Abstract
In spite of the enormous economic progress and development witnessed in Indonesia in the last few decades, still more than 30% of Indonesian children under the age of five suffer from stunting, or low height for age. This concern is exacerbated by the fact that stunting remains more concentrated among the poorer households, leading to further intergenerational transmission of poverty and ill health.
We examine recent trends in the evolution of the prevalence of childhood stunting and severe stunting, its socioeconomic inequality and the factors that appear to have contributed to these developments. Using the two most recent waves of the Indonesia Family Life Survey (IFLS), we study the changes in the prevalence of (severe) stunting between 2007 and 2014 for children aged 0–59 months and their socioeconomic-inequality using the Erreygers Concentration Index (EI) and its regression-based decomposition.
We find a significant drop in the rate of severe stunting but not in stunting, as well as a significant reduction in the degree of absolute inequality of stunting. A decomposition analysis shows that household wealth, maternal education, institutional delivery, and availability of adequate sanitation contribute most to socioeconomic inequality in under-five stunting. Further analysis of the change in inequality over time indicates that the reduction in the association of wealth with stunting and a substantial improvement of health care access of the poor (as proxied by immunizations and institutional deliveries) play the most important role in narrowing the stunting gap between richer and poorer kids.
General economic growth, poverty reduction, and implementation of pro-poor health and social programs during the studied period such as the expansion of health insurance coverage for the poor (Jamkesmas) and Conditional Cash Transfer program (Program Keluarga Harapan, PKH) are some plausible explanations of the observed result.
Keywords: Health inequality, Decomposition analysis, Indonesia, Stunting, Malnutrition
Highlights
-
•
Over a third of Indonesian children under the age of five were stunted in 2007.
-
•
Between 2007 and 2014, this rate dropped significantly for severe stunting, but not for stunting.
-
•
Stunting did become less concentrated among the poor in this period.
-
•
A more equal distribution of access to healthcare contributed to this narrowing of the gap.
-
•
New pro-poor health programs and health insurance coverage may have contributed.
Introduction
Stunting, or low height for age, is a growth problem caused by long-term inadequacy of nutrition intake coupled with frequent cases of diseases, mainly during the first 1000 days of life (de Onis & Branca, 2016). It is associated with significant long-term impact in adulthood in the form of reduced cognitive and physical development, higher risk of metabolic disease, and reduced work productivity that might potentially harm future economic growth at national level (Reinhardt & Fanzo, 2014). Globally, stunting affected 161 million children under five years old in 2013, mostly in low-middle income countries (de Onis & Branca, 2016). Although there was a significant reduction compared to its level in 1990, when around 257 million children suffered from stunting, this improvement was not equally distributed. Asian countries showed a more impressive result with 23 percentage-points reductions (from 48% to 25%) while only eight percentage-points reduction was recorded in African countries (from 42% to 34%) (de Onis & Branca, 2016).
Amidst the impressive Asian regional progress, Indonesia—the most populous country in Southeast Asia— is still left behind. In spite of its significant economic growth and poverty reduction in the last decade (OECD Economic, 2016), the prevalence of under-five stunting has not fallen. Based on the Indonesia Basic Health Research report (NIHRD, 2013), an even slightly higher prevalence of under-five stunting was found in 2013 (37.2%) compared to 2010 (35.6%) and 2007 (36.8%). This burden puts Indonesia at the same average stunting level as Cambodia, a neighboring country with less than a half of Indonesian income per capita, and it compares even worse to the rates of countries with more comparable income levels such as The Philippines and Vietnam (Chaparro, Oot, & Sethuraman, 2014). At this pace, it will be difficult for Indonesia to achieve the 2012 World Health Assembly goal to reduce stunting by 40% in 2025 (de Onis et al., 2013).
