Abstract
The activated partial thromboplastin time (APTT) waveform includes several parameters that are related to various underlying diseases. The APTT waveform was examined in various diseases. Regarding the pattern of APTT waveform, a biphasic pattern of the first or second derivative curve (DC) was observed in patients with hemophilia and patients positive for antiphospholipid (aPL) antibodies or coagulation factor VIII (FVIII) inhibitors. The time of the first and second DC and fibrin formation at 1/2 height were prolonged in patients with hemophilia, patients with inhibitors, patients positive for aPL, patients treated with anti-Xa agents, and patients with disseminated intravascular coagulation (DIC). These values all tended to decrease in pregnant women (at 28-36 weeks’ gestation). The height of the second derivative peak 1 was significantly lower in patients with hemophilia, patients with FVIII inhibitors, patients positive for aPL, patients treated with anti-Xa agents, and patients with DIC; these values tended to be significantly higher in pregnant women. The height of the first DC was significantly lower in patients who were positive for FVIII inhibitors and was significantly higher in patients treated with anti-Xa agents and pregnant women. The height of the first and second DC was useful for the analysis of hemophilia, FVIII inhibitor, and aPL.
Keywords: APTT, waveform, biphasic waveform, hemophilia, anticoagulant
Introduction
The activated partial thromboplastin time (APTT) is an end-point clotting time assay that is useful for diagnosing deficiencies in the intrinsic pathway, such as hemophilia,1 for diagnosing the presence of lupus anticoagulant (LA),2 and for monitoring heparin treatment.3 Automatic optical end-point coagulation analyzers have been recently developed, making it easy to perform multiple assays. Another benefit of optical end-point coagulation analyzers is the ability to visualize the clot reaction curve as the prothrombin time and the APTT. Previous reports have highlighted the usefulness of the visual inspection of APTT clot reaction curves, and abnormal biphasic clot reaction curves have been reported to be associated with the early detection of disseminated intravascular coagulation (DIC).4,5 These reports are only related to the use of Platelin LS (Instrumentation Laboratory, Bedford, Massachusetts) APTT reagent with the MDA II analyzer (Organon Teknika, Cambridge, United Kingdom), which uses an automated waveform analysis software program. Additionally, the visual inspection of clot reaction curves has been shown to detect inaccurate APTT results, which may occur due to the application of particular evaluation algorithms when using the Behring BCS (Dade Behring, Illinois, USA) and BCT coagulation analyzers.6
The software program used for the ACL TOP analyzer for APTT using APTT-synthetic phospholipids (SPs) not only makes it possible to display the clot reaction curves but also allows the associated first and second derivative curves (DCs) to be displayed. These derivative plots are automatically calculated from the absorbance data by the ACL TOP software program and reflect the velocity (first derivative) and acceleration (second derivative) at various points throughout the clotting reaction. These values are depicted as the clot reaction curve.7 The evaluation for the second DC of APTT is useful for detecting any coagulation factor deficiency.8 The differential diagnosis between coagulation factor deficiency and LA or between hemophilia and acquired hemophilia5 is difficult to make based on the result of a clotting time assay. In addition, it is difficult to use the APTT to monitor the direct oral anticoagulant level.
In this study, we measured and analyzed the APTT waveform in patients with various diseases and examined the relationship between the disease and the parameters of the APTT.
