Abstract
Agents that control bleeding and the usage of bypassing agents have made surgery an option to consider in people with hemophilia. However, the lack of consistent definitions for major or minor surgery may lead to inconsistencies in patient management. This literature review has evaluated how surgical procedures in people with hemophilia were categorized as major or minor surgery and assessed the consistency across publications. After screening 926 potentially relevant articles, 547 were excluded and 379 full-text articles were reviewed. Ninety-five articles categorized major or minor surgical procedures; of these, 35 publications categorized three or more major or minor surgical procedures and were included for analysis. Seven (20%) publications provided varying criteria for defining major or minor surgery, five of which defined surgery according to the level of surgical invasiveness. Across all 35 publications, there was considerable variance in the categorization of major and minor surgical procedures and some overlap in surgical nomenclature (eg, type of synovectomy, arthroscopy, and central venous access device insertion/removals). The lack of consistent guidance when referring to major or minor surgery in people with hemophilia needs to be addressed. Clear and consistent definitions, achieved by consensus and promoted by relevant international hemophilia committees, are desirable, to provide guidance on appropriate treatment, to increase the accuracy of trial data and may confound the interpretation of surgical outcomes.
Keywords: major surgery, minor surgery, hemophilia, categorization
Introduction
The availability of clotting factor concentrates and bypassing agents has made elective surgery an option to consider in people with hemophilia. This, combined with increased life expectancy, is resulting in an increase in the proportion of surgical interventions undertaken in people with hemophilia to address medical conditions other than hemophilia-related complications.1
In general, surgery procedures in people with hemophilia have been categorized traditionally as major or minor. While this categorization is often used to indicate the predicted bleeding risk associated with the procedure, a preliminary literature search revealed no standard definitions for major or minor surgery in people with hemophilia.2 As a result, clinicians have little preoperative guidance as to whether a surgical procedure should be considered as major or minor surgery, which would enable them to plan an appropriate level of support. Furthermore, procedures that may be designated “minor” in the general population may be considered “major” for people with hemophilia, in whom other factors may confound the categorization (eg, severity of disease, presence of inhibitors, and other comorbidities). In addition, this lack of standardization, particularly in clinical trials, may confound the interpretation of surgical outcomes.
Our pilot study indicated that while some guidance does exist, the criteria are not standardized and their application is not consistent, particularly in clinical trials. The World Federation of Hemophilia (WFH) guidelines define major surgery as procedures that require hemostatic support for more than 5 consecutive days.3 Latin American guidelines for the diagnosis and treatment of hemophilia with inhibitors considered all types of surgical procedures, but criteria were defined for minor surgery only.4 Australian guidance considered “abdominal, intracranial, and orthopedic” procedures as being major surgery but did not provide actual definitions for major or minor surgery.5 A consensus paper that focused only on orthopedic surgery agreed on a three-way classification of major, intermediate, and minor surgery based upon surgical procedures but did not provide definitions for each type of surgery.6
We find it surprising that there are no consistent defining criteria for major or minor surgery in people with hemophilia. Without such definitions, the categorization of surgical procedures inevitably becomes more subjective, which may result in inconsistencies in the conduct of clinical trials and in the daily management of people with hemophilia requiring/undergoing surgery, potentially impacting the evaluation of surgical and hemostatic outcomes. Consequently, we have further reviewed the published literature to identify accurately how major and minor surgeries are categorized and to assess the consistency across publications.
Methods
Literature Search
A predetermined search strategy designed to find a high proportion of relevant studies was developed and agreed by all authors. Following a pilot study,2 search terms were refined and expanded, and new searches were conducted in PubMed (incorporating MEDLINE) and Embase on November 11, 2015, for articles and abstracts published entirely in English between January 1, 1990 (by which time recombinant activated factor VII [rFVIIa] was available) and November 11, 2015. The composite search term was constructed based on the format (hemophilia search term) AND (surgery search term minor or major), where each term was itself a composite of individual phrases (see Supplemental Table 1). The use of “wildcards” in the surgery search terms (eg, “surg*,” “proced*,” or “operat*”) yielded too many references to analyze (approximately 13 500). No limits by sex, age, and ethnicity of study participants or by study type were imposed.
Inclusion and Exclusion Criteria
Clinical studies reporting minor or major surgical procedures were included, together with clinically related articles discussing major or minor surgical procedures, as well as congress abstracts. Articles were excluded if they were nonclinical (eg, animal models, in vitro and ex vivo experimental studies) or were unrelated to hemophilia. Also excluded were articles that only reported percutaneous procedures (eg, radiosynovectomies, central venous access device [CVAD] insertion/removal, angiographic embolization, transjugular liver biopsies), however, where these procedures were reported in more general articles, the data were extracted and included in our analysis. Articles citing earlier data analyses were also excluded to avoid oversampling.
Literature Review
The literature review followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidance wherever possible.7 At all stages of the review process, all authors had access to the search results and full papers for review and analysis. Following removal of duplicate articles in both PubMed and Embase, titles and abstracts were reviewed. For articles that could not be screened using the title and abstract, screening was carried out using the full-text article. Articles were considered relevant and retained for full evaluation if they met the inclusion criteria and met none of the exclusion criteria; all other articles were excluded. Full-text articles were reviewed for inclusion and were also reviewed to identify any additional publications that categorized major and minor surgery in people with hemophilia that had not been captured in the search strategy used. As there were a high number of articles reporting 1 or 2 procedures, only those publications that categorized ≥3 surgical procedures as being either major or minor were included in a final review, to analyze the consistency across any reported definitions and categorizations. During full article review, cited articles were checked against our literature search, and any articles not captured in the search were then evaluated for inclusion. Additional searches by author name were not carried out. We did not formally rank articles based on the quality of evidence, as we did not feel that such quality assessment would add value to our review given the expected heterogeneity of eligible studies in terms of selection and the number and classification of cases. A meta-analysis was not conducted; a narrative synthesis of our findings is presented.
