Abstract
Classification is the process of grouping similar entities under one category for the ease of their comprehension and better handling. Medical classification dates back to the days of William Farr who is credited with the development of a nosology, which later served as the forerunner for the modern-day disease classification by ICD. The WHO system of classification is a time-honoured system that has prevailed from decades together and is under constant evolution. The classification of odontogenic tumours was first formulated by Pierre Paul Broca and has undergone several transformations over years. Though the earlier classifications and their modifications by several authors and even by the WHO appeared to be fitting for their time, the latest edition of WHO classification of odontogenic and maxillofacial bone tumours neither seems to be complete nor perfect, even at the present context. It is unfortunate that even with the advancement of molecular biology, the present WHO classification on Odontogenic and Maxillofacial bone tumours, fails to serve as a ‘reference standard’ in the true sense of the term. This article highlights the limitations of the current classification with constructive criticism that may help in further improvement.
Keywords: Ameloblastoma, bone tumors, Broca, maxillofacial bone tumors, neoplasms, nonodontogenic cysts, odontogenic cysts, odontogenic keratocyst, odontogenic tumors, World Health Organization Classification
INTRODUCTION
Classifications have been of pivotal importance in shaping medicine and guiding its practice since time immemorial. Classification is the arrangement of things that have properties in common. It groups items together that have more similarities with one another than objects in another group. However, an effective classification is the one that acknowledges both differences and similarities.[1]
The origin of classification dates back to the days of Aristotle, who developed the first classification system, which divided all organisms into two groups: plants and animals. He presented a “schema of things” to account for the particular as well as universal. Another great methodologist, who later came to be known as the Father of taxonomy, Linnaeus, echoed Aristotle's pattern of classification, expanding and simplifying the existing systems.[1]
William Farr, several years later, insisted on the universality of scientific terms and proposed a classification system called “a method of generalization” which later served as the forerunner of the modern International Classification of Diseases.[1] The significant work by John Graunt and Thomas Sydenham in the 17th century further gave medical classification a distinct trajectory.[1] Several evolutions were thus being brought about by the classification theorists who were also clearly defining the aims of classification.
Eventually, in the 19th century, the prominent contemporary disease classification system, namely, the International Classification of Diseases, entrusted with the World Health Organization (WHO), brought about a huge impact in the world of classifications by combining the past and present concepts of the nature of diseases.[1] With the development of molecular and cytogenetic studies, which changes the knowledge and perception regarding diseases, the classification system is on constant evolution. Nevertheless, classification of diseases should be simple, comprehensive and universally accepted.
EVOLUTION OF ODONTOGENIC TUMOURS CLASSIFICATION
Around the mid-19th century, due to increase in reports on odontogenic pathologies from all around the world, a multifaceted personality named Pierre Paul Broca published a monograph in 1869, consisting of several tumor classifications, one among which was on odontogenic tumors.[2] He suggested the use of the term “odontome” for all tumors arising from the odontogenic apparatus, and his classification was based on the stage of tooth development at the onset of the abnormality.[2] However, his work did not focus much on oral pathology and was limited within France, thus failing to gain popularity.[3]
Another popular French histologist, named Malassez, presented Broca's classification with minor modifications in 1885.[4] It, however, did not create much impact globally and faded away soon.[3]
In 1888, Bland and Sutton laid down the ground for the modern taxonomy of odontogenic tumors. They based their classification on the specific cells of the tooth germ that gave rise to the tumors and went on to include odontogenic cysts and fibrous osteogenic tumors in their classification while maintaining the use of the term “odontome.”[5]
An elaborate report on odontomes was sought from Gabell et al., by the British Dental Association in early 1914, who then further modified and elaborated Bland–Sutton's classification.[6] They also used the term odontomes to refer to odontogenic tumors but classified them into three main groups: (1) the epithelial odontomes, (2) the composite odontomes and (3) the connective tissue odontomes.[6]
Continuous extensive studies on odontomes eventually led to the replacement of the term by more pathologically compatible terms. The multilocular odontogenic cysts came to be known as adamantinoma, later renamed by Ivy and Churchill as ameloblastoma.[3] The connective tissue odontomes were called fibromas or cementomas based on their structure. However, the composite odontomes, made of both epithelial and connective tissue components, remained to be called as odontomes or odontomas.[3]
The classification proposed by Thoma and Goldman in 1946 excluded odontogenic cysts that were initially included in the classification by Bland and Sutton.[5] Enamel pearls being developmental malformations rather than neoplasms were considered as tumors and were included in the classification as enamelomas, which is obviously a misnomer. Their classification was in fact widely accepted and in 1952, it was adopted by the American Academy of Oral Pathology with minor changes.[7]
Pindborg and Clausen in 1958 came forward with yet another classification, which was based on the reciprocal interaction between the epithelium and the mesenchyme.[8] They believed that the reciprocal induction was surely the cause of some of the cellular changes in the pathogenesis of these tumors. They classified the tumors primarily into two groups: epithelial and mesodermal, which though was much debated generally received positive reviews. The epithelial tumors were further subclassified into (1) pure epithelial tumors with no inductive changes and (2) epithelial tumors with inductive changes in the mesenchyme.[8]
Furthermore, Gorlin et al. in 1961 brought about slight modifications in the Pindborg and Clausen classification, which then served a key role in the WHO publication of “Histological Typing of Odontogenic Tumours.”[9]
The need for a standard classification of neoplasms was agreed upon by the WHO way back in 1958, and the 1st edition of classification was published in 1971.[10] It was titled as “Histological typing of odontogenic tumours, jaw cysts and allied lesions,” with elaborate inclusion of all neoplasms and cysts of odontogenic origin. However, the classification also included various bone lesions with characteristic features when occurring in jaws. The 2nd edition published in 1992 maintained this elaborate scope.[11] The 3rd edition of 2005 saw the exclusion of odontogenic cysts; however, the “bone-related and tumor-like lesions” were kept intact.[12] The 4th and the latest WHO Classification of Head and Neck Tumours was published in January 2017 by an expert panel consisting of eminent pathologists from around the world.[13] This classification re-included cysts and claimed to simplify the overall classification of both cysts and tumors.
