Abstract
Zika virus (ZIKV) is a RNA virus and belongs to genus Flavivirus and family Flaviviridae. The virus was first discovered from a febrile primate from the Zika forests of Uganda in 1947 and the first human case was documented in 1954. The nonspecific clinical manifestations of ZIKV pose diagnostic dilemmas and delays early and effective treatment. Dental professionals should have a thorough knowledge about the virus and should follow standard infection control measures as the virus has been demonstrated in various body secretions (including salivary secretions). The disease is managed by symptomatic and supportive care and no vaccine exist till date. Recent ZIKV outbreaks and increase association of microcephaly with congenital ZIKV and neurological complications (Guillain-Barré syndrome) has drawn global public health attention. The World Health Organization declared it a public health emergency of international concern in 2016. This review article provides a detailed overview on ZIKV; it is clinical and oral manifestations, diagnostic aids, differential diagnosis, preventive aspects, and management protocol.
KEYWORDS: Guillain-Barré syndrome, microcephaly, pregnancy, public health menace, zika virus
INTRODUCTION
Zika virus (ZIKV) is a single-stranded RNA virus and belongs to the Flavivirus genus and Flaviviridae family.[1,2] Phylogenetically, ZIKV is linked to African and the Asian lineage, with the latter related to the recent Latin American epidemic.[3,4] The year of 1947 marks the isolation of ZIKV from a surveillant macaque in the course of yellow fever surveillance in Uganda's Zika forests, thus, deriving the name of the virus.[5] Soon after, the virus was isolated in the same forest in Aedes africanus mosquitoes.[6]
In Africa, the life cycle of ZIKV usually involves propagation between the various simian species (such as apes and monkeys) and mosquito vectors, with humans being the infrequent accidental hosts. However, in the Asian subcontinent, humans have probably become the main host.[7,8] Infrequently, ZIKV transmission may also occur through various nonmosquito modes such as perinatal,[9] congenital,[10] and sexual.[11] There have also been reported the incidence of the spread of ZIKV by blood transfusion,[12,13] animal bites,[14] and laboratory exposure.[15]
The two major forms of ZIKV infection are-Zika fever and congenital ZIKV syndrome. Zika fever has nonspecific manifestations ranging from asymptomatic infections (80% of cases) to a self-limiting febrile sickness. The sign and symptoms mimic a “dengue-like” syndrome with low-grade fever, bilateral nonpurulent conjunctivitis, maculopapular exanthem, retro-orbital pain, headache, arthritis/arthralgia with small joint edema, myalgia, asthenia, and vertigo. Congenital Zika syndrome most frequently manifest as microcephaly.[16,17,18,19,20]
The laboratory diagnosis of ZIKV infection is confirmed by the demonstration of viral RNA using reverse transcriptase-polymerase chain reaction (RT-PCR) and viral detection.[5]
Until date, there exists no definitive treatment or vaccination for ZIKV. The principal preventive methods for ZIKV spread are as avoidance of insect bites along with abstinence and barrier protection to avoid ZIKV dissemination through sexual mode (especially during pregnancy).[21] Universal precautions are an absolute mandate, particularly necessary until the time a complete knowledge is attained regarding the possible means of ZIKV dissemination.[22]
ZIKV has emerged as a public health menace owing to its implacable geographic dissemination, along with a distressing increased incidence of congenital ZIKV infections (manifesting as microcephaly), and serious neurological complications.[23]
Various schemes and policies are being implemented by Government and Public Health Agencies to combat ZIKV infection and possible complications. The “World Health Organization (WHO) Zika App” has been launched of late by the WHO to enhance the awareness and understanding of this public health disaster.[24]
TRANSMISSION
In urban and suburban settings, ZIKV dissemination involves human – mosquito – human cycle, with Aedes species mosquitoes as the most important vectors.[12] Aedes species are primarily daytime biting mosquitoes. The viral dissemination occurs through the blood-sucking mosquitoes which have a predilection for salivary glands. The virus multiplies in the salivary glands and persists there all its life. Few other mammals, such as elephants, zebras, and rats, may also serve as the likely ZIKV pool.[25]
ZIKV has a predisposition to occur in any natural habitat of the Aedes mosquito vector.[5,26] The virus has been identified in various mosquito species namely - Aedes aegypti, Aedes albopictus, Aedes furcifer, Aedes africanus, Aedes apicoargenteus, Aedes luteocephalus, and Aedes vittatus.[27,28,29,30]
Table 1 depicts the various mosquito species and their peculiar features.[7,31,32,33,34,35,36,37]
Table 1.
Various mosquito species associated with Zika virus
| Mosquito species | Features |
|---|---|
| Aedes hensilii | Yap island Zika virus epidemic (2007)[31] |
| Ae. Aegypti | Brazil Zika virus epidemic (2015)[32] |
| Aedes africanus | Uganda Zika virus epidemic[33,34] |
| Aedes. aegypti and Aedes albopictus | Zika virus vector in Asian continent[7] |
| Ae. Albopictus | Invasive mosquito species as it can be easily carried to other geographic regions[35] Adaptable to both urban and sylvatic habitats[36] Alleged linkage for yellow fever virus in Brazil[37] |
NONMOSQUITO TRANSMISSION
Although mosquitoes serve as the primary vector agency for ZIKV spread, various nonvector means of virus spread have also been proposed.
Sexual mode of ZIKV spread has been suggested by Foy et al. in 2011. The patient contracted the infection in Senegal and got his wife infected via unprotected sex on his visit to the US.[38] Sexual mode of ZIKV spread has been reinforced by the fact that the viral RNA can be detected in the semen even after 17 days of acute illness and 62 days after the symptoms sets in.[11,39] ZIKV demonstration from the semen emphasize the avoidance of unprotected sexual practices and necessitates condom usage (primarily throughout pregnancy), thus preventing ZIKV spread by sexual mode.[40]
ZIKV spread via perinatal route has attracted significant attention due to an alarming increase in microcephaly cases in congenital ZIKV-infected newborns. Isolation of ZIKV RNA from the maternal serum up to 5 days following childbirth and in the young infant up to 6 days, reinforce the perinatal mode of ZIKV spread.[10]
Transfusion with contaminated blood and blood products has also been suggested as a likely mode of ZIKV spread. Demonstration of ZIKV RNA in roughly 3% of asymptomatic blood donors during the French Polynesian outbreak, have supported this mode of disease transmission.[12]
Till date, there is no published literature reporting ZIKV spread through saliva. However, the viral RNA has been demonstrated in saliva during the acute infectious phase. 20 ZIKV RNA concentration was found to be greater in saliva than in blood[20,41] and was equal to that present in urine.[41] Salivary detection of ZIKV requires considerable attention, especially in dental clinics, where salivary contact is frequent with droplets and aerosol generation during varied dental procedures.[42]
ZIKV RNA has also been identified in breast milk, amniotic fluid, placental or fetal tissues; although, there has been no published evidence of ZIKV spread via these routes.[24]
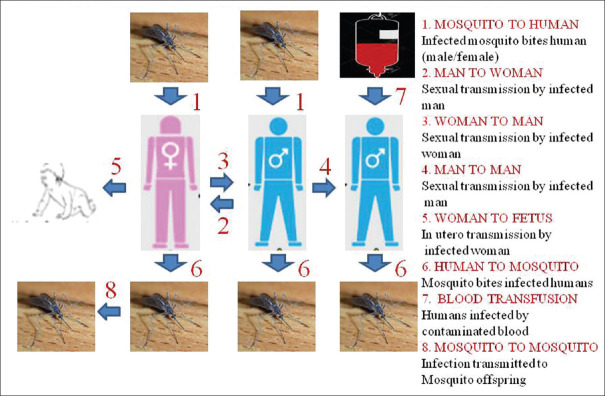
Figure 1 depicts the possible modes of ZIKV transmission.
