Abstract
We examined the institutional variations in anticoagulation therapy for sepsis-induced disseminated intravascular coagulation (DIC) and their effects on patient outcomes. This post hoc analysis of a cohort study included 3195 patients with severe sepsis across 42 intensive care units. To evaluate differences in the intensity of anticoagulation therapy, the proportion of patients receiving anticoagulation therapy and the total number of patients with sepsis-induced DIC were compared. Predicted in-hospital mortality for each patient was calculated using logistic regression analysis. To evaluate survival outcomes, the actual/mean predicted in-hospital mortality ratio in each institution was calculated. Thirty-eight institutions with 2897 patients were included. Twenty-five institutions treated 60% to 100% (high-intensity institutions), while the rest treated 0% to 50% (low-intensity institutions) of patients with sepsis-induced DIC having anticoagulant therapy. Every 10-unit increase in the intensity of anticoagulant therapy was associated with lower in-hospital mortality (odds ratio: 0.904). A higher number of high-intensity institutions (compared to low-intensity institutions) had lower in-hospital mortality and fewer bleeding events than predicted. In conclusion, institutional variations existed in the use of anticoagulation therapy in patients with sepsis-induced DIC. High-intensity anticoagulation therapy was associated with better outcomes.
Keywords: anticoagulant therapy, sepsis, disseminated intravascular coagulation
Introduction
Sepsis, a highly inflammatory condition induced by infection, is associated with high mortality,1 despite the establishment of guidelines and treatment tools.2 Around 30% to 50% of all patients with sepsis have sepsis-induced disseminated intravascular coagulation (DIC). Disseminated intravascular coagulation leads to multiple organ dysfunction3 and high mortality (35%-40%). It is reported that the mortality rate in patients with sepsis having DIC is twice the rate in those without DIC.4–6 Some observational studies and meta-analyses revealed that anticoagulant therapy has survival benefits in patients with sepsis-induced DIC7–9; however, there are no complete randomized controlled trials focusing on such patients. Currently, the effect of anticoagulant therapy on patients with sepsis-induced DIC remains controversial, and there are no established treatment strategies for them.2
Institutional variations have been reported in various fields, and many relevant studies have been published recently, especially those on the management of traumatic brain injury,10–12 successfully resuscitated out-of-hospital cardiac arrest,13 congenital diaphragmatic hernia and gastroschisis,14 and prostate cancer.15 Variable management approaches in different institutions can change clinical outcomes.10,13–16 Closer monitoring of patient with brain injury10 or attempting cardiac surgery for single-ventricular lesions in younger children16 have shown to result in lower mortality. In the management of sepsis-induced DIC, there may be institutional variations in the use of anticoagulant therapy, where such treatment is permitted per medical insurance guidelines, which may impact outcomes. Clarifying the association between institutional variations and survival outcomes will help establish the appropriate strategy for managing patients with sepsis-induced DIC.
The aim of this study was to examine the institutional variations in the use of anticoagulation therapy for patients with sepsis-induced DIC in intensive care units (ICUs) in Japan and to elucidate whether those institutional variations impact outcomes.
Materials and Methods
This post hoc analysis was conducted as part of the Japan Septic Disseminated Intravascular Coagulation (JSEPTIC DIC) study (UMIN000012543 [University Hospital Medical Information Network Clinical Trials Registry]), in which 42 academic or centralized community institutions throughout Japan participated.4 This study was approved by The Independent Ethics Committee of Hokkaido University Graduate School of Medicine as the primary institution (reference number 013-0246), and all the Institutional Review Boards of the participating institutions (Supplementary Appendix 1). All boards waived the requirement for informed consent because of the retrospective nature of the study, in accordance with Japanese guidelines.17
Patient Selection and Data Collection
Patients admitted to ICUs with severe sepsis and septic shock were consecutively enrolled in the JSEPTIC DIC study between January 2011 and December 2013. The definitions used for severe sepsis and septic shock were according to the international guidelines for the management of severe sepsis and septic shock.18 Patients were excluded if they were <16 years of age and had developed severe sepsis and septic shock after ICU admission.
The following data were collected: age, sex, body weight, admission route to the ICU, preexisting organ dysfunction, preexisting hemostatic disorder, Acute Physiology and Chronic Health Evaluation (APACHE) II score,19 Sequential Organ Failure Assessment (SOFA) score20 upon admission, primary infection site, blood culture findings, microorganisms that caused sepsis, daily results of laboratory tests during the first week after ICU admission, treatment with agents including anticoagulants for anti-DIC, with other anticoagulants not for DIC, or with immunoglobulin and low-dose steroids during the first week after ICU admission, renal replacement therapy (RRT), RRT for nonrenal indications, polymyxin B-immobilized fiber column direct hemoperfusion (PMX-DHP), plasma exchange, extracorporeal membrane oxygenation (ECMO), and intra-aortic balloon pumping (IABP) during the first week after ICU admission; survival outcome at discharge from the hospital; and bleeding complications requiring any transfusion therapy during the first week after ICU admission. The severity of DIC was assessed using the DIC scoring algorithm of Japanese Association for Acute Medicine (JAAM).21 Patients with missing values were excluded from the analysis. The following data pertaining to the characteristics of the institutions were also collected: the type of ICU (general or emergency), ICU policy (open or closed), and the number of beds in the ICU. Institutions that enrolled 20 or fewer patients to the JSEPTIC study were excluded.
Definitions and Outcome Measures
To evaluate the intensity of anticoagulant therapy, the ratio of the number of patients with sepsis-induced DIC who received anticoagulant therapy to the total number of patients with sepsis-induced DIC in each institution was calculated. Patients with sepsis-induced DIC were defined as having sepsis and being free of preexisting hemostatic disorders. They had DIC scores ≥4 within 1 week after ICU admission (DIC scores were obtained on days 1, 3, or 7).
