Abstract
Despite continued advances in health care, the cardiovascular disease (CVD) mortality rate has plateaued in recent years and appears to be trending upward. Poor diet is a leading cause of obesity and type 2 diabetes mellitus, which are leading contributors to CVD morbidity and mortality. Although dietary modification is a cornerstone of CVD prevention, implementation in clinical practice is limited by inadequate formal training in nutrition science. In this report, we review the individual components of a heart-healthy diet, evidence-based dietary recommendations, and the impact of diet on CVD risk factor prevention and management. Furthermore, we examine the unique difficulties of dietary counseling in low-socioeconomic-status environments and provide an evidence-based approach to better serve these populations. We utilized PubMed searches in adults with no date restriction with the following search terms: “carbohydrate,” “fat,” protein,” “DASH,” “Mediterranean,” “plant-based,” “vegetarian,” “cardiovascular disease,” “obesity,” “weight loss,” “diabetes,” “socioeconomic status,” and “race.” In this review, we demonstrate that patients should focus on implementing a general diet plan that is high in fruits, whole grains, legumes, and nonstarchy vegetables while low in trans-fats, saturated fats, sodium, red meat, refined carbohydrates, and sugar-sweetened beverages. The Dietary Approaches to Stop Hypertension, Mediterranean, and vegetarian diets have the most evidence for CVD prevention. Clinicians should understand the barriers that patients may face in terms of access to healthy dietary choices. Further research is needed to determine the dietary changes that are most economically, socioculturally, and logistically feasible to reduce these barriers. Improvement in diet is a public health priority that can lead to a significant population-level reduction in CVD morbidity and mortality. It is imperative that clinicians understand current dietary practice guidelines and implement evidence-based dietary counseling in those at high risk for CVD.
Abbreviations and Acronyms: ACC, American College of Cardiology; AHA, American Heart Association; CHD, coronary heart disease; CVD, cardiovascular disease; DASH, Dietary Approaches to Stop Hypertension; HDL-C, high-density lipoprotein cholesterol; LCHF, low-carbohydrate high-protein/fat; LDL-C, low-density lipoprotein cholesterol; MI, myocardial infarction; PURE, Prospective Urban Rural Epidemiology; RCT, randomized control trial; SBP, systolic blood pressure; SES, socioeconomic status; SSB, sugar-sweetened beverage; USDA, US Department of Agriculture
Article Highlights.
-
•
Poor diet is a leading cause of obesity, type 2 diabetes and cardiovascular disease (CVD).
-
•
Dietary modification is a cornerstone of CVD prevention and can reduce CVD morbidity and mortality.
-
•
This review is a guideline for implementation of evidence-based dietary counseling by physicians.
-
•
We review heart-healthy diets and evidence-based dietary recommendations.
-
•
DASH, Mediterranean, and vegetarian diets have the most evidence for CVD prevention.
The rate of cardiovascular disease (CVD) mortality reduction in the United States has plateaued in recent years despite the development of new medical therapies, increased access to health care, and increased health care spending, in large part due to the increasing prevalence of obesity and type 2 diabetes mellitus in younger individuals.1, 2 Furthermore, the US Burden of Disease Collaborators have cited poor diet as the leading cause of premature death and disability nationally, with obesity-related health care costs in the United States totaling as high as $210 billion per year.3, 4
Nutrition counseling is a core aspect of primary and secondary prevention of hyperlipidemia, hypertension, type 2 diabetes mellitus, and CVD. Healthy diet interventions are also central to promoting weight loss and preventing metabolic syndrome, even in those with an elevated genetic risk for obesity.5 Accordingly, it is imperative that clinicians are familiar with the scientific evidence underlying healthy dietary recommendations and that they implement personalized counseling based on their patients' comorbid conditions, health literacy, and financial limitations.
Although clinicians may feel limited in their ability to deliver nutritional advice due to time constraints and lack of reimbursement for dietary counseling, another leading barrier to dietary counseling implementation is the paucity of formal training in nutrition science in graduate and postgraduate medical training.6, 7, 8 Medical students typically receive only approximately 19 hours of diet/nutrition training, which is largely focused on basic science rather than nutrition counseling and clinical practice guidelines.6 There are no formal requirements for nutrition/diet education in either the Accreditation Council for Graduate Medical Education internal medicine residency or fellowship in cardiology or endocrinology.7, 8 Given that it is unrealistic and inefficient to refer all patients to dieticians, it is necessary for clinicians to be knowledgeable and discuss healthy dietary interventions with their patients.
In this review, we include data from individual randomized controlled trials (RCTs) conducted for primary and secondary prevention, meta-analyses, high-quality observational studies and reviews, and major society guidelines pertinent to clinical nutrition, CVD, diabetes mellitus, obesity, and socioeconomic determinants of health. We used PubMed searches in adults with no restriction on published data with the following search terms: “carbohydrate,” “fat,” protein,” “DASH,” “Mediterranean,” “plant-based diet,” “vegetarian,” “cardiovascular disease,” “obesity,” “weight loss,” “diabetes,” “socioeconomic status,” and “race.” Articles published in languages other than English were not considered. The quality of identified studies was assessed in broad terms, based on the quality of study design, duration, control of diet and external confounders, and sample size.
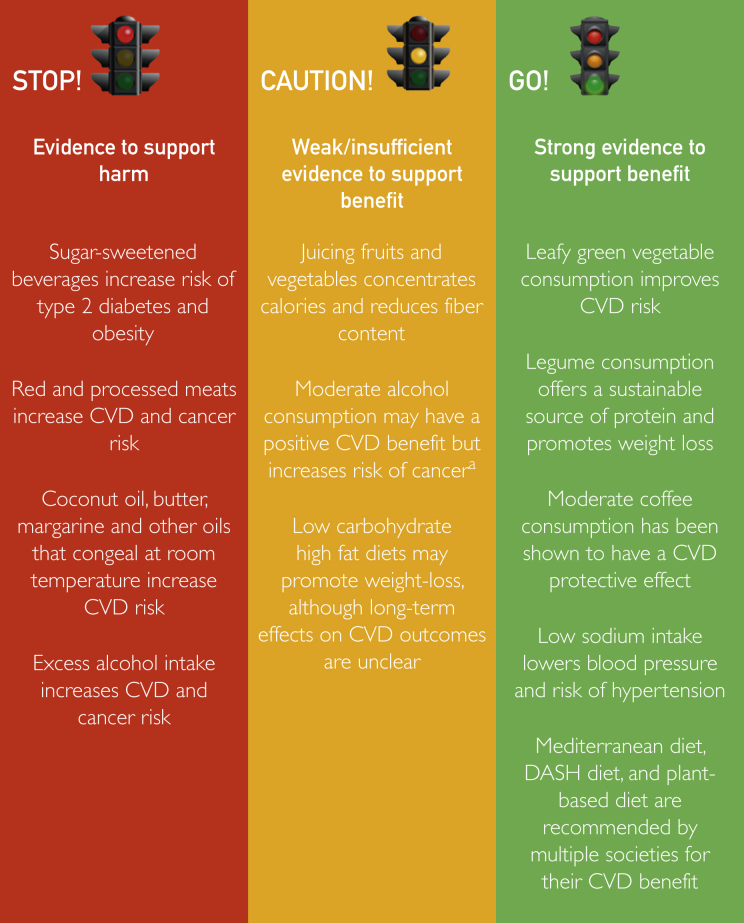
We discuss the general components of a heart-healthy diet, major evidence-based dietary patterns, and specific nutritional approaches to improve CVD risk factors, such as obesity, hypertension, type 2 diabetes mellitus, and hyperlipidemia (Figure 1). Finally, we provide a pragmatic approach to nutrition counseling for all patients, including those of low socioeconomic status (SES).
Figure 1.
Impact of dietary intervention on cardiovascular health classified by evidence to support benefit or harm. aSafe alcohol consumption depends on quantity consumed, timing (such as with driving or sleep), sex, medical history, and the effect of alcohol on the person's overall health and life. CVD, cardiovascular disease; DASH, Dietary Approaches to Stop Hypertension.
Components of the Healthy Diet
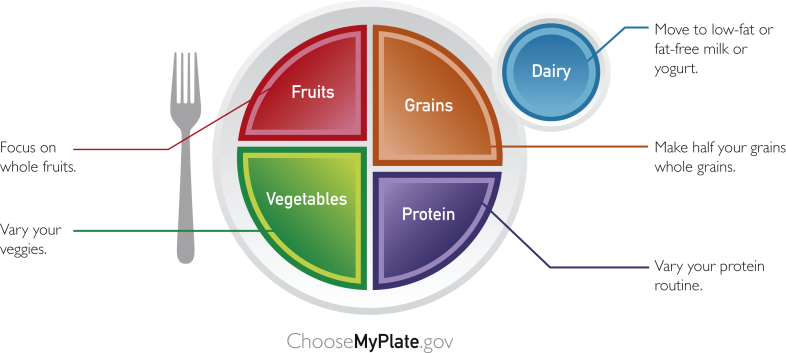
Nutrition science demonstrates that a healthy diet embraces high consumption of nonstarchy vegetables, fruits, whole grains, and legumes in addition to limited to moderate consumption of nuts, seafood, lean meats, low-fat dairy products, and vegetable oil.9 Trans-fats, saturated fats, sodium, red meat, refined carbohydrates, and sugar-sweetened beverages (SSBs) should be minimized or avoided altogether. The “United States Department of Agriculture (USDA) MyPlate” (Figure 2) may be used as a handout to help patients visualize the recommended daily intake of major food groups. The total quantity of food intake is also important, with caloric intake restriction being a key strategy to prevent overconsumption and weight gain.