Data Extraction
The selected citations were collated and summarized using an Excel® (Microsoft Corp, Redmond, Washington) spreadsheet. The original data sources and the extraction tables were made available to all authors for review and analysis. The data extracted were incorporated in this review to analyze reported definitions for major and minor surgery, the categorization of surgical procedures as major or minor, and to assess the consistency across publications.
Results
Literature Search Results
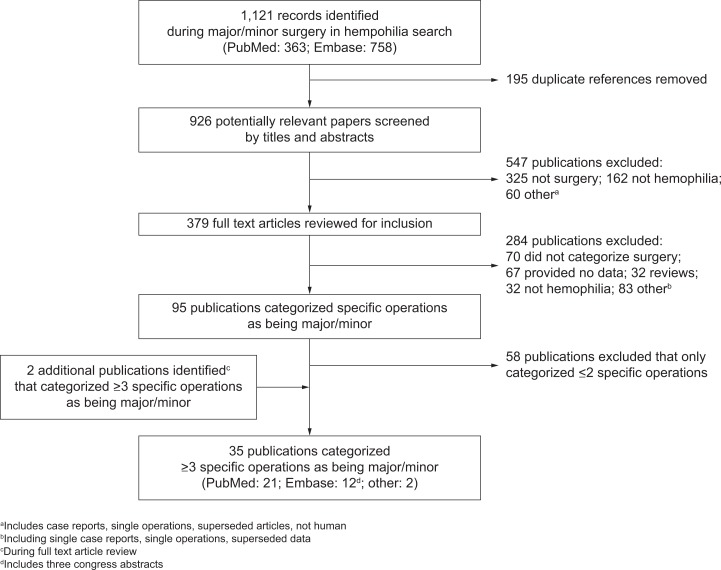
The literature search yielded 926 potentially relevant articles. After screening titles and abstracts, 547 articles were excluded, and 379 full-text articles were reviewed (Figure 1). Of these, 95 articles categorized surgical procedures. Those that categorized 3 or more surgical procedures—35 articles (32 peer-reviewed articles, 3 congress abstracts) in total—as being either major or minor surgery were evaluated further. Of these 35 articles, only two8,9 referred to published guidance (the Perez-Bianco 2008 Latin American guidelines) in order to define or categorize major or minor surgery. Two articles defined major surgery in a similar way to WFH guidance (requiring at least 5 consecutive days of hemostatic support) but did not cite the WFH guidance.10,11
Figure 1.
Flow diagram showing results of the literature search and screening process for hemophilia surgery.
Articles That Defined Major and Minor Surgery
Seven (20%) publications provided formal prespecified definitions for major or minor surgery (Table 1).8,10–15 Five of these publications used the level of surgical invasiveness as a defining factor for major surgery,8,10,13–15 with criteria including: a requirement for a general or spinal anesthetic, provision of respiratory assistance, abdominal surgery, penetration of a major body cavity, orthopedic surgery (joints), and extraction of more than 3 teeth. One publication defined major surgery as any procedure estimated to require daily treatment with FVIII concentrate for at least a week11 with preoperative target FVIII: C levels of 0.5 to 1.0 and 0.2 to 0.5 IU/mL for major and minor surgery, respectively. The remaining publication broadly defined major surgery as being wisdom teeth extraction and all other surgeries.12
Table 1.
Articles That Provided Definitions of Major and/or Minor surgery, and Categorized ≥3 Operations as Being Major and/or Minor in People With Hemophilia (n = 7).
| Publication | Data Source | Surgery Category | No. of Procedures | Defining Criteria | Examples of Procedures in the Surgical Category |
|---|---|---|---|---|---|
| Auerswald et al12 | Prospective single-center study | Major | 23 | Extraction of wisdom teeth and all other surgeries | None (other than wisdom teeth extraction) |
| Minor | 12 | None | Adenectomy, dental surgeries (excluding wisdom tooth extraction) | ||
| Boadas et al8 | Retrospective single-center study | Major | 12 | Any abdominal and orthopedic surgery | Pseudotumor removal/drainage/aspiration, inguinal hernia, achillotenotomy, resection of ear granuloma, reduction of fractured femur, wound debridement (finger), amputation (finger), Moore osteotomy, arthroscopic synovectomy, hip/knee debridement) |
| Minor | 3 | Procedures requiring only skin excision or small sutures, synoviorthesis | Ureteral catheter insertion, cystoscopy and ureteral catheter removal, chemical synoviorthesis | ||
| Klukowska et al10 | Pooled analysis of 5 prospective, open-label multicenter studies | Major | 19 | Require general or spinal anesthesia, opening into the great body cavities (with the possibility of severe hemorrhage requiring hemostatic therapy for at least 6 days), orthopedic interventions Involving joints (ankle, knee, hip, wrist, elbow, shoulder), third molar extraction or extraction of >3 teeth, and surgeries or conditions in which the participant’s life was at stake | None (other than those included within the definition) |
| Minor | 6 | All other surgeries not fulfilling the major criteria were classed as minor | None | ||
| Lusher et al11 | Prospective, multicenter surgery study | Major | 37 | Estimated to require daily treatment with FVIII concentrate for at least a week (no dosages provided) | Total knee replacement, joint fusion, hip replacement, synovectomy, other |
| Minor | 11 | None | Central venous catheter devices, other | ||
| Powell et al13 | Surgery subanalysis of a prospective, open-label, multicenter study | Major | 14 | Any elective or emergent surgical procedure that usually involves general anesthesia and/or respiratory assistance, in which a major body cavity is penetrated and exposed, or for which a substantial impairment of physical or physiological functions is produced | Knee replacements, knee/ankle arthroscopy, external fixation of knee, arm tendon transfer, closure of intestinal fistula, incision, and drainage of dental abscess with multiple extractions, incision and drainage of dental abscess and pilonidal cyst, debridement, fracture dislocation, amputations |
| Minor | 15 | Any elective or emergent surgical procedure that does not involve general anesthesia and/or respiratory assistance | Dental extractions, ankle arthroscopic removal of osteophyte, PCI with stenting, coronary angiography, wart removal, biopsy of alleged paratonsillar abscess, dental crown, alveoplasties, root canal treatment | ||
| Santagostino et al14 | Surgery subanalysis of 3 prospective, open-label, multicenter studies | Major | 15 | An invasive operative procedure where 1 or more of the following occurred: a body cavity was entered; a mesenchymal barrier was crossed; a fascial plane was opened; an organ was removed; normal anatomy was operatively altered | Synovectomy, arthroplasty (knee/hip), ankle arthroscopy, reduction of finger fracture, elbow radial head excision, panproctocolectomy, ileoanal pouch, circumcision |
