Abstract
Introduction
Research for management of benign prostate obstruction (BPO) for adult males remains a cornerstone of urology research. This landscape has witnessed the rise and fall of multiple therapies, both surgical and medical. Our aim was to formally evaluate the publication trends for these interventions over the past 20 years.
Material and methods
A systematic search was performed in a Cochrane style. Data was analysed using the independent t-test and Pearson's correlation coefficient (SPSS version 24). To observe changes in trends more effectively, data was sub-divided into two time periods: 1997 to 2006 and 2007 to 2016.
Results
Over the past 20 years, 4236 papers have been published concerning for BPO (surgical, n = 2177 and medical, n = 2059). For surgical treatments, these included articles on monopolar transurethral resection of prostate (TURP) (n = 340), bipolar TURP (n = 260), HoLEP (n = 293) and Greenlight laser (n = 395). For medical therapies, these included alpha blockers (848), 5-alpha reductase inhibitors (n = 618) and PDE5I (n = 91). Between the two time periods the change was +18.8% (p = 0.108) for monopolar TURP, +497.1% (<0.001) for bipolar TURP, -54.5% (p <0.001 for prostatic stents and -81.9% (p <0.001) for transurethral microwave therapy (TUMT). There was over 290% rise in number of publications related to BPO laser surgery (p <0.001). For medical interventions, the change was +11.5% (p = 0.397) for alpha blockers, -1.9% (p = 0.867), +49.0%( 0.122) for phytotherapy, +2075% (p <0.001) for PDEI and +2375.0% (p <0.001) for combined alpha blocker and anti-muscarinics.
Conclusions
Interventions for BPO have undergone a high volume of research. In particular, minimally invasive laser surgeries and combined medical therapies have seen significant expansion.
Keywords: 5-alpha reductase inhibitor, alpha blockers, benign prostatic hyperplasia, benign prostatic obstruction, lower urinary tract symptoms, minimally invasive surgery, systematic review
INTRODUCTION
A multitude of longitudinal community and epidemiologic studies have confirmed the consensus that benign prostate hyperplasia (BPH) holds a status of ubiquity [1, 2]. Indeed, the natural history of this disease process renders one third of men over 60 years old liable to develop moderate to severe lower urinary tract symptoms (LUTS) as a result of benign prostatic obstruction (BPO) [3]. The rationale and demand to develop effective therapeutic strategies is therefore irrefutable. To this end, the field of urology has witnessed a high volume of valuable research and productivity into BPO related medical and surgical innovations, which has been published and disseminated worldwide. This 'industrial revolution' for BPO treatments has pioneered new solutions in both pharmacotherapy and surgery. Novel medical remedies have included the introduction of phosphodiesterase inhibitors (PDEIs) and phytotherapy [4, 5]. Meanwhile, surgery has fully embraced the minimally invasive approach, which has included the inauguration of laser treatments as well as non-ablative strategies such as Urolift [6]. The advancements of robotic surgery have also supplemented the range of treatments patients can be offered [7]. While this inexorable rise has continued, formal evaluation of such bibliographic trends has remained under-reported. It was our objective to complete such a task and thereby gain greater insight into the temporal changes in research and practice patterns in BPO treatments over the past 20 years.
MATERIAL AND METHODS
Evidence acquisition and criteria for including studies for this review:
Inclusion criteria
Articles published in any language
Primary and secondary research articles
Exclusion criteria
Studies with no published abstract
Case reports
Review articles
Animal studies
Laboratory studies
Search strategy and study selection
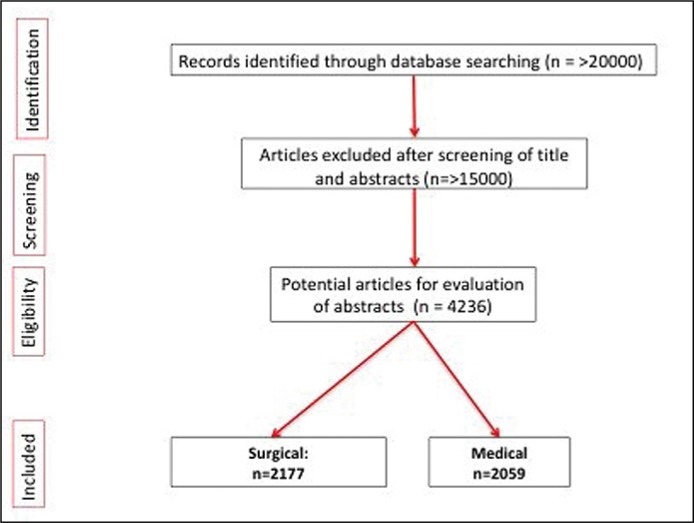
A sensitive search protocol was developed by the author team and then implemented by two of the authors independently. This was performed in accordance with Cochrane methodology and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist [8]. The devised strategy was then applied to the online bibliographic database PubMed to identify all original studies on BPO treatment published between January 1st 1996 to December 31st 2016. Key words used for searching included (not limited to: “lower urinary tract symptoms”, “benign prostate hyperplasia”, “bladder outflow obstruction”, “pharmacotherapy” and “minimally invasive surgery”. Screening and identification of eligible studies also followed a dual approach (Figure 1).