Anticoagulant agents comprised antithrombin, recombinant human thrombomodulin (rhTM), protease inhibitors, and heparins, which are frequently administered to patients with sepsis-induced DIC in Japan.22 Recombinant human-activated protein C is not available in the market in Japan. No predefined protocol for DIC treatment was available at any of the institutions. The attending physicians at each institution decided on the timing and choice of anticoagulants based on personal or institutional preferences. Anticoagulants were administered according to the medical insurance guidelines in Japan: In patients without severe renal dysfunction, 380 U/kg rhTM was administered for 6 days (130 U/kg/day rhTM for 6 days if the patient had experienced renal dysfunction), along with 20 to 39 mg/kg of gabexate mesylate or 0.06 to 0.20 mg/kg of nafamostat mesylate and 10 000 to 20 000 units of heparin until the resolution of DIC. Patients with antithrombin levels <70% received 1500 IU antithrombin for 3 days. Patients with venous thromboembolim (VTE) or at a risk of VTE, atrial fibrillation, and extracorporeal circulation received heparins in the ICUs. As data used to examine the aim (use of the anticoagulant therapies) were included in the JSEPTIC DIC database, patients were excluded if heparin was administered for reasons other than DIC treatment.
The main outcome of this study was in-hospital, all-cause mortality; secondary outcomes were the incidence of bleeding complications requiring transfusion therapy.
Statistical Analysis
Data are expressed as numbers (%) or medians (interquartile range) as appropriate. To evaluate the outcome in each institution, the predicted mortality for each patient was calculated using logistic regression, where the adjusted covariates were demographics, disease severity, treatments used upon arrival, and the characteristics of the institutions. The explanatory variables were age; sex; body weight; admission route to the ICU; preexisting organ dysfunction; preexisting hemostatic disorder; APACHE II score; SOFA score of the liver, respiratory system, cardiovascular system, central nervous system, and kidneys; primary infection site; blood culture findings; the causative microorganism in sepsis; white blood cell count; platelet count; prothrombin time-international normalized ratio; hemoglobin level; JAAM-DIC score upon admission; administered drugs including anticoagulants for DIC or non-DIC reasons, immunoglobulin, and low-dose steroids during the first week after ICU admission; RRT; RRT for non-renal indications; PMX-DHP; plasma exchange; ECMO; IABP during the first week after ICU admission; the type and policy of the ICU (general or emergency, and open or closed, respectively); the number of beds in the ICU; the intensity of anticoagulant therapy (the ratio of the number of patients with sepsis-induced DIC who received anticoagulant therapy to the total number of patients with sepsis-induced DIC in each institution); and the number of patients enrolled into the JSEPTIC DIC study by each institution. The ratio of actual mortality to mean predicted mortality of patients in each institution was used as the index for survival outcome in each institution. For the secondary outcome, the predicted incidence of bleeding complications was calculated using the same method as that used for predicted mortality. The numbers of institutions with better outcomes than expected were compared between institutions providing high- and low-intensity anticoagulation therapy using Fisher exact test. Data were analyzed using SAS software, version 13.2 (SAS Institute Inc., Cary, North Carolina). All statistical tests were performed with a 2-sided significance of 5%.
Results
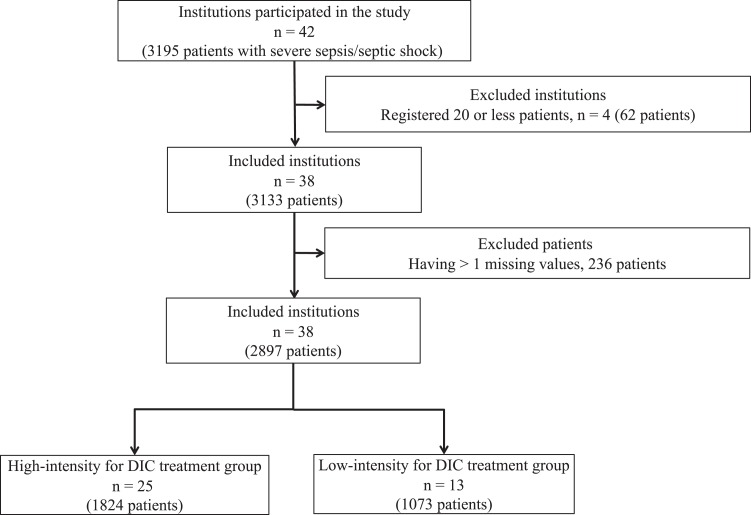
A total of 3195 consecutive patients with severe sepsis, admitted to 42 institutions, were enrolled in the JSEPTIC DIC study. Four institutions with 62 patients were excluded because they enrolled 20 or fewer patients to the JSEPTIC DIC study. Thirty-eight institutions were included in this analysis, including 3133 patients. Of this number, 236 were excluded because they had 1 or more missing values in the JSEPTIC DIC data set. Finally, 38 institutions with 2897 patients were included (Figure 1). Overall, 465 (34.4%) of 1351 patients with sepsis who received anticoagulant therapy and 454 (29.4%) of 1546 patients with sepsis who did not receive such treatment died. Mortality rate in patients with sepsis who also experienced DIC was 436 (36.5%) of 1192 in anticoagulants and 332 (38.4%) of 863 in patients with sepsis who did not receive anticoagulant therapy.
Figure 1.
PRISMA flow Chart of Institution and Participant Selection. DIC indicates disseminated intravascular coagulation.
Characteristics of the Institutions and Patients
The characteristics of the institutions are shown in Table 1. Data on demographics, disease severity, and treatments in each institution are shown in Supplemental Tables 1-3. There were institutional variations in terms of the intensity of anticoagulant therapy (Table 1 and Supplemental Figure 1). Twenty-five institutions administered anticoagulant therapy to 60% to 100% of patients with sepsis-induced DIC, while 7 institutions treated 30% to 50%, and 6 institutions treated 0% to 20% of such patients.
Table 1.