Figure 1.
Possible modes of Zika virus transmission
EPIDEMIOLOGY
History of ZIKV isolation and detection goes back to the year 1947, where a febrile sentinel monkey acquired this virus during the surveillance of yellow fever virus in Zika forests of Uganda.[5,43,44]
The first human case of ZIKV infection was documented in Nigeria and Tanzania during 1952–1954. Further, ZIKV dissemination to the Asian subcontinent alarmed the public health officials about the impending likelihood of ZIKV epidemics.[44,45]
The year of 2007 marks the documentation of the first epidemic outburst of ZIKV from Yap State, Federated States of Micronesia. More than 49 confirmed ZIKV infected patients presented maculo-papular exanthema (rash), bilateral nonpurulent conjunctivitis and arthralgia over the 13 weeks duration of the epidemic.[31] An additional ZIKV epidemic outburst was recognized in the French Polynesian population in 2013, marking the first documentation of ZIKV and Guillain-Barré syndrome (GBS). However, majority of the affected population presented with mild manifestations.[46,47]
Soon, the ZIKV cases were noticed in Canada, Germany, Japan, Italy, Australia, the United States, and Easter Island (Chile-Pacific Ocean).[45] The virus got introduced to Brazil and Latin American sub-continent in April 2015, marking the third reported epidemic of ZIKV.[48,49]
The first incidence of microcephaly with ZIKV was documented in October 2015 in Brazil. ZIKV was affirmed a public health emergency of international concern by the WHO in February 2016 due to alleged linkage with microcephaly and varied neurologic complications.[50]
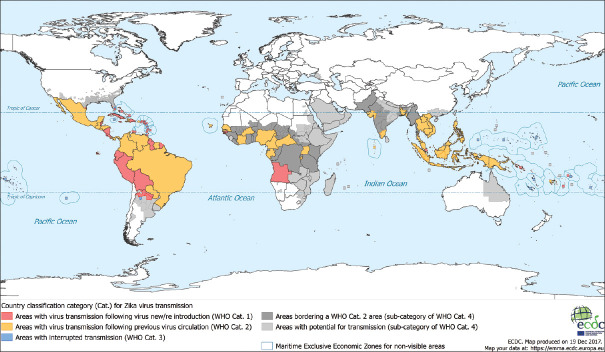
Data till February 2, 2017, revealed that vector-borne transmission of ZIKV has been documented in 70 countries.[51]
Figure 2 shows geographical representation of areas ZIKV dissemination.
Figure 2.
Geographical distribution of Zika virus
Table 2 depicts summary of the historical milestones of ZIKV discovery and epidemics.[52]
Table 2.
Historical milestones of Zika virus
| Year | ZIKV feature | Affected population |
|---|---|---|
| 1947 | ZIKV was first discovered in Zika forests of Uganda | |
| 1952 | ZIKV first human infection in Nigeria | |
| 2007 | First epidemic in Yap island, Micronesia | 49 confirmed cases |
| 2008 | First Sexually transmitted case of Zika virus | |
| 2013 | Second epidemic in French Polynesia | >400 cases |
| 2013 | First reported case of Zika virus with Guillain-Barré syndrome | |
| 2015 | Third epidemic in South America | >1.5 million cases |
| October 2015 | First incidence of microcephaly with ZIKV | |
| February 2016 | WHO declared ZIKV a public health emergency of International Concern |
ZIKV=Zika virus, WHO=World Health Organization
PATHOGENESIS
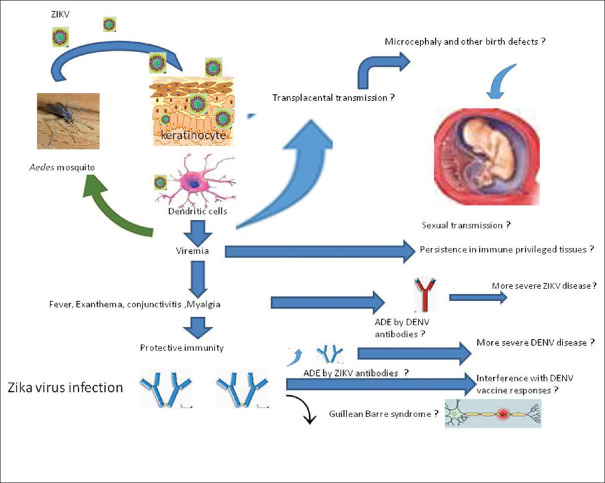
Although the exact pathogenetic mechanism is not clearly elicited, the general consensus proposes that replication of ZIKV takes place in skin dendritic cells after inoculation following the mosquito bite.[26]
The infection further gets disseminated through the bloodstream to the adjacent lymph nodes and other body organs such as myocardium, central nervous system, skeletal muscles, and to the fetus. Viral replication in astroglia and neuronal cells of infected mice brain causes neuronal degeneration, cellular infiltration, and alleviation in the brain, thus explaining ZIKV neurotropism and the related neurological complications (microcephaly in congenital ZIKV infection).[17]
Viremia usually occurs within 3–4 days of the onset of symptoms. 26 Viral RNA can be demonstrated in the bloodstream from the day of disease onset and may remain present till the 11th day of illness.[53]
Figure 3 shows the pathogenesis of ZIKV.
Figure 3.
Pathogenesis of Zika virus
CLINICAL FEATURES AND DIFFERENTIAL DIAGNOSIS
The clinical spectrum of ZIKV infection mimics that of dengue and Chikungunya viral infection (especially during the acute phase), thus necessitating differentiation between these three entities.[54]
About 80% of infections are asymptomatic, thus, posing a diagnostic dilemma and a barrier to the prevention of disease transmission.[55] In general, clinical symptoms appear within 3–12 days of insect bite and resolves in 2–7 days.[31] About 20% of cases present with mild, bizarre, self-limiting manifestations, mimicking other arbovirus infections, thus delaying the accurate diagnosis and treatment protocol.[56]
The most frequently manifesting feature is a macular or maculopapular exanthema (seen in 90% of cases). The rash has a characteristic centrifugal pattern (extends from the trunk to the extremities), often pruritic and persist for a period of 4–5 days.[31,56,57] The typical rash of ZIKV is usually seen within the 1st or 2nd day after the symptoms sets in. This is in contrast to the rash in dengue and Chikungunya, which usually appears after 4 days of clinical symptoms.[58] Other uncommon cutaneous features are as follows: subcutaneous hematomas, ecchymosis, petechiae, aphthous ulcers, and other ulcerative oral mucosal lesions.[58]
Low-grade fever (usually lower than 38°) and fatigue may precede the cutaneous exanthema (rash) in about 65%–70% of cases. The fever usually persists for 1–4 days to a maximum of 7 days.[57,59] Arthralgia accounts for the third most frequently occurring manifestation (seen in 65% of cases). About 20%–45% of patients present with periarticular edema, especially of small joints (hands and feet, and less frequently knees and wrists) in association with Arthralgia, which may last for a week up to a month.[57]
About 55%–60% of patients may present with bilateral, nonpurulent conjunctivitis, which usually shows resolution within 1–2 weeks.[31,57]
ZIKV may also present with uncommon manifestations such as a headache, retro-orbital pain and myalgia.[57] ZIKV is associated with less intense muscle and joint pain as compared to severe intense myalgia of chikungunya infection.[31] Localized or generalized lymphadenopathy may also be seen in a few cases of ZIKV infection.[57]
Criteria defining the suspected and confirmed cases of ZIKV infection by the Brazilian health ministry are:[60]
-
Suspected case: patients presenting with pruritic maculopapular exanthema, in addition to two or more of the following features:
- Fever
- Nonpurulent conjunctivitis and pruritus
- Arthralgia of multiple joints (polyarthralgia)
- Periarticular edema.
