Abstract
Objectives
Eudaimonic well-being (EWB), increasingly recognized as a critical component of health, typically declines in later life, and there are no existing programs to sustain or increase EWB in older adults. Lighten UP! is an 8-week program to promote EWB through facilitated group sessions in community settings and at-home practice. Building on earlier pilot research, the current study assessed the effect of the Lighten UP! Program using a longitudinal, multi-site design.
Methods
Men and women (N = 169) aged 60 and over were recruited from three Wisconsin communities. EWB, life satisfaction, depression, and diverse aspects of health were assessed before and after the program and at 6-month follow up.
Results
Participants reported significantly increased EWB; these changes were maintained 6 months later. The specific EWB domains of self-acceptance, positive relations, and personal growth showed the most robust gains. Participants also showed significant and sustained declines in depressive symptoms, anxiety, and hostility.
Conclusions
Lighten UP! Program confirmed its positive effects for enhancing EWB in older adults living in multiple community settings.
Clinical implications
Programs that sustain or enhance EWB in older adults can be expected to yield improvements in diverse aspects of mental and physical health.
Keywords: eudaimonic well-being, positive aging, group intervention, depression, positive psychotherapy
Introduction
A growing body of research now addresses issues of well-being and quality of life in older age (Cesetti, Vescovelli, & Ruini, 2017; Clarke, Marshall, Ryff, & Wheaton, 2001; Hill et al., 2017). Conceptual frameworks for defining well-being and for implementing interventions aimed at its promotion are part of this literature. Core definitions distinguish between hedonic well-being and eudaimonic well-being (Ryan & Deci, 2001; Ryff & Singer, 2008). The former describes a general sense of satisfaction with life and the presence of positive affect (Diener, Suh, Lucas, & Smith, 1999; Fredrickson, 2001). Conversely, eudaimonic well-being (EWB) is a complex combination of various psychological and personality characteristics, including: self-acceptance, perceived growth, life perspective and positive interpersonal functioning (Ryff, 2014). Various scholars (Brandel, Vescovelli, & Ruini, 2017; Huta & Waterman, 2014; Waterman et al., 2010) have summarized common definitions of eudaimonic well-being, concluding that it refers to optimal human functioning and pursuit of meaningful goals in life. Importantly, hedonic and eudaimonic well-being have been empirically differentiated and their combination has been advanced as a framework for operationalizing human flourishing (Keyes, 2002; Keyes, Shmotkin, & Ryff, 2002).
Hedonic and eudaimonic well-being are both considered key ingredients of positive ageing (Hill, 2011; Vaillant, 2007). Despite known declines in physical health and functional capacities, growing research has documented its positive features. Further, various investigations have shown that the presence/maintenance of well-being in later life may moderate the impact of these declines (Ryff, 2014). Thus, the maintenance of well-being becomes particularly crucial in later life, when frailty, loneliness and chronic conditions may impair quality of life. Converging lines of evidence suggest that eudaimonic well-being (EWB) is linked with better health and longer life in older adults (Ryff, 2014). Purpose in life, in particular, has been shown to predict reduced risk of disease and disability (Boyle, Buchman, & Bennett, 2010), Alzheimer’s Disease (Boyle, Buchman, Barnes, & Bennett, 2010; Boyle et al., 2012), reduced physiological dysregulation (Zilioli, Slatcher, Ong, & Gruenewald, 2015), and reduced risk of mortality (Boyle, Barnes, Buchman, & Bennett, 2009; Cohen, Bavishi, & Rozanski, 2016; Hill & Turiano, 2014). Other findings have linked purpose in life to increased physical activity (Kim, Kawachi, Chen, & Kubzansky, 2017; Rector, Christ, & Friedman, In Press) and greater use of preventive medical services (Kim, Strecher, & Ryff, 2014). Coupled with evidence that absence of EWB is an independent risk factor for depression in middle-aged and older adults (Wood & Joseph, 2010), extant research underscores the importance of EWB for mental and physical health in later life.
A recent meta-analysis showed that psychosocial and/or psychotherapeutic interventions may improve EWB (Weiss, Westerhof, & Bohlmeijer, 2016). For instance, in clinical settings a specific psychotherapeutic strategy (Well-being Therapy, WBT) has been developed and applied in combination with traditional cognitive behavioral therapy to treat depression, mood and anxiety disorders, with long lasting positive effects (Fava, 2016). Authors of this meta-analysis emphasized that of the 27 randomized trials available in literature, only 5 were targeted to older adults. Further, despite growing evidence that eudaimonic aspects of well-being are uniquely related to better mental and physical health, few prior interventions have targeted EWB specifically (one recent exception being Cantarella et al.,2017). Conceptualized as the process of striving to realize one’s full potential, EWB is a life-long challenge, where incremental improvements are always possible (Ruini, 2017; Vittersø, 2004a; Vittersø & Søholt, 2011a). Accordingly, the main therapeutic goals for eudaimonic interventions center on identifying opportunities for continued personal growth and purpose, even in contexts of diminished health and functional capacities that occur in later life (Ruini, 2017).
The lack of programs specifically designed to sustain or enhance EWB in older adults prompted us to develop Lighten UP!, an 8-week, group-based intervention. Preliminary results from 103 adults age 60 and over from Kenosha County, WI showed marked increases in EWB along with significant declines in depressive and physical symptoms and in sleep complaints (Friedman et al., 2017).
