactly the same outcomes we calculated mean differences (MDs) between treatment groups. We displayed continuous outcomes differently according to whether benefit or harm was measured. For most quality of life scores, a high score represented a benefit of treatment, but for the Hospital Anxiety and Depression Scale (HAD), a high score represented a greater degree of anxiety or depression. To present on the same graph quality of life scales that differed in this way, we displayed HAD scores as minus values, so that we could include all quality of life continuous outcomes in a single forest plot.
Subgroup analysis and investigation of heterogeneity
A priori, we planned to explore the possible contribution of differences in trial design to any heterogeneity identified in the manner described above under Assessment of heterogeneity.
We considered whether the clinical and methodological characteristics of the included studies were sufficiently similar for meta‐analysis to provide a meaningful summary. Where meta‐analyses were able to be performed, we checked for heterogeneity by visually inspecting the forest plots for evidence of poor overlap of the 95% CIs. More formally, we used the Chi2 test (with a P value < 0.10 being evidence of significance) and the I2 value. The Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) suggested a rough guide for interpretation of I2 values:
0% to 40% might not be important;
30% to 60% may represent moderate heterogeneity;
50% to 90% may represent substantial heterogeneity;
75% to 100% was considered substantial heterogeneity.
Sensitivity analysis
To assess the robustness of pooled estimates, we conducted the following sensitivity analysis.
Estimates based on all relevant trials regardless of evidence of allocation concealment versus estimates based on trials that provided clear evidence that allocation was concealed.
We planned but did not conduct the following analysis.
Estimates based on all relevant trials regardless of missing data and loss to follow‐up versus estimates based on trials in which incomplete outcome assessment was not likely to cause bias.
Overall quality of the body of evidence: 'Summary of findings' table
We generated Table 1 using GRADEpro software (GRADEpro GDT). This table evaluates the overall quality of the body of evidence for the main review outcomes (woman's perception (proportion with improvement in bleeding symptoms), PBAC score, proportion requiring further surgery for HMB, proportion satisfied with treatment, and adverse events‒short term) using GRADE criteria.
Study limitations (i.e. risk of bias).
Consistency of effect.
Imprecision.
Indirectness.
Publication bias.
We justified, documented and incorporated judgements about evidence quality (high, moderate, low or very low) into reporting of results for each of these main outcomes.
Results
Description of studies
We included nine RCTs comparing techniques of removal or ablation of endometrium versus hysterectomy by any route for the treatment of heavy menstrual bleeding, together with one ongoing trial. Four of these trials had multiple publications, each based on the same study population but providing assessment of different outcomes and different follow‐up times, as well as cost‐utility analyses of previously published data (Dickersin 2007; Dwyer 1993; Pinion 1994; Zupi 2003). We did not consider trials comparing different types of endometrial destruction in this review but they are assessed in Bofill Rodriguez 2019. Details of included studies can be found in the Characteristics of included studies table.
Study design
All included studies used a parallel‐group design. Seven of these studies were carried out at a single centre: three in Italy (Crosignani 1997; Sesti 2011; Zupi 2003); three in the UK (Dwyer 1993; Gannon 1991; Pinion 1994); and one in India (Jain 2016). One study was performed at nine centres throughout the UK (O'Connor 1997); and one study was completed at 25 centres in the USA and Canada (Dickersin 2007).
Participants
Participants in all included studies were premenopausal, had symptomatic heavy menstrual bleeding (regular or irregular prolonged or excessive bleeding) and were eligible for (i.e. had shown no response to medical treatment) or were awaiting hysterectomy. Participants in seven of the included studies had received a diagnosis of menorrhagia (heavy regular bleeding) (Crosignani 1997; Dwyer 1993; Gannon 1991; Jain 2016; O'Connor 1997; Sesti 2011; Zupi 2003), and participants in two of the studies had been given a diagnosis of dysfunctional uterine bleeding (which was defined as both regular and irregular ovulatory heavy bleeding and anovulatory abnormal bleeding not due to pathology) (Dickersin 2007; Pinion 1994). Exclusion criteria included large fibroids ((over 50% intramural extension (Crosignani 1997); or over 5 cm (Jain 2016)), large uterine size over 12 gestational weeks (Dwyer 1993; O'Connor 1997; Zupi 2003), pelvic inflammatory disease (PID) (Gannon 1991), and endometriosis (Gannon 1991) and abnormal pathology. Four studies excluded participants with submucosal fibroids (Crosignani 1997; Jain 2016; O'Connor 1997; Zupi 2003).
Interventions
Available data mostly compared first‐generation ablation techniques (predominantly transcervical resection of the endometrium (TCRE)) versus total hysterectomy. Two trials compared TCRE versus abdominal hysterectomy (Dwyer 1993; Gannon 1991); the former trial also included a preoperative procedure (medroxyprogesterone acetate injection four to six weeks before surgery) to reduce the thickness of the endometrium for participants undergoing endometrial resection. One trial compared endometrial resection versus vaginal hysterectomy (Crosignani 1997); another trial compared endometrial resection versus hysterectomy (50% abdominal, 50% vaginal) (O'Connor 1997); and another trial compared endometrial destruction after preoperative gonadotrophin‐releasing hormone (GnRH) treatment (50% endometrial resection and 50% laser ablation) versus hysterectomy (88% abdominal and 12% vaginal) (Pinion 1994). One study compared endometrial resection or thermal balloon ablation (according to surgeon's choice) versus total hysterectomy (vaginal, laparoscopic or abdominal approach, according to surgeon's choice) (Dickersin 2007); another study compared endometrial resection after preoperative GnRH agonist (GnRHa) treatment versus laparoscopic supracervical hysterectomy (Zupi 2003); and the final study compared thermal balloon endometrial ablation versus laparoscopic supracervical hysterectomy (Sesti 2011).
Outcomes
Follow‐up after surgery for all included studies ranged from four months to four years. Seven studies assessed change in menstrual bleeding patterns (Crosignani 1997; Dickersin 2007; Dwyer 1993; Gannon 1991; Jain 2016; Pinion 1994; Sesti 2011); five of these assessed whether menorrhagia‐like symptoms had resolved (amount and frequency of bleeding), one study (in which participants had a complaint of dysfunctional bleeding) measured separate components of bleeding excess (excessive amount and duration) and another study used PBAC questionnaires. Four studies assessed time to return to work in weeks (Crosignani 1997; Dwyer 1993; Gannon 1991; Pinion 1994). Two studies in which participants had a diagnosis of dysfunctional bleeding assessed whether an improvement in overall symptoms had occurred (recorded in one trial as 'problem solved') (Dickersin 2007; Pinion 1994). Three studies measured costs of treatment (Dwyer 1993; Gannon 1991; Pinion 1994).
Four studies assessed satisfaction with surgery (Crosignani 1997; Dwyer 1993; O'Connor 1997; Pinion 1994) (although this was reported at different follow‐up times); postoperative complications were reported by five trials (Gannon 1991; Jain 2016; O'Connor 1997; Pinion 1994; Sesti 2011); and duration of surgery was reported in six trials (Crosignani 1997; Dwyer 1993; Gannon 1991; Jain 2016; O'Connor 1997; Zupi 2003). Seven studies assessed hospital stay (Crosignani 1997; Dwyer 1993; Gannon 1991; Jain 2016; O'Connor 1997; Pinion 1994; Zupi 2003); and requirement for further surgery was reported by eight trials (Crosignani 1997; Dickersin 2007; Dwyer 1993; Gannon 1991; Jain 2016; O'Connor 1997; Pinion 1994; Zupi 2003).
Some outcomes measured time of surgery or recovery time and strictly speaking were time‐to‐event outcomes, such as duration of surgery, length of stay in hospital and time to return to normal activities and work. However, these were analysed as continuous data, as all participants had initial and end values representing the time that had elapsed. Time‐to‐event analysis is mandatory when censoring is performed and only a subset of participants have an event, but the authors in this review considered comparison of means to be an acceptable analysis.
Seven studies assessed quality of life after surgery (Crosignani 1997; Dickersin 2007; Dwyer 1993; O'Connor 1997; Pinion 1994; Sesti 2011; Zupi 2003), but several different scales were used. This review has assessed quality of life as measured by the Golombok Rust Inventory of Marital State (one year after surgery), the Short Form‐36 Scale (SF‐36), the EuroQol Visual Analogue Scale, the Hospital Anxiety and Depression Scale (HAD) and the Sabbatsberg Sexual Rating Scale (all one or two years after surgery). The SF‐36 is a generic measure of subjective health in the form of a profile with eight multi‐item dimensions (including physical and emotional role limitation, physical and social functioning, mental health, energy, pain and general health perception) developed in the USA and shown to be an acceptable tool when used by women with HMB (Coulter 1994; Ware 1993). The EuroQol health instrument is a generic single index measure of health‐related quality of life validated in several European countries, including the UK (Brazier 1993; EuroQol Group 1990). The Golombok Rust Inventory was modified by the investigators to obtain a brief measure of the overall quality of the marital relationship (Rust 1986), and the Sabbatsberg Sexual Rating Scale was designed to provide a self‐assessment of sexual functioning by women engaging in intercourse (Garrat 1995). The Hospital Anxiety and Depression Scale is a self‐assessment mood scale specifically designed to identify states of anxiety and depression and is regarded as a valid measure of the severity of these mood disorders (Zigmond 1983). Several other scales were used to evaluate aspects of quality of life in some of the trials, including the SF‐12, General Health Questionnaire, the Psychosocial Adjustment to Illness Scale, a psychiatric mood scale, a modified social adjustment scale and an unvalidated questionnaire, but we did not enter these outcomes into the review because the data were not obtained in a suitable form for inclusion in a meta‐analysis (quantitative data provided in graphical form indicated significant skew; data could not be obtained from study authors).
Five publications from three trials (Cameron 1996 and Aberdeen 1999 from the Pinion 1994 study; Gannon 1991; and Sculpher 1998 and Sculpher 1996 from the Dwyer 1993 study) compared costs to the health service of the two techniques. Two of these trials had two publications reporting total health resource costs of the procedures (including the need for retreatment) at different follow‐up times (Cameron 1996 and Aberdeen 1999 (Pinion 1994); Sculpher 1993 and 1996 (Dwyer 1993). One trial measured direct costs to the participant after one year (Cameron 1996 (Pinion 1994)).
Four publications from two trials (Sculpher 1993 and Sculpher 1996 from Dwyer 1993, and Cameron 1996 and Aberdeen 1999 from Pinion 1994) calculated cost per participant based on resource use. The third trial calculated costs by summing the average costs of variable resources and then adding a factor of 100% to allow for fixed costs (Gannon 1991).
Results of the search
We updated the search in December 2018 and included 140 additional potential references. Two review authors (MB and CL) screened titles and abstracts. We obtained full‐text copies of six references that appeared to meet the inclusion criteria; three were re‐publication of a trial already included in the 2013 review and were added to the included studies, one was a long‐term follow‐up of a trial already included in the review (Zupi 2003), one was an ongoing study (ISRCTN49013893), and one was an additional new trial to be included (Jain 2016), leading to a total of nine trials in the updated review.
Included studies
Nine RCTs of endometrial resection/ablation versus hysterectomy with a total of 1300 randomly assigned participants met the criteria for inclusion in the review, although not all participants contributed to the assessment of every outcome. Six authors were contacted for further details: two replied (Crosignani 1997; Dickersin 2007); four did not (Dwyer 1993; Gannon 1991; Pinion 1994; Zupi 2003)
Excluded studies
In the 2008 update of this review, two studies were retrieved for closer inspection and were excluded from the review (Paddison 2003; Lin 2006). One study had allocation according to date of admission and did not satisfy the criteria for true randomisation, and the other was a review of ablation versus hysterectomy.
No further studies were retrieved for closer inspection but subsequently excluded in the 2013 and 2019 updates of the review.
Risk of bias in included studies
We assessed all included studies separately for risk of bias (Higgins 2011). We provide a summary of these assessments in Figure 2 and Figure 3.
Allocation
Six of the nine included studies provided sufficient detail on the adequacy of the randomisation method (Crosignani 1997; Dickersin 2007; Jain 2016; O'Connor 1997; Sesti 2011; Zupi 2003), all at low risk of bias. The other three studies did not describe how randomisation was undertaken and were therefore at unclear risk of bias in this category.
All but three studies provided sufficient details of allocation concealment (Gannon 1991; Jain 2016; Zupi 2003); these three studies were therefore at unclear risk of bias, and all other studies were at low risk of bias in this category.
Blinding
Three of the more recent studies used single blinding for assessment of some outcomes (Dickersin 2007; Sesti 2011; Zupi 2003). The other six studies did not appear to have any blinding of participants, investigators or assessors. All studies were therefore at high risk of bias in this category.
Incomplete outcome data
In two studies (Dickersin 2007; O'Connor 1997), withdrawal from the study and/or missing data were greater than 10%, and explanations were not provided to enable judgement of whether this could have biased the results. In one trial (Dickersin 2007), primary outcomes were analysed by an intention‐to‐treat method (satisfaction rate, quality of life and bleeding outcomes), but intraoperative and perioperative outcomes (adverse events, requirement for further surgery and hospital stay) were analysed according to surgery received. This trial also reported outcomes at three and four years' follow‐up, but as women who were assigned later during the trial had shorter follow‐up, these assessments are likely to be underpowered. The other seven studies had withdrawals of less than 10% at the time of calculation of outcomes at the first time point. However, in studies with longer follow‐up, additional loss to follow‐up increased with the duration of the trial.
Selective reporting
Sufficient information was provided in only one study to indicate that it was free of selective outcome reporting (Dickersin 2007). Before publication of the study results, an earlier publication provided details of the study protocol and changes made throughout the study (Dickersin 2007: 2003 paper on Dickersin 2007). Two studies reported all the outcomes that were previously specified (Jain 2016; Sesti 2011). The other studies did not provide any evidence of measures taken to prevent selective outcome reporting.
Other potential sources of bias
In all of the studies, groups were balanced at baseline. In three studies the prior experience of the operating surgeon was described (Gannon 1991; O'Connor 1997; Zupi 2003). This was not described in the remainder of the studies, however, and could be a potential source of bias, as a less experienced surgeon for either treatment group could alter results such as duration of surgery, adverse outcomes and, in the case of endometrial ablation, effectiveness.
Effects of interventions
See: Table 1
1 Endometrial resection and ablation versus hysterectomy
Primary outcomes
Effectiveness
Hysterectomy is probably associated with better bleeding outcomes when compared to endometrial ablation. These were assessed in different ways in the trials, and we could not pool all outcomes.
1.1 Woman's perception (proportion with improvement in bleeding symptoms)
Five trials assessed whether bleeding symptoms were perceived as improved (Crosignani 1997; Dickersin 2007; Dwyer 1993; Gannon 1991; Pinion 1994). Women randomly assigned to endometrial ablation were less likely to show improvement in bleeding symptoms when compared with those randomly assigned to hysterectomy at one year (RR 0.89, 95% confidence interval (CI) 0.85 to 0.93; 4 studies, 650 women, I² = 31%; low‐quality evidence) (Dickersin 2007; Dwyer 1993; Gannon 1991; Pinion 1994). Differences were also noted at later stages of follow‐up, but the effect reduced over time: at two years (RR 0.92, 95% CI 0.86 to 0.99; 2 studies, 292 women, I² = 53%) (Crosignani 1997; Dickersin 2007); and at four years (RR 0.93, 95% CI 0.88 to 0.99; 2 studies, 237 women, I² = 79%; Figure 4; Analysis 1.1) (Dickersin 2007; Pinion 1994).
4.
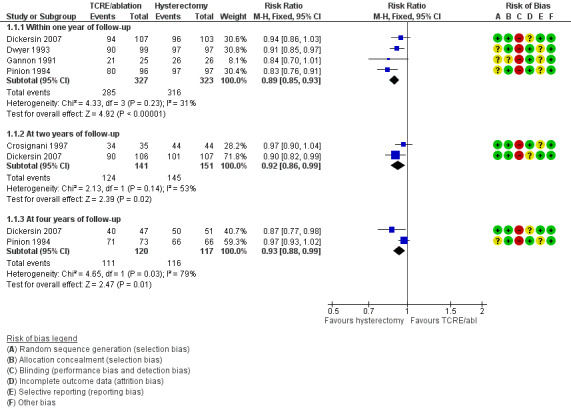
Forest plot of comparison: 1 Endometrial resection/ablation versus hysterectomy, outcome: 1.1 Woman's perception (proportion with improvement in bleeding symptoms).