Figure 2.
The “US Department of Agriculture (USDA) MyPlate” visual guide to a healthy diet.65
The 2015 to 2020 Dietary Guidelines for America recommend 3 healthy eating patterns that incorporate variants of the general principles highlighted above: 1) US healthy eating diet, 2) healthy Mediterranean diet, and 3) the healthy vegetarian diet (Table 1).9 Carbohydrates, which represent the highest proportion of caloric intake in the average diet, can be subdivided into complex and simple carbohydrates, which differ in terms of how quickly they are digested and absorbed. Simple carbohydrates, composed primarily of monosaccharide and disaccharide sugars, are found in refined grains (white flour and white rice) and table sugar; they have been shown to increase the risk for type 2 diabetes mellitus, dyslipidemia, and hypertension, as well as CVD events and mortality.10, 11
Table 1.
General Components of the DASH Diet, USDA Healthy Eating Style Pattern, USDA Healthy Mediterranean-Style Eating Pattern, and USDA Healthy Vegetarian Eating Pattern
| DASH Diet (based on 2000 calorie diet) | USDA Healthy US Style (based on 1800 calorie diet) | USDA Healthy Mediterranean (based on 1800 calorie diet) | USDA Healthy Vegetarian Diet (based on 1800 calorie diet) | |
|---|---|---|---|---|
| Grains | 6-8 servings daily | 6 ounces daily (3 whole and 3 refined) per day | 6 ounces daily (2 whole and 2 refined) per day | 6 ounces daily (3 whole and 3 refined) per day |
| Vegetables | 4-5 servings daily | 2.5 cups daily | 2.5 cups daily | 2.5 cups daily |
| Fruits | 4-5 servings daily | 2 cups daily | 2 cups daily | 1.5 cups daily |
| Nuts, seeds, and legumes | 4-5 servings daily | 3 cups daily | 2 cups daily | 3 cups daily |
| Fat-free and low-fat dairy | 2-3 servings daily | 5 ounces daily | 6 ounces daily | 3 ounces daily |
| Lean meats, poultry, and fish | <6 ounces daily | 2 ounces daily | 2 ounces daily | 2 ounces daily |
| Fats and oils | 2-3 servings daily | 24 g daily | 24 g daily | 24 g daily |
| Sweets and sugars | ≤5 servings weekly | Limit: no quantity specified | Limit: no quantity specified | Limit: no quantity specified |
| Sodium | <2.3 g daily | Limit: no quantity specified | Limit: no quantity specified | Limit: no quantity specified |
| Alcohol | ≤1 drink daily for women, ≤2 drinks daily for men | Limit: no quantity specified | Limit: no quantity specified | Limit: no quantity specified |
DASH, Dietary Approaches to Stop Hypertension; USDA, United States Department of Agriculture.
Although most packaged foods in the United States contain added sugars, SSBs account for approximately half of all added sugar intake and are associated with a dose-dependent increased risk for CVD.12 High fructose corn syrup consumption should be restricted because it is associated with weight gain and greater cholesterol level elevation than consumption of pure glucose.13 Diet soda has additionally been associated with type 2 diabetes mellitus and metabolic syndrome.14 It is thought that artificial sweetener consumption may increase the desire for sweetness and consumption of energy-dense foods. The 2018 American Heart Association (AHA) Science Advisory on Low-Calorie Sweetened Beverages and Cardiometabolic Health acknowledges a role for low-calorie sweetened beverages as a replacement strategy for adults who habitually consume SSBs due to a relatively lower risk for diabetes mellitus and obesity.15 The use of other alternatives to SSBs such as water (plain, carbonated, or unsweetened flavored) should be encouraged.
Complex carbohydrates are found in legumes, whole grains, and starchy vegetables (eg, white potatoes, corn, and green peas), the latter of which should be consumed in moderation given their caloric density. The bran and germ layers that are present in whole grains but filtered out of refined grain are rich in fiber, lignans, and other phytonutrients that are associated with higher satiety and lower glycemic index.16 Compared with refined grain intake, whole grain intake has been associated with lower CVD risk, cancer risk, and all-cause mortality.17
Legumes offer a sustainable source of protein and fiber, promote weight loss due to their low calorie and high nutrient density, and have been associated with a reduction in all-cause mortality.18 Targeting an increased intake of legumes into the diet may be especially helpful for families of low SES due to the low cost relative to nutrient benefit and long shelf life. Dried beans are especially healthful, but patients should pay attention to and avoid added sodium when consuming canned beans. Nuts are additionally an important source of protein and fiber. In addition to its association with reduced low-density lipoprotein cholesterol (LDL-C) levels, increased nut consumption has been associated with decreased all-cause mortality independent of other predictors of death.19
Vegetable consumption is pivotal for cardiovascular health and universally recommended across evidence-based healthy diets.9 Vegetables are heterogeneous in terms of their composition and health benefits, but are generally satiating, have a low glycemic index profile, and are rich in a variety of beneficial micronutrients, such as fiber, vitamins, minerals, and phytochemicals.20 Diets rich in leafy green vegetables have significant benefits on CVD reduction, likely due to multifactorial mechanisms. These include vascular benefits, such as conversion of inorganic nitrates to nitric oxide, and antioxidant and anti-inflammatory benefits from lutein, a carotenoid.21, 22 Vegetable consumption has furthermore been inversely correlated with the risk for developing hypertension, type 2 diabetes mellitus, and CVD.22, 23, 24
Whole fruits are similarly recommended across a variety of heart-healthy diets due to their antioxidant and anti-inflammatory effects, high satiety profile, and generally low glycemic index. Berries in particular are associated with flavonoids called anthocyanins, which regulate endothelial function and glycemic metabolism.25 More than 3 servings of berry consumption weekly has been associated with reduction in blood pressure and decreased risk for type 2 diabetes mellitus.26, 27 Both canned and frozen fruits, without added sugar, are excellent low-cost alternatives in low-SES settings. Fruits and vegetables should be consumed whole because “juicing” and fruit/vegetable smoothies concentrate calories, reduce fiber content, and are often associated with added sugar; fruit juice and smoothies have not been demonstrated to improve health when compared with whole fruit consumption.28 Similarly, whole fruit is preferable to dried fruit given that whole fruit is less calorie dense, has lower sugar content, and is more filling.
When assessing cardiometabolic health benefits of various carbohydrates, it is important to consider multiple nutritional characteristics simultaneously, such as grain composition, fiber content, glycemic index, presence of additional nutrients, and caloric density. Although the glycemic index has traditionally been considered beneficial for CVD and diabetes prevention and treatment,29, 30 its benefit in the prevention of CVD may be confounded by the effect of caloric density and the presence of other nutrients such as fiber, potassium, and polyphenols.
The OmniCarb RCT showed that Dietary Approaches to Stop Hypertension (DASH)-type diets with low glycemic index did not improve insulin sensitivity, lipid levels, or systolic blood pressure (SBP) in isolation and had a modest triglyceride-lowering benefit of 5 mg/dL at 5 weeks.31 Perhaps the most important indicator of high carbohydrate nutritional value is fiber content, which has been shown to be more critical for improving CVD outcomes than glycemic index or composition of grain (ie, whole grain) alone.32
Dietary fat can be categorized into unsaturated fat (mono- and polyunsaturated), saturated fat, and trans-fats. Trans-fats are the most strongly associated with adverse cardiovascular outcomes, followed by saturated fats.33 Trans-fats, which are largely consumed through partially hydrogenated oils, should be eliminated.34 Stearic acid is a saturated fatty acid found in cheese, fish, dairy, grains, and eggs that is converted to oleic acid, a beneficial omega-9 fatty acid. Stearic acid may be used as a substitute for trans-fats, given that multiple studies have shown that it does not increase LDL-C or total cholesterol levels in isolation.35, 36 Some foods that are generally not recommended in the heart-healthy diet (ie, red meats and coconut oil) contain substantial amounts of stearic acids, but these should continue to be avoided given that their overall macronutrient profile portends higher cardiovascular risk.35, 37
Intake of saturated fats, which are typically found in conjunction with trans-fats in a variety of processed foods, cheese, whole milk, butter, and margarine, should be reduced. Reducing saturated fat intake is associated with a reduction in LDL-C level; in the DASH and Dietary Effects on Lipoproteins and Thrombogenic Activity trials, a reduction in saturated fat intake from 16% to 5% resulted in an 11% decrease in LDL-C levels, from 131 to 117 mg/dL.38, 39 Favorable effects on lipid profiles are greater when saturated fat is replaced by polyunsaturated fatty acids, followed by monounsaturated fatty acids and carbohydrates (whole grain greater than refined carbohydrates).34 Cocoa butter, which is found in chocolate, is high in saturated fat and stearic acid; moderate chocolate consumption has been associated with a modest benefit in blood pressure, CVD, and stroke, although consumption of greater than 100 g per week may be deleterious due to high sugar consumption.40, 41, 42 Dark chocolate has less added sugar than milk or white chocolate and should be preferentially recommended.