Patient Characteristics and Outcomes per Institution.
| Institution | No. of Patients, n | No. of Beds in ICU, n | ICU Type | ICU policy | Admission Route to ICU | Intensity of ACT for SI-DIC,a % | In-Hospital Mortality, n (%) | Bleeding Events, n (%) | ||
|---|---|---|---|---|---|---|---|---|---|---|
| ED, n (%) | Other, n (%) | Ward, n (%) | ||||||||
| 1 | 62 | 6 | Emergency | Open | 47 (72.6) | 17 (27.4) | 0 | 0/31 (0) | 19 (30.6) | 3 (4.8) |
| 2 | 54 | 7 | Emergency | Closed | 18 (33.3) | 25 (46.3) | 11 (20.4) | 44/50 (88.0) | 12 (22.2) | 3 (5.6) |
| 3 | 94 | 8 | General | Closed | 19 (10.6) | 37 (39.4) | 47 (50.0) | 46/72 (63.9) | 38 (40.4) | 6 (6.4) |
| 4 | 114 | 6 | General | Open | 86 (75.4) | 9 (7.9) | 19 (16.7) | 62/91 (68.1) | 42 (36.8) | 4 (3.5) |
| 5 | 39 | 8 | Emergency | Closed | 11 (28.2) | 22 (56.4) | 6 (15.4) | 24/37 (64.9) | 15 (38.5) | 3 (7.7) |
| 6 | 62 | 6 | Emergency | Open | 29 (46.8) | 17 (27.4) | 16 (25.8) | 33/44 (75.0) | 23 (37.1) | 3 (4.8) |
| 7 | 23 | 6 | General | Open | 19 (82.6) | 4 (17.3) | 0 | 17/18 (94.4) | 13 (56.5) | 6 (26.1) |
| 8 | 80 | 12 | General | Closed | 17 (21.3) | 6 (7.5) | 57 (71.3) | 55/63 (87.3) | 23 (28.8) | 13 (16.3) |
| 9 | 58 | 19 | Emergency | Open | 23 (39.7) | 35 (60.3) | 0 | 3/47 (6.4) | 18 (31.0) | 12 (20.7) |
| 10 | 127 | 12 | General | Closed | 84 (66.1) | 12 (9.4) | 31 (24.4) | 36/93 (38.7) | 35 (27.6) | 15 (11.8) |
| 11 | 40 | 14 | General | Open | 3 (7.5) | 32 (80.0) | 5 (12.5) | 23/25 (92.0) | 5 (12.5) | 3 (7.5) |
| 12 | 43 | 6 | Emergency | Other | 12 (28.0) | 31 (72.1) | 0 | 37/39 (94.9) | 7 (16.3) | 8 (18.6) |
| 13 | 117 | 12 | Emergency | Closed | 6 (5.1) | 45 (38.5) | 66 (56.4) | 67/103 (65.0) | 46 (39.3) | 3 (2.6) |
| 14 | 21 | 11 | General | Closed | 7 (33.3) | 11 (52.4) | 3 (14.9) | 12/15 (80.0) | 6 (28.6) | 3 (14.3) |
| 15 | 140 | 7 | Emergency | Closed | 63 (45.0) | 34 (24.3) | 43 (30.7) | 71/116 (0.612) | 51 (36.4) | 15 (10.7) |
| 16 | 76 | 10 | General | Open | 26 (34.2) | 15 (19.7) | 35 (46.1) | 38/51 (74.5) | 18 (23.7) | 12 (15.8) |
| 17 | 99 | 18 | Emergency | Closed | 37 (37.4) | 60 (60.1) | 2 (2.0) | 28/75 (37.3) | 25 (25.3) | 11 (11.1) |
| 18 | 186 | 20 | General | Closed | 66 (35.5) | 9 (4.8) | 111 (59.7) | 4/124 (3.2) | 80 (43.0) | 9 (4.8) |
| 19 | 23 | 15 | Emergency | Open | 5 (21.7) | 17 (73.9) | 1 (4.3) | 11/17 (64.7) | 3 (13.0) | 2 (8.7) |
| 20 | 99 | 20 | Emergency | Other | 31 (31.3) | 62 (62.6) | 6 (6.1) | 45/70 (64.3) | 20 (20.2) | 11 (11.1) |
| 21 | 136 | 10 | Emergency | Closed | 51 (37.5) | 83 (61.0) | 2 (1.5) | 55/88 (62.5) | 40 (29.4) | 19 (14.0) |
| 22 | 123 | 12 | General | Other | 55 (44.7) | 22 (17.9) | 46 (37.4) | 64/71 (90.1) | 35 (28.5) | 31 (25.2) |
| 23 | 45 | 20 | Emergency | Other | 8 (17.8) | 35 (77.8) | 2 (4.4) | 23/24 (95.8) | 6 (13.3) | 11 (24.4) |
| 24 | 87 | 20 | Emergency | Closed | 53 (60.9) | 34 (39.1) | 0 | 40/63 (63.5) | 35 (40.2) | 0 |
| 25 | 31 | 10 | General | Open | 19 (61.3) | 3 (9.7) | 9 (29.0) | 23/27 (85.2) | 8 (25.8) | 5 (16.1) |
| 26 | 27 | 4 | General | Open | 12 (44.4) | 0 | 15 (55.6) | 20/24 (83.3) | 12 (44.4) | 17 (63.0) |
| 27 | 50 | 8 | General | Other | 9 (18.0) | 7 (14.0) | 34 (68.0) | 39/43 (90.7) | 29 (58.0) | 9 (18.0) |
| 28 | 21 | 10 | General | Open | 9 (42.9) | 0 | 12 (57.1) | 7/15 (46.7) | 10 (47.6) | 2 (9.5) |
| 29 | 45 | 12 | General | Closed | 13 (28.9) | 5 (11.1) | 27 (60.0) | 3/30 (10.0) | 19 (42.2) | 7 (15.6) |
| 30 | 113 | 10 | General | Closed | 34 (30.1) | 17 (15.0) | 62 (54.9) | 63/85 (74.1) | 31 (27.4) | 19 (16.8) |
| 31 | 26 | 8 | General | Open | 20 (76.9) | 5 (19.2) | 1 (3.8) | 7/16 (43.8) | 11 (42.4) | 3 (11.5) |
| 32 | 150 | 30 | Emergency | Closed | 136 (90.1) | 3 (2.0) | 11 (7.3) | 40/86 (46.5) | 33 (22.0) | 24 (16.0) |
| 33 | 123 | 18 | General | Open | 95 (77.2) | 8 (6.5) | 20 (16.3) | 14/73 (19.2) | 43 (35.0) | 5 (4.1) |
| 34 | 79 | 16 | General | Other | 45 (57.0) | 20 (25.3) | 14 (17.7) | 42/54 (77.8) | 18 (22.8) | 18 (22.8) |
| 35 | 23 | 14 | General | Closed | 0 | 0 | 23 (100) | 1/14 (7.1) | 9 (39.1) | 1 (4.3) |
| 36 | 127 | 10 | Emergency | Open | 102 (80.3) | 12 (9.4) | 13 (10.2) | 20/66 (30.3) | 41 (32.3) | 5 (3.9) |
| 37 | 26 | 12 | General | Open | 20 (76.9) | 2 (7.7) | 4 (15.4) | 5/11 (45.5) | 10 (38.5) | 1 (3.8) |
| 38 | 108 | 20 | Emergency | Open | 43 (39.8) | 29 (26.9) | 36 (33.3) | 70/86 (81.4) | 30 (27.8) | 13 (12.0) |
Abbreviations: ED, emergency department; Other, other hospital; ward, hospital ward; ACT, anticoagulant therapy; SI-DIC, sepsis-induced disseminated intravascular coagulation; ICU, intensive care unit.
