Abstract
Background –
There is concern that mental and physical fatigue among endoscopists over the course of the day will lead to lower adenoma detection rate (ADR). There are mixed findings in the prior literature on whether such an association exists.
Aims –
To measure the association between the number of colonoscopies performed in a day and ADR and withdrawal time.
Methods –
We analyzed 86,624 colonoscopy and associated pathology reports between October 2013 to September 2015 from 131 physicians at two medical centers. A previously validated natural language processing program was used to abstract relevant data. We identified the order of colonoscopies performed in the physcians’ schedule and calculated the ADR and withdrawal time for each colonoscopy position.
Results –
The ADR for our overall sample was 29.9 (CI, 29.6–30.2). The ADR for colonoscopies performed at the 9th+ position was significantly lower than those at the 1st–4th or 5th–8th position, 27.2 (CI, 25.8–28.6) vs. 29.9 (CI, 29.5–30.3), 30.2 (CI, 29.6–30.9) respectively. Withdrawal time steadily decreased by colonoscopy position going from 11.6 (CI, 11.4–11.9) minutes for the 1st colonoscopy to 9.6 (8.9–10.3) minutes for the 9th colonoscopy.
Conclusion –
In our study population ADR and withdrawal time decrease by roughly 7% and 20% respectively by the end of the day. Our results imply that rather than mental or physical fatigue, lower ADR at the end of the day might be driven by endoscopists rushing.
Keywords: adenoma detection rate, colonoscopy, quality measurement
Introduction
In the United States, colorectal cancer is the second leading cause of cancer-related deaths and third most common cause of cancer.[1] While colonoscopy and sigmoidoscopy are effective means of screening for colorectal cancer, the benefit of screening may be reduced due to variation in the quality of the endoscopic study.[2, 3]
Adenoma detection rate (ADR) is the most validated measure of colonoscopy quality.[4] Lower physician ADR is associated with higher rates of interval colorectal cancer.[5] In a recent modeling study by Meester at al, a 5% decrease in ADR was associated with a 12.3% and 13.3% increase in colorectal cancer incidence and mortality, respectively.[6] One potential driver of lower ADR is that, over the course of a day, an endoscopist may become fatigued and thereby detect fewer adenomas.
Prior research on the association between ADR and fatigue is mixed.[7–13] Fatigue has generally been measured by time of day (morning vs. afternoon colonoscopies) or number of colonoscopies performed on that day until that point. Chan and colleagues found that among early-morning colonoscopies 27% more polyps and 21% more adenomas were identified compared to those later in the day.[11] However, other studies find no association between fatigue and ADR.[9, 10, 14] Lee and colleagues recently analyzed over a quarter million colonoscopies in the Kaiser Permanente system and found no association between ADR and the number of colonoscopies performed.[9]
Given the lack of consensus across prior studies we measured the association between fatigue and ADR in a large multi-system database of colonoscopies and for the first time assess whether changes in withdrawal time might explain prior associations between time of day and adenoma detection.
Methods
We analyzed all colonoscopy and associated pathology reports from October 2013-September 2015 at UPMC, an academic center in Western Pennsylvania, and Central Illinois Endoscopy (CIE), a private endoscopy center in Peoria, IL. In total the dataset contains 86,624 colonoscopies performed by 131 physicians.
Relevant data on indication, removal of polyps, and adenoma detection was abstracted using a natural language processing (NLP) program. NLP is a branch of computer science that uses a computer to read free text and abstract relevant information.[15] Our study group has developed and validated an NLP-based computer program that identifies the necessary data for physician quality measurement.[16–18] The accuracy of the NLP progam was confirmed by comparing specific data elements in 2127 colonoscopy and associated pathology reports which were abstracted both by the NLP system and by trained human coders.[16] The NLP program has been applied to measure quality across several health systems in the US.[17, 19, 20] The data from colonoscopy and pathology notes was supplemented by data on withdrawal time for each colonoscopy which was recorded in a separate field in the medical record for only one of the two sites.
For each colonoscopy, we identified its position (nth colonoscopy) in the physician’s schedule for the day. At one site, this was based on the insertion time and for the other site, it was based on when the colonoscopy report was started (usually at the beginning of the procedure or soon after withdrawal). ADR for each colonoscopy position was the number of adenomas detected in colonoscopies in that position divided by the total number of colonoscopies in that position. To address whether any changes in ADR based on position were driven by patient characteristics, we conducted a sensitivity analysis in which we used a multivariate logistic regression model in which the outcome was whether an adenoma was identified in that colonoscopy and predictor variables were colonoscopy position, patient age, gender, and indication for the procedure (screening, surveillance, diagnostic). If a colonoscopy was performed for both screening and diagnostic purposes (for example, rectal bleeding), it was classified as screening.
