Abstract
The sticky platelet syndrome (SPS) is a common cause of both arterial and venous thrombosis, being a dominant autosomal disease with qualitative platelet alterations and familial occurrence. It is characterized by platelet hyperreactivity with increased platelet aggregability in response to low concentrations of platelet agonists: epinephrine, adenosine diphosphate, or both. The clinical manifestations involve venous or arterial thrombosis, recurrent pregnancy loss, and fetal growth retardation. To analyze the localization of the thrombotic episodes in a cohort of Mexican mestizo patients with SPS. Between 1992 and 2016, 86 Mexican mestizo patients with SPS as the single thrombophilic condition were prospectively identified; all of them had a history of thrombosis. There were 15 males and 71 females. The thrombotic episodes were arterial in 26 cases and venous in 60 (70%). Arterial thrombosis was mainly pulmonary thromboembolism, whereas venous thromboses were identified most frequently in the lower limbs. Mexican mestizo population with SPS is mainly female; the type I of the condition is the most frequent; both arterial and venous thrombosis can occur, and they are mainly pulmonary embolism and lower limbs venous thrombosis, respectively.
Keywords: sticky platelet syndrome, platelet hyperaggregability, Mexican mestizo
Introduction
The sticky platelet syndrome (SPS) is a common cause of arterial and venous thrombosis. Initially described by Holiday in 1983 at the Ninth Conference on Stroke and Cerebral Circulation in Arizona, it is the second most common hereditary thrombophilic condition in Mexican mestizos.1,2 Sticky platelet syndrome is an autosomal dominant disease with qualitative platelet alterations and familial occurrence characterized by platelet hyperreactivity with increased platelet aggregability in response to low concentrations of platelet agonists: epinephrine (EPI), adenosine diphosphate (ADP), or both.1–4 The diagnosis is based on platelet aggregometry, and according to this study, there are 3 types5:
Type I: Hyperaggregation after EPI and ADP.
Type II: Hyperaggregation after EPI alone.
Type III: Hyperaggregation after ADP alone.
Type II is the most common presentation in Caucasians, type I is frequent in Mexican mestizos,1 whereas type III is very uncommon.1,4–7 The clinical manifestations involve venous and arterial thrombosis, fetal loss, and fetal growth retardation.1,3,6,8,9 In this study, we analyze the localization of both the arterial and venous thrombotic events in a cohort of Mexican mestizo patients with the SPS.
Material and Methods
We conducted a retrospective, descriptive study in a period of 30 years, at a single center (Centro de Hematología y Medicina Interna de Puebla, Puebla, Mexico). We analyzed Mexican mestizo patients with a clinical marker of primary thrombophilia and a history of thrombosis.1 In this cohort, we recorded gender, type of SPS, type of thrombotic events, number of thrombotic events, and localization of the thrombosis (Table 1). All patients had a proven (angiography or doppler ultrasound) thrombotic episode and one of the clinical markers of a primary thrombophilic condition1, 5,7–11: (a) family history of thrombosis, (b) thrombosis at uncommon anatomic locations, and (c) resistance to conventional antithrombotic therapy. The SPS was defined by specific laboratory methods described by Mammen et al,4,12,13 Kubisz et al,6,7,14 and Ruiz-Delgado et al.1 Patients with clinical conditions related to secondary thrombophilia were excluded, as well as patients who had other inherited thrombophilic in addition to the SPS.15
Table 1.
Salient Features of the 86 Patients With Sticky Platelet Syndrome and Thrombosis.
| Arterial (n = 26) | Venous (n = 60) | P (<.05) | ||
|---|---|---|---|---|
| Age (years) | Mean | 36.6 | 38.8 | Ns |
| Median | 26 | 28 | Ns | |
| Gender | Male (%) | 3 (3) | 12 (13) | Ns |
| Female (%) | 23 (26) | 48 (58) | Ns | |
| SPS | Type 1 (%) | 14 (16) | 42 (49) | Ns |
| Type 2 (%) | 4 (5) | 5 (6) | Ns | |
| Type 3 (%) | 8 (9) | 13 (15) | Ns | |
Abbreviations: NS, non significant; SPS, sticky platelet syndrome.