Materials and Methods
An APTT assay was performed with plasma samples from 30 healthy volunteers (HVs, female, n = 10; male, n = 20; median age, 21 years; range, 20-24 years), 11 patients with hemophilia (median age, 62.0 years; range, 42.3-70.5 years), 5 patients who were positive for factor VIII (FVIII) inhibitors (median age, 67.0 years; range, 59.8-70.5 years; Table 1), 12 patients who were positive for antiphospholipid (aPL) antibodies (female, n = 10 and male, n = 2; median age, 61.0 years; range, 43.5-71.6 years), 10 patients who were treated with warfarin (female, n = 8 and male, n = 2; median age, 59.0 years; range, 48.0-72.0 years), 18 patients who underwent total hip arthroplasty or total knee arthroplasty and who were treated with edoxaban (30 mg; Daiichi-Sankyo, Tokyo, Japan; female, n = 12 and male, n = 6; median age, 70.5 years; range, 60.0-77.0 years) as an anti-Xa agent to prevent deep vein thrombosis, 12 pregnant women at 28 to 36 weeks’ gestation (median age, 32.5 years; range, 30.0-35.0 years), 6 patients with thrombophilia (female, n = 6; median age, 45.5 years; range, 30.0-56.0 years), and 20 patients with DIC (female, n = 8; male, n = 12; median age, 62.5 years; range, 54.5-75.5 years). The samples were obtained at Mie University Hospital from January 28, 2016, to December 22, 2016. Patients with hemophilia included 8 patients with hemophilia A and 3 patients with hemophilia B; their coagulation factor activity was ≤10%. Patients with FVIII inhibitors included 4 patients with FVIII inhibitor-associated hemophilia and 1 patient with acquired hemophilia. Their inhibitor titer was 5.6 to 95.1 Bethesda units. The aPL status was determined based on the diluted Russell viper venom time, the detection of anticardiolipin immunoglobulin G antibodies, or anticardiolipin β2–GPI complex antibodies.9 Six of the 12 patients with aPL had thrombotic complications. Prothrombin time of the patients who were treated with warfarin was controlled to keep it within the range of 1.6 to 2.6, according to the international normalized ratio. Disseminated intravascular coagulation was diagnosed according to the Japanese Ministry Health, Labor and Welfare DIC diagnostic criteria.10 The patients with DIC included 9 patients with infection, 5 patients with aneurysm, 2 patients after liver transplantation, 2 patients with multiple organ failure, 1 patient with gastric cancer, and 1 patient with obstetric disease.
Table 1.
Patients Having Hemophilic With and Without Inhibitor.
| Type | Inhibitor BU | FVIII or FIX activity, % | Treatment | APTT: Acceleration Peak 1 | |||
|---|---|---|---|---|---|---|---|
| Time, second | Height, mAbs/s2 | Width, second | |||||
| 1 | Hemophilia A | <0.5 | 2.9 | On-demand | 58.2 | 20.4 | 178 |
| 2 | Hemophilia B | <0.5 | 3.6 | On-demand | 53.2 | 11.6 | 242 |
| 3 | Hemophilia A | <0.5 | <1.0 | Prophylaxis treatment | 89.7 | 51 | 37.5 |
| 4 | Hemophilia A | <0.5 | <1.0 | Prophylaxis treatment | 58.1 | 25.4 | 116 |
| 5 | Hemophilia A | <0.5 | 9.3 | On-demand | 49.2 | 18.4 | 379 |
| 6 | Hemophilia A | <0.5 | <1.0 | Prophylaxis treatment | 25.6 | 6.1 | 656 |
| 7 | Hemophilia B | <0.5 | 9.4 | On-demand | 41.4 | 9.8 | 736 |
| 8 | Hemophilia A | <0.5 | <1.0 | Prophylaxis treatment | 39.9 | 9.3 | 414 |
| 9 | Hemophilia B | <0.5 | <1.0 | On-demand | 62.7 | 28 | 161 |
| 10 | Hemophilia B | <0.5 | <1.0 | Prophylaxis treatment | 70.1 | 20.6 | 282 |
| 11 | Hemophilia A | <0.5 | 1.3 | On-demand | 52.5 | 15.2 | 15.6 |
| 12 | Pancreas cancer | 9.2 | 4.1 | Prednisolone | 65.1 | 19.5 | 31.6 |
| 13 | Hemophilia A | 5.6 | <1.0 | Bypass therapy | 125.6 | 24.2 | 14.4 |
| 14 | Hemophilia A | 93.2 | <1.0 | Bypass therapy | 69 | 62.1 | 33.5 |
| 15 | Hemophilia A | 76.2 | 2.3 | Bypass therapy | 68.4 | 23.1 | 114 |
| 16 | Hemophilia A | 95.1 | <1.0 | Bypass therapy | 114.4 | 113 | 24.5 |
Abbreviations: Abs, absorbance; APTT, activated partial thromboplastin time; BU, Bethesda unit; FVIII, factor VIII; FIX, factor IX.
