Key Points
Question
Is the risk of wrong-patient orders increased among multiple-birth infants compared with singleton-birth infants in the neonatal intensive care unit?
Findings
In this cohort study of 1 536 160 orders placed for 10 819 infants in 6 neonatal intensive care units at 2 health care systems, the risk of wrong-patient orders was significantly higher among multiple-birth infants compared with singleton-birth infants. The excess risk among multiple-birth infants may have been owing to identification errors that occurred between siblings, with the greatest risk among sets of higher-order multiple-birth infants.
Meaning
Requirements for newborn identification may provide insufficient protection against wrong-patient errors among multiple-birth infants in neonatal intensive care units.
Abstract
Importance
Multiple-birth infants in neonatal intensive care units (NICUs) have nearly identical patient identifiers and may be at greater risk of wrong-patient order errors compared with singleton-birth infants.
Objectives
To assess the risk of wrong-patient orders among multiple-birth infants and singletons receiving care in the NICU and to examine the proportion of wrong-patient orders between multiple-birth infants and siblings (intrafamilial errors) and between multiple-birth infants and nonsiblings (extrafamilial errors).
Design, Setting, and Participants
A retrospective cohort study was conducted in 6 NICUs of 2 large, integrated health care systems in New York City that used distinct temporary names for newborns per the requirements of The Joint Commission. Data were collected from 4 NICUs at New York–Presbyterian Hospital from January 1, 2012, to December 31, 2015, and 2 NICUs at Montefiore Health System from July 1, 2013, to June 30, 2015. Data were analyzed from May 1, 2017, to December 31, 2017. All infants in the 6 NICUs for whom electronic orders were placed during the study periods were included.
Main Outcomes and Measures
Wrong-patient electronic orders were identified using the Wrong-Patient Retract-and-Reorder (RAR) Measure. This measure was used to detect RAR events, which are defined as 1 or more orders placed for a patient that are retracted (ie, canceled) by the same clinician within 10 minutes, then reordered by the same clinician for a different patient within the next 10 minutes.
Results
A total of 10 819 infants were included: 85.5% were singleton-birth infants and 14.5% were multiple-birth infants (male, 55.8%; female, 44.2%). The overall wrong-patient order rate was significantly higher among multiple-birth infants than among singleton-birth infants (66.0 vs 41.7 RAR events per 100 000 orders, respectively; adjusted odds ratio, 1.75; 95% CI, 1.39-2.20; P < .001). The rate of extrafamilial RAR events among multiple-birth infants (36.1 per 100 000 orders) was similar to that of singleton-birth infants (41.7 per 100 000 orders). The excess risk among multiple-birth infants (29.9 per 100 000 orders) appears to be owing to intrafamilial RAR events. The risk increased as the number of siblings receiving care in the NICU increased; a wrong-patient order error occurred in 1 in 7 sets of twin births and in 1 in 3 sets of higher-order multiple births.
Conclusions and Relevance
This study suggests that multiple-birth status in the NICU is associated with significantly increased risk of wrong-patient orders compared with singleton-birth status. This excess risk appears to be owing to misidentification between siblings. These results suggest that a distinct naming convention as required by The Joint Commission may provide insufficient protection against identification errors among multiple-birth infants. Strategies to reduce this risk include using given names at birth, changing from temporary to given names when available, and encouraging parents to select names for multiple births before they are born when acceptable to families.
This cohort study examines the risk of wrong-patient orders among multiple-birth vs singleton-birth infants receiving care in 6 neonatal intensive care units of 2 large, integrated health care systems in New York City.
Introduction
Each year, more than 135 000 twins, triplets, and higher-order multiples are born in the United States.1 Most of these multiple-birth infants are preterm and have low birth weight, making them more likely to require admission to a neonatal intensive care unit (NICU).1,2 Newborns receiving care in the NICU have a significantly higher risk of identification errors compared with patients receiving care in general pediatric units.3 An estimated 1 in 10 medical errors and 1 in 4 serious medication errors in the NICU are reported to be patient misidentification errors.4,5 One study conducted in Pennsylvania hospitals reported an average of 2 newborn identification errors each day over a 2-year period, or 1 error per 217 live births.6 These wrong-patient errors included ordering tests and medications, administering medications, feeding breast milk, and performing medical procedures on the wrong infant.
