Abstract
Objectives:
Treatment of dry mouth is the most common clinical challenge in the dental field. Although some remedies have been used to improve the signs and symptoms of xerostomia, none of them are absolutely satisfactory for the patients who have this alteration. In the current years, non-pharmacological treatments based on neuro-electro-stimulation for the treatment of xerostomia were developed. This review aimed at presenting recent developments for the treatment of xerostomia, applying neuro-electro-stimulation by miniaturized intraoral electrostimulators.
Materials and Methods:
A thorough literature search between 1986 and 2018 was carried out using PubMed Central, Scopus, National Science Library, ProQuest, and Google Scholar databases; the results were reviewed, prioritized, and the findings were compiled. Twenty-two studies were evaluated for the review.
Results:
This tool increases salivary secretion and improves xerostomia symptoms. Scientific trials have been carried out, which have revealed the wetting effect of the method described in this text.
Conclusion:
Neuro-electro-stimulation of the salivary gland plays an important role in the stimulation of saliva in patients who need further therapy and have poor quality of life. Intraoral electrostimulator offers a new non-pharmacological method for treating dry mouth.
KEYWORDS: Device and stimuli, electrostimulation, saliva, xerostomia
INTRODUCTION
Sreebny (1988) defined xerostomia as the subjective feeling of oral dryness and it is the result of salivary gland hypofunction. These symptoms are more typical of older people but are not caused by aging. Unstimulated/resting saliva flow is 0.3 mL/min, whereas the flow rate in sleep is 0.1 mL/min and increases to 4.0–5.0 mL/min during chewing.[1] Prevalence has been estimated to range from 14% to 35% and has become increasingly common in developed countries.[2] Although it is more likely that treatment will take place in the middle to the end of life, xerostomia can occur in adolescent people, but less common in children.[3,4]
Saliva has many important functions, including mechanical cleansing action, solubilization of food, detritus dilution, bolus, oral cavity lubrication, remineralization, and maintaining the integrity of the oral mucosa formed. Saliva provides antimicrobial activity and a buffer that protects teeth from decay.[5,6] People with xerostomia often complain of eating, talking, swallowing, and wearing dentures. Prosthetic users may have problems with prosthetic retention, oral mucositis, and the tongue attached to the palate. Patients with xerostomia often complain about dysgeusia, glossodynia, and the increased thirst, especially at night. Xerostomia can cause a significant increase in carious activity, parotid enlargement, inflammation and cracking of the lips, glossitis, oral mucositis, oral candidiasis, sialadenitis, and bad breath.[7,8,9,10,11] Usage of artificial saliva, chewing sugarless gums, and sucking sugarless candies provide symptomatic relief, but the likelihood of recurrence is high when the treatment is stopped.[7] Direct acting cholinergic agonists, such as cevimeline and pilocarpine, promote salivary secretion but these drugs show side effects such as digestive disorders, sweating, altered heart rate, irregular heartbeat, increased pulmonary muscle tone and urine frequency, and blurred vision.[8,9] Current studies have shown that people with xerostomia expressed a desire for effective and secure methods but none of them are currently available to meet this expectation.[10]
Neurological control of salivary secretion: The autonomic nervous system plays a vital role in salivary gland secretion. Cholinergic agonists act on muscarinic and parasympathetic receptors of these exocrine glands inducing saliva with high electrolytes, whereas sympathetic stimulation produces a portion of protein from saliva. Salivation is mainly mediated by autonomous nervous system which consists of sympathetic and parasympathetic nerve fibres. Smell, taste, sound, and sight of food, initiate the salivary secretion process by stimulating superior and inferior salivatory nucleus in medulla. Signals go to otic and submandibular ganglion through parasympathetic nerves and ultimately parotid and submandibular gland causes salivary secretion via effects on acinar secretion and vasodilation.
Sympathetic stimulation causes vasoconstriction, so a small amount of saliva is produced from submandibular gland that is rich in organic material. Parasympathetic stimulation causes vasodilation, so it leads to profuse secretion of watery saliva that contains low content of organic material.[12]
The aim of this review was to demonstrate the development of neuro-electro-stimulation for the treatment of xerostomia, based on neurological control of salivary secretions.
MATERIALS AND METHODS
A thorough review of literature search between 1986 and 2018 was carried out using PubMed, National Science Library, ProQuest, Google Scholar, and Scopus. All the records identified by the searches were screened based on the title first and then followed by the abstract. The first online search was carried out by the reviewer using a search term. We had even activated additional filters, such as number of years to the last 5 years and clinical trials only published in English, with human studies and reviews considered for writing the descriptive review. The later search was duplicated by the second reviewer to confirm the number of items found from the search strategy used. Manual queries and cross-reference queries to identify studies not found online were carried out by the third reviewer. The search terms used were medical subject headings, terms or key words mentioned under all field’s category. The key words of the search strategy were saliva, xerostomia, electrostimulation, and device and stimuli. Any disputes regarding eligibility of a study were resolved by discussion among the reviewers. All identified articles underwent an abstract review and/or full article review to confirm the eligibility. Personal communication was sent to the authors where required.