The study protocol was approved by the Human Ethics Review Committee of the Mie University School of Medicine, and written informed consent was obtained from each of the patient. This study was faithfully carried out in accordance with the principles of the Declaration of Helsinki.
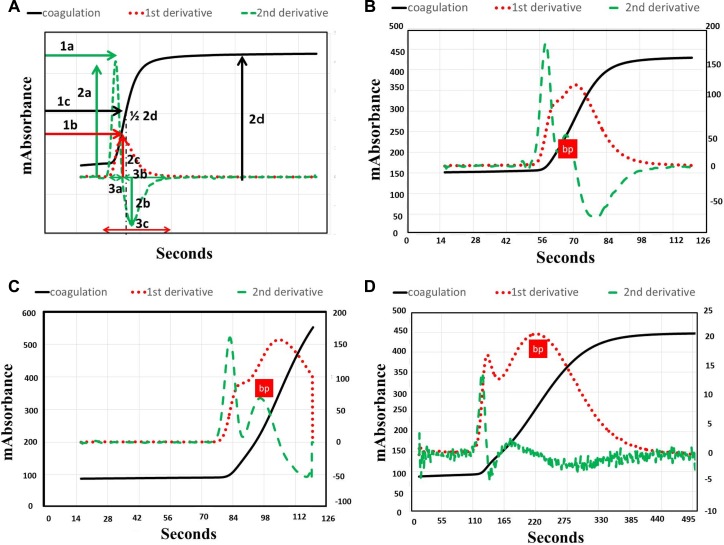
Activated partial thromboplastin time was measured using the APTT-SP (Instrumentation Laboratory, Bedford, Massachusetts), which uses silica as an activator of FXII and SPs. This is suitable for detecting deficiencies in the intrinsic coagulation factors or LA when using an ACL-TOP system. After measuring the APTT, we performed a waveform analysis based on the results of each APTT assay. Three types of curves are shown in the monitor of the ACL-TOP system (Figure 1A). One curve shows the changes in the absorbance observed while measuring the APTT, which corresponds to fibrin formation. The second is the first DC of the absorbance, which corresponds to the coagulation velocity. The third is the second DC of the absorbance, which corresponds to the coagulation acceleration. For the waveform analysis, we first checked for the presence of an abnormal curve showing a biphasic waveform on the first and/or second DCs. Furthermore, as shown in Figure 1A, we calculated the following 9 parameters on the first or second DC manually using a mouse: 1A, the second DC; 1B, the first DC; 1C, time for 1/2 the height of fibrin formation; 2A, the height of the second DC peak 1; 2B, the height of the second DC peak 2; 2C, the height of the first DC; 2D, the height of fibrin formation; 3A, the width of the second DC peak 1; 3B, the width of the second DC peak 2; 3C, the width of the first DC.
Figure 1.
Activated partial thromboplastin time (APTT) waveform. A, Normal volunteer. B, Patient with antiphospholipid antibody. C, Patient with hemophilia. D, Patient with inhibitor for factor VIII (FVIII). 1A, first derivative curve (DC); 1B, second DC; 1C, time for 1/2 height of fibrin formation; 2A, height of the second DC peak 1; 2B, height of the second DC peak 2; 2C, height of the first DC; 2D, height of fibrin formation; 3A, width of the second DC peak 1; 3B, width of the second DC peak 2; 3C, width of the first DC, bp, biphasic waveform.