| Minor | 26 | An invasive operative procedure in which only skin, mucous membranes, or superficial connective tissue was manipulated | Dental, nail extirpation, central venous access device procedures, incision of periumbilical abscess, closure of fistula and debridement and pus drainage | ||
| Serban et al15 | Observational, retrospective single-center study | Major | 27 | According to invasivenessa | Comminuted fracture reduction, displacement of the femur, thigh pseudotumor resection, bilateral shank and thigh amputation for pseudotumor, total hip arthroplasty, total knee arthroplasty, knee prosthesis, evacuation of compressive, giant hematomas (forearm, shank, or thigh) |
| Minor | 46 | According to invasivenessa | Arthrocentesis, intra-articular administration of hyaluronic acid |
aInvasiveness not defined.
Consistency Between Surgical Procedures Classified as Major or Minor Surgery
Across all 35 publications, there was a wide range of surgical procedures categorized as being major or minor (Tables 1 and 2).9,16–42 Two articles defined surgical specialties (eg, orthopedic, cardiothoracic, neurosurgical), rather than individual procedures, as being major or minor.18,40 In general, major surgical procedures were more likely to have been carried out under general anesthetic, while minor surgical procedures tended to be carried out under local anesthetic (Table 2). Dental extractions were often categorized based upon the complexity of the procedure (eg, by the number of teeth </≥3 or the tooth, such as third molar, wisdom tooth, etc, being extracted). Notable exceptions classed as minor surgery were excision of splenic tumor, excision of ear, excision of axillary mass, tonsillectomy, and inguinal hernia repair. Across publications, there was some overlap in the categorization of surgery; for example, some articles categorized synovectomy, arthroscopic synovectomy, arthroscopy, and CVAD insertion/removals as minor surgery, while other articles considered them major surgery. The most common major surgical procedures were general “-ectomy” procedures, joint replacements or arthroplasties, and dental extraction (Table 3). The insertion and removal of CVADs, synovectomies, dental extraction, and cataract operations were the most common minor procedures.
Table 2.
Articles That Categorized ≥3 Operations as Being Major and/or Minor, in People With Hemophilia (n = 27).
| # | Publication | Data Source | Surgery Category | No. of Procedures | Examples of Procedures in the Surgical Category |
|---|---|---|---|---|---|
| Peer-reviewed journal publications | |||||
| 38 | Balkan et al16 | Retrospective single-center study | Major | 11 | Evacuation of subdural hematoma + ventricoperitoneal shunt, ventricoperitoneal shunt revision, open synovectomy, antegrade esophageal dilatation (for corrosive liquid intake), molar teeth extraction |
| Minor | 42 | Radioisotope synovectomy, circumcision | |||
| 54 | Berkouk-Redjimi et al17 | Retrospective multicenter study | Major | 228 | Synovectomy, osteotomy or arthrodesis, joint replacement with a prosthesis |
| Minor | 98 | Synoviorthesis | |||
| 59 | Bhushan et al18 | Retrospective and prospective single-center study | Major | 26 | Orthopedic, general surgery, cardiothoracic and vascular, neurosurgical, obstetric or gynecological, plastic surgery |
| Minor | 30 | Dental extractions, excision of splenic tumor, epulis excision and dental scaling with curettage; wound debridement, biopsies, circumcision, hematoma decompression, urethrotomy, and Hickman-line insertion | |||
| 112 | Caviglia et al9 | Retrospective single-center study | Major | 15 | Arthroscopic synovectomy, pseudotumor removal, osteotomy, arthroscopy, arthrotomy, articular drainage, fracture osteosynthesis |
| Minor | 25 | Chemical/radioactive synovectomy, embolization (angiographic/joint) | |||
| 928 | Dimichele and Negrier19 | Retrospective, multicenter, postmarketing surveillance study | Major | 4 | Ankle fusion, lower leg fasciotomy and split thickness graft, laparoscopic cholecystectomy, knee arthroplasty |
| Minor | 12 | Central line insertion, dental extraction, full mouth rehabilitation, skin graft, cataract removal, radionuclide synovectomy, subclavian port replacement | |||
| 256 | Goudemand et al20 | Retrospective single-center study | Major | 9 | Nephrectomy, osteosynthesis, prostatectomy, total hip prosthesis |
| Minor | 4 | Not described | |||
| 451 | Lusher et al21 | Randomized, blinded, multicenter study, open-label study, and a compassionate-use program | Major | 21 | Herniotomy, tracheotomy, laparotomy, synovectomy, skin grafting, bone fractures, abscess/cyst extirpation |
| Minor | 57 | Central line insertion, arterioventricular shunt, punctures, injections, dental | |||
| 544 | Negrier et al22 | Retrospective, multicenter study | Major | 8 | Bilateral knee arthroplasty, musculocutaneous plasty, prostatic adenomectomy, complete dental extraction, forearm amputation, bilateral tibial osteotomy and splenectomy |
| Minor | 19 | Synoviorthesis, arthroscopic synovectomy, knee arthroscopy | |||
| 549 | Negrier et al23 | Prospective, open-label, multicenter study | Major | 22 | Hip replacement, knee/ankle/shoulder arthroplasty |
| Minor | 35 | Ulnar nerve transposition, ankle/knee/elbow synovectomy, vasectomy, circumcision, tonsillectomy, transjugular liver biopsy, excision of ear, axillary mass excision | |||
| 596 | Pérez-Garrido et al24 | Retrospective, multicenter study | Major | 10 | Laparotomy, appendectomy, neck lipoblastoma tumor resection, ankle osteophyte resection and filling with bone substitute, cement-free hip arthroplasty, knee arthroplasty, knee osteotomy, humerus osteosynthesis, septoplasty for chondrovomerian fracture |