Moreover, the prevalence of stunting in Indonesia is higher among poorer households (Rachmi, Agho, Li, & Baur, 2016; De Silva & Sumarto, 2018; The World Bank, 2017). The association with living standards might be explained by several factors, including insufficiency of food (both quality and quantity), worse sanitation, unavailability of clean water, difficult access to health care and other health-related behaviors (Torlesse et al., 2016). In order to address some of those problems, between 2007 and 2014, several government programs were implemented. Starting from 2007, the Indonesia government has piloted a Conditional Cash Transfer (CCT) program called Program Keluarga Harapan (Family Hope Program) and a community level intervention called Generasi which were aimed to reward child health, maternal health, and child education inputs such as immunization, growth monitoring, ante and post-natal care, and nine years of compulsory schooling (Olken, Onishi, & Wong, 2014). Other notable efforts include the implementation of Jamkesmas, a central government-financed health insurance for the poor and of several local government programs called Jamkesda (Harimurti, Pambudi, Pigazzini, & Tandon, 2013). Additionally, a specific scheme for maternal health care called Jampersal was introduced, but only for a short period between 2011 and 2013 (Achadi, Achadi, Pambudi, & Marzoeki, 2014). Subsequently, all of those schemes were integrated into a single national health insurance program named Jaminan Kesehatan Nasional (JKN) in 2014 (Mboi, 2015).
Recent studies in Vietnam, Zambia, and Bangladesh find that the rich-poor disparity in stunting prevalence has grown. In Vietnam and Bangladesh, the main driver of that change was the growing inequality of household wealth (Huda, Hayes, & Dibley, 2017; Kien et al., 2016) while in Zambia, the largest contributor is institutional delivery (Hangoma, Aakvik, & Robberstad, 2017). In Indonesia, whether and to what extent socioeconomic-related inequality in childhood stunting has changed over time and what accounts for that is largely unknown. Available evidence to date (Mani, 2014; Rachmi et al., 2016; De Silva & Sumarto, 2018; Torlesse, Cronin, Sebayang, & Nandy, 2016) has only focused on the trend and the potential determinants of childhood stunting. Better evidence about the change and degree of socioeconomic inequality and its contributing factors may help guide and improve any policies aimed at narrowing this gap. That is why this study mainly aims to examine: (1) trend of childhood stunting's prevalence over time; (2) the magnitude and trend of socioeconomic-related inequality in childhood stunting; and (3) the contributing factors to those inequalities and their change over time.
We analyse individual and household level data from the fourth and fifth wave of the Indonesia Family Life Survey (IFLS) collected in 2007 and 2014. Child's nutritional status is measured using the WHO growth standard (WHO, 2006) while socioeconomic status is measured using household wealth index. Inequality analysis is measured using the Erreygers Concentration Index (EI), as well as the decomposition of the index and of its change (Erreygers, 2009; Van Doorslaer & Van Ourti, 2011; Wagstaff, Van Doorslaer, & Watanabe, 2003). Discussion of the determinants of stunting on the basis of the UNICEF (1990) conceptual framework and as measured in the IFLS is deferred until section 2.4 below.
Data and methods
Data
We use the two latest waves of the Indonesia Family Life Survey (IFLS) collected in 2007 (fourth wave) and 2014 (fifth wave). The IFLS is an ongoing longitudinal individual-level, household-level, and community-level survey covered 13 out of 26 provinces when it started in 1993 and representing 83% of the Indonesian population. In the first IFLS, stratified random sampling at province level was used based on National Socioeconomic Smith & Haddad, 2015 sampling frame with household as its primary sampling unit. Later waves also included split-off households. The 4th and 5th IFLS contain 10,435 households and 15,349 households respectively (Strauss, Beegle, Sikoki, & Wattie, 2009; Strauss, Witoelar, and Bondan, 2016).
All children aged 0–59 months in each wave with complete records of anthropometric measurement (height and weight), age, and gender are included. Because of the long (seven years) interval between surveys, the two waves were treated as two separate cross-sections. While none of the children could be in the analysis in both waves, only about 1 in 7 households are in both waves (1081 from 6993 households, 15.46%).