Several factors are associated with wrong-patient errors in the NICU. Newborns lack distinguishing physical characteristics, and medical apparatus in their isolettes often visually obscures their physical features, making differentiation difficult.6,7,8 An analysis by Gray et al7 estimated that, on any given day, approximately half of the infants receiving care in the NICU were at risk of wrong-patient errors owing to the similarity of their names and/or medical record numbers.7 A main factor associated with patient misidentification in the NICU is the use of temporary nondistinct names (eg, Babyboy or Babygirl) that are assigned to newborns at birth and retained throughout their hospital stay.3,9 A national survey conducted in 2013 noted that 82% of NICUs reported using nondistinct naming conventions for newborns, and only 15% of NICUs changed temporary names to given names during hospitalization based on concerns about the lack of systems interoperability.10
The use of a distinct newborn naming convention that incorporates the mother’s first name (eg, Wendysboy or Wendysgirl) has been associated with a 36% reduction in wrong-patient orders in the NICU compared with a nondistinct naming convention.9 Based on this finding, as of January 2019, The Joint Commission requires all hospitals to use distinct methods of newborn identification, such as naming conventions that incorporate the mother’s first name, as part of its National Patient Safety Goals (Box).11 However, the distinct naming convention examined in previous studies3,9 may not be as effective for multiple-birth infants as for singletons because siblings of multiple births have the same last name and nearly identical first names (eg, Wendysboy1 and Wendysboy2).7,9,10,12 Furthermore, in a national NICU survey, 20% of respondents reported that long names were visually truncated in the electronic health record, potentially removing the distinctive last character from the first names of multiple-birth infants and resulting in identical-looking names.10
Box. The Joint Commission 2019 Requirement for Newborn Identification.
Applicable to Hospitals and Critical Access Hospitals Effective January 1, 2019
National Patient Safety Goal NPSG.01.01.01
Use at least 2 patient identifiers when providing care, treatment, and services.
Element of Performance for NPSG.01.01.01
-
EP 3. Use distinct methods of identification for newborn patients. Examples of methods to prevent misidentification may include the following:
Distinct naming systems could include using the mother’s first and last names and the newborn’s sex (for example: “Smith, Judy Girl” or “Smith, Judy Girl A” and “Smith, Judy Girl B” for multiple-birth infants).a
Standardized practices for identification banding (eg, 2 body-site identification and bar coding).
Establish communication tools among staff (eg, visually alerting staff with signage noting newborns with similar names).
Although the use of distinct naming conventions has been associated with reductions in the risk of wrong-patient order errors in NICUs, it is unclear if multiple-birth infants remain at increased risk. To our knowledge, no studies have assessed the rate of wrong-patient order errors among multiple-birth infants compared with singleton-birth infants receiving care in the NICU. Furthermore, no studies to our knowledge have assessed the proportion of wrong-patient order errors that are intrafamilial (ie, between multiple-birth infants and siblings) and extrafamilial (ie, between multiple-birth infants and nonsiblings). Therefore, this multicenter study examined wrong-patient orders among multiple-birth infants compared with singleton-birth infants receiving care in NICUs that used distinct naming conventions, and it assessed the rates of intrafamilial and extrafamilial wrong-patient order errors. We hypothesized that multiple-birth infants would have a higher risk of wrong-patient order errors compared with singletons and that the excess risk associated with multiple-birth infants would be owing to intrafamilial identification errors between siblings.
Methods
Design and Setting
We conducted a retrospective cohort study in 6 NICUs of 2 large, integrated health care systems in New York City: 4 NICUs at New York–Presbyterian Hospital (site 1) from January 1, 2012, to December 31, 2015, and 2 NICUs at Montefiore Health System (site 2) from July 1, 2013, to June 30, 2015. Data were analyzed from May 1, 2017, to December 31, 2017. The 6 NICUs comprised a total of 156 beds: 3 were level 3 NICUs with 29 beds, and 3 were level 4 NICUs with 127 beds. The study sites used 2 different electronic health record systems: site 1 used Sunrise Clinical Manager (Allscripts Corp), and site 2 used Centricity EMR (GE Healthcare). The study was approved by the institutional review boards of the Columbia University Irving Medical Center and the Albert Einstein College of Medicine. A waiver of consent was granted by both institutions because the data were extracted retrospectively and deidentified for analysis.
Throughout the study periods, both study sites used distinct newborn naming conventions that incorporated the mother’s first name and the infant’s sex, as required by The Joint Commission.11,13 At site 1, the naming convention included the mother’s last name followed by MC (male child) or FC (female child) and the mother’s first name (eg, Jones, MC Wendy). At site 2, the naming convention included the mother’s last name followed by the mother’s first name, the letter “s,” and the infant’s sex (eg, Jones, Wendysboy). For multiple-birth infants, a letter was added after the infant’s sex at site 1 (eg, MC A Wendy and MC B Wendy), and a number was added before the infant’s name at site 2 (eg, 1Wendysboy and 2Wendysboy). At both institutions, additional safeguards were in place to reduce wrong-patient order entry errors in the electronic health record, such as patient verification alerts14 and a required field for reentry of patient identifiers.15 These interventions predated the current study and were used consistently for all patients.
