Abstract
Objectives
The aim is to present the technique of successful management of a superior mesenteric artery (SMA) dissecting aneurysm by a purely endovascular approach.
Methods
This was a single centre case report.
Results
Isolated spontaneous SMA dissecting aneurysm is rare, and previously was usually treated by an open or hybrid approach. This is a single centre case report of the successful management of a SMA dissecting aneurysm by a purely endovascular approach.
Conclusions
A pure endovascular approach is feasible and effective in the management of isolated SMA dissecting aneurysm, which is a rare but life threatening condition.
Keywords: Aneurysm, Dissection, Endovascular, Superior mesenteric artery
Highlights
-
•
Isolated spontaneous superior mesenteric artery (SMA) dissecting aneurysm is rare.
-
•
SMA dissecting aneurysm is life-threatening.
-
•
SMA dissecting aneurysm was previously usually treated by open or hybrid approach.
-
•
Management of SMA dissecting aneurysm with pure endovascular approach is effective.
Case report
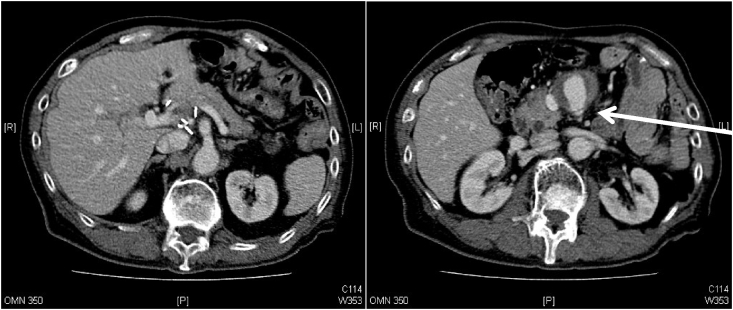
A 69 year old man attended the Accident and Emergency Department in April 2016 with sudden onset of epigastric pain. There was a history of hypertension and stomach cancer treated by radical total gastrectomy in June 2013. The pathology report showed pT3N1M0R0 disease and he had completed adjuvant chemotherapy. Physical examination showed mild epigastric tenderness with no peritoneal signs. A computed tomography scan showed a superior mesenteric artery (SMA) dissecting aneurysm 6.6 cm × 4.8 cm × 4.1 cm (length × width × anteroposterior). It contained circumferential mural thrombus, measuring 2.3 cm maximum thickness. The aneurysm arose from the false lumen measuring 3.0 cm × 2.2 cm (anteroposterior × transverse) in cross sectional diameter (Fig. 1). Endovascular stenting of the SMA and embolisation of the false lumen was the selected treatment after considering the history of total gastrectomy.
Figure 1.
Contrast enhanced computed tomography scan shows the isolated superior mesenteric artery dissecting aneurysm arising from the false lumen. The arrow shows the compressed true lumen.
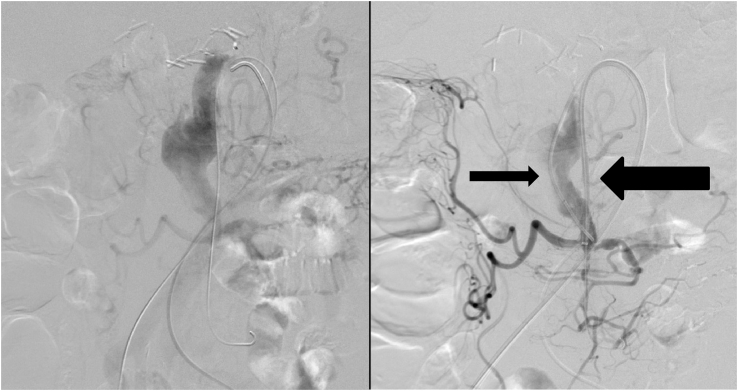
A 5 F arterial sheath was inserted into the right common femoral artery. A transfemoral SMA angiogram confirmed the presence of an entry tear in the proximal SMA. Autofenestration with communication between the true and false lumen was seen. The jejunal and ileal branches were supplied by the true lumen.
The true lumen of the SMA was cannulated with an 0.035 inch guidewire (Terumo Co, Ltd, Tokyo, Japan) and a 4 F angled catheter (Terumo Co, Ltd, Tokyo, Japan). A Rosen guidewire (Cook Medical, Bloomington, IN, USA) was inserted. The 5 F arterial sheath was changed to a 7 F, 70 cm Ansel guiding sheath (Cook Medical) over the Rosen guidewire and engaged in the SMA (Fig. 2).