Observational data from the Prospective Urban Rural Epidemiology (PURE) cohort study challenged contemporary thought by suggesting that saturated and unsaturated fat intake are associated with reduced stroke and mortality when compared with intake of refined carbohydrates.43 In this study, saturated fat was not associated with CVD risk; however, the PURE study design was limited in that it was self-reported and observational and the questionnaire was not validated. The study's generalizability to the developed world is unclear given that the high-carbohydrate diet was closely correlated with white rice consumption in lower-SES countries.44 Moreover, the study did not address trans-fats. Assessment of all current evidence suggests that patients should generally minimize consumption of both trans-fats and saturated fats in addition to reducing refined carbohydrates to mitigate the development of obesity and maximize cardiovascular health benefit.44
Meta-analysis of observational studies indicates either neutral or, for some dairy product types (ie, yogurt and cheese), protective associations for diabetes and coronary heart disease (CHD).45 Data from a recent PURE study subanalysis demonstrated an association with higher intake of total dairy (>2 servings daily) and lower total mortality, cardiovascular mortality, major CVD, and stroke when compared with no intake when adjusted for lifestyle considerations (eg, smoking and physical activity), dietary pattern, caloric intake, region, and country.46 Furthermore, there is little evidence demonstrating that dairy has harmful effects on CVD risk factors irrespective of fat content.47
The LDL-C level increasing effects of saturated fats have been shown to be attenuated when contained within complex foods such as cheese as compared with butter.48 Despite these data, major society guidelines continue to emphasize moderate consumption of low-fat dairy9, 49, 50 due to concerns regarding the impact on serum LDL-C level elevation, high caloric density, and lack of robust RCT-level evidence suggesting otherwise. Along these lines, skim or 1% milk should be recommended over whole milk given that they contain fewer calories and less saturated fat.
The 2015 to 2020 Dietary Guidelines for America generally emphasize moderate intake of lean poultry and seafood while encouraging limited intake of lean red meat. Both processed and unprocessed meats increase the risk for CVD and cancer, with processed meats such as deli/cold cuts, sausage, and bacon associated with the greatest increased risk.51 Replacing processed and unprocessed red meats with seafood, lean poultry, and nuts is associated with a reduction in CHD.52
Fish is an especially beneficial source of omega-3 polyunsaturated fatty acids. The Greenland Inuit, who ingest whale omega-3 fatty acids, have a myocardial infarction (MI) rate one-tenth that of North Americans.53 Japan has the highest ingestion of fish and the lowest risk for CHD in the world. In the Diet and Reinfarction Trial, men after MI randomly assigned to increased fish intake had a 29% reduction in total mortality and 32% reduction in CHD death compared with those randomly assigned to either increased intake of cereal or 30% decreased total fat.54 In 2 prospective cohort studies, the Multi-Ethnic Study of Atherosclerosis and Coronary Health Study, higher levels of the active compounds in omega-3 fatty acids, eicosapentaenoic acid and docosahexaenoic acid, were associated with lower rates of CVD and death.55, 56 In the Nurses' Health Study, 2 or more servings of fish per week were associated with 30% lower risk for CHD in women.57 Therefore, omega-3 fatty acids can be recommended to replace saturated fat.
In recent observational studies, mild to moderate coffee consumption, or about 3 to 4 cups per day, was associated with a reduction in all-cause mortality, decreased cancer risk, and a dose-dependent inverse relationship with risk for developing type 2 diabetes mellitus.58, 59 Observational studies are subject to confounding, and other factors associated with a healthy lifestyle may account for benefit. Addition of sugar and cream to coffee should be limited because these may significantly increase calorie consumption.
There appears to be a U-shaped association between alcohol intake and CVD risk, with those who consume 1 to 2 drinks (1 “drink” is equivalent to 12 ounces of beer, 5 ounces of wine, or 1.5 ounces of distilled spirits) per day appearing to be at lowest risk, and those with excessive intake, at higher risk.60 Alcohol has additionally been associated with an increased risk for cancer, even when consumed at low levels.61, 62 The AHA currently recommends that adults who drink alcohol should limit daily consumption to 1 to 2 drinks for men and 1 drink for women.63 However, recent research has demonstrated that risk for all-cause mortality and cancer increases with increasing levels of alcohol consumption, and that optimal alcohol consumption to maximize health may be zero.64 Current evidence for cardiovascular benefit is not high enough quality to recommend initiation of alcohol consumption in those who currently abstain.
Commonly Encountered Diets and Their Effects on Weight and Cardiovascular Outcomes
A number of diets have been popularized primarily for weight loss but have unclear or neutral effects on cardiovascular health.66 Clinicians should focus on diets with the highest level of evidence to support cardiovascular benefit. Different dietary patterns including the Mediterranean and DASH diets have been linked to decreased risk of mortality from CHD and CVD, as well as decreased total mortality.67, 68 The underlying mechanism has been explored from various perspectives, including individual food components, psychosocial health, and pathophysiologic pathways such as inflammation, oxidative stress, hypertension, and autonomic and endothelial dysfunction. A diet rich in healthful plant foods and fish is associated with low risk for CVD.69, 70 Major diets supported by national guidelines include the DASH diet, the Mediterranean diet, and the plant-based diet (Table 2). Although less evidence based, clinicians should additionally be aware of the risks and benefits of popular diets such as the low-carbohydrate high-protein/fat (LCHF) diet, discussed further later.
Table 2.
Summary of US Dietary Food Guideline Recommendations by Major Societies
| Comorbidity Addressed | Society Guideline | Diets Recommended | Dietary Interventions |
|---|---|---|---|
| Hyperlipidemia | 2018 AHA/ACC Multi-Society Guideline on the Management of Blood Cholesterol | Mediterranean diet, DASH diet | - Increase intake of vegetables, fruits, whole grains, legumes, fish, seafood, nuts, and nontropical vegetable oils - Limit intake of salt, sweets, sugar-sweetened beverages, and red meats - Dietary patterns should be adjusted to appropriate calorie requirements and nutritional therapy for specific medical conditions (ie, diabetes, hypertension) |
| Hypertension | 2017 ACC/AHA Multi-Society Guideline for High Blood Pressure in Adults | DASH diet | - Weight loss is recommended to reduce BP in adults with hypertension who are obese or overweight - Increase intake of dietary potassium, aim for 3.5-5 g/d - Sodium: optimal goal is <1.5 g/d, but aim for at least a 1-g/d reduction in most adults - Limit alcohol consumption (≤1 drink/d for women and ≤2 drinks/d for men) |
| Diabetes mellitus | 2018 ADA Standards of Medical Care in Diabetes: Lifestyle Management | Mediterranean style diet, DASH, and plant-based diet | - A medical nutrition treatment plan is recommended for diabetic patients, emphasizing portion control and healthy food choices - Weight loss >5% is recommended for obese or overweight adults with type 2 diabetes and prediabetes - Carbohydrate preferred sources are vegetables, fruits, legumes, whole grains, and dairy products - Avoid sugar-sweetened beverages - Emphasize foods higher in fiber and lower glycemic load - Eat foods rich in long-chain n-3 FA, such as fatty fish, nuts, and seeds - Limit alcohol consumption (≤1 drink/d for women and ≤2 drinks/d for men) - Limit sodium intake to <2.3 g/d |
| Obesity | 2016 AACE/ACE Obesity Guidelines | Mediterranean diet, DASH diet, low-carbohydrate diet, low-fat diet, volumetric diet, high-protein diet, and vegetarian diet | - Weight loss goal of 5%-15% for CV indications - Recommend calorie deficit of 500-750 daily - Reduced-calorie healthy meal plan that minimizes sugars and refined carbohydrates, avoids trans-fats, limits alcohol use, and emphasizes fiber |
| General diet | 2015-2020 USDA Dietary Guidelines for Americans | Moderate consumption of a wide variety of protein foods (seafood, lean meats, poultry, eggs, legumes, soy), fat-free or low-fat dairy, and olive/canola oils | - High consumption of vegetables (dark green, red and orange, legumes), fruits, grains (at least half of which are whole grains) - Moderate consumption of consider a wide variety of protein foods (seafood, lean meats, poultry, eggs, legumes, soy), fat-free or low-fat dairy, and olive/canola oils in moderate amounts - Limited consumption of saturated fats (<10% of daily calories), trans-fats, added sugars (<10% of daily calories), sodium (<2.3 g/d), and alcohol (≤1 drink/d for women and ≤2 drinks/d for men) |
| General Diet and CV Prevention | 2016 ESC Guidelines on CV disease prevention | Mediterranean diet, DASH diet | - ≥200 g of vegetables per day (2-3 servings) - ≥200 g of fruit per day (2-3 servings) - 30-45 g/d of fiber, preferably whole grain - 30 g/d of unsalted nuts - Fish 1-2 times/wk - Saturated fats <10% of total energy intake and as little as possible trans unsaturated FA - Alcohol ≤20 g/d for men, ≤10 g/d for women - Avoid sugar-sweetened beverages - <5 g/d of salt |
AACE, American Association of Clinical Endocrinologists; ACC, American College of Cardiology; ACE, American College of Endocrinology; ADA, American Diabetes Association; AHA, American Heart Association; BP, blood pressure; CV, cardiovascular; DASH, Dietary Approaches to Stop Hypertension; ESC, European Society of Cardiology; FA, fatty acid; USDA, United States Department of Agriculture.