Outcomes and Measures
The primary outcome was wrong-patient electronic orders that were identified using the Wrong-Patient Retract-and-Reorder (RAR) Measure, which is an automated, validated, and reliable measure for capturing near-miss wrong-patient orders.15 A wrong-patient order was defined as an order placed for patient A that was intended for patient B. By definition, a wrong-patient order error involves 2 patients: the 1 for whom the order was intended and the 1 for whom the order was placed in error. The Wrong-Patient RAR Measure uses an electronic query to detect RAR events, which are defined as 1 or more orders placed for a patient that are retracted (ie, canceled) by the same clinician within 10 minutes, then reordered by the same clinician for a different patient within the next 10 minutes. The measure is endorsed by the National Quality Forum16 and has been used to evaluate interventions to prevent wrong-patient orders in the NICU3,9 and other settings.14,15,17,18,19
This study compared the rate of RAR events between multiple-birth infants and singleton-birth infants receiving care in the NICU and assessed the proportion of RAR events that occurred between multiple-birth infants and siblings (intrafamilial errors) and between multiple-birth infants and nonsiblings (extrafamilial errors). Only infants with siblings receiving care in the NICU at the same time were classified as multiple-birth infants; infants born as a member of a set of multiple births with no siblings receiving care in the NICU were classified as singleton births for the purposes of this study. To determine whether an infant was a member of a set of multiple-birth infants with siblings receiving care in the NICU, we used a combination of codes from the International Classification of Diseases, version 9, for multiple births and matched infants based on their dates of birth, mother’s name, and home address. An RAR event was classified as intrafamilial if the error occurred between siblings of the same set of multiple-birth infants receiving care in the NICU at the same time and as extrafamilial if the error occurred between a multiple-birth infant and a nonsibling receiving care in the NICU.
Data Collection and Analysis
We extracted data retrospectively from the study sites’ electronic data warehouse for all orders placed in the 6 NICUs during the study periods, including orders for medications, laboratory tests, radiology and imaging tests, and medical procedures. To identify RAR events, we extracted data for each order, including the order description, the patient location at the time the order was placed, the date and time of the order, and whether the order was retracted. We also collected available patient demographic information, including sex, race/ethnicity, and health insurance status. We included all infants receiving care in the study NICUs for whom an order was placed during the study periods. No exclusion criteria were applied at the order, patient, or clinician level.
We used descriptive statistics to summarize the characteristics of the sample, and we conducted χ2 analyses to examine the association of demographic variables with singleton and multiple births. In the primary analysis, we examined the rate of RAR events using the order as the unit of analysis. First, to compare the rate of RAR events between multiple and singleton births, we constructed logistic regression models with patient-level random intercepts to calculate unadjusted and adjusted odds ratios (ORs) with 95% CIs using the Wald test with a 2-tailed significance threshold of P = .05. We included race/ethnicity, and health insurance status as covariates based on the a priori assumption that these variables may be associated with differential use of assisted reproductive technologies (such as in vitro fertilization)20,21 that are more likely to result in multiple births.22 Next, we examined the rate of intrafamilial and extrafamilial RAR events among multiple births to assess the proportion of errors that occurred between multiple-birth infants and siblings and between multiple-birth infants and nonsiblings. These analyses were performed for the overall study population and for each study site. To evaluate the difference in RAR events between sites, we used a logistic regression model with the study site as a covariate and a patient-level random intercept. To examine whether the risk of wrong-patient orders associated with multiple birth was similar across study sites, a random-effects logistic regression model, including an interaction term (study site and singleton birth vs multiple birth), was used for both unadjusted analyses and analyses adjusted for sex, race/ethnicity, and health insurance status. Finally, we examined the rate of RAR events among twins and higher-order multiple-birth infants at the order level. Results of these analyses are reported as the number of RAR events per 100 000 orders.