Statistical Analysis
The data are expressed as the median (25th-75th percentiles). The differences between the groups were examined using the Mann-Whitney U test. P values of <.05 were considered to indicate statistical significance. All of the statistical analyses were performed using the Stat Flex software package (version 6; Artec Co Ltd, Osaka, Japan).
Results
The APTT waveform of a patient with aPL (Figure 1B) shows a biphasic pattern of the second DC and a prolonged peak time of the first and second DC and fibrin formation. The APTT waveform of a patient with hemophilia (Figure 1C) shows a biphasic pattern of the second DC and a markedly prolonged peak time of the first and second DC and fibrin formation. There were no significant differences in the APTT waveforms of patients with hemophilia A and B. The APTT waveform of a patient positive for FVIII inhibitors (Figure 1D) shows a biphasic first DC, markedly prolonged peak time of the first and second DC and fibrin formation, and a markedly low height of the first and second DC.
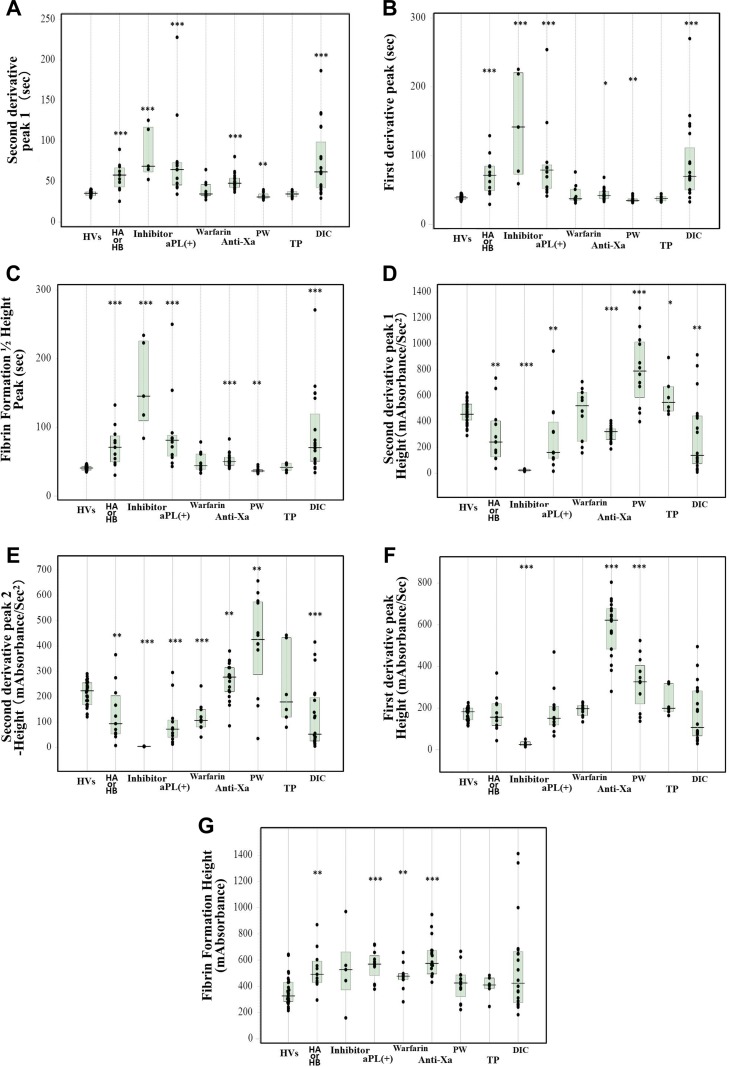
In HVs, the peak second DC time is 35.5 seconds (range, 32.6-37.4 seconds). The time is significantly prolonged in patients with hemophilia, patients with FVIII inhibitors, patients positive for aPL, patients treated with anti-Xa agents, and patients with DIC; in contrast, the time is significantly shortened in pregnant women (Table 2 and Figure 2a). In HVs, the times of the first DC and fibrin formation at 1/2 height were 38.7 (36.2-40.8) seconds and 40.9 (37.8-42.7) seconds, respectively. These times were prolonged in patients with hemophilia, patients with FVIII inhibitors, patients positive for aPL, patients treated with anti-Xa agents, and patients with DIC; these times were shortened in pregnant women (Figure 2B and C). In HVs, the height of the second DC peak 1 was 457 (411-535) mAbs/s2; the height was significantly lower in patients with hemophilia, patients with FVIII inhibitors, patients positive for aPL, patients treated with anti-Xa agents, and patients with DIC; the height was significantly higher in pregnant women (Figure 2D). In HVs, the height of the second DC peak 2 was 224 (170-255) mAbs/s2. The height was significantly lower in patients with hemophilia, patients with FVIII inhibitors, patients positive for aPL, patients treated with warfarin, and patients with DIC. The height was significantly higher in pregnant women and in patients treated with anti-Xa agents (Figure 2E). In HVs, the height of the first DC was 183 (144-200) mAbs/s. The height of the first DC was significantly lower in patients who were positive for FVIII inhibitors and was significantly higher in patients who were treated with anti-Xa agents and pregnant women (Figure 2F). In HVs, the height of fibrin formation was 328 (286-431) mAbs. The height was significantly higher in patients with hemophilia, patients positive for aPL, and patients treated with warfarin or anti-Xa agents (Figure 2G).
Table 2.
Parameters of the APTT Wave Form in Patients With Various Diseases.
| HVs | Hemophilia | Inhibitor | aPL | Warfarin | Anti-Xa | PW | TP | DIC | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Second derivative | Peak 1 | Time (second) | 35.5 (32.6-37.4) | 58.1 (43.4-6.0) | 69.0 (62.0-117.2) | 64.8 (45.8-73.3) | 34.8 (32.5-46.3) | 48.0 (42.7-54.3) | 30.9 (29.4-34.7) | 34.7 (31.0-37.7) | 61.9 (42.4-98.9) |
| Height (mAbs/s2) | 457 (411-535) | 242 (127-405) | 24.5 (15.3-32.1) | 161 (116-396) | 523 (247-625) | 323 (263-344) | 791 (586-1015) | 549 (481-671) | 139 (74.2-444) | ||
| Wide (second) | 7.45 (6.80-8.00) | 20.4 (10.3-24.8) | 24.2 (18.4-74.8) | 22.5 (15.8-29.3) | 7.30 (6.90-14.0) | 11.4 (10.4-13.0) | 7.70 (7.15-8.90) | 7.65 (7.20-7.90) | 12.7 (9.70-23.8) | ||
| Peak 2 | Height, mAbs/s2 | 224 (170-255) | 94.2 (54.1-204) | 4.60 (3.78-5.58) | 72.9 (40.8-109) | 107 (81.2-150) | 278 (220-315) | 426 (289-574) | 180 (120-433) | 52.8 (26.0-198) | |
| Wide, second | 17.7 (16.7-18.7) | 57.1 (35.0-95.0) | 100 (57.5-185) | 44.1 (34.4-75.0) | 45.6 (29.9-60.3) | 36.9 (32.1-40.9) | 23.2 (19.7-25.4) | 24.4 (22.1-60.3) | 47.9 (40.1-73.4) | ||
| First derivative | Time, second | 38.7 (36.2-40.8) | 71.4 (49.3-84.7) | 142 (72.9-220) | 79.1 (52.4-56.6) | 37.2 (35.1-51.1) | 42.0 (37.7-48.1) | 34.7 (33.2-37.1) | 37.7 (34.2-40.5) | 69.9 (50.2-111) | |
| Height, mAbs/s | 183 (144-200) | 156 (117-221) | 24.7 (19.4-38.2) | 151 (119-209) | 197 (164-213) | 622 (483-677) | 326 (220-404) | 199 (183-317) | 107 (66.5-283) | ||
| Wide, second | 19.5 (18.0-20.3) | 52.9 (34.4-88.8) | 174 (74.6-272) | 51.0 (33.1-66.4) | 49.3 (39.2-60.7) | 45.4 (40.9-51.9) | 26.8 (19.6-30.2) | 30.3 (26.2-60.3) | 57.6 (47.0-86.5) | ||
| Fibrin formation | Height, mAbs | 328 (286-431) | 492 (430-592) | 528 (373-663) | 570 (483-633) | 478 (452-498) | 575 (495-674) | 426 (322-488) | 411 (383-464) | 424 (277-665) | |
| 1/2 height, second | 40.9 (37.8-42.7) | 71.0 (49.8-87.7) | 146 (110-226) | 81.2 (58.2-88.3) | 44.2 (39.1-61.2) | 50.2 (44.8-56.4) | 36.5 (35.0-38.5) | 41.8 (37.4-47.9) | 70.5 (50.8-119) | ||