Outcome variables
Height/length-for-age Z-score (HAZ-score) is measured using the WHO, 2006 growth standard. It categorizes children as stunted if their HAZ-score is below -2 and categorized as severely stunted when it is below -3 (de Onis, 2007). In the IFLS, physical health measurement, including anthropometrics, was done by professional nurses who accompanied the interviewer1 (Frankenberg, Karoly, Gertler, Peterson, & Wesley, 1995). We excluded statistically implausible values — i.e. HAZ less than -6 and more than +6 — based on WHO Anthro software manual (WHO, 2006).
Socioeconomic status
Socioeconomic status was measured using a household wealth index, obtained from a Principal Components Analysis (PCA) (Filmer & Pritchett, 2001). We pooled both waves to avoid any difference in the wealth index deriving from changes in the weighting factors (Houweling, Kunst, & Mackenbach, 2003). The index is based on the ownership of assets such as home, land, building, electronic devices (television, radio, refrigerator, etc), any type of vehicle, jewelry, savings, poultry and some household characteristics such as their roof, floor, and wall materials, the use of pipe water source, and the type of fuel used for cooking. From the predicted wealth index, wealth quintiles and wealth tertiles in each wave were created.
Explanatory variables
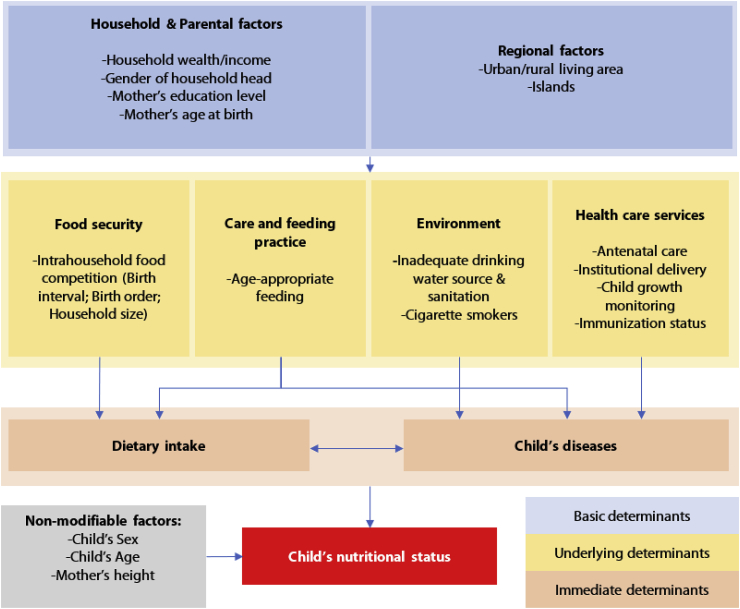
For identifying the explanatory variables, we rely on the UNICEF (1990) conceptual framework of the determinants of child nutritional status (Smith and Haddad, 2015) and the previous work of Torlesse et al. (2016) and Beal, Tumilowicz, Sutrisna, Izwardy, and Neufeld (2018) as presented in Fig. 1. Generally, we divide the determinants into non-modifiable and potentially modifiable factors. For non-modifiable factors, the most crucial determinants are child's age and sex (Victora, de Onis, Hallal, Blossner, & Shrimpton, 2010). Additionally, mother's height is also considered as a nonmodifiable factor (in the short run, for any given child) since some part of a child's height is explained by genetic factors (Sinha et al., 2018).
Fig. 1.
Conceptual Framework on the determinants of child's nutritional status. Source: Author, based on the UNICEF (1990)conceptual framework.
The modifiable factors can be further categorized as immediate, underlying, and basic determinants. Immediate factors are the channels through which the underlying determinants influence the child's nutritional status. It includes adequacy of child's dietary intake and the presence of child's diseases. The adequacy of nutritional needs is determined by food security and feeding practice. Adequacy of feeding practice is partially reflected by proper infant and young child feeding (IYCF) practices (Campbell et al., 2017) as measured using the definition of age-appropriate feeding by WHO (2009). The other causes, grouped as food security, can be measured by a proxy for intrahousehold food competition, captured by the their birth order and interval as well as the number of children and their household size (Ali Naser et al., 2014).
