Abstract
U.S. military veterans are a large and racially heterogeneous population. There are reasons to expect that racial disparities in mortality among veterans are smaller than those for non-veterans. For example, blacks are favorably selected into the military, receive relatively equitable treatment within the military, after service accrue higher socioeconomic status and receive health and other benefits after service. Using the 1997–2009 National Health Interview Survey (N=99,063) with Linked Mortality Files through the end of 2011 (13,691 deaths), we fit Cox proportional hazard models to estimate whether racial disparities in the risk of death are smaller for veterans than for non-veterans. We find that black/white disparities in mortality are smaller for veterans than for non-veterans, and that this is explained by the elevated socioeconomic resources of black veterans relative to black non-veterans. Leveraging birth cohort differences in military periods, we document that the smaller disparities are concentrated among All-Volunteer era veterans.
Keywords: Veterans, Mortality, Race, Cohort, Cox Proportional Hazard Models
1. Introduction
Life expectancy in the United States varies significantly by race/ethnicity and especially so between Non-Hispanic black (hereafter black) and Non-Hispanic white (hereafter white) men (Williams and Mohammed 2013). In 2014, life expectancy at birth for black men was 4.5 fewer years than it was for white men (National Center of Health Statistics 2016). Racial disparities in mortality not only indicate a deeply unequal society but are also expensive: these disparities cost the U.S. economy around one trillion dollars between 2003 and 2006 alone (LaVeist, Gaskin, and Richard 2011).
Racial inequality in health and mortality extends to military veterans. Black veterans report worse health and experience higher levels of premature death than do white veterans (Egede, Dismuke, and Echols 2012; Jha et al. 2001; Landes, Wilder and Williams 2017; McGinnis et al. 2003; Oddone et al. 2002; Sheehan et al. 2015; Teachman 2011; Young, Maynard, and Boyko 2003). Yet, there is comparably little research on whether the magnitude of racial inequality in health and risk of mortality differs between veteran and non-veteran males. This comparison is important because the military has been shown to equalize risks and resources among blacks and whites, thereby reducing inequality in other important domains relative to the non-veteran population (Moskos and Butler 1997).
Indeed, several studies have compared differences in marriage, income, and self-reported health, all important precursors to mortality risk, by race and military/veteran status (Lundquist 2004; Teachman and Call 1996; Teachman and Tedrow 2007). These studies find that black veterans have higher levels of marriage, and income than their peers who never served in the military. While difficult to completely separate the role of military service from issues related to selection into the military, these results suggest that black males’ military service history could provide resources that their non-veteran peers do not have. This leads us to anticipate that the racial gap in mortality will be smaller among veterans than among non-veterans. Previous research has compared racial disparities in self-reported measures of health between veterans and non-veterans at midlife among specific cohorts and found little racial difference in reported health after accounting for selection into the military (Rackin 2017; Teachman 2011). These analyses had discerning research designs and strong internal validity but were limited to single birth cohorts and self-reported measures of health. Other recent research has documented mortality differences among adult men by race and veteran status but has not examined potential reasons for race differences in relation to military service (Landes, Wilder and Williams 2017).
We draw on data for men in the National Health Interview Survey’s Linked Mortality File (hereafter NHIS-LMF). While these data do not allow us to directly identify the casual impact of military service on racial disparities in mortality, they do allow us to document the extent of black/white inequality in mortality for a large segment of the adult male population. They also allow us to document inequality among multiple birth cohorts while simultaneously examining the influence of important covariates on any observed inequality. Specifically, we use Cox proportional hazard models (Singer and Willett 2003) to test if the observed differences for the adult male population can be explained by demographic, behavioral health, health insurance, and socioeconomic controls. We then document black/white and veteran/non-veteran differences in risk of mortality stratified by birth cohort while also progressively controlling for groups of important covariates to test potential explanations for the observed mortality advantage of veterans and how this advantage varies by cohort and between black and white men.
Documenting black/white inequality in mortality among veterans and non-veterans is important. Military veterans are a large and increasingly heterogeneous population. In 2014, there were over 19 million veterans (United States Census Bureau 2014), roughly the same population as the state of Florida. A large and growing proportion of military veterans are racial and ethnic minorities. In 2010, racial and ethnic minorities comprised 21% of veterans; by 2040, they will comprise 34% of veterans (Department of Veterans Affairs 2013). The substantial size of the overall veteran population and the growth in the proportion of minority veterans warrants more attention regarding the unique health and well-being of these individuals, including how their health compares to other veterans and civilian non-veterans. Our research builds on previous research comparing racial inequality among veterans to non-veterans (Rackin 2017; Teachman 2011; Landes, Wilder, and Williams 2017), by analyzing all adult males rather than a single birth cohort, by predicting mortality rather than self-reported measures of health at midlife and by explicitly testing pathways that may explain the observed mortality advantage of black veterans compared to non-veterans for the entire adult population and by birth cohort.
2.1. Background
Serving in the military is a transformative institutional experience (Elder 1998), often considered a “turning point” or “bridging environment” (Browning, Lopreato, and Poston Jr 1973; Sampson and Laub 1996) that can significantly alter the life course and subsequent health of those who serve (MacLean and Elder Jr 2007). Previous research has shown that blacks who serve are positively selected in that they have certain personal advantages over those who do not (Rackin 2017; Teachman, Call, and Segal 1993). Those who serve are exposed to an institutional climate that has strived to minimize racism for longer than almost any other major institution (Moskos and Butler 1997). Blacks who serve also have higher rates of marriage (Lundquist 2004) and socioeconomic attainment (Teachman and Call 1996). If eligible, they can also receive lifetime health benefits. Thus, selection into the military, characteristics of military life, and experiences after military life may all help reduce racial disparities in mortality among veterans. Below we review reasons for this, and discuss the importance of documenting mortality differences by birth cohort.
2.2. Selection into the Military
At the turn of the 21st century, blacks in high school had some of the highest levels of interest in military service (Bachman et al. 2000; Segal et al. 1999), a possible result of military recruitment targeting minority-majority schools (Furumoto 2005). Indeed, in the All-Volunteer era of the late twentieth century, black men have comprised a disproportionate number of service members (Kleykamp 2007). The large group of black men who served in the armed forces had better education and physical health than those who did not serve, characteristics which undoubtedly positively influence later-life health (MacLean and Elder Jr 2007; Teachman et al. 1993). The process of favorable selection into the military by some black men has long been identified as “creaming,” in which positively selected black men serve in the military partially due to labor market constraints and discrimination in other occupations (Mare and Winship 1984). Whites do not have a similar process of “creaming” for the military. For example, blacks who served in the military had higher high-school grades than blacks who did not, but whites who served in the military had lower grades than their peers who did not serve (Teachman et al. 1993). More generally, whites may see the military as a “fallback plan” when other occupational opportunities or markets are constrained (Rackin 2017). That is, whites who serve in the military are negatively selected whereas blacks who serve are positively selected.
Even passing the physical entrance exam and completing the rigors of boot camp and military service requires good health. For example, the pre-induction physical exam rejection rate for military service was roughly 70% in 1950 (Lopoo, Wing, and Wolf 2011). This suggests that at one time all who enter the military, regardless of race, have relatively comparable health, with the least healthy excluded from military service (Teachman 2011). The comparable health at baseline in the military, positive selection of blacks, and negative selection of whites all suggest smaller differences in risk of death between blacks and whites among those who have served in the military than among those who have not.
Previous research has shown that selection is relevant for differences among veteran and non-veteran in health (Rackin 2017; Teachman 2011) In fact, Rackin (2017) found no differences by race or veteran status in self-reported physical or mental health among middle-aged adults after using propensity-score matching to account for important measurable aspects of selection into the military. Teachman (2011) also found little evidence of the influence of military service on self-reported health differences by race among mid-life veterans after using a quasi-natural experimental design that partially accounted for selection. Overall, however, the favorable selection of blacks into the military, and results of previous research, lead us to anticipate less black/white inequality in mortality among veterans than non-veterans.
2.3. Characteristics of Military Life
Characteristics of military life also may lead to smaller racial differences in mortality among veterans than among non-veterans. Executive Order 9981, which outlawed racial discrimination within the military, preceded the Civil Rights Act by almost 20 years. As a result of this order, the military became one of the first major social institutions to desegregate. To be sure, progress towards positive race relations has been slow and incomplete in the military (for an overview see: Burk and Espinoza 2012). Yet good race relations are imperative for the military and important to being an effective fighting force. Indeed, military sociologists have stressed the importance of good race relations within the military in its service to a society which emphasizes diversity and equal opportunity (Burk 2007; Burk and Espinoza 2012).