-
Confirmed case: features of a suspected case along with either one of the following positive test or demonstration of a particular response for ZIKV evaluation:
- Viral RNA identification
- RT technique demonstrating ZIKV RNA
- Immunoglobulin M (IgM) serological reaction (may exhibit false positive reaction if a dengue virus infection co-exists)
- Confirming ZIKV acute cases by incorporating various clinical-epidemiological measures.
ZIKV infection is usually mild and severe forms are rarely encountered from earlier reported epidemics. This supports the infrequent rate of hospitalizations and death rates with ZIKV.[31,61]
Table 3 depicts differentiating features of Zika, dengue, and chikungunya.
Table 3.
Differentiating features of Zika, Dengue, and Chikungunya
| Features | Dengue | Zika | Chikungunya |
|---|---|---|---|
| Incubation period | 3-14 days | 3-12 days | 1-12 days |
| Etiology | RNA virus belongs to the genus Flavivirus of family Flaviviridae. (4 different serological types exists - DENV 1, 2, 3 and 4) Mostly, Infection with one serotype Leads to lifelong immunity against the same type. However, occasionally, exposure of the individual to a second type of dengue virus Leads to a very severe form of illness (dengue shock syndrome and dengue hemorrhagic fever) | RNA virus belongs to the genus Flavivirusof family Flaviviridae. Lifelong immunity after infection with one type has not been reported in Zika virus infections | RNA virus of genus Alphavirusof the family Togaviridae |
| Fever (duration) | Higher (≥40°) +++ Lasts for 4-7 days |
Lower (≤38.5) ++ Lasts for 1-2 days |
High fever++Lasts for 2-3 days |
| Rash (maculopapular exanthema) | Moderately elevated + |
Elevated +++ |
Moderately elevated ++ |
| Headaches | Frequent and high intensity +++ | Frequent and moderate intensity + | Frequent and moderate intensity + |
| Arthralgia | Mild | Mild/moderate | Frequent and in multiple joints +++ |
| Nausea and vomiting | Seen | Unusual | Unusual |
| Blood dyscrasias (shock and thrombocytopenia) | +++ | +/_ | +/_ |
| Non-purulent conjunctivitis | + | +++ | ++ |
| Peripheral edema | _ | + | _ |
| lymphadenopathy | ++ | + | ++ |
| Neurological complications | Encephalitis | Guillain-Barré syndrome and encephalitis | Guillain-Barré syndrome and encephalitis (especially in neonates) |
| Course of disease | Mostly, dengue infection is benign and limited to fever during the acute phase followed by a Gradual return to normal. Occasionally, after exposure to secondary serological type of dengue, there are three distinct phases of disease: an acute febrile phase, a critical (plasma leak) phase where hematologic abnormalities, shock and death can occur, and a recovery phase | Usually self-limiting (2-7 days) | The illness is usually self-limiting and resolves with time. However, preexisting signs of chronic joint disease and other causes of chronic rheumatism predispose patients to chronicity of chikungunya infection |
| Hospitalization | Secondary dengue infection often requires hospitalization and 2.5% of infected individuals will develop a lethal illness | Most cases are managed on an outpatient basis | Patients with severe chikungunya fever requiring hospitalization tend to be older and have comorbidities such as cardiovascular, neurologic, and respiratory disorders or diabetes |
| Role of NSAIDS | NSAIDS can increase risk of bleeding | Acceptable to use in Zika virus infection as long as dengue has been excluded | Taking nonsteroidal anti-inflammatory drugs may reducethe symptoms of fever and pain |
| Neutropenia | ++ | Not demonstrable | + |
| Lymphopenia | ++ | Not demonstrable | +++ |
NSAIDS=Nonsteroidal anti-inflammatory drugs. +: Mild, ++: Moderate, +++: Severe, +/-: May or may not be present
The oral manifestations in ZIKV are not a frequent occurrence; although, Foy et al. have reported oral aphthous ulcers on the lip mucosa.[38] Aphthous ulcers were also a frequent oral feature during the 2013 French Polynesian epidemic. However, the data supporting other oral features in ZIKV infection is scarce.[62,63] Hyperemia and petechial lesions on the hard palate of ZIKV-infected patient were documented by Brasil et al.[64]
Lin H Chen and Derrington also described petechial palatal lesions; vesicles, or aphthous ulcerations in a ZIKV-infected patients.[65,66]
Thorough and advanced researches are necessary to demonstrate the various oral features of ZIKV. Saliva may have a significant function in the human-to-human spread of ZIKV and salivary diagnostics may serve as an important investigative tool for ZIKV infection.[67]
Table 4 depicts summary of reported orofacial features in ZIKV infection.
Table 4.
Summary of reported orofacial features in Zika virus infection
| Author and year | Reported orofacial feature |
|---|---|
| Foy et al., 2011 | Aphthous ulcers on lip mucosa |
| Brasil et al., 2016 | Local hyperemia and petechiae on the hard palate |
| Derrington et al., 2016 | Palatal petechiae |
| Mondolfi et al., 2018 | Petechial lesions on the hard palate of a female patient with acute Zika virus |
CONGENITAL ZIKA SYNDROME
ZIKV has drawn global public health attention due to its alleged linkage with the increasing incidence of microcephaly. In September 2015, increased frequency of microcephalic babies was documented in females residing in ZIKV endemic regions of Brazil, thus, raising the question of a probable association. Thereafter, a total of 2366 confirmed cases of microcephaly associated with ZIKV infection have been noted in Brazil.[68]
In cases of microcephaly, the headoccipto-frontal circumference dimensions are more than two standard deviations lower than the mean for age and sex. The proportionally smaller brain of these individuals account for the varying degree of intellectual disability.[69]
Microcephaly occurs during the neuronal proliferation phase in the initial stages of pregnancy (3–4 months) and may correspond to the infectious symptoms in the mother. Various proposed mechanisms for microcephaly in ZIKV infection are: (1) Increased occurrence of microcephaly cases associated with ZIKV epidemics (2) 2 Documented cases of pregnant females with features coherent with ZIKV infection, fetal microcephaly, and RT-PCR showing ZIKV positivity in amniotic fluid.[70]
NEUROLOGICAL COMPLICATIONS
GBS refers to a polyneuropathy of acute onset. More than two-thirds of the reported cases have an underlying infectious etiology.[71] In July 2015, neurological features were documented in Brazilian patients with a recent history of ZIKV infection in the Bahia state. 26 patients out of the 42 established GBS patients had features coherent with ZIKV infection.[61]
LABORATORY DIAGNOSIS
As ZIKV infection presents with atypical features, mimicking other arboviral infections, clinical assessment alone is unpredictable and definitive diagnosis is based on laboratory parameters. Patients presenting with acute onset fever, cutaneous exanthema, myalgia, or arthralgia after recent (previous 2 weeks) trip to a ZIKV endemic region should be assessed simultaneously for ZIKV infection.[56]
Laboratory diagnosis of ZIKV infections mostly relies on molecular biology and serology.[53,72] Viral RNA isolation from clinical samples (blood, urine) forms the confirmatory laboratory diagnosis for ZIKV. Viral RNA may be demonstrated from blood samples up to 1–5 days after the onset of symptoms.[73,74] The diagnosis should not be excluded even in cases of negative results because the RT-PCR has a sensitivity of 40%.