Figure 1.
Search flowchart.
Data extraction and analysis
Data was extracted by two authors (RG and AP) and any discrepancies or disagreements were resolved by the senior author (BKS). Information was collected from the abstracts. Outcome data from individual studies was not gathered. Analysis was performed using the independent t-test and Pearson's correlation coefficient (SPSS version 24). To observe and analyse changes more effectively, data was sub-divided into two, 10-year time periods, 1997 to 2006 and 2007 to 2016.
RESULTS
Overall number of papers on BPO treatments
Over the past two decades, 4236 original articles have been published on treatments for BPO (surgical, n = 2177 and medical, n = 2059). For medical therapies, these included alpha blockers (n = 848), 5-alpha reductase inhibitors (5-ARIs) (n = 618), phosphodiesterase 5 inhibitors (PDE5-I, n = 91), phytotherapy (n = 127), combined alpha blockers/ 5-alpha reductase inhibitors (n = 218), combined alpha blockers/PDE5-Is (n= 28) and combined alpha blocker/anti-muscarinics (n = 103). For surgical treatments, these included articles on monopolar transurethral resection of prostate (TURP, n = 340), bipolar TURP (n = 260), transurethral incision of prostate (TUIP, n = 47), simple prostatectomy (n = 104), transurethral microwave therapy (TUMT, n = 268), transurethral needle ablation (TUNA, n = 60), prostate stents (n = 64), Holmium laser enucleation of prostate (HoLEP, n = 293) and Greenlight laser (n = 395).
Although there was a significant increase for both medical and surgical papers respectively when comparing the period of 1997 to 2006 (n = 1619) to 2007 to 2016 (n = 2528) (p <0.001, 95% CI: 31.5 to 59.4), there was no difference between the numbers of medical and surgical papers published (p = 0.69, 95% CI: -24.6 to 16.5).
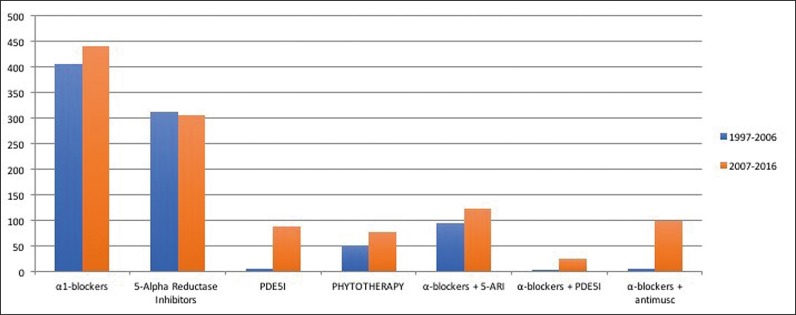
Medical therapies
Comparing the volume of papers published between these two time periods, there were non-significant increases of +11.5% (p = 0.397) for alpha blockers, +49.0% (p = 0.122) for phytotherapy, and +29.5% (p = 0.089) for combined alpha blockers/5-ARIs (Table 1, Figure 2). While there were significant increases in studies published in the following: +2075% (p <0.001) for PDE5-Is, +733.3% (p = 0.003) for combined alpha blockers/PDE5-Is, +2375.0% (p <0.001) for combined alpha blockers/anti-muscarinics. For studies on 5-ARIs, there was a non-significant drop by -1.9% (p = 0.867).
Table 1.