Other institutional characteristics of military life beyond its commitment to racial equality may also minimize black/white mortality inequality. The military is a deeply structured organization wherein individual characteristics such as race are subjugated to a strict hierarchy and broader organizational goals (Burk and Espinoza 2012; Goffman 1968; Lundquist 2008; Moskos and Butler 1997). For example, one of the first activities in basic training is to cut the hair of the recruit, removing an important aspect of individuality in favor of conformity. The military is also often portrayed as an example of a meritocracy (Lundquist 2008), that is, an organization in which advancement is based on ability and results, rather than on factors such as nepotism or race. Such institutional characteristics could be why blacks in the military report greater occupational satisfaction than whites do (Lundquist 2008). Military service has still other mechanisms to equalize health among its members. The military mandates physical fitness and self-discipline, and it promotes healthy behaviors and skills, such as exercise, self-esteem, and personal responsibility (Rackin 2017). By regulating some behaviors and emphasizing healthy behaviors, the military offers direct and beneficial social control (Umberson 1987, 1992). These characteristics presumably endure throughout adulthood and positively influence health (LaVerda, Vessey, and Waters 2006; Teachman 2011).
In addition to being disproportionately represented in the military (Kleykamp 2007), blacks generally serve in the military longer than whites, lengthening exposure to an institution with largely better race relations than in the general public (Lutz 2008). Even brief military service may lessen exposure to racial discrimination and its negative health consequences (Lundquist 2008; Moskos and Butler 1997; Williams and Mohammed 2013). Military service also occurs when young black men are disproportionately vulnerable to incarceration (Pettit 2012; Pettit and Western 2004; Sheehan 2018), drug use, mortality, and victimization from crime (Harper et al. 2007). Thus, military service (Faragher, Cass, and Cooper 2005) likely has a positive influence on the health of blacks afterward, especially compared to their peers who did not serve and characteristics of military life indicate that black/white differences in mortality will be smaller among veterans.
2.4. Experiences After Military Life
After military life circumstances, especially the elevated socioeconomic status of black veterans, could also reduce the mortality risk of black veterans compared to their non-veteran peers. Teachman and Tedrow (2007) reported that while highly educated white veterans earned less than their nonveteran peers, the least-educated black veterans earned more than their nonveteran black peers. Similarly, Angrist (1995), using social security data, showed an income disadvantage for white Vietnam veterans compared to non-veterans, while Kleykamp (2013) descriptively showed that employed black veterans received an earnings premium relative to non-black veterans. The higher earnings of black veterans may be due to occupational selection within the military. Blacks are apt to choose occupations that train skills transferable to the civilian workforce (Burk and Espinoza 2012). These transferable skills are beneficial; experimental data indicate that blacks with administrative military experience were more likely to be called for an interview than blacks with no military experience (Kleykamp 2007). The differences in income relative to non-veteran peers appear to be contingent on pre-service education, historical context, and time since leaving the military (Phillips et al. 1992; Teachman and Call 1996). Still, the enhanced socioeconomic profile of black veterans is likely critical for minimizing racial disparities in mortality, given that previous research has estimated that roughly 80% of the black/white life expectancy gap results from socioeconomic inequality (Geruso 2012). The countervailing associations between post-military socioeconomic status and military service among blacks and whites also points to a smaller black/white gap in mortality among veterans. Given the negative association between income and mortality (Phelan et al. 2004), we expect that the smaller racial gap in income among veterans relative to non-veterans will likewise reduce black/white inequality among veterans compared to non-veterans.
The health benefits of military service may extend beyond socioeconomic status for black male veterans. Black servicemen are more likely to be married than their peers who are not in the military (Lundquist 2004; Teachman 2007). Marriage is beneficial for later-life health, especially for men (Umberson et al. 2006). Hence, the greater likelihood of marriage for black veterans could improve their subsequent health relative to their non-veteran peers. Health behaviors also affect the health of veterans (Bedard and Deschênes 2006). Recent evidence suggests that veterans generally practice worse health behaviors than non-veterans, including higher levels of smoking and drinking (Hoerster et al. 2012). However, findings regarding racial differences in health behaviors among veterans are mixed. Research on Veteran Administration (hereafter VA) patients finds higher rates of smoking and heavy drinking among blacks than whites (Conigliaro et al. 2000; Mickelson, Blum, and Geraci 1997), while other studies have reported black veterans have lower levels of smoking and drinking than white veterans do (Richards et al. 1990; Sheehan et al. 2015).
Black/white differences in access to medical care and health insurance among the general population are well documented (Blendon et al. 1989; Fiscella et al. 2002; Weinick, Zuvekas, and Cohen 2000; Williams and Collins 1995). Access to insurance and care are important for health (Franks, Clancy, and Gold 1993; Wilper et al. 2009), and the lower access that blacks have to these helps to partially explain racial disparities in health and life expectancy (Williams and Jackson 2005). Veterans, however, may receive comprehensive health insurance and care through the VA. While the VA is not without racial biases or problems (Burk and Espinoza 2012), the care it offers could reduce racial disparities in health among veterans. Altogether, the favorable selection of black men into the military, characteristics of military life, and experiences after military service may all help reduce black/white differences in mortality among veterans, particularly by reducing the mortality risk of black veterans.
2.5. Importance of Documenting Cohort Differences
While cohorts have long been considered instrumental for social change (Ryder 1965), recent research has shown cohorts to have distinct profiles of aging (Riley 1987) and mortality (Masters, Hummer, and Powers 2012; Yang 2008). Significant cohort differences in aging and mortality risk have led scholars to argue that cohorts have distinct morbidity and mortality phenotypes (Crimmins and Finch 2006; Hayward and Sheehan 2016). Similarly, the influence of military service on subsequent life outcomes has varied substantially by birth cohort (Elder 1998). This is not surprising given that age of entry, method of entry (e.g. draft versus volunteering), physical requirements to serve, duration of service, exposure to combat or toxins such as Agent Orange, and benefits provided by the military have all varied over time (Lopoo et al. 2011; MacLean and Elder Jr 2007).
For example, military service was generally beneficial for socioeconomic outcomes among World War II veterans, who largely served immediately after high school and were provided generous benefits after service (Elder 1998). In contrast, Vietnam veterans generally experienced worse socioeconomic outcomes than their peers who did not serve. Scholars attribute the disadvantage of Vietnam veterans to disruption of higher education, less generous benefits, and stigma from service (Edwards 2010). There are also likely differences within the military regarding combat which vary by birth cohort and race and may ultimately influence health. In Vietnam (Dohrenwend et al. 2008) and Operation Iraqi Freedom (Rundell 2006) black servicemen faced disproportionate levels of post-traumatic stress disorder.
The distinct cohort health and mortality profiles and differential impact of military service on subsequent life outcomes by cohort (Elder 1998; MacLean and Elder Jr 2007) make it crucial to document black/white and veteran disparities in mortality by birth cohort. Indeed, recent research has descriptively documented significant race/ethnic differences in returns to military service by cohort and found that blacks in non-war cohorts generally benefited more from military service than whites (Landes, Wilder, and Williams 2017). We build on this research in a few important ways, first we document the difference for the whole adult population, and second, we explicitly test potential pathways through which blacks may have benefited more from military service and how these pathways may have varied by cohort. Examining these pathways is critical as socioeconomic and other factors related to military service varied considerably by cohort and evaluating which of these factors are important is thus important to better understanding why blacks in some cohorts were advantaged in terms of their mortality (Phillips et al. 1992; Teachman and Call 1996). While our data source limits our ability to analyze how specific military experiences to which non-veterans were not exposed affects racial differences in mortality, we can document racial disparities between veterans and non-veterans by birth cohort. Thus, in this analysis we assess differences in mortality by race, veteran status, and birth cohort.
3. Materials and Methods
3.1. Data
We used thirteen years (1997–2009) of the publicly available Integrated Health Interview Series version of the National Health Interview Survey (Minnesota Population Center and State Health Access Data Assistance Center 2016) with mortality follow-up through the end of 2011. The NHIS is a large nationally representative annual survey of non-institutionalized American households with detailed information about health and socioeconomic status. Its household response rate varied by year from 91.8% in 1997 to 82.2% in 2009, with the response rate for sample adults in these households ranging from 89.0% in 1997 to 80.1% in 2009 (Czajka and Beyler 2016). As a result, the overall response rate for sample adults ranged from 81.7% (91.8%X 89.0%) to 65.8% (82.2% × 80.1%). A 14-point matching algorithm links NHIS respondents to death certificates in the National Death Index (NDI). Results from the publicly released data have been shown to be extremely similar to the restricted data when investigating all-cause mortality (Lochner et al. 2008).
The NHIS had major strengths for this analysis. First, it contained a large nationally representative sample of American non-veteran and veteran males from multiple birth cohorts. Second, it included information regarding respondents’ veteran status. Third, it had many other variables associated with health outcomes such as socioeconomic factors and health behaviors. Fourth, when weights are employed its results were representative of the U.S. non-institutionalized adult population. Most importantly, the NHIS-LMF was linked to the National Death Index, allowing the analysis of risk of death (Lochner et al. 2008).
Our sample included male respondents from the 1997 to 2009 surveys who were 30 to 84 years old at the time of survey, eligible for mortality follow up, reported being non-Hispanic white or black, and were not currently enlisted in the military. We excluded those aged under 30 because they could still be serving in the military and had a low risk of mortality. We excluded those 85 or older because NHIS top-codes age at 85. Notably, our substantive results were similar when including those currently in the military or those younger than 30 or older than 84.