| Minor | 5 | Implant of Ahmed glaucoma valve, cataract, ankle arthroscopy for osteophyte resection, implant of synthetic bone, hematoma drainage, and reconstruction. | |||
| 611 | Polyanskaya et al25 | Retrospective, single-center case series | Major | 16 | Knee endoprosthesis, hip osteotomy, pseudotumor removal, knee arthrolysis, osteosynthesis, leg amputation |
| Minor | 7 | Achilloplasty, synoviorthesis | |||
| 630 | Quintana-Molina et al26 | Retrospective, single-center study | Major | 10 | Placement of hip/knee prosthesis, knee arthrodesis, femur fracture, craniotomy, pyloroplasty, appendectomy, corneal transplant |
| Minor | 54 | Central catheter/Hickman line insertion, radiosynoviorthesis, dental extractions, cataract operations, lipoma removal | |||
| 645 | Rangarajan et al27 | Retrospective, multicenter case series | Major | 18 | Orthopedic: hernia repair, hip fracture repair, knee replacement or synovectomy, ankle fusion or arthrodesis, hemiarthroplasty Other: AV fistula, spinal stenosis surgery, hepatectomy, colectomy, skin grafts, fasciotomy, debridement |
| Minor | 8 | Needle aspiration of knee, bone-marrow aspiration, endoscopic cholangiopancreatography, subungual hematoma washout, catheter insertion | |||
| 647 | Rea et al28 | Retrospective single-center study | Major | 3 | Total knee replacement, laparotomy, and a cerebral tumor resection |
| Minor | 8 | Not described | |||
| 673 | Rodriguez-Merchan et al29 | Retrospective, single-center case series | Major | 13 | Orthopedic surgeries (total knee/hip arthroplasty, fixation of bone fracture, ankle arthrodesis, thoracotomy (lobectomy), craniotomy, pyloroplasty, appendicectomy, corneal transplant |
| Minor | 79 | Radiosynovectomies and central catheter placements, dental extractions, inguinal hernia, lipoma, hydrocele, cataract | |||
| 675 | Rodriguez-Merchan et al30 | Retrospective, single-center orthopedic case series | Major | 7 | Knee/hip arthroplasty, bone fracture fixation, ankle/knee arthrodesis |
| Minor | 20 | Radiosynovectomies | |||
| 679 | Rodriguez-Merchan et al31 | Retrospective, multicenter elective orthopedic surgery case series | Major | 20 | Knee/hip arthroplasty, fracture fixation, removal of pseudotumor, hip osteotomy (varus osteotomy), removal of osteosynthetic material, ankle arthrodesis; elbow synovectomy, forearm fasciotomy, and knee arthroscopic debridement |
| Minor | 88 | Radiosynovectomies (knees, elbows, and ankles) | |||
| 704 | Santagostino et al32 | Prospective, open-label, multicenter study | Major | 11 | Knee arthroplasty, femoral osteosynthesis, plastic surgeries, prosthesis of jejunostomy, polypectomy plus hemorrhoidectomy |
| Minor | 14 | AV fistula, wound revision, tooth extraction, Port-A-Cath insertions and removal | |||
| 743 | Serban et al33 | Prospective, open-label, multicenter surgery study | Major | 5 | Liver biopsy, dental extraction >3 teeth, bilateral synovectomy |
| Minor | 7 | Synovectomy, undercutting of frenulum tongue, dental extraction ≤3 teeth | |||
| 754 | Shapiro et al34 | Prospective, double-blinded, multicenter study | Major | 11 | Synovectomy, hip arthroplasties, knee joint manipulation, cartilage repair, bone graft, laparoscopic renal biopsy |
| Minor | 18 | Central venous catheter placement and removal | |||
| 763 | Siboni et al35 | Retrospective, single-center case series | Major | 4 | Knee/hip replacements, arthroscopy |
| Minor | 2 | Carpal tunnel treatment, hand surgery for trigger finger | |||
| 929 | Tagariello et al36 | Prospective, single-center study | Major | 35 | Cholecystectomy, arthroscopic synovectomy, sigmoidectomy, lumboperitoneal shunt placement |
| Minor | 21 | Suture removal, port placement, dental | |||
| 824 | Tjonnfjord et al37 | Prospective, single-center case series | Major | 7 | Knee/hip arthroplasty, nephrectomy/splenectomy, sigmoidectomy, wound rupture revision |
| Minor | 17 | Dental extraction, cataract removal and lens implantation, trephine biopsy, Hickman line insertion, circumcision, tongue laser coagulation, cystoscopy/pyelography, endoscopic treatment of eroded vessel in esophageal ulcer, prepatellar burse excision, toenail excision | |||
| 893 | Windyga et al38 | Prospective, open-label, multicenter study | Major | 11 | Residual femur fracture nail removal, joint replacement, open synovectomy, abdominal hernia, dental extraction (third molar), neurofibroma excision |
| Minor | 3 | Dental extraction (first molar), intra-articular injection | |||
| 901 | Wolf et al39 | Major | 10 | Knee/hip arthroplasty, neck lipoma excision requiring general anesthetic | |
| Minor | 7 | Dental extractions, onychia | |||
| Congress publications | |||||
| 80 | Brand et al40 | Prospective, open-label, multicenter surgery study | Major | 11 | Orthopedic, dental, cardiovascular, abdominal |
| Minor | 4 | Orthopedic, dental, endoscopy, and dermatological | |||
| 579 | Oldenburg et al41 | Surgery subanalysis from a prospective, open-label, multicenter study | Major | 14 | Joint replacements, ankle fusion, pseudotumor extirpations, foreign body excision, elbow capsular release and ortholysis, ulnar nerve neurolysis, compartment syndrome splitting, cholecystectomy, hemorrhoidectomy, and dental extractions |
| Minor | 46 | Not described | |||
| 924 | Zulfikar et al42 | Retrospective, single-center case series | Major | 12 | Circumcision, bilateral knee arthroscopy, unilateral knee arthroscopy, osteotomy of the knee, port catheters placement, central venous catheter placement, resection of iliopsoas pseudotumor, resection of iliopsoas pseudotumor, hamstring release, achilloplasty |
| Minor | 63 | Orthopedic procedures, dental procedures, gastroscopy, port catheter removal, puncture of hematoma from finger, extraction of cataract, and biopsy of oral leukoplakia | |||
Table 3.