Figure 2.
On table angiogram shows cannulation of the true (marked with thick arrow) and false (marked with thin arrow) lumens of the superior mesenteric artery dissecting aneurysm.
Another 5 F arterial sheath was inserted into the left common femoral artery. The false lumen of the SMA was cannulated with another 0.035 inch guidewire (Terumo Co, Ltd, Tokyo, Japan) and a 5 F C1 catheter (Cordis Corp, Warren, NJ, USA) (Fig. 2).
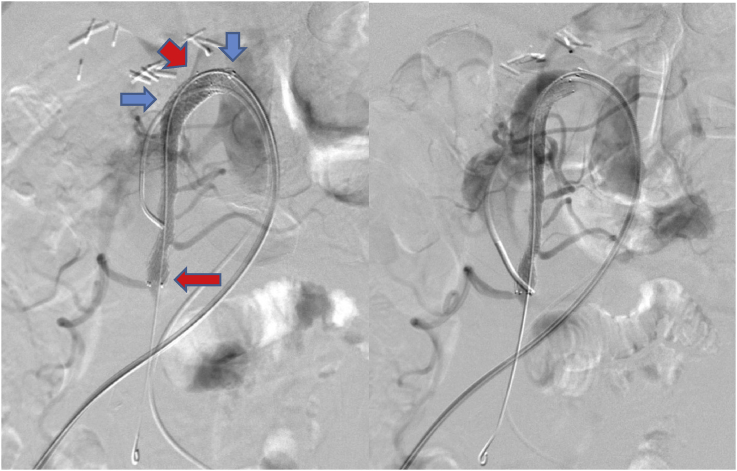
A 10 mm × 38 mm iCAST covered stent (Atrium, Hudson, NH, USA) was implanted via the guiding sheath and deployed at the SMA orifice to cover the entry tear (Fig. 3). Moulding of the iCAST covered stent was performed with a 10 mm × 40 mm Admiral Xtreme balloon (Medtronic PLC, Dublin, Ireland). The false lumen was embolised because of persistent perfusion, and was performed via the C1 catheter with Interlock-35 coils (five 15 mm × 40 cm, five 12 mm × 40 cm, three 10 mm × 40 cm, and one 8 mm × 40 cm) (Boston Scientific, Marlborough, MA, USA). The C1 catheter was removed from the false lumen. A 9 mm × 80 mm Complete self expanding bare stent (Medtronic PLC, Dublin, Ireland) was deployed within the true lumen of the proximal SMA to aid remodelling. The completion angiogram showed successful obliteration of the aneurysm with no endoleak and preservation of the jejunal and ileal branches of the SMA. No side branches of the SMA were covered (Fig. 4). After the procedure, the right femoral arterial access site was closed using the Perclose Proglide Suture Mediated Closure System (Abbott, Chicago, IL, USA), and left groin haemostasis was secured by manual compression.
Figure 3.
On table angiogram after deployment of a bare stent within the true lumen of the proximal SMA and a covered stent at the SMA orifice demonstrates the expansion of true lumen and preservation of the jejunal and ileal branches of SMA. The red arrows point to the ends of the bare stent, and the blue arrows mark the ends of the covered stent. SMA = superior mesenteric artery.
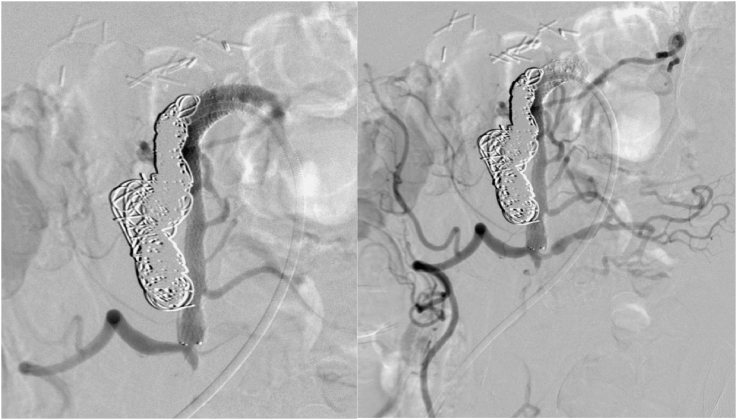
Figure 4.