3.2. Measures
We analyzed two racial categories: non-Hispanic whites (coded 0) and non-Hispanic blacks (coded 1). We also estimated models including other racial and ethnic groups (Table A.1). We found no significant differences for other race/ethnic groups, we discuss this finding further in the Discussion. Our measure of veteran status was based on whether respondents were ever honorably discharged. Consistent with past research (Landes, London, and Wilmoth 2018; Landes, Wilder, and Williams 2017; Kramarow & Pastor 2017) we coded those who reported being honorably discharged “1” and “0” if otherwise. The utilization of this measure is further discussed in the Discussion.
We examined several characteristics related to health. Given the importance of region for health and mortality (Fenelon 2013; Sheehan, Montez, and Sasson 2018), the first control we add is that for Census region of residence. Our codes were Northeast (0=reference), (1) Midwest, (2) South, (3) West. We coded four categories smoking history: (0=reference) never smoker, (1) past smoker, (2) current some-day smoker and, (3) current every-day smoker. We coded three categories of body mass, based on clinical classifications: underweight (BMI 0–18.49), normal weight (BMI 18.5–29.99: reference), and obese and greater (BMI 30+). We coded three categories of alcohol consumption: never drinkers (0= reference), (1) former drinkers, and (2) current drinkers of alcohol. While also not a health behavior, we also included a dichotomous variable on health insurance (0=no health insurance, 1=has health insurance). In terms of family characteristics, we coded four categories of marital status: married (0= reference), (1) divorced/separated, (2) widowed, and (3) never married. We also included a continuously coded variable on number of other family members.
To examine how socioeconomic disparities influence racial disparities in mortality, we first included a categorical measure of yearly household income coded as: (0=reference) $0-$34,999, (1) $35,000-$74,999, and (2) $75,000+. We added an educational attainment categorical variable coded as: (0=reference) less than high school, (1) high school, and (2) more than high school. We accounted for home ownership through a dummy variable coded as (1) owns home and does not own home (0=reference). Homeownership is a substantial source of wealth for middle-class Americans and also an important source of inequality in wealth between blacks and whites (Krivo and Kauffman 2004). We also included a dummy variable on current employment, coded as (1) employed and is not employed (0=reference).
To document potential cohort differences, we stratified the sample into four subsamples based on year of birth. These cohorts were defined by important historical and military events. The first cohort was defined as those born before 1927. These men would have been eligible to serve during World War II. Our second was those born between 1928 and 1942, who would have been eligible for post – World War II service, including conflicts in Korea and Vietnam. Our third next cohort was those born between 1944 and 1952, who were eligible for the Vietnam draft lottery. The Vietnam lottery ended in 1973, when only 646 men were drafted, so we made the cut-off 1952 (Selective Services System 2016). Our final cohort was those born after 1952, all of whom were of military age during the All-Volunteer era. The stratification by veteran status and race did not yield enough deaths for analysis by even finer cohorts, especially for the All-Volunteer era. However, in sensitivity analyses described below, we briefly considered the robustness of the results of the cohort classifications.
3.3. Methods
To analyze the extent of differences by race and veteran status in mortality for the adult population and by cohort, we implemented the following protocol. We first calculated weighted descriptive statistics of the sample by race and veteran status. We next estimated a series of progressively adjusted Cox proportional hazard models predicting mortality (Singer and Willett 2003). Cox proportional hazard models have been previously used with NHIS–LMF data to analyze mortality (Masters et al. 2013; Montez and Zajacova 2013) due to their ease of interpretability and because they do not assume a distribution of survival time or of death across age (Denney et al. 2010). More exactly, the baseline hazard is unspecified. This allows the hazard to differ at each age and to be modeled non-parametrically. As a result, no estimated baseline hazards are produced.
The first possible survey interview day was January 1, 1997 while mortality follow-up ended on December 31, 2011, giving a maximum 14 years of observation or follow-up. We specified time as age in quarter-years (Kom, Graubard, and Midthune 1997; Verweij and van Houwelingen 1995), the most precise time specification available in the public data. These decisions yielded 810,150.75 person-years of observation among 99,063 respondents. Because attained age was our specification of time, we excluded age at survey from the models. Nevertheless, including age at survey yielded similar results. We also estimated piecewise exponential models that also produced similar substantive results.
One important assumption of Cox models is that the hazard of mortality is the same or proportional for all respondents. Using the Schonenfeld residual test, we found a violation of the global proportionality assumption. This violation, we discovered, was due to small cell sizes among black veterans who had aged to at least 90 years of age by our mortality cut-off date of December 31, 2011. Similarly, non-proportionality was only apparent in pre-Vietnam draft birth cohorts. After we corrected for non-proportionality, using an interaction term with age, the substantive results for those of the oldest ages were similar for the entire sample (see Table A.2). Given these results and evidence that Cox model estimates from large nationally representative samples are relatively robust to non-proportionality (Therneau and Grambsch 2000) we are confident in our analyses.
For the Cox models, we implemented the following progressive adjustment strategy. We began with a main effects model with race and veteran status. Next, to analyze if black/white differences in mortality were smaller among veterans than non-veterans, we fit Cox proportional hazard models with an interaction term between race and veteran status. We first estimated the interaction model with no controls, then a model only controlling for region of residence, then added health behaviors and health insurance, then added family characteristics, and finally added the socioeconomic variables. This strategy allowed us to test potential pathways (e.g. socioeconomic status) through which post-military characteristics could influence observed black/white and veteran/non-veteran differences in mortality risk. We then stratified the sample by birth cohort and followed an abbreviated progressive adjustment analysis where we first control for region and then add the entire set of controls. Aside from household income, for which just under 15% of respondents had missing values, there was generally little missing data in our sample. We used STATA’s multiple imputation suite to impute all missing data except that for our independent variables of race and veteran status. We also fit models with a flag for missing reports of income and list-wise deletion which provided similar substantive results.
4. Results
4.1. Descriptive Statistics
Table 1 provides the weighted descriptive statistics for the analytical sample by race and veteran status. Black (55.2) and white (60.9) veterans were older on average than their non-veteran counterparts. Consistent with previous research (Hoerster et al. 2012) indicating higher smoking levels of veterans, black (31.3%) and white (47.1%) veterans reported considerably higher rates of former smoking than black (19.6%) or white (27.0%) non-veterans. Not surprising given VA coverage, Black veterans (90.3%) reported considerably higher levels of health insurance coverage than black non-veterans (79.2%). A similar, albeit less strong, pattern was apparent for whites. Among blacks, veterans reported higher levels of income, educational attainment, and homeownership than non-veteran blacks did; among whites, veterans had lower levels for these. These results are consistent with findings from previous research (e.g. Teachman and Call 1996) suggesting a socioeconomic advantage for black veterans and a socioeconomic disadvantage for white veterans, as well as clear differences in the characteristics of veterans and non-veterans.
Table 1:
Descriptive Statistics, Males, aged 30–84. National Health Interview Survey, 1997–2009.
| Non-Hispanic Blacks | Non-Hispanic Whites | Entire Sample | |||
|---|---|---|---|---|---|
| Non Veterans | Veterans | Non Veterans | Veterans | ||
| Age (Average) | 47.3 | 55.2 | 47.5 | 60.9 | 51.5 |
| Region of Residence | |||||
| Northeast (Ref) | 15.9% | 12.1% | 19.9% | 18.6% | 19.0% |
| Northcentral/Midwest | 19.2% | 19.4% | 29.5% | 26.8% | 27.5% |
| South | 57.4% | 57.1% | 33.3% | 36.0% | 36.9% |
| West | 7.5% | 11.5% | 17.3% | 18.6% | 16.6% |
| Smoking | |||||
| Never Smoker (Ref) | 51.6% | 37.7% | 47.4% | 29.9% | 42.5% |
| Past Smoker | 19.6% | 31.3% | 27.0% | 47.1% | 32.2% |
| Current Someday Smoker | 6.7% | 6.4% | 3.9% | 2.7% | 3.9% |
| Current Everyday Smoker | 22.1% | 24.6% | 21.6% | 20.3% | 21.4% |
| Alcohol Consumption | |||||
| Never Drinker (Ref) | 21.0% | 14.0% | 11.0% | 9.4% | 11.5% |
| Former Drinker | 19.9% | 26.4% | 15.7% | 23.4% | 18.6% |
| Current Drinker | 59.1% | 59.5% | 73.4% | 67.2% | 69.9% |
| BMI | |||||
| 0–18.49 | 0.8% | 0.8% | 0.6% | 0.8% | 0.6% |
| 18.50–29.99 (Ref) | 68.9% | 70.8% | 74.2% | 74.0% | 73.5% |
| 30+ | 30.3% | 28.4% | 25.2% | 25.3% | 25.8% |
| Health Insurance Status | |||||
| Has Health Insurance | 79.2% | 90.3% | 87.2% | 93.5% | 88.3% |
| Marital Status | |||||
| Married (Ref) | 41.9% | 42.7% | 59.6% | 63.1% | 58.5% |
| Divorced/Separated | 25.0% | 33.9% | 19.0% | 19.5% | 20.1% |
| Widowed | 4.8% | 8.7% | 3.0% | 9.4% | 5.1% |
| Never Married | 28.3% | 14.7% | 18.4% | 8.0% | 16.2% |
| Family Size (Average) | 2.28 | 2.00 | 2.4 | 2.03 | 2.29 |
| Income | |||||
| $0-$34,999 (ref) | 54.0% | 50.1% | 30.9% | 40.2% | 36.3% |
| $35,000–$74,999 | 31.5% | 34.2% | 37.1% | 36.8% | 36.3% |
| $75,000+ | 14.5% | 15.7% | 32.1% | 23.1% | 27.4% |
| Educational Attainment | |||||
| Less than High School Degree (Ref) | 26.2% | 16.0% | 12.7% | 12.3% | 13.9% |
| High School Degree | 31.7% | 32.3% | 28.0% | 31.9% | 29.6% |
| Greater than High School Degree | 42.0% | 51.6% | 59.3% | 55.8% | 56.5% |
| Home Ownership | |||||
| Owns home | 51.2% | 58.2% | 76.4% | 81.5% | 75.0% |
| Employment Status | |||||
| Employed | 67.8% | 57.0% | 78.3% | 50.3% | 68.8% |
| Birth Cohort | |||||
| Born 1927 and Before | 3.0% | 11.4% | 3.2% | 19.4% | 8.0% |
| Born 1928–1943 | 15.7% | 26.6% | 14.8% | 36.7% | 21.5% |
| Born 1944–1952 | 16.7% | 22.8% | 17.8% | 23.4% | 19.4% |
| Born after 1953 | 64.6% | 39.1% | 64.2% | 20.5% | 51.1% |
| N | 11,159 | 4,031 | 56,146 | 27,727 | 99,063 |
| Deaths | 1,414 | 842 | 6,516 | 4,919 | 13,691 |
Source: National Health Interview Survey, (1997–2009). Linked Mortality File through 2011.