Mean dilation areas and mean dilation diameters for each device in pig and cadaver kidneys
| α-blockers | 5-alpha reductase inhibitors | PDE5-i | Phytotherapy | α-blockers + 5-ARI | α-blockers + PDE5I | α-blockers + antimuscarinics | |
|---|---|---|---|---|---|---|---|
| 1997–2006 | 407 | 312 | 4 | 51 | 95 | 3 | 4 |
| 2007–2016 | 441 | 306 | 87 | 76 | 123 | 25 | 99 |
| % change | +11.5% | -1.9% | +2075.0% | +49.0% | +29.5% | +733.3% | +2375.0% |
| p value | 0.397 | 0.867 | <0.001 | 0.122 | 0.089 | 0.003 | <0.001 |
PDE5-i – phosphodiesterase 5 inhibitors
Figure 2.
Trends of medical treatments over time.
PDE5-i – phosphodiesterase 5 inhibitors
These increases were reflected in trend analyses with Pearson's correlation done for each group.
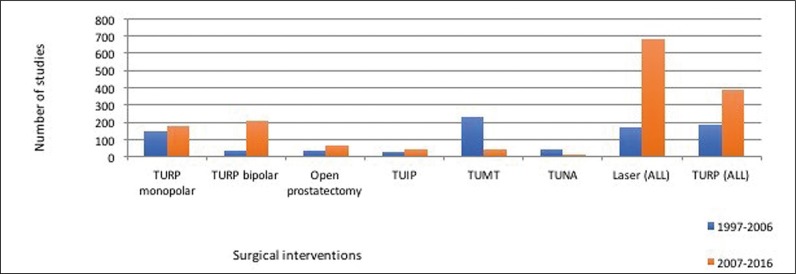
Surgical therapies
Between the two time periods there was a rise of +18.8% (p = 0.108) for monopolar TURP, +497.1% (p <0.001) for bipolar TURP and +73.7% (p = 0.117) for open simple prostatectomy. Overall, there was over 290% rise in number of publications related to BPO laser surgery (p <0.001) and this included +245.9% (p <0.001) for HoLEP, +702.4% (p <0.001) for Greenlight, +2266.6% (p = 0.002) for Thulium and +750.0% (<0.001) for Diode laser (Tables 2 and 3, Figure 3). Although from 1997 to 2006, the largest number of laser publications was on HoLEP (n = 61), between 2007 to 2016, Greenlight became the laser receiving the most new articles (n = 337). However, there was a significant drop of -54.5% (p <0.001) for prostatic stents, -81.9% (p <0.001) for TUMT, -63.6% (0.004) for TUNA and -80.3% (p = 0.002) for Nd:YAG laser. Urolift emerged in the latter decade as a new surgical option (n = 31).
Table 2.
Changes in surgical treatments over time
| TURP monopolar | TURP bipolar | Open prostatectomy | TUIP | TUMT | TUNA | Laser (ALL) | TURP (ALL) | Urolift | Stent | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1997–2006 | 149 | 35 | 38 | 25 | 227 | 44 | 173 | 184 | 0 | 44 |
| 2007–2016 | 177 | 209 | 66 | 41 | 41 | 16 | 682 | 386 | 31 | 20 |
| % change | +18.8% | +497.1% | +73.7% | +64.0% | -81.9% | -63.6% | 294.2% | +109.8% | / | -54.5% |
| P value | 0.108 | <0.001 | 0.117 | 0.610 | 0.001 | 0.004 | <0.001 | <0.001 | <0.001 | <0.001 |
TURP – transurethral resection of prostate; TUIP – transurethral incision of prostate; TUMT – transurethral microwave therapy; TUNA – transuretheral needle ablation
Table 3.
Trends in laser treatments
| HoLEP | Diode | Nd:YAG | Thulium | Greenlight | |
|---|---|---|---|---|---|
| 1997–2006 | 61 | 6 | 61 | 3 | 42 |
| 2007–2016 | 211 | 51 | 12 | 71 | 337 |
| % change | +245.9% | +750.0% | -80.3% | +2266.6% | +702.4% |
| P value | <0.001 | <0.001 | 0.002 | 0.002 | <0.001 |
HoLEP – holmium laser enucleation therapy; Nd:YAG – Neodymium:YAG.
Figure 3.
Trends of benign prostatic hyperplasia surgical interventions over time.