The Mediterranean and DASH diets have been linked to lower risk for mortality from CHD, CVD, and all causes.67, 68 The DASH diet was promoted originally by the US National Heart, Lung, and Blood Institute as a strategy to control hypertension and was later recommended by the AHA and USDA as an ideal eating plan for all Americans.9, 49 The OmniHeart RCT demonstrated that the DASH diet lowers blood pressure, LDL-C levels, and overall cardiovascular risk.71 The standard DASH diet permits up to 2300 mg of sodium daily, with the 1500-mg sodium daily DASH variant associated with an even greater reduction in blood pressure.72
The Mediterranean diet is based on food consumption patterns originally described in Southern Italy and Greece, highlighted by: 1) high leafy green vegetable intake, fruits, whole grains, nuts, legumes, and extra virgin olive oil; 2) moderate intake of fish, lean meats, low-fat dairy, and poultry; 3) low intake of red meat and sweets; and 4) wine in moderation. It differs from the USDA Healthy Eating Guidelines and DASH diet in that there is less emphasis placed on dairy consumption and more emphasis on seafood, fruits, and vegetables. Adhering to the Mediterranean diet is strongly recommended because it has been shown to lower both CHD and all-cause mortality.67, 68
The Prevention With Mediterranean Diet study was the first large RCT to show that a Mediterranean diet is able to reduce clinical events in primary cardiovascular prevention.73 Conducted in Spain from 2003 to 2011, a total of 7447 men and women at high CVD risk were randomly assigned into 1 of 3 diets: 1) Mediterranean diet supplemented with extra virgin olive oil, 2) Mediterranean diet supplemented with nuts, or 3) control diet (advice to follow a low-fat diet). Those randomly assigned to a Mediterranean diet with either extra virgin olive oil or nuts had multivariable-adjusted hazard ratios of 0.70 (95% CI, 0.54-0.92) and 0.72 (95% CI, 0.54-0.96), respectively, for the primary end point of MI, stroke, or death from cardiovascular causes when compared with a low-fat diet. These event reductions are comparable to those of statin drugs. Of note, the original Prevention With Mediterranean Diet study was withdrawn due to methodologic concerns but was republished after these corrections with the same conclusions.
In the Lyon Diet Heart Study, individuals post-MI randomly assigned to a Mediterranean diet had a 72% reduction in cardiac death and nonfatal MI and 56% reduction in total mortality at the 4-year follow-up compared with those randomly assigned to an AHA Step I diet with total fat comprising less than 30% of the diet.68 The Mediterranean diet was further shown to be beneficial in the arena of secondary prevention in the Stabilization of Atherosclerotic Plaque by Initiation of Darapladib Therapy trial, which showed significant reduction in major adverse cardiovascular events in patients with high-risk stable coronary artery disease.74
The vegetarian diet, one of the 3 major dietary strategies supported in the 2015 to 2020 Healthy Eating guidelines, substitutes meat, seafood, and poultry with the consumption of soy products, legumes, nuts, and whole grains. The vegetarian diet is associated with a large range of health benefits, including reduced body mass index (calculated as the weight in kilograms divided by the height in meters squared), non–high-density lipoprotein cholesterol (HDL-C) level, and SBP in addition to lower risk for CVD.75, 76 The vegan diet is a vegetarian diet that eliminates all animal-derived products, including eggs, dairy, gelatin, and whey. The vegan diet has been linked with a weight loss benefit in addition to reduced risk for heart disease, type 2 diabetes mellitus, and death.77 However, vitamin B12 and D supplementation are required due to increased risk for deficiency.78 Plant-based diets are recommended when they follow similar patterns as described in the DASH and Mediterranean diets. High intake of plant-based diet index rich in healthier plant foods (ie, whole grains, fruits/vegetables, nuts/legumes, and olive/canola oil) are associated with substantially lower CHD risk as compared with plant-based diets that emphasize less-healthy plant foods (refined grains, SSBs, potatoes/fries, and sweets).52
LCHF diets such as the ketogenic, Atkins, and paleo diets are currently an area of interest in popular culture, nutrition science, and clinical practice. LCHF diets typically restrict carbohydrate intake to 50 to 150 g daily, with less than 50 g daily recommended for the ketogenic diet. LCHF diets are associated with improved weight loss and increased insulin sensitivity but an increase in LDL-C levels.79, 80 Some studies have suggested that the Atkins style diet was as effective as the Mediterranean diet for weight loss81; both diets were superior to a low-fat diet.82 A meta-analysis of the very low-carbohydrate ketogenic diets demonstrated greater weight loss than a low-fat diet, with an increase in LDL-C and HDL-C levels, though the quality of studies included was limited.83
Dietary patterns focusing on low intake of carbohydrates at the expense of high intake of animal fat and protein may be associated with increased all-cause mortality when used for extended periods.67 Currently there is insufficient evidence for clinicians to recommend LCHF diets to improve cardiovascular health, but in individuals who choose to pursue an LCHF diet, high leafy green vegetable and increased plant-based protein consumption should be encouraged.
On review of the evidence, the 2013 AHA/American College of Cardiology (ACC) guidelines on lifestyle management endorse a dietary pattern that emphasizes intake of vegetables, fruits, whole grains, legumes, healthy protein sources (low-fat dairy products, low-fat poultry without skin, fish/seafood, and nuts), and nontropical vegetable oils. They limit intake of sweets, SSBs, and red meats in addition to recommending regular activity for primary and secondary cardiovascular prevention.34, 49 The 2018 AHA/ACC multisociety cholesterol guidelines support the evidence-based recommendations provided in the 2013 AHA/ACC guidelines on lifestyle management.34
Weight Loss and Prevention of Obesity and Metabolic Syndrome
Overweight and obesity epidemics are a major target of primordial, primary, and secondary cardiovascular prevention, affecting nearly three-fourths of adults in the United States.84 A normal weight is defined by body mass index of 18.5 to 24.9 kg/m2, although several other measures may be important markers of cardiometabolic risk, including body composition, adiposity, waist circumference, waist to hip ratio, and lean muscle mass.85 Excess caloric intake and poor diet quality are the strongest drivers of obesity, along with an increase in the proportion of individuals who lead a sedentary lifestyle.33
Among available strategies for weight reduction, the most important dietary intervention is portion control and restriction of caloric intake because total negative energy balance is fundamental to weight loss. A variety of tools exist for patients to calculate their basal metabolic energy requirements, and in combination with extra energy burned through exercise, patients can calculate daily caloric limits. Use of a food diary or smart phone applications may be helpful for some to quantify caloric intake and nutritional patterns.86
The quality of food intake in addition to quantity has a meaningful effect on weight loss. One RCT showed that lowering dietary carbohydrate intake over 20 weeks increased energy expenditure during weight loss maintenance by 91 and 209 kcal/d in those with a moderate-carbohydrate diet and low-carbohydrate diet, respectively, as compared with a high-carbohydrate diet. Additional benefit was seen in those with the highest baseline insulin secretion.87 They observed decreased leptin and ghrelin hormone levels in the low-carbohydrate group, suggesting that carbohydrate consumption may affect neurohormonal regulation of basal metabolic expenditure. Generally, consumption of foods that are high in fiber and water content such as fruit, vegetables, and whole grains can help promote a healthy weight given their high satiety index and fiber/water content.88 Simultaneous limiting of “empty calorie” foods such as SSBs, candy, starchy vegetables (corn, peas, and white potatoes), and processed foods is essential to sustained weight loss.89
When considering a healthy diet, it is important to take into account cultural and SES factors because patients will benefit most if their diet is sustainable. The most well-studied dietary patterns for weight loss are the Mediterranean and DASH diets, which have been shown to be highly effective attainable long-term strategies.90 Although a healthy plant-based diet has demonstrated a weight loss benefit, it may be more difficult to sustain in the long term for many individuals.75, 77
Special Dietary Considerations for Hypertension, Hyperlipidemia, and Type 2 Diabetes Mellitus
In line with the 2017 AHA/ACC Hypertension Guidelines, lifestyle and nonpharmacologic interventions are pivotal to prevent and reduce SBP in those at risk for and diagnosed with systemic hypertension.91 Diets focused on reduced sodium intake have been shown to reduce blood pressure and cardiovascular events.92, 93 The DASH diet in combination with a 2-g sodium restriction is associated with an 11–mm Hg reduction in SBP in those with baseline SBP of 150 mm Hg or greater and a reduction by 4 mm Hg in those with baseline SBP of 130 mm Hg or less.72 Dietary potassium supplementation with potassium-rich fruits and vegetables have a blood pressure–lowering effect and should be considered in patients who are not at risk for hyperkalemia.94
A meta-analysis of 7 RCTs and 32 observational studies showed that vegetarian diets were associated with a reduction in SBP of 5 and 7 mm Hg, respectively.95 The majority of sodium consumption in the typical diet comes from sodium added before consumer purchase. In all patients, there should be an attempt to limit the “salty 6,” which are composed of cold cuts/cured meats, preseasoned poultry, sandwiches, bread, canned soup, and pizza.