Note: Data are weighted.
4.2. Multivariable Results
Table 2 depicts results of our progressively adjusted Cox models fit to test whether black/white disparities in mortality were smaller among veterans than among non-veterans. The first model shows the main effects of race and veteran status. Blacks had a significantly higher risk of mortality than whites (HR: 1.41, p < 0.001), but the difference between veterans and non-veterans was not statistically significant. The next model included an interaction between race and veteran status. The interaction between veteran status and race was significant and negative (HR: 0.85, p < 0.01), suggesting that the black/white differences in mortality were significantly smaller among veterans than non-veterans. More precisely, the point estimate for black non-veterans (HR 1.51, p < 0.001) was significantly higher than that for black veterans (HR: 1.51*1.03*0.85= 1.31). There was no statistical difference between white veterans and white non-veterans (HR: 1.03, NS). In ancillary analyses focused exclusively on veterans (results not shown here), we found that black veterans have a significantly higher hazard of mortality than white veterans (HR: 1.21, p < .001).
Table 2:
Hazard Ratios from Cox Proportional Hazard Model Predicting Death, Males aged 30–84. National Health Interview Survey,1997–2009.
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |
|---|---|---|---|---|---|---|
| Race/Ethnicity | ||||||
| White (Ref) | ||||||
| Black | 1.41*** | 1.51*** | 1.46*** | 1.31*** | 1.22*** | 1.05 |
| Veteran Status | ||||||
| Nonveteran (ref) | ||||||
| Veteran | 1.00 | 1.03 | 1.03 | 1.00 | 1.01 | 1.02 |
| Race/Ethnicity × Veteran Status | ||||||
| Black × Veteran | 0.85*** | 0.85** | 0.88** | 0.88** | 0.93 | |
| Region of Residence | ||||||
| Northeast (Ref) | ||||||
| Northcentral/Midwest | 1.05 | 1.01 | 1.02 | 1.04 | ||
| South | 1.15*** | 1.09** | 1.12*** | 1.14*** | ||
| West | 0.99 | 0.99 | 0.99 | 1.02 | ||
| Smoking | ||||||
| Never Smoker (Ref) | ||||||
| Past Smoker | 1.39*** | 1.41*** | 1.33*** | |||
| Current Someday Smoker | 2.10*** | 2.01*** | 1.78*** | |||
| Current Everyday Smoker | 2.79*** | 2.69*** | 2.33*** | |||
| Alcohol Consumption | ||||||
| Never Drinker (Ref) | ||||||
| Former Drinker | 1.17*** | 1.15*** | 1.16*** | |||
| Current Drinker | 0.82*** | 0.82*** | 0.91** | |||
| BMI | ||||||
| 0–18.49 | 2.31*** | 2.24*** | 2.06*** | |||
| 18.50–29.99 (Ref) | ||||||
| 30+ | 1.15*** | 1.16*** | 1.12*** | |||
| Health Insurance Status | ||||||
| Has Health Insurance | 0.83*** | 0.90** | 1.01 | |||
| Family Characteristics | ||||||
| Number of Family Members | 0.97* | 1.00 | ||||
| Marital Status | ||||||
| Married (Ref) | ||||||
| Divorced/Separated | 1.37*** | 1.23*** | ||||
| Widowed | 1.22*** | 1.13*** | ||||
| Never Married | 1.58*** | 1.36*** | ||||
| Income | ||||||
| $0-$34,999 (ref) | ||||||
| $35,000–$74,999 | 0.85*** | |||||
| $75,000+ | 0.72*** | |||||
| Educational Attainment | ||||||
| Less than High School Degree (Ref) | ||||||
| High School Degree | 0.94** | |||||
| Greater than High School Degree | 0.86*** | |||||
| Home Ownership | ||||||
| Owns Home | 0.81*** | |||||
| Employment Status | ||||||
| Currently Employed | 0.56*** | |||||
| N | 99,063 | |||||
| Person Years | 810,151 | |||||
| Deaths | 13,691 |
p <0.05
p <0.01
p < 0.001
Source: National Health Interview Survey, (1997–2009). Linked Mortality File through 2011.
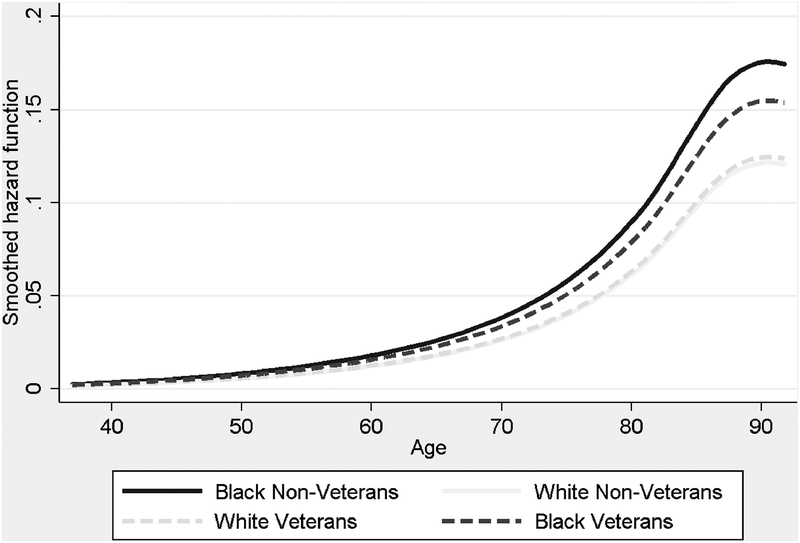
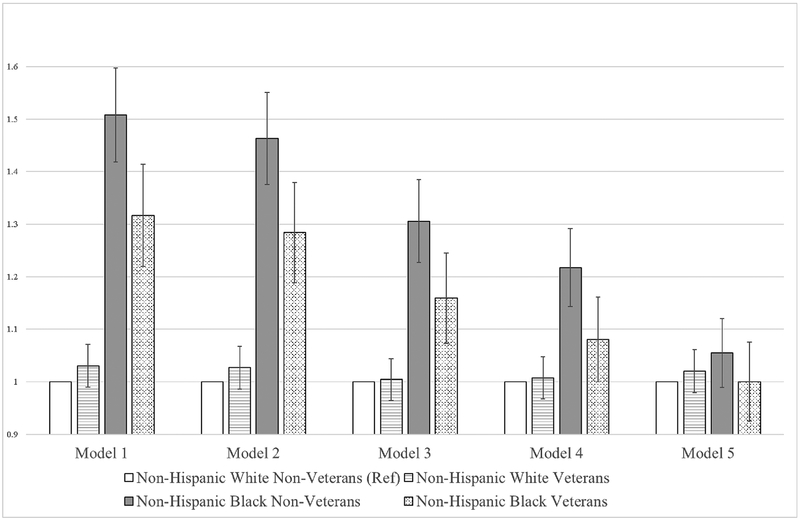
Model 3 added controls for region of residence. The interaction term remained significant and negative (HR 0.85, p < 0.01). The results of Model 3 are also presented in Figure 1, which depicts the risk of death by age, race, and veteran status adjusted only for region of residence. White veterans had virtually the same mortality risk by age as white non-veterans did. Black veterans had a substantially higher mortality risk than white veteran and non-veterans, but a significantly lower hazard than black non-veterans. Notably, the racial difference in mortality risk was significantly larger among non-veterans than veterans. Model 4 added controls for smoking, drinking, self-reported body mass index, and health insurance. The interaction term between race and veteran status remained significant (HR: 0.88, p < 0.01) in this model, suggesting that racial differences in mortality risk remained smaller among military veterans and that black veterans had a lower mortality risk than their non-veteran peers. Model 5 included controls for marital status and number of family members. Once again, in this model, the interaction term between race and veteran status remained statistically significant (HR: 0.88, p <0.01), while non-veteran blacks had a significantly higher risk of mortality (HR: 1.22, p <0.001). The specific hazard ratios by race and veteran status were also calculated and are presented in Figure 2.