To examine the risk of wrong-patient order errors for individual infants, we performed an additional analysis with the patient as the unit of analysis. First, to describe the risk associated with increasing numbers of siblings receiving care in the NICU (0, 1, or ≥2 siblings), we calculated the rate of RAR events among singletons, twins, and higher-order multiples. Next, we calculated the percentage of infants for whom an order was placed in error and the percentage of sets of multiple-birth infants that included at least 1 sibling who was subject to at least 1 order error. Each RAR event was associated only with the patient for whom the initial order was placed and not with the patient for whom it was subsequently reordered (ie, a wrong-patient order between a set of twins was counted once). All statistical analyses were conducted using Stata software, version 15.0 (StataCorp).
Results
Study Population
A total of 1 536 160 orders placed for 10 819 infants were included in the analyses. Of those, 55.8% were male, 44.2% were female; 85.5% were singleton-birth infants and 14.5% were multiple-birth infants (Table 1). Multiple-birth infants were more likely than singleton-birth infants to be female (49.5% [777 of 1569] vs 43.3% [4007 of 9250]), white (35.8% [562 of 1569] vs 23.1% [2140 of 9250]), and have commercial health insurance (73.1% [1147 of 1569] vs 52.2% [4825 of 9250]).
Table 1. Participant Characteristics.
| Variable | Participants, No. (%) | ||
|---|---|---|---|
| All Births (N = 10 819) | Singleton Births (n = 9250)a | Multiple Births (n = 1569)a | |
| Sex | |||
| Male | 6035 (55.8) | 5243 (56.7) | 792 (50.5) |
| Female | 4784 (44.2) | 4007 (43.3) | 777 (49.5) |
| Race/ethnicity | |||
| White | 2702 (25.0) | 2140 (23.1) | 562 (35.8) |
| Hispanic | 1559 (14.4) | 1404 (15.2) | 155 (9.9) |
| Black | 1277 (11.8) | 1134 (12.3) | 143 (9.1) |
| Other/unknown | 5281 (48.8) | 4572 (49.4) | 709 (45.2) |
| Health insurance | |||
| Commercial | 5972 (52.2) | 4825 (52.2) | 1147 (73.1) |
| Medicaid | 4772 (44.1) | 4352 (47.0) | 420 (26.8) |
| Self-paid | 75 (0.7) | 73 (0.8) | 2 (0.1) |
P < .001 for all comparisons using χ2 analyses of singleton and multiple births adjusted for sex, race/ethnicity, and health insurance status.
Wrong-Patient RAR Events: Multiple vs Singleton Births
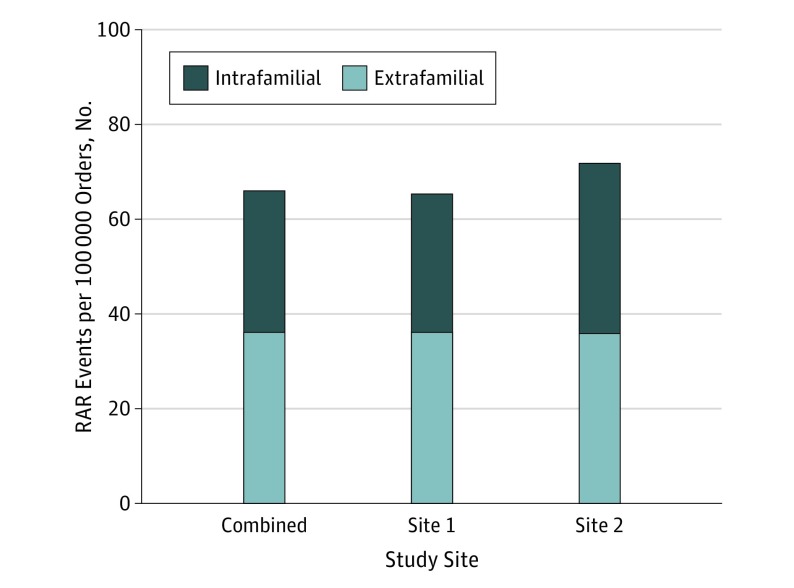
Overall, the rate of RAR events was significantly higher among multiple-birth infants than singleton-birth infants (66.0 vs 41.7 RAR events per 100 000 orders, respectively; adjusted OR, 1.75; 95% CI, 1.39-2.20; P < .001). Unadjusted analyses and analyses adjusted for sex, race/ethnicity, and health insurance status yielded comparable results (Table 2). The risk of wrong-patient order errors occurring between unrelated infants in the NICU was similar regardless of multiple-birth status. The rate of extrafamilial RAR events among multiple-birth infants was 36.1 per 100 000 orders compared with 41.7 per 100 000 orders among singletons (OR, 0.95; 95% CI, 0.80-1.20; P = .63). The excess risk among multiple-birth infants was accounted for by the rate of intrafamilial RAR events, consisting of an additional 29.9 errors per 100 000 orders between siblings of the same set of multiple births (Figure). Results were similar at both study sites.