aIntensity of anticoagulant therapy for sepsis-induced DIC indicates the ratio of the number of patients with sepsis-induced-DIC who received anticoagulant therapy to the number of patients with sepsis-induced DIC.
Intensity of Anticoagulant Therapy and Survival Outcomes
In the logistic regression model, in which the covariates described in the Methods section were adjusted, the intensity of anticoagulant therapy was associated with lower in-hospital mortality, with an odds ratio of 0.904 (95% confidence interval 0.842-0.970) for every 10-point increase in the intensity of anticoagulant therapy (Table 2).
Table 2.
Logistic Regression Analysis of in-Hospital Mortality.
| Odds ratio (95% CI) | |
|---|---|
| Intensity of anticoagulant therapy for sepsis-induced DICa (for every 10-point increase) | 0.904 (0.842-970) |
| Age (in each 10 years) | 1.28 (1.17 -1.38) |
| Sex, female | 0.746 (0.60-0.924) |
| Body weight | 0.990 (0.981-0.998) |
| APACHE II score | 1.037 (1.019 -1.055) |
| JAAM DIC score | 1.135 (1.069 -1.04) |
| Pre-existing liver insufficiency | 2.326 (1.083-4.975) |
| Preexisting chronic heart failure | 2.146 (1.418-3.236) |
| Preexisting chronic hemodialysis | 1.481 (1.004-2.183) |
| Preexisting immunocompromised status | 1.426 (1.076 -1.988) |
| Preexisting hematologic malignancy | 1.905 (1.067-3.401) |
| Hemoglobin level on admission | 0.924 (0.886-0.964) |
| Blood culture positive (vs negative) | 1.305 (1.021 -1.667) |
Abbreviations: APACHE, Acute Physiology and Chronic Health Evaluation; CI, confidence interval; DIC, disseminated intravascular coagulation; JAAM, Japanese Association for Acute Medicine.
aIntensity of anticoagulant therapy for sepsis-induced DIC indicates the ratio of the number of patients with sepsis-induced-DIC who received anticoagulant therapy to the number of patients with sepsis-induced DIC.
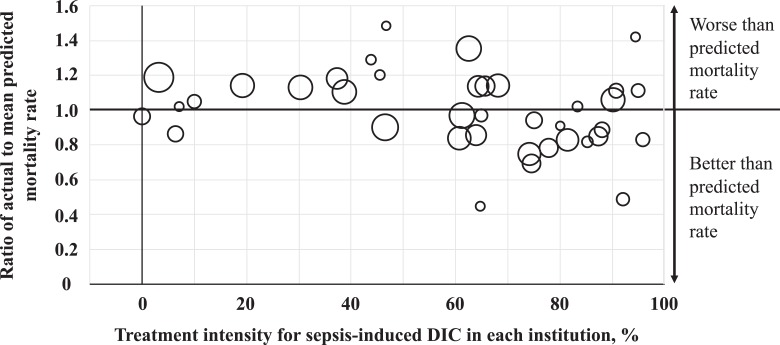
Data on actual mortality, mean predicted mortality, and actual/mean predicted mortality ratio are shown in Supplementary Table 3. An actual/mean predicted mortality ratio value <1 indicated better outcomes than predicted, whereas a ratio >1 indicated worse outcomes than predicted. The relationship between the actual/mean predicted mortality ratio and the intensity of anticoagulant therapy is shown in Figure 2. Based on the distribution observed in Figure 2 (and Supplemental Figure 1), the institutions were divided into 2 groups according to the intensity of anticoagulant therapy: >60% (high-intensity institutions) or <50% (low-intensity institutions). A higher number of high-intensity institutions had an actual/mean predicted mortality ratio <1 (16 of 25, 64.0%) compared to the low-intensity institutions (3 of 13, 23.1%; P = .0382). The relationship between actual/mean predicted mortality ratio and the intensity of anticoagulant therapy in patients having severe sepsis with or without DIC is shown in Supplementary Figure 2-1.
Figure 2.
Actual to mean predicted mortality ratio and intensity of anticoagulant therapy for sepsis-induced DIC in each institution. The intensity of anticoagulant therapy for sepsis-induced DIC indicates the ratio of the number of patients who received anticoagulant therapy to the number of patients with sepsis-induced DIC in each institution. The size of the circle indicates the volume of patients with sepsis-induced DIC in each institution. DIC indicates disseminated intravascular coagulation.