Figure 1.
Hazard of All-Cause Mortality, Differences by Race and Veteran Status.
Figure 2. Hazard Ratios from Cox Proportional Hazard Models Predicting Mortality among American Males Aged 30–84. National Health Interview Survey, 1997–2009.
Notes: Model 1: Unadjusted. Model 2 additionally includes regions, Model 3 additionally includes health behaviors, Model 4 additionally includes family characteristics, and Model 5 includes socioeconomic characteristics.
Model 6 added controls for household income, educational attainment, home ownership, and current employment status. These added socioeconomic controls explained both racial differences in risk of mortality as well as the interaction term. We fit additional models (results not shown here) to explore which specific control explained the interaction. None of the socioeconomic status variables individually explained the interaction; it was only when they all were collectively added to the model that the interaction became insignificant. This stresses the importance of overall social class rather than one specific measure (e.g. income) in explaining the interaction. Overall, these results suggest that the lower mortality risk of black veterans relative to black non-veterans is attributable to the elevated socioeconomic status of black veterans. The results also suggest that the higher mortality risk for black non-veterans relative to non-veteran whites was also attributable to disadvantaged socioeconomic status.
We next documented results from cohort-stratified Cox models that employed an abbreviated progressive adjustment strategy. Table 3 depicts these results. There were no significant differences by race or veteran status in risk of mortality for the cohort born before 1928 (World War II and before cohort). For the second cohort, men born 1928 to 1943 (Post-World War II-Vietnam cohort), there were significant racial differences, with non-veteran black males having significantly higher hazard of mortality (HR: 1.45, p >.001) in Model 1—a difference explained by controls for behavioral health and socioeconomic status. For the third cohort born 1944 to 1952 (Vietnam draft eligible cohort), non-veteran blacks again had significantly higher hazard of mortality (HR: 1.77, p > .001), with these differences also explained by controls for behavioral health and socioeconomic status. Notably, there were no significant racial differences in the risk of death that varied by veteran status among this cohort. In the fourth cohort, those born after 1953 (All-Volunteer cohort), there were significant differences by veteran status. While black non-veterans had significantly higher risk of death (HR: 1.71, p > .001) than others, the interaction term suggests that black male veterans had a lower risk than their non-veteran counter-parts (HR: 0.63, p>.01). We found, however, that differences in the interaction term were explained by differences in income and education, suggesting that the elevated socioeconomic attainment of black veterans in the All-Volunteer cohort lowered their risk of mortality relative to their peers who did not serve.
Table 3:
Hazard Ratios from Cox Proportional Hazard Model Predicting Death, Males aged 30–84, Stratified by Birth Cohort National Health Interview Survey, 1997–2009.
| World War II and Before | Post-World War II-Vietnam | Vietnam Draft eligible | All-Volunteer-Cohort | |||||
|---|---|---|---|---|---|---|---|---|
| (Born 1913–1927) | (Born 1928–1943) | (Born 1944–1952) | (Born after 1953 and After) | |||||
| Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | |
| Race/Ethnicity | ||||||||
| White (Ref) | ||||||||
| Black | 1.06 | 0.85* | 1.45*** | 0.99 | 1.77*** | 1.09 | 1.71*** | 1.19* |
| Veteran Status | ||||||||
| Nonveteran (ref) | ||||||||
| Veteran | 0.99 | 1.03 | 1.00 | 0.98 | 1.01 | 0.96 | 1.18* | 1.02 |
| Race/Ethnicity × Veteran Status | ||||||||
| Black × Veteran | 1.06 | 1.10 | 0.92 | 1.03 | 0.88 | 1.01 | 0.63** | 0.79 |
| N | 8,598 | 22,100 | 19,730 | 48,635 | ||||
| Person Years | 61,283 | 177,486 | 167,623 | 403,759 | ||||
| Deaths (Black Deaths) | 5,234 (572) | 5,130 (905) | 1,799 (412) | 1,528 (367) | ||||
p <0.05
p <0.01
p < 0.001
Source: National Health Interview Survey, (1997–2009). Linked Mortality File through 2011.
Notes: Model 1 includes no controls.
Model 2 includes controls for Region of Residence, Smoking, Alcohol Consumption, BMI, Health Insurance, Family size, Marital Status, Household Income, Education, Home Ownership, Employment Status.
5. Discussion
Veterans are a large diverse population with unique health challenges (Bedard and Deschênes 2006; London and Wilmoth 2006). This study compared the extent of black/white inequality in risk of mortality among veterans and non-veterans. While previous research has examined racial health disparities among veterans and non-veterans (Haas, Krueger, and Rohlfsen 2012; Hummer et al. 2013; Rackin 2017; Sheehan et al. 2015), little has compared the magnitude of disparities between veterans and non-veterans among all adult males. This comparison is important given the well-documented favorable life-prospects of black veterans resulting from selection processes into the military, experiences within the military, and benefits after military service. Previous research has used shrewd designs to compare the extent of racial inequality in health among veterans (Teachman 2011; Rackin 2017) but has relied on self-reported measures of health at midlife and focused on single cohorts.
We found that black/white inequality in risk of death was smaller among veterans than among non-veterans, due to the significantly lower mortality risk of black veterans compared to their non-veteran counterparts. While past research has found a larger veteran advantage by blacks in non-war cohorts (Landes, Wilder, and Williams 2017), we show that when the cohorts are combined there does seem to be an overall benefit of military service for black veterans relative to their non-veteran counterparts for the adult male population. Additionally, there were no significant differences in the risk of mortality between white veterans and non-veterans, despite the socioeconomic disadvantage of white veterans relative to white non-veterans.
These results do not suggest that veterans are immune from racial health inequality. In fact, consistent with previous research on self-reported health and disability (Sheehan et al. 2015), we found systematically higher risk of death among black veterans than white veterans. This finding underscores the severity of racial inequality in health in the United States. Black veterans are a favorably selected population in terms of their health and other characteristics, who have elevated socioeconomic status and are given benefits after military service. Yet, black veterans still have a significantly higher risk of mortality than white veterans.
Notably, we find that statistical controls for socioeconomic status explained the mortality advantage of black veterans compared to their non-veteran peers. This suggests that the higher socioeconomic status that black veterans gain reduces their risk of mortality relative to black non-veterans. This comports with previous research (Geruso 2012) that has stressed the critical importance of socioeconomic inequality for racial inequality in life expectancy as well as other research which stresses the importance of socioeconomic status for inequality in longevity (Hayward and Sheehan 2016). Extensive previous research has documented the socioeconomic benefits of military service for blacks (Teachman and Tedrow 2007; Kleykamp 2013), we find that these socioeconomic benefits in turn increase the longevity of black veterans relative to their non-veteran peers. Racial differences in socioeconomic attainment reflect structural inequality and systematic racism (Phelan and Link 2015). These results suggest that minimizing racial inequality in socioeconomic resources could help reduce racial inequality in mortality.
When we stratified the sample by birth cohort, we found the advantage of black veterans was concentrated in the All-Volunteer cohort (or those born after 1952). This is consistent with previous research that showed that in non-war cohorts black male veterans enjoyed a mortality advantage over their non-veteran peers (Landes, Wilder, and Williams 2017). It is unclear whether the non-significant findings in other eras are due to constrained ability to self-select into the military, experiences (such as higher levels of combat) within the military, or still other factors such as small cell sizes. Further documenting cohort differences in post-military outcomes, especially for blacks and those who are currently serving, is ripe for future research. Consistent with the entire adult population, when we included controls for socioeconomic status the interaction term was no longer significant for blacks in the All-Volunteer era. This suggests that the socioeconomic advantages garnered by black veterans in the All-Volunteer era benefited their longevity, at least compared to their peers who never served. While our data are unable to explicitly test if the advantaged socioeconomic status among black veterans in the All-Volunteer era was due to selection into the military, experiences within the military, or yet other characteristics, previous research on racial disparities in health among veterans in the All-Volunteer era has stressed the importance of selection for minimizing racial inequality in self-reported health of veterans (Rackin 2017). Overall, our findings contribute to previous research which has discussed cohort differentials in mortality (Yang 2008) and the implications of military service (MacLean and Elder 2007; Landes, Wilder, and Williams 2017) by documenting how – and why black/white inequality in mortality among veterans varied by cohort.