TURP – transurethral resection of prostate; TUIP – transurethral incision of prostate; TUMT – transurethral microwave therapy; TUNA – transuretheral needle ablation
DISCUSSION
Key findings
Both medical and surgical treatments for BPO have been the subject of large volumes of research over the past 2 decades. There has been a significant increase in the volume of publications in the past decade compared to the previous in both medical and surgical treatments.
Advances in surgical and medical treatments
While TURP has remained the gold standard for over 30 years and its efficacy for small to medium sized prostate burdens is well established, the search for new techniques has remained ongoing [9]. Since HoLEP was first described in 1996, it has become an active an area of research along with the other new laser technologies [10]. Its success is largely related to the enucleation technique, which allows large prostates to be treated [11]. Alongside HoLEP, Greenlight laser technology has gained notable attention. Ow et al. recently reported an increase in year on year of Greenlight laser use in a tertiary centre [12]. This was largely owing to its suitability in high risk anti-coagulated patients. There is also now growing evidence to support its use in larger prostates [13]. Stents, TUMT and TUNA have far less research interest in recent years and this would likely reflect its diminishing use in clinical practice. Recent study by Gill et al. recorded patients undergoing tissue eliminating procedures to record higher levels of discontinuing alpha blockers and 5-ARIs than those patients undergoing tissue necrosing procedures such as microwave (TUMT) and radio frequency ablation (TUNA) [14].
While HoLEP has become an established intervention for large prostate burdens (>80cc), it is interesting to see our results support the ongoing place of open simple prostatectomy as a surgical option [15, 16]. This ongoing attention may be related to its continued application particularly in poorer healthcare communities [17].
Despite a high volume of drug research, a recent meta-analysis concluded there to have been very limited advances in pharmacotherapy for LUTS secondary to BPO [18]. The authors analysed data from 48 studies and found none of the newer medications or combination therapies yielded superior outcomes compared to alpha blockers alone.
Strengths, limitations and future directions
This review provides formal confirmation of trends observed by the urology community worldwide. To our knowledge, this is the first such evaluation of its kind. In order to truly demonstrate worldwide trends and reduce bias, our review included non-English publications also. Our search application was limited to PubMed only and therefore non-indexed articles will exist, which this review does not capture. An exhaustive review of such material was considered beyond the scope of this article. Nonetheless, the authors feel confident that bibliographic patterns are accurately captured by use of PubMed alone [19]. This review also primarily covers surgical intervention but does not cover radiological interventions such as prostate artery embolization (PAE) [20]. The Rezum system and iTind are both other novel interventions, which have emerged in recent years, however their formal roles in current practice are yet to be determined beyond the research setting [21].
Supplementary Table 1.
Summary of trends analysis
| Independent T-Test (1997–2006 vs. 2007–2016) | Pearson’s Correlation | |||
|---|---|---|---|---|
| Therapy | p | 95% CI | p | Correlation Coefficient |
| Medical | ||||
| α-blockers | 0.397 | -4.84 to 11.64 | 0.42 | 0.191 |
| 5-ARI | 0.867 | -7.06 to 8.26 | 0.65 | -0.109 |
| PDE5-i | <0.001 | 4.81 to 11.79 | <0.001 | 0.806 |
| Phytotherapy | 0.122 | -0.75 to -5.75 | 0.044 | 0.454 |
| α-blockers + 5-ARI | 0.089 | -1.56 to 6.07 | 0.023 | 0.505 |
| α-blockers + PDE5i | 0.003 | 0.98 to 3.43 | <0.001 | 0.707 |
| α-blockers + antimuscarinics | <0.001 | 5.70 to 13.30 | <0.001 | 0.827 |
| Surgical | ||||
| TURP monopolar | 0.108 | -0.68 to 6.28 | 0.055 | 0.436 |
| TURP bipolar | <0.001 | 11.35 to 23.45 | <0.001 | 0.956 |
| Open prostatectomy | 0.117 | -0.81 to 6.41 | 0.203 | 0.297 |
| TUIP | 0.610 | -0.92 to 1.52 | 0.334 | -0.228 |
| TUMT | 0.001 | 9.67 to 27.53 | <0.001 | -0.815 |
| TUNA | 0.004 | 0.99 to 4.61 | <0.001 | -0.761 |
| Laser (all) | <0.001 | 36.66 to 65.14 | <0.001 | 0.947 |
| TURP (all) | <0.001 | 12.73 to 27.67 | <0.001 | 0.937 |
| MIPS | <0.001 | 2.89 to 3.31 | ||
| Urolift | <0.001 | 1.05 to 3.10 | ||
| Stent | <0.001 | 1.20 to 2.40 | ||
| Laser treatments | ||||
| HoLEP | <0.001 | 8.32 to 21.68 | <0.001 | 0.877 |
| Diode | <0.001 | 3.18 to 5.82 | <0.001 | 0.798 |
| Nd:YAG | 0.002 | 2.04 to 7.76 | <0.001 | 0.865 |
| Thulium | 0.002 | 3.28 to 10.33 | <0.001 | 0.877 |
| Greenlight | <0.001 | 21.58 to 37.42 | <0.001 | 0.945 |
5-ARI – 5-alphareductase inhibitors; PDE5-i – phosphodiesterase 5 inhibitors; TURP – transurethral resection of prostate; TUIP – transurethral incision of prostate; TUMT – transurethral microwave therapy; TUNA – transuretheral needle ablation; HoLEP – Holmium laser enucleation therapy; Nd:YAG – Neodymium:YAG.