The Most Common (Cited ≥5 times) Surgical Procedures Classified as Either Major or Minor.
| General Surgery | Orthopedic Surgery | Other | |
|---|---|---|---|
| Major | “-ectomy” procedures | Osteotomy/arthrodesis | Dentala |
| “-otomy” procedures | Joint replacement/arthroplasty | ||
| Pseudotumor | Synovectomy/arthroscopic synovectomy | ||
| Bone fracture reduction | |||
| Osteosynthesis | |||
| Arthroscopy | |||
| Amputation | |||
| Minor | Central line insertion/removal | Chemical-/radio-/arthroscopic synovectomy | Dentalb |
| Cataract removal/insertion |
aSome defined as ≥3 teeth; third molar extraction.
b<3 teeth.
Major or Minor Surgery Defined According to Dosage Regimen in People With Hemophilia
Two publications described dosages of either plasma-derived FVIII (pdFVIII)39 or rFVIIa29 in people with hemophilia undergoing major or minor surgery. Wolf et al reported that the preoperative dose of pdFVIII required by previously treated patients with severe hemophilia A without FVIII inhibitors (<0.6 BU mL) was between 48 and 65 IU/kg (16 to 40 infusions) for major surgery or between 42 and 57 IU/kg (1 to 2 infusions) for patients undergoing minor surgery.39 In people with hemophilia who had inhibitors, Rodriguez-Merchan et al reported preoperative rFVIIa dosage regimens of 120 µg/kg for major surgery and 90 to 120 µg/kg for minor surgery.29 Following major surgery, 120 µg/kg rFVIIa was administered every 3 hours on days 1 to 5, and then 90 to 120 µg/kg rFVIIa was administered every 6 hours on days 6 to 14. Following minor surgery, 2 to 4 infusions of 90 to 120 µg/kg rFVIIa were administered every 3 to 6 hours every day on days 1 to 5. While a dosage regimen for FEIBA administration to cover minor surgery was described (initial dose of 100 IU/kg preoperatively, followed 6 hours later by 50 IU/kg every 12 hours for at least 4 days), regimens to cover major surgery were not.29
Discussion
Even though it is often difficult to define a surgical procedure as being major or minor, the usage of these terms, however, imprecise, is firmly established in the surgical lexicon. Our literature review has highlighted the considerable variance in the categorization of surgical procedures. While definitions for minor and major surgery in people with hemophilia have been published, there is no consistency across them, and our literature search has found that they are not widely used. Only 2 (6%) of 35 analyzed articles followed published guidance for defining major or minor surgery. Our literature review also shows that while some procedures are consistently classified—for example, joint replacement and dental extraction were the most common major and minor surgical procedures cited, respectively—there was overlap in the categorization of some procedures (eg, synovectomy, arthroscopic synovectomy, arthroscopy, CVAD insertion/removals) as either major or minor. This overlap may reflect the clinical situation: Factors that may drive a minor procedure to be considered as major surgery include the severity of the patient’s hemophilia, potential duration and intensity of surgical hemorrhage, a wound drain, and longer postoperative treatment and rehabilitation. Interestingly, despite the difficulties in classification, 1 consensus article on surgery in people with hemophilia with inhibitors considered it essential to include an intermediate type of surgery,6 although only 2 of 35 analyzed articles included an intermediate category.17,33 We do not consider that criteria for intermediate surgery are necessary as it would be unlikely to change aspects of management for patients about to undergo surgery and would most probably create confusion among clinicians.
At present, despite a lack of definitions, major and minor surgeries are undertaken safely and effectively in people with hemophilia. Current national and international recommendations and guidelines are based on data from observational, uncontrolled studies,3–6 and as our literature review has found, very few publications refer to, or use, these guidelines. The variability in the use of consensus definitions inevitably results in inconsistencies in reporting and interpreting surgical outcomes and clinical trial results, particularly when considering the effectiveness of a product used during surgical procedures. For example, the categorization of synoviorthesis as being a minor surgical procedure remains a topic of discussion (Luigi Solimeno, personal opinion). One area of concern might be where articles report surgical efficacy without describing the procedures adequately: for example, reports describing the efficacy of bypassing agents in “surgery” that actually relate to data derived from mostly chemosynovectomies or radiosynovectomies (21 of 40 surgical procedures).9 The complexity of categorizing surgery in patients with hemophilia can be illustrated by the fact that open synovectomy and arthroscopic synovectomy can both be considered major surgery, but arthroscopic treatment for a meniscal tear may be considered minor surgery, even though similar instruments and surgical approach are used for all procedures. (Luigi Solimeno, personal opinion). In addition, despite the placement of central venous catheters (or Hickman lines) requiring open cutdown and a general anesthetic, we consider this a minor surgical procedure, as with other CVAD insertion/removal.