THE PRESENT SCENARIO
The latest classification was formulated with the objective of simplicity, scientific accuracy, reproducibility and utility for the surgical pathologists globally.[14]
The current classification (WHO 2017) proposed various additions, deletions and modifications of lesions based on evidence and molecular studies. Classification, as discussed earlier, plays a vital role in not just understanding the pathogenesis of a disease but also elaborating its behavior and prognosis.
As far as other lesions are concerned, the latest blue book contains major changes in terms of refinement of existing entities, description of new tumor types, deletion of defunct categories and an update on the biology of various tumor types.[15] However, the present WHO Classification on “Odontogenic and Maxillofacial Bone Tumours” simply lists lesions in a rational order and attempts to provide evidence for their validity. Although it offers direction for the management of these diseases, its value and diagnostic utility appears to be limited owing to its acuity and want of precise terminology.[16]
Although the reversal of changes of widely used classification and terminologies is often unreal, it sometimes becomes important to understand the caveats in their use and deficiencies of these systems. The WHO classification is expected to act as a “reference standard” internationally and thus, changes made in it should be carefully scrutinized and supported by adequate evidence and documentation. Although changes and their reversal have been made multiple times in WHO classifications, it however seems insufficient in defining/categorizing the lesions listed under “odontogenic and maxillofacial bone tumours.”
This article is thus only an attempt to express our views and constructive criticism in the hope that it will be an aid for further development of the WHO classification and not intended to add knowledge or update the lesions.
The current classification (2017) of odontogenic cysts and tumors saw changes from its inception. It primarily divided odontogenic tumors into malignant and benign. The complex and elaborative classification of the benign tumors (based on the epithelial-mesenchymal induction; odontogenic epithelium with mature fibrous, stroma without odontogenic ectomesenchyme; odontogenic epithelium with odontogenic ectomesenchyme with or without hard-tissue formation and mesenchyme and/or odontogenic ectomesenchyme with or without odontogenic epithelium)[12] was shunned. Rather, a simpler division of those tumors was devised under the headings of epithelial, mesenchymal and mixed odontogenic tumors, with the aim of simplifying the new classification. Another significant change in the latest 2017 classification was the re-inclusion of odontogenic cysts. The classification of 1992[11] last saw the modification of odontogenic cysts, following which they were eliminated from the 2005 version.[12] In the 4th classification of odontogenic tumors, however, it was again added to the classification with certain modifications.[13] The changes made to the classification of cysts, time and again, were however without any solid explanation and were not entirely inclusive even in the latest edition.[17,18,19,20,21]
The classification of odontogenic and maxillofacial tumors should start with the definition of terminologies. The literal meaning of “tumor” is swelling.[22,23] However, in the WHO classification, the word “tumor” is used to denote inflammatory, benign or malignant growths, and is not very specific. Instead, it can be replaced by the word “neoplasm” referring to a new growth, which can either be benign or malignant. Various authors have recommended and supported the use of the term “tumor” in a broader context in the WHO classification as it includes a myriad of lesions.[24]
With the evolution of terminologies and advances in the field of science in general and molecular biology in particular, it is rather unfortunate to go reverse and use a word that is nonspecific instead of implementing a perfect terminology that would avoid confusion and increase the preciseness of an international classification.
The odontogenic and maxillofacial bone tumors include a heterogeneous group of lesions ranging from benign neoplasms, cysts, hamartomas to malignant neoplasms, with metastatic potential.[13] The various lesions included in the classification differ in their nature, clinical features and biological behavior, and therefore, separate classifications comprising like-featured entities would be a better alternative. The inclusion of all these lesions under one umbrella is rather bizarre and is almost like grouping Asians, Caucasians and Mongolians under the same category!
The classification of odontogenic tumors in the 2nd and 3rd editions[11,12] was based on the type of odontogenic tissues that were involved and the inductive changes that led to hard-tissue formation. The 3rd edition further classified tumors based on their supposed biological origin or histological variants.[12] However, the 4th edition of 2017[13] formed a very concise classification despite the addition of three new tumors. It lists a total of 23 odontogenic lesions in contrast to the 30 in the 3rd classification, and there is around 50% increase in the number of entities when compared to the previous classification.[13] In order to simplify the latest classification, tumors have merely been classified into benign and malignant.
Three new lesions were included in the list of odontogenic tumors namely sclerosing odontogenic carcinoma, odontogenic carcinosarcoma and primordial odontogenic tumor.[13] Although only nine cases of sclerosing odontogenic carcinoma,[25] seven cases of primordial odontogenic tumor[26] and less than ten cases of odontogenic carcinosarcoma[27] have been reported in literature, these have been newly included in the current edition of the WHO classification. The WHO classification is regarded as a standard reference worldwide and therefore, larger epidemiological studies should be conducted before inclusion of such rare lesions. These lesions may rather be included under the (new) heading of “rare lesions” in the WHO classification.