1.1. Analysis.
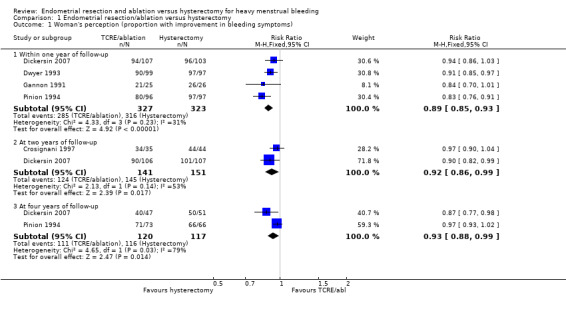
Comparison 1 Endometrial resection/ablation versus hysterectomy, Outcome 1 Woman's perception (proportion with improvement in bleeding symptoms).
1.2 PBAC score
One trial assessed menstrual blood loss using the PBAC (Pictorial Blood Loss Assessment Chart) score (Sesti 2011). Compared with pretreatment scores, the PBAC score was clearly reduced in both groups at one and two years postoperatively; however, this finding overall favoured women randomly assigned to hysterectomy at one year (MD 24.40, 95% CI 16.01 to 32.79; 1 study, 68 women), and even more so at two years (MD 44.00, 95% CI 36.09 to 51.91; 1 study, 68 women; moderate‐quality evidence, Analysis 1.2).
1.2. Analysis.
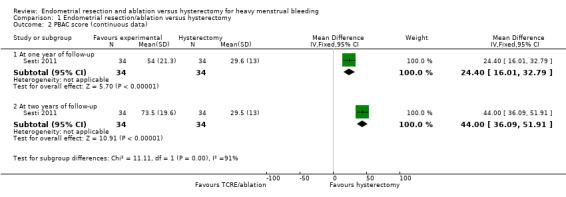
Comparison 1 Endometrial resection/ablation versus hysterectomy, Outcome 2 PBAC score (continuous data).
1.3 Requirement for further surgery
Risk of repeat surgery for failure of the initial surgical treatment was reported at different follow‐up times. Six trials reported the requirement for further surgery at one year's follow‐up (Crosignani 1997; Dwyer 1993; Gannon 1991; O'Connor 1997; Pinion 1994; Zupi 2003); and six reported at two years' follow‐up (Crosignani 1997; Dickersin 2007; Dwyer 1993; O'Connor 1997; Sesti 2011; Zupi 2003). One trial reported it at three years' follow‐up (O'Connor 1997); and one at four years' follow‐up (Pinion 1994). The risk of having a further surgery for treatment failure was more likely for TCRE/ablation than for hysterectomy at all follow‐up periods (all eight trials contributed data for at least one time point): within the first year (RR 16.17, 95% CI 5.53 to 47.24; 7 studies, 927 women, I² = 0%; low‐quality evidence), at two years (RR 34.06, 95% CI 9.86 to 117.65; 6 studies, 930 women, I² = 0%), at three years (RR 22.90, 95% CI 1.42 to 370.26; 1 study, 172 women), and at four years (RR 36.32, 95% CI 5.09 to 259.21; 1 study, 197 women) (Figure 5; Analysis 1.3). One study reported three requirements for further surgery on the hysterectomy group, but two were oophorectomies and one cystoscopy for persistent urinary symptoms after the surgery (O'Connor 1997), but no further surgery for HMB. One study reported 14 years' follow‐up with clear evidence of difference favouring hysterectomy (RR 19.60, 95% CI 1.15 to 333.63; 1 study, 153 women), but with more than 20% lost to follow‐up in the ablation group (18 women; 11 declined to participate and 7 could not be contacted).
5.
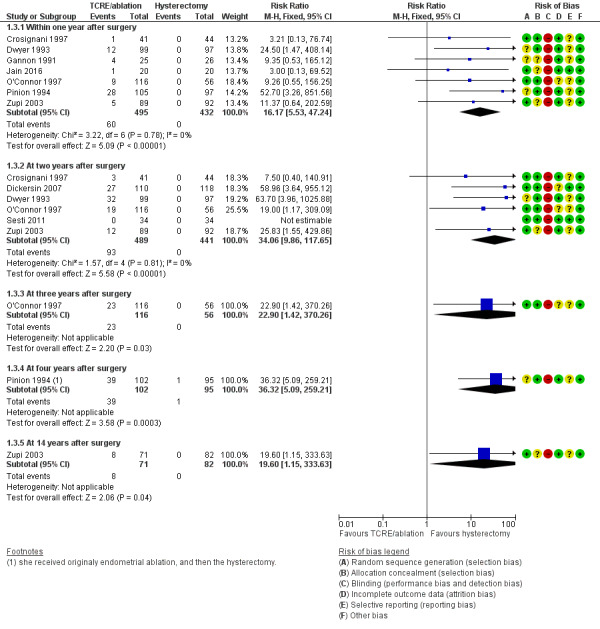
Forest plot of comparison: 1 Endometrial resection/ablation versus hysterectomy, outcome: 1.3 Proportion requiring further surgery for HMB.
1.3. Analysis.
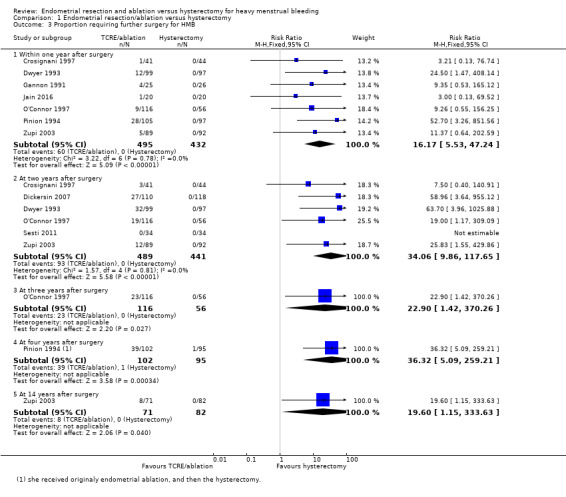
Comparison 1 Endometrial resection/ablation versus hysterectomy, Outcome 3 Proportion requiring further surgery for HMB.
Acceptability
1.4 Proportion satisfied with treatment
Satisfaction (very or moderately satisfied) rates were compared in five trials (Crosignani 1997; Dickersin 2007; Dwyer 1993; O'Connor 1997; Pinion 1994). Although satisfaction rate was lower amongst those who had endometrial ablation at two years after surgery (RR 0.87, 95% CI 0.80 to 0.95; 4 studies, 567 women, I² = 0%; moderate‐quality evidence), no evidence of clear difference was reported between post‐treatment satisfaction rates in groups at other follow‐up times (1 and 4 years) (Figure 6; Analysis 1.4).
6.
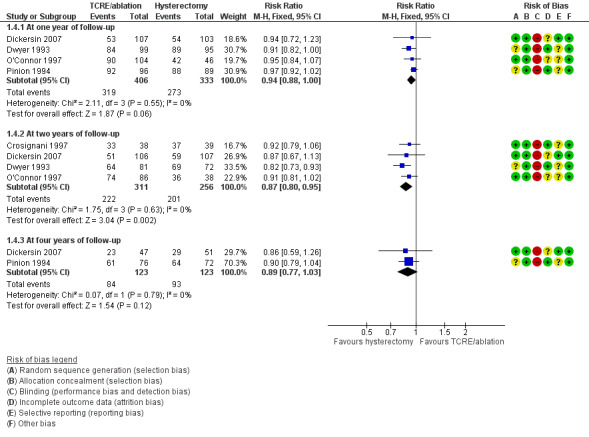
Forest plot of comparison: 1 Endometrial resection/ablation versus hysterectomy, outcome: 1.4 Proportion satisfied with treatment.
1.4. Analysis.
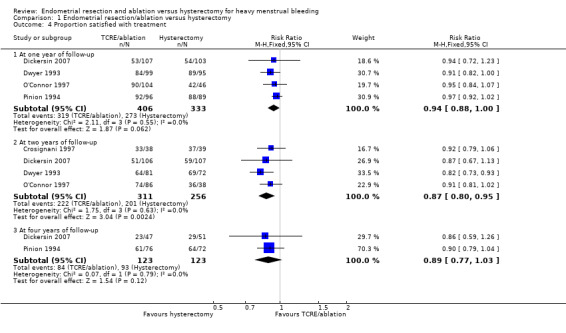
Comparison 1 Endometrial resection/ablation versus hysterectomy, Outcome 4 Proportion satisfied with treatment.
Safety (adverse events)
1.5 Adverse events: short term (intraoperative and immediately postoperative)
Six trials reported short‐term adverse effects, assessing sixteen different types (Figure 7; see Analysis 1.5) (Dickersin 2007; Dwyer 1993; Gannon 1991; O'Connor 1997; Pinion 1994; Zupi 2003). Other than sepsis, there was no clear evidence of difference between groups regarding (eventually) life‐threatening complications.
7.
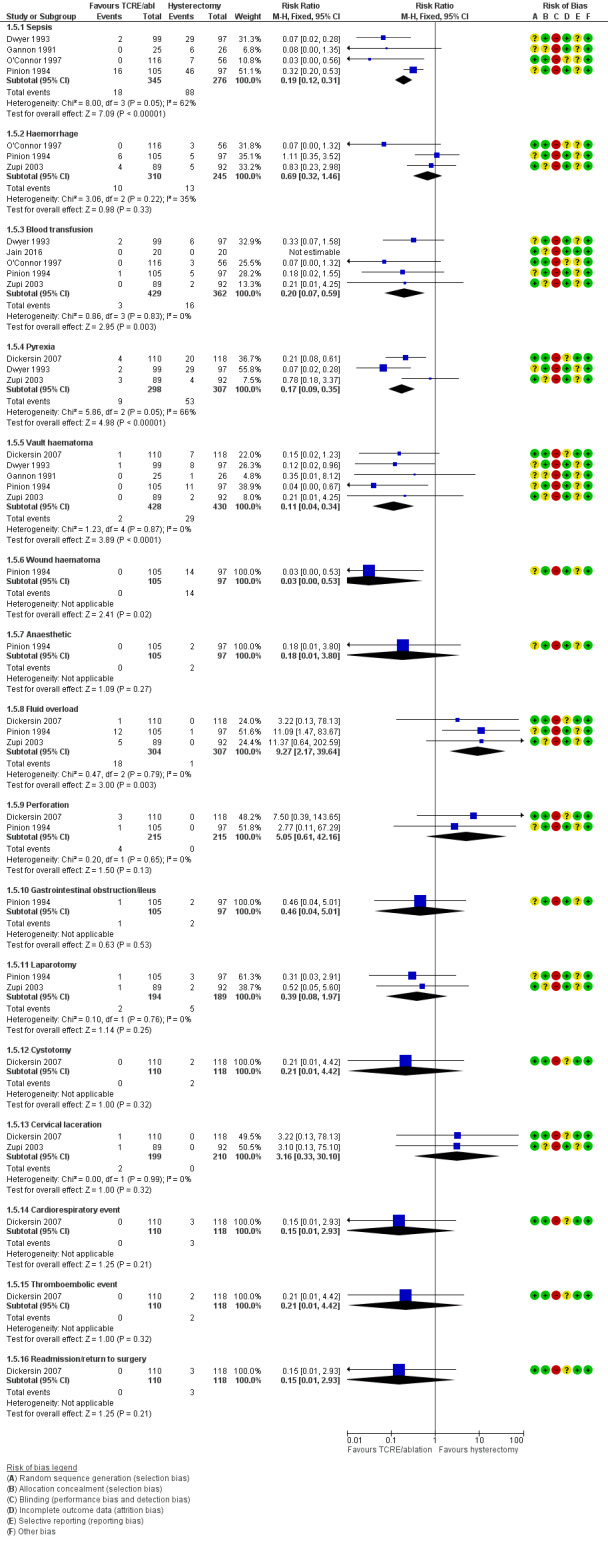
Forest plot of comparison: 1 Endometrial resection/ablation versus hysterectomy, outcome: 1.5 Adverse events—short term (intraoperative and immediate postoperative).
1.5. Analysis.
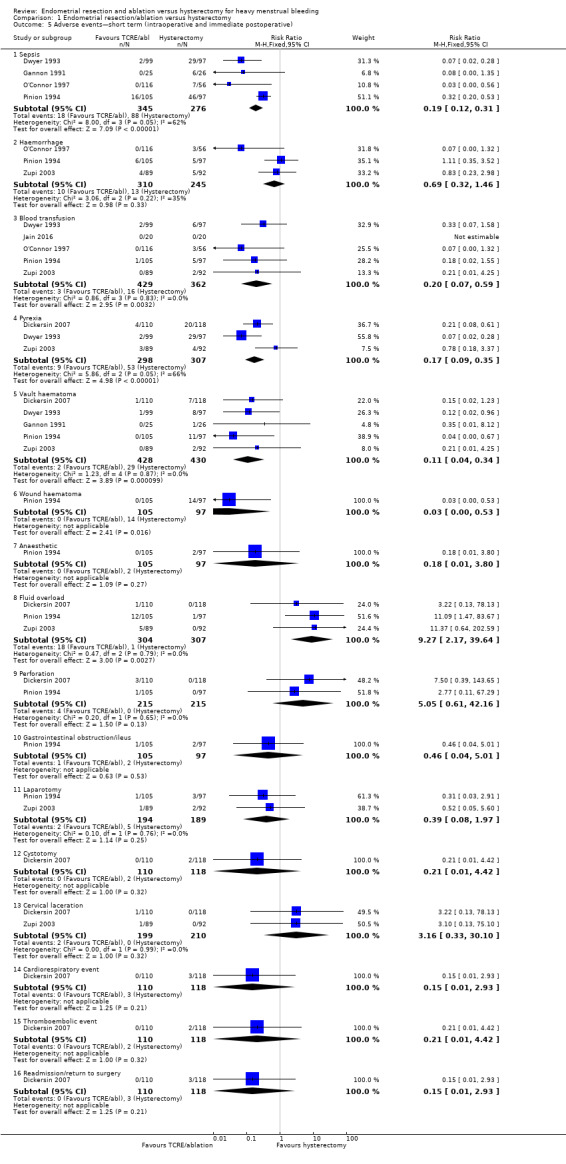
Comparison 1 Endometrial resection/ablation versus hysterectomy, Outcome 5 Adverse events—short term (intraoperative and immediate postoperative).
There was clear evidence of difference between endometrial resection or ablation and hysterectomy favouring endometrial resection or ablation in the following adverse effects.
Sepsis (RR 0.19, 95% CI 0.12 to 0.31; 621 women; 4 studies; I2 = 62%; low‐quality evidence) (Dwyer 1993; Gannon 1991; O'Connor 1997; Pinion 1994).
Blood transfusion (RR 0.20, 95% CI 0.07 to 0.59; 5 studies, 791 women, I² = 0%) (Dwyer 1993; Jain 2016; O'Connor 1997; Pinion 1994; Zupi 2003).
Pyrexia ((RR 0.17, 95% CI 0.09 to 0.35; participants = 605; studies = 3; I2 = 66%) (Dickersin 2007; Dwyer 1993; Zupi 2003)
Vault haematoma (RR 0.10, 95% CI 0.04 to 0.30; 5 studies, 858 women, I² = 0%) (Dickersin 2007; Dwyer 1993; Gannon 1991; Pinion 1994; Zupi 2003).
Wound haematoma ((RR 0.03, 95% CI 0.00 to 0.53; 202 women; 1 study) (Pinion 1994).
However, there was clear evidence of difference between endometrial resection or ablation and hysterectomy favouring hysterectomy in fluid overload (RR 9.27, 95% CI 2.17 to 39.64; 611 women; 3 studies; I2 = 0%) (Dickersin 2007; Pinion 1994; Zupi 2003).