It is may be reasonable to consider that minimal hemostatic levels and optimal durations for replacement therapy in people with hemophilia undergoing surgery may help define a procedure as either minor or major. However, only 1 publication in our review defined major surgery according to the duration of FVIII replacement, with preoperative target FVIII: C levels for major and minor surgery,11 while 2 articles reported replacement therapy dosage regimens according to major or minor surgery.29,39 In their 2014 article, the ISTH Definitions Committee provide consensus definitions in many areas such as classification, inhibitors, and response to therapy including surgical hemostasis. However, they provide only limited guidance on surgical procedures (similar to that of the WFH3) suggesting only that they may be classified as major or minor depending on whether the planned duration of hemostatic support is more or less than 5 consecutive days.43 In fact, planning for factor replacement needs to consider the surgery being undertaken, plasma factor levels, inhibitor status, and intra-operative and postoperative conditions.33 In an ideal world, all surgery would involve multidisciplinary teams that include a hematologist, an experienced surgeon, a physical therapist, and other trained health-care professionals (eg, nurses, pharmacist) to assist with the management and to assess the level of bleeding risk and laboratories that can reliably monitor factor levels. Nevertheless, we believe that standardized categorizations of major and minor surgery would support those involved in patient care and researchers attempting to assess and improve surgical outcomes.
Our literature analysis provides an accurate view of the current situation concerning the way that surgery is currently categorized in people with hemophilia. However, we do recognize that there are limitations in our analysis. We did not adopt all PRISMA guidelines: For example, there was no formal protocol, although an extensive pilot study2 provided the basis for the methodology of our literature search and review. In addition, there was no qualitative analysis, although we do not feel that this would have improved the review. Focusing on articles published after 1990 could limit our analysis, as major and minor surgical categorizations were in general use long before that date. However, focusing upon the last 25 years (the era of recombinant replacement factors and the period during which surgery in people with hemophilia has increased) should represent more current experience. Excluding articles that did not report ≥3 procedures might potentially limit our analysis, but we think that this cutoff resulted in a stronger data set (as the inclusion of articles reporting ≤2 procedures could potentially skew the results), and we do not feel that the inclusion of these articles would benefit our analysis. Although searching both PubMed and Embase helped to minimize publication bias, we may have missed relevant reports (eg, institutional or association guidelines) stored within other databases or prepared in languages other than English.
Our literature review suggests a lack of consensus for the categorization of major and minor surgery in people with hemophilia. We believe that it is essential that the definitions for major and minor surgery are accurate and relevant for people with hemophilia and should be developed by consensus between hemophilia specialists, surgeons, and anesthetists. Several factors need to be considered to achieve this: The classification must be simple and easy to understand; it must be applicable across all surgery types; and it should be flexible so that new surgical techniques can be included. Moreover, definitions of minor and major surgery for people with hemophilia should be modified for those patients who have developed inhibitors, as surgery in these patients is more challenging, and so, the risks of uncontrolled bleeding are increased.
In conclusion, clear and consistent definitions, achieved by consensus and promoted by relevant international hemophilia committees, are desirable, to provide guidance on the appropriate treatment regimen to be administered preoperatively, perioperatively, and postoperatively, to increase the accuracy of trial data being reported and to help standardize the interpretation of surgical outcomes.
Supplemental Material
Supplementary_material for Major and Minor Classifications for Surgery in People With Hemophilia: A Literature Review by Luigi Piero Solimeno, Miguel A. Escobar, Snejana Krassova, and Stephanie Seremetis in Clinical and Applied Thrombosis/Hemostasis
Footnotes
Authors’ Note: LS, ME, SK, and SS approved the search strategy and subsequent source selections and reviewed and approved the findings of the data analysis. All authors contributed to the content of the article, with LS and ME providing insight into the impact of the findings from a surgical perspective.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article. LS has received speaker fees from Novo Nordisk and Baxalta. ME has received honoraria for consulting and for participating in advisory boards for Baxalta, Pfizer, NovoNordisk, Bayer, CSL Berhing, and Genentech. SK and SS are both full-time employees of Novo Nordisk.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Data analysis support was provided by Carolyn Bowler, Fiona Bedford, and Graham Joint (search strategy development, article review, and data collation) of Bioscript Medical Ltd (Macclesfield, UK), which was funded by Novo Nordisk Health Care AG (Zurich, Switzerland). Medical writing support was provided by Carolyn Bowler and Graham Joint of Bioscript Medical Ltd (Macclesfield, UK), funded by Novo Nordisk Health Care AG (Zurich, Switzerland).
Supplemental Material: Supplementary material is available for this article online.