RESULTS
A total of 120 articles were identified through our search. After the elimination of the external and internal duplicates, only 52 articles were included. After reviewing titles and abstracts, only 22 articles were included. Animal studies confirmed that the application of electrical stimuli to this reflex arc increases saliva production and alleviates the symptoms of xerostomia.[13] Schneyer and Hall[14] in their study reported that electrical neurostimulation in mice was more effective in replacing pilocarpine to induce saliva. Similarly, the use of electrical stimulation through the mucous membrane of oral cavity increases salivary production in patients with salivary gland hypofunction.[15,16,17] Hargitai et al. reported that application of externally placed pads over the parotid gland results in increased salivary production in normal and radiation-induced subjects with xerostomia.[18,19]
DISCUSSION
Applying electrical stimulation to one or three components of the salivary reflex arc must theoretically increase salivation and indirectly decrease the long-term effects of xerostomia.
TECHNOLOGICAL ADVANCEMENTS IN SALIVARY PACEMAKERS
Salitron system
The results of the first attempt to conduct neuro-electro-stimulation to reduce dry mouth are marketed in the US (Biosonics Inc, USA). The Salitron system is a battery-powered electrostimulation system that consists of an electronic control module, a connecting cord, and a handheld stimulus probe with two metal electrodes [Figure 1]. The probe is held by the user every day for several minutes between the tongue and palate. It increases the salivation by producing impulses, which stimulates sensory nerves of oral mucous membrane.[16,17,18,19] This device was approved in 1988 by the US Food and Drug Administration. It was not used commonly due to its large size and high cost.
Figure 1.
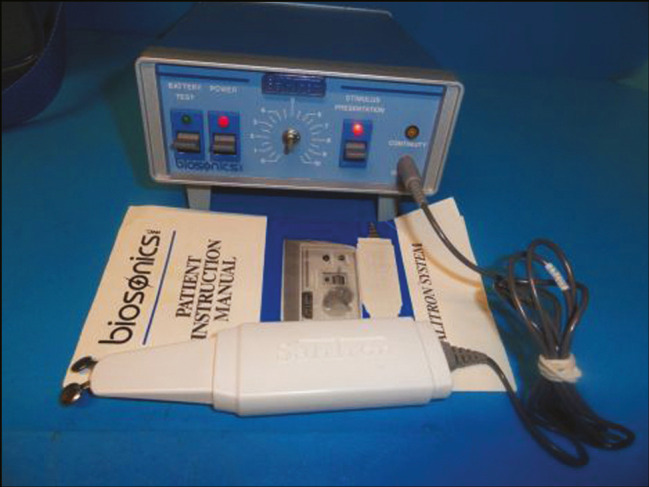
Salitron system
Saliwell GenNarino
GenNarino is a new intraoral miniature neuroelectric stimulator to increase salivary secretion [Figure 2]. It consists of two units: a mouthpiece and a push button to on and off the device.[19] Mouthpiece consists of two plastic sheets. GenNarino attaches an electronic module enclosed between two sheets and a power source consisting of two small 3 V batteries. Two electrodes made of biocompatible material are connected to an electronic module, emerging from a plastic sheet and meeting the lower dental arch of the lingual side. Electronic circuits allow you to turn on and turn off stimulation through external remote control. The user presses the “ON” button on the remote control to turn on the electronic circuit and then places the device on the lower dental arch. Usually, users remove the device from the mouth for up to 5 min and deactivate stimulation by pressing the “OFF” button on the remote control. This device is used “as needed” (i.e., when the user feels dry in the oral cavity), but not more than five times a day. These devices are allowed for a cumulative use of up to 50 months. A clinical trial has shown that GenNarino use increases the relative production of saliva, which leads to more oral lubrication, due to mechanical and electrical stimulation. Mechanical stimulation occurs through contact of the mouthpiece with the oral mucosa. Electrical stimulation is achieved by giving a biphasic low-voltage pulse from the electrode to the oral mucosa to stimulate the lingual nerve. GenNarino electrodes are located in the lower third molar near the lingual nerve where electrostimulation is preferred because these nerves are known to control the secretion of the salivary glands. The selected stimulation parameters provide effective stimulation, but far below the sensitive threshold and pain threshold.
Figure 2.