| Number | 30 | 11 | 5 | 12 | 10 | 18 | 12 | 6 | 20 | ||
Abbreviations: Anti-Xa, patients treated with anti-Xa agent; aPL, patients positive anti-phospholipid antibody; DIC, disseminated intravascular coagulation; HVs, healthy volunteers; mAbs, m-absorbance; PW, pregnant women; TP, thrombophilia; warfarin, patients treated with warfarin.
Figure 2.
Second DC peak 1 (A), first DC peak (B), and time for 1/2 height of fibrin formation (C), second DC peak 1 height (D), Second DC peak 2 height (E), first DC peak height (F), and fibrin formation height (G). DC indicates derivative curve; Anti-Xa, patients treated with an anti-Xa agent; aPL(+), patients positive for antiphospholipid antibody; DIC, patients with disseminated intravascular coagulation; HA, hemophilia A; HB, hemophilia B; HVs, healthy volunteers; Inhibitor, patients positive for anti-FVIII antibody; PW, pregnant women; TP, thrombophilia; Warfarin, patients treated with warfarin.
In HVs, the width of the second DC peak 1 was 7.45 (6.80-8.00) seconds. The width was significantly longer in patients with hemophilia, patients with FVIII inhibitors, patients positive for aPL, patients treated with anti-Xa agents, and patients with DIC. In HVs, the width of the second DC peak 2 and first DC was 17.7 (16.7-18.7) seconds and 19.5 (18.0-20.3) seconds, respectively. The values were significantly longer in patients with hemophilia, patients with FVIII inhibitor, patients positive for aPL, patients treated with warfarin or anti-Xa agents, pregnant women, patients with thrombophilia, and patients with DIC.
Discussion
Although the biphasic waveform has recently gained attention in the analysis of the APTT waveform,5,6,11 various parameters, such as the time of the first and second DC and fibrin formation at 1/2 height and the height of the first and second DC, were found to be important in this study. In addition to patients with hemophilia, patients with FVIII inhibitors, and patients with aPL, the biphasic waveform was seen in patients treated with anti-Xa agents. Changes in the APTT waveform have been reported to predict coagulation factor deficiency or LA positivity.7 The results of the APTT waveform analysis are reported to be well correlated with the FVIII activity and to be useful for the management of hemophilia.12–14 There were no significant differences in the APTT waveform or various parameters between patients with hemophilia A and B. As our study was small, a larger study should be performed to examine the differences between hemophilia A and B.