References
- 1. Oldenburg J, Dolan G, Lemm G. Haemophilia care then, now and in the future. Haemophilia. 2009;15(suppl 1):2–7. [DOI] [PubMed] [Google Scholar]
- 2. Krassova S, Seremetis S, Solimeno LP. Major and Minor Surgery in Haemophilia: A Literature Review of Definitions. Belgrade: European Haemophilia Consortium; 2015. [Google Scholar]
- 3. Srivastava A, Brewer AK, Mauser-Bunschoten EP, et al. Guidelines for the management of hemophilia. Haemophilia. 2013;19(1):e1–e47. [DOI] [PubMed] [Google Scholar]
- 4. Perez Bianco R, Ozelo MC, Villaca PR, et al. Diagnosis and treatment of congenital hemophilia with inhibitors a Latin American perspective. Medicina (B Aires). 2008;68(3):227–242. [PubMed] [Google Scholar]
- 5. Rickard KA. Guidelines for therapy and optimal dosages of coagulation factors for treatment of bleeding and surgery in haemophilia. Haemophilia. 1995;1(suppl 1):8–13. [DOI] [PubMed] [Google Scholar]
- 6. Rodriguez-Merchan EC, Rocino A, Ewenstein B, et al. Consensus perspectives on surgery in haemophilia patients with inhibitors: summary statement. Haemophilia. 2004;10(suppl 2):50–52. [DOI] [PubMed] [Google Scholar]
- 7. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Boadas A, Fernandez-Palazzi F, De Bosch NB, Cedeno M, Ruiz-Saez A. Elective surgery in patients with congenital coagulopathies and inhibitors: experience of the National Haemophilia Centre of Venezuela. Haemophilia. 2011;17(3):422–427. [DOI] [PubMed] [Google Scholar]
- 9. Caviglia H, Candela M, Galatro G, Neme D, Moretti N, Bianco RP. Elective orthopaedic surgery for haemophilia patients with inhibitors: single centre experience of 40 procedures and review of the literature. Haemophilia. 2011;17(6):910–919. [DOI] [PubMed] [Google Scholar]
- 10. Klukowska A, Windyga J, Batorova A. Clinical efficacy of a novel VWF-containing FVIII concentrate, Wilate((R)), in the prophylaxis and treatment of bleeding episodes in previously treated haemophilia A patients. Thromb Res. 2011;127(3):247–253. [DOI] [PubMed] [Google Scholar]
- 11. Lusher JM, Lee CA, Kessler CM, Bedrosian CL; ReFacto Phase 3 Study Group. The safety and efficacy of B-domain deleted recombinant factor VIII concentrate in patients with severe haemophilia A. Haemophilia. 2003;9(1):38–49. [DOI] [PubMed] [Google Scholar]
- 12. Auerswald G, Bade A, Haubold K, Overberg D, Masurat S, Moorthi C. No inhibitor development after continuous infusion of factor concentrates in subjects with bleeding disorders undergoing surgery: a prospective study. Haemophilia. 2013;19(3):438–444. [DOI] [PubMed] [Google Scholar]
- 13. Powell JS, Apte S, Chambost H, et al. Long-acting recombinant factor IX Fc fusion protein (rFIXFc) for perioperative management of subjects with haemophilia B in the phase 3 B-LONG study. Br J Haematol. 2015;168(1):124–134. [DOI] [PubMed] [Google Scholar]
- 14. Santagostino E, Lentz SR, Misgav M, et al. Safety and efficacy of turoctocog alfa (NovoEight(R)) during surgery in patients with haemophilia A: results from the multinational guardian clinical trials. Haemophilia. 2015;21(1):34–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Serban M, Poenaru D, Patrascu J, et al. Risks and challenges of orthopaedic invasive interventions in haemophilia in a low-resource country. A single-center experience. Hämostaseologie. 2014;34(suppl 1):S30–S35. [DOI] [PubMed] [Google Scholar]
- 16. Balkan C, Karapinar D, Aydogdu S, et al. Surgery in patients with haemophilia and high responding inhibitors: Izmir experience. Haemophilia. 2010;16(6):902–909. [DOI] [PubMed] [Google Scholar]
- 17. Berkouk-Redjimi Y, Ouarlent Y, Hamdi S, et al. Orthopaedic status and surgical needs of patients with haemophilia in Algeria. Open J Hematol. 2012;4:1. [Google Scholar]
- 18. Bhushan V, Chandy M, Khanduri U, Dennison D, Srivastava A, Apte S. Surgery in patients with congenital coagulation disorders. Natl Med J India. 1994;7(1):8–12. [PubMed] [Google Scholar]
- 19. Dimichele D, Negrier C. A retrospective postlicensure survey of FEIBA efficacy and safety. Haemophilia. 2006;12(4):352–362. [DOI] [PubMed] [Google Scholar]
- 20. Goudemand J. Hemophilia. Treatment of patients with inhibitors: cost issues. Haemophilia. 1999;5(6):397–401. [DOI] [PubMed] [Google Scholar]
- 21. Lusher J, Ingerslev J, Roberts H, Hedner U. Clinical experience with recombinant factor VIIa. Blood Coagul Fibrinolysis. 1998;9(2):119–128. [DOI] [PubMed] [Google Scholar]
- 22. Negrier C, Goudemand J, Sultan Y, Bertrand M, Rothschild C, Lauroua P. Multicenter retrospective study on the utilization of FEIBA in France in patients with factor VIII and factor IX inhibitors. French FEIBA Study Group. Factor Eight Bypassing Activity. Thromb Haemost. 1997;77(6):1113–1119. [PubMed] [Google Scholar]
- 23. Negrier C, Shapiro A, Berntorp E, et al. Surgical evaluation of a recombinant factor VIII prepared using a plasma/albumin-free method: Efficacy and safety of Advate in previously treated patients. Thromb Haemost. 2008;100(2):217–223. [PubMed] [Google Scholar]