Saturated fat and trans-fat intake have been shown to increase serum LDL-C levels and increase the risk for CHD.96 Substitution of saturated fat with whole grains (unrefined carbohydrate) is preferable to refined carbohydrates. Patients should substitute butter, margarine, coconut oil, and other oils that congeal at room temperature with extra virgin olive oil and canola oil. The latter have been shown in cohort studies and RCTs to reduce MI, stroke, and risk for cardiovascular death.73, 97, 98 Despite health claims purporting the benefit of coconut oil in popular media, the National Lipid Association has concluded that there is no evidence supporting the health benefits of coconut oil and furthermore acknowledges that its use must be limited in the heart-healthy diet due to its propensity to increase LDL-C and non–HDL-C levels.37
Butter has 51 g of saturated fat per 100 g. In contrast, canola and olive oil, which can be substituted for butter, have 7 g and 14 g of saturated fat, respectively. Applesauce, which has no saturated fat, can be substituted for butter in baking. By making these easy substitutions, saturated fat content can be lowered dramatically. Coconut oil has 87 g of saturated fat per 100 g and should be avoided.99
Patients can continue to eat their ethnic/native diets by making substitutions to lower saturated fat content and also eating smaller portion sizes. For example, some Middle Eastern dishes use either lamb or chicken, which have 9 g and 1 g of saturated fat, respectively, per 100 g. By preparing dishes with chicken rather than lamb, saturated fat content is reduced markedly. Finally, although several diets have been associated with reduction in serum LDL-C levels, recent AHA/ACC recommendations endorse the DASH and Mediterranean diets as the most evidence based for the treatment of primary and secondary cholesterol prevention.49
As with prevention of type 2 diabetes mellitus, dietary interventions to manage diabetes focus on minimizing the contribution of carbohydrate intake to total daily caloric consumption, as well as intake of foods with a low glycemic index. In patients with type 2 diabetes mellitus, the American Diabetes Association recommends moderate intake of carbohydrates (44%-46% of total calories), with a focus on carbohydrate intake from vegetables, legumes, fruits, low-fat dairy, and whole grains in conjunction with reduced refined and added sugar intake.30 Whole wheat products should be substituted for refined grains when possible. Brown rice has a higher fiber content than white rice and is less likely to increase triglyceride levels.
Quality of fat intake, as opposed to total fat intake, has a role in the development of type 2 diabetes mellitus. In the Nurses' Health Study, higher intake of polyunsaturated fatty acids was associated with a decreased incidence of type 2 diabetes mellitus, whereas greater trans-fat intake was associated with an increased incidence of type 2 diabetes mellitus.100 Eliminating the consumption of sugar and artificially sweetened beverages can also decrease the risk for developing type 2 diabetes mellitus because a single daily serving is associated with a 20% increased risk for developing diabetes.101
Dietary Counseling
A lifestyle interview is required before effective counseling can occur. More than 10 years ago, Eckel102 proposed a 15-question assessment for lifestyle interviews that could be accomplished in a 3-minute interview (Table 3). Another approach was advocated by Lehr et al,103 recommending that clinicians ask 9 questions to determine whether the ABCDs of “Assess, Barriers, Commit and Demonstrate” are useful in understanding opportunities for improved diet and activity. With widespread use of the electronic medical record, both sets of questions could be printed out and given to the patient to be filled in before the clinician visit.
Table 3.
Nutrition Questionnaire and Motivational Interviewing Discussion Points to Facilitate Effective Lifestyle Optimization102
| Lifestyle Interview Nutrition Questionnaire | Assessment | Are you interested in having a healthier lifestyle? |
|---|---|---|
| How many servings of fruits and vegetables do you eat per day? | Are you concerned about the effects your diet is having on your health? | |
| How many servings of whole grains do you eat per day? | On a scale of 1-10, how do you rate your diet from poor to optimal? | |
| How many servings of fish do you eat per week? | On a scale of 1-10, how confident are you in your ability to make a change to your diet? | |
| Do you eat desserts? If so, how often? | What does a typical day look like for you in terms of your eating? | |
| What are your favorite snack foods? | Is there anything you are hoping or have been trying to change about your eating? | |
| Do you eat because you're hungry? | Affirmation & Reflective Listening | I can tell that you have already started to think about making some changes. You are doing a great job with X, Y and Z. |
| Do you weigh the most now that you've ever weighed? | It sounds like you are working hard to eat more fruits and vegetables into your diet AND I'm hearing that you would really like to eat less fast food. | |
| Are you interested in losing weight? | Barriers | What do you believe are the barriers to making a change in your diet? |
| Commit | What would it take to change your diet before our next appointment? | |
| Demonstrate | How do you suggest we monitor your dietary progress? |
Reproduced with permission from [Preventive cardiology by lifestyle intervention: opportunity and/or challenge? 2006. 113(22): 2657-2661]. Copyright 2006. American Medical Association. All rights reserved.
Manson et al104 counseled more than 14 years ago that “counseling about weight and physical activity need not be time-consuming or intricate.”104(pp253) Coupled with improved knowledge about nutrition, we believe it is reasonable for clinicians to consider implementing one of these strategies into their clinical practice to facilitate dietary counseling. Given time constraints and the complexity of outpatient care, it may be reasonable to start with the goal of asking patients at least 1 question about nutrition and physical activity per visit. A focused approach using the lifestyle assessment and counseling tool (Supplemental Figure, available online at http://mcpiqojournal.org) incorporates many of the recommendations in this article and can be used to provide nutritional counseling for the patient within the limited time frame of an office visit.
Dietary Counseling in Low-Resource Settings
Worsening SES disparities have led to a widening gap in diet quality between the rich and poor communities from 1999 to 2010 in the United States, with improvements in diet driven by those of higher SES.105 Food insecurity, or lack of consistent access to enough food for an active and healthy lifestyle, may serve as a fundamental barrier to improvement in diet, leading to consumption of inexpensive foods that are low quality out of convenience or necessity.
Patients at low SES are more likely to live in areas with long distances to supermarkets and poor access to fresh foods (ie, “food deserts”) in addition to areas with an abundance of unhealthy processed and fast foods (ie, “food swamps”). Access to fruits and vegetables, core components of the healthy diet, are shown to differ by race and SES, disproportionately negatively affecting African American and low-SES communities.106 Time scarcity, such as in the scenario of single parents and working multiple jobs to support a family, has been shown to promote poor food choices in low-SES populations by promoting consumption of regular fast food or precooked processed meals, ultimately leading to caloric overconsumption and poor micronutrient intake.107
Providers should ask patients what is affordable and reasonable from a cost perspective when coaching regarding a healthy diet. Replacing SSBs with water can have a significant impact on both CVD risk factors and total caloric intake and has the potential to save patients money in the long term.12, 108 Frozen or canned fruits, vegetables, and legumes are inexpensive sources of protein and nutritious complex carbohydrates that have a long shelf life, an important factor for patients who live a far distance from or cannot shop at supermarkets frequently. As mentioned, it is important to counsel patients purchasing canned foods to select low-sodium options when possible.
Studies assessing nutrient properties in conjunction with food price analysis show that milk, yogurt, legumes, carrots, cabbage, and nonsweetened whole grain cereals/oatmeal offer high nutrient density at low cost, as do many low-sodium canned and frozen foods.109 Affordable nonstarchy frozen vegetables such as cauliflower, rice, and zucchini spirals may be used as a substitute for starchy foods such as rice, pasta, and white potatoes. The impact of healthy food choices pays dividends because food choices tend to be shared among family members and may affect children at an important time in their development.110
Conclusion
With the current obesity epidemic contributing to the slowed rate of improvement in CVD morbidity and mortality, dietary counseling has become increasingly important to improve overall cardiovascular outcomes. There is no “1-size-fits-all” diet, and clinicians should incorporate a shared decision-making strategy to find healthy and sustainable alternatives to which patients will adhere. The DASH diet, Mediterranean diet, and vegetarian diet are the most evidence based with regard to CVD prevention and weight loss. Clinicians should implement a team-based approach to dietary intervention, using nurses and dieticians to help supplement education and reinforce dietary habits. In patients with low SES or cultural barriers to incorporating a healthy diet, particular attention should be sought to determine which dietary changes are most economically and logistically feasible.
Footnotes
Potential Competing Interests: Ms Davis reports legal consulting for Vera Juris. The other authors report no competing interests.
Supplemental Online Material
Supplemental material can be found online at http://mcpiqojournal.org. Supplemental material attached to journal articles has not been edited, and the authors take responsibility for the accuracy of all data.
References
- 1.Sidney S., Quesenberry C.P., Jaffe M.G., et al. Recent trends in cardiovascular mortality in the United States and public health goals. JAMA Cardiol. 2016;1(5):594–599. doi: 10.1001/jamacardio.2016.1326. [DOI] [PubMed] [Google Scholar]
- 2.Jones D.S., Greene J.A. The decline and rise of coronary heart disease: understanding public health catastrophism. Am J Public Health. 2013;103(7):1207–1218. doi: 10.2105/AJPH.2013.301226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murray C.J.L., Atkinson C., Bhalla K., et al. U.S. Burden of Disease Collaborators The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cawley J., Meyerhoefer C. The medical care costs of obesity: an instrumental variables approach. J Health Econ. 2012;31(1):219–230. doi: 10.1016/j.jhealeco.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Wang T., Heianza Y., Sun D., et al. Improving adherence to healthy dietary patterns, genetic risk, and long term weight gain: gene-diet interaction analysis in two prospective cohort studies. BMJ. 2018;360:j5644. doi: 10.1136/bmj.j5644. [erratum in: Improving adherence to healthy dietary patterns, genetic risk, and long term weight gain: gene-diet interaction analysis in two prospective cohort studies. BMJ. 2018] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adams K.M., Butsch W.S., Kohlmeier M. The state of nutrition education at US medical schools. J Biomed Educ. 2015:357627. https://www.hindawi.com/journals/jbe/2015/357627/ [Google Scholar]
- 7.Devries S., Freeman A.M. Nutrition education for cardiologists: the time has come. Curr Cardiol Rep. 2017;19(9):77. doi: 10.1007/s11886-017-0890-6. [DOI] [PubMed] [Google Scholar]
- 8.ACGME ACGME program requirements for graduate medical education in endocrinology, diabetes, and metabolism (internal medicine) July 2016. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/143_endocrinology_diab_metab_2016.pdf Accessed February 17, 2019.