The current study extends the preliminary work in multiple directions. First, a key question was whether improvements in well-being would be maintained over time. Recent reviews of positive interventions in older adults found that only two studies included follow-up evaluations (Sutipan, Intarakamhang, & Macaskill, 2017; Weiss, Westerhof, & Bohlmeijer, 2016); the majority of interventions adopted only a pre-post design. Thus, research on the longitudinal effect of psychological interventions to promote well-being in older adults is largely lacking.
Second, the clinical effect of Lighten UP! in multiple communities with difference demographic and socioeconomic characteristics was of interest. The current study thus included a larger, more diverse sample involving older adults from 3 communities – Brown, Kenosha, and Rock counties in Wisconsin – thereby yielding greater variability in county-level demographic and socioeconomic indicators. Such a sample provides enriched data on the generalizability of the intervention and its potential for more widespread dissemination. The broader sample also afforded opportunities to evaluate the demographic, socioeconomic, and clinical characteristics of participants who derived the most significant benefits from the intervention.
Method
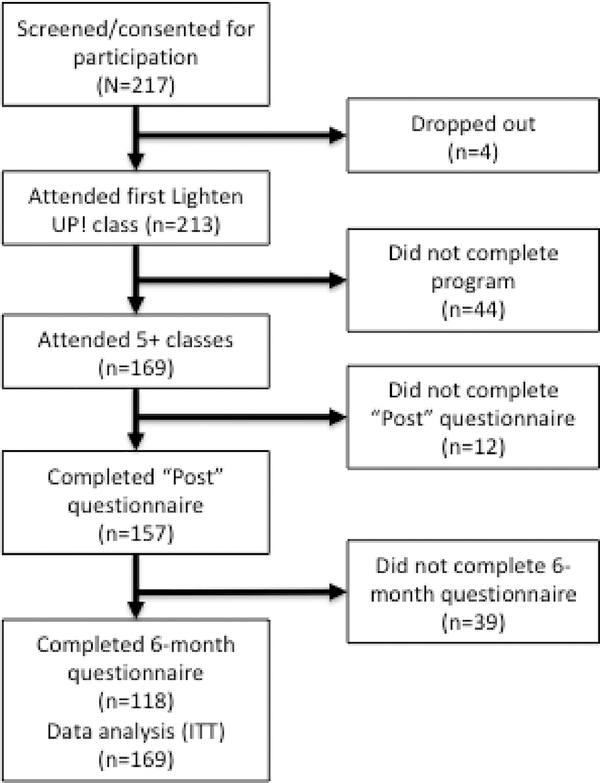
Men and women age 60 or over living independently in 3 different Midwestern communities in the U.S. were referred by local community service organizations for older adults and recruited using advertisements in local newspapers and informational flyers. Candidate participants (N = 217) were screened for severe cognitive impairment by trained staff at each local community center, using a short form of the Mini Mental State Examination (Haubois et al., 2011). Local personnel involved in the screening procedures did not take part to the rest of the intervention. The Mini Mental test was employed as a screening criterion (scores<3), but no candidates were screened out based on their MMSE scores. Four participants declined to start the first class, and not all participants completed the program (see Figure 1 and “Statistical Analyses” below).
Figure 1.
CONSORT diagram.
Protocol
The 8-week program is designed to teach participants how to identify and nurture positive experiences related to meaningful life engagement and how to negotiate negative experiences across multiple domains of life. Participants were placed into groups (23 groups, average size = 10 people) and attended 90 min classes once per week in local community settings (e.g. senior centers; public libraries in the three different Midwestern counties).
The program consisted of 8 classes each building on concepts and material from previous classes (see Appendix). Earlier classes introduce concepts of EWB and ask participants to identify sources of well-being, including from their life histories, as well as obstacles to current well-being, such as functional impairments. Concepts from Cognitive Behavioral Therapy (Beck, 1979), such as automatic thought processes, are then introduced. Participants are taught to recognize such thoughts as well as alternative responses. As with EWB-based interventions targeted to clinical and adolescent populations (Ruini, 2017), part of the focus of Lighten UP! is on automatic thought processes related to positive psychological experiences rather than the more typical negative thought processes that underlie depression or anxiety (Beck, 1979). Later classes focus on enhancing eudaimonia in present life, strategies for overcoming obstacles, and consideration of realistic changes to normal routines that may allow for greater experiences of eudaimonia. In-class group activities – brainstorming, encouragement, discussion – are supported by individual daily at-home practice, including short homework assignments related to the week’s topic. (See Appendix)
To maintain treatment fidelity, all group leaders (9 total) received initial training by a team of scientists, nurses, and social workers those who participated in the initial pilot investigation (Friedman et al., 2017). The training encompassed the use of a standardized manual with protocol descriptions for all sessions. The standardized manual for protocol delivery was carefully followed by new group leaders during the 8 group sessions, via routine supervision by one group leader who was actively involved in the first pilot investigation of Lighten UP!. Supervision was performed by listening to recorded sessions (at least 2 for each group), or by discussing emerging problems encountered by group leaders during the delivery of the protocol (e.g., some participants found journaling activities too difficult or too boring; some participants found it hard to discuss personal events in the class, etc.). Specific suggestions and problem-solving techniques were used to address such issues as they emerged.
All procedures and data use were overseen and approved by the Institutional Review Board at the University of Wisconsin-Madison.