There was no clear evidence of difference between groups for:
haemorrhage (RR 0.69, 95% CI 0.32 to 1.46; 3 studies, 555 women, I² = 35%);
anaesthetic complications (RR 0.18, 95% CI 0.01 to 3.80, 1 study, 202 women) (Pinion 1994);
perforation (RR 5.05, 95% CI 0.61 to 42.16; 2 studies, 430 women, I² = 0%) (Dickersin 2007; Pinion 1994);
gastrointestinal obstruction (RR 0.46, 95% CI 0.04 to 5.01; 1 study, 202 women) (Pinion 1994);
laparotomy (RR 0.39, 95% CI 0.08 to 1.97; 2 studies, 383 women, I² = 0%) (Pinion 1994; Zupi 2003);
cystotomy (RR 0.21, 95% CI 0.01 to 4.42; 1 study, 228 women) (Dickersin 2007);
cervical laceration (RR 3.16, 95% CI 0.33 to 30.10; 409 women; 2 studies; I2 = 0%) (Dickersin 2007; Zupi 2003)
cardiorespiratory event (RR 0.15, 95% CI 0.01 to 2.93; 228 women; 1 study) (Dickersin 2007);
thromboembolic event (RR 0.21, 95% CI 0.01 to 4.42, 1 study, 228 women) (Dickersin 2007);
readmission or return to surgery as causes of postoperative complications (RR 0.15, 95% CI 0.01 to 2.93; 1 study, 228 women) (Dickersin 2007)
1.6 Adverse events: long term (after hospital discharge)
Adverse events after hospital discharge were reported in two trials (Dwyer 1993; O'Connor 1997). There was clear evidence of difference in sepsis rate between the two groups favouring endometrial resection or ablation ((RR 0.27, 95% CI 0.13 to 0.58; 1 study, 172 women) (O'Connor 1997).
There was no clear evidence of difference between groups after hospital discharge in terms of haematoma (RR 0.59, 95% CI 0.15 to 2.37; 2 studies, 368 women, I² = 0%) (Dwyer 1993; O'Connor 1997); and haemorrhage (RR 2.94, 95% CI 0.12 to 71.30; 1 study, 196 women) (Dwyer 1993).
No other adverse events were reported. See Figure 8; Analysis 1.6.
8.
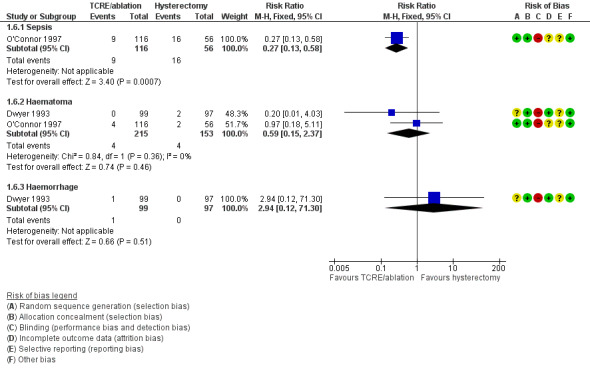
Forest plot of comparison: 1 Endometrial resection/ablation versus hysterectomy, outcome: 1.6 Adverse events—long term (after hospital discharge).
1.6. Analysis.
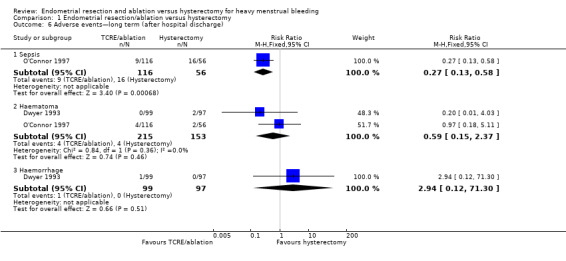
Comparison 1 Endometrial resection/ablation versus hysterectomy, Outcome 6 Adverse events—long term (after hospital discharge).
Secondary outcomes
Quality of life
Quality of life was measured by a number of validated scales. It was not possible to combine scales, as the domains differed, measuring different aspects of quality of life.
1.7 Quality of life scores (continuous data)
We detected clear evidence of difference between groups in five domains of the SF‐36 scale measured one and two years after surgery.
There was clear evidence of difference between groups favouring hysterectomy in:
social functioning at one year (MD ‐21.20, 95% CI ‐24.73 to ‐17.67, 1 study, 181 women) (Zupi 2003); and two years (MD ‐10.06, 95% CI ‐13.55 to ‐6.58; 3 studies, 300 women, I² = 25%) (Crosignani 1997; Dwyer 1993; Sesti 2011);
pain at two years (MD −9.50, 95% CI −12.80 to −6.20; 4 studies, 513 women, I² = 63%) (Crosignani 1997; Dickersin 2007; Dwyer 1993; Sesti 2011);
Energy at one year (MD ‐10.99, 95% CI ‐14.45 to ‐7.53, 211 women,2 studies; I² = 0%) (Dickersin 2007; Zupi 2003);
General health perception at one year (MD ‐7.27, 95% CI ‐10.72 to ‐3.81; 2 studies, 385 women, I² = 81%) (Dickersin 2007; Sesti 2011); and two years (MD ‐7.42, 95% CI ‐10.64 to ‐4.20; 4 studies, 509 women, I² = 41%) (Crosignani 1997; Dickersin 2007; Dwyer 1993; Sesti 2011).
There was clear evidence of difference between groups favouring endometrial ablation and resection in:
emotional role limitation at two years (MD 10.22, 95% CI 5.48 to 14.96; 3 studies, 300 women, I² = 92%) (Crosignani 1997; Dwyer 1993; Sesti 2011).
We noted no clear evidence of differences in SF‐36 scores between the two interventions in the domains of physical role limitation, mental health and physical functioning (Figure 9; Analysis 1.7).
9.
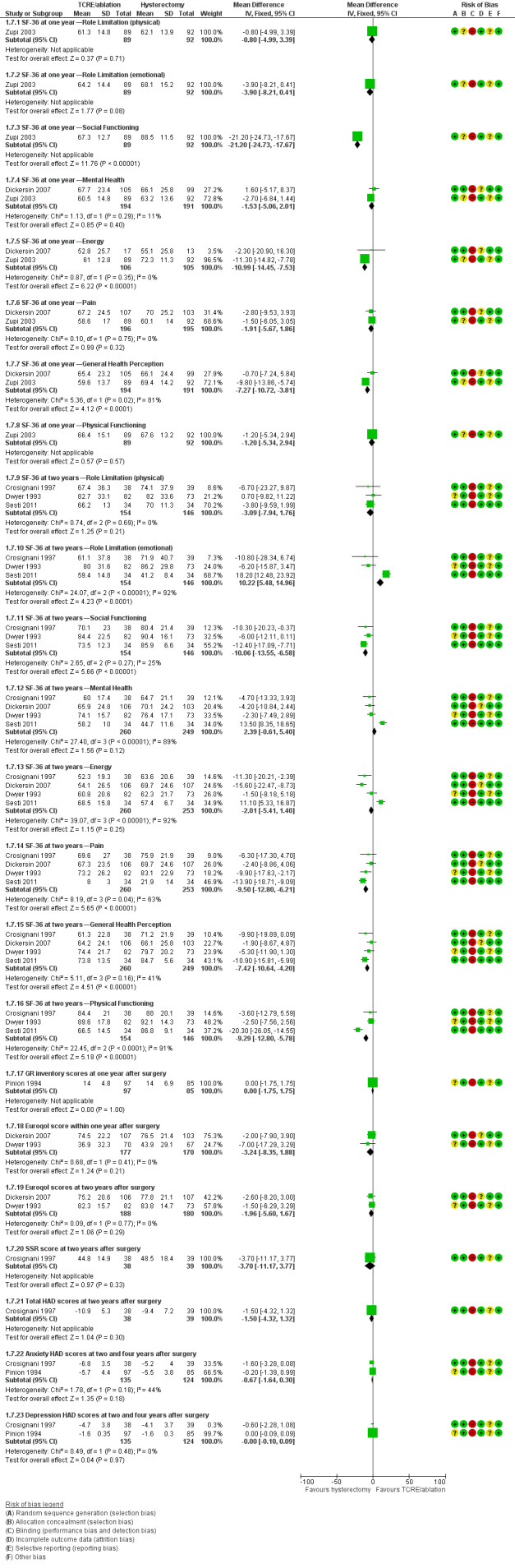
Forest plot of comparison: 1 Endometrial resection/ablation versus hysterectomy, outcome: 1.7 Quality of life scores (continuous data).
1.7. Analysis.
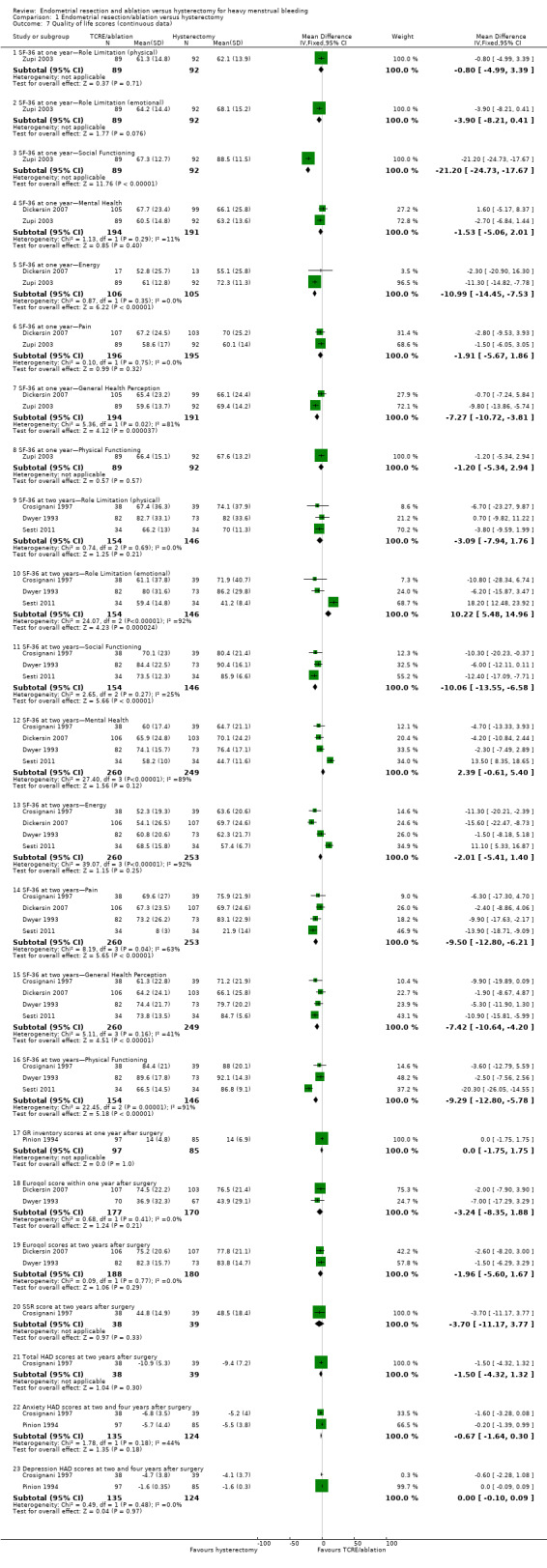
Comparison 1 Endometrial resection/ablation versus hysterectomy, Outcome 7 Quality of life scores (continuous data).
1.8. Quality of life at 14 years' follow‐up
One trial reported physical and mental quality of life at 14 years' follow‐up (Zupi 2003), suggesting a higher quality of life in the hysterectomy group compared to the ablation group. The physical component ranged from 57.50 to 51.40 for the hysterectomy group and from 55.04 to 45.40 for the ablation group. On the mental component, the hysterectomy group ranged from 56.80 to 50.40 and the ablation group ranged from 51.90 to 36.10. We could not enter these data on the meta‐analysis (See Analysis 1.8)
1.8. Analysis.
Comparison 1 Endometrial resection/ablation versus hysterectomy, Outcome 8 Quality of life at 14 years follow up.
| Quality of life at 14 years follow up | |||
|---|---|---|---|
| Study | Hysterectomy group | Endometrial ablation group | Heading 3 |
| Zupi 2003 | Physical score ranged from 57.5 to 51.4 Mental score ranged from 56.8 to 50.4 |
Physical score ranged from 55.04 to 45.4 Mental score ranged from 51.9 to 36.1 |
P < 0.0001 (for both) |
1.9 Quality of life (proportion with improvement)
Differences between groups were not reported in quality of life dimensions as measured by any of the other scales: Golombok Inventory, EuroQol scale, Sabbatsberg scale or HAD scale. The dichotomous outcome of proportion with improvement in pain at two years did not differ between surgical groups. However, a greater proportion of those who had undergone a hysterectomy reported an improvement in their general health one year after surgery when compared with those who had received TCRE/ablation (RR (Non‐event) 4.17, 95% CI 1.47 to 11.85; 1 study, 185 women) (Pinion 1994). At four years, this difference between groups had narrowed and did not report a clear difference (RR (Non‐event) 2.76, 95% CI 0.93 to 8.17; 146 women) (Analysis 1.9) (Pinion 1994).
1.9. Analysis.
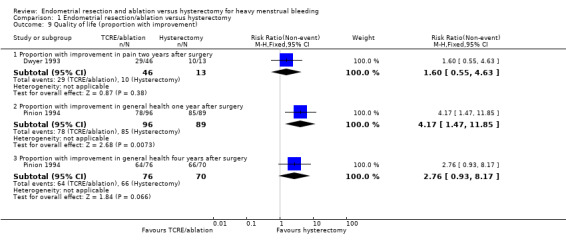
Comparison 1 Endometrial resection/ablation versus hysterectomy, Outcome 9 Quality of life (proportion with improvement).
1.10 Duration of surgery
The duration of surgery was available in all but one trial (Dickersin 2007) and reported a clear difference between groups, being longer for hysterectomy in all eight trials, and ranging from ten minutes' to two hours' average difference between trials. We do not include a pooled estimate in this analysis as we noted a high degree of heterogeneity, as discussed below under 'Heterogeneity' (Analysis 1.10).
1.10. Analysis.
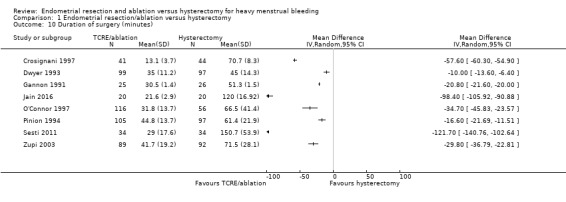
Comparison 1 Endometrial resection/ablation versus hysterectomy, Outcome 10 Duration of surgery (minutes).
1.11. Duration of hospital stay
Seven trials evaluated this outcome (Crosignani 1997; Dickersin 2007; Dwyer 1993; Gannon 1991; O'Connor 1997; Pinion 1994; Zupi 2003). We do not include a pooled estimate in this analysis as we noted a high degree of heterogeneity (Analysis 1.11).
1.11. Analysis.
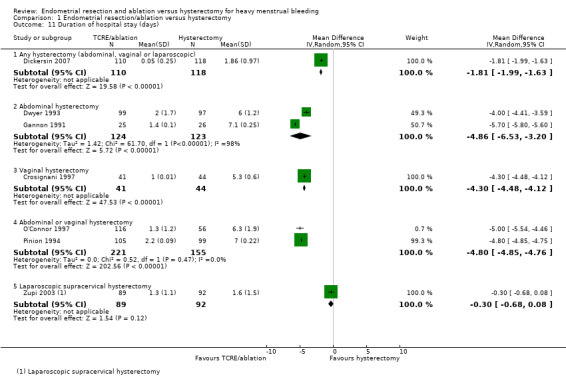
Comparison 1 Endometrial resection/ablation versus hysterectomy, Outcome 11 Duration of hospital stay (days).
Mean differences in hospital stay showed clear evidence of difference for all the hysterectomy groups when compared with TCRE/ablation, being shorter in the TCRE/ablation groups in the following comparisons.
TCRE/ablation versus abdominal hysterectomy (MD −4.86, 95% CI −6.53 to −3.20; 2 studies, 247 women, I² = 98%) (Dwyer 1993; Gannon 1991).
TCRE/ablation versus vaginal hysterectomy (MD −4.30, 95% CI −4.48 to −4.12; 1 study, 85 women) (Crosignani 1997).
TCRE/ablation versus either abdominal or vaginal hysterectomy (MD −4.80, 95% CI −4.85 to −4.76; 2 studies, 376 women) (O'Connor 1997; Pinion 1994).
TCRE/ablation versus any route of hysterectomy (MD −1.81, 95% CI −1.99 to −1.63; 1 study, 228 women) (Dickersin 2007).
There was no clear evidence of difference in the duration of hospital stay between TCRE/ablation and laparoscopic supracervical hysterectomy (MD −0.30, 95% CI −0.68 to 0.08; 1 study, 181 women) (Zupi 2003).
1.12. and 1.13 Time to return to normal activity and Time to return to work
Time to return to normal activity (in days) was reported in four trials (Crosignani 1997; Dwyer 1993; O'Connor 1997; Zupi 2003). There was clear evidence of difference between groups favouring endometrial ablation or resection, ranging from 1.5 to 21 days. We do not include a pooled estimate in this analysis as we noted a high degree of heterogeneity, as discussed below under 'Heterogeneity' (Analysis 1.12).