As the virus remain present in the urine for a relatively long period, individuals examined after 5 days of infection must undertake RT-PCR test. The RT-PCR may be employed up to 15 days after the onset of signs and symptoms.[73,74]
ELISA technique (IgM and IgG) or plaque-reduction neutralization test constitutes the basic serological tests for ZIKV. These tests must be performed and interpreted with caution, particularly in previous dengue virus-infected individuals, possibly due to cross-reactive reactions.[53]
Serological assays may demonstrate IgM and IgG antibodies from the 4th to 12th day of ZIKV infection, respectively.[73,74]
PREVENTION OF ZIKA VIRUS INFECTIONS
MOSQUITO CONTROL MEASURES
Mass community education regarding the safety measures for insect bite and controlling mosquito vector is extremely essential. Involvement of the homeowners to minimize mosquito breeding environment may serve as an essential preventive method.[75]
INSECT BITE PRECAUTIONS
Preventive measures against mosquito bite should be employed in the natural habitats of Aedes mosquito species. Various precautionary measures to prevent day time insect bites are:
Preventing skin exposure (staying covered with long-sleeved shirts, pants, and hats)
Wearing light-colored clothing
Treat clothing with permethrin
Use of mosquito repellents-Icaridin has been used as the repellent of choice for adults and pregnant women (providing 10 h protection). Use of mosquito nets
The use of air-conditioning
Staying indoors with protective barriers against mosquito entry, especially during sunset and dawn.[24,45,76]
VECTOR SOURCE CONTROL
The prevention of accumulation of stagnant water in dark automobile tires and plants (preferred mosquito breeding sites); mosquito larvae areas to be sprayed and debris removal are the few vector source control measures that need to be undertaken.[77] Climatic changes (global warming and changes in humidity or rainfall) may also play a role in predicting vector abundance. Previous reported studies have suggested that rainfall had a positive and negative predilection on ZIKV and dengue isolation, respectively.[78]
Various preventive measures to mitigate the mosquito population are summarized in Table 5.[79]
Table 5.
Summary of various preventive measures to mitigate mosquito population
| Method | Mechanism | Application method | |
|---|---|---|---|
| 1 | Organophosphates | Larvicide; neurotoxic | Liquid or granules applied to aquatic habitat |
| 2 | Bti | Larvicide; larvae eat spores, cause larvae to stop eating | Liquid or granules applied to aquatic habitat |
| 3 | Surface oils (e.g., CocoBear™) | Larvicide; cuts off access to surface air | Liquid or granules applied to aquatic habitat |
| 4 | Hormone regulators (S-methoprene) | Larvicide; disrupts development | Liquid or granules/briquettes applied to aquatic habitat |
| 5 | Mosquitofish (Gambusia) | Larval predator | Fish released into mosquito producing water sources |
| 6 | Copepods | Larval predator | |
| 7 | Organophosphates | Adulticide; neurotoxic | Liquid spray, truck/aircraft/backpack |
| 8 | Pyrethroids | Adulticide; neurotoxic | Liquid spray |
| 9 | Wolbachia pipientis | Naturally occurring bacteria, renders mosquitoes unable to transmit RNA viruses or shortens lifespan | Release of treated mosquitoes with Wolbachia transmission to the offsprings |
| 10 | Sterile insect release | Laboratory-raised mosquito are sterilized via irradiation | Release of sterilized male mosquitoes |
| 11 | Genetically altered mosquitoes | Various mechanisms | Release of treated male mosquitoes |
| 12 | Traps | Oviposition or adult traps | Deploy traps with attractants |
| 13 | Reduction of breeding habitat (automobile tyres) | Reduce standing water | Reducing man-made containers, draining flood water, etc. |
Bti=Bacillus thuringiensis israelensis
Other preventive measures include avoiding a visit to Zika endemic areas and transfusion-related ZIKV spread, and adopting safe sexual practices using condoms.[24]
A thorough screening of donors should be done by employing a validated RT-PCR to demonstrate the ZIKV in semen.[80]
Table 6 shows the UK guidelines on preventing sexual transmission of ZIKV.[51]
Table 6.
UK guidelines on preventing sexual transmission of Zika virus
| Population group exposed to ZIKV (by travel or sexual contact) | Recommended period of abstinence/safe sex practice |
|---|---|
| Pregnant women and their sexual partners | If both partners, or just the male, have travelled to an area with moderate or high risk of Zika transmission, barrier methods or abstinence should be practised for the duration of the pregnancy |
| If only the female partner has been exposed, barrier methods or abstinence should be practiced for 8 weeks | |
| Women planning pregnancy or of child-bearing age and their sexual partners | Avoid conception while travelling to an area with moderate or high risk of Zika transmission and: For 8 weeks from last possible exposure if the woman alone travelled (asymptomatic and symptomatic) For 6 months from last possible exposure if the male partner/both partners travelled (asymptomatic and symptomatic) |
Border quarantine (screening of travelers at airports and the border) may serve as an important preventive tool for ZIKV infection import. However, border quarantine is associated with low detection rate as >80% of cases are asymptomatic.[81,82]
Implementation of universal infection control strategies may play an essential role in preventing the spread of ZIKV in healthcare background, including dental settings.[24]
The center for diseases control has proposed intervening measures for assessment of newborns with congenital ZIKV infection. The guidelines comprise serial monitoring of fetal ultrasounds and the evaluation of mothers for ZIKV infection. ZIKV evaluation is suggested in following cases: (1) infants with microcephaly or intracranial calcifications born to women who traveled to or reside in an area with ZIKV transmission while pregnant or (2) infants born to mothers with positive or inconclusive test results for ZIKV infection.[83]
PHARMACOLOGICAL INTERVENTION
One of the major challenges to combat ZIKV is the lack of a ZIKV vaccine. However, extensive researches are being carried out on ZIKV vaccine development by the Butantan laboratory in San Paulo, Brazil in collaboration with two other institutions of Brazil and US health ministry.[24]
Numerous candidate vaccines have progressed to the stage of clinical assessment. In brief, four types of vaccines, namely, three DNA, one modified RNA, four purified formalin-inactivated virus, and one live measles-vectored vaccine have advanced to phase 1 clinical trial.[84,85,86]
GENETIC ADJUSTMENTS TO DIMINISH VECTOR GROWTH
The published research of 1991 dealt with genetic isolation of A. aegypti mosquito phenotype, showing resistance to flavivirus infection.[87] Detection of resistant versus susceptible mosquito phenotypes may demonstrate genetic disparity. The induction of strains that are nonsusceptible to infection and also do not cause viral dissemination into the mosquito breeding sites may serve as a probable mode to alleviate the ZIKV transmission. Although, this is still a conceptual idea, inherited adjustment of wild type Aedes species might show promising results to mitigate the universal dissemination of infection.