Measures
Participants completed self-administered questionnaires consisting of diverse measures of mental (hedonic and eudaimonic well-being, depression, anxiety, loneliness) and physical health (sleep, somatic symptoms). All reliability estimates provided below are based on baseline scores from the study sample.
Eudaimonic well-being
Eudaimonic well-being was assessed using the Ryff Psychological Well-Being (PWB) scales (Ryff, 1989; Ryff & Keyes, 1995), including sub-scales assessing Environmental Mastery, Personal Growth, Purpose in Life, Positive Relations with Others, Self-Acceptance, and Autonomy (7 statement items for each scale; response options were 1=Disagree Strongly; 7=Agree Strongly). Possible scores ranged from 7–49 with higher scores indicating greater well-being. In the national Mid-Life in the United States (MIDUS) sample, reliability for the full 42-item PWB measure was α=0.94, with estimates ranging from 0.70–0.84 for each of the 6 subscales.
Hedonic well-being
Hedonic well-being was assessed by the Satisfaction with Life Scale (SWLS) (Diener, Emmons, Larsen, & Griffin, 1985), a 5-item scale that used the same 7 response options as the PWB scales. Possible scores ranged from 5–35. Reliability for the SLWS scale was α=0.89.
Additional assessments of physical and mental health
Depressive symptoms were assessed using the Geriatric Depression Scale (GDS) (Yesavage, 1986), a set of 15 questions requiring a “yes” or “no” response. “Yes” responses were scored a ‘1’ and total score ranged from 0–15. Scores on the GDS were ln-transformed to impose a normal distribution for analyses. Reliability for the GDS was α=0.95.
The UCLA Loneliness scale consists of 20-items focused on how often individuals feel lonely and disconnected. Response options are 1=never to 5=always, and possible scores range from 20–100. This scale was also used to examine whether social engagement, particularly among those with higher loneliness profiles, would derive more benefit from the intervention because of its group format. Reliability for the UCLA scale was α=0.87.
The Kellner Symptom Questionnaire (Kellner, 1987) is a 92-item checklist of items grouped into 4 subscales – anxiety, depression, somatic symptoms, and hostility – each consisting of 23 items. Participants indicated any emotion or feeling (e.g. “nervous,” “feeling friendly”) they experienced during the prior week. Scores ranged from 0–23 for each scale.
Sleep quality was assessed using the Pittsburgh Quality of Sleep Index (PSQI; Buysse, Reynolds, Monk, Berman, & Kupfer, 1989; Buysse et al., 1991). The measure includes 19 individual items that yield 7 component scores (e.g. sleep duration, sleep disturbances, daytime dysfunction), resulting in a global score ranging from 0 to 21, where lower scores denote a healthier sleep quality. Participants were also asked about trouble falling or staying asleep in the prior month (1=not at all; 6=almost every day).
Baseline assessments were completed before the first class session with follow-up assessments after the last class and at 6-month follow-up.
Statistical Analyses
All statistical analyses were conducted using Stata version 15 (StataCorp LLC, College Station, TX). Repeated measures analysis of variance (RMANOVA) was used to estimate pre-post-6-month changes in key outcome measures. Pairwise means comparisons were used post hoc to detect mean differences for any significant omnibus effects. Of the 169 participants who completed the pre-program assessments and attended at least 5 classes, 12 did not complete the post-program assessments and 39 did not complete the 6-month follow-up assessments. Data were analysed according to last-observation-carried-forward intention-to-treat (ITT) approaches. An alpha of .05 was the threshold for statistically significant change. The CONSORT diagram for the study is shown in Figure 1. Descriptive and comparative statistics were performed to detect participants who derived the most beneficial effects from intervention (≥1 SD improvements in PWB aggregate scores at post-intervention). In addition to the main analyses of changes in EWB, effects of Lighten UP! on hedonic well-being and other aspects of physical and mental health were assessed. As these were replications of previously observed effects, experiment-wise corrections were not applied.
Results
Descriptive demographic statistics for the full sample and across program sites are shown in Table 1. Participants from Rock County were older, had less educational attainment, and were more likely to be female. There was more racial diversity in participants from Kenosha County compared to Rock and Brown Counties. Participants who failed to complete one or both of the post and follow-up assessments (n = 45; 8 male, 37 female; mean age = 74.4) had poorer sleep (PSQI), but otherwise did not differ from completers on socio-demographic variables or baseline assessments (data not shown).
Table 1.
Descriptive statistics for study sample (N = 169).
| Variables | All Participants (N = 169) | Brown County (n = 55) | Kenosha County (n = 67) | Rock County (n = 47) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Range | % | Mean (SD) | Range | % | Mean (SD) | Range | % | Mean (SD) | Range | % | |
| Demographics | ||||||||||||
| Age | 73.0 (8.1) | 60–92 | 72.2 (8.9) | 60–92 | 73.7 (8.5) | 60–90 | 73.0 (6.1) | 62–84 | ||||
| Sex (% Female) | 85.1 | 85.5 | 82.1 | 89.1 | ||||||||
| Education | ||||||||||||
| High School/GED | 40.0 | 31.5 | 41.5 | 47.8 | ||||||||
| Some college | 31.5 | 37.1 | 29.2 | 28.3 | ||||||||
| College or more | 28.5 | 31.5 | 29.2 | 23.9 | ||||||||
| Race (% non-White) | 4.2 | 1.8 | 7.6 | 2.1 | ||||||||
| Marital status | ||||||||||||
| Married | 28.6 | 29.1 | 32.4 | 21.7 | ||||||||
| Single | 9.5 | 12.7 | 11.9 | 2.2 | ||||||||
| Divorced | 25.0 | 23.6 | 16.4 | 39.1 | ||||||||
| Widowed | 36.9 | 34.6 | 38.8 | 37.0 | ||||||||
Eudaimonic well-being
Table 2 shows scores on the PWB scales and other measures of mental and physical health from the pre-post-6 month assessments along with F-values and partial eta-squared effect size estimates from the RMANOVA models.