1.12. Analysis.
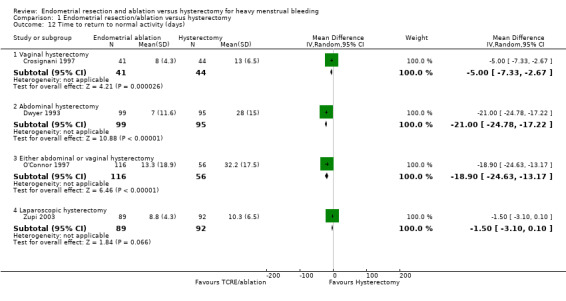
Comparison 1 Endometrial resection/ablation versus hysterectomy, Outcome 12 Time to return to normal activity (days).
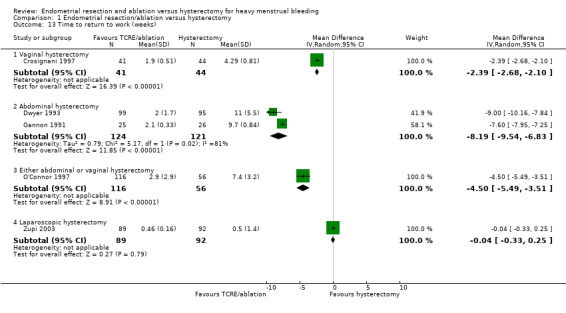
Time to return to work (in weeks) was reported in five trials (Crosignani 1997; Dwyer 1993; Gannon 1991; O'Connor 1997; Zupi 2003). There was clear evidence of difference between groups favouring endometrial resection and ablation in four trials, ranging from 2.4 to 9 weeks (Crosignani 1997; Dwyer 1993; Gannon 1991; O'Connor 1997); in Zupi 2003 there was no clear evidence of difference between groups. We do not include a pooled estimate in this analysis as we noted a high degree of heterogeneity (Analysis 1.13). Abdominal hysterectomy was associated with the greatest difference in time to return to normal activities (MD 21 days, 95% CI ‐24.78 to ‐17.22) and time to return to work (MD 8.2 weeks,95% CI ‐9.54 to ‐6.83) when compared with TCRE/ablation (Dwyer 1993; Gannon 1991). For the same outcomes, when TCRE/ablation was compared against vaginal hysterectomy (MD 5 days, 95% CI 7.33 to 2.67; MD 2.4 weeks,95% CI 2.68 to 2.10, respectively) (Crosignani 1997), the difference was less, particularly when compared against laparoscopic hysterectomy (MD 1.5 days, 95% CI 3.10 to 0.10 and MD 0.04 weeks, 95% CI 0.33 to 0.25, respectively) (Zupi 2003).
1.13. Analysis.
Comparison 1 Endometrial resection/ablation versus hysterectomy, Outcome 13 Time to return to work (weeks).
1.14. Total health service cost per woman
Three trials assessed the costs (Dwyer 1993; Gannon 1991; Pinion 1994). There was clear evidence of difference between groups favouring endometrial ablation and resection for the management of heavy menstrual bleeding at short‐term follow‐up. This difference continued over a prolonged follow‐up time, but the cost gap narrowed primarily because of the retreatment rate for women who underwent endometrial resection. By four years, ablation techniques cost between 5% and 11% less than a hysterectomy in one study that evaluated long‐term follow‐up (Aberdeen 1999 (Pinion 1994); Analysis 1.14).
1.14. Analysis.
Comparison 1 Endometrial resection/ablation versus hysterectomy, Outcome 14 Total health service cost per woman.
| Total health service cost per woman | |
|---|---|
| Study | |
| Dwyer 1993 | FOUR MONTHS FOLLOW UP
Mean resource cost per patient (UK pounds) in 1991/92 prices:
Endometrial resection: UK pounds 560.05 (SD 261.22)
Hysterectomy: UK pounds 1059.73 (SD 198.04)
These costs were made up of pre‐operative, operative and post‐operative costs, hotel costs, complications costs, re‐treatment and general practice costs.
Mean difference in cost between groups : UK pounds ‐499.68 (95% CI ‐567 to ‐432)
Statistical test not specifically stated.
Mean cost of resection at 4 months follow up 53% the cost of hysterectomy. 2.2 YEARS OF FOLLOW UP Mean resource cost per patient (UK pounds) in 1994 prices: Endometrial resection: UK pounds 790 (SD 493) Hysterectomy: UK pounds 1110 (SD 168) Costs made up of initial surgery, re‐treatment costs, other resource use after 4 months and HRT. Wilcoxon Rank Sum test used to test the difference between groups with a 5% significance level, p=0.0001. Mean cost of resection at 2.2 years of follow up 71% the cost of hysterectomy. |
| Gannon 1991 | INITIAL COSTS (NHS) Mean cost per operation (UK pounds) in 1991: Endometrial resection: UK pounds 407 Abdominal hysterectomy: UK pounds 1270 This cost was made up of: (1) variable costs: average cost of theatre consumables, staffing and maintenance in the operating theatre, marginal cost of a bed on the gynaecological ward; and (2) fixed costs: capital depreciation, hospital staffing and energy. The difference between groups in resource cost was not assessed in a statistical test. |
| Pinion 1994 | ONE YEAR OF FOLLOW UP
Mean resource cost per patient in UK pounds in 1994:
Endometrial resection: UK pounds 1001.00
Laser ablation: UK pounds 1046.00
Hysterectomy: UK pounds 1315.00
No statistical test used to compare the difference between groups.
Mean cost of endometrial resection at 1 year of follow up 76% of cost of hysterectomy.
Mean cost of laser ablation at 1 year of follow up 80% of cost of hysterectomy.
Costs based on pre‐operative costs, nights in hospital, theatre and ward costs, GP and out‐patient costs, re‐treatment costs and technical equipment costs. FOUR YEARS OF FOLLOW UP Mean resource cost per patient in UK pounds in 1994: Endometrial destruction techniques: UK pounds 1231 Hysterectomy: UK pounds 1332 Includes additional costs for re‐treatment or additional procedures arising between 1 and 4 years after surgery. Data reported as 1994 rates (discounted by 6%). Sensitivity analysis performed with variations in the discount rate. Cost of endometrial ablation techniques at 4 years reported as between 89% and 95% the costs of hysterectomy. |
1.15. Total individual cost per woman
One trial measured costs to the women (Cameron 1996 (Pinion 1994)). At one‐year follow‐up, total personal costs, in terms of travel, loss of pay and child care, were higher for women who had a hysterectomy than for women who underwent endometrial ablation. However, women who had a hysterectomy estimated greater savings in the cost of sanitary protection when compared with those who underwent endometrial ablation (savings of GBP 85.10 per year versus GBP 58.30 per year; Analysis 1.15).
1.15. Analysis.
Comparison 1 Endometrial resection/ablation versus hysterectomy, Outcome 15 Total individual cost per woman.
| Total individual cost per woman | |
|---|---|
| Study | |
| Pinion 1994 | ONE YEAR OF FOLLOW UP
Mean patient cost in UK pounds in 1994 prices:
Hysteroscopic surgery: UK pounds 21.00 (95% CI 13.3, 33.1)
Hysterectomy: UK pounds 73.40 (95% CI 42.1, 127)
Mean cost of hysteroscopic surgery 29% the cost of hysterectomy surgery.
Costs estimated included loss of pay, child care and travel expenses.
Student t test used to compare differences between surgery groups, p<0.05. Mean annual savings from sanitary protection after treatment in UK pounds in 1994: Hysteroscopic surgery: UK pounds 58.30 (95% CI 51.4, 66) Hysterectomy: UK pounds 85.10 (95% CI 72.2, 100) Student t test used to compare differences between surgery groups, p<0.05. |
Funnel plots
We were unable to include enough studies in the review for funnel plots to have sufficient power to distinguish chance from true asymmetry.
Heterogeneity
We observed a high level of heterogeneity for some outcomes.
For many outcomes, only one trial contributed data, and analysis of heterogeneity was therefore not applicable. Data were, however, contributed from several or all trials for four outcomes and we visually inspected the forest plots for these outcomes. The estimate for proportion requiring further surgery showed a low level of heterogeneity (all confidence intervals overlapping and I² = 0% at one and two years of follow‐up). However, a very high degree of heterogeneity was evident for outcomes such as duration of surgery (I² = 99%), time to return to work (I² = 100%) and time to return to normal activities (I² = 97%).
The level of clinical heterogeneity for these outcomes may be explained in part by differences in interventions (most notably, mode of hysterectomy) throughout the trials. Two trials included abdominal hysterectomies only (Dwyer 1993;Gannon 1991); one trial included only vaginal hysterectomies (Crosignani 1997); and two trials included only laparoscopic hysterectomies (Zupi 2003; Sesti 2011). All other studies included two or all modes of hysterectomy. We conducted a sensitivity analysis as set out below to investigate this further.
All trials had similar risk profiles for most measures in the 'Risk of bias' table. We therefore assume that no significant methodological heterogeneity was present.
Sensitivity analysis
We performed an analysis to investigate the effect of clear evidence of allocation concealment on estimates. For six of the eight trials, clear evidence indicated that allocation was concealed, but for two trials (Gannon 1991 and Zupi 2003), this was not the case. When we included only trials with clear evidence of allocation concealment in the meta‐analysis, there was no significant change in the estimates compared with inclusion of all trials.
We planned but did not conduct the following analysis: estimates based on all relevant trials regardless of missing data and loss to follow‐up versus estimates based on trials for which incomplete outcome assessment was not likely to cause bias. We did not conduct this analysis as no data were missing from the included trials.
Discussion
Summary of main results
This review assessed the benefits and harms of two types of surgical procedures for the treatment of heavy menstrual bleeding. When the primary outcomes of this review—effectiveness (woman's perception of improvement in bleeding outcomes, PBAC score, requirement for further surgery), acceptability and safety (satisfaction with treatment and adverse outcomes)—are considered, this review shows that both hysterectomy and endometrial ablation and resection are effective, acceptable and safe surgical treatments for heavy menstrual bleeding.
Whilst hysterectomy is more effective at reducing bleeding symptoms and improving quality of life and is associated with less repeated surgery than endometrial ablation, considerable short‐term benefits are associated with endometrial ablation and resection techniques when compared with hysterectomy, mainly in the areas of recovery time and cost.
Hysterectomy was completely successful in treating bleeding problems (over 96% success in all trials at different follow‐up times). Endometrial ablation and resection techniques were also highly successful in reducing menstrual blood loss in most participants, but a proportion of participants (ranging from 3% to 18%) showed no improvement. At most durations of follow‐up, regardless of how bleeding symptoms were measured, women in the hysterectomy groups showed a greater reduction in symptoms than those in the endometrial ablation‐resection groups. For some outcomes, it was suggested that these differences were no longer experienced at longer durations of follow‐up; this might be due to a number of reasons, including reduced numbers, retreatment in the TCRE/ablation group and some women reaching menopause.
Hysterectomy led to very high levels of participant satisfaction up to four years after surgery. Satisfaction levels were also high for women who underwent endometrial ablation‐resection but they were lower for these women when compared with hysterectomy at two time periods.
Most quality of life measures were not markedly different between the two types of surgery, although evidence from analysis of SF‐36 scores shows that women who had a hysterectomy perceived greater benefit for their general health, social functioning and energy levels at both one and two years and for pain levels at two years after surgery was completed compared with those having endometrial ablation. All other aspects of quality of life as measured by different instruments did not differ between groups.
Both surgical treatments were considered to be safe, with low complication rates reported. However, hysterectomy was associated with higher rates of sepsis, pyrexia, requirement for blood transfusion, and haematoma of the vault and wound.
Duration of surgery, hospital stay, time to return to normal activities and time to return to work were shorter for those who had endometrial ablation‐resection when compared with those who underwent hysterectomy. Although we were unable to pool the findings from the included studies, almost all of the individual trials consistently reported a benefit for endometrial ablation‐resection in these areas. Likely causes of heterogeneity for duration of surgery were variations in surgical route (e.g. vaginal vs abdominal vs laparoscopic hysterectomy or first‐generation vs second‐generation endometrial resection/ablation techniques), surgical technique and the expertise of surgeons carrying out the procedures.
Duration of hospital stay was likely to be affected by changes outside the control of investigators. Hospital policy for maximum stay can vary significantly between hospitals and could have accounted for the heterogeneity observed in the results for this outcome. Route of surgery (e.g. vaginal vs abdominal vs laparoscopic) partially explains the extreme heterogeneity in the time taken for recovery after discharge from hospital. Many hospitals worldwide are adopting a policy of 'enhanced recovery' following elective surgery, including shorter times to discharge for major operations such as abdominal hysterectomy. Future updates of this review may include trials that reflect this change.
Significant differences in operating time, hospital stay and time to return to normal activities and work can be seen in most of the trials, but the magnitude of these differences varies, depending on which mode of hysterectomy is being compared. Although we cannot give precise estimates, endometrial resection‐ablation for HMB takes less time to perform and has a shorter recovery time than hysterectomy. These differences are associated with a reduction in health service costs.
Evaluation of comparative costs between the two surgical procedures is affected by the increasing retreatment rate. Initially, treatment costs are much lower for women undergoing endometrial resection‐ablation than for those undergoing hysterectomy, but the difference in costs between the groups narrows over time because of the cost of retreatment. In one study with a minimum of four years of follow‐up, endometrial ablation was reported to be only 5% to 11% less costly than hysterectomy compared with 24% and 29% less costly at one and two years of follow‐up. Again here, 'enhanced recovery' policies may reflect a narrower difference in duration of hospital stay and therefore a corresponding narrower difference in patient costs.
As described previously, outcomes may be altered by the prior experience of the surgeon for both surgical procedures. A less experienced surgeon for either treatment group could alter results such as duration of surgery, adverse outcomes and, in the case of endometrial ablation, effectiveness.
Overall completeness and applicability of evidence
The included studies adequately addressed the review question: to assess the relative effectiveness, acceptability and safety of any technique of endometrial resection‐ablation and hysterectomy via any route for the treatment of HMB, as well as the secondary outcomes described above. The inclusion and exclusion criteria were met, and the interventions well described. Unfortunately, the outcomes (particularly measures of improvement in bleeding symptoms) were measured in several different ways, and it was not possible for us to pool all estimates, making meta‐analysis impossible for some outcomes.
Quality of the evidence
In total, nine studies were included with a total of 1300 randomly assigned participants.
All studies were at high risk of performance/detection bias, as it is not feasible to blind women or the surgeon to the type of operation that was performed. Several of the older studies were at high risk of selection bias.
As the studies used many different measurements for the outcomes (particularly for effectiveness of treatment), it was not possible to pool data for every outcome. However, the results were largely comparable; both treatments are considered to be effective and safe, hysterectomy was generally superior in improving symptoms and in leading to less requirement for future surgery, and endometrial ablation was superior in terms of fewer adverse outcomes, shorter operating times and faster return to activities/work.
For many outcomes, assessment of heterogeneity was not relevant, as only one trial contributed data. For outcomes that displayed a high level of clinical heterogeneity, this was explained in part by differences in outcomes for different modes of hysterectomy (further described under 'Sensitivity analysis').
Quality of evidence was low to moderate, depending on the outcome. PBAC score, adverse events and proportion satisfied with treatment generated a moderate GRADE score, suggesting that further research may change the estimate. Outcomes that generated a low GRADE score included the woman’s perception of bleeding and the proportion of women requiring further surgery for HMB. For these two outcomes, further evidence is likely to change the estimate.
Potential biases in the review process
Electronic searches in combination with handsearches performed by the review authors identified all relevant studies known to be available currently. Our inability to pool data for particular outcomes is likely to decrease the power of results; this may change if future studies are able to add data to the existing outcomes.
Agreements and disagreements with other studies or reviews
Bhattacharya 2011 performed a systematic review that compared clinical effectiveness and cost‐effectiveness analyses of hysterectomy, endometrial ablation and levonorgestrel‐releasing intrauterine device (LNG‐IUS) for heavy menstrual bleeding. These findings were in accordance with the findings of this review; satisfaction rates at 12 months were highest for hysterectomy, and rates of further surgery after endometrial resection/ablation were comparable (8.5%). The authors also noted longer hospital stay and longer time to return to normal activities for hysterectomy.
Women who have undergone hysterectomy have experienced more postoperative complications than women who have received TCRE/ablation, although for some types of complications, no differences were reported. Because some complications are rare, these rates are best compared with those of large audits, such as the Mistletoe audit in the UK (Overton 1997). The low rate of complications for TCRE/ablation in this review confirms the findings of the Mistletoe study.