Results
The ADR for our overall sample was 29.9 (95% Confidence Interval (CI), 29.6–30.2). The ADR for the first 7 colonoscopies in a day ranged from 29.5 to 30.8 (Table). The ADR for the 8th, 9th, and 10+ colonoscopies in a day decreased to 27.7 (CI, 26.0–29.5), 27.4 (CI, 25.3–29.6), and 27.5 (CI, 25.7–29.2), respectively. When we pool the colonoscopy into groups, the ADR for the 9th or higher position 27.2 (CI, 25.8–28.6) was lower than those performed at the 1st-4th, 5th-8th position, respectively 29.9 (CI, 29.5–30.3), 30.2 (CI, 29.6–30.9), (p< 0.001). Similar trends were seen for polyp detection rate. The decrease in ADR seen after the 8th colonoscopy are attenuated, but remain after adjusting for differences patient and procedure characteristics (Table). In a sensitivity analysis limited only to colonoscopies performed for screening purposes, we also found similar trends with the ADR for the 9th or higher position 28.2 (CI, 26.2–30.4) was lower than those performed at the 1st-4th, 5th-8th position 29.5 (CI, 28.9–30.0), 30.2 (CI, 29.2–31.2), (p< 0.001), respectively.
Table:
Association between colonoscopy position and adenoma detection, polyp detection, and withdrawal time
| Colonoscopy position (nth colonoscopy of the day) | Number of colonoscopies | Adenoma Detection Rate (%, 195% CI) | Polyp detection rate (%, 95% CI) |
Wthdrawal time* (minutes, 95% CI) | Adenoma Detection Rate adjusted for patient characteristics (%, 95% CI) |
|---|---|---|---|---|---|
| 1 | 20,348 | 29.5 (28.9–30.1) | 49.9 (49.2–50.6) | 11.6 (11.4–11.9) | 29.8 (29.1–30.4) |
| 2 | 16,885 | 30.2 (29.5–30.8) | 50.2 (49.4–50.9) | 11.4 (11.2–11.7) | 30.1 (29.4–30.8) |
| 3 | 13,898 | 30.0 (29.2–30.7) | 50.0 (49.2–50.8) | 11.1 (10.9–11.4) | 29.8 (29.0–30.5) |
| 4 | 11,037 | 30.2 (29.3–31.0) | 49.1 (48.2–50.0) | 11.2 (10.9–11.5) | 29.8 (28.9–30.6) |
| 5 | 8,111 | 30.8 (29.8–31.8) | 48.6 (47.5–49.7) | 10.8 (10.5–11.1) | 30.2 (29.2–31.2) |
| 6 | 5,765 | 30.3 (29.1–31.5) | 47.3 (46.0–48.6) | 10.2 (9.8–10.6) | 29.7 (28.6–30.9) |
| 7 | 3,851 | 30.5 (29.1–32.0) | 46.5 (45.0–48.1) | 9.7 (9.3–10.1) | 30.7 (29.2–32.1) |
| 8 | 2,520 | 27.7 (26.0–29.5) | 45.0 (43.1–46.9) | 9.7 (9.2–10.3) | 28.0 (26.2–29.8) |
| 9 | 1,647 | 27.4 (25.3–29.6) | 44.9 (42.5–47.3) | 9.6 (8.9–10.3) | 28.2 (26.0–30.5) |
| 10+ | 2,562 | 27.5 (25.7–29.2) | 43.4 (41.5–45.4) | 9.3 (8.6–9.9) | 28.5 (26.7–30.3) |
Data on withdrawal time were only available at one site and available for 12,637 colonoscopies.