Completion angiogram shows successful obliteration of the aneurysm with no endoleak observed.
The patient was discharged after four days on aspirin and one month of clopidogrel. There were no post-operative or follow up complications. The epigastric pain subsided and he remained asymptomatic. Interval magnetic resonance imaging scans performed two, 10, and 18 months after the surgery showed patent stents with an occluded aneurysm sac. The perfusion in major branches of the SMA was good (Fig. 5). The hypertension was well controlled by anti-hypertensive medication after the procedure.
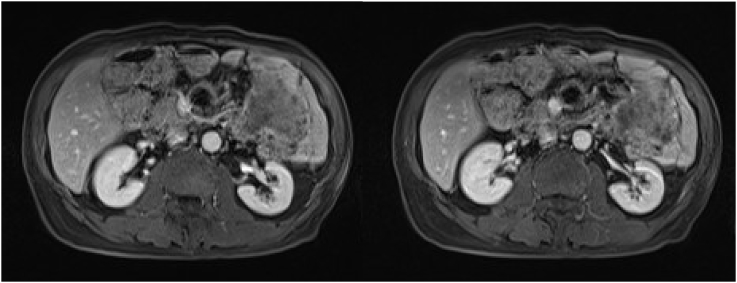
Figure 5.
Magnetic resonance imaging scans performed post-operatively show patent stents with an occluded aneurysm sac.
Discussion
Abdominal visceral artery aneurysm is uncommon with an incidence of 0.01%–2%, with 8% of them arising from the SMA.1 Isolated SMA dissection is also a rare condition, and the pathology includes cystic medial necrosis, fibromuscular dysplasia, atherosclerosis, and trauma.2 As in this case, most patients with SMA dissection present with sudden onset of abdominal pain because of intestinal ischaemia and/or the dissection itself.2, 3, 4, 5, 6, 7, 8
Isolated SMA dissecting aneurysm was previously usually treated by an open or hybrid approach. The open approach includes ligation and bypass or reconstruction with autologous arterial5 or vein6 grafts, and fixation of the intimal flap.8 Hybrid management would involve a transmesenteric approach with midline laparotomy, isolation, and puncture of the ileal artery.9 There are case series and reports on endovascular management (Table 1). Endovascular treatment is less invasive and offers a quicker recovery. This approach takes reference from the endovascular management of type B aortic dissection, with covering of the entry tear by a covered stent, and re expansion of the true lumen by a bare stent, the Provisional ExTension to Induce COmplete ATtachment technique (PETTICOAT technique),10 and embolisation of the false lumen.
Table 1.
Literature review of endovascular treatment of isolated spontaneous SMA dissecting aneurysms over the past five years
| Paper | Year of publication | Type of pathology | Modality of treatment |
|---|---|---|---|
| Wall ML, Newman JE, Slaney PL, et al. Isolated dissecting aneurysms of the abdominal aorta and the superior mesenteric artery. A case report and literature review. Ann Vasc Surg 2014; 28:1937.e5–1937.e8 | 2014 | Dissecting aneurysm of SMA | Endovascular management (infrarenal aortoiliac grafting in this case) has high success rate. |
| Tkalčić L, Budiselić B, Kovačević M, et al. Endovascular management of superior mesenteric artery (sma) aneurysm - adequate access is essential for success - case report. Pol J Radiol 2017; 82:379–83. | 2017 | 2.2 cm SMA aneurysm without dissection | Stenting with covered stents |
| Björck M, Koelemay M, Acosta S, et al. Editor's Choice – Management of the diseases of mesenteric arteries and veins. Eur J Vasc Endovasc Surg 2017; 53:460–510. | 2017 | SMA aneurysms | Asymptomatic aneurysms less than 25mm can be observed (except women of child-bearing age, recipients of abdominal organ transplant, or aneurysms of pancreaticoduodenal and gastroduodenal arcades or hepatic artery) If intervention is indicated, open, laparoscopic, or endovascular repairs can be considered. No modalities are proven to be superior than others Open or laparoscopic repair: resection and end to end anastomosis, re-implantation, graft interposition, or simple ligation Endovascular repair: implantation of a covered or flow diverting stents, embolisation with coils or glue, percutaneous thrombin injection |
| Björck M, Koelemay M, Acosta S, et al. Editor's Choice – management of the diseases of mesenteric arteries and veins. Eur J Vasc Endovasc Surg 2017; 53:460–510 | 2017 | SMA dissections | Asymptomatic patients can be treated by medical therapy (antiplatelet therapy, control of hypertension) Symptomatic patients can be treated by endovascular method most often by stenting If endovascular treatment fails, surgical bypass, intimectomy, thrombectomy, or patch angioplasty can be performed |
| Hussein D, Ashraf A, Ahmed S, Habeeb K. Isolated superior mesenteric artery dissection: a case Report and Literature Review. Gastroenterology Res 2018; 11:374–8 | 2018 | SMA dissection | Conservative management and anticoagulation, endovascular stenting, open surgical repair |
| Waqas U, Maryam M, Hafez MA MD, et al. Diagnosis and management of isolated superior mesenteric artery dissection: a systematic review and meta-analysis. Korean Circ J 2019; 49:400–18 | 2019 | SMA dissection | Conservative or endovascular management can be used in most patients with lower costs, morbidity and mortality. Surgical management should be reserved for complicated cases or indications like vessel rupture or bowel infarction |
SMA = superior mesenteric artery.