A comparison of costs of endometrial resection and ablation techniques versus those of hysterectomy cannot adequately provide information on the relative value in terms of money of these two surgical procedures. The availability of TCRE/ablation as a treatment for HMB may result in an earlier recourse to surgery than a woman would have considered if the only surgery available was hysterectomy (Bridgman 1994; Coulter 1994), and this will have a significant impact on costs. Additional studies have provided assessments of cost‐effectiveness based on the Dwyer 1993 trial through a cost‐utility analysis (Sculpher 1998); preference‐based treatment allocation (woman allocated to the treatment that she prefers) (Sculpher 1998); and four other cost‐utility analyses (Clegg 2007; Garside 2004; Roberts 2011; You 2006). Garside 2004 concluded that abdominal hysterectomy is likely to be more cost‐effective than endometrial resection if healthcare purchasers are willing to pay an additional cost of at least GBP 6500 per extra quality‐adjusted life‐year (QALY) generated by hysterectomy, although an area of uncertainty is attached to this conclusion in the form of variation in the parameters used in the analysis. Clegg 2007 found that a preference‐based treatment allocation was more cost‐effective than reliance on a single intervention for all women requiring surgery for HMB. Garside 2004 reported that hysterectomy was more expensive than endometrial ablation but accrued more QALYs over 10 years. The incremental cost per QALY of hysterectomy compared with two second‐generation endometrial ablation techniques was approximately GBP 2000. You 2006 also confirmed that hysterectomy was a more expensive option than endometrial ablation (cost per woman: USD 6878 vs USD 6185 over five years) but was more effective (4.725 QALYs vs 4.624 QALYs). Roberts 2011 found that hysterectomy produced more QALYs relative to second‐generation endometrial ablation, with an incremental cost‐effectiveness ratio of GBP 970 per additional QALY. Data from the Clegg 2007 cost‐utility analysis contradicted this finding: the authors reported that second‐generation methods accrued marginally more QALYs than hysterectomy over five years (4.13 vs 4.01 QALYs). Evaluation of the comparative cost‐effectiveness of endometrial destruction techniques and hysterectomy is complex, and the simple conclusion that endometrial destruction is cheaper than hysterectomy, with the difference narrowing over time, may not represent an adequate economic assessment.
On the whole, the review findings were consistent with currently accepted clinical advice and are in agreement with current guidelines. National Institute for Health and Care Excellence (NICE) guidelines for menorrhagia (NICE 2007 and NICE 2018) suggest that hysterectomy should not be used as a first‐line treatment for benign HMB and should be considered only when other treatment options have failed, are contraindicated or are declined by the woman; when there is a wish for amenorrhoea; when the woman (who has been fully informed) requests it; and/or when the woman no longer wishes to retain her uterus and fertility. NICE 2007 and NICE 2018 guidelines are in agreement with the findings of this review with regard to potential complications associated with both modes of surgical treatment.
Authors' conclusions
Implications for practice.
Although hysterectomy is more effective at resolving bleeding problems and satisfaction rates are high, endometrial destruction by ablation is an alternative to hysterectomy that should be offered to women with heavy menstrual bleeding.
Ablation techniques have high satisfaction rates, similar to hysterectomy at one year's and four years' follow‐up, with shorter operation time and hospital stay and earlier recovery and reduced postoperative complications. The shorter recovery varies according to the route of the hysterectomy. The only eventually serious complication that was more frequent in the hysterectomy group was sepsis, and no further details were given about it. A preoperative discussion should focus on the possibility of further surgery being necessary for those women who choose endometrial destruction techniques for relief of their heavy menstrual bleeding.
The initial cost of endometrial destruction is clearly lower than that of hysterectomy, but because retreatment is often necessary, the cost difference narrows over time.
Laparoscopic hysterectomy represents an improvement on several of the previously described disadvantages of hysterectomy, and some outcomes such as duration of hospital stay, time to return to work and time to return to normal activities have become more comparable with those of endometrial ablation. It should be noted, however, that laparoscopic hysterectomy may be associated with longer operating time than other modes of hysterectomy and requires specific surgical expertise and equipment.
It is recommended that women be encouraged to play an active role in selecting the type of surgery, based on the personal value that they place on the advantages and disadvantages of each surgical approach.
Implications for research.
Additional trials are needed in the following areas.
Comparison of more recent types of hysterectomy (supracervical, vaginal and laparoscopically assisted vaginal) versus endometrial ablation techniques. One further trial in this category was added in the 2013 update (Sesti 2011); however, more data are needed to reduce heterogeneity for some outcomes. Results from this trial did not contribute data to cost comparisons, and this is likely to be clinically important.
Comparison of second‐generation ablation methods versus hysterectomy. Evidence suggests that whereas first‐generation ablation methods did not have an impact on hysterectomy rates for HMB, second‐generation methods have overtaken first‐generation methods in the UK and are now the most common operation for HMB (Reid 2007). One further trial in this category was added in the 2013 update (Sesti 2011).
Trials with follow‐up of four years or longer to adequately assess the cost differential between the two types of surgery and the requirement for further surgical treatment in women randomly assigned to TCRE or to endometrial ablation, even though this may cause confusion with the proportion of women going through menopause.
Trials that incorporate 'enhanced recovery' programmes. In the future, findings of these trials may reflect shorter hospital stay for women undergoing hysterectomy, and therefore a smaller difference between the two procedures for this particular outcome.
What's new
| Date | Event | Description |
|---|---|---|
| 1 April 2019 | New citation required but conclusions have not changed | The inclusion of data from 1 new and 1 follow‐up study did not lead to a change in the conclusions of this review. |
| 11 December 2018 | New search has been performed | Updated; 1 new trial (Jain 2016) and 1 long‐term follow up to Zupi 2003 added. |
History
Protocol first published: Issue 3, 1996 Review first published: Issue 2, 1999
| Date | Event | Description |
|---|---|---|
| 1 November 2013 | New search has been performed | One new study added: Sesti 2011. |
| 1 November 2013 | New citation required but conclusions have not changed | One new study added: Sesti 2011. |
| 15 January 1999 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
The authors of the 2019 update acknowledge the contribution of Dr Sasha Shepperd to previous versions of this review. They thank Gabriela Cooper, Andy Watson, Gaity Ahmad and Justin Clark for providing peer review comments. They also thank Marian Showell (Information Specialist) and Helen Nagels (Managing Editor) at the Cochrane Gynaecology and Fertility Group's editorial base for their time and support.
The authors of the 2013 update acknowledge the contribution of Dr Inez Cooke, who wrote the protocol for the 2008 review.
The review authors acknowledge the helpful comments of those who refereed previous versions of this review. We are especially grateful to Professor Pier Crosignani, Dr Kay Dickerson and Dr Sbracia, who answered queries and provided additional material for this review. Special thanks are also due to Helen Nagels, Managing Editor of the Menstrual Disorders and Subfertility Group, for her professionalism and help with the inevitable problems that arose; and to Marion Showell, Trials Search Co‐ordinator, for her assistance in identifying trials.
Appendices
Appendix 1. Cochrane Gynaecology and Fertility Group specialised register search strategy
ProCite platform
Searched 10 December 2018
Keywords CONTAINS "menorrhagia" or "heavy bleeding" or "heavy menstrual bleeding" or "heavy menstrual loss" or "dysfunctional uterine bleeding" or "dysfunctional bleeding" or Title CONTAINS "menorrhagia" or "heavy bleeding "or "heavy menstrual bleeding" or "heavy menstrual loss" or "dysfunctional uterine bleeding" or "dysfunctional bleeding"
AND
Keywords CONTAINS "Hysterectomy" or "Hysterectomy,abdominal" or "hysterectomy, laparoscopically assisted vaginal" or "Hysterectomy, subtotal" or "Hysterectomy, Vaginal" or "subtotal hysterectomy" or "abdominal hysterectomy" or "laparoscopic assisted vaginal hysterectomy" or "laparoscopic hysterectomy" or "vaginal hysterectomy" or "hysterectomy, laparoscopic" or Title CONTAINS "Hysterectomy" or "Hysterectomy,abdominal" or "hysterectomy, laparoscopically assisted vaginal" or "Hysterectomy, subtotal" or "Hysterectomy, Vaginal" or "subtotal hysterectomy" or "abdominal hysterectomy" or "laparoscopic assisted vaginal hysterectomy" or "laparoscopic hysterectomy" or "vaginal hysterectomy" or "hysterectomy, laparoscopic (94 records)
Appendix 2. CENTRAL via the Cochrane Register of Studies Online (CRSO) search strategy
Web platform
Searched 10 December 2018
#1 MESH DESCRIPTOR menorrhagia EXPLODE ALL TREES 330
#2 menorrhag*:TI,AB,KY 718
#3 (menstrua* adj5 (bleed* or blood)):TI,AB,KY 860
#4 (heavy adj5 menstrua*):TI,AB,KY 236
#5 (dysfunctional adj5 uter*):TI,AB,KY 139
#6 hypermenorrh*:TI,AB,KY 24
#7 #1 OR #2 OR #3 OR #4 OR #5 OR #6 1435
#8 MESH DESCRIPTOR Hysterectomy EXPLODE ALL TREES 1676
#9 hysterectom*:TI,AB,KY 4384
#10 (uter* adj5 excis*):TI,AB,KY 10
#11 #8 OR #9 OR #10 4392
#12 #7 AND #11 205
Appendix 3. MEDLINE search strategy
OVID platform
Searched from 1946 to 10 December 2018
1 menorrhagia/ (4083) 2 menorrhag$.tw. (3170) 3 (menstrua$ adj5 (bleed$ or blood)).tw. (4431) 4 (heavy adj5 menstrua$).tw. (940) 5 (dysfunctional adj5 uter$).tw. (1008) 6 hypermenorrh$.tw. (289) 7 or/1‐6 (9955) 8 exp hysterectomy/ or hysterectomy, vaginal/ (29086) 9 hysterectom$.tw. (33746) 10 (uter$ adj5 excis$).tw. (431) 11 or/8‐10 (45666) 12 7 and 11 (1693) 13 exp Electrocoagulation/ (11557) 14 exp Endometrium/su [Surgery] (1190) 15 Laser Coagulation/ (7168) 16 (endometri$ adj5 (ablat$ or excis$ or laser or electrocautery or destruct$ or radiofrequency)).tw. (2411) 17 (endometri$ adj5 resect$).tw. (1322) 18 (electrosurgery or thermal balloon or hypertherm$ or thermotherapy or photodynamic therapy or phototherapy or cryoablation or microwave ablation).tw. (63668) 19 (Thermachoice or rollerball).tw. (195) 20 or/13‐19 (85057) 21 12 and 20 (638) 22 randomized controlled trial.pt. (472057) 23 controlled clinical trial.pt. (92771) 24 randomized.ab. (428436) 25 placebo.tw. (198983) 26 clinical trials as topic.sh. (185394) 27 randomly.ab. (301468) 28 trial.ti. (190979) 29 (crossover or cross‐over or cross over).tw. (78507) 30 or/22‐29 (1213585) 31 exp animals/ not humans.sh. (4519948) 32 30 not 31 (1115167) 33 21 and 32 (94)
Appendix 4. Embase search strategy
OVID platform
Searched from 1980 to 10 December 2018
1 menorrhagia/ (8794) 2 menorrhag$.tw. (5057) 3 (menstrua$ adj5 (bleed$ or blood)).tw. (5787) 4 (heavy adj5 menstrua$).tw. (1645) 5 (dysfunctional adj5 uter$).tw. (1202) 6 hypermenorrh$.tw. (389) 7 or/1‐6 (14778) 8 exp hysterectomy/ or hysterectomy, vaginal/ (62699) 9 hysterectom$.tw. (49322) 10 (uter$ adj5 excis$).tw. (602) 11 or/8‐10 (71361) 12 7 and 11 (3534) 13 electrosurgery/ or exp electrocoagulation/ or laser surgery/ (41183) 14 exp laser coagulation/ (22954) 15 endometrium ablation/ (2520) 16 (endometri$ adj5 (ablat$ or excis$ or laser or electrocautery or destruct$ or radiofrequency)).tw. (4269) 17 (endometri$ adj5 resect$).tw. (2289) 18 (electrosurgery or thermal balloon or hypertherm$ or thermotherapy or photodynamic therapy or phototherapy or cryoablation or microwave ablation).tw. (77220) 19 (Thermachoice or rollerball).tw. (312) 20 or/13‐19 (138823) 21 12 and 20 (1155) 22 Clinical Trial/ (942899) 23 Randomized Controlled Trial/ (523265) 24 exp randomization/ (80398) 25 Single Blind Procedure/ (33297) 26 Double Blind Procedure/ (153077) 27 Crossover Procedure/ (57463) 28 Placebo/ (313868) 29 Randomi?ed controlled trial$.tw. (192316) 30 Rct.tw. (30475) 31 random allocation.tw. (1837) 32 randomly allocated.tw. (31084) 33 allocated randomly.tw. (2377) 34 (allocated adj2 random).tw. (797) 35 Single blind$.tw. (21733) 36 Double blind$.tw. (186112) 37 ((treble or triple) adj blind$).tw. (857) 38 placebo$.tw. (276040) 39 prospective study/ (488511) 40 or/22‐39 (1954581) 41 case study/ (57987) 42 case report.tw. (357892) 43 abstract report/ or letter/ (1039805) 44 or/41‐43 (1446525) 45 40 not 44 (1905027) 46 21 and 45 (277)
Appendix 5. PsycINFO search strategy
OVID platform
Searched from 1806 to 10 December 2018
1 exp menstrual disorders/ (1194) 2 menorrhag$.tw. (83) 3 (menstrua$ adj5 (bleed$ or blood)).tw. (242) 4 (heavy adj5 menstrua$).tw. (29) 5 (dysfunctional adj5 uter$).tw. (25) 6 hypermenorrh$.tw. (2) 7 or/1‐6 (1472) 8 exp Hysterectomy/ (432) 9 hysterectom$.tw. (786) 10 (uter$ adj5 excis$).tw. (3) 11 or/8‐10 (811) 12 7 and 11 (33)
Appendix 6. Additional searches
CINAHL, Google, Google Scholar PubMed,and the trial registries, were searched using the key words ‘endometrial ablation’, ‘endometrial resection’, ‘hysterectomy’, ‘heavy menstrual bleeding’, ‘menorrhagia’, ‘disordered uterine bleeding’ and ‘abnormal uterine bleeding’.