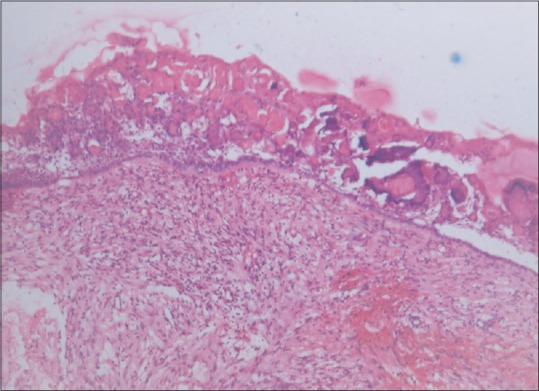
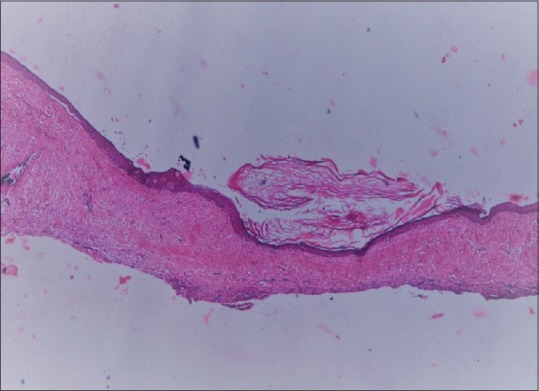
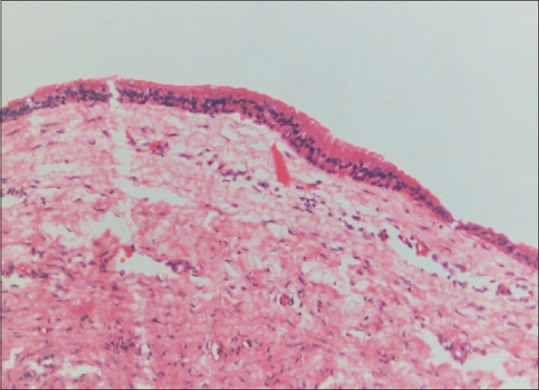
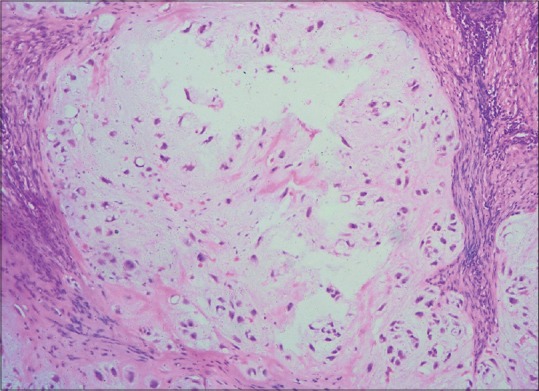
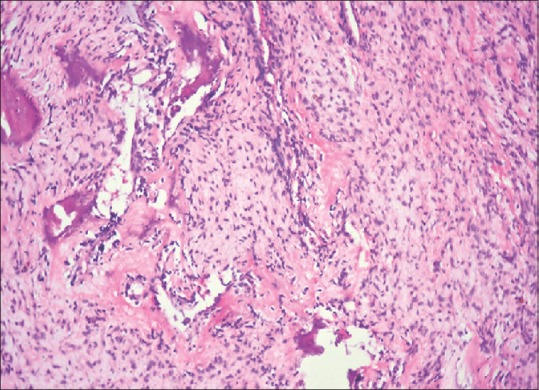
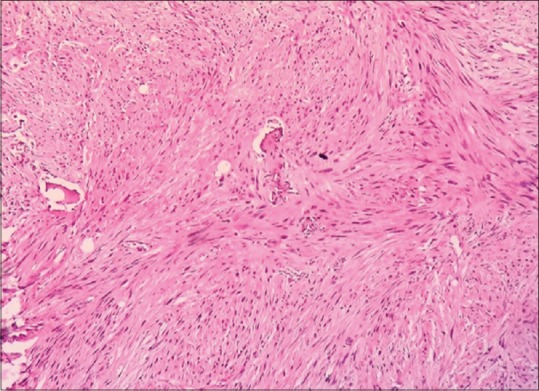
The decision to remove the term solid/multicystic ameloblastoma from the current classification is a good one as it is almost synonymous with conventional ameloblastoma[12,13] [Figure 1]. However, desmoplastic ameloblastoma, which was subclassified as a separate clinical type in the WHO 2005 classification, was re-included only as a histological subtype in the 2017 classification [Figure 2]. This change seems questionable as desmoplastic ameloblastomas show distinct variations in their clinical and radiographical presentation and biological behavior in comparison to other histological subtypes of ameloblastoma. Furthermore, the hybrid odontogenic tumors have not been mentioned in the WHO classification of odontogenic neoplasms despite reasonably good number of cases being reported in literature[28,29,30,31,32] [Figure 3].
Figure 1.