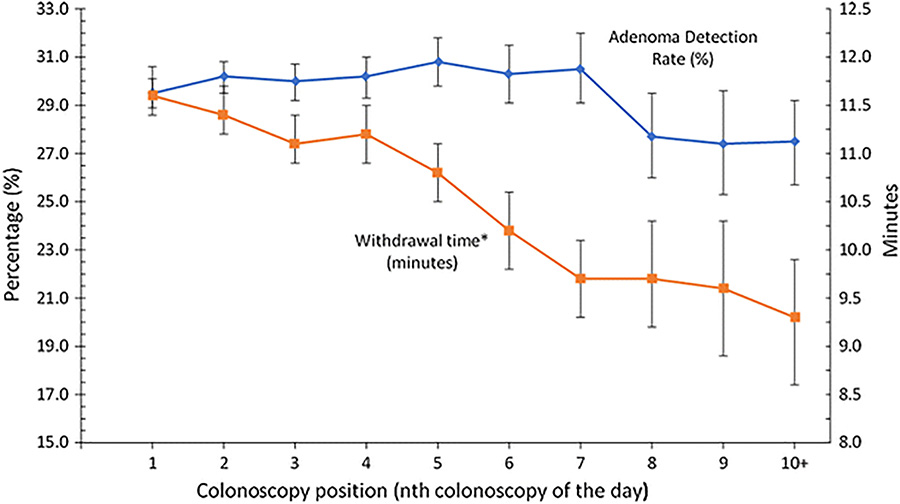
Among colonoscopies for which we have withdrawal time (N=12,637), withdrawal time decreased as colonoscopy position increased going from 11.6 (CI, 11.4–11.9) minutes for the 1st colonoscopy to 9.3 (CI, 8.6–9.9) minutes for the 10th + colonoscopy (Table, Figure).
Figure 1.
Adenoma detection rate and withdrawal time by colonoscopy of the day (data on withdrawal time were only available at one site and available for 12,637 colonoscopies). Error bars reflect the 95% confidence intervals.
Throughout the day, ADR decreased by roughly 7% (percent difference between the first colonoscopy to the last colonoscopy of the day, 29.5% to 27.4%), and withdrawal time decreased by roughly 20% percent (percent difference between the first colonoscopy to the last colonoscopy of the day, 11.6 to 9.3 min) (Table).
Discussion
We find that after the 7th colonoscopy within a procedure day, ADR drops by roughly 7 percent and there is a roughly 20 percent decrease in withdrawal time.
Our results differ from other studies which found no association between fatigue and adenoma detection. However, many of these negative studies had smaller sample sizes (400–4,000 colonoscopies), [7, 8, 10–12, 14] which may have limited their power to identify a difference. Another possibility for the discrepancy is differences in physician payment and practice style between settings. In the large Kaiser Permanente study which found no association between fatigue and ADR,[9] the physicians did not have a strong financial incentive to perform more colonoscopies. We studied two health systems where physician income is at least partially dependent on procedure volume. In the Kaiser Permanente study the median number of colonoscopies performed on a given day by a physician was 3 and the maximum number was 14. In our sample the median was 4 and the maximum number was 18 colonoscopies per day.
Prior literature has hypothesized that mental and physical fatigue over the course of a procedure day drives lower ADR.[7, 11, 21, 22] Our results highlight a potential other mechanism. The steady drop in withdrawal time we observe over the course of the day raises the potential that the drop in ADR seen later in the day is driven not by mental and physical fatigue but rather by physicians being more rushed through the course of the day.
The associations we observe imply that overall ADR would be higher if physicians only performed seven or fewer colonoscopies in a day. However, the impact of such a restriction on overall ADR may be small, given the magnitude of the association between fatigue and ADR and the fraction of all colonoscopies in our sample that are performed in the 8th position or higher. In total, there would be roughly 125 more adenomas if colonoscopies in the 8th position or above had the same ADR as the first 7 colonoscopies of the day.
Our study had several key limitations. The associations we observe are small in magnitude and, even with a sample size of over 80,000 colonoscopies, are only significant when we group colonoscopies. We include only two study sites and data for withdrawal time was only available for one of the sites which limits our generalizability.
In a sample about 80,000 colonoscopies, we evaluated changes in ADR and withdrawal time as the day progressed. We observed that ADR is generally constant up to 7th colonoscopy performed in a day after which ADR decreases by roughly 7%. Withdrawal time appears to decrease over the course of the day (by roughly 20%). Together our results imply that decreases in ADR over the course of the day may be attributed not simply to fatigue, but also to endoscopists being more rushed as the work day progresses.
Grant Support:
Support comes from National Cancer Institute 5R01CA168959
Abbreviations:
- ADR
Adenoma detection rate
- CIE
Central Illinois Endoscopy
- CI
95% confidence interval
Footnotes
Disclosures and Writing Assistance: The authors disclose no conflicts and no writing assistance was provided other than from listed authors.