The time of peak for the first and second DC and fibrin formation was prolonged in patients with hemophilia and patients with FVIII inhibitors, and the time of peak for the first DC was especially prolonged in patients with FVIII inhibitors (Table 3). The present study had only 1 patient with acquired hemophilia A; thus, it is not appropriate to discuss the differences between hemophilia A and acquired hemophilia A based on the findings of the present study. The peak times were prolonged in patients who were positive for aPL; however, the relationship between the complication of thrombosis and the waveform was not clear. With regard to anticoagulation therapy, these times were prolonged in the patients treated with anti-Xa agents, but not in patients treated with warfarin. These differences may depend on the anticoagulation mechanism associated with the respective anticoagulants. The height of the second DC peak 1 was significantly lower in patients with hemophilia, patients with FVIII inhibitors, patients positive for aPL, patients treated with anti-Xa agents, and patients with DIC; the value was the lowest in those with FVIII inhibitors. These findings suggested that patients with FVIII inhibitors show severe bleeding.15 However, it was not clear that the aPL-positive patients were in a hypocoagulable state. Interestingly, the height of the second DC peak 1 was significantly higher in pregnant women, suggesting that the pregnant women were in a hypercoagulable state.16 The findings varied among patients with DIC due to the various states of DIC, which include pre-DIC, infectious DIC, and hematological DIC.17–19 Although the height of the second DC peak 1 was low in patients treated with anti-Xa agents, the height of the second DC peak 2 was high in the same patients. The height of the first DC was significantly higher in patients treated with anti-Xa agents and pregnant women. Pregnant women are in a hypercoagulable state, but patients treated with anti-Xa agents are not; thus, the meaning of the height of the velocity is not clear. The elevation in the height of the velocity in patients treated with anti-Xa agents may reflect that the patients was in a hypercoagulable state prior to the administration of the anti-Xa agent.
Table 3.
Summary of Parameters in the APTT Wave Form in Patients With Typical Diseases.
| Hemophilia | Inhibitor | aPL | Warfarin | Anti-Xa | PW | TP | DIC | ||
|---|---|---|---|---|---|---|---|---|---|
| Second derivative | Time | Long | Long | Long | ND | Slightly long | ND | ND | Long |
| Height | Low | Significantly low | Low | ND | Slightly low | High | Slightly high | Low | |
| Wide | Long | Long | Long | ND | Slightly long | ND | ND | Slightly long | |
| First derivative | Time | Long | Significantly long | Long | ND | Slightly long | ND | ND | Long |
| Height | Slightly low | Significantly low | Slightly low | ND | High | High | ND | Low | |
| Fibrin formation | Height | High | High | High | High | High | High | High | High |
| Time | Long | Significantly long | Long | ND | Slightly long | ND | ND | Long | |
Abbreviations: aPL, patients positive for antiphospholipid antibody; DIC, disseminated intravascular coagulation; mAbs, m-absorbance; PW, pregnant women; TP, thrombophilia; Warfarin, patients treated with warfarin, Anti-Xa, patients treated with anti-Xa agent.
The width of the second DC of peak 1 and peak 2 and the first DC was significantly longer in almost all of the diseases, thereby suggesting that these diseases were associated with some hemostatic abnormalities.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported in part by a Grant-in-Aid from the Ministry of Health, Labour and Welfare of Japan and the Ministry of Education, Culture, Sports, Science and Technology of Japan. The APTT assay was supported by the Instrumentation Laboratory.
References
- 1. Matsumoto T, Nogami K, Shima M. A combined approach using global coagulation assays quickly differentiates coagulation disorders with prolonged aPTT and low levels of FVIII activity. Int J Hematol. 2017;105(9):174–183. [DOI] [PubMed] [Google Scholar]