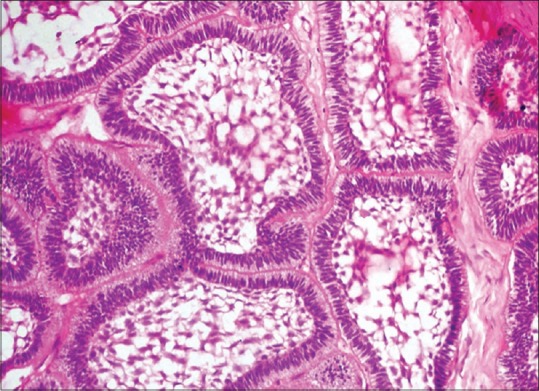
Follicular ameloblastoma (Courtesy of Dr. V. Ramesh, Professor and Dean, MGPGI Dental Sciences, Puducherry, India)
Figure 2.
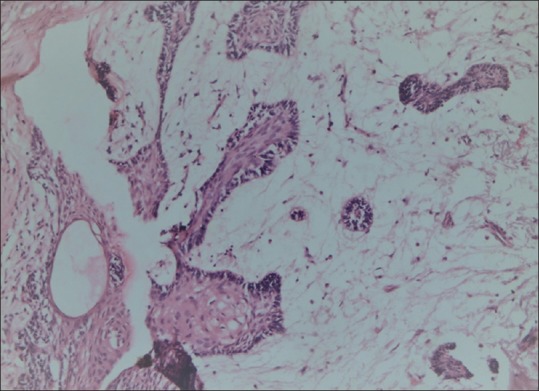
Desmoplastic ameloblastoma
Figure 3.
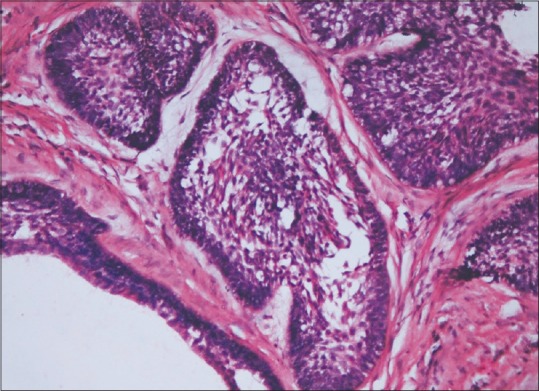
Hybrid ameloblastoma
Peripheral ameloblastoma was rightly retained as a separate clinical entity in the 2017 classification.[13] However, the peripheral varieties of adenomatoid odontogenic tumor,[33,34] squamous odontogenic tumor[35,36] or calcifying epithelial odontogenic tumor[37,38] were not included in the classification despite adequate evidences in the literature.
Yet another striking change in the latest classification is the shift of metastasizing (malignant) ameloblastoma from the malignant to benign category of tumors[12,13] given that metastasis is an essential feature of malignancy. This change is pretty questionable and demands adequate justification.
The next section of the classification involves odontogenic and nonodontogenic cysts,[13] which, by itself, seems unfitting. Although cysts appear as swelling, they are in fact cavities filled with liquid or gaseous substance and not composed of solid mass. Furthermore, they do not show neoplastic nature (i.e., unrestrained growth) and hence certainly do not qualify as neoplasms. Merely owing to the conceptual overlap of cysts and cystic neoplasms in odontogenic keratocyst (OKC) and calcifying odontogenic cyst (COC), the general classification of cysts should not be altered. Therefore, it is only appropriate for cysts to have a separate classification of their own, which may include cysts of all origins.
The 2017 classification divided odontogenic cysts into developmental and inflammatory. Inflammatory odontogenic cysts include radicular cysts and inflammatory collateral cysts. Developmental odontogenic and nonodontogenic cysts include dentigerous cysts, OKCs, lateral periodontal cysts, botryoid odontogenic cysts, gingival cysts, glandular odontogenic cysts, COCs, orthokeratinized odontogenic cysts (OOCs) and nasopalatine duct cysts.[13]
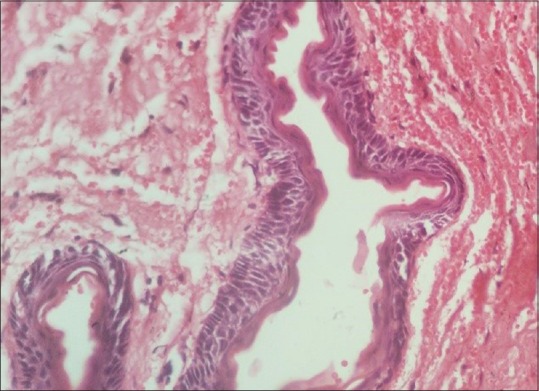
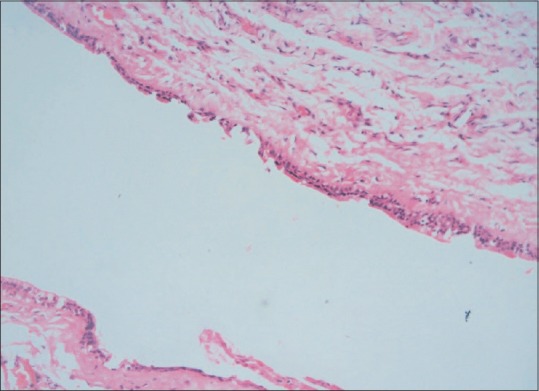
The most noticeable change in the latest classification is keratocystic odontogenic tumor and calcifying cystic odontogenic tumor that were included in the classification of tumors in 2005 were again brought back under the heading of cysts in the 2017 classification and are called OKC and COC, respectively [Figures 4 and 5]. OOC, for the first time, has been listed as a separate entity[13] [Figure 6]. It has striking features in contrast to OKC with regard to its histology and behavior, which has prompted it to be called as a separate lesion rather than a subtype of OKC.[39,40]
Figure 4.