Results
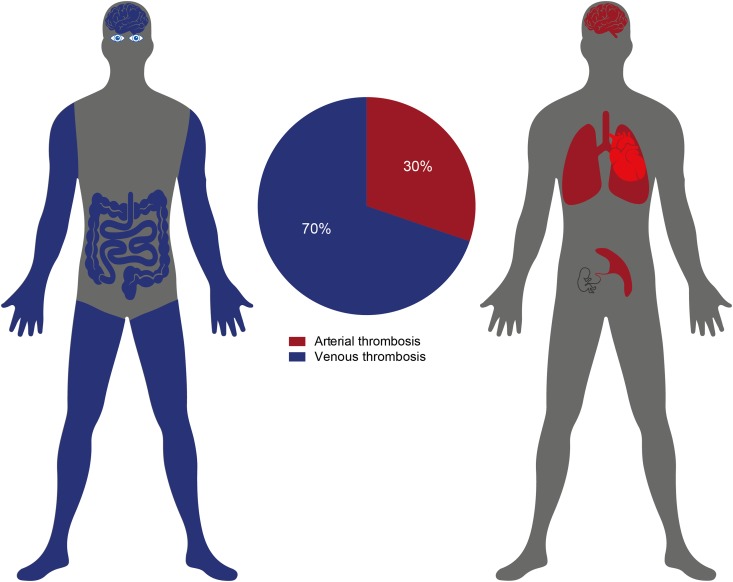
Based on the abovementioned criteria, we identified a cohort of 86 patients with SPS as the single thrombophilic condition; 15 (17%) were male and 71 (83%) were female. All of them were referred to our facility for evaluation after having suffered a thrombotic event and displaying at least one clinical marker of thrombophilia.1,11,15–18 In this cohort, we found SPS type I in 65%, type II in 10%, and type III in 25% of the patients (Tables 2 and 3). We also found that the thrombotic event was more frequently venous (70%) than arterial (30%) and that the localization of the venous thromboses were lower limbs (59%), central nervous system (13%), upper limbs (8%), mesenteric veins (7%), and retinal venous thrombosis (5%), whereas the arterial localizations were pulmonary embolism (50%), central nervous system (38%), placental infarction (9%), and only one case of myocardial infarction (see Figure 1). There was no association between the SPS type and the localization (arterial or venous) of the vaso-occlusive episode, and there was no correlation between gender and localization of the thrombosis nor between gender and the subtype of the SPS (see Tables 1 to 3).
Table 2.
Arterial and Venous Thrombosis in Patients With Sticky Platelet Syndrome According to the Subtype of the Condition.
| Arterial (%) | Venous (%) | P (<.05) | ||
|---|---|---|---|---|
| SPS type | Type 1 (n = 56) | 14 (54) | 42 (70) | Ns |
| Type 2 (n = 9) | 4 (16) | 5 (8) | Ns | |
| Type 3 (n = 21) | 8 (30) | 13 (22) | Ns | |
Abbreviations: NS, non significant; SPS, sticky platelet syndrome.
Table 3.
Frequency of Thrombotic Events Among Male and Female Patients With Sticky Platelet Syndrome According to the Subtype of the Condition.
| Arterial (n = 26) | Venous (n = 60) | P (<.05) | |||
|---|---|---|---|---|---|
| Male | Female | Male | Female | ||
| Type 1 (%) | 14 (25) | 3 (5) | 30 (54) | 9 (16) | Ns |
| Type 2 (%) | 1 (11) | 0 (0) | 5 (55) | 3 (34) | Ns |
| Type 3 (%) | 8 (38) | 0 (0) | 13 (62) | 0 (0) | Ns |
Abbreviation: NS, non significant.
Figure 1.
In the cohort of patients with the sticky platelet syndrome, the thrombotic event was more frequently venous (70%) than arterial (30%). In venous thrombosis, the localization was in lower limbs (59%), central nervous system (13%), upper limbs (8%), mesenteric veins (7%), and retinal venous thrombosis (5%), whereas in arterial thrombosis, the localizations were pulmonary embolism (50%), central nervous system (38%), placental infarction (9%), and only one case of myocardial infarction.