Another prospective outlook is the introduction of genetically modified or genetically engineered male mosquitoes lacking the potential to produce progeny in the insect infiltrated domains, thus reducing the mosquito population. For example, introduction of genetically engineered GE OX513A A. aegypti mosquitoes incapable to produce progency, thus, curbing their wildlife populations.[88]
MEDICATIONS
Conducted researchers have demonstrated that Amotosalen and ultraviolet light A may inactivate ZIKV in vitro. The use of these medications may also result in a decreased amount of replicative virus, thus showing the way to the discovery of effective anti-ZIKV drugs.[89]
TREATMENT
The management of ZIKV mainly relies on the supportive and symptomatic therapy,[90,91] and till date, no antiviral medications for ZIKV exist. The management protocol entails complete bed rest, antipyretics for fever, hydration and nutritional therapy, along with monitoring the features of coagulopathies and multi-organ dysfunction.[92]
Acetaminophen is the preferred antipyretic for fever. Prescribing Aspirin and other nonsteroidal anti-inflammatory drugs in ZIKV is usually not acceptable, but may be prescribed cautiously after eliminating dengue virus infection (avoidance of hemorrhagic complications).[76] Aspirin should be avoided in pregnancy beyond the 32nd week of gestation due to possible premature arterial duct closure and young children (<12 years) to prevent the risk of Reye's syndrome.[76,93]
Antihistaminics may prove useful in controlling itching in patients with an exanthematous rash. Suspected cases of ZIKV infection must be shielded from additional insect contact through the initial infectious phase, thus, preventing other mosquito vectors from getting infected and limiting the local spread of disease.[76]
Few patients may require intravenous (IV) hydration therapy along with oxygen administration and monitoring of vital signs. Rarely, patients present with features of sepsis and multi-organ failure (coagulopathies, hepatic, and renal failure), thus necessitating intensive care admission.[47]
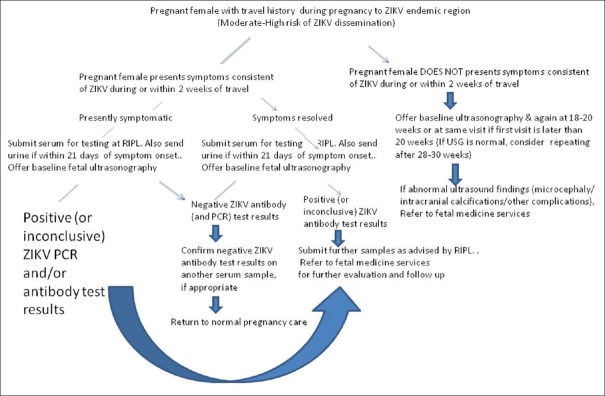
Pregnant female with a positive laboratory test for ZIKV should be immediately referred to an expert gynecologist or infectious disease specialist. Review of fetal ultrasounds to monitor fetal growth and malformations make an essential mandate of the high-risk prenatal care.[94]
GBS patients necessitate intensive care unit admission due to the possible development of paralysis of respiratory muscles. The management protocol for GBS involves the use of plasmapheresis or hyperimmune IV IG (hyperimmune). These modalities are costly but diminish the revival time.[95]
Figure 4 shows the evaluation of pregnant female with a travel history to regions with moderate-to-high risk of ZIKV transmission.[51]
Figure 4.
Evaluation of pregnant female with a travel history to regions with moderate-high risk of Zika virus transmission
CONCLUSION
ZIKV was a neglected tropical disease over the last 50 years (since its isolation in 1947). The disease is mainly transmitted through mosquito vector, although, various nonmosquito modes of spread are also known, with the virus being detected in body fluids (semen, saliva, urine, and breast milk). Therefore, preventive measures including vector control, prevention of insect bite, abstinence and use of condoms, avoiding travel to ZIKV endemic regions play an important role. Adopting universal infection control methods may significantly prevent dissemination in oral health-care settings. Recent advancements are being carried out in the form of effective ZIKV vaccine and anti-ZIKV drugs. However, Rapid geographic dissemination, nonspecific clinical presentation, lack of vaccine, and specific diagnostic test are the possible challenges to combat this dreaded public health menace.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
REFERENCES
- 1.Tetro JA. Zika and microcephaly: Causation, correlation, or coincidenceXS? Microbes Infect. 2016;18:167–8. doi: 10.1016/j.micinf.2015.12.010. [DOI] [PubMed] [Google Scholar]
- 2.Choumet V, Desprès P. Dengue and other Flavivirus infections. Rev Sci Tech. 2015;34:473. [PubMed] [Google Scholar]
- 3.Wang L, Valderramos SG, Wu A, Ouyang S, Li C, Brasil P, et al. From mosquitos to humans: Genetic evolution of Zika virus. Cell Host Microbe. 2016;19:561–5. doi: 10.1016/j.chom.2016.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pettersson JH, Eldholm V, Seligman SJ, Lundkvist Š, Falconar AK, Gaunt MW, et al. How did Zika virus emerge in the pacific islands and Latin America? MBio. 2016;7 doi: 10.1128/mBio.01239-16. pii: e01239-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ioos S, Mallet HP, Leparc Goffart I, Gauthier V, Cardoso T, Herida M, et al. Current Zika virus epidemiology and recent epidemics. Med Mal Infect. 2014;44:302–7. doi: 10.1016/j.medmal.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 6.Dick GW, Kitchen SF, Haddow AJ. Zika virus. I. Isolations and serological specificity. Trans R Soc Trop Med Hyg. 1952;46:509–20. doi: 10.1016/0035-9203(52)90042-4. [DOI] [PubMed] [Google Scholar]
- 7.Haddow AD, Schuh AJ, Yasuda CY, Kasper MR, Heang V, Huy R, et al. Genetic characterization of Zika virus strains: Geographic expansion of the Asian lineage. PLoS Negl Trop Dis. 2012;6:e1477. doi: 10.1371/journal.pntd.0001477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodriguez-Morales AJ, Bandeira AC, Franco-Paredes C. The expanding spectrum of modes of transmission of Zika virus: A global concern. Ann Clin Microbiol Antimicrob. 2016;15:13. doi: 10.1186/s12941-016-0128-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oliveira Melo AS, Malinger G, Ximenes R, Szejnfeld PO, Alves Sampaio S, Bispo de, Filippis AM, et al. Zika virus intrauterine infection causes fetal brain abnormality and microcephaly: Tip of the iceberg? Ultrasound Obstet Gynecol. 2016;47:6–7. doi: 10.1002/uog.15831. [DOI] [PubMed] [Google Scholar]
- 10.Besnard M, Lastere S, Teissier A, Cao-Lormeau V, Musso D. Evidence of perinatal transmission of Zika virus, French Polynesia, December 2013 and February 2014. Euro Surveill. 2014;19 pii: 20751. [PubMed] [Google Scholar]
- 11.Musso D, Roche C, Robin E, Nhan T, Teissier A, Cao-Lormeau VM, et al. Potential sexual transmission of Zika virus. Emerg Infect Dis. 2015;21:359–61. doi: 10.3201/eid2102.141363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Musso D, Nhan T, Robin E, Roche C, Bierlaire D, Zisou K, et al. Potential for Zika virus transmission through blood transfusion demonstrated during an outbreak in French Polynesia, November 2013 to February 2014. Euro Surveill. 2014;19 doi: 10.2807/1560-7917.es2014.19.14.20761. pii: 20761. [DOI] [PubMed] [Google Scholar]