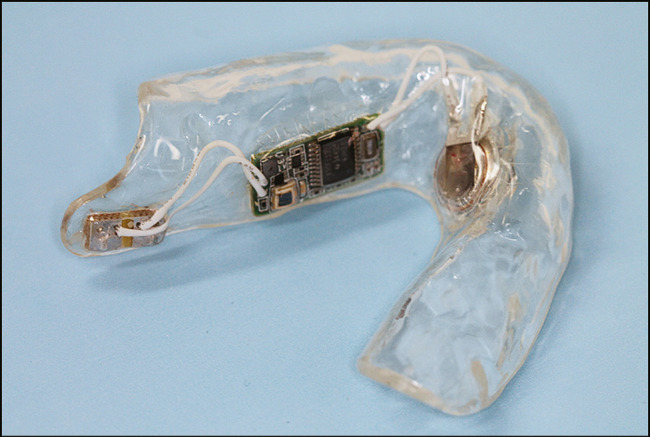
Saliwell GenNarino
Indications:
Xerostomia
Physician prescription
Contraindications:
Under 18 years of age
Allergic to platinum, iridium, polyurethane, and polycarbonate materials of device
During the development of GenNarino, a greater number of scientific trials were performed. Alajbeg et al. conducted an open clinical trial on 94 subjects having oral dryness, and changes were observed from the 5th month of trial period.[9] The protection and efficiency of device were evaluated by Strietzel et al. by conducting trials in several clinical research centers, and they concluded that routine usage reduces signs and symptoms of xerostomia with some complications such as difficulty in pronunciation and sialorrhea.[10] A study was performed by Zadik et al.[20] on six patients with graft versus host disease and it was concluded that the device usage is purely safe.
SaliPen
SaliPen is the device used by the method of electrostimulation of salivary glands [Figure 3]. It has two arms, which are flexible, and these arms, with the electrodes at the tip of each arm, are placed in the oral cavity, beneath the tongue.[21] This device alleviates the feeling of dry mouth over time with no side effects and discomfort. No electrical current is felt and the safety and efficacy of this method were proven in a number of clinical trials performed in many countries. This device is very easy to use and noninvasive. Just place the device in the mouth few times a day and for few minutes every time.[20]
Figure 3.

SaliPen
Saliwell Crown (implant-supported miniature device)
Miniature neuroelectric stimulators assisted by dental implantation [Figure 3] have been designed to provide permanent salivary stimuli in extreme cases [Figure 4]. Use of this fixed device avoids any inconvenience associated with using mobile devices. The components of the removable device are miniaturized into small modules and packaged into devices of the size and shape of molar teeth. This is adjusted to standard osseointegrated dental implants. It also includes a sensor to identify any alteration in intraoral dryness. Saliwell Crown produces continuous stimulation in the mouth without affecting normal function. Any increase or decrease in stimulation is automatically adjusted according to the status of dry mouth and even it can be managed by patients with an on and off button. An osseointegrated implant is positioned distal to second molar area close to lingual nerve, which stimulates salivary gland. At present, a clinical research is needed to study the long-term effects of intraoral neuro-electro-stimulators in xerostomia patients and if the outcome is satisfactory, it is hoped that this can be the comfortable and better way to improve the function of the salivary gland.[22]
Figure 4.

Saliwell Crown
CONCLUSION
Xerostomia has several causes, but regardless of the etiology, it affects the quality of normal life. Neuroelectric stimulation provides new non-pharmacological agents that overtake the role of salivary therapeutic stimulation in patients who need further therapy. Preliminary results show an increase in salivation and gradually subsides the symptoms of oral dryness, suggesting the efficacy of this intraoral neuroelectric stimulation device.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
ACKNOWLEDGEMENT
We would like to thank Dr. B. Lakshmana Rao for giving latest information for this review article.