Data and analyses
Comparison 1. Endometrial resection/ablation versus hysterectomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Woman's perception (proportion with improvement in bleeding symptoms) | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Within one year of follow‐up | 4 | 650 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.85, 0.93] |
| 1.2 At two years of follow‐up | 2 | 292 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.86, 0.99] |
| 1.3 At four years of follow‐up | 2 | 237 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.88, 0.99] |
| 2 PBAC score (continuous data) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 At one year of follow‐up | 1 | 68 | Mean Difference (IV, Fixed, 95% CI) | 24.4 [16.01, 32.79] |
| 2.2 At two years of follow‐up | 1 | 68 | Mean Difference (IV, Fixed, 95% CI) | 44.0 [36.09, 51.91] |
| 3 Proportion requiring further surgery for HMB | 9 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Within one year after surgery | 7 | 927 | Risk Ratio (M‐H, Fixed, 95% CI) | 16.17 [5.53, 47.24] |
| 3.2 At two years after surgery | 6 | 930 | Risk Ratio (M‐H, Fixed, 95% CI) | 34.06 [9.86, 117.65] |
| 3.3 At three years after surgery | 1 | 172 | Risk Ratio (M‐H, Fixed, 95% CI) | 22.90 [1.42, 370.26] |
| 3.4 At four years after surgery | 1 | 197 | Risk Ratio (M‐H, Fixed, 95% CI) | 36.32 [5.09, 259.21] |
| 3.5 At 14 years after surgery | 1 | 153 | Risk Ratio (M‐H, Fixed, 95% CI) | 19.60 [1.15, 333.63] |
| 4 Proportion satisfied with treatment | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 At one year of follow‐up | 4 | 739 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.88, 1.00] |
| 4.2 At two years of follow‐up | 4 | 567 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.80, 0.95] |
| 4.3 At four years of follow‐up | 2 | 246 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.77, 1.03] |
| 5 Adverse events—short term (intraoperative and immediate postoperative) | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 Sepsis | 4 | 621 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.12, 0.31] |
| 5.2 Haemorrhage | 3 | 555 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.32, 1.46] |
| 5.3 Blood transfusion | 5 | 791 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.07, 0.59] |
| 5.4 Pyrexia | 3 | 605 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.09, 0.35] |
| 5.5 Vault haematoma | 5 | 858 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.04, 0.34] |
| 5.6 Wound haematoma | 1 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.03 [0.00, 0.53] |
| 5.7 Anaesthetic | 1 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.18 [0.01, 3.80] |
| 5.8 Fluid overload | 3 | 611 | Risk Ratio (M‐H, Fixed, 95% CI) | 9.27 [2.17, 39.64] |
| 5.9 Perforation | 2 | 430 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.05 [0.61, 42.16] |
| 5.10 Gastrointestinal obstruction/ileus | 1 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.04, 5.01] |
| 5.11 Laparotomy | 2 | 383 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.39 [0.08, 1.97] |
| 5.12 Cystotomy | 1 | 228 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.01, 4.42] |
| 5.13 Cervical laceration | 2 | 409 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.16 [0.33, 30.10] |
| 5.14 Cardiorespiratory event | 1 | 228 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.15 [0.01, 2.93] |
| 5.15 Thromboembolic event | 1 | 228 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.01, 4.42] |
| 5.16 Readmission/return to surgery | 1 | 228 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.15 [0.01, 2.93] |
| 6 Adverse events—long term (after hospital discharge) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Sepsis | 1 | 172 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.13, 0.58] |
| 6.2 Haematoma | 2 | 368 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.15, 2.37] |
| 6.3 Haemorrhage | 1 | 196 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.94 [0.12, 71.30] |
| 7 Quality of life scores (continuous data) | 6 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 SF‐36 at one year—Role Limitation (physical) | 1 | 181 | Mean Difference (IV, Fixed, 95% CI) | ‐0.80 [‐4.99, 3.39] |
| 7.2 SF‐36 at one year—Role Limitation (emotional) | 1 | 181 | Mean Difference (IV, Fixed, 95% CI) | ‐3.90 [‐8.21, 0.41] |
| 7.3 SF‐36 at one year—Social Functioning | 1 | 181 | Mean Difference (IV, Fixed, 95% CI) | ‐21.20 [‐24.73, ‐17.67] |
| 7.4 SF‐36 at one year—Mental Health | 2 | 385 | Mean Difference (IV, Fixed, 95% CI) | ‐1.53 [‐5.06, 2.01] |
| 7.5 SF‐36 at one year—Energy | 2 | 211 | Mean Difference (IV, Fixed, 95% CI) | ‐10.99 [‐14.45, ‐7.53] |
| 7.6 SF‐36 at one year—Pain | 2 | 391 | Mean Difference (IV, Fixed, 95% CI) | ‐1.91 [‐5.67, 1.86] |
| 7.7 SF‐36 at one year—General Health Perception | 2 | 385 | Mean Difference (IV, Fixed, 95% CI) | ‐7.27 [‐10.72, ‐3.81] |
| 7.8 SF‐36 at one year—Physical Functioning | 1 | 181 | Mean Difference (IV, Fixed, 95% CI) | ‐1.20 [‐5.34, 2.94] |
| 7.9 SF‐36 at two years—Role Limitation (physical) | 3 | 300 | Mean Difference (IV, Fixed, 95% CI) | ‐3.09 [‐7.94, 1.76] |
| 7.10 SF‐36 at two years—Role Limitation (emotional) | 3 | 300 | Mean Difference (IV, Fixed, 95% CI) | 10.22 [5.48, 14.96] |
| 7.11 SF‐36 at two years—Social Functioning | 3 | 300 | Mean Difference (IV, Fixed, 95% CI) | ‐10.06 [‐13.55, ‐6.58] |
| 7.12 SF‐36 at two years—Mental Health | 4 | 509 | Mean Difference (IV, Fixed, 95% CI) | 2.39 [‐0.61, 5.40] |
| 7.13 SF‐36 at two years—Energy | 4 | 513 | Mean Difference (IV, Fixed, 95% CI) | ‐2.01 [‐5.41, 1.40] |
| 7.14 SF‐36 at two years—Pain | 4 | 513 | Mean Difference (IV, Fixed, 95% CI) | ‐9.50 [‐12.80, ‐6.21] |
| 7.15 SF‐36 at two years—General Health Perception | 4 | 509 | Mean Difference (IV, Fixed, 95% CI) | ‐7.42 [‐10.64, ‐4.20] |
| 7.16 SF‐36 at two years—Physical Functioning | 3 | 300 | Mean Difference (IV, Fixed, 95% CI) | ‐9.29 [‐12.80, ‐5.78] |
| 7.17 GR inventory scores at one year after surgery | 1 | 182 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐1.75, 1.75] |
| 7.18 Euroqol score within one year after surgery | 2 | 347 | Mean Difference (IV, Fixed, 95% CI) | ‐3.24 [‐8.35, 1.88] |
| 7.19 Euroqol scores at two years after surgery | 2 | 368 | Mean Difference (IV, Fixed, 95% CI) | ‐1.96 [‐5.60, 1.67] |
| 7.20 SSR score at two years after surgery | 1 | 77 | Mean Difference (IV, Fixed, 95% CI) | ‐3.70 [‐11.17, 3.77] |
| 7.21 Total HAD scores at two years after surgery | 1 | 77 | Mean Difference (IV, Fixed, 95% CI) | ‐1.5 [‐4.32, 1.32] |
| 7.22 Anxiety HAD scores at two and four years after surgery | 2 | 259 | Mean Difference (IV, Fixed, 95% CI) | ‐0.67 [‐1.64, 0.30] |
| 7.23 Depression HAD scores at two and four years after surgery | 2 | 259 | Mean Difference (IV, Fixed, 95% CI) | ‐0.00 [‐0.10, 0.09] |
| 8 Quality of life at 14 years follow up | Other data | No numeric data | ||
| 9 Quality of life (proportion with improvement) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 Proportion with improvement in pain two years after surgery | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.60 [0.55, 4.63] |
| 9.2 Proportion with improvement in general health one year after surgery | 1 | 185 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.17 [1.47, 11.85] |
| 9.3 Proportion with improvement in general health four years after surgery | 1 | 146 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.76 [0.93, 8.17] |
| 10 Duration of surgery (minutes) | 8 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11 Duration of hospital stay (days) | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 11.1 Any hysterectomy (abdominal, vaginal or laparoscopic) | 1 | 228 | Mean Difference (IV, Random, 95% CI) | ‐1.81 [‐1.99, ‐1.63] |
| 11.2 Abdominal hysterectomy | 2 | 247 | Mean Difference (IV, Random, 95% CI) | ‐4.86 [‐6.53, ‐3.20] |
| 11.3 Vaginal hysterectomy | 1 | 85 | Mean Difference (IV, Random, 95% CI) | ‐4.3 [‐4.48, ‐4.12] |
| 11.4 Abdominal or vaginal hysterectomy | 2 | 376 | Mean Difference (IV, Random, 95% CI) | ‐4.80 [‐4.85, ‐4.76] |
| 11.5 Laparoscopic supracervical hysterectomy | 1 | 181 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.68, 0.08] |
| 12 Time to return to normal activity (days) | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 12.1 Vaginal hysterectomy | 1 | 85 | Mean Difference (IV, Random, 95% CI) | ‐5.0 [‐7.33, ‐2.67] |
| 12.2 Abdominal hysterectomy | 1 | 194 | Mean Difference (IV, Random, 95% CI) | ‐21.0 [‐24.78, ‐17.22] |
| 12.3 Either abdominal or vaginal hysterectomy | 1 | 172 | Mean Difference (IV, Random, 95% CI) | ‐18.90 [‐24.63, ‐13.17] |
| 12.4 Laparoscopic hysterectomy | 1 | 181 | Mean Difference (IV, Random, 95% CI) | ‐1.50 [‐3.10, 0.10] |
| 13 Time to return to work (weeks) | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 13.1 Vaginal hysterectomy | 1 | 85 | Mean Difference (IV, Random, 95% CI) | ‐2.39 [‐2.68, ‐2.10] |
| 13.2 Abdominal hysterectomy | 2 | 245 | Mean Difference (IV, Random, 95% CI) | ‐8.19 [‐9.54, ‐6.83] |
| 13.3 Either abdominal or vaginal hysterectomy | 1 | 172 | Mean Difference (IV, Random, 95% CI) | ‐4.5 [‐5.49, ‐3.51] |
| 13.4 Laparoscopic hysterectomy | 1 | 181 | Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.33, 0.25] |
| 14 Total health service cost per woman | Other data | No numeric data | ||
| 15 Total individual cost per woman | Other data | No numeric data |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Crosignani 1997.
| Methods | Randomisation by computer‐generated sequence using numbered opaque sealed envelopes Single‐centre, parallel‐group with no blinding Number of women randomly assigned: n = 92 Number of withdrawals: n = 7 (4 in the resection group: 1 refused treatment, 1 underwent surgery in another hospital, 1 did not want further treatments, and 1 was lost to follow‐up before surgery; 3 in the hysterectomy group: 1 refused treatment, 1 had surgery in another hospital and 1 decided on long‐term medical treatment) Power calculation for sample size performed and analysis by intention to treat Source of funding not reported | |
| Participants | Women 42 to 49 years of age, with menorrhagia not responding to medical treatment and requiring hysterectomy, recruited from an outpatient clinic in Milan, Italy Inclusion criteria: ≤ 50 years, mobile uterus with volume < 12 weeks in gestational size and < 380 mL on ultrasound, negative cervical smear, no evidence of atypical hyperplasia at endometrial biopsy, no adnexal tumours at clinical and ultrasound examination Exclusion criteria: known PID or endometriosis, urinary stress incontinence, moderate/severe genital prolapse, clotting disorders, use of IUD or drugs that may affect MBL, unstable general conditions, submucous myomas > 3 cm in diameter or > 50% intramural extension | |
| Interventions | Treatment 1: hysteroscopic endometrial resection
Treatment 2: vaginal hysterectomy
Duration: 2 years of follow‐up Prior experience of the surgeon not mentioned |
|
| Outcomes | Participant satisfaction with treatment Improvement in MBL Quality of life Duration of surgery (minutes) Duration of hospital stay (days) Return to work (weeks) Requirement for further surgery | |
| Notes | Author contacted for additional information and reply received | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation sequence |
| Allocation concealment (selection bias) | Low risk | Numbered opaque sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not feasible for a comparison of surgical techniques |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Clear reasons given for withdrawal—appeared balanced in numbers between groups |
| Selective reporting (reporting bias) | Unclear risk | Unclear—no protocol identified. Study did not measure adverse events |
| Other bias | Low risk | Groups appeared balanced at baseline (although the table did not include dropouts), and no other biases were identified |
Dickersin 2007.
| Methods | Randomisation by computer‐generated permuted blocks of random size stratified by age and site Multi‐centre (n = 25), parallel‐group, single‐blinded (only assessors) Number of women randomly assigned: n = 237 Number of withdrawals: at 1 year: 16 in endometrial ablation group, 11 in hysterectomy group; at 2 years: 17 in endometrial ablation group, 7 in hysterectomy group Power calculation for sample size (90% power based on quality of life measures) but recruitment did not quite achieve the required sample size Analysis was by intention to treat for primary bleeding and satisfaction outcomes. Analysis was not by intention to treat for assessment of intraoperative and perioperative events Source of funding: AHRQ and Brown Medical School |
|
| Participants | Women with dysfunctional bleeding (not explained by pathology, drugs, etc.), most of whom were younger than 45 years of age (85%), recruited from 25 clinical centres in the USA and Canada. Inclusion: 18 years of age or older; premenopausal; dysfunctional uterine bleeding for at least 6 months (defined as 1 or more of excess duration, amount or unpredictability); refractory to medical treatment for at least 3 months. Exclusion: postmenopausal; bilateral oophorectomy; pregnant; wishing to retain fertility; refusal to consider surgery | |
| Interventions | Treatment 1: resectoscopic endometrial ablation with electrodesiccation/coagulation or vaporisation OR ablation with thermal balloon Treatment 2: vaginal, laparoscopic or abdominal hysterectomy under general or regional anaesthesia. In both groups, women > 45 years were allowed oophorectomy Duration of trial: enrolment was staggered, with some women having data for 5 years Prior experience of the surgeon not mentioned |
|
| Outcomes | Pain, bleeding and fatigue at 1 year Other outcomes at different time points: QoL outcomes, sexual function, employment, housework, leisure activities, out‐of‐pocket costs, health provider visits, surgical complications, additional surgery |
|
| Notes | Author contacted for clarification of some points and reply received | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation schedule (computer‐generated permuted blocks) was developed by the Co‐ordinating Centre and was stratified by participating centre |
| Allocation concealment (selection bias) | Low risk | Central allocation |
| Blinding (performance bias and detection bias) All outcomes | High risk | Single blinding for interviewers requesting information on bleeding history, quality of life, etc. But women providing this information knew of their assignment |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No reasons given for dropouts |
| Selective reporting (reporting bias) | Low risk | Protocol published with details on prespecified outcomes |
| Other bias | Low risk | Groups appear balanced at baseline. However, some outcomes (intraoperative and perioperative events, including adverse events) reported according to surgery received |
Dwyer 1993.
| Methods | Randomisation by sealed numbered envelopes in variable blocks of 20, 30 and 50 Single‐centre, parallel‐group, no blinding Number of women randomly assigned: n = 200 Number of withdrawals: n = 4 (3 from the hysterectomy group and 1 from the resection group) Power calculation for sample size performed but intention‐to‐treat analysis not reported Source of funding: South West Regional Health Authority | |
| Participants | Women with mean age of 40 years, recruited from an outpatient gynaecology clinic at a teaching hospital in Bristol, UK Inclusion criteria: < 52 years of age, complaint of menorrhagia that could not be controlled by conservative means, candidates for abdominal hysterectomy Exclusion criteria: uterine size ≤ 12 gestational weeks, additional symptoms or other pathology, making hysterectomy the preferred treatment | |
| Interventions | Treatment 1: endometrial resection, n = 99
Treatment 2: abdominal hysterectomy, n = 97
Duration: 4 months of follow‐up, 2.8 years of follow‐up Prior experience of the surgeon not mentioned |
|
| Outcomes | Satisfaction with surgery at 4 months Satisfaction with surgery at 2.8 years Change in menstrual blood loss after surgery (subjective) at 4 months Change in menstrual blood loss after surgery (subjective) at 2.8 years Quality of life at 2.8 years Postoperative complications Duration of hospital stay (days) Duration of surgery (minutes) Return to work (weeks) Requirement for further surgery within 1 year Requirement for further surgery at 2.8 years Total health service resource cost at 4 months Total health service resource cost at 2.8 years | |
| Notes | 3 publications used the same study population: Dwyer 1993; Sculpher 1993; Sculpher 1996 Dr Dwyer contacted for additional information but no reply received | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation sequence not described |
| Allocation concealment (selection bias) | Low risk | Sealed numbered envelopes in variable blocks |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not feasible for a comparison of surgical techniques |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts from trial minimal and not likely to bias results |
| Selective reporting (reporting bias) | Unclear risk | No prior protocol identified |
| Other bias | Low risk | Groups appeared balanced at baseline. No other bias identified |
Gannon 1991.
| Methods | Randomisation by sealed envelope Single‐centre, parallel‐group, no blinding Number of women randomly assigned: n = 54 Number of withdrawals: n = 3 (1 from the resection group who wanted hysterectomy, 1 from the hysterectomy group who wanted resection and 1 from the hysterectomy group who postponed surgery and was treated elsewhere) Power calculation and intention‐to‐treat analysis not reported Source of funding: not reported | |
| Participants | Women with median age 40 years and awaiting abdominal hysterectomy for menorrhagia, recruited from the Royal Berkshire Hospital in Reading, UK Exclusion criteria: leiomyomata, endometrial or cervical neoplasia, concomitant ovarian pathology, pelvic inflammatory disease or endometriosis | |
| Interventions | Treatment 1: endometrial resection, n = 25
Treatment 2: abdominal hysterectomy, n = 26
Duration: 12 months (mean) of follow‐up Procedures performed by 'experienced surgeons on routine operating lists' |
|
| Outcomes | Change in menstrual blood loss Duration of surgery (minutes) Duration of hospital stay (days) Return to work (weeks) Postoperative complications Requirement for further surgery Resource cost of surgery (theatre and ward) (per woman) | |
| Notes | Endometrial resection women given an intramuscular injection of medroxyprogesterone acetate 150 mg 4 to 6 weeks before surgery to reduce endometrial thickness Author contacted but no reply received | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation sequence not described |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelope but no other safeguards described |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not feasible for a comparison of surgical techniques |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts minimal and not likely to cause bias |
| Selective reporting (reporting bias) | Unclear risk | No prior protocol identified |
| Other bias | Low risk | Groups appeared balanced at baseline, although very few parameters examined |
Jain 2016.