Table 2.
Mean scores on measures of mental and physical well-being pre, post, and 6-month follow-up assessments (N = 169).
| Pre-intervention | Post-intervention | 6-month follow-up | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Range | Mean (SD) | Range | Mean (SD) | Range | F-value | Partial eta-squared | |
| Eudaimonic Well-Being | ||||||||
| Psychological Well-Being Scale | 34.7 (6.9) | 17–47.7 | 35.9 (7.0) | 17.7–49 | 35.9 (7.3) | 14.8–49 | 8.92 *** | 0.05 |
| Hedonic Well-Being | ||||||||
| Satisfaction With Life | 4.2 (1.6) | 1–7 | 4.3 (1.5) | 1–7 | 4.4 (1.6) | 1–7 | 1.30 | 0.01 |
| Additional assessments of physical and mental health | ||||||||
| Geriatric Depression Scale | 4.1 (4.0) | 0–14 | 3.4 (3.8) | 0–15 | 3.5 (4.1) | 0–14 | 8.81*** | 0.05 |
| UCLA Loneliness Scale | 42.7 (11.3) | 21–77 | 41.6 (10.2)a | 21–70 | 41.6 (10.8)a | 20–70 | 2.61# | 0.02 |
| Sleep complaints | 4.5 (1.8) | 1–6 | 4.4 (1.8) | 1–6 | 4.1 (1.9)a,b | 1–8 | 2.74# | 0.02 |
| Sleep quality (PSQI) | 7.2 (4.0) | 1–17 | 7.0 (4.0) | 1–17 | 7.1 (4.2) | 1–18 | 0.27 | 0.00 |
| Self-rated health | 3.3 (0.9) | 2–5 | 3.3 (1.0) | 3.3 (0.9) | 0.02 | 0.00 | ||
| Kellner Symptom Q | ||||||||
| Somatization | 7.8 (3.9) | 0–22 | 7.7 (3.9) | 0–19 | 7.7 (3.8) | 0–17 | 0.35 | 0.00 |
| Depression | 7.0 (5.5) | 0–23 | 6.2 (5.1) | 0–23 | 6.5 (5.1) | 0–21 | 4.33* | 0.03 |
| Anxiety | 7.4 (4.5) | 0–22 | 6.2 (4.4) | 0–19 | 6.3 (4.4) | 0–20 | 11.30*** | 0.06 |
| Hostility | 5.1 (3.8) | 0–17 | 4.5 (3.9) | 0–17 | 4.5 (3.4) | 0–16 | 5.16** | 0.03 |
p<.001
p<.01
p<.05
p<.10
p<.001 vs. Pre
p=.02 vs. Post
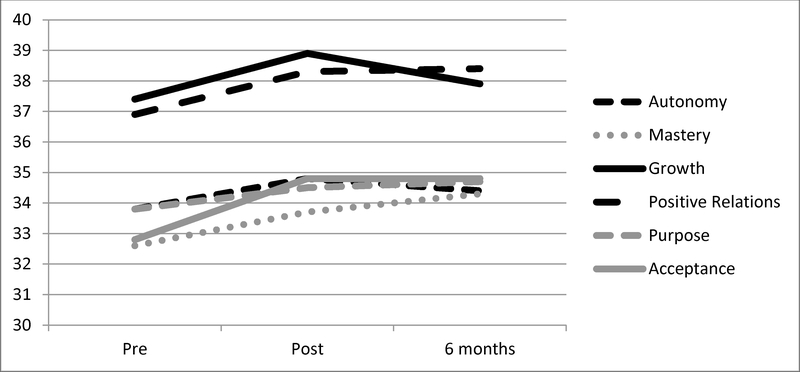
Aggregate scores on PWB increased significantly across the study [F(2,167) = 16.69, p<.001]; pairwise mean comparisons showed significant pre-post increases (p<.001) that were maintained at 6-month follow-up (pre vs. 6-months: p<.001). The partial eta-squared value of 0.05 is interpreted as a medium effect size analogous to a Cohen’s d of 0.4–0.6 (Richardson, 2011). Analyses were repeated using only data from individuals with complete data, and results were identical (data not shown). Additional analyses showed that this pattern of changes remained after adjusting for scores on the UCLA Loneliness Scale, suggesting that improvements on PWB scores were not explained by changes in loneliness that might have resulted from increased social contact during the Lighten UP program. Examination of the 6 individual PWB domains showed significant increases in 5 domains (p<.05), with the most robust increases evident for Self-Acceptance, Personal Growth, and Positive Relations with Others (mean pre-post increases of 2.0, 1.5, and 1.4, respectively). All increases, except Personal Growth (which declined between post and 6-month assessments), were maintained at 6 months (p<.01) (see Figure 2).
Figure 2.