Another immediate cause is the presence of diseases. Those are influenced by three other underlying factors namely inadequate feeding and care, unhealthy environment and inadequate health services. Environmental conditions are proxied by variables indicating water source, toilet sanitation, the presence of smokers in the household, and presence of animal or human faeces around the house (Best et al., 2008; D.; Headey et al., 2017; Torlesse et al., 2016). The sufficiency of health care services is represented by maternal antenatal care visits, place of birth delivery, and completeness of child immunization (Beal et al., 2018, pp. 1–10).
In addition to household wealth, maternal education is also known to have a substantial role in explaining child's health and nutritional status, either through its positive correlation with better health-seeking behavior or though enhanced capability to provide adequate care (Alderman & Headey, 2017; Onah et al., 2014). Regional variation was controlled for using a dummy variable for urban residence and for five of Indonesia's islands (Sumatra, Java, Kalimantan, Sulawesi, Bali and Nusa Tenggara). Details on the operational definition of each variable are provided in Appendix A.
Analysis
As all of our outcomes and determinants are binary (bounded to 0 and 1), we use the Erreygers Concentration Index (EI) (Erreygers, 2009), to analyse the degree of socioeconomic-inequality in childhood stunting. The EI values range between -1 and 1, with a negative value indicating that the health outcome is more concentrated amongst the poor (Kjellsson & Gerdtham, 2013). EI is formally defined as follow:
| (1) |
where is the sample size, is the binary outcome variable of interest for person and is the fractional rank of individual i by wealth index (O’Donnell, O’Neill, Van Ourti, & Walsh, 2016).
To examine the contribution of each determinant to stunting inequality, the outcome variable is first explained using a linear regression (Equation (2)) and then decomposed using Equation (3).
| (2) |
| (3) |
where is the set of determinants (in binary form) of stunting, as its coefficient, as its adjusted concentration index, and as the error terms (Van Doorslaer & Van Ourti, 2011; Wagstaff et al., 2003).
Finally, the change in EI from 2007 (t-1) to 2014 (t) was decomposed using the Oaxaca-like decomposition to estimate the contribution of the change in determinants’ inequality and the change of their partial associations with health outcome (Van Doorslaer & Van Ourti, 2011). The formal decomposition of change in EI can be written as equation (4).
| (4) |
Statistical analysis was conducted using Stata 15.1 (StataCorp, College Station, Texas, USA). Household sample weights for cross-sectional analysis were applied when constructing household wealth index, wealth quintiles, and wealth tertiles. Individual sample weights were used for estimating national prevalence, regression analysis, and inequality analysis. Standard error estimates were adjusted for heteroskedasticity and household level clustering.
Results
Descriptive statistics
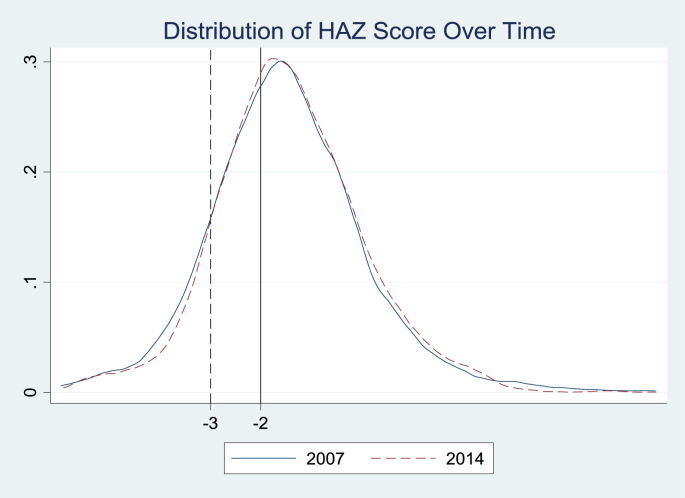
Due to statistically implausible values of anthropometric z-scores, we excluded 465 observations in 2007 and 204 observations in 2014. The final sample of children under five years old in 2007 and 2014 was 4247 and 4723 respectively. Results presented in Table 1 suggest that over this period Indonesia experienced a slight improvement in children's linear growth status, but the change is only statistically significant for the prevalence of severe stunting. The mean HAZ-score increased from -1.438 to -1.412, the stunting rate decreased from 35.4% to 34.2%, while the severe stunting rate decreased from 13.7% to 11.2%. Among the determinants, only age-appropriate feeding, full immunization (in all children aged 0–59 months), and clean household environment show some deterioration while most other variables show some improvement.