- 9.U.S. Department of Health and Human Services and the U.S. Department of Agriculture Dietary Guidelines for Americans 2015-2020. 8th ed. https://health.gov/dietaryguidelines/2015/guidelines/
- 10.Li Y., Hruby A., Bernstein A.M., et al. Saturated fats compared with unsaturated fats and sources of carbohydrates in relation to risk of coronary heart disease: a prospective cohort study. J Am Coll Cardiol. 2015;66(14):1538–1548. doi: 10.1016/j.jacc.2015.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Te Morenga L.A., Howatson A.J., Jones R.M., Mann J. Dietary sugars and cardiometabolic risk: systematic review and meta-analyses of randomized controlled trials of the effects on blood pressure and lipids. Am J Clin Nutr. 2014;100(1):65–79. doi: 10.3945/ajcn.113.081521. [DOI] [PubMed] [Google Scholar]
- 12.Malik V.S., Hu F.B. Fructose and cardiometabolic health: what the evidence from sugar-sweetened beverages tells us. J Am Coll Cardiol. 2015;66(14):1615–1624. doi: 10.1016/j.jacc.2015.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stanhope K.L., Bremer A.A., Medici V., et al. Consumption of fructose and high fructose corn syrup increase postprandial triglycerides, LDL-cholesterol, and apolipoprotein-B in young men and women. J Clin Endocrinol Metab. 2011;96(10):E1596–E1605. doi: 10.1210/jc.2011-1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nettleton J.A., Lutsey P.L., Wang Y., Lima J.A., Michos E.D., Jacobs D.R. Diet soda intake and risk of incident metabolic syndrome and type 2 diabetes in the Multi-Ethnic Study of Atherosclerosis (MESA) Diabetes Care. 2009;32(4):688–694. doi: 10.2337/dc08-1799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johnson R.K., Lichtenstein A.H., Anderson C.A.M., et al. American Heart Association Nutrition Committee of the Council on Lifestyle and Cardiometabolic Health. Council on Cardiovascular and Stroke Nursing. Council on Clinical Cardiology. Council on Quality of Care and Outcomes Research; and Stroke Council Low-calorie sweetened beverages and cardiometabolic health: a science advisory from the American Heart Association. Circulation. 2018;138(9):e126–e140. doi: 10.1161/CIR.0000000000000569. [DOI] [PubMed] [Google Scholar]
- 16.Okarter N., Liu R.H. Health benefits of whole grain phytochemicals. Crit Rev Food Sci Nutr. 2010;50(3):193–208. doi: 10.1080/10408390802248734. [DOI] [PubMed] [Google Scholar]
- 17.Aune D., Keum N., Giovannucci E., et al. Whole grain consumption and risk of cardiovascular disease, cancer, and all cause and cause specific mortality: systematic review and dose-response meta-analysis of prospective studies. BMJ. 2016;353:i2716. doi: 10.1136/bmj.i2716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim S.J., de Souza R.J., Choo V.L., et al. Effects of dietary pulse consumption on body weight: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr. 2016;103(5):1213–1223. doi: 10.3945/ajcn.115.124677. [DOI] [PubMed] [Google Scholar]
- 19.Bao Y., Han J., Hu F.B., et al. Association of nut consumption with total and cause-specific mortality. N Engl J Med. 2013;369(21):2001–2011. doi: 10.1056/NEJMoa1307352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Slavin J.L., Lloyd B. Health benefits of fruits and vegetables. Adv Nutr. 2012;3(4):506–516. doi: 10.3945/an.112.002154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bondonno C.P., Liu A.H., Croft K.D., et al. Short-term effects of a high nitrate diet on nitrate metabolism in healthy individuals. Nutrients. 2015;7(3):1906–1915. doi: 10.3390/nu7031906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hozawa A., Jacobs D.R., Steffes M.W., Gross M.D., Steffen L.M., Lee D.-H. Circulating carotenoid concentrations and incident hypertension: the Coronary Artery Risk Development in Young Adults (CARDIA) study. J Hypertens. 2009;27(2):237–242. doi: 10.1097/HJH.0b013e32832258c9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li M., Fan Y., Zhang X., Hou W., Tang Z. Fruit and vegetable intake and risk of type 2 diabetes mellitus: meta-analysis of prospective cohort studies. BMJ Open. 2014;4(11):e005497. doi: 10.1136/bmjopen-2014-005497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gammone M.A., Riccioni G., D'Orazio N. Carotenoids: potential allies of cardiovascular health? Food Nutr Res. 2015;59:26762. doi: 10.3402/fnr.v59.26762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wedick N.M., Pan A., Cassidy A., et al. Dietary flavonoid intakes and risk of type 2 diabetes in US men and women. Am J Clin Nutr. 2012;95(4):925–933. doi: 10.3945/ajcn.111.028894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johnson S.A., Figueroa A., Navaei N., et al. Daily blueberry consumption improves blood pressure and arterial stiffness in postmenopausal women with pre- and stage 1-hypertension: a randomized, double-blind, placebo-controlled clinical trial. J Acad Nutr Diet. 2015;115(3):369–377. doi: 10.1016/j.jand.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 27.Muraki I., Imamura F., Manson J.E., et al. Fruit consumption and risk of type 2 diabetes: results from three prospective longitudinal cohort studies. BMJ. 2013;347:f5001. doi: 10.1136/bmj.f5001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.George T.W., Waroonphan S., Niwat C., Gordon M.H., Lovegrove J.A. Effects of acute consumption of a fruit and vegetable purée-based drink on vasodilation and oxidative status. Br J Nutr. 2013;109(8):1442–1452. doi: 10.1017/S0007114512003315. [DOI] [PubMed] [Google Scholar]
- 29.Fan J., Song Y., Wang Y., Hui R., Zhang W. Dietary glycemic index, glycemic load, and risk of coronary heart disease, stroke, and stroke mortality: a systematic review with meta-analysis. PLoS One. 2012;7(12):e52182. doi: 10.1371/journal.pone.0052182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.American Diabetes Association 4. Lifestyle Management: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018;41(suppl 1):S38–S50. doi: 10.2337/dc18-S004. [DOI] [PubMed] [Google Scholar]
- 31.Sacks F.M., Carey V.J., Anderson C.A.M., et al. Effects of high vs low glycemic index of dietary carbohydrate on cardiovascular disease risk factors and insulin sensitivity: the OmniCarb randomized clinical trial. JAMA. 2014;312(23):2531–2541. doi: 10.1001/jama.2014.16658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reynolds A., Mann J., Cummings J., Winter N., Mete E., Te Morenga L. Carbohydrate quality and human health: a series of systematic reviews and meta-analyses. Lancet. 2019;393(10170):434–445. doi: 10.1016/S0140-6736(18)31809-9. [erratum in Department of Error. Lancet. 2019] [DOI] [PubMed] [Google Scholar]
- 33.Mozaffarian D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review. Circulation. 2016;133(2):187–225. doi: 10.1161/CIRCULATIONAHA.115.018585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eckel R.H., Jakicic J.M., Ard J.D., et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 suppl 2):S76–S99. doi: 10.1161/01.cir.0000437740.48606.d1. [DOI] [PubMed] [Google Scholar]
- 35.Kris-Etherton P.M., Griel A.E., Psota T.L., Gebauer S.K., Zhang J., Etherton T.D. Dietary stearic acid and risk of cardiovascular disease: intake, sources, digestion, and absorption. Lipids. 2005;40(12):1193–1200. doi: 10.1007/s11745-005-1485-y. [DOI] [PubMed] [Google Scholar]
- 36.Hunter J.E., Zhang J., Kris-Etherton P.M. Cardiovascular disease risk of dietary stearic acid compared with trans, other saturated, and unsaturated fatty acids: a systematic review. Am J Clin Nutr. 2010;91(1):46–63. doi: 10.3945/ajcn.2009.27661. [DOI] [PubMed] [Google Scholar]
- 37.Jacobson T.A., Maki K.C., Orringer C.E., et al. NLA Expert Panel National Lipid Association recommendations for patient-centered management of dyslipidemia: part 2. J Clin Lipidol. 2015;9(6 Suppl):S1–122.e1. doi: 10.1016/j.jacl.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 38.Obarzanek E., Sacks F.M., Vollmer W.M., et al. DASH Research Group Effects on blood lipids of a blood pressure-lowering diet: the Dietary Approaches to Stop Hypertension (DASH) Trial. Am J Clin Nutr. 2001;74(1):80–89. doi: 10.1093/ajcn/74.1.80. [DOI] [PubMed] [Google Scholar]
- 39.Berglund L., Lefevre M., Ginsberg H.N., et al. DELTA Investigators Comparison of monounsaturated fat with carbohydrates as a replacement for saturated fat in subjects with a high metabolic risk profile: studies in the fasting and postprandial states. Am J Clin Nutr. 2007;86(6):1611–1620. doi: 10.1093/ajcn/86.5.1611. [DOI] [PubMed] [Google Scholar]