Odontogenic keratocyst
Figure 5.
Calcifying odontogenic cyst
Figure 6.
Orthokeratinized odontogenic cyst
This classification does not list the variants of the lesions which are however discussed in the text. The lesions such as “residual,” “apical” and “lateral” cysts are not included as distinct subsets of radicular cyst, whereas “eruption” cyst is mentioned only as a variant of dentigerous cyst. Although this makes the classification less complex, it may however cause confusion among the clinicians.
Nasopalatine duct cyst [Figure 7], a nonodontogenic developmental cyst,[38] has found its place in the list of cysts in the 2017 classification; however, the other nonodontogenic developmental cysts such as median palatine, or palatal cysts of neonates, have not been included. This remains unexplained. The inclusion of a soft-tissue cyst such as gingival cyst in the present cyst classification prompts to question the noninclusion of nasolabial cyst, also a soft-tissue cyst [Figure 8]. Apart from the developmental nonodontogenic intraosseous cysts, the extraosseous cysts and most of the nonodontogenic cysts (thyroglossal duct cyst, oral lymphoepithelial cyst, epidermoid and dermoid cysts, salivary cyst, antral cyst, parasitic cyst and Stafne bone cyst) are also missing from the current classification.[39]
Figure 7.
Nasopalatine duct cyst
Figure 8.
Nasolabial cyst
A separate classification for cysts including odontogenic and nonodontogenic cysts (developmental and inflammatory) as well as the other bone and soft-tissue cysts should be formulated under a possible heading of “cysts of maxillofacial region” for better clarity. Besides, the title of the current classification reads “WHO classification of odontogenic and maxillofacial bone tumours,” and it is rather imbecile to include cysts as a part of that classification.
The next segment of the WHO 2017 classification consists of maxillofacial bone tumors.[13] Most of the articles published thus far seem to be interested in discussing about only the first part of the classification (odontogenic).[14,16,21,24] However, the heading of this classification is “WHO classification of odontogenic and maxillofacial bone tumours” which includes other bone tumors of nonodontogenic origin and is therefore equally important to throw adequate light.[13]
In the previous edition, few nonodontogenic lesions were arbitrarily included under the title of “WHO histological classification of odontogenic tumours,” the reason for which was not justified.[12] In the current classification, however, this list was expanded further to include 19 more lesions. According to the WHO group, these tumors “either have jaws or other maxillofacial bones as their predilection sites or are important in view of their differential diagnosis.”[13] However, some of these lesions, for example, chondroma, chondrosarcoma and osteosarcoma, though occur in the jaws, do not essentially show greater predilection for this site.[41] In addition, listing of unrelated entities together under a specific heading does not seem to be logical (e.g., central giant cell granuloma, peripheral giant cell granuloma, aneurysmal bone cyst [ABC] and simple bone cyst [SBC]).[13] If it were to acknowledge these lesions just for the sake of differential diagnosis, the list still appears incomplete. Thus, grouping other maxillofacial tumors under a separate classification would be better as they differ significantly from odontogenic neoplasms.
The WHO Blue Book of Classifications is based on the topography of the lesions included in the classification.[13] However, in the “WHO classification of odontogenic and maxillofacial bone tumours,” the first segment containing the odontogenic neoplasms seems to be based on the origin of the lesions (odontogenic) and the next part of the classification, on origin as well as topography of the lesions. This is rather unclear and creates difficulty in comprehending the basis of classification of the odontogenic and maxillofacial bone tumors as it appears to be a mix of both. While there seems to be a uniformity in the classification of other neoplasms in the WHO blue book, this is surely an exception.
Chondrosarcoma and osteosarcoma have been included in the present classification under the heading of malignant maxillofacial bone and cartilage tumors [Figures 9 and 10]. However, fibrosarcoma, which is also a malignant neoplasm occurring in the jaws, is left out [Figure 11]. Although fibrosarcoma is a neoplasm of the fibroblasts, and not the cartilage or bone, this neoplasm also occurs in the jaws.[41] Therefore, this remains quite unexplained and further fuels our observation of the ambiguity in the basis of classification of these neoplasms (topography/tissue of origin?). Strangely enough, desmoplastic fibroma, despite being a benign neoplasm of fibroblastic origin, is included in the list of benign maxillofacial bone and cartilage tumors, further highlighting the disparity.
Figure 9.
Chondrosarcoma (Courtesy of Dr. Madhavan Nirmal, Professor and Head, Department of Oral Pathology, Raja Muthaiah Dental College, Chidambaram, Tamilnadu, India)
Figure 10.
Osteosarcoma (Courtesy of Dr. Madhavan Nirmal, Professor and Head, Department of Oral Pathology, Raja Muthaiah Dental College, Chidambaram, Tamil Nadu, India)
Figure 11.