Table 2. Wrong-Patient Orders Among Multiple and Singleton Births.
| Variable | Orders, No. | RAR Events, No.a | RAR Events per 100 000 Orders, No. a | Odds Ratio (95% CI)b | |
|---|---|---|---|---|---|
| Unadjusted | Adjustedc | ||||
| Singleton-birth infants | 1 225 632 | 511 | 41.7 | 1 [Reference] | 1 [Reference] |
| Multiple-birth infants | 310 528 | 205 | 66.0 | 1.72 (1.37-2.15)d | 1.75 (1.39-2.20)d |
| Extrafamilial | NAe | 112 | 36.1 | NA | NA |
| Intrafamilial | NAe | 93 | 29.9 | NA | NA |
Abbreviations: RAR, retract-and-reorder; NA, not applicable.
Retract-and-reorder events are defined as 1 or more orders placed for a patient that are retracted (ie, canceled) by the same clinician within 10 minutes, then reordered by the same clinician for a different patient within the next 10 minutes.
Odds ratios and 95% CIs were calculated using logistic regression analyses.
Analysis was adjusted for sex, race/ethnicity, and health insurance status.
P < .001.
The total number of orders for multiple-birth infants was used as the denominator to calculate the rate of extrafamilial (ie, between multiple-birth infants and nonsiblings) and intrafamilial (ie, between multiple-birth infants and siblings) RAR events.
Figure. Proportion of Extrafamilial and Intrafamilial Wrong-Patient Orders Among Multiple-Birth Infants Receiving Care in the Neonatal Intensive Care Unit.
Retract-and-reorder (RAR) events are defined as 1 or more orders placed for a patient that are retracted (ie, canceled) by the same clinician within 10 minutes, then reordered by the same clinician for a different patient within the next 10 minutes. Extrafamilial errors occur between a multiple-birth infant and a nonsibling receiving care in the neonatal intensive care unit (NICU) at the same time. Intrafamilial errors occur between a multiple-birth infant and a sibling receiving care in the NICU at the same time.
Study Sites
Infants at study site 1 were more likely to be white (28.9% [2493 of 8629]) and to have commercial health insurance (63.3% [5459 of 8629]) than infants at study site 2, who were more likely to be black (31.2% [684 of 2190]) or Hispanic (20.8% [456 of 2190]) and to have Medicaid as their primary health insurance (76.3% [1671 of 2190]). The overall rate of RAR events per 100 000 orders was similar across study sites (46.8 at site 1 vs 45.6 at site 2; P = .78). In addition, the increased risk associated with multiple births vs singleton births was similar at the 2 study sites based on unadjusted analyses (OR, 1.72; 95% CI, 1.35-2.20 for site 1 vs OR, 1.83; 95% CI, 1.01-3.29 for site 2; P = .89) and analyses adjusted for sex, race/ethnicity, and health insurance status (adjusted OR, 1.74; 95% CI, 1.36-2.23 for site 1 vs adjusted OR, 1.84; 95% CI, 1.02-3.31 for site 2; P = .89). Participant characteristics and primary results by study site are shown in eTables 1 and 2 in the Supplement.
Twins and Higher-Order Multiple Births
The rate of wrong-patient orders increased as the number of siblings receiving care in the NICU increased (Table 3). At the level of the order, RAR events per 100 000 orders occurred at a rate of 41.7 among singleton births, 61.2 among twin births, and 98.2 among higher-order multiple births (ie, triplets and quadruplets in these data). At the level of the patient, at least 1 order was placed in error for 3.8% of singletons (352 of 9250), 7.9% of twins (112 of 1410), and 14.5% of higher-order multiple-birth infants (23 of 159). At the level of the set of multiple births, 14.3% sets of twins (101 of 705) and 38.5% sets of higher-order multiples (20 of 52) included at least 1 sibling who was subject to at least 1 order error.
Table 3. Wrong-Patient Orders Among Singleton-Birth Infants, Twins, and Higher-Order Multiple-Birth Infants.
| Variable | Wrong-Patient Orders, by Order | Wrong-Patient Orders, by Patient | Wrong-Patient Orders, by Set | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total Orders, No. | RAR Events, No.a | RAR Events per 100 000 Orders, No.a | Total Patients, No. | RAR Events, No.a | RAR Events, % of Patientsa | Total Sets, No. | RAR Events, No.a | RAR Events, % of Setsa | |
| Singleton-birth infants | 1 225 632 | 511 | 41.7 | 9250 | 352 | 3.8 | NA | NA | NA |
| Twins | 269 808 | 165 | 61.2 | 1410 | 112 | 7.9 | 705 | 101 | 14.3 |
| Higher-order multiple-birth infantsb | 40 720 | 40 | 98.2 | 159 | 23 | 14.5 | 52 | 20 | 38.5 |
Abbreviations: RAR, retract-and-reorder; NA, not applicable.