Discussion
Sticky platelet syndrome is an autosomal inherited platelet disorder, with familial occurrence.7,17 Although there are certain discrepancies about the inheritance pattern, it seems that the SPS may involve various mutations resulting in the different phenotypes; however, up to now, the diagnosis relies on clinical and laboratory criteria.7,10 There is limited data about the prevalence of this entity in the whole population; some data indicate that up to 15% of the general population displays the phenotype of the SPS, whereas more than 60% of persons with a clinical marker of thrombophilia are found to display the SPS phenotype.7,11,14–19 Other authors have found that the SPS is identified in approximately 21% of unexplained arterial thrombotic episodes and 13% of unexplained venous thromboembolism3,13; one of the possible reasons to explain these differences is the way to define the SPS; we and others1,7,11,18,19 have elected the criteria proposed by Mammen and Bick12,14,20–24 aiming to produce comparable results, but not all authors have employed the same criterion.12
Type II SPS is more frequent in Caucasians,2,3,25 whereas type I is the most frequent in Mexican mestizos,1,25 a population in which this condition is the second most frequent cause of thrombophilia.1,5,11,19 It has been previously shown that the SPS may lead to both arterial and venous thromboses3,11,13,24 and there are scant data about the localization of these vaso-occlusive episodes.7,14 Kubisz et al7 gathered data from several publications and described the localization of the thrombotic episodes in this condition, the distribution of the thrombotic episodes being similar to the ones that we are describing here.
The thrombotic episodes stemming from SPS have been described as anticoagulant resistant,6,25,24 this being important in selecting the antithrombotic therapeutic approach of such patients. In a prospective study, we have shown that the rethrombosis rate in persons with SPS treated with adequate antiplatelet drugs is as low as 3.6%,26 this observation supporting the need to include the investigation of the SPS in the studies of persons with suspected thrombophilia. In previous papers, we have shown that some persons with the SPS do thrombose sometimes in the presence of other thrombophilic conditions, either inherited or acquired,15 thus supporting the concept of multifactorial thrombophilia.15,27 In this cohort of patients, we have excluded those with other thrombophilic conditions, either inherited or acquired, in order to more precisely define the locations of the thrombotic episodes of persons with the SPS as the single thrombophilic condition.
In summary, we have described some features of the thrombotic episodes of the SPS presenting in Mexican mestizos, which are somehow different from those described in Caucasians: type I is the most frequent; it presents mainly in females; it is more frequently found in venous than in arterial thrombosis; and it is a frequent cause of lower limbs thromboses and pulmonary embolism. Additional studies are needed to define more precisely other clinical features of the SPS.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Ruiz-Delgado GJ, Cantero-Fortiz Y, Mendez-Huerta MA, et al. Primary thrombophilia in México XII: miscarriages are more frequent in persons with the sticky platelet syndrome (SPS). Turk J Hematol. 2017;34(3):239–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Holiday PL, Mammen E, Gilroy J. Sticky platelet syndrome and cerebral infarction in young adults. Paper Presented at: The Ninth International Joint Conference on Stroke and Cerebral Circulation; February 16-18, 1983; Phoenix, AZ. [Google Scholar]
- 3. Sokol J, Skerenova M, Jedinakova Z, et al. Progress in the understanding of sticky platelet syndrome. Semin Thromb Hemost. 2017;43(1):8–13. [DOI] [PubMed] [Google Scholar]
- 4. Mammen EF. Ten years’ experience with the “sticky platelet syndrome”. Clin Appl Thromb Hemost. 1995;1(1):66–72. [Google Scholar]
- 5. Ruiz-Arguelles GJ, González-Estrada S, Garces-Eisele J, Ruiz-Arguelles A. Primary thrombophilia in México: a prospective study. Am J Hematol. 1999;60(1):1–5. [DOI] [PubMed] [Google Scholar]
- 6. Kubisz P, Stanciakova L, Stasko J, et al. Sticky platelet syndrome: an important cause of life-threatening complications. Expert Rev Hematol. 2016;9(1):21–35. [DOI] [PubMed] [Google Scholar]