Table 1.
Summary statistics for analysis sample.
| Variable | 2007 | 2014 | Change |
|---|---|---|---|
| Outcomes | |||
| HAZ Score | −1.438 (0.024) | −1.412 (0.021) | 0.026 (0.036) |
| Stunting | 0.354 (0.007) | 0.342 (0.007) | −0.013 (0.011) |
| Severe Stunting | 0.137 (0.005) | 0.112 (0.005) | −0.025*** (0.008) |
| Underlying Determinants | |||
| Care and Feeding Practice | |||
| Age-appropriate feeding | 0.679 (0.007) | 0.568 (0.007) | −0.111*** (0.011) |
| Health Care Services | |||
| Full immunization | 0.33 (0.007) | 0.308 (0.007) | −0.022* (0.011) |
| Full immunization (Age 12–23 months) | 0.389 (0.016) | 0.445 (0.016) | 0.056** (0.026) |
| 4 + ANC | 0.899 (0.005) | 0.936 (0.004) | 0.037*** (0.007) |
| Institutional delivery | 0.591 (0.008) | 0.803 (0.006) | 0.211*** (0.011) |
| Posyandu participation | 0.454 (0.008) | 0.495 (0.007) | 0.041*** (0.012) |
| Healthy Environment | |||
| Safe drinking water | 0.934 (0.004) | 0.938 (0.004) | 0.004 (0.006) |
| Improved sanitation | 0.636 (0.007) | 0.736 (0.006) | 0.1*** (0.011) |
| Clean HH environment | 0.941 (0.004) | 0.918 (0.004) | −0.023*** (0.006) |
| >1 smoker in HH | 0.106 (0.005) | 0.109 (0.005) | 0.003 (0.008) |
| Intrahousehold food competition | |||
| Birth order and interval | |||
| First born | 0.053 (0.003) | 0.034 (0.003) | −0.03*** (0.01) |
| Short birth interval (<24 month) | 0.320 (0.007) | 0.369 (0.007) | −0.019*** (0.004) |
| Long birth interval (≥24 month) | 0.053 (0.003) | 0.034 (0.003) | 0.049*** (0.01) |
| Number of HH member >4 | 0.476 (0.008) | 0.458 (0.007) | −0.018 (0.012) |
| Basic Determinants | |||
| Household and Parental Factors | |||
| Household wealth | |||
| Poorest third | 0.357 (0.007) | 0.339 (0.007) | −0.018 (0.011) |
| Middle third | 0.311 (0.007) | 0.324 (0.007) | 0.013 (0.012) |
| Richest third | 0.332 (0.007) | 0.337 (0.007) | 0.005 (0.012) |
| Electricity | 0.963 (0.003) | 0.993 (0.001) | 0.03*** (0.004) |
| Mother's education min.Junior High School | 0.607 (0.007) | 0.714 (0.007) | 0.108*** (0.011) |
| Mother's age at birth <20 years | 0.132 (0.005) | 0.129 (0.005) | −0.003 (0.008) |
| Male HH head | 0.902 (0.005) | 0.886 (0.005) | −0.016** (0.008) |
| Non-modifiable factors | |||
| Male Child | 0.508 (0.008) | 0.507 (0.007) | −0.002 (0.012) |
| Child's age | |||
| 0–5 months | 0.101 (0.005) | 0.106 (0.004) | 0.004 (0.007) |
| 6–11 months | 0.1 (0.005) | 0.103 (0.004) | 0.003 (0.007) |
| 12–23 months | 0.206 (0.006) | 0.196 (0.006) | −0.01 (0.009) |
| ≥>=24 months | 0.593 (0.008) | 0.595 (0.007) | 0.003 (0.011) |
| Mother short stature (<145 cm) | 0.103 (0.005) | 0.104 (0.004) | 0.001 (0.007) |
| Regional Factors | |||
| Urban | 0.454 (0.008) | 0.501 (0.007) | 0.048*** (0.012) |
| Island | |||
| Sumatra | 0.21 (0.006) | 0.188 (0.006) | −0.023*** (0.008) |
| Java | 0.669 (0.007) | 0.692 (0.007) | 0.023** (0.009) |