Retract-and-reorder (RAR) events are defined as 1 or more orders placed for a patient that are retracted (ie, canceled) by the same clinician within 10 minutes, then reordered by the same clinician for a different patient within the next 10 minutes.
In these data, higher-order multiple-birth infants include triplets and quadruplets.
Discussion
The results of this large multicenter study suggest that, among infants receiving care in the NICU, the risk of wrong-patient order errors associated with multiple-birth infants was nearly double that of singleton-birth infants. Furthermore, the excess risk of wrong-patient order errors among multiple-birth infants appeared to be attributable to misidentification between siblings (ie, siblings within a set of multiple-birth infants being mistaken for one another). The risk among multiple-birth infants increased with the number of siblings receiving care in the NICU. These findings were consistent across study sites, despite differences in settings, patient populations, and electronic health record systems. Notably, both study sites already had in place a Joint Commission–compliant distinct naming convention designed to minimize wrong-patient errors. Our findings suggest that existing safeguards may be insufficient to reduce the risk of wrong-patient order errors among multiple-birth infants.
Although the primary analysis examined the risk of errors at the order level, our results can be extrapolated to assess the risk for individual infants and families. We found a graded increase in the risk of errors as the number of siblings receiving care in the NICU increased. The probability that a wrong-patient order would be placed for at least 1 member of a set of twins receiving care in the NICU was 1 in 7 sets, and the probability that a wrong-patient order would be placed for a set of triplets or higher-order multiple-birth infants was 1 in 3 sets. In our study, multiple-birth infants with siblings receiving care in the NICU comprised approximately 15% of the study population. Infants in the NICU may be particularly vulnerable to experiencing harm from order errors and other types of medical errors owing to their prematurity, low birth weight, underdeveloped organ systems, and undergoing complex treatments.23,24,25
Multiple-birth infants receiving care in the NICU may be more likely to experience wrong-patient errors owing in part to temporary newborn naming conventions that result in nearly identical identifiers.7 In previous research, a hospital-wide intervention that changed the temporary newborn naming convention (eg, Babyboy Jones) to a more distinct convention that incorporated the mother’s first name (eg, Wendysboy Jones) reduced the risk of wrong-patient orders by 36%.9 Based on these results, The Joint Commission issued a requirement effective January 2019 as part of its National Patient Safety Goals that all hospitals and health care systems must adopt a distinct temporary newborn naming convention, such as incorporating the mother’s first name.11 However, throughout the present study, both study sites used a Joint Commission–compliant distinct naming convention.3,9 The results of this study suggest that a considerable risk of misidentification among multiple-birth infants remains despite use of the recommended naming convention because temporary names for multiple-birth infants are typically distinguished by a single character.9,10,11 Thus, the requirement from The Joint Commission may provide insufficient protection against wrong-patient errors between multiple-birth infants receiving care in NICUs.
Given the limitations of temporary naming conventions, we propose alternate strategies that may mitigate the risk of newborn misidentification, particularly among multiple births. First, we propose that hospitals use the newborn’s given name when available, or use a pseudonym when the newborn’s given name is not yet chosen or when cultural or religious beliefs preclude its use. In these cases, parents should be assured that on return for care after hospital discharge, the pseudonym will be changed according to the infant’s birth certificate (as is done with other temporary naming conventions). Second, we propose that hospitals switch from the temporary name to the given name as soon as it becomes available if the infant is admitted to the NICU, with the caution that systems interoperability should be tested and any issues should be addressed. Third, we propose that obstetricians consider approaches to encourage parents, particularly of multiple gestation pregnancies, to select names or pseudonyms to use at birth, while ensuring that parents’ cultural and religious practices are respected. It should be noted that implementing these solutions would require changes to health information technology systems, workflows, and training, with the potential for additional costs and unintended consequences.