Fibrosarcoma (Courtesy of Dr. Prathiba Ramani, Professor and Head, Saveetha Dental College, Chennai, Tamilnadu, India)
Moreover, with the inclusion of osteosarcoma in the current classification, it only seems natural to include Ewings sarcoma and the like, which also occur in other bones [Figure 12]. The oral vasoformative tumors (central hemangioma, central lymphangioma, etc.) and locally aggressive fibrous lesions (fibrous histiocytoma, nodular fasciitis, etc.)[40] have also been given a miss from the classification.
Figure 12.
Ewings sarcoma (Courtesy of Dr. Leena Dennis Joseph, Professor of Pathology, Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamilnadu, India)
Fibro-osseous lesions namely fibrous dysplasia, cemento-osseous dysplasia, ossifying fibroma or familial gigantiform cementoma should ideally be classified under a separate heading. Fibrous dysplasia is essentially a developmental anomaly, wherein bone gets replaced by fibrous tissue, whereas ossifying fibroma, cemento-osseous dysplasia or familial gigantiform cementoma are either reactive or dysplastic, derived from periodontal ligament, extraligamentary bone or remnants of cementum.[42,43,44,45] Although they occur in the jaws and may even present as swellings, they do not show neoplastic nature and can be classified separately. Cherubism, a genetically inherited developmental anomaly affecting the jaws of children, also seems unfitting in the classification of neoplasms for the same justification as fibro-osseous lesions.[46]
The current classification encompasses certain lesions under the heading of giant cell lesions and bone cysts. However, there exist several other lesions that contain giant cells and are also found in the jaws (giant cell tumor (?), Brown's tumor),[47] which have not been included in the list. Interestingly, peripheral giant cell granuloma has found a place in the classification of odontogenic and maxillofacial bone tumors, which is rather bizarre as it is a reactive lesion which does not occur in the bone and is neither a counterpart of central giant cell granuloma.[41] In that case, fibroma and fibroepithelial polyp may also be included in the classification of odontogenic and maxillofacial tumors given their similarities with peripheral giant cell granuloma.
The “bone cysts” that have been included under “giant cell lesions and bone cysts” are ABCs and SBCs. This is pretty enigmatic as both ABC and SBC are only pseudocysts[39] and to top it, most cysts discussed under this classification occur in the bone/jaws; therefore, a separate subheading of “bone cysts” under the main classification seems unnecessary. They can rather be included in the cyst classification with a separate heading of “pseudocysts.”
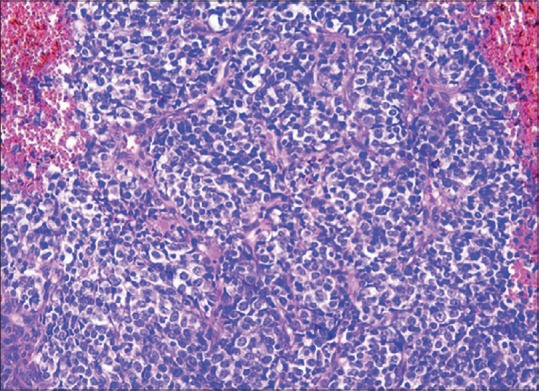
The list of hematolymphoid tumors in the current classification includes solitary plasmacytoma of bone alone.[13] However, Burkitt's lymphoma, primary lymphoma of bone, multiple myeloma, etc., are other hematolymphoid tumors that occur in the jaws[48,49,50,51] but are not involved in the classification of maxillofacial bone tumors, which also remains arguable.
CONCLUSION
To conclude, this commentary strives to highlight the limitations of the 4th edition of the WHO Classification of Odontogenic and Maxillofacial Tumours. This may not be ideal and most certainly not the end of nomenclature or classification of odontogenic and maxillofacial neoplasms. Science is a constant revelation, and the medical field is no different. With the development in molecular biology, diseases and classification will surely be on progressive evolution. It is only fair and just to make the best possible use of the resources and information at hand and conduct wider epidemiological surveys involving the developed as well as the developing countries, in order to make the WHO classification truly universal and the highest possible reference standard worldwide.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Dr. Manoj Prabhakar, Assistant Professor, Meenaksi Ammal Dental College, for his help rendered in the preparation of the photomicrographs.