- 7. Kubisz P, Ruiz-Argüelles GJ, Stasko J, Holly P, Ruiz-Delgado GJ. Sticky platelet syndrome: history and future perspectives. Semin Thromb Hemost. 2014; 40(5):526–534. [DOI] [PubMed] [Google Scholar]
- 8. Velásquez A II, Carmona V, Ramos G. El síndrome de la plaqueta pegajosa: serie de casos en gestantes en el Hospital Militar Central. Rev Colomb Obstet Ginecol. 2004;55(3):232–239. [Google Scholar]
- 9. Emre T, Demir M. Sticky platelet syndrome in patients with uninduced venous thrombosis. Turk J Haematol. 2013;30(1):48–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Šimonová R, Bartosová L, Chudý P, et al. Nine kindreds of familial sticky platelet syndrome phenotype. Clin Appl Thromb Hemost. 2013;19(4):395–401. [DOI] [PubMed] [Google Scholar]
- 11. Ruiz-Argüelles GJ, Alarcón-Urdaneta C, Calderón-García J, Ruiz-Delgado GJ. Primary thrombophilia in México VIII: description of five kindreds of familial sticky platelet syndrome phenotype. Rev Hematol Mex. 2011;12(2):73–78. [Google Scholar]
- 12. Mammen EF. Sticky platelet syndrome. Semin Thromb Hemost. 1999;25(4):361–365. [DOI] [PubMed] [Google Scholar]
- 13. Mammen EF, Barnhart MI, Selik NR, Gilroy J, Klepach GL. “Sticky platelet syndrome”: a congenital platelet abnormality predisposing to thrombosis? Folia Haematol Int Mag Klin Morphol Blutforsch. 1988;115(3):361–365. [PubMed] [Google Scholar]
- 14. Kubisz P, Stasko J, Holly P. Sticky platelet syndrome. Semin Thromb Hemost. 2013;39(6):674–683. [DOI] [PubMed] [Google Scholar]
- 15. Ruiz-Argüelles GJ, López-Martínez B, Valdés-Tapia P, Gómez-Rangel JD, Reyes-Núñez V, Garcés-Eisele J. Primary thrombophilia in Mexico. V. A comprehensive prospective study indicates that most cases are multifactorial. Am J Hematol. 2005;78(1):21–26. [DOI] [PubMed] [Google Scholar]
- 16. Moncada B, Castillo-Martínez C, Ruiz-Argüelles GJ, Valdés-Tapia P, Arenas-Velázquez E. Sticky platelets syndrome: a frequent cause of primary thrombophilia. J Invest Dermatol. 2013;133(suppl 1):S180. [Google Scholar]
- 17. Johnson AD, Yanek LR, Chen MH, et al. Genome-wide meta-analyses identifies seven loci associated with platelet aggregation in response to agonists. Nat Genet. 2010;42(7):608–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ruiz-Argüelles GJ, López-Martínez B, Cruz-Cruz D, Esparza-Silva L, Reyes-Aulis MB. Primary thrombophilia in Mexico III: a prospective study of the sticky platelet syndrome. Clin Appl Thromb Hemost. 2002;8(3):273–277. [DOI] [PubMed] [Google Scholar]
- 19. Ruiz-Argüelles GJ, Ruiz-Delgado GJ. Trombofilia In: Ruiz-Argüelles GJ, Ruiz-Delgado GJ, eds. Fundamentos de Hematología, 5th ed Ciudad de México, Mexico: Editorial Médica Panamericana; 2014:287–296. [Google Scholar]
- 20. Staško J, Bartošová L, Mýtnik M, Kubisz P. Are the platelets activated in sticky platelet syndrome? Thromb Res. 2011;128(1):96–97. [DOI] [PubMed] [Google Scholar]
- 21. Mears KA, Van Stavern GP. Bilateral simultaneous anterior ischaemic optic neuropathy associated with sticky platelet syndrome. Br J Ophthalmol. 2009;93(7):885–886, 913. [DOI] [PubMed] [Google Scholar]
- 22. Randhawa S, Van Stavern GP. Sticky platelet syndrome and anterior ischaemic optic neuropathy. Clin Experiment Ophthalmol. 2007;35(8):779–781. [DOI] [PubMed] [Google Scholar]
- 23. Fodor M, Facskó A, Berényi E, Sziklai I, Berta A, Pfliegler G. Transient visual loss triggered by scuba diving in a patient with a petrous epidermoid and combined thrombotic risk factors. Pathophysiol Haemost Thromb. 2007;36(6):311–314. [DOI] [PubMed] [Google Scholar]
- 24. Bick RL. Sticky platelet syndrome: a common cause of unexplained arterial and venous thrombosis. Clin Appl Thromb Hemost. 1998;4(2):77–81. [Google Scholar]
- 25. Stanciakova L, Skerenova M, Holly P, et al. Genetic origin of the sticky platelet syndrome. Rev Hematol Mex. 2016;17(2):139–143. [DOI] [PubMed] [Google Scholar]
- 26. Velázquez-Sánchez-de-Cima S, Zamora-Ortiz G, Hernández-Reyes J, et al. Primary thrombophilia in México X: a prospective study of the treatment of the sticky platelet syndrome. Clin Appl Thromb Hemost. 2015;21(1):91–95. [DOI] [PubMed] [Google Scholar]
- 27. Ruiz-Argüelles GJ, González-Carrillo ML, Reyes-Núñez V, et al. Primary thrombophilia in México VI: lack of correlation among the inherited thrombophilic conditions. Gac Méd Méx. 2007;143:317–322. [PubMed] [Google Scholar]