| Kalimantan | 0.05 (0.003) | 0.049 (0.003) | −0.001 (0.003) |
| Bali and Nusa Tenggara | 0.035 (0.003) | 0.038 (0.003) | 0.004 (0.003) |
| Sulawesi | 0.036 (0.003) | 0.034 (0.003) | −0.003 (0.003) |
| Observations | 4247 | 4723 | |
Robust standard errors in parentheses; *p < 0.10, **p < 0.05, ***p < 0.01.
Trends in socioeconomic inequality in childhood stunting and severe stunting
The evolution in the distribution of stunting and severe stunting over time and by wealth quintiles is shown graphically in Fig. 2, Fig. 3. We find that the reduction in stunting level mainly occurred in the first and second quintile (3.7 and 5.9-percentage point drops respectively) while, perhaps surprisingly, a slight increase was observed in the fourth and fifth quintile (2.9-percentage points and 1.9-percentage points, respectively). Severe stunting declined in all wealth quintiles with the greatest reduction observed in the second quintile (5.5-percentage points). However, the difference over time was only statistically significant in the 2nd quintile for both stunting and severe stunting.
Fig. 2.
Density distribution of HAZ score of under-five children, 2007 and 2014.
Fig. 3.
The estimated prevalence of under-five stunting and severe stunting across different quintile of socioeconomic status in 2007 and 2014.
Changes in the degree of wealth-related inequality of childhood (severe) stunting, as measured with the Erreygers Concentration Index (EI), are presented in Table 2. We estimate negative values of EI for both stunting and severe stunting, meaning that the distribution of both outcomes is more concentrated among the poor. The last column indicates that there was a significant decrease in the inequality for stunting (0.07 points reduction) but not for severe stunting. For reasons of space, we proceed only with a decomposition of the significant change in the next section.2
Table 2.
Change in socioeconomic-related inequality in under-five stunting and severe stunting.
| Population | 2007 | 2014 | Change over Time |
|---|---|---|---|
| N=4247 | N=4723 | ||
| Stunting | −0.172*** (0.018) | −0.099*** (0.018) | 0.073*** (0.025) |
| Severe Stunting | −0.062*** (0.013) | −0.043*** (0.012) | 0.018 (0.018) |
Notes: Robust standard error in parentheses; *p < 0.10, **p < 0.05, ***p < 0.01; All indices were computed for restricted sample using conindex command (O'Donnell et al., 2016).
Decomposition of socioeconomic inequalities of stunting and their change over time
An OLS estimated Linear Probability Model (LPM) is used to assess the association between stunting and its determinants since the decomposition only holds exactly for linear models. For comparison, we also show the marginal effects obtained from logistic regression. It can be seen that both the magnitude and significance of the point estimates are quite similar to those obtained from the LPM (see Table 3).
Table 3.