Limitations
Our study had several limitations. First, the study was conducted in 2 urban health care systems, which may limit its generalizability to patient populations in different settings and geographic areas. However, results in the large sample were remarkably similar across study sites. Second, significant demographic differences existed between multiple-birth infants and singleton-birth infants. To address this limitation, we constructed models adjusted for sex, race/ethnicity, and health insurance status, and we found that the increased risk associated with multiple births persisted. Third, we used a measure of wrong-patient orders (the Wrong-Patient RAR Measure) that captured near-miss errors intercepted by the ordering clinician. Although these errors were self-caught, research has shown that near-miss errors share the same pathway as errors that reach the patient.26 Furthermore, the use of near-miss errors to test safety improvements in health care is endorsed by major organizations dedicated to improving patient safety, including the Agency for Healthcare Research and Quality, the Institute of Medicine, the World Health Organization, the Institute for Healthcare Improvement, and The Joint Commission.26,27,28,29,30
Conclusions
The results of this study suggest that multiple-birth infants receiving care in the NICU have nearly double the risk of wrong-patient order errors compared with singleton births. The excess risk among multiple-birth infants appeared to be attributable to errors that occurred between siblings, and the risk of errors increased with the number of siblings receiving care in the NICU at the same time. Current requirements for distinct naming conventions may provide incomplete protection against identification errors among multiple-birth infants. We propose potential strategies to reduce this risk including using given names at birth, changing temporary names to given names when they become available, and developing approaches to encourage parents of multiple-birth infants to select names before birth when this practice is acceptable to the families.
eTable 1. Participant Characteristics by Study Site
eTable 2. Wrong-Patient Orders Among Multiple-Birth Versus Singleton-Birth Infants by Study Site
Footnotes
References
- 1.Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: final data for 2017. Natl Vital Stat Rep. 2018;67(8):1-50. [PubMed] [Google Scholar]
- 2.Harrison W, Goodman D. Epidemiologic trends in neonatal intensive care, 2007-2012. JAMA Pediatr. 2015;169(9):855-862. doi: 10.1001/jamapediatrics.2015.1305 [DOI] [PubMed] [Google Scholar]
- 3.Adelman JS, Aschner JL, Schechter CB, et al. Evaluating serial strategies for preventing wrong-patient orders in the NICU. Pediatrics. 2017;139(5):e20162863. doi: 10.1542/peds.2016-2863 [DOI] [PubMed] [Google Scholar]
- 4.Suresh G, Horbar JD, Plsek P, et al. Voluntary anonymous reporting of medical errors for neonatal intensive care. Pediatrics. 2004;113(6):1609-1618. doi: 10.1542/peds.113.6.1609 [DOI] [PubMed] [Google Scholar]
- 5.Simpson JH, Lynch R, Grant J, Alroomi L. Reducing medication errors in the neonatal intensive care unit. Arch Dis Child Fetal Neonatal Ed. 2004;89(6):F480-F482. doi: 10.1136/adc.2003.044438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wallace SC. Newborns pose unique identification challenges. Pennsylvania Patient Safety Advisory. 2016;13(2):42-49. http://patientsafety.pa.gov/ADVISORIES/documents/201606_42.pdf. Accessed July 22, 2019. [Google Scholar]
- 7.Gray JE, Suresh G, Ursprung R, et al. Patient misidentification in the neonatal intensive care unit: quantification of risk. Pediatrics. 2006;117(1):e43-e47. doi: 10.1542/peds.2005-0291 [DOI] [PubMed] [Google Scholar]
- 8.Hyman D, Laire M, Redmond D, Kaplan DW. The use of patient pictures and verification screens to reduce computerized provider order entry errors. Pediatrics. 2012;130(1):e211-e219. doi: 10.1542/peds.2011-2984 [DOI] [PubMed] [Google Scholar]
- 9.Adelman J, Aschner J, Schechter C, et al. Use of temporary names for newborns and associated risks. Pediatrics. 2015;136(2):327-333. doi: 10.1542/peds.2015-0007 [DOI] [PubMed] [Google Scholar]
- 10.Adelman JS, Aschner JL, Schechter CB, et al. Babyboy/babygirl: a national survey on the use of temporary, nondistinct naming conventions for newborns in neonatal intensive care units. Clin Pediatr (Phila). 2017;56(12):1157-1159. doi: 10.1177/0009922817701178 [DOI] [PubMed] [Google Scholar]
- 11.Joint Commission Distinct newborn identification requirement. R3 Report; Issue 17. https://www.jointcommission.org/assets/1/18/R3_17_Newborn_identification_6_22_18_FINAL.pdf. Published June 25, 2018. Accessed August 30, 2018.