- 13.US Food and Drug Administration. Recommendations for Donor Screening, Deferral, and Product Management to Reduce the Risk of Transfusion Transmission of Zika Virus, Recommendations for Industry. US Food and Drug Administration. 2016 Feb 16; [Google Scholar]
- 14.Leung GH, Baird RW, Druce J, Anstey NM. Zika virus infection in Australia following a monkey bite in Indonesia. Southeast Asian J Trop Med Public Health. 2015;46:460–4. [PubMed] [Google Scholar]
- 15.Simpson DI. Zika virus infection in man. Trans R Soc Trop Med Hyg. 1964;58:335–8. [PubMed] [Google Scholar]
- 16.Ginier M, Neumayr A, Günther S, Schmidt-Chanasit J, Blum J. Zika without symptoms in returning travellers: What are the implications? Travel Med Infect Dis. 2016;14:16–20. doi: 10.1016/j.tmaid.2016.01.012. [DOI] [PubMed] [Google Scholar]
- 17.Chan JF, Choi GK, Yip CC, Cheng VC, Yuen KY. Zika fever and congenital Zika syndrome: An unexpected emerging arboviral disease. J Infect. 2016;72:507–24. doi: 10.1016/j.jinf.2016.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Calvet GA, Filippis AM, Mendonça MC, Sequeira PC, Siqueira AM, Veloso VG, et al. First detection of autochthonous Zika virus transmission in a HIV-infected patient in Rio De Janeiro, Brazil. J Clin Virol. 2016;74:1–3. doi: 10.1016/j.jcv.2015.11.014. [DOI] [PubMed] [Google Scholar]
- 19.Gautret P, Simon F. Dengue, chikungunya and Zika and mass gatherings: What happened in Brazil, 2014. Travel Med Infect Dis. 2016;14:7–8. doi: 10.1016/j.tmaid.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 20.Musso D, Roche C, Nhan TX, Robin E, Teissier A, Cao-Lormeau VM, et al. Detection of Zika virus in saliva. J Clin Virol. 2015;68:53–5. doi: 10.1016/j.jcv.2015.04.021. [DOI] [PubMed] [Google Scholar]
- 21.Oster AM, Brooks JT, Stryker JE, Kachur RE, Mead P, Pesik NT, et al. Interim guidelines for prevention of sexual transmission of Zika virus – United States, 2016. MMWR Morb Mortal Wkly Rep. 2016;65:120–1. doi: 10.15585/mmwr.mm6505e1. [DOI] [PubMed] [Google Scholar]
- 22.Marano G, Pupella S, Vaglio S, Liumbruno GM, Grazzini G. Zika virus and the never-ending story of emerging pathogens and transfusion medicine. Blood Transfus. 2016;14:95–100. doi: 10.2450/2015.0066-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nunes ML, Carlini CR, Marinowic D, Neto FK, Fiori HH, Scotta MC, et al. Microcephaly And zika virus: A clinical and epidemiological analysis of the current outbreak in Brazil. J Pediatr (Rio J) 2016;92:230–40. doi: 10.1016/j.jped.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 24.Leão JC, Gueiros LA, Lodi G, Robinson NA, Scully C. Zika virus: Oral healthcare implications. Oral Dis. 2017;23:12–7. doi: 10.1111/odi.12512. [DOI] [PubMed] [Google Scholar]
- 25.Lindenbach BD, Rice CM. Molecular biology of flaviviruses. Adv Virus Res. 2003;59:23–61. doi: 10.1016/s0065-3527(03)59002-9. [DOI] [PubMed] [Google Scholar]
- 26.Hayes EB. Zika virus outside Africa. Emerg Infect Dis. 2009;15:1347–50. doi: 10.3201/eid1509.090442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marchette NJ, Garcia R, Rudnick A. Isolation of Zika virus from Aedes Aegypti mosquitoes in Malaysia. Am J Trop Med Hyg. 1969;18:411–5. doi: 10.4269/ajtmh.1969.18.411. [DOI] [PubMed] [Google Scholar]
- 28.Akoua-Koffi C, Diarrassouba S, Bénié VB, Ngbichi JM, Bozoua T, Bosson A, et al. Investigation surrounding a fatal case of yellow fever in Côte D'ivoire in 1999. Bull Soc Pathol Exot. 2001;94:227–30. [PubMed] [Google Scholar]
- 29.Fagbami A. Zika virus infections in Nigeria: virological and seroepidemiological investigations in Oyo state. J Hyg (Lond) 1979;83:213–9. doi: 10.1017/s0022172400025997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McCrae AW, Kirya BG. Yellow fever and Zika virus epizootics and enzootics in Uganda. Trans R Soc Trop Med Hyg. 1982;76:552–62. doi: 10.1016/0035-9203(82)90161-4. [DOI] [PubMed] [Google Scholar]
- 31.Duffy MR, Chen TH, Hancock WT, Powers AM, Kool JL, Lanciotti RS, et al. Zika virus outbreak on yap island, federated states of Micronesia. N Engl J Med. 2009;360:2536–43. doi: 10.1056/NEJMoa0805715. [DOI] [PubMed] [Google Scholar]
- 32.Cadu R, Harish T. Zika virus: a new global threat for 2016. Health. 2015;386:243–4. [Google Scholar]
- 33.Boorman JP, Porterfield JS. A simple technique for infection of mosquitoes with viruses; transmission of Zika virus. Trans R Soc Trop Med Hyg. 1956;50:238–42. doi: 10.1016/0035-9203(56)90029-3. [DOI] [PubMed] [Google Scholar]
- 34.Weinbren MP, Williams MC. Zika virus: Further isolations in the Zika area, and some studies on the strains isolated. Trans R Soc Trop Med Hyg. 1958;52:263–8. doi: 10.1016/0035-9203(58)90085-3. [DOI] [PubMed] [Google Scholar]
- 35.Juliano SA, Lounibos LP. Ecology of invasive mosquitoes: Effects on resident species and on human health. Ecol Lett. 2005;8:558–74. doi: 10.1111/j.1461-0248.2005.00755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.de Marques CC, Marques GR, Dégallier N. Is Aedes albopictus only a pest mosquito or also a vector of arboviruses in Brazil? In: Travassos da Rosa AP, Vasconcelos PF, Travassos da Rosa JF, editors. An Overview of Arbovirology in Brazil and Neighbouring Countries. Belém: Instituto Evandro Chagas; 1998. pp. 248–60. [Google Scholar]
- 37.Dibo MR, Menezes RM, Ghirardelli CP, Mendonça AL, Chiaravalloti Neto F. The presence of culicidae species in medium-sized cities in the state of São Paulo, Brazil and the risk of West Nile fever and other arbovirus infection. Rev Soc Bras Med Trop. 2011;44:496–503. doi: 10.1590/s0037-86822011000400019. [DOI] [PubMed] [Google Scholar]
- 38.Foy BD, Kobylinski KC, Chilson Foy JL, Blitvich BJ, Travassos da, Rosa A, Haddow AD, et al. Probable non-vector-borne transmission of Zika virus, Colorado, USA. Emerg Infect Dis. 2011;17:880–2. doi: 10.3201/eid1705.101939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Atkinson B, Hearn P, Afrough B, Lumley S, Carter D, Aarons EJ, et al. Detection of Zika virus in semen. Emerg Infect Dis. 2016;22:940. doi: 10.3201/eid2205.160107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.D'Ortenzio E, Matheron S, Yazdanpanah Y, de Lamballerie X, Hubert B, Piorkowski G, et al. Evidence of sexual transmission of Zika virus. N Engl J Med. 2016;374:2195–8. doi: 10.1056/NEJMc1604449. [DOI] [PubMed] [Google Scholar]