| Methods | Randomisation by sealed envelope Single‐centre, parallel‐group, no blinding Number of women randomly assigned: n = 40 Number of withdrawals: n = 0 | |
| Participants | Department of Obstetrics and Gynecology, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India 40 women randomized Inclusion criteria: 1. Women over 40 years 2. No desire for future childbearing 3. HMB PBAC score ≥100 4. Uterine size up to 14 weeks of pregnancy 5. leiomyomas of 5 cm in diameter or less 6. uterocervical length of 12 cm or less Exclusion criteria: 1. Acute pelvic inflammatory disease or pelvic pathology (e.g. adenomyosis, gynaecologic cancers (including endometrial malignancy)) 2. Atypical endometrial hyperplasia 3. Submucosal leiomyomas |
|
| Interventions | Thermal balloon ablation: 20 woman Vaginal hysterectomy: 20 woman |
|
| Outcomes | Amenorrhoea and hypomenorrhoea at 1, 6, 12 and 24 months Requirement of further HT Haemoglobin level at 6 months Operative time, blood loss Intraoperative and postoperative events (VAS up to 72 hrs post procedure, adverse events) Hospital stay Improvement from baseline UFS_QOL scores. |
|
| Notes | Source of funding: not reported Declare no conflicts of interest Timeframe: 1 November 2012 and 31 October 2014. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly allocated into 2 groups (TBA and vaginal hysterectomy) in a 1:1 ratio using computer‐generated random number tables |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding: participants, investigators, and data analysts were not masked to group assignment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | All the outcomes previously specified were reported |
| Other bias | Low risk | Source of funding: not reported Declare no conflicts of interest |
O'Connor 1997.
| Methods | Randomisation at a ratio of 2:1 from a computer‐generated random number sequence, with the code kept at the Royal Free Hospital Multi‐centre, parallel‐group with no blinding Number of women randomly assigned: n = 202 Number of withdrawals: n = 30 (26 before surgery and 4 lost to follow‐up) Power calculation for sample size performed and analysis by intention to treat Source of funding: Medical Research Council | |
| Participants | Women 30 to 50 years of age who had symptomatic menorrhagia that required hysterectomy were recruited from several centres in the UK (King's Lynn, Portsmouth, Plymouth, London, Bradford, Chelmsford, Northampton, Birmingham and Exeter) Inclusion criteria: 30 to 50 years of age, decision to have no more children, regular menstrual cycles of between 21 and 35 days, with each period lasting for less than 50% of the cycle, documented evidence of normal endometrial histology within the previous 12 months and normal cervical smear within the previous 3 years Exclusion criteria: serious intercurrent illness, intermenstrual or postcoital bleeding, uterine size corresponding to pregnancy of greater than 12 weeks of gestation, submucous fibroids larger than 5 cm in diameter, adnexal tenderness that is suggestive of pelvic inflammatory disease or endometriosis, major uterovaginal prolapse or severe urinary symptoms, severe premenstrual syndrome or menopausal symptoms | |
| Interventions | Treatment 1: transcervical endometrial resection, n = 116
Treatment 2: hysterectomy, n = 46 (n = 28 abdominal, n = 28 vaginal)
Duration: 2 years (median) of follow‐up Surgeons performing TCRE required prior experience of at least 20 procedures. Surgeons performing hysterectomy were 'experienced' or were supervised by an experienced surgeon |
|
| Outcomes | Satisfaction rate at 2 years Quality of life (General Health Questionnaire, Mood scales, Social Adjustment Scale)—these were not entered in this review because the data were in graphical form and were not provided in numerical form by the authors Duration of surgery (minutes) Duration of hospital stay (days) Blood loss (this outcome not entered in the review because SD was too large and data were not available for transformation) Difficulty of surgery (this outcome not entered in the review) Complication rate Requirement for further surgery | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number sequence |
| Allocation concealment (selection bias) | Low risk | Code to randomisation kept separate, with telephoning for next assignment |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not feasible for a comparison of surgical techniques |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dropouts greater than 10% and reasons not given |
| Selective reporting (reporting bias) | Unclear risk | No prior protocol identified |
| Other bias | Low risk | Groups appeared balanced at baseline. No other potential bias identified |
Pinion 1994.
| Methods | Randomisation, ratio of 2:1:1 (hysterectomy:resection:ablation), by a series of numbered opaque envelopes in a random order Single‐centre, parallel‐group, no blinding Number of participants randomly assigned: n = 204 Number of withdrawals: n = 6 (2 before surgery and 4 refused the allocated treatment) Power calculation for sample size performed and analysis by intention to treat Source of funding: Scottish Office Home and Health Dept and ICI (Zeneca) | |
| Participants | Women with mean age of 40 years, eligible to undergo hysterectomy for menorrhagia, recruited from the general gynaecology clinics of the Aberdeen Royal Infirmary in Scotland, UK Inclusion criteria: age < 50 years, weight < 100 kg, clinical diagnosis of dysfunctional uterine bleeding, uterus < 10 weeks of gestational size, normal endometrial histology No exclusion criteria reported | |
| Interventions | Treatment 1: laser ablation (n = 53) or endometrial resection (n = 52)
Treatment 2: hysterectomy (n = 87 abdominal, n = 12 vaginal), n = 99
Duration: 4 years of follow‐up Prior experience of the surgeon not mentioned |
|
| Outcomes | Satisfaction rate at 1 and 4 years Change in general health Change in MBL Duration of surgery (minutes) Duration of hospital stay (days) Return to work (weeks) Complication rate Quality of life (Hospital Anxiety and Depression Scale, Golombok Rust Inventory of Marital State) Quality of life (Psychosocial Adjustment to Illness Scale)—this outcome not entered in the review because not enough information provided about categories Health service costs at 1 and 4 years Participant costs at 1 year Requirement for further surgery | |
| Notes | Author contacted for additional data but no reply received This trial has 4 publications using the same study population and assessing different outcomes Data usually available only for the laser ablation and endometrial resection combined | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation sequence not described |
| Allocation concealment (selection bias) | Low risk | Series of numbered opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not feasible for a comparison of surgical techniques |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts minimal and unlikely to cause bias |
| Selective reporting (reporting bias) | Unclear risk | No prior protocol identified |
| Other bias | Low risk | Groups appeared balanced at baseline and no other potential bias identified |
Sesti 2011.
| Methods | Randomisation by computer‐generated sequence of serially numbered opaque envelopes Single‐centre parallel‐group with blinding of assessors Number of women randomly assigned: n = 68 Number of withdrawals: n = 0 Power calculation for sample size performed and analysis by intention to treat Source of funding: Italian Ministry of University |
|
| Participants | Women 35 to 50 years of age with heavy menstrual bleeding, who had failed appropriate first‐line oral medical therapy and required surgical treatment Inclusion criteria: PBAC score ≥ 100 (average of 2 consecutive cycles), completed family, normal smear, pelvic ultrasound scan and endometrial biopsy Exclusion criteria: previous endometrial resection/ablation, previous levonorgestrel intrauterine system, any uterine pathology on pelvic ultrasound scan or hysteroscopy, any pathology whereby hysterectomy was indicated, uninvestigated abnormal bleeding or postmenopausal bleeding |
|
| Interventions | Treatment 1: endometrial ablation via Thermachoice III thermal balloon ablation Treatment 2: laparoscopic subtotal hysterectomy Duration of follow‐up: 24 months All surgery was performed by the same 2 surgeons; however, prior experience of the surgeon not mentioned |
|
| Outcomes | Primary: Menstrual bleeding (PBAC score) at 3, 6, 12 and 24 months Secondary: Quality of life (SF‐36 score) at 24 months Improvement in bleeding patterns (frequency and duration of bleeding) at 3, 6, 12 and 24 months Haemoglobin levels at 3, 6, 12 and 24 months Intensity of postoperative pain Early postoperative complications |
|
| Notes | Information included in the study was sufficient for meta‐analysis—not necessary to contact authors | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation sequence |
| Allocation concealment (selection bias) | Low risk | Serially numbered, opaque sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not feasible for a comparison of surgical techniques |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All women accounted for in groups to which they were randomly assigned |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported. |
| Other bias | Low risk | Groups balanced at baseline. No other potential bias identified |
Zupi 2003.
| Methods | Computer‐generated randomisation number sequence Single‐centre, parallel‐group, single‐blind (assessors of SF‐36 results) Number of women randomly assigned: 203 Number of women analysed: 181 Power calculation for sample size (power of 0.8 for difference in satisfaction rate of 50% between groups) Analysis was by intention to treat Source of funding: not reported |
|
| Participants | Women with mean age of 43 years with menometrorrhagia unresponsive to medical treatment, recruited between March 1995 and February 1997 from Departmental O and G Clinic in the Tor Vergarta University of Rome, Italy Inclusion: younger than 50 years of age; weight less than 100 kg; not seeking contraception; normal endometrial histology and Pap smear within the previous 6 months; uterus not greater than 12 weeks of pregnancy in size; without submucosal fibroids, adnexal masses or endometriosis Exclusion: no further exclusion criteria reported |
|
| Interventions | Treatment 1: pretreatment with GnRHa 1 month before surgery, then hysteroscopic endometrial resection Treatment 2: laparoscopic supracervical hysterectomy Duration: 2 years (follow‐up at 3 months, at 1 and 2 years) All surgeons were proficient in both endometrial resection and laparoscopic hysterectomy |
|
| Outcomes | Pain (immediately after surgery and then for a week) Duration of vaginal bleeding Date resumed normal activities, sexual intercourse, work Quality of life (SF‐36) Further surgery Operative outcomes (duration of surgery, blood loss, complications, hospital stay) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number sequence |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not feasible for a comparison of surgical techniques. Single blinding of assessors who administered the SF‐36, but women who provided the answers knew of their assignment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts minimal and unlikely to cause bias |
| Selective reporting (reporting bias) | Unclear risk | No prior protocol identified |
| Other bias | Low risk | Groups appeared balanced at baseline and no other potential bias identified |
GnRHa = gonadotrophin‐releasing hormone agonists IUD = intrauterine device MBL = menstrual blood loss PBAC = pictorial blood assessment chart PID = pelvic inflammatory disease VAS = visual analogue scale (pain)
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Lin 2006 | Not an RCT |
| Paddison 2003 | Not an RCT |
Characteristics of ongoing studies [ordered by study ID]
ISRCTN49013893.
| Trial name or title | Hysterectomy or Endometrial AbLation Trial for Heavy menstrual bleeding (HEALTH) |
| Methods | Multicentre randomised controlled trial |
| Participants | Premenopausal women with heavy menstrual bleeding eligible for surgical treatment. Target number 648. |
| Interventions | Laparoscopic supracervical hysterectomy versus endometrial ablation. |
| Outcomes | Primary outcome measure 1. Menorrhagia multi‐attribute scale (MMAS), a condition‐specific Quality of Life outcome 2. Patient satisfaction, measured on a 6‐point scale (from “totally satisfied” to “totally dissatisfied”) measured at 12 months post surgery 3. Incremental cost (to the health service) per quality‐adjusted life year (QALY) gained (LASH versus EA) Secondary outcome measures Patient reported: 1. MMAS at 6 months 2. Patient reported satisfaction at 6 months 3. Acceptability of procedure measured at 6 weeks 4. Severity of post‐operative pain using a pain Numerical Rating Scale (NRS) measured at 1 to 14 days and at 6 weeks, symptom diary days 1 to 14 (including analgesic use) 5. Generic health related quality of life (SF‐12, EQ‐5D 3‐L) measured at baseline, 6 and 12 months 6. Sexual Activity Questionnaire (SAQ) at baseline, 6 and 12 months Clinical 1. Duration of operation 2. Peri‐operative complications and recovery details including analgesia requirements 3. Time to discharge 4. Further gynaecological surgery by 12 months Economic Wider societal costs associated with changes in productivity based on information on the time taken to return to normal activities (following intervention) combined with questions on work productivity delivered during the follow‐up period. Further, a simple Markov model, based on within‐trial data supplemented by available published data on the requirement for further gynaecological surgery over time (following the alternative procedures) will be developed and used to extrapolate cost‐effectiveness beyond 12 months. Overall trial start date |
| Starting date | January 2014, completed October 2018 |
| Contact information | Centre for Healthcare Randomised Trials chart@abdn.ac.uk |
| Notes |
Differences between protocol and review
On the protocol and previous versions of the review the outcome 'Further gynaecological surgery' included any further gynaecological surgery, meaning if the woman had a oophorectomy or a cystoscopy this was valid as further surgery. In the 2019 update, the outcome was limited to further gynaecological surgery for HMB, and the data extraction was re‐checked and updated.
Contributions of authors
In the 2019 version of the review Magdalena Bofill Rodriguez performed selection of trials, data extraction, and data entry and prepared all versions of drafts and the final version of the review for comments from the other review authors. Rosalie Fergusson performed selection of trials, data extraction and commented on drafts and final version of the review. Anne Lethaby commented on all versions of drafts and the final version of the review. Cindy Farquhar commented on the final version of the review.
In the 2013 version of the review, Dr Rosalie Fergusson rewrote all sections of the review, including updating the protocol in line with current Cochrane Collaboration standards.
Dr Rosalie Fergusson and Anne Lethaby performed searches for relevant studies, selected studies for inclusion based on the protocol criteria, assessed the included trials for quality and performed data extraction and entered data, aside from the sections involving cost, for the 2013 update. They also incorporated changes suggested by the peer review.
In the 2008 version of the review, Dr Sasha Shepperd was involved in selection of trials for inclusion and independently assessed the quality of the included studies and performed data extraction. She performed a significant role in editing the final draft and analysing the cost data. Dr Cindy Farquhar wrote the conclusions to the first published version of the review and helped edit the final draft when the review was first published.
Sources of support
Internal sources
Department of Obstetrics and Gynaecology, National Women's Hospital, Auckland, New Zealand.
External sources
NHS Executive, Anglia and Oxford Region R&D Programme, UK.
Health Research Council, Auckland, New Zealand.