OLS estimated coefficients of LPM and Average Marginal Effects from Logistic Regression for determinants of under-five stunting.
| Determinants | LPM |
Average Marginal Effect |
||
|---|---|---|---|---|
| 2007 | 2014 | 2007 | 2014 | |
| Care and Feeding Practice | ||||
| Age-appropriate feeding | −0.016(0.018) | −0.027* (0.016) | −0.016 (0.017) | −0.027* (0.016) |
| Health care services | ||||
| Full immunization | −0.043** (0.018) | −0.031* (0.018) | −0.042** (0.018) | −0.029* (0.018) |
| 4 + ANC visits | −0.008 (0.029) | −0.015 (0.034) | −0.007 (0.027) | −0.014 (0.033) |
| Institutional delivery | −0.042** (0.020) | −0.021(0.022) | −0.040**(0.019) | −0.019(0.021) |
| Posyandu participation | 0.015(0.017) | −0.012(0.017) | 0.015(0.017) | −0.011(0.017) |
| Healthy environment | ||||
| Safe drinking water | −0.066**(0.032) | −0.014(0.035) | −0.060**(0.029) | −0.011(0.033) |
| Improved sanitation | −0.015(0.019) | −0.036*(0.020) | −0.014(0.018) | −0.035*(0.019) |
| Clean HH environment | −0.075**(0.036) | −0.027(0.031) | −0.069**(0.033) | −0.026(0.029) |
| >1 smoker in HH | 0.022(0.028) | 0.041(0.027) | 0.022(0.027) | 0.041(0.026) |
| Intrahousehold food competition | ||||
| Birth order and interval | ||||
| First-born | Reference | |||
| Short birth interval | 0.084**(0.036) | 0.119***(0.041) | 0.082**(0.033) | 0.116***(0.038) |
| Long birth interval | 0.007(0.018) | 0.057***(0.017) | 0.007(0.018) | 0.056***(0.017) |
| Number of HH members >4 | 0.006(0.017) | −0.018(0.017) | 0.006(0.017) | −0.019(0.017) |
| Household and parental factor | ||||
| Household wealth | ||||
| Poorest third | Reference | |||
| Middle third | −0.054**(0.022) | −0.026(0.022) | −0.050**(0.021) | −0.026(0.021) |
| Richest third | −0.083***(0.025) | −0.007(0.024) | −0.082***(0.025) | −0.006(0.023) |
| Electricity | −0.020(0.049) | −0.080(0.083) | −0.017(0.044) | −0.076(0.078) |
| Mother's education min. Junior High School | −0.041**(0.019) | −0.054***(0.020) | −0.040**(0.018) | −0.052***(0.019) |
| Mother's age at birth <20 years | 0.028(0.024) | 0.085***(0.026) | 0.028(0.023) | 0.081***(0.024) |
| Male HH head | 0.020(0.027) | −0.018(0.026) | 0.020(0.027) | −0.017(0.025) |
| Non-modifiable factors | ||||
| Male Child | 0.020(0.016) | 0.012(0.015) | 0.020(0.015) | 0.012(0.015) |
| Child's age | ||||
| 0-5 months | Reference | |||
| 6–11 months | 0.004(0.035) | 0.031(0.033) | 0.006(0.039) | 0.041(0.040) |
| 12–23 months | 0.158***(0.030) | 0.239***(0.030) | 0.160***(0.032) | 0.248***(0.034) |
| ≥24 months | 0.103***(0.027) | 0.158***(0.026) | 0.106***(0.029) | 0.173***(0.032) |
| Mother short stature (<145 cm) | 0.170***(0.028) | 0.229***(0.027) | 0.157***(0.025) | 0.209***(0.023) |
| Regional factors | ||||
| Urban | −0.024(0.018) | −0.035*(0.018) | −0.025(0.018) | −0.034*(0.018) |
| Island | ||||
| Java | Reference | |||
| Sumatra | −0.015(0.023) | −0.020(0.021) | −0.013(0.022) | −0.020(0.021) |
| Kalimantan | 0.050**(0.025) | 0.074***(0.025) | 0.048**(0.024) | 0.072***(0.024) |
| Bali and Nusa Tenggara | −0.010(0.040) | 0.025(0.037) | −0.010(0.038) | 0.024(0.035) |
| Sulawesi | 0.074**(0.038) | 0.051(0.039) | 0.068**(0.035) | 0.051(0.037) |
| Constant | 0.490***(0.076) | 0.421***(0.101) | ||
| Observations | 4247 | 4723 | 4247 | 4723 |
| Adjusted R2 | 0.055 | 0.066 | ||
Note: Robust standard errors in parentheses. *p < 0.10, **p < 0.05, ***p < 0.01.