- 12.Stavroudis TA, Miller MR, Lehmann CU. Medication errors in neonates. Clin Perinatol. 2008;35(1):141-161, ix. Ix. doi: 10.1016/j.clp.2007.11.010 [DOI] [PubMed] [Google Scholar]
- 13.Joint Commission Temporary names put newborns at risk. Quick Safety; Issue 17. https://www.jointcommission.org/assets/1/23/Quick_Safety_Issue_17_Oct_2015_10_20_15.pdf. Published October 17, 2015. Accessed March 3, 2017.
- 14.Green RA, Hripcsak G, Salmasian H, et al. Intercepting wrong-patient orders in a computerized provider order entry system. Ann Emerg Med. 2015;65(6):679-686.e1. doi: 10.1016/j.annemergmed.2014.11.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adelman JS, Kalkut GE, Schechter CB, et al. Understanding and preventing wrong-patient electronic orders: a randomized controlled trial. J Am Med Inform Assoc. 2013;20(2):305-310. doi: 10.1136/amiajnl-2012-001055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Quality Forum Patient safety 2015: final technical report. http://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=81724. Published February 12, 2016. Accessed July 27, 2018.
- 17.Lombardi D, Gaston-Kim J, Perlstein D, et al. Preventing wrong-patient electronic orders in the emergency department. Journal of Clinical Outcomes Management. 2016;23(12):550-554. [Google Scholar]
- 18.Kannampallil TG, Manning JD, Chestek DW, et al. Effect of number of open charts on intercepted wrong-patient medication orders in an emergency department. J Am Med Inform Assoc. 2018;25(6):739-743. doi: 10.1093/jamia/ocx099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adelman JS, Applebaum JR, Schechter CB, et al. Effect of restriction of the number of concurrently open records in an electronic health record on wrong-patient order errors: a randomized clinical trial. JAMA. 2019;321(18):1780-1787. doi: 10.1001/jama.2019.3698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shapiro AJ, Darmon SK, Barad DH, Albertini DF, Gleicher N, Kushnir VA. Effect of race and ethnicity on utilization and outcomes of assisted reproductive technology in the USA. Reprod Biol Endocrinol. 2017;15(1):44. doi: 10.1186/s12958-017-0262-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dieke AC, Zhang Y, Kissin DM, Barfield WD, Boulet SL. Disparities in assisted reproductive technology utilization by race and ethnicity, United States, 2014: a commentary. J Womens Health (Larchmt). 2017;26(6):605-608. doi: 10.1089/jwh.2017.6467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sunderam S, Kissin DM, Crawford SB, et al. Assisted reproductive technology surveillance—United States, 2015. MMWR Surveill Summ. 2018;67(3):1-28. doi: 10.15585/mmwr.ss6703a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaushal R, Bates DW, Landrigan C, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285(16):2114-2120. doi: 10.1001/jama.285.16.2114 [DOI] [PubMed] [Google Scholar]
- 24.Kanter DE, Turenne W, Slonim AD. Hospital-reported medical errors in premature neonates. Pediatr Crit Care Med. 2004;5(2):119-123. doi: 10.1097/01.PCC.0000112370.55948.8E [DOI] [PubMed] [Google Scholar]
- 25.Krzyzaniak N, Bajorek B. Medication safety in neonatal care: a review of medication errors among neonates. Ther Adv Drug Saf. 2016;7(3):102-119. doi: 10.1177/2042098616642231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aspden P, Corrigan JM, Wolcott J, Erickson SM, eds. Patient Safety: Achieving a New Standard for Care. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 27.Quality Interagency Coordination Task Force Doing what counts for patient safety: federal actions to reduce medical errors and their impact. https://archive.ahrq.gov/quic/Report/errors6.pdf. Published February 2000. Accessed July 27, 2018.
- 28.Leape L, Abookire S; World Alliance for Patient Safety WHO draft guidelines for adverse event reporting and learning systems: from information to action. http://apps.who.int/iris/bitstream/handle/10665/69797/WHO-EIP-SPO-QPS-05.3-eng.pdf?sequence=1&isAllowed=y. Published December 2005. Accessed July 27, 2018.
- 29.Institute for Healthcare Improvement Create a reporting system. Institute for Healthcare Improvement website. http://www.ihi.org/resources/Pages/Changes/CreateaReportingSystem.aspx. Accessed July 27, 2018.
- 30.Wu AW, ed. The Value of Close Calls in Improving Patient Safety: Learning How to Avoid and Mitigate Patient Harm. Oakbrook Terrace, IL: Joint Commission Resources; 2011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Participant Characteristics by Study Site
eTable 2. Wrong-Patient Orders Among Multiple-Birth Versus Singleton-Birth Infants by Study Site