REFERENCES
- 1.Jutel A. Classification, disease, and diagnosis. Perspect Biol Med. 2011;54:189–205. doi: 10.1353/pbm.2011.0015. [DOI] [PubMed] [Google Scholar]
- 2.Broca P. Traite des Tumeurs. Vol. 2. Paris: Asselin P, Libraire de la Faculte’ de Medicine; 1869. [Google Scholar]
- 3.Philipsen HP, Reichart PA. Classification of odontogenic tumours. A historical review. J Oral Pathol Med. 2006;35:525–9. doi: 10.1111/j.1600-0714.2006.00470.x. [DOI] [PubMed] [Google Scholar]
- 4.Soukup JW, Bell CM. Nomenclature and classification of odontogenic tumors. Part I: historical review. J Vet Dent. 2014;31:228–32. doi: 10.1177/089875641403100402. [DOI] [PubMed] [Google Scholar]
- 5.Bland-Sutton J. Odontomes. Trans Odont Soc (Lond) 1888;20:32–87. [Google Scholar]
- 6.Gabell DP, James W, Payne JL. The report on odontomes. London: John Bale, Sons & Danielsson; 1914. [Google Scholar]
- 7.Thoma KH, Goldman HM. Odontogenic tumours. A classification based on observations of epithelial, mesenchymal and mixed varieties. Am J Pathol. 1946;22:433–71. [PubMed] [Google Scholar]
- 8.Pindborg JJ, Clausen F. Classification of odontogenic tumours. A suggestion. Acta Odont Scand. 1958;16:293–301. [Google Scholar]
- 9.Gorlin RJ, Chaudhry AP, Pindborg JJ. The odontogenic tumours: Their classification, histopathology and clinical behavior in man and domesticated animals. Cancer. 1961;14:73–101. doi: 10.1002/1097-0142(196101/02)14:1<73::aid-cncr2820140111>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 10.Pindborg JJ, Kramer JR, Torloni H. Histological Typing of Odontogenic Tumours, Jaw Cysts and Allied Lesions. Geneva: World Health Organization; 1971. [Google Scholar]
- 11.Kramer IR, Pindborg JJ, Shear M. 2nd ed. Heidelberg: Springer-Verlag; 1992. WHO International Histological Classification of Tumours: Histological Typing of Odontogenic Tumours. [Google Scholar]
- 12.Barnes L, Eveson JW, Reichart P, Sidransky D. Lyon: IARC Press; 2005. WHO Classification of Tumours: Pathology & Genetics, Head and Neck Tumours. [Google Scholar]
- 13.Takata T, Slootweg PJ. Odontogenic and maxillofacial bone tumours. In: El-Naggar AK, Chan JK, Grandis JR, Takata T, Slootweg PJ, editors. WHO Classification of Head and Neck Tumours. 4th ed. Lyon: IARC; 2017. [Google Scholar]
- 14.Soluk-Tekkeşin M, Wright JM. The World Health Organization Classification of Odontogenic Lesions: A Summary of the Changes of the 2017 (4th) Edition. Turk Patoloji Derg. 2018;34:1–18. doi: 10.5146/tjpath.2017.01410. [DOI] [PubMed] [Google Scholar]
- 15.Seethala RR. Update from the 4th edition of the World Health Organization classification of head and neck tumours: Preface. Head Neck Pathol. 2017;11:1–2. doi: 10.1007/s12105-017-0785-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Speight PM, Takata T. New tumour entities in the 4th edition of the World Health Organization classification of head and neck tumours: Odontogenic and maxillofacial bone tumours. Virchows Arch. 2018;472:331–9. doi: 10.1007/s00428-017-2182-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pindborg JJ, Kramer IR. Geneva: World Health Organization; 1971. International Histological Classification of Tumours: Histological Typing of Odontogenic Tumours, Jaw Cysts, and Allied Lesions. [Google Scholar]
- 18.Martin LH, Speight PM. Odontogenic cysts: An update. Diagn Histopathol. 2017;23:260–5. [Google Scholar]
- 19.Kramer IR, Pindborg JJ, Shear M. The WHO histological typing of odontogenic tumours. A commentary on the second edition. Cancer. 1992;70:2988–94. doi: 10.1002/1097-0142(19921215)70:12<2988::aid-cncr2820701242>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 20.Şahin O, Odabaşı O. Clinical and histopathological evaluation of odontogenic cysts according to World Health Organization new classification of odontogenic cysts: A preliminary study. Ponte Int J Sci Res. 2018;74:59–74. [Google Scholar]
- 21.Wright JM, Vered M. Update from the 4th edition of the World Health Organization classification of head and neck tumours: Odontogenic and maxillofacial bone tumors. Head Neck Pathol. 2017;11:68–77. doi: 10.1007/s12105-017-0794-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dorlands Illustrated Medical Dictionary. 32nd ed. Saunders: Elsevier; 2012. p. 1985. [Google Scholar]
- 23.Stedmans Medical Dictionary. 27th ed. Philadelphia: Lippincott Williams Wilkins; 2000. p. 1894. [Google Scholar]
- 24.Wright JM, Odell EW, Speight PM, Takata T. Odontogenic tumors, WHO 2005: Where do we go from here? Head Neck Pathol. 2014;8:373–82. doi: 10.1007/s12105-014-0585-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gordon P, Morrison J, Wood A, Conn B. A case report of sclerosing odontogenic carcinoma of the hard palate. Br J Oral Maxillofac Surg. 2015;53:49. [Google Scholar]
- 26.Amer H, Hafed L, Ibrahim S. Case report: A primordial odontogenic tumor. F1000Res. 2018;7:562. doi: 10.12688/f1000research.14735.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim IK, Pae SP, Cho HY, Cho HW, Seo JH, Lee DH, et al. Odontogenic carcinosarcoma of the mandible: A case report and review. J Korean Assoc Oral Maxillofac Surg. 2015;41:139–44. doi: 10.5125/jkaoms.2015.41.3.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gupta A, Jindal C. Hybrid ameloblastoma: Report of a rare case and review of literature. Int J Oral Maxillofac Pathol. 2011;2:68–72. [Google Scholar]