- 40.Buitrago-Lopez A., Sanderson J., Johnson L., et al. Chocolate consumption and cardiometabolic disorders: systematic review and meta-analysis. BMJ. 2011;343:d4488. doi: 10.1136/bmj.d4488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ried K., Sullivan T.R., Fakler P., Frank O.R., Stocks N.P. Effect of cocoa on blood pressure. Cochrane Database Syst Rev. 2012;8:CD008893. doi: 10.1002/14651858.CD008893.pub2. [DOI] [PubMed] [Google Scholar]
- 42.Ren Y., Liu Y., Sun X.-Z., et al. Chocolate consumption and risk of cardiovascular diseases: a meta-analysis of prospective studies. Heart. 2019;105(1):49–55. doi: 10.1136/heartjnl-2018-313131. [DOI] [PubMed] [Google Scholar]
- 43.Dehghan M., Mente A., Zhang X., et al. Prospective Urban Rural Epidemiology (PURE) study investigators Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet. 2017;390(10107):2050–2062. doi: 10.1016/S0140-6736(17)32252-3. [DOI] [PubMed] [Google Scholar]
- 44.Gianos E., Williams K.A., Freeman A.M., Kris-Etherton P., Aggarwal M. How pure is PURE? Dietary lessons learned and not learned from the PURE Trials. Am J Med. 2018;131(5):457–458. doi: 10.1016/j.amjmed.2017.11.024. [DOI] [PubMed] [Google Scholar]
- 45.Drouin-Chartier J.-P., Brassard D., Tessier-Grenier M., et al. Systematic review of the association between dairy product consumption and risk of cardiovascular-related clinical outcomes. Adv Nutr. 2016;7(6):1026–1040. doi: 10.3945/an.115.011403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dehghan M., Mente A., Rangarajan S., et al. Prospective Urban Rural Epidemiology (PURE) study investigators Association of dairy intake with cardiovascular disease and mortality in 21 countries from five continents (PURE): a prospective cohort study. Lancet. 2018;392(10161):2288–2297. doi: 10.1016/S0140-6736(18)31812-9. [DOI] [PubMed] [Google Scholar]
- 47.Drouin-Chartier J.-P., Côté J.A., Labonté M.-È., et al. Comprehensive review of the impact of dairy foods and dairy fat on cardiometabolic risk. Adv Nutr. 2016;7(6):1041–1051. doi: 10.3945/an.115.011619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.de Goede J., Geleijnse J.M., Ding E.L., Soedamah-Muthu S.S. Effect of cheese consumption on blood lipids: a systematic review and meta-analysis of randomized controlled trials. Nutr Rev. 2015;73(5):259–275. doi: 10.1093/nutrit/nuu060. [DOI] [PubMed] [Google Scholar]
- 49.Grundy S.M., Stone N.J., Bailey A.L., et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;73(24):3168–3209. doi: 10.1016/j.jacc.2018.11.002. [erratum in Correction. J Am Coll Cardiol. 2019] [DOI] [PubMed] [Google Scholar]
- 50.Arnett D.K., Blumenthal R.S., Albert M.A., et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published online ahead of print March 17, 2019] https://doi.org/10.1016/j.jacc.2019.03.009 J Am Coll Cardiol. [DOI] [PMC free article] [PubMed]
- 51.Pan A., Sun Q., Bernstein A.M., et al. Red meat consumption and mortality: results from 2 prospective cohort studies. Arch Intern Med. 2012;172(7):555–563. doi: 10.1001/archinternmed.2011.2287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bernstein A.M., Sun Q., Hu F.B., Stampfer M.J., Manson J.E., Willett W.C. Major dietary protein sources and risk of coronary heart disease in women. Circulation. 2010;122(9):876–883. doi: 10.1161/CIRCULATIONAHA.109.915165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.O'Keefe J.H., Harris W.S. From Inuit to implementation: omega-3 fatty acids come of age. Mayo Clin Proc. 2000;75(6):607–614. doi: 10.4065/75.6.607. [DOI] [PubMed] [Google Scholar]
- 54.Burr M.L., Fehily A.M., Gilbert J.F., et al. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: Diet and Reinfarction Trial (DART) Lancet. 1989;2(8666):757–761. doi: 10.1016/s0140-6736(89)90828-3. [DOI] [PubMed] [Google Scholar]
- 55.de Oliveira Otto M.C., Wu J.H.Y., Baylin A., et al. Circulating and dietary omega-3 and omega-6 polyunsaturated fatty acids and incidence of CVD in the Multi-Ethnic Study of Atherosclerosis. J Am Heart Assoc. 2013;2(6):e000506. doi: 10.1161/JAHA.113.000506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mozaffarian D., Lemaitre R.N., King I.B., et al. Circulating long-chain ω-3 fatty acids and incidence of congestive heart failure in older adults: the Cardiovascular Health Study: a cohort study. Ann Intern Med. 2011;155(3):160–170. doi: 10.1059/0003-4819-155-3-201108020-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hu F.B., Bronner L., Willett W.C., et al. Fish and omega-3 fatty acid intake and risk of coronary heart disease in women. JAMA. 2002;287(14):1815–1821. doi: 10.1001/jama.287.14.1815. [DOI] [PubMed] [Google Scholar]
- 58.Poole R., Kennedy O.J., Roderick P., Fallowfield J.A., Hayes P.C., Parkes J. Coffee consumption and health: umbrella review of meta-analyses of multiple health outcomes. BMJ. 2017;359:j5024. doi: 10.1136/bmj.j5024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.van Dam R.M. Coffee and type 2 diabetes: from beans to beta-cells. Nutr Metab Cardiovasc Dis. 2006;16(1):69–77. doi: 10.1016/j.numecd.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 60.Mukamal K., Lazo M. Alcohol and cardiovascular disease. BMJ. 2017;356:j1340. doi: 10.1136/bmj.j1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bagnardi V., Blangiardo M., La Vecchia C., Corrao G. A meta-analysis of alcohol drinking and cancer risk. Br J Cancer. 2001;85(11):1700–1705. doi: 10.1054/bjoc.2001.2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bagnardi V., Rota M., Botteri E., et al. Light alcohol drinking and cancer: a meta-analysis. Ann Oncol. 2013;24(2):301–308. doi: 10.1093/annonc/mds337. [DOI] [PubMed] [Google Scholar]
- 63.American Heart Association Alcohol and heart health. http://www.heart.org/en/healthy-living/healthy-eating/eat-smart/nutrition-basics/alcohol-and-heart-health
- 64.GBD 2016 Alcohol Collaborators Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392(10152):1015–1035. doi: 10.1016/S0140-6736(18)31310-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.US Department of Agriculture. MyPlate Graphic Resources. https://www.choosemyplate.gov/myplate-graphic-resources. Accessed February 17, 2017.
- 66.Montesi L., El Ghoch M., Brodosi L., Calugi S., Marchesini G., Dalle Grave R. Long-term weight loss maintenance for obesity: a multidisciplinary approach. Diabetes Metab Syndr Obes. 2016;9:37–46. doi: 10.2147/DMSO.S89836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Trichopoulou A., Psaltopoulou T., Orfanos P., Hsieh C.-C., Trichopoulos D. Low-carbohydrate-high-protein diet and long-term survival in a general population cohort. Eur J Clin Nutr. 2007;61(5):575–581. doi: 10.1038/sj.ejcn.1602557. [DOI] [PubMed] [Google Scholar]
- 68.de Lorgeril M., Salen P., Martin J.L., Monjaud I., Delaye J., Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999;99(6):779–785. doi: 10.1161/01.cir.99.6.779. [DOI] [PubMed] [Google Scholar]
- 69.Satija A., Bhupathiraju S.N., Spiegelman D., et al. Healthful and unhealthful plant-based diets and the risk of coronary heart disease in U.S. adults. J Am Coll Cardiol. 2017;70(4):411–422. doi: 10.1016/j.jacc.2017.05.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hengeveld L.M., Praagman J., Beulens J.W.J., Brouwer I.A., van der Schouw Y.T., Sluijs I. Fish consumption and risk of stroke, coronary heart disease, and cardiovascular mortality in a Dutch population with low fish intake. Eur J Clin Nutr. 2018;72(7):942–950. doi: 10.1038/s41430-018-0190-2. [DOI] [PubMed] [Google Scholar]
- 71.Appel L.J., Sacks F.M., Carey V.J., et al. OmniHeart Collaborative Research Group Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA. 2005;294(19):2455–2464. doi: 10.1001/jama.294.19.2455. [DOI] [PubMed] [Google Scholar]
- 72.Juraschek S.P., Miller E.R., 3rd, Weaver C.M., Appel L.J. Effects of sodium reduction and the DASH diet in relation to baseline blood pressure. J Am Coll Cardiol. 2017;70(23):2841–2848. doi: 10.1016/j.jacc.2017.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Estruch R., Ros E., Salas-Salvadó J., et al. PREDIMED Study Investigators Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med. 2018;378(25):e34. doi: 10.1056/NEJMoa1800389. [DOI] [PubMed] [Google Scholar]
- 74.Stewart R.A.H., Wallentin L., Benatar J., et al. STABILITY Investigators Dietary patterns and the risk of major adverse cardiovascular events in a global study of high-risk patients with stable coronary heart disease. Eur Heart J. 2016;37(25):1993–2001. doi: 10.1093/eurheartj/ehw125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Crowe F.L., Appleby P.N., Travis R.C., Key T.J. Risk of hospitalization or death from ischemic heart disease among British vegetarians and nonvegetarians: results from the EPIC-Oxford cohort study. Am J Clin Nutr. 2013;97(3):597–603. doi: 10.3945/ajcn.112.044073. [DOI] [PubMed] [Google Scholar]