- 24. Pérez-Garrido R, Alonso N, Jiménez-Yuste V, et al. Efficacy of factor IX Grifols® in surgery: experience of an international multicentre retrospective study. Haemophilia. 2012;18(5):e372–e373. [DOI] [PubMed] [Google Scholar]
- 25. Polyanskaya T, Zorenko V, Karpov E, Sampiev M, Mishin G, Vasiliev D. Experience of recombinant activated factor VII usage during surgery in patients with haemophilia with inhibitors. Haemophilia. 2012;18(6):997–1002. [DOI] [PubMed] [Google Scholar]
- 26. Quintana-Molina M, Martinez-Bahamonde F, Gonzalez-Garcia E, et al. Surgery in haemophilic patients with inhibitor: 20 years of experience. Haemophilia. 2004;10(suppl 2):30–40. [DOI] [PubMed] [Google Scholar]
- 27. Rangarajan S, Yee TT, Wilde J. Experience of four UK comprehensive care centres using FEIBA(R) for surgeries in patients with inhibitors. Haemophilia. 2011;17(1):28–34. [DOI] [PubMed] [Google Scholar]
- 28. Rea C, Dunkerley A, Sorensen B, Rangarajan S. Pharmacokinetics, coagulation factor consumption and clinical efficacy in patients being switched from full-length FVIII treatment to B-domain-deleted r-FVIII and back to full-length FVIII. Haemophilia. 2009;15(6):1237–1242. [DOI] [PubMed] [Google Scholar]
- 29. Rodriguez-Merchan EC, Jimenez-Yuste V, Gomez-Cardero P, Alvarez-Roman M, Martin-Salces M, Rodriguez de la Rua A. Surgery in haemophilia patients with inhibitors, with special emphasis on orthopaedics: Madrid experience. Haemophilia. 2010;16(102):84–88. [DOI] [PubMed] [Google Scholar]
- 30. Rodriguez-Merchan EC, Quintana M, Jimenez-Yuste V, Hernandez-Navarro F. Orthopaedic surgery for inhibitor patients: a series of 27 procedures (25 patients). Haemophilia. 2007;13(5):613–619. [DOI] [PubMed] [Google Scholar]
- 31. Rodriguez-Merchan EC, Wiedel JD, Wallny T, et al. Elective orthopedic surgery for hemophilia patients with inhibitors: new opportunities. Semin Hematol. 2004;41(1 suppl 1):109–116. [DOI] [PubMed] [Google Scholar]
- 32. Santagostino E, Morfini M, Rocino A, Baudo F, Scaraggi FA, Gringeri A. Relationship between factor VII activity and clinical efficacy of recombinant factor VIIa given by continuous infusion to patients with factor VIII inhibitors. Thromb Haemost. 2001;86(4):954–958. [PubMed] [Google Scholar]
- 33. Serban M, Skotnicki AB, Colovic M, et al. Clinical efficacy, safety and pharmacokinetic properties of the plasma-derived factor IX concentrate Haemonine in previously treated patients with severe haemophilia B. Haemophilia. 2012;18(2):175–181. [DOI] [PubMed] [Google Scholar]
- 34. Shapiro AD, Gilchrist GS, Hoots WK, Cooper HA, Gastineau DA. Prospective, randomised trial of two doses of rFVIIa (NovoSeven) in haemophilia patients with inhibitors undergoing surgery. Thromb Haemost. 1998;80(5):773–778. [PubMed] [Google Scholar]
- 35. Siboni SM, Biguzzi E, Pasta G, et al. Management of orthopaedic surgery in rare bleeding disorders. Haemophilia. 2014;20(5):693–701. [DOI] [PubMed] [Google Scholar]
- 36. Tagariello G, Davoli PG, Gajo GB, et al. Safety and efficacy of high-purity concentrates in haemophiliac patients undergoing surgery by continuous infusion. Haemophilia. 1999;5(6):426–430. [DOI] [PubMed] [Google Scholar]
- 37. Tjonnfjord GE. Surgery in patients with hemophilia and inhibitors: a review of the Norwegian experience with FEIBA. Semin Hematol. 2006;43(2 suppl 4):S18–S21. [DOI] [PubMed] [Google Scholar]
- 38. Windyga J, Lissitchkov T, Stasyshyn O, et al. Efficacy and safety of a recombinant factor IX (Bax326) in previously treated patients with severe or moderately severe haemophilia B undergoing surgical or other invasive procedures: a prospective, open-label, uncontrolled, multicentre, phase III study. Haemophilia. 2014;20(5):651–658. [DOI] [PubMed] [Google Scholar]
- 39. Wolf DM, Rokicka-Milewska R, Lopaciuk S, et al. Clinical efficacy, safety and pharmacokinetic properties of the factor VIII concentrate Haemoctin SDH in previously treated patients with severe haemophilia A. Haemophilia. 2004;10(5):438–448. [DOI] [PubMed] [Google Scholar]
- 40. Brand B, Gruppo R, Wynn TT, et al. Initial results of a clinical trial evaluating a full-length pegylated recombinant factor VIII with extended half-life for the perioperative control of hemostasis in hemophilia A. J Thromb Haemost. 2015;13(suppl 2):349–350. [Google Scholar]
- 41. Oldenburg J, Windyga J, Hampton K, et al. Safety and efficacy of bay 81-8973 for surgery in previously treated patients with severe haemophilia A: results of the Leopold clinical trial program. Haemophilia. 2015;21(suppl 2):50–51. [DOI] [PubMed] [Google Scholar]
- 42. Zulfikar B, Koc B, Kilicoglu O, et al. Operative management and outcomes in haemophilia with inhibitor. Haemophilia. 2014;20(suppl 2):82. [Google Scholar]
- 43. Hermans C, Altisent C, Batorova A, et al. Replacement therapy for invasive procedures in patients with haemophilia: literature review, European survey and recommendations. Haemophilia. 2009;15(3):639–658. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary_material for Major and Minor Classifications for Surgery in People With Hemophilia: A Literature Review by Luigi Piero Solimeno, Miguel A. Escobar, Snejana Krassova, and Stephanie Seremetis in Clinical and Applied Thrombosis/Hemostasis