To fully analyze the role of selection relative to the causal influence of military service, researchers would need either rich lifelong data or a random assigned experiment. Still, going forward researchers could adopt a causal-modeling approach such as using the draft as an instrument or other quasi-experiments (such as Teachman 2011) to analyze if there is a causal impact of military service on mortality risks for black men relative to their peers. Of course, this work will likely lack the external validity to multiple birth cohorts that analyses such as this one can provide.
Unfortunately, we were unable to examine detailed information regarding military service (duration, rank, branch, combat exposure, occupation, etc.), given the NHIS just had one question regarding veteran status. Critical for the context of our research, by definition non-veterans are not exposed to these military conditions which would have not allowed the comparison of the differences between veterans and non-veterans—the key research objective. Nevertheless, recent research suggests that controlling for detailed conditions faced within the military (e.g. duration of service, exposure to combat, and more) did little to explain racial differences in self-reported health and disability among veterans (Sheehan et al. 2015). Still the long-term implications of military factors on subsequent mortality and black white differences in mortality is an important area of future research. Additionally, we used only one measure of veteran status, a question on whether respondents were honorably discharged. Although more than 90% of those who serve are honorably discharged (Minnesota Population Center and State Health Access Data Assistance Center 2012), using this measure limits the external validity of our findings to those who were honorably discharged. We urge future researchers using datasets with more detailed questions regarding military history to examine how including those with other-than-honorable discharges influences conclusions about racial disparities in health.
There are other important limitations. While we were able to track respondents’ mortality information longitudinally, we only had their other information for one point in time. This sufficed to help us explain the mortality advantage of black veterans, however, we still lacked an exhaustive set of time-varying controls for post-military life. Future research should examine the extent to which other characteristics of post-military life such as the lower rates of residential segregation among black veterans (Fischer, Lundquist, and Vachon 2016), may influence black/white disparities in the health of veterans.
6. Conclusion
Overall this research has important policy and scientific implications. Its policy implication is straightforward: black veterans still face a higher risk of death than white counterparts. This suggests that the military and the Veterans Administration should continue to strive to eliminate racial health disparities. Additionally, our work stresses the importance of socioeconomic inequality in racial inequality in health. Policies aimed at minimizing social inequality could reduce health inequality. We also found no difference in the influence of military service on the mortality risk of Hispanics or non-Hispanic other males (Table A.1). As the proportion of Hispanics who serve in the military continues to climb (Department of Veteran Affairs 2013), this issue should be revisited. Additionally, why white, Hispanic, and non-Hispanic other male veterans are comparable to their non-veteran peers in terms of mortality risk while black male veterans are advantaged compared to non-veteran blacks, is an important question for future research.
Its scientific implications are more diverse. This research builds on previous work stressing the importance of large social institutions such as the military in reducing racial disparities in critical social outcomes. These results also suggest that future research which does not include controls for veteran status may underestimate black/white disparities in mortality. Our results are only generalizable to male veterans; as female enrollment in the military continues to increase, future research should include female veterans as well. Future research should consider how to best differentiate the impacts of selection, military service, and post-military life, while acknowledging that the military is a transformative life experience. Researchers should also explicitly examine how racial inequality in health and mortality unfolds among those who most recently served along with those who are currently serving in the military and how their lived experiences, health, and mortality compares to previous cohorts. While racial disparities in health remain among veterans, analyses of veteran populations can also help in reducing such disparities for others.
Acknowledgements:
We thank the University of Texas Population Research Center (Grant R24 HD42849) for administrative and computing support; the NICHD Ruth L. Kirschstein National Research Service Award (T32 HD007081–35) for training support; the National Institute of Aging training grant (T32 AG000037), the University of Minnesota for preparing and making the data available to the public, and the members of the Population Health lab and Anonymous Reviewers for their helpful suggestions. The contents of this manuscript are solely the responsibility of the authors and do not represent the official views of the NIA, NICHD, the University of Texas at Austin, the University of Southern California or Arizona State University.
APPENDICIES
Table A.1:
HAZARD RATIOS FROM COX PROPORTIONAL HAZARD MODEL PREDICTING DEATH, MALES AGE 30–84, 1997–2009.
| Model 1 | Model 2 | |
|---|---|---|
| Race/Ethnicity | ||
| White (Ref) | ||
| Black | 1.46*** | 1.13*** |
| Hispanic | 0.90** | 0.79*** |
| Other Race | 0.80** | 0.82** |
| Veteran Status | ||
| Nonveteran (ref) | ||
| Veteran | 1.04 | 1.05* |
| Race/Ethnicity × Veteran Status | ||
| Black × Veteran | 0.86** | 0.90* |
| Hispanic × Veteran | 0.92 | 0.93 |
| Other Race × Veteran | 1.22 | 1.06 |
| Age (Continuous) | 1.01 | 1.00 |
| Region of Residence | ||
| Northeast (Ref) | ||
| Northcentral/Midwest | 1.03 | 1.00 |
| South | 1.14*** | 1.10*** |
| West | 0.98 | 1.01 |
| Smoking | ||
| Never Smoker (Ref) | ||
| Past Smoker | 1.34*** | |
| Current Someday Smoker | 1.85*** | |
| Current Every Day Smoker | 2.36*** | |
| Alcohol Consumption | ||
| Never Drinker (Ref) | ||
| Former Drinker | 1.16*** | |
| Current Drinker | 0.89*** | |
| BMI | ||
| 0–18.49 | 2.10*** | |
| 18.50–29.99 (Ref) | ||
| 30+ | 1.15*** | |
| Health Insurance Status | ||
| Has Health Insurance | 1.02 | |
| Income | ||
| $0-$34,999 | ||
| $35,000–$74,999 | 0.75*** | |
| $75,000+ | 0.62*** | |
| Educational Attainment | ||
| Less than High School Degree (Ref) | ||
| High School Degree | 0.90*** | |
| Greater than High School Degree | 0.83*** | |
| Marital Status | ||
| Married (Ref) | ||
| Divorced/Separated | 1.29*** | |
| Widowed | 1.16*** | |
| Never Married | 1.46*** | |
| N | 122,722 |
p <0.05
p <0.01
p < 0.001
Source: National Health Interview Survey, (1997–2009). Linked Mortality File through 2011.
Table A.2:
Hazard Ratios from Cox Proportional Hazard Model Predicting Death, Males age 30–84, 1997–2009.
| Model 1 | Model 2 | |
|---|---|---|
| Race/Ethnicity | ||
| White (Ref) | ||
| Black | 1.48*** | 1.14*** |
| Veteran Status | ||
| Nonveteran (ref) | ||
| Veteran | 1.02 | 1.03 |
| Race/Ethnicity × Veteran Status | ||
| Black × Veteran | 0.86** | 0.91* |
| Interaction with Time | ||
| Black × Time over 90 | 0.42** | 0.37*** |
| Veteran Status × Time over 90 | 1.06 | 1.08 |
| Black × Veteran × Time over 90 | 1.43 | 1.55 |
| N | 99,063 | |
p <0.05
p <0.01
p < 0.001
Source: National Health Interview Survey, (1997–2009). Linked Mortality File through 2011.
Notes: Model 1 Controls for Age and Current Region. Model 2 includes all controls.
N = 99,063
Contributor Information
Connor Sheehan, T. Denny Sanford School of Social and Family Dynamics Arizona State University.