Trajectories of change in the 6 sub-domains of EWB from before Lighten UP! (“pre”), immediately after the final class (“post”), and at 6-month follow-up.
Hedonic well-being; additional assessments of physical and mental health
Analyses of other measures showed significant and sustained decreases in scores on the Geriatric Depression Scale (p<.001) and the depression, anxiety, and hostility components of the Kellner Symptom Questionnaire (p<.001 for all). Post hoc analyses showed significant pre-post and pre vs. 6-month declines in scores on the UCLA scale (p=.002). There were also significant overall increases in subjective sleep ratings (p<.01), although the effect was most robust at 6-month follow-up. There were no marked changes in life satisfaction (hedonic well-being; see Table 2).
Discussion
This study builds upon a robust literature demonstrating the positive effects of psychotherapy for reducing symptoms of depression and anxiety in older adults (Weiss et al., 2016) and extends prior pilot work on Lighten UP! to a larger, more diverse sample involving multiple communities that varied by county-level socioeconomic and demographic characteristics. It also included follow-up assessments. The main finding of this study was significant improvement (both statistically and practically, given the effect sizes) in overall eudaimonic well-being that were maintained 6 months after the end of the program. Additional analysis indicated significant and lasting declines in depressive symptoms, anxiety, and hostility, along with modest improvements in loneliness and sleep complaints. These results replicate earlier results from Lighten UP! and extend them by showing the maintenance of improvements in multiple aspects of mental health in a more diverse sample of older adults.
We note that improvements in eudaimonic well-being occurred without the need for interim booster sessions. This result is consistent with earlier work from clinical populations and community settings and nursing homes (Cesetti et al., 2017; Fava et al., 2004; Ruini & Fava, 2009; Ruini et al., 2009). Taken together, these investigations provide evidence that EWB can be promoted in diverse populations with effects persisting beyond the end of the intervention. Nonetheless, the lack of a control condition is a notable limitation of the study – a point we revisit later in the discussion.
Analyses focused on changes in specific domains of eudaimonia showed that Lighten-UP! yielded particularly robust increases in Self-Acceptance, a dimension considered key to self-development and ego-integrity. Self-Acceptance builds on theoretical formulations of successful aging, including Erikson’s final stage of ego development – integrity vs. despair – (Erikson, 1950) as well as ideas undergirding the process of life review (Butler, 1974). The current results thus support the potential for Lighten Up! to facilitate successful outcomes for late-life developmental tasks.
The results also confirm the distinct relationship between hedonic and eudaimonic well-being in later life (Huta & Ryan, 2010), in that participants showed gains in EWB without parallel changes in life satisfaction. Both hedonic and eudaimonic aspects of well-being have been linked to positive mental and physical health in adults across the lifespan, and both are considered ingredients of positive aging (Hill, 2011; Vaillant, 2007). However, there are important distinctions between hedonic and eudaimonic well-being, especially in the context of aging. While hedonic well-being tends to increase with age and peak in older adults (Gana, Bailly, Saada, Joulain, & Alaphilippe, 2013; Gaymu & Springer, 2010; George, 2010; Sutterlin, Paap, Babic, Kubler, & Vogele, 2012), eudaimonic aspects of well-being, such as purpose in life, show a significant degree of variability between aging individuals (Hill, Turiano, Spiro, & Mroczek, 2015) and may show variable trends of change through the course of middle and later life (Mitchell & Helson, 2016), sometimes resulting in steep declines during the aging process (Irving, Davis, & Collier, 2017).
Conceptual and empirical distinctions between hedonic and eudaimonic have important implications for the success of well-being interventions, particularly in older adults. Some domains of eudaimonia (e.g. self-acceptance) have at their core the process of accepting both positive and negative aspects of oneself and one’s prior life history (Ryff, 1989; Ryff & Keyes, 1995). In contrast, interventions based on hedonic well-being typically aim to increase positive affect and life satisfaction in part through shifting focus away from negative experiences (e.g. age-related adversities) and toward more positive ones (Ruini, 2017). The Lighten UP! intervention thus offers the potential to help aging men and women sustain optimal levels of meaningful engagement, even in the midst of age-related declines and challenges that impair well-being (Fiske, Wetherell, & Gatz, 2009).
Finally, the ability to deliver Lighten UP! in community rather than medical settings enhances its relevance for the broader aging population. Impaired well-being and presence of psychological distress in older adults often go unrecognized in primary care practice as both older patients and their physicians may perceive many of the associated symptoms to be typical age-related declines rather than signs of poor mental health (Alexopoulos, 2005; Cherubini et al., 2012). In addition, while many existing pharmacological and non-pharmacological treatments are effective for reducing distress (Kiosses, Leon, & Arean, 2011; Lee et al., 2012; Wolf & Hopko, 2008), older adults may be less likely to seek treatment for depression or depressive symptoms in traditional medical settings (Laidlaw, 2013). Community-based interventions may be more attractive to many older adults. In fact, the attrition rate for the current intervention was relatively low, with most of the sample expressing appreciation for the group intervention as shown by prior qualitative data (Friedman et al., 2017). Thus, Lighten Up! can fill a valuable niche as a community based intervention to promote complete mental health by enhancing well-being and targeting psychological distress in older adults.