Declarations of interest
No conflicts of interest were reported by RF, MB, AL, or CF.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Crosignani 1997 {published data only}
- Crosignani PG, Vercellini P, Apolone G, Giorgi O, Cortesi I, Meschia M. Endometrial resection versus vaginal hysterectomy for menorrhagia: long‐term clinical and quality‐of‐life outcomes. American Journal of Obstetrics and Gynecology 1997;177(1):95‐101. [DOI] [PubMed] [Google Scholar]
Dickersin 2007 {published data only}
- Dickersin K, Munro M, Langenberg P, Scherer R, Frick KD, Weber AM, et al. Surgical treatments outcomes project for dysfunctional uterine bleeding (STOP‐DUB): design and methods. Controlled Clinical Trials 2003;24(5):591‐609. [DOI] [PubMed] [Google Scholar]
- Dickersin K, Munro MG, Clark M, Langenberg P, Scherer R, Frick K, et al. Hysterectomy compared with endometrial ablation for dysfunctional uterine bleeding. Obstetrics and Gynecology 2007;110(6):1279‐89. [DOI] [PubMed] [Google Scholar]
- Munro M, Dickerson K, Clark M, Langenberg P, Scherer R, Frick K. The Surgical Treatments Outcomes Project for Dysfunctional Uterine Bleeding: summary of an Agency for Health Research and Quality‐sponsored randomized trial of endometrial ablation versus hysterectomy for women with heavy menstrual bleeding. Menopause 2011;18(4):451‐8. [DOI] [PubMed] [Google Scholar]
Dwyer 1993 {published data only}
- Dwyer N, Hutton J, Stirrat GM. Randomised controlled trial comparing endometrial resection with abdominal hysterectomy for the surgical treatment of menorrhagia. British Journal of Obstetrics and Gynaecology 1993;100(3):237‐43. [DOI] [PubMed] [Google Scholar]
- Sculpher M. A cost‐utility analysis of abdominal hysterectomy versus transcervical endometrial resection for the surgical treatment of menorrhagia. International Journal of Technology Assessment in Health Care 1998;14(2):302‐19. [DOI] [PubMed] [Google Scholar]
- Sculpher MJ, Bryan S, Dwyer N, Hutton J, Stirrat GM. An economic evaluation of transcervical endometrial resection versus abdominal hysterectomy for the treatment of menorrhagia. British Journal of Obstetrics and Gynaecology 1993;100(3):244‐52. [DOI] [PubMed] [Google Scholar]
- Sculpher MJ, Dwyer N, Byford S, Stirrat GM. Randomised trial comparing hysterectomy and transcervical endometrial resection: effect on health related quality of life and costs two years after surgery. British Journal of Obstetrics and Gynaecology 1996;103(2):142‐9. [DOI] [PubMed] [Google Scholar]
Gannon 1991 {published data only}
- Gannon MJ, Holt EM, Fairbank J, Fitzgerald M, Milne MA, Crystal AM, et al. A randomised trial comparing endometrial resection and abdominal hysterectomy for the treatment of menorrhagia. BMJ (Clinical Research Ed.) 1991;303(6814):1362‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jain 2016 {published data only}
- Jain P, Rajaram S, Gupta B, Goel N, Srivastava H. Randomized controlled trial of thermal balloon ablation versus vaginal hysterectomy for leiomyoma‐induced heavy menstrual bleeding. International Journal of Gynaecology and Obstetrics 2016;135(2):140‐4. [https://doi.org/10.1016/j.ijgo.2016.04.020] [DOI] [PubMed] [Google Scholar]
O'Connor 1997 {published data only}
- O'Connor H, Broadbent JA, Magos AL, McPherson K. Medical Research Council randomised trial of endometrial resection versus hysterectomy in management of menorrhagia. Lancet 1997;349(9056):897‐901. [DOI] [PubMed] [Google Scholar]
Pinion 1994 {published data only}
- Aberdeen Endometrial Ablation Trials Group. A randomised trial of endometrial ablation versus hysterectomy for the treatment of dysfunctional uterine bleeding: outcome at four years. British Journal of Obstetrics and Gynaecology 1999;106(4):360‐6. [DOI] [PubMed] [Google Scholar]
- Alexander DA, Naji AA, Pinion SB, Mollison J, Kitchener HC, Parkin DE, et al. Randomised trial comparing hysterectomy with endometrial ablation for dysfunctional uterine bleeding: psychiatric and psychosocial aspects. BMJ (Clinical Research Ed.) 1996;312(7026):280‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron IM, Mollison J, Pinion SB, Atherton‐Naji A, Buckingham K, Torgerson D. A cost comparison of hysterectomy and hysteroscopic surgery for the treatment of menorrhagia. European Journal of Obstetrics and Gynaecology 1996;70(1):87‐92. [DOI] [PubMed] [Google Scholar]
- Pinion SB, Parkin DE, Abramovich DR, Naji A, Alexander DA, Russell IT, et al. Randomised trial of hysterectomy, endometrial laser ablation, and transcervical endometrial resection for dysfunctional uterine bleeding. British Medical Journal (Clinical Research Ed.) 1994;309(6960):979‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sesti 2011 {published data only}
- Sesti F, Ruggeri V, Pietropolli A, Piancatelli R, Piccione E. Thermal balloon ablation versus laparoscopic supracervical hysterectomy for the surgical treatment of heavy menstrual bleeding: a randomized study. Journal of Obstetrics and Gynaecology Research 2011;37(11):1650‐7. [DOI] [PubMed] [Google Scholar]
Zupi 2003 {published data only}
- Centini G, Lazzeri L, Finco A, Afors K, Zupi E. Quality of life and risk of reintervention comparing endometrial ablation and laparoscopic sutotal hysterectomy: A 15 years follow up study. Gynecological Surgery 2015;12(Suppl 1):S11. [Google Scholar]
- Zupi E, Centini G, Lazzeri L, Finco A, Exacoustos C, Afors, et al. Hysteroscopic endometrial resection versus laparoscopic supracervical hysterectomy for abnormal uterine bleeding: long term follow‐up of a prospective randomized trial. Journal of Minimally Invasive Gynecology 2015;22(5):841‐5. [DOI: 10.1016/j.jmig.2015.08.108] [DOI] [PubMed] [Google Scholar]
- Zupi E, Zullo F, Marconi D, Sbracia M, Pellicano M, Solima E, et al. Hysteroscopic endometrial resection versus laparoscopic supracervical hysterectomy for menorrhagia: a prospective randomized trial. American Journal of Obstetrics and Gynecology 2003;188(1):7‐12. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Lin 2006 {published data only}
- Lin H. Comparison between microwave endometrial ablation and total hysterectomy. Chinese Medical Journal 2006;119(14):1195‐7. [PubMed] [Google Scholar]
Paddison 2003 {published data only}
- Paddison K. Menorrhagia: endometrial ablation or hysterectomy. Nursing Standard 2003;18(1):33‐7. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
ISRCTN49013893 {published data only}
- Cooper K, McCormack K, Breeman S, Wood J, Scott NW, et al. HEALTH: Laparoscopic supracervical hysterectomy versus second‐generation endometrial ablation for the treatment of heavy menstrual bleeding: Study protocol for a randomised controlled trial. Trials 2018;19(1):63. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Adelman 2014
- Adelman MR, Bardsley TR, Sharp HT. Urinary tract injuries in laparoscopic hysterectomy: a systematic review. Journal of Minimally Invasive Gynecology 2014;21(4):558‐66. [DOI: 10.1016/j.jmig.2014.01.006] [DOI] [PubMed] [Google Scholar]
Athanatos 2015
- Athanatos D, Pados G, Venetis CA, Stamatopoulos P, Rousso D, Tsolakidis D. Novasure impedance control system versus microwave endometrial ablation for the treatment of dysfunctional uterine bleeding: a double‐blind, randomized controlled trial. Clinical and Experimental Obstetrics & Gynecology 2015;42(3):347‐51. [PUBMED: 26152008] [PubMed] [Google Scholar]
Bhattacharya 2011
- Bhattacharya S, Middleton L, Tsourapas A, Champaneria R, Daniels J, Roberts T, et al. Hysterectomy, endometrial ablation and Mirena for heavy menstrual bleeding: a systematic review of clinical effectiveness and cost‐effectiveness analysis. Health Technology Assessment April 2011; Vol. 19:1‐252. [DOI] [PMC free article] [PubMed]
Bofill Rodriguez 2019
- Bofill Rodriguez M, Lethaby A, Grigore M, Brown J, Hickey M, Farquhar C. Endometrial resection and ablation techniques for heavy menstrual bleeding. Cochrane Database of Systematic Reviews 2019, Issue 1. [DOI: 10.1002/14651858.CD001501.pub5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bourdrez 2004
- Bourdrez P, Bongers MY, Mol BWJ. Treatment of dysfunctional uterine bleeding: patient preferences for endometrial ablation, a levonorgestrel‐releasing intrauterine device, or hysterectomy. Fertility and Sterility 2004;82(1):160‐6. [DOI] [PubMed] [Google Scholar]
Brazier 1993
- Brazier JE, Jones NMB, Kind P. Testing the validity of the Euroqol and comparing it with the SP36 health survey questionnaire. Quality of Life Research 1993;2(3):169‐80. [DOI] [PubMed] [Google Scholar]
Bridgman 1994
- Bridgman SA. Increasing operative rates for dysfunctional uterine bleeding after endometrial ablation (letter). Lancet 1994;344:893. [DOI] [PubMed] [Google Scholar]
Clegg 2007
- Clegg JP, Guest JF, Hurskainen R. Cost‐utility of levonorgestrel intrauterine system compared with hysterectomy and second generation endometrial ablative techniques in managing patients with menorrhagia in the UK. Current Medical Research and Opinion 2007;23(7):1673‐48. [DOI] [PubMed] [Google Scholar]
Cooper 2011
- Cooper K, Lee A, Chien P, Raja E, Timmaraju V, Bhattacharya S. Outcomes following hysterectomy or endometrial ablation for heavy menstrual bleeding: retrospective analysis of hospital episode statistics in Scotland. British Journal of Obstetrics and Gynaecology 2011;118(10):1171‐9. [DOI] [PubMed] [Google Scholar]
Coulter 1991
- Coulter A, Bradlow J, Agass M, Martin‐Bates C, Tullock A. Outcomes of referrals to gynaecology outpatient clinics for menstrual problems: an audit of general practice records. British Journal of Obstetrics and Gynaecology 1991;98(8):789‐96. [DOI] [PubMed] [Google Scholar]
Coulter 1994
- Coulter A. Trends in gynaecological surgery (letter). Lancet 1994;344:1367. [DOI] [PubMed] [Google Scholar]
EuroQol Group 1990
- EuroQol Group. EuroQol—a new facility for the measurement of health‐related quality of life. Health Policy (Amsterdam, Netherlands) 1990;16(3):199‐208. [DOI] [PubMed] [Google Scholar]
Fernandez 2011
- Fernandez H. Update on the management of menometrorrhagia: new surgical approaches. Gynecological Endocrinology 2011;Suppl 1:1131‐6. [DOI] [PubMed] [Google Scholar]
Garrat 1995
- Garrat AM, Torgerson DJ, Wyness J, Hall MH, Reid DM. Measuring sexual functioning in premenopausal women. British Journal of Obstetrics and Gynaecology 1995;102(4):311‐6. [DOI] [PubMed] [Google Scholar]
Garside 2004
- Garside R, Stein K, Wyatt K, et al. A cost‐utility analysis of microwave and thermal balloon endometrial ablation techniques for the treatment of heavy menstrual bleeding. British Journal of Obstetrics and Gynaecology 2004;111(10):1103‐14. [DOI] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- McMaster University (developed by Evidence Prime). GRADEpro GDT. Version accessed prior to 17 July 2019. Hamilton (ON): McMaster University (developed by Evidence Prime).
Higgins 2008
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2008;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org. Version 5.0.0. New York: John Wiley & Sons, 2011.
Kalampolas 2017
- Kalampokas E, McRobbie S, Payne F, Parkin DE. Long‐term incidence of hysterectomy following endometrial resection or endometrial ablation for heavy menstrual bleeding. International Journal of Gynaecology and Obstetrics 2017;139(1):61‐4. [DOI: 10.1002/ijgo.12259] [DOI] [PubMed] [Google Scholar]
Kennedy 2002
- Kennedy ADM, Sculpher MJ, Coulter A, Dwyer N, Rees M, Abrams KR, et al. Effects of decision aids for menorrhagia on treatment choices, health outcomes and costs. JAMA 2002;288(21):2701‐8. [DOI] [PubMed] [Google Scholar]
Kumar 2016
- Kumar V, Chodankar R, Gupta J K. Endometrial ablation for heavy menstrual bleeding. Women's Health (London, England) 2016;12(1):45‐52. [DOI: 10.2217/whe.15.86] [DOI] [PMC free article] [PubMed] [Google Scholar]
Laberge 2016
- Laberge P, Leyland N, Murji A, Fortin C, Martyn P, Vilos G, et al. Endometrial ablation in the management of abnormal uterine bleeding. Journal d'Obstetrique et Gynecologie du Canada : JOGC [Journal of Obstetrics and Gynaecology Canada : JOGC] 2015;37(4):362‐79. [PUBMED: 26001691] [DOI] [PubMed] [Google Scholar]
Li 2012
- Li M, Han Y, Feng YC. Single‐port laparoscopic hysterectomy vs conventional laparoscopic hysterectomy: a prospective randomised trial. Journal of International Medical Research 2012;40(2):701‐8. [DOI] [PubMed] [Google Scholar]
Madhu 2009
- Madhu CK, Nattey J, Naeem T. Second generation endometrial ablation techniques: an audit of clinical practice. Archives of Gynecology and Obstetrics 2009;280(4):599‐602. [DOI: 10.1007/s00404-009-0982-7] [DOI] [PubMed] [Google Scholar]
Munro 2011
- Munro MG, Critchley HO, Broder MS, Fraser IS. FIGO classification system (PALM‐COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. International Journal of Gynaecology and Obstetrics 2011;113(1):3‐13. [DOI] [PubMed] [Google Scholar]
Nagele 1998
- Nagele F, Rubinger T, Magos A. Why do women choose endometrial ablation rather than hysterectomy?. Fertility and Sterility 1998;69(6):1063‐6. [DOI] [PubMed] [Google Scholar]
NICE 2007
- National Collaborating Centre for Women's and Children's Health. Heavy Menstrual Bleeding. London: RCOG Press, 2007. [PubMed] [Google Scholar]
NICE 2018
- NICE guideline. Heavy menstrual bleeding: assessment and management. www.nice.org.uk/guidance/ng88 2018.
Overton 1997
- Overton C, Hargreaves J, Maresh M. A national survey of the complications of endometrial destruction for menstrual disorders: the MISTLETOE study. British Journal of Obstetrics and Gynaecology 1997;104(12):1351‐9. [DOI] [PubMed] [Google Scholar]
Reich 1989
- Reich H, DeCaprio J, McGlynn F. Laparoscopic hysterectomy. Journal of Gynaecological Surgery 1989;5:213. [Google Scholar]
Reid 2007
- Reid PC. Endometrial ablation in England—coming of age? An examination of hospital episode statistics 1989/1990 to 2004/2005. European Journal of Obstetrics and Gynecology 2007;135(2):191‐4. [DOI] [PubMed] [Google Scholar]
Roberts 2011
- Roberts T, Tsourapas A, Champaneria R, Daniels J, Cooper K, Bhattacharya S, et al. Hysterectomy, endometrial ablation, and levonorgestrel releasing intrauterine system (Mirena) for treatment of heavy menstrual bleeding: cost effectiveness analysis. BMJ April 2011;342:d2202. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rust 1986
- Rust J, Bennum I, Crowe M, Golombok S. The construction and validation of the Golombok Rust inventory of marital state. Sexual and Marital Therapy 1986;1:34‐40. [Google Scholar]
Sculpher 1998
- Sculpher M. The cost‐effectiveness of preference‐based treatment allocation: the case of hysterectomy versus endometrial resection in the treatment of menorrhagia. Health Economics 1998;7(2):129‐42. [DOI] [PubMed] [Google Scholar]
Sharp 2012
- Sharp HT. Endometrial ablation: postoperative complications. American Journal of Obstetrics and Gynecology 2012;207(4):242‐7. [DOI] [PubMed] [Google Scholar]
Vessey 1992
- Vessey M, Villard‐Mackintosh L, McPherson K, Coulter A, Yeates D. The epidemiology of hysterectomy: findings in a large cohort study. British Journal of Obstetrics and Gynaecology 1992;99(5):402‐7. [DOI] [PubMed] [Google Scholar]
Ware 1993
- Ware JE, Snow KK, Kosinski M, et al. SF‐36 Health survey: manual and interpretation guide. The Health Institute. Boston: New England Medical Centre, 1993. [Google Scholar]
Woolcock 2008
- Woolcock JG, Critchley HO, Munro MG, Broder MS, Fraser IS. Review of the confusion in current and historical terminology and definitions for disturbances in menstrual bleeding. Fertility and Sterility 2008;90(6):2269. [DOI] [PubMed] [Google Scholar]
You 2006
- You JH, Sahota DS, Yuen PM. A cost‐utility analysis of hysterectomy, endometrial resection and ablation and medical therapy for menorrhagia. Human Reproduction (Oxford, England) 2006;21(7):1878‐83. [DOI] [PubMed] [Google Scholar]
Zigmond 1983
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica 1983;67(6):361‐70. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Cooke 1996
- Cooke I, Shepperd S. Comparison of the effectiveness of endometrial resection and ablation to reduce heavy menstrual bleeding versus hysterectomy. Cochrane Database of Systematic Reviews 1996, Issue 2. [DOI: 10.1002/14651858.CD000329] [DOI] [PubMed] [Google Scholar]
Lethaby 1999
- Lethaby A, Shepperd S, Cooke I, Farquhar C. Endometrial resection and ablation versus hysterectomy for heavy menstrual bleeding. Cochrane Database of Systematic Reviews 1999, Issue 2. [DOI: 10.1002/14651858.CD000329] [DOI] [PubMed] [Google Scholar]
Lethaby 2009
- Lethaby A, Shepperd S, Farquhar C, Cooke I. Endometrial resection and ablation versus hysterectomy for heavy menstrual bleeding. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD000329] [DOI] [PubMed] [Google Scholar]
Lethaby 2013
- Fergusson RJ, Lethaby A, Shepperd S, Farquhar C. Endometrial resection and ablation versus hysterectomy for heavy menstrual bleeding. Cochrane Database of Systematic Reviews 2013, Issue 11. [DOI: 10.1002/14651858.CD000329.pub2] [DOI] [PubMed] [Google Scholar]


