Sir,
Talaromycosis (penicilliosis) is an opportunistic fungal infection seen in immunocompromised setting. Talaromyces marneffei (T. marneffei) was first isolated from bamboo rat's liver. Disseminated talaromycosis was first reported in 1988 in a 61-year-old HIV-infected American missionary.[1] Number of cases of talaromycosis have been reported from Manipur, India, but very few cases have been reported from Assam, a neighboring state of Manipur.[2]
We, hereby, report a case of classical disseminated talaromycosis from Silchar, a district located in South Assam. A 39-year-old female patient presented to us with moderate intermittent fever, dry cough, and skin lesions distributed mainly over the face for 8 days. Her husband was a truck driver who was HIV positive and died 2 years back due to the chest infection. On examination, there were multiple lesions on the face with different morphologies such as vesicles, papules, and nodules interspersed with hemorrhagic and crusted lesions [Figure 1]. Few lesions were also present over the trunk and upper limbs. In addition, the patient also had oral and vaginal candidiasis. On the first impression, it was thought to be hemorrhagic varicella in an immunocompromised individual. Hence, she was given intravenous acyclovir. However, no significant improvement was noted even after 5 days of treatment. Laboratory investigation showed HIV positivity with CD4 T cell count 62/μL. Her chest X-ray revealed bilateral diffuse reticulonodular opacities with prominent bronchovascular markings. Differential diagnosis such as histoplasmosis, talaromycosis, and cryptococcosis were considered. For confirmation of diagnosis, skin biopsy, and fungal culture in Sabouraud's dextrose agar (SDA) was carried out. Biopsy revealed multiple fungal elements with nonbudding yeast cell having transverse septum [Figure 2]. SDA culture showed flat, glabrous, moist, and radially folded colonies. After 5 days of incubation at 25°C, a diffusible red pigment was found around the colonies [Figure 3]. Fungal mycelia were clearly seen in microscopy after lactophenol cotton blue staining [Figure 4]. All these features confirmed the diagnosis of talaromycosis. Administration of anti-retroviral therapy (ART) and amphotericin B, resulted in significant clinical and radiological improvement in 2 weeks. The patient was discharged with oral itraconazole 400 mg/day. Unfortunately, the patient did not turn up for follow-up. T. marneffei, the etiological fungus of talaromycosis is transmitted to human through inhalation of spores from soil. It then spreads to the reticuloendothelial system, skin and other organ system through the hematogenous route. Cutaneous manifestations may mimic histoplasmosis, having mucocutaneous papules with central umbilication; ulceration, and lymphadenopathy may also be seen. It may precipitate Sweet's syndrome, erythema nodosum, and exanthematous pustulosis. It can be misdiagnosed as pulmonary tuberculosis, melioidosis, cryptococcosis, and leishmaniasis.[3] Sample from skin lesions, blood, or bone marrow may show characteristic nonbudding yeast cell with transverse septum. Definitive diagnosis can be made with culture from the lesional specimen.
Figure 1.

Multiple lesions on the face showing various morphological patterns like vesicles, papules and nodules
Figure 2.
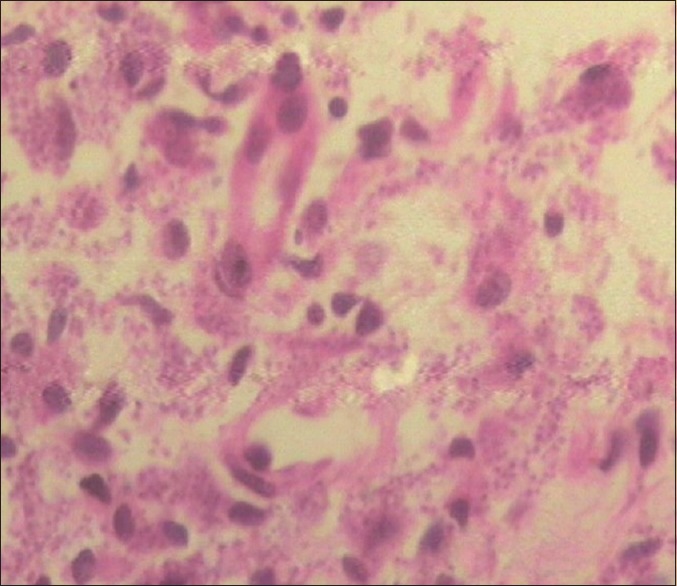
Multiple small fungal elements in yeast form, (H and E, ×400)
Figure 3.