Intensity of Anticoagulant Therapy and Bleeding Events
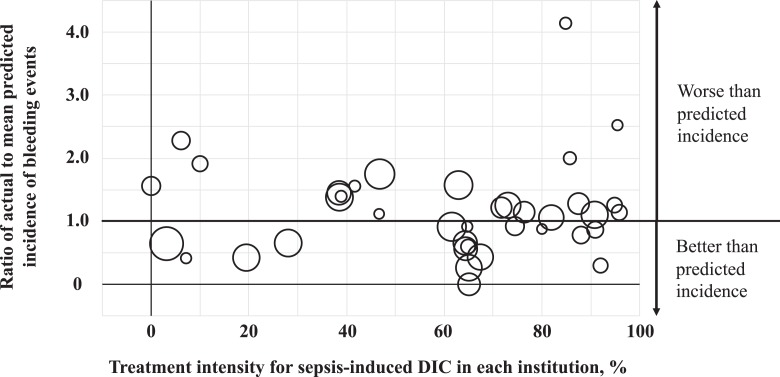
The actual incidence of bleeding events (requiring any transfusion therapy), mean predicted incidence of bleeding events, and the actual/mean predicted incidence of bleeding events’ ratio are shown in Supplemental Table 3. An actual/mean predicted incidence of bleeding events ratio <1 indicated better outcomes than predicted, whereas a ratio >1 predicted worse outcomes. The relationship between the actual/mean predicted incidence of bleeding events ratio and the intensity of anticoagulant therapy is shown in Figure 3. A higher number of high-intensity institutions had an actual/mean predicted incidence of bleeding events ratio lower than 1 (15 of 25, 60.0%) than the low-intensity institutions (3 of 13, 23.1%; P = .0434). The relationship between actual/mean predicted incidence of bleeding events ratio and the intensity of anticoagulant therapy in patients having severe sepsis with or without DIC is shown in Supplementary Figure 2-2.
Figure 3.
Ratio of actual to mean predicted incidence of bleeding events and intensity of anticoagulant therapy for sepsis-induced DIC in each institution. Bleeding events indicate the presence of events requiring any transfusion therapy. The intensity of anticoagulant therapy for sepsis-induced DIC indicates the ratio of the number of patients who received anticoagulant therapy to the number of patients with sepsis-induced DIC in each institution. The size of the circle indicates the volume of patients with sepsis-induced DIC in each institution. DIC indicates disseminated intravascular coagulation.
Discussion
In this study, we observed institutional variations in the intensity of anticoagulation therapy in patients with sepsis-induced DIC in academic and centralized community institutions in Japan, which impacted outcomes. Institutions providing a higher intensity of anticoagulation therapy for patients with sepsis-induced DIC had lower in-hospital mortality and lower incidence of bleeding events. This study did not focus on a single drug or intervention but on the preference or strategies of the institutions. To our knowledge, this is the first study to examine institutional variations in the use of anticoagulation therapy for patients with sepsis-induced DIC in intensive care units in Japan and to elucidate their association with outcomes.
In our study, two-third of the institutions provided anticoagulation therapy to >60% of patients with sepsis-induced DIC, while the rest provided anticoagulation therapy to <50% of such patients. In the latest international guidelines on the management of sepsis and septic shock, the use of anticoagulants is not recommended in patients with sepsis, even in the presence of DIC.2 However, a recent meta-analysis suggested that anticoagulation therapy is beneficial only to patients with sepsis-induced DIC and not the entire population of patients with sepsis.8 Besides, the Guidance for diagnosis and treatment of DIC by the International Society on Thrombosis and Haemostasis (ISTH) states that therapeutic doses of heparin should be considered in cases of DIC where thrombosis is predominant. The administration of AT, recombinant human TM (rhTM), may even be considered in patients with DIC.23 The use of anticoagulants is allowed only in patients with DIC per medical insurance guidelines in Japan. In addition, in the Japanese clinical practice guidelines for the management of sepsis and septic shock, anticoagulant therapy recommendations, or suggestions are limited to patients with sepsis-induced DIC.22 These guidelines suggest the use of antithrombin and recommend against the use of protease inhibitor, heparin, and heparin analogs. The guidelines do not offer clear recommendations on the use of rhTM. In practice, the use of anticoagulants, especially antithrombin and rhTM, in patients with sepsis-induced DIC may depend on the preferences of the physicians or institutions.
Institutional variations in disease management have been shown in various fields10–16 and are associated with survival outcomes in some cases. Trauma centers providing high-intensity ICP monitoring of patients with severe traumatic brain injury,10 and institutions with a higher presence of cardiologists (as admitting consultants) in the treatment of successfully resuscitated out-of-hospital patients with cardiac arrest were associated with better survival outcomes.13 In addition, Yamakawa et al recently showed that screening patients with severe sepsis for DIC impacted survival outcomes.24 To diagnose patients with severe sepsis as having sepsis-induced DIC, several blood values are required,21,25 but about 30% of the patients in the database lacked 1 or more of these values for DIC diagnosis. Patients without missing values had decreased in-hospital mortality. Interestingly, the provision of ICP monitoring, presence of a cardiologist (as a consultant), and screening for diagnosis (despite not being regarded as treatment measures) were associated with better survival outcomes. In the current study, not all patients with sepsis-induced DIC (60%-90%) received anticoagulation therapy in high-intensity institutions. However, institutions providing a higher intensity of therapy had better survival outcomes. The results of the aforementioned studies suggest that treatment preference or strategy impacts clinical outcomes.10,13,24
The presence of an association between institutional volume and treatment-associated complications has been reported in the field of percutaneous coronary intervention,26 abdominal aortic aneurysm treatment,27 nephrectomy,28 hypospadias surgery,29 gastrectomy,30 and spine surgery.31 In our study, the volume of patients with severe sepsis or sepsis-induced DIC who received anticoagulation therapy was not associated with the incidence of bleeding events (Supplemental Figure 3). However, the intensity of the treatment (the ratio of the number of patients who received anticoagulant therapy to those with sepsis-induced DIC) was associated with a lower number of bleeding events. These results suggest that the presence of experienced physicians and/or institutional characteristics lowers complication incidence rates.