Mark D. Hayward, Department of Sociology and Population Research Center University of Texas at Austin
References:
- Angrist Joshua D. 1995. Estimating the Labor Market Impact of Voluntary Military Service Using Social Security Data on Military Applicants. National Bureau of Economic Research. [Google Scholar]
- Bachman Jerald G., Segal David R., Peter Freedman-Doan, and O’Malley Patrick M.. 2000. “Who Chooses Military Service? Correlates of Propensity and Enlistment in the US Armed Forces.” Military Psychology 12(1):1. [Google Scholar]
- Bedard Kelly and Olivier Deschênes. 2006. “The Long-Term Impact of Military Service on Health: Evidence from World War II and Korean War Veterans.” The American Economic Review 176–194. [DOI] [PubMed] [Google Scholar]
- Blendon Robert J., Aiken Linda H., Freeman Howard E., and Corey Christopher R.. 1989. “Access to Medical Care for Black and White Americans: A Matter of Continuing Concern.” JAMA 261(2),278–281. [PubMed] [Google Scholar]
- Browning Harley L., Lopreato Sally C., and Poston Dudley L. Jr. 1973. “Income and Veteran Status: Variations among Mexican Americans, Blacks and Anglos.” American Sociological Review 74–85. [Google Scholar]
- Burk James. 2007. “The Changing Moral Contract for Military Service” The Long War: A New History of US National Security Policy since World War II (New York: Columbia University Press, 2007). [Google Scholar]
- Burk James and Espinoza Evelyn. 2012. “Race Relations within the US Military.” Annual Review of Sociology 38, 401–422. [Google Scholar]
- Conigliaro Joseph et al. 2000. “Understanding Racial Variation in the Use of Coronary Revascularization Procedures: The Role of Clinical Factors.” Archives of Internal Medicine 160(9), 1329–1335. [DOI] [PubMed] [Google Scholar]
- Crimmins Eileen M. and Finch Caleb E.. 2006. “Infection, Inflammation, Height, and Longevity.” Proceedings of the National Academy of Sciences of the United States of America 103(2), 498–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czajka John L., and Beyler Amy. 2016. Declining Response Rates in Federal Surveys: Trends and Implications. Mathematica Policy Research. [Google Scholar]
- Denney Justin T., Rogers Richard G., Hummer Robert A., and Pampel Fred C.. 2010. “Education Inequality in Mortality: The Age and Gender Specific Mediating Effects of Cigarette Smoking.” Social Science Research 39(4), 662–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Veterans Affairs. 2013. “Minority Veterans: 2011.” Prepared by the National Center for Veteran Analysis and Statistics; <http://www.va.gov/VETDATA/docs/SpecialReports/Minority_Veterans_2011.pdf> (Retrieved 12/13/16). [Google Scholar]
- Dohrenwend Bruce P., Turner J. Blake, Turse Nicholas A., Lewis-Fernandez Roberto, and Yager Thomas J.. 2008. “War-Related Posttraumatic Stress Disorder in Black, Hispanic, and Majority White Vietnam Veterans: The Roles of Exposure and Vulnerability.” Journal of Traumatic Stress 21(2), 133–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards Ryan D. 2010. Health, Income, and the Timing of Education among Military Retirees. National Bureau of Economic Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egede Leonard E., Dismuke Clara, and Echols Carrae. 2012. “Racial/Ethnic Disparities in Mortality Risk among US Veterans with Traumatic Brain Injury.” American Journal of Public Health 102(S2), S266–S271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder Glen H. 1998. “The Life Course as Developmental Theory.” Child Development 69(1), 1–12. [PubMed] [Google Scholar]
- Faragher E.Brian, Monica Cass, and Cooper Cary L.. 2005. “The Relationship between Job Satisfaction and Health: A Meta-Analysis.” Occupational and Environmental Medicine 62(2), 105–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenelon Andrew. 2013. Geographic divergence in mortality in the United States. Population and Development Review, 39(4), 611–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiscella Kevin, Franks Peter, Doescher Mark P., and Saver Barry G.. 2002. “Disparities in Health Care by Race, Ethnicity, and Language among the Insured: Findings from a National Sample.” Medical Care 40(1), 52–59. [DOI] [PubMed] [Google Scholar]
- Fischer Mary J., Lundquist Jennifer Hickes, and Vachon Todd E.. 2016. “Residential Segregation: The Mitigating Effects of Past Military Experience.” Social Science Research (60), 61–73. [DOI] [PubMed] [Google Scholar]
- Franks Peter, Clancy Carolyn M., and Gold Marthe R.. 1993. “Health Insurance and Mortality: Evidence from a National Cohort.” JAMA 270(6), 737–741. [PubMed] [Google Scholar]
- Furumoto Rosa. 2005. No poor child left unrecruited: How NCLB codifies and perpetuates urban school militarism. Equity & Excellence in Education, 38(3), 200–210. [Google Scholar]
- Goffman Erving. 1968. “Asylums: Essays on the Social Situation of Mental Patients and Other Inmates.” Aldine Transaction. [Google Scholar]
- Geruso Michael. 2012. “Black-white disparities in life expectancy: how much can the standard SES variables explain?.” Demography,49(2), 553–574. [DOI] [PubMed] [Google Scholar]
- Haas Steven A., Krueger Patrick M., and Rohlfsen Leah. 2012. “Race/Ethnic and Nativity Disparities in Later Life Physical Performance: The Role of Health and Socioeconomic Status over the Life Course.” The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 67(2), 238–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper Sam, Lynch John, Burris Scott, and Smith George Davey. 2007. “Trends in the Black-White Life Expectancy Gap in the United States, 1983–2003.” JAMA 297(11), 1224–1232. [DOI] [PubMed] [Google Scholar]
- Hayward Mark D. and Sheehan Connor M.. 2016. “Does the Body Forget? Adult Health, Life Course Dynamics, and Social Change.” Pp. 355–368 in Handbook of the Life Course. Springer. [Google Scholar]
- Hoerster Katherine D. et al. 2012. “Health and Health Behavior Differences: US Military, Veteran, and Civilian Men.” American Journal of Preventive Medicine 43(5), 483–489. [DOI] [PubMed] [Google Scholar]
- Hummer Robert A., Melvin Jennifer E., Sheehan C, and Wang Y. 2013. “Race/Ethnicity, Mortality, and Longevity” Handbook of Minority Aging. New York, NY: Springer Publishers; 131–151. [Google Scholar]
- Jha Ashish K., Shlipak Michael G., Hosmer Wylie, Frances Craig D., and Browner Warren S.. 2001. “Racial Differences in Mortality among Men Hospitalized in the Veterans Affairs Health Care System.” JAMA 285(3), 297–303. [DOI] [PubMed] [Google Scholar]
- Krivo LJ, & Kaufman RL (2004). Housing and wealth inequality: Racial-ethnic differences in home equity in the United States. Demography, 41(3), 585–605. [DOI] [PubMed] [Google Scholar]
- Kleykamp Meredith A. 2007. “Military Service as a Labor Market Outcome.” Race, Gender & Class 65–76. [Google Scholar]
- Kleykamp Meredith. 2013. Unemployment, earnings and enrollment among post 9/11 veterans. Social Science Research, 42(3), 836–851. [DOI] [PubMed] [Google Scholar]
- Kramarow EA, & Pastor PN (2012). The health of male veterans and nonveterans aged 25–64, United States, 2007–2010. [PubMed]
- Kom Edward L., Graubard Barry I., and Midthune Douglas. 1997. “Time-to-Event Analysis of Longitudinal Follow-up of a Survey: Choice of the Time-Scale.” American Journal of Epidemiology 145(1), 72–80. [DOI] [PubMed] [Google Scholar]
- Landes SD, London AS, & Wilmoth JM (2018). Mortality Among Veterans and Non-veterans: Does Type of Health Care Coverage Matter?. Population Research and Policy Review, 37(4), 517–537. [Google Scholar]
- Landes SD, Wilder J, & Williams D (2017). The effect of race and birth cohort on the veteran mortality differential. Social Science & Medicine, 179, 36–44. [DOI] [PubMed] [Google Scholar]
- LaVeist Thomas A., Gaskin Darrell, and Richard Patrick. 2011. “Estimating the Economic Burden of Racial Health Inequalities in the United States.” International Journal of Health Services 41(2), 231–238. [DOI] [PubMed] [Google Scholar]
- LaVerda Nancy, Vessey Andrea, and Waters William F.. 2006. “Use of the Veterans History Project to Assess World War II Veterans’ Perceptions of Military Experiences and Health.” Military Medicine 171(11), 1076–1082. [DOI] [PubMed] [Google Scholar]
- Lochner Kimberly, Hummer Robert A., Bartee Stephanie, Wheatcroft Gloria, and Cox Christine. 2008. “The Public-Use National Health Interview Survey Linked Mortality Files: Methods of Reidentification Risk Avoidance and Comparative Analysis.” American Journal of Epidemiology 168(3), 336–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- London Andrew S. and Wilmoth Janet M.. 2006. “Military Service and (Dis) Continuity in the Life Course Evidence on Disadvantage and Mortality from the Health and Retirement Study and the Study of Assets and Health Dynamics Among the Oldest-Old.” Research on Aging 28(1), 135–159. [Google Scholar]
- Lopoo L, Wing C, and Wolf D. 2011. “Methodological Problems in Determining the Consequences of Military Service” Unpublished Manuscript. Life Course Perspectives on Military Service. New York: Routledge. [Google Scholar]
- Lundquist Jennifer Hickes. 2004. “When Race Makes No Difference: Marriage and the Military.” Social Forces 83(2), 731–757. [Google Scholar]
- Lundquist Jennifer Hickes. 2008. “Ethnic and Gender Satisfaction in the Military: The Effect of a Meritocratic Institution.” American Sociological Review 73(3), 477–496. [Google Scholar]
