Abstract
This study of Medicare-defined avoidable hospital stays for conditions such as urinary tract infection and complications of diabetes uses Medicare Fee-for-Service Inpatient and Outpatient Claim Files to investigate whether a decrease in inpatient admissions from 2011 to 2015 represented real gains in ambulatory care.
Hospitalizations related to ambulatory care–sensitive conditions (ACSCs) are widely considered a key measure of access to high-quality primary care.1 The Agency for Healthcare Research and Quality defines ACSCs as conditions, such as urinary tract infection and dehydration, for which hospitalization is generally avoidable if patients have access to effective primary care.2 In recent years, there has been substantial focus on improving ambulatory care nationally.3 Therefore, rates of hospital admissions related to ACSCs are used with increasing frequency to assess and incentivize the performance in the ambulatory setting of health care professionals participating in national Medicare alternative payment programs, such as accountable care organizations and alternative quality contracts administered by private payers, which increase pressure on hospitals to admit fewer patients.4 To date, there is some evidence that rates of avoidable hospitalizations have indeed been falling.2 However, during this same period, the rates of hospital admissions “for observation,” which do not count as inpatient admissions, have been increasing.5 The degree to which reported drops in avoidable hospitalizations related to ACSCs represent real gains in ambulatory care and not simply an artifact of an increasing shift from inpatient status to observation status is unknown.
Methods
We obtained a national 20% sample of the Medicare Fee-for-Service Inpatient and Outpatient Claim Files from 2011 to 2015 and used the Agency for Healthcare Research and Quality Prevention Quality Indicators software to identify avoidable hospitalizations and observation stays related to ACSCs.6 These included all hospital stays related to both acute conditions (dehydration, bacterial pneumonia, urinary tract infection, and perforated appendix) and chronic conditions (including diabetes short-term complications, diabetes long-term complications, uncontrolled diabetes, lower extremity amputation related to diabetes, asthma in adults, chronic obstructive pulmonary disease, hypertension, heart failure, and angina without procedure). The Harvard T. H. Chan School of Public Health institutional review board’s Committee on the Use of Human Subjects approved this study and waived the need for informed patient consent because all data were retrospective and deidentified. We used multivariable linear regression models to estimate yearly rates of avoidable hospitalizations and observation stays within each hospital referral region (HRR), the geographic territory representing each regional tertiary care market. The models included adjustments for patient age, sex, race, dual Medicare and Medicaid status, and comorbidities (using comorbidities data obtained from the Chronic Conditions Data Warehouse) and treated time as a categorical variable. We then estimated yearly slopes, similarly adjusting for patient demographics and comorbidities and using time as a continuous variable. Statistical analyses were performed from November 2018 to March 2019 using SAS software, version 9.4 (SAS Institute Inc). A 2-sided P < .05 was considered statistically significant.
Results
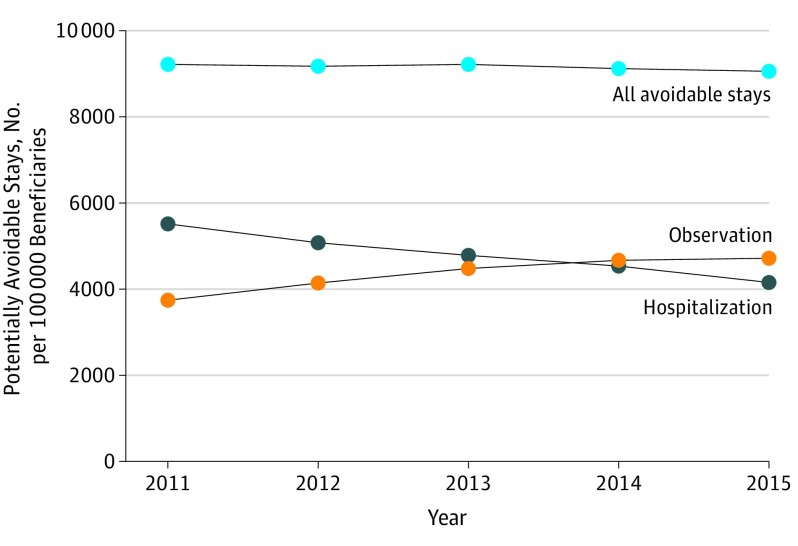
In 2011, there were 5517 ACSC-related, potentially avoidable inpatient hospitalizations and 3743 similarly avoidable observation stays per 100 000 Medicare beneficiaries (Figure). By 2015, the rate of potentially avoidable inpatient hospitalizations had decreased to 4158 and the rate of potentially avoidable hospital observation stays had increased to 4718 per 100 000 beneficiaries. The risk-adjusted slopes were −326.2 per 100 000 beneficiaries per year (95% CI, −332.8 to −319.7; P < .001) for avoidable inpatient hospitalizations and 245.6 per 100 000 beneficiaries per year (95% CI, 233.4 to 257.7; P < .001) for avoidable observation stays (Table). Approximately 75.2% of the decrease in national avoidable hospitalizations from 2011 to 2015 was offset by the increase in hospital stays under observation status. A greater shift from inpatient to observation stays was seen for chronic ACSCs than for acute ACSCs.