Interpretations of the current results are tempered by notable limitations, the largest being the lack of a control condition. The current study was designed in collaboration with our community partners, and issues surrounding the cost and feasibility of a control condition ultimately led the team to decide to reserve a controlled study for future efforts. Nevertheless, the lack of a control condition does raise the issue of potential alternative explanations for observed effects other than key aspects of the intervention (Wampold, 2015). Improvements in eudaimonic well-being along with declines in depressive symptoms, for example, could be linked to social engagement – participating in a group weekly for 8 weeks. However, significant increases in PWB were observed in models that adjusted for scores on the UCLA Loneliness Scale, suggesting that increased social engagement via the intervention does not explain the observed gains in well-being. Nonetheless, ruling out this and other alternative explanations will require a controlled trial. In addition, the change in mean scores on aggregate EWB and the GDS scale were small, and while these represented moderate effect sizes, it will be important to further determine the significance of these changes, both in the context of a controlled study and by extending the analyses to additional measures of well-being, including biological processes. The analyses also did not account for potential clustering of participant responses by group leaders and participating site, although there did not appear to be differences among the sites. Finally, the large percentage of female participants and general lack of racial/ethnic diversity may limit the broad generalizability of these findings.
There are notable strengths to this study that bolster earlier pilot results on the promise of Lighten UP! to promote EWB in later life. The current study shows that gains in EWB are largely maintained 6-months after the conclusion of the program. These gains were observed across 3 socio-demographically distinct regions in Wisconsin, suggesting that Lighten UP! can be effective for aging adults broadly. It is notable that previous psychosocial interventions in community dwellers have lacked such methodological strengths (Sutipan et al., 2017), such as the use of a multi-center and longitudinal design. Future randomized controlled investigations are needed to distill its unique efficacy in improving eudaimonic well-being and distress in community dwelling older adults.
Clinical Implications.
Group intervention based on the promotion of EWB yielded improvements in well-being, depression, loneliness and sleep quality in a large sample of community dwellers, with diverse sociodemographic characteristics.
The positive effects of this intervention were maintained over 6 months, with no additional booster sessions.
Lighten up! is a structured, manualized group interventions that can be easily delivered by trained group leaders in community centers, nursing homes, or other community facilities for older adults.
Acknowledgements
The authors are grateful to Gayle Love for her extensive assistance with the study and the data collection. Support for this study was from the Wisconsin Partnership Program (WPP) at the University of Wisconsin-Madison and from the National Institute on Aging (AG041750 to EMF).
Appendix
Appendix.
Lighten UP! Eudaimonic Well-Being (EWB) Program
| Sessions | Goal(s) | Activities |
|---|---|---|
| Initial Sessions (1–2) | Identification of episodes of well-being; self-observation | Participants are asked to maintain a structured diary of episodes of well-being |
| Intermediate Sessions (3–5) | Promotion of well-being by scheduling of pleasant activities. Identification of premature interruptions of well-being, either by negative events, physical symptoms or negative thoughts and attitudes toward well-being. |
Participants are encouraged to engage in individually rewarding activities that foster well-being. They are asked to identify specific events, thoughts and beliefs leading to premature interruption of well-being or distorted interpretations of well-being. |
| Final Sessions (6–8) | Positive cognitive restructuring, promotion of a balanced attitude toward well-being, by negotiating individual vulnerabilities with personal resources and skills | Ryff’s six dimensions of psychological well-being are progressively introduced to participants. Participants are not encouraged to pursue the highest levels of well-being in all domains, but to obtain balanced, individualized positive functioning according to their specific needs and living conditions. |
REFERENCES
- Alexopoulos GS (2005). Depression in the elderly. Lancet, 365(9475), 1961–1970. doi:S0140-6736(05)66665-2 [pii] 10.1016/S0140-6736(05)66665-2 [doi] [DOI] [PubMed] [Google Scholar]
- Beck AT (1979). Cogntive Therapy and the Emotional Disorders. New York, NY: Penguin Group. [Google Scholar]