- 2. Tokutake T, Baba H, Shimada Y, et al. Exogenous magnesium chloride reduces the activated partial thromboplastin times of lupus anticoagulant-positive patients. PLoS One. 2016;11(6):e0157835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Byun JH, Jang IS, Kim JW, Koh EH. Establishing the heparin therapeutic range using aPTT and anti-Xa measurements for monitoring unfractionated heparin therapy. Blood Res. 2016;51(3):171–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Toh CH, Giles AR. Waveform analysis of clotting test optical profiles in the diagnosis and management of disseminated intravascular coagulation (DIC). Clin Lab Haematol. 2002;24(6),321–327. [DOI] [PubMed] [Google Scholar]
- 5. Matsumoto T, Wada H, Nishioka Y, et al. Frequency of abnormal biphasic aPTT clot waveforms in patients with underlying disorders associated with disseminated intravascular coagulation. Clin Appl Thromb Hemost. 2006;12(2):185–192. [DOI] [PubMed] [Google Scholar]
- 6. Mair G, Dunhill S, Tiplady C. Prognostic implications of a biphasic waveform for APTT analysis in a district general hospital. Int J Lab Hematol. 2008;30(6):467–472. [DOI] [PubMed] [Google Scholar]
- 7. Solano C, Zerafa P, Bird R. A study of atypical APTT derivative curves on the ACL TOP coagulation analyser. Int J Lab Hematol. 2011;33(1):67–78. [DOI] [PubMed] [Google Scholar]
- 8. Tokunaga N, Inoue C, Sakata T, et al. Usefulness of the second-derivative curve of activated partial thromboplastin time on the ACL-TOP coagulation analyzer for detecting factor deficiencies. Blood Coagul Fibrinolysis. 2016;27(4):474–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Habe K, Wada H, Matsumoto T, et al. Presence of antiphospholipid antibodies as a risk factor for thrombotic events in patients with connective tissue diseases and idiopathic thrombocytopenic purpura. Intern Med. 2016;55(6):589–595. [DOI] [PubMed] [Google Scholar]
- 10. Kobayashi N, Maegawa T, Takada M, Tanaka H, Gonmori H. Criteria for diagnosis of DIC based on the analysis of clinical and laboratory findings in 345 DIC patients collected by the research committee on DIC in Japan. Bibl Haemotol. 1983;49:265–275. [DOI] [PubMed] [Google Scholar]
- 11. Zakariah AN, Cozzi SM, Van Nuffelen M, Clausi CM, Pradier O, Vincent JL. Combination of biphasic transmittance waveform with blood procalcitonin levels for diagnosis of sepsis in acutely ill patients. Crit Care Med. 2008;36(5):1507–1512. [DOI] [PubMed] [Google Scholar]
- 12. Trampuš Bakija A, Debeljak M, Preložnik Zupan I, Benedik Dolničar M, Kovač J, Jazbec J. Specific and global coagulation tests in patients with mild haemophilia A with a double mutation (Glu113Asp, Arg593Cys). Blood Transfus. 2015;13(4):622–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Siegemund T, Scholz U, Schobess R, Siegemund A. Clot waveform analysis in patients with haemophilia A. Hamostaseologie. 2014;34(suppl 1):S48–S52. [DOI] [PubMed] [Google Scholar]
- 14. Milos M, Coen Herak D, Zupancic-Salek S, Zadro R. New quantitative aPTT waveform analysis and its application in laboratory management of haemophilia A patients. Haemophilia. 2014;20(6):898–904. [DOI] [PubMed] [Google Scholar]
- 15. Janbain M, Leissinger CA, Kruse-Jarres R. Acquired hemophilia A: emerging treatment options. J Blood Med. 2015;6:143–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bennett A, Chunilal S. Diagnosis and management of deep vein thrombosis and pulmonary embolism in pregnancy. Semin Thromb Hemost. 2016;42(7):760–773. [DOI] [PubMed] [Google Scholar]
- 17. Aota T, Wada H, Fujimoto N, et al. The valuable diagnosis of DIC and pre-DIC and prediction of a poor outcome by the evaluation of diagnostic criteria for DIC in patients with hematopoietic injury established by the Japanese Society of Thrombosis and Hemostasis. Thromb Res. 2016;147:80–84. [DOI] [PubMed] [Google Scholar]
- 18. Aota T, Wada H, Yamashita Y, et al. An evaluation of the modified diagnostic criteria for DIC established by the Japanese Society of Thrombosis and Hemostasis Clin Appl Thromb Hemost. 2016. [DOI] [PubMed] [Google Scholar]
- 19. Aota T, Wada H, Fujimoto N, et al. Evaluation of the diagnostic criteria for the basic type of DIC established by the Japanese society of thrombosis and hemostasis Clin Appl Thromb Hemost. 2016. [DOI] [PubMed] [Google Scholar]