- Lutz Amy. 2008. “Who Joins the Military? A Look at Race, Class, and Immigration Status.” Journal of Political and Military Sociology 36(2), 167. [Google Scholar]
- MacLean Alair and Elder Glen H. Jr. 2007. “Military Service in the Life Course.” Sociology 33(1), 175. [Google Scholar]
- Mare Robert D. and Winship Christopher. 1984. “The Paradox of Lessening Racial Inequality and Joblessness among Black Youth: Enrollment, Enlistment, and Employment, 1964–1981.” American Sociological Review 39–55. [Google Scholar]
- Masters Ryan K. et al. 2013. “The Impact of Obesity on US Mortality Levels: The Importance of Age and Cohort Factors in Population Estimates.” American Journal of Public Health 103(10), 1895–1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masters Ryan K., Hummer Robert A., and Powers Daniel A.. 2012. “Educational Differences in US Adult Mortality a Cohort Perspective.” American Sociological Review 77(4), 548–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinnis Kathleen A. et al. 2003. “Understanding Racial Disparities in HIV Using Data from the Veterans Aging Cohort 3-Site Study and VA Administrative Data.” American Journal of Public Health 93(10), 1728–1733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mickelson Judith K., Blum Cynthia M., and Geraci Jane M.. 1997. “Acute Myocardial Infarction: Clinical Characteristics, Management and Outcome in a Metropolitan Veterans Affairs Medical Center Teaching Hospital.” Journal of the American College of Cardiology 29(5), 915–925. [DOI] [PubMed] [Google Scholar]
- Minnesota Population Center and State Health Access Data Assistance Center, Integrated Health Interview Series: Version 6.21 Minneapolis: University of Minnesota, 2016. [Google Scholar]
- Montez Jennifer Karas and Zajacova Anna. 2013. “Trends in Mortality Risk by Education Level and Cause of Death among US White Women from 1986 to 2006.” American Journal of Public Health 103(3), 473–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskos Charles C. and John Sibley Butler. 1997. All That We Can Be: Black Leadership and Racial Integration the Army Way. Basic Books. [Google Scholar]
- National Center of Health Statistics. 2016. “Health, United States, 2015: With Special Feature on Racial and Ethnic Health Disparities.” [PubMed] [Google Scholar]
- Oddone Eugene Z., Petersen Laura A., Weinberger Morris, Freedman Jay, and Kressin Nancy R.. 2002. “Contribution of the Veterans Health Administration in Understanding Racial Disparities in Access and Utilization of Health Care: A Spirit of Inquiry.” Medical Care 40(1), I–3. [DOI] [PubMed] [Google Scholar]
- Pettit Becky. 2012. Invisible Men: Mass Incarceration and the Myth of Black Progress: Mass Incarceration and the Myth of Black Progress. Russell Sage Foundation. [Google Scholar]
- Pettit Becky and Western Bruce. 2004. “Mass Imprisonment and the Life Course: Race and Class Inequality in US Incarceration.” American Sociological Review 69(2):151–169. [Google Scholar]
- Phelan Jo C., Link Bruce G., Ana Diez-Roux Ichiro Kawachi, and Levin Bruce. 2004. “‘Fundamental Causes’ of Social Inequalities in Mortality: A Test of the Theory.” Journal of Health and Social Behavior 45(3), 265–285. [DOI] [PubMed] [Google Scholar]
- Phelan Jo C., & Link Bruce. G. (2015). “Is racism a fundamental cause of inequalities in health?” Annual Review of Sociology, 41(1), 311–330. [Google Scholar]
- Phillips Robert L., Andrisani Paul J., Daymont Thomas N., and Gilroy Curtis L.. 1992. “The Economic Returns to Military Service: Race-Ethnic Differences.” Social Science Quarterly 340–359. [Google Scholar]
- Rackin Heather M. 2017. “Comparing Veteran and Non-Veteran Racial Disparities in Mid-Life Health and Well-Being.” Population Research and Policy Review 36(3), 331–356. [Google Scholar]
- Richards Margaret S., Goldberg Jack, Anderson Robert J., and Rodin MB. 1990. “Alcohol Consumption and Problem Drinking in Vietnam Era Veterans and Nonveterans.” Journal of Studies on Alcohol 51(5), 396–402. [DOI] [PubMed] [Google Scholar]
- Riley Matilda White. 1987. “On the Significance of Age in Sociology.” American Sociological Review 1–14. [Google Scholar]
- Rundell James R. 2006. “Demographics of and Diagnoses in Operation Enduring Freedom and Operation Iraqi Freedom Personnel Who Were Psychiatrically Evacuated from the Theater of Operations.” General Hospital Psychiatry 28(4), 352–356. [DOI] [PubMed] [Google Scholar]
- Ryder Norman B. 1965. “The Cohort as a Concept in the Study of Social Change.” American Sociological Review 843–861. [PubMed] [Google Scholar]
- Sampson Robert J. and Laub John H.. 1996. “Socioeconomic Achievement in the Life Course of Disadvantaged Men: Military Service as a Turning Point, circa 1940–1965.” American Sociological Review 347–367. [Google Scholar]
- Segal David R., Bachman Jerald G., Peter Freedman-Doan, and O’Malley Patrick M.. 1999. “Propensity to Serve in the US Military: Temporal Trends and Subgroup Differences.” Armed Forces & Society 25(3), 407–427. [Google Scholar]
- Selective Services System. 2016. “Induction Statistics” < https://www.sss.gov/About/History-And-Records/Induction-Statistics> (Retrieved 12/13/16).
- Sheehan Connor M. “Education and Health Conditions Among the Currently Incarcerated and the Non-incarcerated Populations.” Population Research and Policy Review (2018): 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan Connor M., Hummer Robert A., Moore Brenda L., Huyser Kimberly R., and Butler John Sibley. “Duty, honor, country, disparity: race/ethnic differences in health and disability among male veterans.” Population research and policy review 34, no. 6 (2015): 785–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan Connor, Montez Jennifer Karas, and Isaac Sasson. “Does the functional form of the association between education and mortality differ by US region?.” Biodemography and social biology 64, no. 1 (2018): 63–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer Judith D. and Willett John B.. 2003. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. Oxford university press. [Google Scholar]
- Teachman Jay D., 2007. “Race, Military Service, and Marital Timing: Evidence from the NLSY-79.” Demography 44(2), 389–404. [DOI] [PubMed] [Google Scholar]
- Teachman Jay D. 2011. “Are Veterans Healthier? Military Service and Health at Age 40 in the All-Volunteer Era.” Social Science Research 40(1), 326–335. [Google Scholar]
- Teachman Jay D., and Vaughn RA Call. 1996. “The Effect of Military Service on Educational, Occupational, and Income Attainment.” Social Science Research 25(1), 1–31. [Google Scholar]
- Teachman Jay D., Vaughn RA Call, and Segal Mady W.. 1993. “The Selectivity of Military Enlistment.” Journal of Political and Military Sociology 21(2), 287–309. [Google Scholar]
- Teachman Jay D., and Tedrow Lucky. 2007. “Joining up: Did Military Service in the Early All Volunteer Era Affect Subsequent Civilian Income?” Social Science Research 36(4), 1447–1474. [Google Scholar]
- Therneau Terry M. and Grambsch Patricia M.. 2000. Modeling Survival Data: Extending the Cox Model. Springer Science & Business Media. [Google Scholar]
- United States Census Bureau / American FactFinder. 2014. “Number of Veterans.” U.S. Census Bureau’s American Community Survey Office, 2014. Web. December 2016 <http://factfinder2.census.gov>. [Google Scholar]
- Umberson Debra. 1987. “Family Status and Health Behaviors: Social Control as a Dimension of Social Integration.” Journal of Health and Social Behavior 306–319. [PubMed] [Google Scholar]
- Umberson Debra. 1992. “Gender, Marital Status and the Social Control of Health Behavior.” Social Science & Medicine 34(8), 907–917. [DOI] [PubMed] [Google Scholar]
- Umberson Debra, Williams Kristi, Powers Daniel A., Liu Hui, and Needham Belinda. 2006. “You Make Me Sick: Marital Quality and Health over the Life Course.” Journal of Health and Social Behavior 47(1), 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verweij Pierre JM and van Houwelingen Hans C.. 1995. “Time-Dependent Effects of Fixed Covariates in Cox Regression.” Biometrics 1550–1556. [PubMed] [Google Scholar]
- Weinick Robin M., Zuvekas Samuel H., and Cohen Joel W.. 2000. “Racial and Ethnic Differences in Access to and Use of Health Care Services, 1977 to 1996.” Medical Care Research and Review 57(suppl 1), 36–54. [DOI] [PubMed] [Google Scholar]
- Williams David R. and Collins Chiquita. 1995. “US Socioeconomic and Racial Differences in Health: Patterns and Explanations.” Annual Review of Sociology 349–386. [Google Scholar]
- Williams David R. and Jackson Pamela Braboy. 2005. “Social Sources of Racial Disparities in Health.” Health Affairs 24(2), 325–334. [DOI] [PubMed] [Google Scholar]
- Williams David R. and Mohammed Selina A.. 2013. “Racism and Health I: Pathways and Scientific Evidence.” American Behavioral Scientist 57(8), 1152–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilper Andrew P. et al. 2009. “The Health and Health Care of US Prisoners: Results of a Nationwide Survey.” American Journal of Public Health 99(4), 666–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Yang. 2008. “Trends in US Adult Chronic Disease Mortality, 1960–1999: Age, Period, and Cohort Variations.” Demography 45(2), 387–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young Bessie A., Maynard Charles, and Boyko Edward J.. 2003. “Racial Differences in Diabetic Nephropathy, Cardiovascular Disease, and Mortality in a National Population of Veterans.” Diabetes Care 26(8), 2392–2399. [DOI] [PubMed] [Google Scholar]