Limitations
There were some limitations to the current study, including those pertaining to its retrospective design. First, the exact timing of the administration of anticoagulant agents to the patients in each institution was not known. However, anticoagulant therapies and other therapeutic interventions are usually administered within a few hours after admission. We regarded that it is acceptable for anticoagulant therapies and therapeutic interventions to be used as explanatory variables in the logistic regression model for calculating the predicted mortality and incidence of bleeding events because the use of anticoagulant therapies did not influence the use of other interventional therapies. The results of laboratory testing after the initiation of anticoagulant therapy were not used as explanatory variables. Second, data on the exact dose and treatment duration of anticoagulant agents were not recorded in the database, so we were unable to identify whether all patients in all institutions received the same medication dose. However, anticoagulant agents were administered according to the medical insurance guidelines in Japan as described in detail under the subheading Definitions and outcome measures in Material and Methods section. Therefore, the dose and treatment duration did not vary between different institutions. Third, we only used the DIC scoring algorithm of JAAM to diagnose DIC in this study. Previous studies have reported varied outcomes depending on the scoring algorithms used.5,32 Thus, our results might also change if another scoring algorithm, such as ISTH system, was used to diagnose DIC. The sensitivity of JAAM scoring algorithm for mortality was reportedly higher in DIC.5,32 Therefore, we applied this scoring algorithm in this study. Finally, there may have been unknown confounders that we did not include as explanatory variables, which might have affected the results.
Conclusions
The current study elucidated that there were institutional variations in the use of anticoagulation therapy in patients with sepsis-induced DIC in academic and centralized community institutions in Japan. It also indicated that institutions providing high-intensity anticoagulation therapy had better survival outcomes and lower rate of adverse events. These results suggest that the preference or strategy used for anticoagulation therapy for patients with sepsis-induced DIC impacts their outcomes, which may help in developing appropriate strategies and policies. To generalize these results, a further observational study with a higher number of institutions providing both high- and low-intensity anticoagulation therapy across various regions and countries is needed.
Supplemental Material
Supplemental Material, Appendix1_Ethics_committee_071618 for The Treatment Intensity of Anticoagulant Therapy for Patients With Sepsis-Induced Disseminated Intravascular Coagulation and Outcomes: A Multicenter Cohort Study by Daisuke Kudo, Mineji Hayakawa, Hiroaki Iijima, Kazuma Yamakawa, Shinjiro Saito, Shigehiko Uchino, Yusuke Iizuka, Masamitsu Sanui, Kohei Takimoto, Toshihiko Mayumi, and JSEPTIC DIC Study Investigators in Clinical and Applied Thrombosis/Hemostasis
Supplemental Material
Supplemental Material, CATHAppendix2_List_authors_082418_(1) for The Treatment Intensity of Anticoagulant Therapy for Patients With Sepsis-Induced Disseminated Intravascular Coagulation and Outcomes: A Multicenter Cohort Study by Daisuke Kudo, Mineji Hayakawa, Hiroaki Iijima, Kazuma Yamakawa, Shinjiro Saito, Shigehiko Uchino, Yusuke Iizuka, Masamitsu Sanui, Kohei Takimoto, Toshihiko Mayumi, and JSEPTIC DIC Study Investigators in Clinical and Applied Thrombosis/Hemostasis
Supplemental Material
Supplemental Material, Supplemental_figure_1 for The Treatment Intensity of Anticoagulant Therapy for Patients With Sepsis-Induced Disseminated Intravascular Coagulation and Outcomes: A Multicenter Cohort Study by Daisuke Kudo, Mineji Hayakawa, Hiroaki Iijima, Kazuma Yamakawa, Shinjiro Saito, Shigehiko Uchino, Yusuke Iizuka, Masamitsu Sanui, Kohei Takimoto, Toshihiko Mayumi, and JSEPTIC DIC Study Investigators in Clinical and Applied Thrombosis/Hemostasis
Supplemental Material
Supplemental Material, Supplemental_figure_3 for The Treatment Intensity of Anticoagulant Therapy for Patients With Sepsis-Induced Disseminated Intravascular Coagulation and Outcomes: A Multicenter Cohort Study by Daisuke Kudo, Mineji Hayakawa, Hiroaki Iijima, Kazuma Yamakawa, Shinjiro Saito, Shigehiko Uchino, Yusuke Iizuka, Masamitsu Sanui, Kohei Takimoto, Toshihiko Mayumi, and JSEPTIC DIC Study Investigators in Clinical and Applied Thrombosis/Hemostasis
Supplemental Material
Supplemental Material, Suppl_figure_2_021519_(1) for The Treatment Intensity of Anticoagulant Therapy for Patients With Sepsis-Induced Disseminated Intravascular Coagulation and Outcomes: A Multicenter Cohort Study by Daisuke Kudo, Mineji Hayakawa, Hiroaki Iijima, Kazuma Yamakawa, Shinjiro Saito, Shigehiko Uchino, Yusuke Iizuka, Masamitsu Sanui, Kohei Takimoto, Toshihiko Mayumi, and JSEPTIC DIC Study Investigators in Clinical and Applied Thrombosis/Hemostasis
Acknowledgments
This manuscript was edited by a native English speaker associated with Editage, Tokyo, Japan. We would like to thank the JSEPTIC DIC study investigators for contributing to the data collection and assessment (Online Appendix 2): Takeo Azuhata, Fumihito Ito, Shodai Yoshihiro, Katsura Hayakawa, Tsuyoshi Nakashima, Takayuki Ogura, Eiichiro Noda, Yoshihiko Nakamura, Ryosuke Sekine, Yoshiaki Yoshikawa, Motohiro Sekino, Keiko Ueno, Yuko Okuda, Masayuki Watanabe, Akihito Tampo, Nobuyuki Saito, Yuya Kitai, Hiroki Takahashi, Iwao Kobayashi, Yutaka Kondo, Wataru Matsunaga, Sho Nachi, Toru Miike, Hiroshi Takahashi, Shuhei Takauji, Kensuke Umakoshi, Takafumi Todaka, Hiroshi Kodaira, Kohkichi Andoh, Takehiko Kasai, Yoshiaki Iwashita, Hideaki Arai, Masato Murata, Masahiro Yamane, Kazuhiro Shiga, and Naoto Hori.