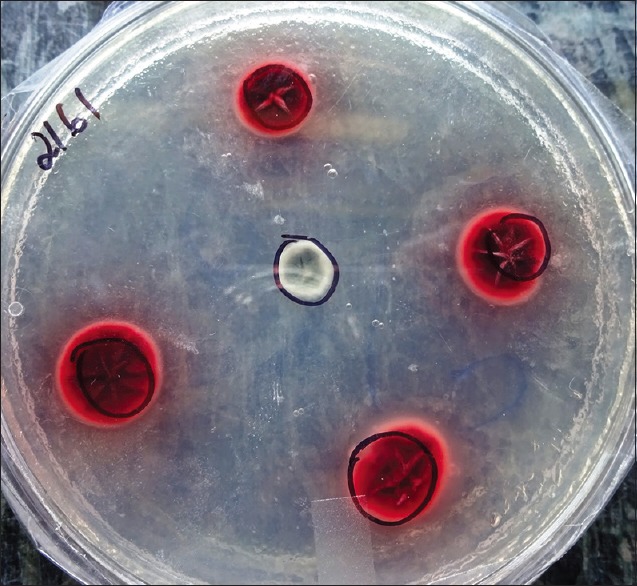
Culture in Sabouraud's dextrose agar showing flat, glabrous, moist, radially folded colonies, with diffusible red pigment
Figure 4.
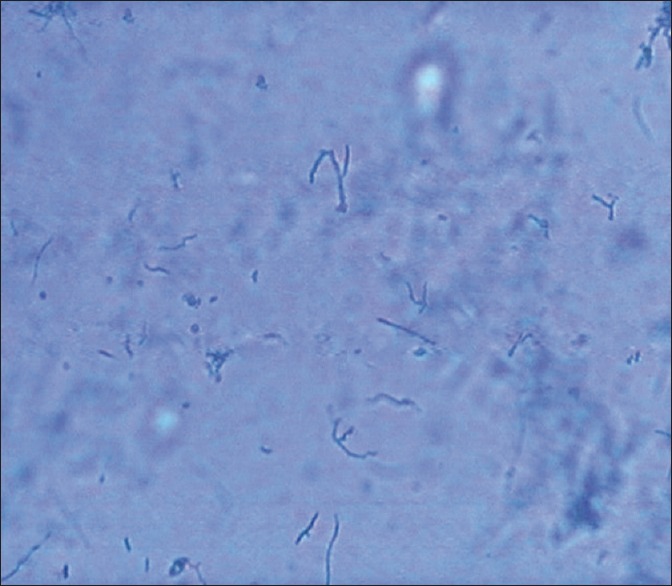
Lactophenol cotton blue staining showing multiple fungal mycelia (×100)
In a study, Raju et al. described how cutaneous manifestations correlated with CD4 count.[4] These infections may also appear after starting ART, as a manifestation of immune reconstitution inflammatory syndrome.[5] T. marneffei can affect persons with normal immunity also, but it is very rare and quite reasonably it produces mild localized infection.[6] As the prognosis and severity depend on the patient's immune status, antifungal drugs mainly amphotericin B, itraconazole, and ART improve the clinical condition.
Reports of talaromycosis are quite infrequent, especially of cases that are diagnosed and confirmed on the basis of histopathology, with special stains and culture. We, thus report one such case with all supporting evidence.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Jung JY, Jo GH, Kim HS, Park MY, Shin JH, Chin BS, et al. Disseminated penicilliosis in a Korean human immunodeficiency virus infected patient from Laos. J Korean Med Sci. 2012;27:697–700. doi: 10.3346/jkms.2012.27.6.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saikia L, Nath R, Mahanta J. Penicillium marneffei infection in Assam. Indian J Dermatol Venereol Leprol. 2010;76:75–6. doi: 10.4103/0378-6323.58692. [DOI] [PubMed] [Google Scholar]
- 3.Thomas CF, Jr, Limper AH. Pneumocystis pneumonia. N Engl J Med. 2004;350:2487–98. doi: 10.1056/NEJMra032588. [DOI] [PubMed] [Google Scholar]
- 4.Raju PV, Rao GR, Ramani TV, Vandana S. Skin disease: Clinical indicator of immune status in human immunodeficiency virus (HIV) infection. Int J Dermatol. 2005;44:646–9. doi: 10.1111/j.1365-4632.2004.02067.x. [DOI] [PubMed] [Google Scholar]
- 5.Samson JF, Suja V, Samad KA, Sankar S, Libu GK. Immune reconstitution inflammatory syndrome: A therapeutic paradox. Indian Dermatol Online J. 2012;3:205–7. doi: 10.4103/2229-5178.101822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yap FB, Thevarajah S, Asmah J. Penicillium marneffei infection in an African man. Dermatol Online J. 2010;16:2. [PubMed] [Google Scholar]