While robot technology has made a profound impact on uro-oncological surgery, its application has also extended to benign prostate disease. Its role as an alternative to open simple prostatectomy has received increased attention as has its use in aquablation [22, 23]. In the field of new medical treatments, new intra-prostatic injections are currently being studied in the trial setting [24, 25]. These include intraprostatic onabotulinum toxin A and Fexapotide triflutate (NX-1207) [26, 27].
CONCLUSIONS
Medical and surgical treatments for BPO have undergone a high volume of research over the past 20 years. In particular, minimally invasive laser surgeries such as Greenlight have seen significant expansion as well as combined medical therapies such as blockers and anti-muscarinics. While others such as TUMT and TUNA have stopped attracting research interest. There are now of plethora of management options available but these should be tailored to the individual needs of the presenting patient.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Chute CG, Panser LA, Girman CJ, et al. The prevalence of prostatism: a population-based survey of urinary symptoms. J Urol. 1993;150:85–89. doi: 10.1016/s0022-5347(17)35405-8. [DOI] [PubMed] [Google Scholar]
- 2.Soler R, Gomes CM, Averbeck MA, et al. The prevalence of lower urinary tract symptoms (LUTS) in Brazil: Results from the epidemiology of LUTS (Brazil LUTS) study. Neurourol Urodyn. 2018;37:1356–1364. doi: 10.1002/nau.23446. [DOI] [PubMed] [Google Scholar]
- 3.McVary KT. BPH: epidemiology and comorbidities. Am J Manag Care. 2016;15(5 Suppl):122–128. [PubMed] [Google Scholar]
- 4.Wilt TJ, Ishani A, Rutks I, et al. Phytotherapy for benign prostatic hyperplasia. Public Health Nutr. 2000;3:459–472. doi: 10.1017/s1368980000000549. [DOI] [PubMed] [Google Scholar]
- 5.Mavuduru RS, Pattanaik S, Panda A, et al. Phosphodiesterase inhibitors for lower urinary tract symptoms consistent with benign prostatic hyperplasia. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones P, Rajkumar GN, Rai BP, et al. Medium-term outcomes of Urolift (minimum 12 months follow-up): evidence from a systematic review. Urology. 2016;97:20–24. doi: 10.1016/j.urology.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 7.Wedmid A, Llukani E, Lee DI. Future perspectives in robotic surgery. BJU Int. 2011;108:1028–1036. doi: 10.1111/j.1464-410X.2011.10458.x. [DOI] [PubMed] [Google Scholar]
- 8.Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–784. doi: 10.7326/M14-2385. [DOI] [PubMed] [Google Scholar]
- 9.Mayer EK, Kroeze SG, Chopra S, et al. Examining the 'gold standard': a comparative critical analysis of three consecutive decades of monopolar transurethral resection of the prostate (TURP) outcomes. BJU Int. 2012;110:1595–1601. doi: 10.1111/j.1464-410X.2012.11119.x. [DOI] [PubMed] [Google Scholar]
- 10.Gilling PJ, Cass CB, Cresswell MD, et al. Holmium laser resection of the prostate: preliminary results of a new method for the treatment of benign prostatic hyperplasia. Urology. 1996;47:48–51. doi: 10.1016/s0090-4295(99)80381-1. [DOI] [PubMed] [Google Scholar]
- 11.Krambeck AE. Evolution and success of holmium laser enucleation of the prostate. Indian J Urol. 2010;26:404–409. doi: 10.4103/0970-1591.70582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ow D, Papa N, Perera M, et al. Trends in the surgical treatment of benign prostatic hyperplasia in a tertiary hospital. ANZ J Surg. 2018;88:95–99. doi: 10.1111/ans.13904. [DOI] [PubMed] [Google Scholar]