Figure. Trends in Potentially Avoidable Hospitalizations and Hospital Observation Stays Related to Ambulatory Care–Sensitive Conditions.
Multivariable linear regression models were used to estimate yearly hospitalization rates and observation stays while adjusting for patient demographics and comorbidities, treating time as a categorical variable, and including hospital referral region–fixed effects.
Table. Change in Rates of Hospitalization and Observation Stays Related to Overall, Acute, and Chronic ACSCsa.
| Admission Status by ACSC Category | Year | Yearly Change, Slope (95% CI) | P Value for Trend | |
|---|---|---|---|---|
| 2011 | 2015 | |||
| All ACSCs, No. per 100 000 Medicare beneficiaries | ||||
| Hospitalization | 5517 | 4158 | −326.2 (−332.8 to −319.7) | <.001 |
| Observation | 3743 | 4718 | 245.6 (233.4 to 257.7) | <.001 |
| Chronic ACSCs, No. per 100 000 Medicare beneficiariesb | ||||
| Hospitalization | 3055 | 2340 | −167.8 (−172.9 to −162.7) | <.001 |
| Observation | 2617 | 3350 | 188.6 (178.5 to 198.7) | .001 |
| Acute ACSCs, No. per 100 000 Medicare beneficiariesc | ||||
| Hospitalization | 2463 | 1819 | −158.4 (−162.4 to −154.4) | <.001 |
| Observation | 1126 | 1368 | 57.0 (51.7 to 62.3) | <.001 |
Abbreviation: ACSCs, ambulatory care–sensitive conditions.
Multivariable linear regression models were used to estimate yearly hospitalization rates and observation stays by using a 20% national sample of Medicare inpatient and outpatient data for 2011 to 2015 after adjusting for patient demographics and comorbidities, and treating time as a categorical variable. Yearly slopes were estimated by treating time as a continuous variable. All models included HRR fixed effects. The study baseline was 2011, and 2015 was the latest year for which relevant national data were available.
Chronic ACSCs included short-term and long-term complications of diabetes, uncontrolled diabetes, lower extremity amputation related to diabetes, asthma in adults, chronic obstructive pulmonary disease, hypertension, heart failure, and angina without procedure.
Acute ACSCs included dehydration, bacterial pneumonia, urinary tract infection, and perforated appendix.
Discussion
The rates of avoidable hospitalizations related to ACSCs have declined over time in the Medicare population. However, there has been a concomitant increase in the rates of avoidable observation stays for the same types of conditions, especially for chronic ACSCs. Our study results suggest that the major part of the improvement in hospitalization rates for ACSCs is likely related to increased designation of patients for observation status. Although the observational nature of this study limits our ability to establish a definitive causal relationship between these trends, the findings have important policy implications. First, they call into question how much progress is being made in improving ambulatory care, particularly for chronic conditions such as diabetes and heart failure. Second, they suggest that any alternative payment model that uses avoidable hospitalizations as a quality measure to assess performance in the primary care setting should also account for potentially avoidable observation stays.
References
- 1.Gao J, Moran E, Li YF, Almenoff PL. Predicting potentially avoidable hospitalizations. Med Care. 2014;52(2):164-171. doi: 10.1097/MLR.0000000000000041 [DOI] [PubMed] [Google Scholar]
- 2.Agency for Healthcare Research and Quality (AHRQ) Potentially avoidable hospitalizations. http://www.ahrq.gov/research/findings/nhqrdr/chartbooks/carecoordination/measure3.html. Published 2016. Accessed April 3, 2019.
- 3.Blumenthal D, Abrams M, Nuzum R. The Affordable Care Act at 5 years. N Engl J Med. 2015;373(16):1580. [DOI] [PubMed] [Google Scholar]
- 4.CMS Medicare Shared Savings Program Accountable Care Organization (ACO) 2018 Quality Measures: Narrative Specifications Document https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/2018-reporting-year-narrative-specifications.pdf. Published January 20, 2018. Accessed July 1, 2019.
- 5.Dharmarajan K, Qin L, Bierlein M, et al. . Outcomes after observation stays among older adult Medicare beneficiaries in the USA: retrospective cohort study. BMJ. 2017;357:j2616. doi: 10.1136/bmj.j2616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agency for Healthcare Research and Quality (AHRQ) QI modules. https://www.qualityindicators.ahrq.gov/Archive/default.aspx#. Accessed March 12, 2019.