- Boyle PA, Barnes LL, Buchman AS, & Bennett DA (2009). Purpose in life is associated with mortality among community-dwelling older persons. Psychosom Med, 71(5), 574–579. 10.1097/PSY.0b013e3181a5a7c0 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle PA, Buchman AS, Barnes LL, & Bennett DA (2010). Effect of a purpose in life on risk of incident Alzheimer disease and mild cognitive impairment in community-dwelling older persons. Arch Gen Psychiatry, 67(3), 304–310. 10.1001/archgenpsychiatry.2009.208 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle PA, Buchman AS, & Bennett DA (2010). Purpose in life is associated with a reduced risk of incident disability among community-dwelling older persons. Am J Geriatr Psychiatry, 18(12), 1093–1102. doi: 10.1097/JGP.0b013e3181d6c259 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle PA, Buchman AS, Wilson RS, Yu L, Schneider JA, & Bennett DA (2012). Effect of purpose in life on the relation between Alzheimer disease pathologic changes on cognitive function in advanced age. Arch Gen Psychiatry, 69(5), 499–505. doi: 10.1001/archgenpsychiatry.2011.1487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler RN (1974). Successful aging and the role of the life review. Journal of the American Geriatrics Society, 22(12), 529–535. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, & Kupfer DJ (1989). The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res, 28(2), 193–213. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF 3rd, Monk TH, Hoch CC, Yeager AL, & Kupfer DJ (1991). Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh Sleep Quality Index (PSQI). Sleep, 14(4), 331–338. [PubMed] [Google Scholar]
- Cantarella A, Borella E, Marigo C, & De Beni R (2017). Benefits of Well-Being Training in Healthy Older Adults. Appl Psychol-Hlth We, 9(3), 261–284. doi: 10.1111/aphw.12091 [DOI] [PubMed] [Google Scholar]
- Cesetti G, Vescovelli F, & Ruini C (2017). The Promotion of Well-Being in Aging Individuals Living in Nursing Homes: A Controlled Pilot Intervention with Narrative Strategies. Clinical Gerontologist, 40(5), 380–391. doi: 10.1080/07317115.2017.1292979 [DOI] [PubMed] [Google Scholar]
- Cherubini A, Nistico G, Rozzini R, Liperoti R, Di Bari M, Zampi E, … Trabucchi M (2012). Subthreshold depression in older subjects: an unmet therapeutic need. J Nutr Health Aging, 16(10), 909–913. doi: 10.1007/s12603-012-0373-9 [DOI] [PubMed] [Google Scholar]
- Clarke PJ, Marshall VW, Ryff CD, & Wheaton B (2001). Measuring Psychological Well-Being in the Canadian Study of Health and Aging. International Psychogeriatrics, 13(S1), 79–90. doi: 10.1017/S1041610202008013 [DOI] [PubMed] [Google Scholar]
- Cohen R, Bavishi C, & Rozanski A (2016). Purpose in Life and Its Relationship to All-Cause Mortality and Cardiovascular Events: A Meta-Analysis. Psychosom Med, 78(2), 122–133. doi: 10.1097/psy.0000000000000274 [DOI] [PubMed] [Google Scholar]
- Diener E, Emmons RA, Larsen RJ, & Griffin S (1985). The Satisfaction With Life Scale. J Pers Assess, 49(1), 71–75. doi: 10.1207/s15327752jpa4901_13 [doi] [DOI] [PubMed] [Google Scholar]
- Erikson EH (1950). Childhood and society. New York: Norton. [Google Scholar]
- Fava GA (2016). Well-being therapy: Treatment manual and clinical applications: Karger Medical and Scientific Publishers. [Google Scholar]
- Fava GA, Ruini C, Rafanelli C, Finos L, Conti S, & Grandi S (2004). Six-year outcome of cognitive behavior therapy for prevention of recurrent depression. Am J Psychiatry, 161(10), 1872–1876. [DOI] [PubMed] [Google Scholar]
- Fiske A, Wetherell JL, & Gatz M (2009). Depression in older adults. Annu Rev Clin Psychol, 5, 363–389. doi: 10.1146/annurev.clinpsy.032408.153621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman EM, Ruini C, Foy R, Jaros L, Sampson H, & Ryff CD (2017). Lighten UP! A community-based group intervention to promote psychological well-being in older adults. Aging Ment Health, 21(2), 199–205. doi: 10.1080/13607863.2015.1093605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gana K, Bailly N, Saada Y, Joulain M, & Alaphilippe D (2013). Does life satisfaction change in old age: results from an 8-year longitudinal study. J Gerontol B Psychol Sci Soc Sci, 68(4), 540–552. doi: 10.1093/geronb/gbs093 [DOI] [PubMed] [Google Scholar]
- Gaymu J, & Springer S (2010). Living conditions and life satisfaction of older Europeans living alone: a gender and cross-country analysis. Ageing Soc, 30, 1153–1175. [Google Scholar]
- George LK (2010). Still happy after all these years: research frontiers on subjective well-being in later life. J Gerontol B Psychol Sci Soc Sci, 65B(3), 331–339. 10.1093/geronb/gbq006 [doi] [DOI] [PubMed] [Google Scholar]
- Haubois G, Annweiler C, Launay C, Fantino B, de Decker L, Allali G, & Beauchet O (2011). Development of a short form of Mini-Mental State Examination for the screening of dementia in older adults with a memory complaint: a case control study. BMC Geriatr, 11, 59. doi: 10.1186/1471-2318-11-59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill NL, McDermott C, Mogle J, Munoz E, DePasquale N, Wion R, & Whitaker E (2017). Subjective cognitive impairment and quality of life: a systematic review. International Psychogeriatrics, 29(12), 1965–1977. doi: 10.1017/S1041610217001636 [DOI] [PubMed] [Google Scholar]
- Hill PL, & Turiano NA (2014). Purpose in Life as a Predictor of Mortality Across Adulthood. Psychol Sci, 25(7), 1482–1486. doi: 10.1177/0956797614531799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill PL, Turiano NA, Spiro A 3rd, & Mroczek DK (2015). Understanding inter-individual variability in purpose: Longitudinal findings from the VA Normative Aging Study. Psychol Aging, 30(3), 529–533. doi: 10.1037/pag0000020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill RD (2011). A Positive Aging Framework for Guiding Geropsychology Interventions. Behav Ther, 42(1), 66–77. 10.1016/j.beth.2010.04.006 [DOI] [PubMed] [Google Scholar]