References
- 1.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics,2010. CA Cancer J Clin. 2010;60:277–300. [DOI] [PubMed] [Google Scholar]
- 2.Schoen RE, Pinsky PF, Weissfeld JL, et al. Colorectal-cancer incidence and mortality with screening flexible sigmoidoscopy. N Engl J Med. 2012;366:2345–2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nishihara R, Wu K, Lochhead P, et al. Long-term colorectal-cancer incidence and mortality after lower endoscopy. N Engl J Med. 2013;369:1095–1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Calderwood AH, Jacobson BC. Colonoscopy quality: metrics and implementation. Gastroenterol Clin North Am. 2013;42:599–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Corley DA, Jensen CD, Marks AR et al. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med. 2014;370:1298–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meester RGS, Doubeni CA, Zauber AG, van Ballegooijen M, Corley DA, Lansdorp-Vogelaar I. Impact of adenoma detection on the benefit of faecal testing versus colonoscopy for colorectal cancer. Int J Cancer. 2017;141:2359–2367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanaka MR, Deepinder F, Thota PN, Lopez R, Burke CA. Adenomas are detected more often in morning than in afternoon colonoscopy. Am J Gastroenterol. 2009;104:1659–1664;quiz 1665. [DOI] [PubMed] [Google Scholar]
- 8.Leffler DA, Kheraj R, Bhansali A, et al. Adenoma detection rates vary minimally with time of day and case rank: a prospective study of 2139 first screening colonoscopies. Gastrointest Endosc. 2012;75:554–560. [DOI] [PubMed] [Google Scholar]
- 9.Lee A, Jensen CD, Marks AR, et al. Endoscopist fatigue estimates and colonoscopic adenoma detection in a large community-based setting. Gastrointest Endosc. 2017;85:601–610.e602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Freedman JS, Harari DY, Bamji ND, et al. The detection of premalignant colon polyps during colonoscopy is stable throughout the workday. Gastrointest Endosc. 2011;73:1197–1206. [DOI] [PubMed] [Google Scholar]
- 11.Chan MY, Cohen H, Spiegel BM. Fewer polyps detected by colonoscopy as the day progresses at a Veteran’s Administration teaching hospital. Clin Gastroenterol Hepatol. 2009;7:1217–1223;quiz 1143. [DOI] [PubMed] [Google Scholar]
- 12.Almadi MA, Sewitch M, Barkun AN, Martel M, Joseph L. Adenoma detection rates decline with increasing procedural hours in an endoscopist’s workload. Can J Gastroenterol Hepatol. 2015;29:304–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Almario CV, Spiegel BMR. Does endoscopist fatigue impact adenoma detection rate? A review of the evidence to date. Gastrointest. Endosc 2017;85:611–613. [DOI] [PubMed] [Google Scholar]
- 14.Lurix E, Hernandez AV, Thoma M, Castro F. Adenoma detection rate is not influenced by full-day blocks, time, or modified queue position. Gastrointest Endosc. 2012;75:827–834. [DOI] [PubMed] [Google Scholar]
- 15.Nadkarni PM, Ohno-Machado L, Chapman WW. Natural language processing: an introduction. J Am Med Inform Assoc. 2011;18:544–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carrell DS, Schoen RE, Leffler DA, et al. Challenges in adapting existing clinical natural language processing systems to multiple, diverse healthcare settings. J Am Med Inform Assoc. 2017;24;986–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mehrotra A, Dellon ES, Schoen RE, et al. Applying a natural language processing tool to electronic health records to assess performance on colonoscopy quality measures. Gastrointest. Endosc 2012;75:1233–1239e1214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harkema H, Chapman WW, Saul M, Dellon ES, Schoen RE, Mehrotra A. Developing a natural language processing application for measuring the quality of colonoscopy procedures. J Am Med Inform Assoc. 2011;18(Suppl 1):i150–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mehrotra A, Morris M, Gourevitch RA, et al. Physician characteristics associated with higher adenoma detection rate. Gastrointest. Endosc 2017;S0015–5107:32205–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marcondes FO, Dean KM, Schoen RE, et al. The impact of exclusion criteria on a physician’s adenoma detection rate. Gastrointest. Endosc 2015;82:668–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Long MD, Martin C, Sandler RS, Herfarth HH, Shaheen NJ, Dellon ES. Reduced polyp detection as endoscopy shift progresses: experience with screening colonoscopy at a tertiary-care hospital. J Clin Gastroenterol. 2011;45:253–258. [DOI] [PubMed] [Google Scholar]
- 22.Munson GW, Harewood GC, Francis DL. Time of day variation in polyp detection rate for colonoscopies performed on a 3-hour shift schedule. Gastrointest Endosc. 2011;73:467–475. [DOI] [PubMed] [Google Scholar]