- 13.Stone BV, Chughtai B, Kaplan SA, et al. GreenLight laser for prostates over 100 ml: what is the evidence? Curr Opin Urol. 2016;26:28–34. doi: 10.1097/MOU.0000000000000237. [DOI] [PubMed] [Google Scholar]
- 14.Gill B, Sabharwal N, Ulchaker J, Fareed K, Shoskes D. Comparative effectiveness of benign prostate enlargement interventions at facilitating urologic medication discontinuation. J Urol. 2018;199:e994. doi: 10.1016/j.urology.2019.07.039. [DOI] [PubMed] [Google Scholar]
- 15.Gratzke C, Bachmann A, Descazeaud A, et al. EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2015;67:1099–1109. doi: 10.1016/j.eururo.2014.12.038. [DOI] [PubMed] [Google Scholar]
- 16.Oelke M, Bachmann A, Descazeaud A, et al. EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2013;64:118–140. doi: 10.1016/j.eururo.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 17.Tubaro A, de Nunzio C. The current role of open surgery in BPH. EAU-EBU Update Series. 2006;4:191–201. [Google Scholar]
- 18.Dahm P, Brasure M, MacDonald R, et al. Comparative effectiveness of newer medications for lower urinary tract symptoms attributed to benign prostatic hyperplasia: a systematic review and meta-analysis. Eur Urol. 2017;71:570–581. doi: 10.1016/j.eururo.2016.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pietropaolo A, Proietti S, Geraghty R, et al. Trends of 'urolithiasis: interventions, simulation, and laser technology' over the last 16 years (2000-2015) as published in the literature (PubMed): a systematic review from European section of Uro-technology (ESUT) World J Urol. 2017;35:1651–1658. doi: 10.1007/s00345-017-2055-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jones P, Rai BP, Nair R, Somani BK. Current status of prostate artery embolization for lower urinary tract symptoms: review of world literature. Urology. 2015;86:676–681. doi: 10.1016/j.urology.2015.05.011. [DOI] [PubMed] [Google Scholar]
- 21.Winebrake JP, Thomas D, Te A, Chughtai B. Future Surgical Procedures: iTind, Rezūm, and Aquablation. A Comprehensive Guide to the Prostate. 2018:197–204. [Google Scholar]
- 22.Pokorny M, Novara G, Geurts N, et al. Robot-assisted simple prostatectomy for treatment of lower urinary tract symptoms secondary to benign prostatic enlargement: surgical technique and outcomes in a high-volume robotic centre. Eur Urol. 2015;68:451–457. doi: 10.1016/j.eururo.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 23.Gilling P, Anderson P, Tan A. Aquablation of the prostate for symptomatic benign prostatic hyperplasia: 1-year results. J Urol. 2017;197:1565–1572. doi: 10.1016/j.juro.2017.01.056. [DOI] [PubMed] [Google Scholar]
- 24.Peyronnet B, Brucker BM, Michel MC. Lower Urinary Tract Symptoms: What's New in Medical Treatment? Eur Urol Focus. 2018;4:17–24. doi: 10.1016/j.euf.2018.04.005. [DOI] [PubMed] [Google Scholar]
- 25.Andersson KE. Intraprostatic injections for lower urinary tract symptoms treatment. Curr Opin Urol. 2015;25:12–18. doi: 10.1097/MOU.0000000000000122. [DOI] [PubMed] [Google Scholar]
- 26.Shore N, Cowan B. The potential for NX-1207 in benign prostatic hyperplasia: an update for clinicians. Ther Adv Chronic Dis. 2011;2:377–383. doi: 10.1177/2040622311423128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mch Vary KT, Roehrborn CG, Chartier-Kastler E, et al. A multicenter, randomized, double-blind, placebo controlled study of onabotulinumtoxinA 200 U to treat lower urinary tract symptoms in men with benign prostatic hyperplasia. J Urol. 2014;192:150–156. doi: 10.1016/j.juro.2014.02.004. [DOI] [PubMed] [Google Scholar]