- 41.Bingham AM, Cone M, Mock V, Heberlein-Larson L, Stanek D, Blackmore C, et al. Comparison of test results for Zika virus RNA in urine, serum, and saliva specimens from persons with travel-associated Zika virus disease – Florida, 2016. MMWR Morb Mortal Wkly Rep. 2016;65:475–8. doi: 10.15585/mmwr.mm6518e2. [DOI] [PubMed] [Google Scholar]
- 42.Matthews A, Brown GC. Zika virus in the dental settings. Decis Dent. 2016;2:40–3. [Google Scholar]
- 43.Sikka V, Chattu VK, Popli RK, Galwankar SC, Kelkar D, Sawicki SG, et al. The emergence of Zika virus as a global health security threat: A Review and a consensus statement of the INDUSEM joint working group (JWG) J Glob Infect Dis. 2016;8:3–15. doi: 10.4103/0974-777X.176140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Macnamara FN. Zika virus: A report on three cases of human infection during an epidemic of jaundice in Nigeria. Trans R Soc Trop Med Hyg. 1954;48:139–45. doi: 10.1016/0035-9203(54)90006-1. [DOI] [PubMed] [Google Scholar]
- 45.Ministry of Health. Secretariat of Health Surveillance. Surveillance protocol and response to the occurrence of microcephaly related to Zika virus infection. Brasília: Ministry of Health; 2015. Department of Surveillance of Communicable Diseases; p. 55. [Google Scholar]
- 46.Hancock WT, Marfel M, Bel M. Zika virus, French Polynesia, South Pacific, 2013. Emerg Infect Dis. 2014;20:1960. doi: 10.3201/eid2011.141253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Oehler E, Watrin L, Larre P, Leparc-Goffart I, Lastere S, Valour F, et al. Zika virus infection complicated by Guillain-Barre syndrome – Case report, French Polynesia, December 2013. Euro Surveill. 2014;19 doi: 10.2807/1560-7917.es2014.19.9.20720. pii: 20720. [DOI] [PubMed] [Google Scholar]
- 48.Campos GS, Bandeira AC, Sardi SI. Zika virus outbreak, Bahia, Brazil. Emerg Infect Dis. 2015;21:1885–6. doi: 10.3201/eid2110.150847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cardoso CW, Paploski IA, Kikuti M, Rodrigues MS, Silva MM, Campos GS, et al. Outbreak of exanthematous illness associated with Zika, Chikungunya, and dengue viruses, Salvador, Brazil. Emerg Infect Dis. 2015;21:2274–6. doi: 10.3201/eid2112.151167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kindhauser MK, Allen T, Frank V, Santhana RS, Dye C. Zika: The origin and spread of a mosquito-borne virus. Bull World Health Organ. 2016;94:675–686C. doi: 10.2471/BLT.16.171082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Perry H, Khalil A, Aarons E, Russell K, O'Brien P. Management of Zika virus in pregnancy: A review. Br Med Bull. 2017;124:157–69. doi: 10.1093/bmb/ldx038v1. [DOI] [PubMed] [Google Scholar]
- 52.Abushouk AI, Negida A, Ahmed H. An updated review of Zika virus. J Clin Virol. 2016;84:53–8. doi: 10.1016/j.jcv.2016.09.012. [DOI] [PubMed] [Google Scholar]
- 53.Lanciotti RS, Kosoy OL, Laven JJ, Velez JO, Lambert AJ, Johnson AJ, et al. Genetic and serologic properties of Zika virus associated with an Epidemic, Yap state, Micronesia, 2007. Emerg Infect Dis. 2008;14:1232–9. doi: 10.3201/eid1408.080287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mardekian SK, Roberts AL. Diagnostic options and challenges for dengue and chikungunya viruses. Biomed Res Int. 2015;2015:834371. doi: 10.1155/2015/834371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lopes N, Nozawa C, Linhares REC. General features and epidemiology of emerging arboviruses in Brazil. Rev Pan Am Saude. 2014;5:55–64. [Google Scholar]
- 56.Plourde AR, Bloch EM. A literature review of Zika virus. Emerg Infect Dis. 2016;22:1185–92. doi: 10.3201/eid2207.151990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mallet H, Vial A, Musso D. Assessment of the zika virus outbreak in French Polynesia between October 2013 and March 2014. From the description of the outbreak to knowledge gained subsequently. Health, Epidemiological and Health Information Bulletin. 2015;20-21:367–73. [Google Scholar]
- 58.Mondolfi PA, Blohm GM, Hernandez-Perez M, Larrazabal A, Moya D, Marquez M, et al. Cutaneous features of Zika virus infection: a clinicopathological overview. Clin Exp Dermatol. 2019;44:13–9. doi: 10.1111/ced.13793. [DOI] [PubMed] [Google Scholar]
- 59.Waddell LA, Greig JD. Scoping review of the Zika virus literature. PLoS One. 2016;11:e0156376. doi: 10.1371/journal.pone.0156376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.De Oliveira WK, Cortez-Escalante J, De Oliveira WT, Carmo GM, Henrique CM, Coelho GE, et al. Increase in reported prevalence of microcephaly in infants born to women living in areas with confirmed Zika virus transmission during the first trimester of pregnancy – Brazil, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:242. doi: 10.15585/mmwr.mm6509e2. [DOI] [PubMed] [Google Scholar]
- 61.European Centre for Disease Prevention and Control. Rapid Risk Assessment: Zika Virus Epidemic in the Americas: potential Association with Microcephaly and Guillain-Barré Syndrome. Stockholm, Sweden: European Centre for Disease Prevention and Control; 2016. Feb 8, [Google Scholar]
- 62.Scully C, Robinson A. Check before you travel: Zika virus – Another emerging global health threat. Br Dent J. 2016;220:265–7. doi: 10.1038/sj.bdj.2016.182. [DOI] [PubMed] [Google Scholar]
- 63.Shakib K. Epidemic of Zika virus and maxillofacial surgery. Br J Oral Maxillofac Surg. 2016;54:355–7. doi: 10.1016/j.bjoms.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 64.Brasil P, Calvet GA, de Souza RV, Siqueira AM. Exanthema associated with Zika virus infection. Lancet Infect Dis. 2016;16:866. doi: 10.1016/S1473-3099(16)30117-7. [DOI] [PubMed] [Google Scholar]
- 65.Chen LH. Oral lesions in a patient with confirmed Zika virus infection. J Travel Med. 2018;25:1–2. doi: 10.1093/jtm/tay113. [DOI] [PubMed] [Google Scholar]
- 66.Derrington SM, Cellura AP, McDermott LE, Gubitosi T, Sonstegard AM, Chen S, et al. Mucocutaneous findings and course in an adult with Zika virus infection. JAMA Dermatol. 2016;152:691–3. doi: 10.1001/jamadermatol.2016.1433. [DOI] [PubMed] [Google Scholar]
- 67.Siqueira WL, Zuanazzi D, Khurshid Z, Khan RS, Oliverira TM, Paula K, et al. Oral clinical manifestations of patients infected with Zika virus. Oral Health. 2016:1–2. [Google Scholar]
- 68.World Health Organization. Zika Virus, Microcephaly and Guillain-Barre Syndrome Situation Report. World Health Organization. 2017 Feb 2; [Google Scholar]