Authors’ Note: The data sets generated and analyzed during the current study are available in the University Hospital Medical Information Network Individual Case Data Repository (UMIN000012543, http://www.umin.ac.jp/icdr/index-j.html).
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: M.H. received grants and personal fees from Asahi Kasei Pharma Corporation, and personal fees from the Japan Blood Products Organization and Nihon Pharmaceutical Co., Ltd. The other authors declare that there is no conflict of interest.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by JSPS KAKENHI Grant Number 15K20331.
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Fleischmann C, Scherag A, Adhikari NK, et al. Assessment of global incidence and mortality of hospital-treated sepsis. Current estimates and limitations. Am J Respir Crit Care Med. 2016;193(3):259–272. [DOI] [PubMed] [Google Scholar]
- 2. Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43(3):304–377. [DOI] [PubMed] [Google Scholar]
- 3. Levi M, Schultz M, van der Poll T. Sepsis and thrombosis. Semin Thromb Hemost. 2013;39(5):559–566. [DOI] [PubMed] [Google Scholar]
- 4. Hayakawa M, Saito S, Uchino S, et al. Characteristics, treatments, and outcomes of severe sepsis of 3195 ICU-treated adult patients throughout Japan during 2011-2013. J Intensive Care. 2016;4:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kushimoto S, Gando S, Saitoh D, et al. Clinical course and outcome of disseminated intravascular coagulation diagnosed by Japanese Association for Acute Medicine criteria. Comparison between sepsis and trauma. Thromb Haemost. 2008;100(6):1099–1105. [PubMed] [Google Scholar]
- 6. Zeerleder S, Hack CE, Wuillemin WA. Disseminated intravascular coagulation in sepsis. Chest. 2005;128(4):2864–2875. [DOI] [PubMed] [Google Scholar]
- 7. Kienast J, Juers M, Wiedermann CJ, et al. Treatment effects of high-dose antithrombin without concomitant heparin in patients with severe sepsis with or without disseminated intravascular coagulation. J Thromb Haemost. 2006;4(1):90–97. [DOI] [PubMed] [Google Scholar]
- 8. Umemura Y, Yamakawa K, Ogura H, Yuhara H, Fujimi S. Efficacy and safety of anticoagulant therapy in three specific populations with sepsis: a meta-analysis of randomized controlled trials. J Thromb Haemost. 2016;14(3):518–530. [DOI] [PubMed] [Google Scholar]
- 9. Yamakawa K, Ogura H, Fujimi S, et al. Recombinant human soluble thrombomodulin in sepsis-induced disseminated intravascular coagulation: a multicenter propensity score analysis. Intensive Care Med. 2013;39(4):644–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bulger EM, Nathens AB, Rivara FP, et al. Management of severe head injury: institutional variations in care and effect on outcome. Crit Care Med. 2002;30(8):1870–1876. [DOI] [PubMed] [Google Scholar]
- 11. Cnossen MC, Huijben JA, van der Jagt M, et al. Variation in monitoring and treatment policies for intracranial hypertension in traumatic brain injury: a survey in 66 neurotrauma centers participating in the CENTER-TBI study. Crit Care. 2017;21(1):233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Huijben JA, Volovici V, Cnossen MC, et al. Variation in general supportive and preventive intensive care management of traumatic brain injury: a survey in 66 neurotrauma centers participating in the Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI) study. Crit Care. 2018;22(1):90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Couper K, Kimani PK, Gale CP, et al. Patient, health service factors and variation in mortality following resuscitated out-of-hospital cardiac arrest in acute coronary syndrome: analysis of the Myocardial Ischaemia National Audit Project. Resuscitation. 2018;124:49–57. [DOI] [PubMed] [Google Scholar]
- 14. Baird R, Eeson G, Safavi A, et al. Institutional practice and outcome variation in the management of congenital diaphragmatic hernia and gastroschisis in Canada: a report from the Canadian Pediatric Surgery Network. J Pediatr Surg. 2011;46(5):801–807. [DOI] [PubMed] [Google Scholar]
- 15. Ong WL, Foroudi F, Evans S, Millar J. Large institutional variations in use of androgen deprivation therapy with definitive radiotherapy in a population-based cohort of men with intermediate- and high-risk prostate cancer. BJU Int. 2017;120(Suppl 3):35–42. [DOI] [PubMed] [Google Scholar]
- 16. Hill GD, Rudd NA, Ghanayem NS, Hehir DA, Bartz PJ. Center variability in timing of stage 2 palliation and association with interstage mortality: a report from the National Pediatric Cardiology Quality Improvement Collaborative. Pediatr Cardiol. 2016;37(8):1516–1524. [DOI] [PubMed] [Google Scholar]
- 17. Ministry of Education Culture, Sports, Science and Technology, and Ministry of Health, Labour and Welfare, JAPAN. Ethical Guidelines for Medical and Health Research Involving Human Subjects, 2015. http://www.mhlw.go.jp/file/06-Seisakujouhou-10600000-Daijinkanboukouseikagakuka/0000080278.pdf. (accessed 20 July, 2018)
- 18. Dellinger RP, Levy MM, Carlet JM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med. 2008;34(1):17–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–829. [PubMed] [Google Scholar]
- 20. Vincent JL, de Mendonca A, Cantraine F, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998;26(11):1793–1800. [DOI] [PubMed] [Google Scholar]