- 76.Kwok C.S., Umar S., Myint P.K., Mamas M.A., Loke Y.K. Vegetarian diet, Seventh Day Adventists and risk of cardiovascular mortality: a systematic review and meta-analysis. Int J Cardiol. 2014;176(3):680–686. doi: 10.1016/j.ijcard.2014.07.080. [DOI] [PubMed] [Google Scholar]
- 77.Barnard N.D., Cohen J., Jenkins D.J., et al. A low-fat vegan diet improves glycemic control and cardiovascular risk factors in a randomized clinical trial in individuals with type 2 diabetes. Diabetes Care. 2006;29(8):1777–1783. doi: 10.2337/dc06-0606. [DOI] [PubMed] [Google Scholar]
- 78.Craig W.J., Mangels A.R., American Dietetic Association Position of the American Dietetic Association: vegetarian diets. J Am Diet Assoc. 2009;109(7):1266–1282. doi: 10.1016/j.jada.2009.05.027. [DOI] [PubMed] [Google Scholar]
- 79.Brouns F. Overweight and diabetes prevention: is a low-carbohydrate–high-fat diet recommendable? Eur J Nutr. 2018;57(4):1301–1312. doi: 10.1007/s00394-018-1636-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mansoor N., Vinknes K.J., Veierød M.B., Retterstøl K. Effects of low-carbohydrate diets v. low-fat diets on body weight and cardiovascular risk factors: a meta-analysis of randomised controlled trials. Br J Nutr. 2016;115(3):466–479. doi: 10.1017/S0007114515004699. [DOI] [PubMed] [Google Scholar]
- 81.Shai I., Schwarzfuchs D., Henkin Y., et al. Dietary Intervention Randomized Controlled Trial (DIRECT) Group Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med. 2008;359(3):229–241. doi: 10.1056/NEJMoa0708681. [DOI] [PubMed] [Google Scholar]
- 82.Naude C.E., Schoonees A., Senekal M., Young T., Garner P., Volmink J. Low carbohydrate versus isoenergetic balanced diets for reducing weight and cardiovascular risk: a systematic review and meta-analysis. PLoS One. 2014;9(7):e100652. doi: 10.1371/journal.pone.0100652. [erratum in Correction: Low carbohydrate versus isoenergetic balanced diets for reducing weight and cardiovascular risk: a systematic review and meta-analysis. PLoS One. 2018] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bueno N.B., de Melo I.S.V., de Oliveira S.L., da Rocha Ataide T. Very-low-carbohydrate ketogenic diet v. low-fat diet for long-term weight loss: a meta-analysis of randomised controlled trials. Br J Nutr. 2013;110(7):1178–1187. doi: 10.1017/S0007114513000548. [DOI] [PubMed] [Google Scholar]
- 84.Centers for Disease Control and Prevention National Center for Health Statistics. Obesity and Overweight. September 11, 2018. https://www.cdc.gov/nchs/fastats/obesity-overweight.htm
- 85.Huxley R., Mendis S., Zheleznyakov E., Reddy S., Chan J. Body mass index, waist circumference and waist:hip ratio as predictors of cardiovascular risk--a review of the literature. Eur J Clin Nutr. 2010;64(1):16–22. doi: 10.1038/ejcn.2009.68. [DOI] [PubMed] [Google Scholar]
- 86.Coughlin S.S., Whitehead M., Sheats J.Q., Mastromonico J., Hardy D., Smith S.A. Smartphone applications for promoting healthy diet and nutrition: a literature review. Jacobs J Food Nutr. 2015;2(3):021. [PMC free article] [PubMed] [Google Scholar]
- 87.Ebbeling C.B., Feldman H.A., Klein G.L., et al. Effects of a low carbohydrate diet on energy expenditure during weight loss maintenance: randomized trial. BMJ. 2018;363:k4583. doi: 10.1136/bmj.k4583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Rolls B.J. The relationship between dietary energy density and energy intake. Physiol Behav. 2009;97(5):609–615. doi: 10.1016/j.physbeh.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bertoia M.L., Mukamal K.J., Cahill L.E., et al. Changes in intake of fruits and vegetables and weight change in United States men and women followed for up to 24 years: analysis from three prospective cohort studies. PLoS Med. 2015;12(9):e1001878. doi: 10.1371/journal.pmed.1001878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.McGuire S. Scientific Report of the 2015 Dietary Guidelines Advisory Committee. Washington, DC: US Departments of Agriculture and Health and Human Services, 2015. Adv Nutr. 2016;7(1):202–204. doi: 10.3945/an.115.011684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Whelton P.K., Carey R.M., Aronow W.S., et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269–1324. doi: 10.1161/HYP.0000000000000066. [DOI] [PubMed] [Google Scholar]
- 92.Appel L.J., Moore T.J., Obarzanek E., et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336(16):1117–1124. doi: 10.1056/NEJM199704173361601. 1. [DOI] [PubMed] [Google Scholar]
- 93.Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure. The Trials of Hypertension Prevention, phase II. The Trials of Hypertension Prevention Collaborative Research Group. Arch Intern Med. 1997;157(6):657–667. [PubMed] [Google Scholar]
- 94.Whelton S.P., Blumenthal R.S. Beyond the headlines: insights on potassium supplementation for the treatment of hypertension from the CHEP Guidelines. Circulation. 2017;135(1):3–4. doi: 10.1161/CIRCULATIONAHA.116.024525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Yokoyama Y., Nishimura K., Barnard N.D., et al. Vegetarian diets and blood pressure: a meta-analysis. JAMA Intern Med. 2014;174(4):577–587. doi: 10.1001/jamainternmed.2013.14547. [DOI] [PubMed] [Google Scholar]
- 96.Woodside J.V., McKinley M.C., Young I.S. Saturated and trans fatty acids and coronary heart disease. Curr Atheroscler Rep. 2008;10(6):460–466. doi: 10.1007/s11883-008-0072-5. [DOI] [PubMed] [Google Scholar]
- 97.Mensink R.P., Zock P.L., Kester A.D.M., Katan M.B. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr. 2003;77(5):1146–1155. doi: 10.1093/ajcn/77.5.1146. [DOI] [PubMed] [Google Scholar]
- 98.Covas M.-I., Nyyssönen K., Poulsen H.E., et al. EUROLIVE Study Group The effect of polyphenols in olive oil on heart disease risk factors: a randomized trial. Ann Intern Med. 2006;145(5):333–341. doi: 10.7326/0003-4819-145-5-200609050-00006. [DOI] [PubMed] [Google Scholar]
- 99.Sacks F.M., Lichtenstein A.H., Wu J.H.Y., et al. American Heart Association Dietary fats and cardiovascular disease: a Presidential Advisory from the American Heart Association. Circulation. 2017;136(3):e1–e23. doi: 10.1161/CIR.0000000000000510. [DOI] [PubMed] [Google Scholar]
- 100.Salmerón J., Hu F.B., Manson J.E., et al. Dietary fat intake and risk of type 2 diabetes in women. Am J Clin Nutr. 2001;73(6):1019–1026. doi: 10.1093/ajcn/73.6.1019. [DOI] [PubMed] [Google Scholar]
- 101.Löfvenborg J.E., Andersson T., Carlsson P.-O., et al. Sweetened beverage intake and risk of latent autoimmune diabetes in adults (LADA) and type 2 diabetes. Eur J Endocrinol. 2016;175(6):605–614. doi: 10.1530/EJE-16-0376. [DOI] [PubMed] [Google Scholar]
- 102.Eckel R.H. Preventive cardiology by lifestyle intervention: opportunity and/or challenge? Presidential address at the 2005 American Heart Association Scientific Sessions. Circulation. 2006;113(22):2657–2661. doi: 10.1161/CIRCULATIONAHA.106.175744. [DOI] [PubMed] [Google Scholar]
- 103.Lehr A.L., Driver S.L., Stone N.J. The ABCDs of lifestyle counseling. JAMA Cardiol. 2016;1(5):505–506. doi: 10.1001/jamacardio.2016.1419. [DOI] [PubMed] [Google Scholar]
- 104.Manson J.E., Skerrett P.J., Greenland P., VanItallie T.B. The escalating pandemics of obesity and sedentary lifestyle. A call to action for clinicians. Arch Intern Med. 2004;164(3):249–258. doi: 10.1001/archinte.164.3.249. [DOI] [PubMed] [Google Scholar]
- 105.Wang D.D., Leung C.W., Li Y., et al. Trends in dietary quality among adults in the United States, 1999 through 2010. JAMA Intern Med. 2014;174(10):1587–1595. doi: 10.1001/jamainternmed.2014.3422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Zenk S.N., Schulz A.J., Israel B.A., James S.A., Bao S., Wilson M.L. Fruit and vegetable access differs by community racial composition and socioeconomic position in Detroit, Michigan. Ethn Dis. 2006;16(1):275–280. [PubMed] [Google Scholar]
- 107.Popkin B.M., Hawkes C. The sweetening of the global diet, particularly beverages: patterns, trends and policy responses for diabetes prevention. Lancet Diabetes Endocrinol. 2016;4(2):174–186. doi: 10.1016/S2213-8587(15)00419-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Xi B., Huang Y., Reilly K.H., et al. Sugar-sweetened beverages and risk of hypertension and CVD: a dose–response meta-analysis. Br J Nutr. 2015;113(5):709–717. doi: 10.1017/S0007114514004383. [DOI] [PubMed] [Google Scholar]
- 109.Darmon N., Drewnowski A. Editor's choice: contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev. 2015;73(10):643–660. doi: 10.1093/nutrit/nuv027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Pachucki M.A., Jacques P.F., Christakis N.A. Social network concordance in food choice among spouses, friends, and siblings. Am J Public Health. 2011;101(11):2170–2177. doi: 10.2105/AJPH.2011.300282. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.