- 29.Iwase M, Fukuoka A, Tanaka Y, Saida N, Onaka E, Bando S, et al. Hybrid desmoplastic/Follicular ameloblastoma of the mandible: A case report and review of the literature. Case Rep Pathol. 2017;2017:7031414. doi: 10.1155/2017/7031414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Philipsen HP, Reichart PA, Takata T. Desmoplastic ameloblastoma (including “hybrid” lesion of ameloblastoma). Biological profile based on 100 cases from the literature and own files. Oral Oncol. 2001;37:455–60. doi: 10.1016/s1368-8375(00)00111-1. [DOI] [PubMed] [Google Scholar]
- 31.Takata T, Miyauchi M, Ogawa I, Zhao M, Kudo Y, Sato S, et al. So-called ‘hybrid’ lesion of desmoplastic and conventional ameloblastoma: Report of a case and review of the literature. Pathol Int. 1999;49:1014–8. doi: 10.1046/j.1440-1827.1999.00972.x. [DOI] [PubMed] [Google Scholar]
- 32.Angadi PV, Kale A, Hallikerimath S, Kotrashetti V, Mane D, Bhatt P, et al. ‘Hybrid’ desmoplastic ameloblastoma: An unusual case report with immunohistochemical investigation for TGF-β and review of literature. Eastern J Med. 2011;16:9–17. [Google Scholar]
- 33.Philipsen HP, Reichart PA, Siar CH, Ng KH, Lau SH, Zhang X, et al. An updated clinical and epidemiological profile of the adenomatoid odontogenic tumour: A collaborative retrospective study. J Oral Pathol Med. 2007;36:383–93. doi: 10.1111/j.1600-0714.2007.00536.x. [DOI] [PubMed] [Google Scholar]
- 34.Lavanya N, Rajeshwari MR, Bharathi R, Shaheen A. Peripheral adenomatoid odontogenic tumour – Is it really peripheral?: A case report. J Clin Diagn Res. 2013;7:1524–6. doi: 10.7860/JCDR/2013/5382.3179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Badni M, Nagaraja A, Kamath V. Squamous odontogenic tumor: A case report and review of literature. J Oral Maxillofac Pathol. 2012;16:113–7. doi: 10.4103/0973-029X.92986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Saxby MS, Rippin JW, Sheron JE. Case report: Squamous odontogenic tumor of the gingiva. J Periodontol. 1993;64:1250–2. doi: 10.1902/jop.1993.64.12.1250. [DOI] [PubMed] [Google Scholar]
- 37.Shetty D, Jayade BV, Jayade G, Gopalkrishnan K. Peripheral calcifying epithelial odontogenic tumor – Case report. J Oral Biol Craniofac Res. 2014;4:147–50. doi: 10.1016/j.jobcr.2014.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Houston GD, Fowler CB. Extraosseous calcifying epithelial odontogenic tumor: Report of two cases and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:577–83. doi: 10.1016/s1079-2104(97)90123-2. [DOI] [PubMed] [Google Scholar]
- 39.Sivapathasundharam B, Rajendran R. Cysts of orofacial region. In: Sivapathasundharam B, editor. Shafer's Textbook of Oral Pathology. 8th ed. India: Elsevier; 2016. pp. 62–99. [Google Scholar]
- 40.Byatnal A, Natarajan J, Narayanaswamy V, Radhakrishnan R. Orthokeratinized odontogenic cyst-critical appraisal of a distinct entity. Braz J Oral Sci. 2013;12:1–10. [Google Scholar]
- 41.Sivapathasundharam B. 8th ed. India: Elsevier; 2016. Shafer's Textbook of Oral Pathology. [Google Scholar]
- 42.Sivapathasundharam B, Madhavan Nirmal R, Rajendran R. Bone and joints diseases. In: Sivapathasundharam B, editor. Shafer's Textbook of Oral Pathology. 8th ed. India: Elsevier; 2016. pp. 457–99. [Google Scholar]
- 43.Anitha N, Sankari SL, Malathi L, Karthick R. Fibrous dysplasia-recent concepts. J Pharm Bioallied Sci. 2015;7:S171–2. doi: 10.4103/0975-7406.155892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mangala M, Ramesh DN, Surekha PS, Santosh P. Florid cemento-osseous dysplasia: Review and report of two cases. Indian J Dent Res. 2006;17:131–4. doi: 10.4103/0970-9290.29875. [DOI] [PubMed] [Google Scholar]
- 45.Young SK, Markowitz NR, Sullivan S, Seale TW, Hirschi R. Familial gigantiform cementoma: Classification and presentation of a large pedigree. Oral Surg Oral Med Oral Pathol. 1989;68:740–7. doi: 10.1016/0030-4220(89)90165-5. [DOI] [PubMed] [Google Scholar]
- 46.Waldron CA. Bone pathology. In: Neville BW, Damm DD, Allen CM, Bouquot JE, editors. Oral & Maxillofacial Pathology. Philadelphia: W.B. Saunders Company; 1995. [Google Scholar]
- 47.Pogrel AM. The diagnosis and management of giant cell lesions of the jaws. Ann Maxillofac Surg. 2012;2:102–6. doi: 10.4103/2231-0746.101325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mbulaiteye SM. Burkitt lymphoma: Beyond discoveries. Infect Agent Cancer. 2013;8:35. doi: 10.1186/1750-9378-8-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Choi JY, Hahn JS, Suh CO, Yang WI. Primary lymphoma of bone – Survival and prognosis. Korean J Intern Med. 2002;17:191–7. doi: 10.3904/kjim.2002.17.3.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gerecke C, Fuhrmann S, Strifler S, Schmidt-Hieber M, Einsele H, Knop S. The diagnosis and treatment of multiple myeloma. Dtsch Arztebl Int. 2016;113:470–6. doi: 10.3238/arztebl.2016.0470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gujral S. Hematolymphoid neoplasms: World Health Organization versus rest of the world. Leukemia. 2009;23:978. doi: 10.1038/leu.2008.327. [DOI] [PubMed] [Google Scholar]