- 69.De Carvalho NS, De Carvalho BF, Fugaça CA, Dóris B, Biscaia ES. Zika virus infection during pregnancy and microcephaly occurrence: A review of literature and Brazilian data. Braz J Infect Dis. 2016;20:282–9. doi: 10.1016/j.bjid.2016.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Marrs C, Olson G, Saade G, Hankins G, Wen T, Patel J, et al. Zika virus and pregnancy: A review of the literature and clinical considerations. Am J Perinatol. 2016;33:625–39. doi: 10.1055/s-0036-1580089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yuki N, Hartung HP. Guillain-Barré syndrome. N Engl J Med. 2012;366:2294–304. doi: 10.1056/NEJMra1114525. [DOI] [PubMed] [Google Scholar]
- 72.Faye O, Faye O, Diallo D, Diallo M, Weidmann M, Sall AA, et al. Quantitative real-time PCR detection of Zika virus and evaluation with field-caught mosquitoes. Virol J. 2013;10:311. doi: 10.1186/1743-422X-10-311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.World Health Organization. WHO Statement on the First Meeting of the International Health Regulations (2005) (IHR 2005) Emergency Committee on Zika Virus and Observed Increase in Neurological Disorders and Neonatal Malformations. World Health Organization. 2016 Feb 1; [Google Scholar]
- 74.Rabe IB, Staples JE, Villanueva J, Hummel KB, Johnson JA, Rose L, et al. Interim guidance for interpretation of Zika virus antibody test results. MMWR Morb Mortal Wkly Rep. 2016;65:543–6. doi: 10.15585/mmwr.mm6521e1. [DOI] [PubMed] [Google Scholar]
- 75.Healy K, Hamilton G, Crepeau T, Healy S, Unlu I, Farajollahi A, et al. Integrating the public in mosquito management: Active education by community peers can lead to significant reduction in peridomestic container mosquito habitats. PLoS One. 2014;9:e108504. doi: 10.1371/journal.pone.0108504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sampathkumar P, Sanchez JL. Zika virus in the Americas: A review for clinicians. Mayo Clin Proc. 2016;91:514–21. doi: 10.1016/j.mayocp.2016.02.017. [DOI] [PubMed] [Google Scholar]
- 77.Rodriguez-Morales AJ. Zika: The new arbovirus threat for Latin America. J Infect Dev Ctries. 2015;9:684–5. doi: 10.3855/jidc.7230. [DOI] [PubMed] [Google Scholar]
- 78.Althouse BM, Hanley KA, Diallo M, Sall AA, Ba Y, Faye O, et al. Impact of climate and mosquito vector abundance on sylvatic arbovirus circulation dynamics in Senegal. Am J Trop Med Hyg. 2015;92:88–97. doi: 10.4269/ajtmh.13-0617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Thompson SJ, Pearce JM, Ramey AM. Vectors, Hosts, and Control Measures for Zika Virus in the Americas. Eco Health. 2017;14:821–39. doi: 10.1007/s10393-017-1277-2. [DOI] [PubMed] [Google Scholar]
- 80.Baud D, Musso D, Vouga M, Alves MP, Vulliemoz N. Zika virus: A new threat to human reproduction. Am J Reprod Immunol. 2017;77:1–3. doi: 10.1111/aji.12614. [DOI] [PubMed] [Google Scholar]
- 81.Sato H, Nakada H, Yamaguchi R, Imoto S, Miyano S, Kami M, et al. When should we intervene to control the 2009 influenza A (H1N1) pandemic? Euro Surveill. 2010;15 doi: 10.2807/ese.15.01.19455-en. pii: 19455. [DOI] [PubMed] [Google Scholar]
- 82.Scalia Tomba G, Wallinga J. A simple explanation for the low impact of border control as a countermeasure to the spread of an infectious disease. Math Biosci. 2008;214:70–2. doi: 10.1016/j.mbs.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 83.Staples JE, Dziuban EJ, Fischer M, Cragan JD, Rasmussen SA, Cannon MJ, et al. Interim guidelines for the evaluation and testing of infants with possible congenital Zika virus infection – United States, 2016. MMWR Morb Mortal Wkly Rep. 2016;65:63–7. doi: 10.15585/mmwr.mm6503e3. [DOI] [PubMed] [Google Scholar]
- 84.Tebas P, Roberts CC, Muthumani K, Reuschel EL, Kudchodkar SB, Zaidi FI, et al. Safety and immunogenicity of an anti-Zika virus DNA vaccine – Preliminary report. N Engl J Med. 2017 doi: 10.1056/NEJMoa1708120. doi: 10.1056/NEJMoa1708120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Modjarrad K, Lin L, George SL, Stephenson KE, Eckels KH, De La, Barrera RA, et al. Preliminary aggregate safety and immunogenicity results from three trials of a purified inactivated Zika virus vaccine candidate: Phase 1, randomised, double-blind, placebo-controlled clinical trials. Lancet. 2018;391:563–71. doi: 10.1016/S0140-6736(17)33106-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Gaudinski MR, Houser KV, Morabito KM, Hu Z, Yamshchikov G, Rothwell RS, et al. Safety, tolerability, and immunogenicity of two Zika virus DNA vaccine candidates in healthy adults: Randomised, open-label, phase 1 clinical trials. Lancet. 2018;391:552–62. doi: 10.1016/S0140-6736(17)33105-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Miller BR, Mitchell CJ. Genetic selection of a flavivirus-refractory strain of the yellow fever mosquito Aedes aegypti. Am J Trop Med Hyg. 1991;45:399–407. doi: 10.4269/ajtmh.1991.45.399. [DOI] [PubMed] [Google Scholar]
- 88.Meghani Z, Boëte C. Genetically engineered mosquitoes, Zika and other arboviruses, community engagement, costs, and patents: Ethical issues. PLoS Negl Trop Dis. 2018;12:e0006501. doi: 10.1371/journal.pntd.0006501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Aubry M, Richard V, Green J, Broult J, Musso D. Inactivation of Zika virus in plasma with amotosalen and ultraviolet A illumination. Transfusion. 2016;56:33–40. doi: 10.1111/trf.13271. [DOI] [PubMed] [Google Scholar]
- 90.Centers for Disease Control and Prevention. Zika Virus. Centers for Disease Control and Prevention. 2016. [Last viewed on 2016 Jan 24]. Available from: http://www.cdc.gov/zika/index.html .
- 91.Centers for Disease Control and Prevention. CDC Health Advisory: Recognizing, Managing, and Reporting Zika Virus Infections in Travelers Returning from Central America, South America, the Caribbean and Mexico: Centers for Disease Control and Prevention. 2016. [Last accessed on 2016 Jan 24]. Available from: http://www.emergency.cdc.gov/han/han00385. asp .
- 92.Tappe D, Rissland J, Gabriel M, Emmerich P, Gunther S, Held G, et al. First case of laboratory-confirmed Zika virus infection imported into Europe, November 2013. Euro Surveill. 2014;19 doi: 10.2807/1560-7917.es2014.19.4.20685. pii: 20685. [DOI] [PubMed] [Google Scholar]
- 93.Petersen EE, Staples JE, Meaney-Delman D, Fischer M, Ellington SR, Callaghan WM, et al. Interim guidelines for pregnant women during a Zika virus outbreak – United states, 2016. MMWR Morb Mortal Wkly Rep. 2016;65:30–3. doi: 10.15585/mmwr.mm6502e1. [DOI] [PubMed] [Google Scholar]
- 94.Jamieson DJ, Rasmussen SA, Uyeki TM, Weinbaum C. Pandemic influenza and pregnancy revisited: Lessons learned from 2009 pandemic influenza A (H1N1) Am J Obstet Gynecol. 2011;204:S1–3. doi: 10.1016/j.ajog.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 95.Li R, Ding J, Ding G, Fan X, He Y, Wang X, et al. Zika virus infections, a review. Radiol Infect Dis. 2017;4:88–93. [Google Scholar]