In conclusion, a pure endovascular approach is feasible and effective in the management of isolated SMA dissecting aneurysm, which is a rare but life threatening condition.
Conflicts of interest
None.
Funding
None.
References
- 1.Carmeci C., James M.C. Visceral artery aneurysm as seen in a community hospital. Am J Surg. 2000;179:486–489. doi: 10.1016/s0002-9610(00)00380-9. [DOI] [PubMed] [Google Scholar]
- 2.Vignati P.V., Welch J.P., Ellison L., Cohen J.L. Acute mesenteric ischemia caused by isolated superior mesenteric artery dissection. J Vasc Surg. 1992;16:109–112. [PubMed] [Google Scholar]
- 3.Suzuki S., Furui S., Kohtake H., Sakamoto T., Yamasaki M., Furukawa A. Isolated dissection of the superior mesenteric artery: CT findings in six cases. Abdom Imaging. 2004;29:153–157. doi: 10.1007/s00261-003-0110-2. [DOI] [PubMed] [Google Scholar]
- 4.Gouëffic Y., Costargent A., Dupas B., Heymann M.F., Chaillou P., Patra P. Superior mesenteric artery dissection: case report. J Vasc Surg. 2002;35:1003–1005. doi: 10.1067/mva.2002.122152. [DOI] [PubMed] [Google Scholar]
- 5.Picquet J., Abilez O., Pénard J., Jousset Y., Rousselet M.C., Enon B. Superficial femoral artery transposition repair for isolated superior mesenteric artery dissection. J Vasc Surg. 2005;42:788–791. doi: 10.1016/j.jvs.2005.05.048. [DOI] [PubMed] [Google Scholar]
- 6.Iha K., Nakasone H., Nakachi H., Horikawa Y., Gushiken M., Matsuda H. Surgical treatment of spontaneous dissection of the superior mesenteric artery: a case report. Ann Thorac Cardiovasc Surg. 2000;6:65–69. [PubMed] [Google Scholar]
- 7.Barmeir E., Halachmi S., Croitoru S., Torem S. CT angiography diagnosis of spontaneous dissection of the superior mesenteric artery. Am J Roentgen. 1998;171:1429–1430. doi: 10.2214/ajr.171.5.9798897. [DOI] [PubMed] [Google Scholar]
- 8.Cormier F., Ferry J., Artru B., Wechsler B., Cormier J.M. Dissecting aneurysms of the main trunk of the superior mesenteric artery. J Vasc Surg. 1992;16:109–112. [PubMed] [Google Scholar]
- 9.Nomura Yoshikatsu, Yamaguchi Masato, Kitagawa Atsushi, Okada Takuya, Okita Yutaka, Sugimoto Koji. Hybrid management of ruptured isolated superior mesenteric artery dissecting aneurysm. J Vasc Surg. 2011;54:1808–1811. doi: 10.1016/j.jvs.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 10.Melissano G., Bertoglio L., Rinaldi E., Civilini E., Tshomba Y., Kahlberg A. Volume changes in aortic true and false lumen after the “PETTICOAT” procedure for type B aortic dissection. J Vasc Surg. 2012;55:641–651. doi: 10.1016/j.jvs.2011.10.025. [DOI] [PubMed] [Google Scholar]