- Huta V, & Ryan RM (2010). Pursuing Pleasure or Virtue: The Differential and Overlapping Well-Being Benefits of Hedonic and Eudaimonic Motives. Journal of Happiness Studies, 11(6), 735–762. doi: 10.1007/s10902-009-9171-4 [DOI] [Google Scholar]
- Irving J, Davis S, & Collier A (2017). Aging With Purpose: Systematic Search and Review of Literature Pertaining to Older Adults and Purpose. Int J Aging Human Devel, 85(4), 403–437. doi: 10.1177/0091415017702908 [DOI] [PubMed] [Google Scholar]
- Kellner R (1987). Symptom questionnaire. J Clin Psychiatry, 48, 269–274. [PubMed] [Google Scholar]
- Kim ES, Kawachi I, Chen Y, & Kubzansky LD (2017). Association Between Purpose in Life and Objective Measures of Physical Function in Older Adults. JAMA Psychiatry. doi: 10.1001/jamapsychiatry.2017.2145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim ES, Strecher VJ, & Ryff CD (2014). Purpose in life and use of preventive health care services. Proc Natl Acad Sci U S A, 111(46), 16331–16336. doi: 10.1073/pnas.1414826111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiosses DN, Leon AC, & Arean PA (2011). Psychosocial interventions for late-life major depression: evidence-based treatments, predictors of treatment outcomes, and moderators of treatment effects. Psychiatr Clin North Am, 34(2), 377–401, 10.1016/j.psc.2011.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laidlaw K (2013). A deficit in psychotherapeutic care for older people with depression and anxiety. Gerontology, 59(6), 549–556. doi: 10.1159/000351439 [DOI] [PubMed] [Google Scholar]
- Lee SY, Franchetti MK, Imanbayev A, Gallo JJ, Spira AP, & Lee HB (2012). Non-pharmacological prevention of major depression among community-dwelling older adults: a systematic review of the efficacy of psychotherapy interventions. Arch Gerontol Geriatr, 55(3), 522–529. doi: 10.1016/j.archger.2012.03.003 [DOI] [PubMed] [Google Scholar]
- Mitchell V, & Helson RM (2016). The place of purpose in life in women’s positive aging. Women Ther, 39(1–2), 213–234. doi: 10.1080/02703149.2016.1116856 [DOI] [Google Scholar]
- Rector JL, Christ SL, & Friedman EM (In Press). Well-being and long-term physical activity participation in midlife adults: A latent class analysis. Ann Behav Med [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson JTE (2011). Eta squared and partial eta squared as measures of effect size in educational research. Educ Res Rev, 6(2), 135–147. 10.1016/j.edurev.2010.12.001 [DOI] [Google Scholar]
- Ruini C (2017). Positive Psychology in the Clinical Domains: Research and Practice. New York: Springer. [Google Scholar]
- Ruini C, & Fava GA (2009). Well-being therapy for generalized anxiety disorder. J Clin Psychol, 65(5), 510–519. doi: 10.1002/jclp.20592 [doi] [DOI] [PubMed] [Google Scholar]
- Ruini C, Ottolini F, Tomba E, Belaise C, Albieri E, Visani D, … Fava GA (2009). School intervention for promoting psychological well-being in adolescence. J Behav Ther Exp Psychiatry, 40(4), 522–532. 10.1016/j.jbtep.2009.07.002 [doi] [DOI] [PubMed] [Google Scholar]
- Ryff CD (1989). Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol, 57(6), 1069. [Google Scholar]
- Ryff CD (2014). Psychological well-being revisited: advances in the science and practice of eudaimonia. Psychother Psychosom, 83(1), 10–28. doi: 10.1159/000353263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryff CD, & Keyes CL (1995). The structure of psychological well-being revisited. J Pers Soc Psychol, 69(4), 719–727. doi: 10.1037/0022-3514.69.4.719 [DOI] [PubMed] [Google Scholar]
- Sutipan P, Intarakamhang U, & Macaskill A (2017). The Impact of Positive Psychological Interventions on Well-Being in Healthy Elderly People. J Happiness Stud, 18(1), 269–291. doi: 10.1007/s10902-015-9711-z [DOI] [Google Scholar]
- Sutterlin S, Paap MC, Babic S, Kubler A, & Vogele C (2012). Rumination and age: some things get better. J Aging Res, 2012, 267327. doi: 10.1155/2012/267327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaillant GE (2007). Aging well. Am J Geriatr Psychiatry, 15(3), 181–183. [Google Scholar]
- Wampold BE (2015). How important are the common factors in psychotherapy? An update. World Psychiatry, 14(3), 270–277. doi: 10.1002/wps.20238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss LA, Westerhof GJ, & Bohlmeijer ET (2016). Can We Increase Psychological Well-Being? The Effects of Interventions on Psychological Well-Being: A Meta-Analysis of Randomized Controlled Trials. PLoS One, 11(6), e0158092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf NJ, & Hopko DR (2008). Psychosocial and pharmacological interventions for depressed adults in primary care: a critical review. Clin Psychol Rev, 28(1), 131–161. doi: 10.1016/j.cpr.2007.04.004 [DOI] [PubMed] [Google Scholar]
- Wood AM, & Joseph S (2010). The absence of positive psychological (eudemonic) well-being as a risk factor for depression: a ten year cohort study. J Affect Disord, 122(3), 213–217. doi: 10.1016/j.jad.2009.06.032 [DOI] [PubMed] [Google Scholar]
- Yesavage R (1986). The use of rating depression scales in the elderly In Poon L (Ed.), Memory Assessment of Older Adults. Washington, DC: American Psychological Association. [Google Scholar]
- Zilioli S, Slatcher RB, Ong AD, & Gruenewald TL (2015). Purpose in life predicts allostatic load ten years later. J Psychosom Res, 79(5), 451–457. doi: 10.1016/j.jpsychores.2015.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]