REFERENCES
- 1.Porter SR, Scully C, Hegarty AM. An update of the etiology and management of xerostomia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:28–46. doi: 10.1016/j.tripleo.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 2.Turner MD. Hyposalivation and xerostomia: Etiology, complications, and medical management. Dent Clin N Am. 2016;60:435–43. doi: 10.1016/j.cden.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 3.Ohara Y, Hirano H, Yoshida H, Obuchi S, Ihara K, Fujiwara Y, et al. Prevalence and factors associated with xerostomia and hyposalivation among community-dwelling older people in Japan. Gerodontology. 2016;33:20–7. doi: 10.1111/ger.12101. [DOI] [PubMed] [Google Scholar]
- 4.Schein OD, Hochberg MC, Muñoz B, Tielsch JM, Bandeen-Roche K, Provost T, et al. Dry eye and dry mouth in the elderly: A population-based assessment. Arch Intern Med. 1999;159:1359–63. doi: 10.1001/archinte.159.12.1359. [DOI] [PubMed] [Google Scholar]
- 5.Mardani H, Ghannadi A, Rashnavadi B, Kamali R. The effect of ginger herbal spray on reducing xerostomia in patients with type II diabetes. Avicenna J Phytomed. 2017;7:308–16. [PMC free article] [PubMed] [Google Scholar]
- 6.Humphrey SP, Williamson RT. A review of saliva: Normal composition, flow, and function. J Prosthet Dent. 2001;85:162–9. doi: 10.1067/mpr.2001.113778. [DOI] [PubMed] [Google Scholar]
- 7.Greenspan D. Xerostomia: Diagnosis and management. Oncology (Williston Park) 1996;10:7–11. [PubMed] [Google Scholar]
- 8.Grisius MM. Salivary gland dysfunction: A review of systemic therapies. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:156–62. doi: 10.1067/moe.2001.116601. [DOI] [PubMed] [Google Scholar]
- 9.Alajbeg I, Densie P Falaco, Simon D Tran. Intraoral electrostimulator for xerostomia relief – a long-term multicenter open-label uncontrolled clinical trial. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:773–81. doi: 10.1016/j.oooo.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 10.Strietzel FP, Martín-Granizo R, Fedele S, Lo Russo L, Mignogna M, Reichart PA. Electrostimulating device in the management of xerostomia. Oral Dis. 2007;13:206–13. doi: 10.1111/j.1601-0825.2006.01268.x. [DOI] [PubMed] [Google Scholar]
- 11.Drosos A, Voulgari P, Psychos D, Tsifetaki N, Bai M. Sicca syndrome in patients with sarcoidosis. Rheumatol Int. 1999;18:177–80. doi: 10.1007/s002960050081. [DOI] [PubMed] [Google Scholar]
- 12.Ojha S, Bhovi TV, Jaju PP, Gupta M, Singh N, Shrivastava K. Effectiveness of transcutaneous electrical nerve stimulation on saliva production in postradiated oral cancer patients. J Indian Acad Oral Med Radiol. 2016;28:246–51. [Google Scholar]
- 13.Konidena A, Sharma D, Puri G, Dixit A, Jatti D, Gupta R. Effect of TENS on stimulation of saliva in postmenopausal women with or without oral dryness—An interventional study. J Oral Biol Craniofac Res. 2016;6:44–50. doi: 10.1016/j.jobcr.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schneyer CA, Hall HD. Comparison of rat salivas evoked by auriculo-temporal and pilocarpine stimulation. Am J Physiol. 1965;209:484–8. doi: 10.1152/ajplegacy.1965.209.3.484. [DOI] [PubMed] [Google Scholar]
- 15.Barbe AG, Heinzler A, Derman S, Hellmich M, Timmermann L, Noack MJ. Hyposalivation and xerostomia among Parkinson’s disease patients and its impact on quality of life. Oral Dis. 2017;23:464–70. doi: 10.1111/odi.12622. [DOI] [PubMed] [Google Scholar]
- 16.Talal N, Quinn JH, Daniels TE. The clinical effects of electrostimulation on salivary function of Sjögren’s syndrome patients. A placebo controlled study. Rheumatol Int. 1992;12:43–5. doi: 10.1007/BF00300975. [DOI] [PubMed] [Google Scholar]
- 17.Weiss WW, Jr, Brenman HS, Katz P, Bennett JA. Use of an electronic stimulator for the treatment of dry mouth. J Oral Maxillofac Surg. 1986;44:845–50. doi: 10.1016/0278-2391(86)90219-3. [DOI] [PubMed] [Google Scholar]
- 18.Hargitai IA, Sherman RG, Strother JM. The effects of electrostimulation on parotid saliva flow: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:316–20. doi: 10.1016/j.tripleo.2004.06.080. [DOI] [PubMed] [Google Scholar]
- 19.Gil-Montoya JA, Barrios R, Sánchez-Lara I, Carnero-Pardo C, Fornieles-Rubio F, Montes J, et al. Prevalence of drug-induced xerostomia in older adults with cognitive impairment or dementia: An observational study. Drugs Aging. 2016;33:611–8. doi: 10.1007/s40266-016-0386-x. [DOI] [PubMed] [Google Scholar]
- 20.Zadik Y, Zeevi I, Luboshitz-Shon N, Dakwar N, Wolff A, Shapira MY, et al. Safety and efficacy of an intra-oral electrostimulator for the relief of dry mouth in patients with chronic graft versus host disease: Case series. Med Oral Patol Oral Cir Bucal. 2014;19:212–9. doi: 10.4317/medoral.19429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ara SA, Patil A, Patil BM. Current trends in the management of xerostomia: A review. Arch Dent Med Res. 2016;2:15–21. [Google Scholar]
- 22.Lafaurie G, Fedele S, López RM, Wolff A, Strietzel F, Porter SR, et al. Biotechnological advances in neuro-electro-stimulation for the treatment of hyposalivation and xerostomia. Med Oral Patol Oral Cir Bucal. 2009;14:76–80. [PubMed] [Google Scholar]