- 21. Gando S, Iba T, Eguchi Y, et al. A multicenter, prospective validation of disseminated intravascular coagulation diagnostic criteria for critically ill patients: comparing current criteria. Crit Care Med. 2006;34(3):625–631. [DOI] [PubMed] [Google Scholar]
- 22. Nishida O, Ogura H, Egi M, et al. The Japanese Clinical Practice Guidelines for Management of Sepsis and Septic Shock 2016 (J-SSCG 2016). Acute Med Surg. 2018;5(1):3–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wada H, Thachil J, Di Nisio M, et al. Guidance for diagnosis and treatment of DIC from harmonization of the recommendations from three guidelines. J Thromb Haemost. 2013;11:761–767. [DOI] [PubMed] [Google Scholar]
- 24. Umemura Y, Yamakawa K, Hayakawa M, Hamasaki T, Fujimi S; Japan Septic Disseminated Intravascular Coagulation (J-Septic DIC) study group. Screening itself for disseminated intravascular coagulation may reduce mortality in sepsis: a nationwide multicenter registry in Japan. Thromb Res. 2018;161:60–66. [DOI] [PubMed] [Google Scholar]
- 25. Taylor FB, Jr, Toh CH, Hoots WK, Wada H, Levi M; Scientific Subcommittee on Disseminated Intravascular Coagulation (DIC) of the International Society on Thrombosis and Haemostasis (ISTH). Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost. 2001;86(5):1327–1330. [PubMed] [Google Scholar]
- 26. Kimmel SE, Berlin JA, Laskey WK. The relationship between coronary angioplasty procedure volume and major complications. JAMA. 1995;274(14):1137–1142. [PubMed] [Google Scholar]
- 27. Trenner M, Kuehnl A, Salvermoser M, et al. Editor’s Choice - High annual hospital volume is associated with decreased in hospital mortality and complication rates following treatment of abdominal aortic aneurysms: secondary data analysis of the nationwide German DRG Statistics from 2005 to 2013. Eur J Vasc Endovasc Surg. 2018;55(2):185–194. [DOI] [PubMed] [Google Scholar]
- 28. Arora S, Keeley J, Pucheril D, Menon M, Rogers CG. What is the hospital volume threshold to optimize inpatient complication rate after partial nephrectomy? Urol Oncol. 2018;36(7):339, e17,–339. e23. [DOI] [PubMed] [Google Scholar]
- 29. Wilkinson DJ, Green PA, Beglinger S, et al. Hypospadias surgery in England: higher volume centres have lower complication rates. J Pediatr Urol. 2017;13(5):481, e1,–481. e6. [DOI] [PubMed] [Google Scholar]
- 30. Kurokawa Y, Yamaguchi T, Sasako M, et al. Institutional variation in short- and long-term outcomes after surgery for gastric or esophagogastric junction adenocarcinoma: correlative study of two randomized phase III trials (JCOG9501 and JCOG9502). Gastric Cancer. 2017;20(3):508–516. [DOI] [PubMed] [Google Scholar]
- 31. Paul JC, Lonner BS, Goz V, et al. Complication rates are reduced for revision adult spine deformity surgery among high-volume hospitals and surgeons. Spine J. 2015;15(9):1963–1972. [DOI] [PubMed] [Google Scholar]
- 32. Takemitsu T, Wada H, Hatada T, et al. Prospective evaluation of three different diagnostic criteria for disseminated intravascular coagulation. Thromb Haemost. 2011;105(1):40–44. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, Appendix1_Ethics_committee_071618 for The Treatment Intensity of Anticoagulant Therapy for Patients With Sepsis-Induced Disseminated Intravascular Coagulation and Outcomes: A Multicenter Cohort Study by Daisuke Kudo, Mineji Hayakawa, Hiroaki Iijima, Kazuma Yamakawa, Shinjiro Saito, Shigehiko Uchino, Yusuke Iizuka, Masamitsu Sanui, Kohei Takimoto, Toshihiko Mayumi, and JSEPTIC DIC Study Investigators in Clinical and Applied Thrombosis/Hemostasis
Supplemental Material, CATHAppendix2_List_authors_082418_(1) for The Treatment Intensity of Anticoagulant Therapy for Patients With Sepsis-Induced Disseminated Intravascular Coagulation and Outcomes: A Multicenter Cohort Study by Daisuke Kudo, Mineji Hayakawa, Hiroaki Iijima, Kazuma Yamakawa, Shinjiro Saito, Shigehiko Uchino, Yusuke Iizuka, Masamitsu Sanui, Kohei Takimoto, Toshihiko Mayumi, and JSEPTIC DIC Study Investigators in Clinical and Applied Thrombosis/Hemostasis
Supplemental Material, Supplemental_figure_1 for The Treatment Intensity of Anticoagulant Therapy for Patients With Sepsis-Induced Disseminated Intravascular Coagulation and Outcomes: A Multicenter Cohort Study by Daisuke Kudo, Mineji Hayakawa, Hiroaki Iijima, Kazuma Yamakawa, Shinjiro Saito, Shigehiko Uchino, Yusuke Iizuka, Masamitsu Sanui, Kohei Takimoto, Toshihiko Mayumi, and JSEPTIC DIC Study Investigators in Clinical and Applied Thrombosis/Hemostasis
Supplemental Material, Supplemental_figure_3 for The Treatment Intensity of Anticoagulant Therapy for Patients With Sepsis-Induced Disseminated Intravascular Coagulation and Outcomes: A Multicenter Cohort Study by Daisuke Kudo, Mineji Hayakawa, Hiroaki Iijima, Kazuma Yamakawa, Shinjiro Saito, Shigehiko Uchino, Yusuke Iizuka, Masamitsu Sanui, Kohei Takimoto, Toshihiko Mayumi, and JSEPTIC DIC Study Investigators in Clinical and Applied Thrombosis/Hemostasis
Supplemental Material, Suppl_figure_2_021519_(1) for The Treatment Intensity of Anticoagulant Therapy for Patients With Sepsis-Induced Disseminated Intravascular Coagulation and Outcomes: A Multicenter Cohort Study by Daisuke Kudo, Mineji Hayakawa, Hiroaki Iijima, Kazuma Yamakawa, Shinjiro Saito, Shigehiko Uchino, Yusuke Iizuka, Masamitsu Sanui, Kohei Takimoto, Toshihiko Mayumi, and JSEPTIC DIC Study Investigators in Clinical and Applied Thrombosis/Hemostasis