We can see that child's age and maternal stature show a significant positive association with stunting in both periods while child's sex does not. As for intra-household food competition, compared to first-borns, subsequent children are more likely to be stunted, this association is higher for those who have short birth interval. Of the health care utilization variables, complete immunization, at least four ANC visits during pregnancy, and being born in any type of health facility are all negatively associated with stunting, but only full immunization shows a statistically significant coefficient in both years.
Safe drinking water and the availability of electricity in the household are associated with a lower stunting risk while the opposite is true for the presence of cigarette smokers in the household. Improved household sanitation and a clean household environment show a negative association with stunting (albeit only significant in 2014 for the former and only in 2007 for the latter). At household and parental level, wealth, maternal education, and older mother all show a significant protective effect against stunting (except for wealth in 2014 and mother's age in 2007). Lastly, children living in urban areas and in Java island are on average less likely to be stunted.
Next, Table 4 shows – for each determinant – its contribution to the EI of stunting as the product of its (partial) effect on stunting () and its distribution by wealth (). In both years, the strongest driver of inequalities is household wealth itself, followed by maternal education and institutional delivery. In 2007, household wealth contributed 44% of total inequality while in 2014 this was to only 5%. Institutional delivery also showed much lower contribution in the second period (from 11% to only 5%). On the other hand, maternal education became slightly more important in 2014 with the contribution going from 8% to 13%. Mother's stature, maternal age at birth, and household sanitation also showed a similar trend. Living in the urban area had a moderate role with 6% and 12% contribution in 2007 and 2014 respectively while regional differences as captured by the island fixed effects only show a limited contribution to total inequality. Lastly, there are no other covariates with a substantial role in lowering the disparities between these years.
Table 4.
Decomposition of Erreygers Concentration Index (EI) in 2007, 2014, and of its change.
| Determinants | 2007 |
2014 |
Change |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Contr.() | % | Contr.() | % | Equation 4 |
||||||||||
| Absolute Contr. |
% Contr. |
|||||||||||||
| Age-appropriate feeding | −0.016 | 0.094 | −0.002 | 1% | −0.027 | 0.087 | −0.002 | 2% | −0.011 | −0.007 | 0.000 | −0.001 | −0.001 | −1% |
| Full immunization | −0.043 | 0.132 | −0.006 | 3% | −0.031 | 0.081 | −0.003 | 3% | 0.012 | −0.051 | 0.002 | 0.001 | 0.003 | 4% |
| 4 + ANC | −0.008 | 0.168 | −0.001 | 1% | −0.015 | 0.066 | −0.001 | 1% | −0.007 | −0.102 | 0.001 | 0.000 | 0.000 | 0% |
| Institutional delivery | −0.042 | 0.450 | −0.019 | 11% | −0.021 | 0.242 | −0.005 | 5% | 0.021 | −0.208 | 0.009 | 0.005 | 0.014 | 19% |
| Posyandu participation | 0.015 | 0.099 | 0.001 | −1% | −0.012 | 0.094 | −0.001 | 1% | −0.026 | −0.005 | 0.000 | −0.002 | −0.003 | −3% |
| Safe drinking water | −0.066 | 0.118 | −0.008 | 5% | −0.014 | 0.104 | −0.001 | 1% | 0.053 | −0.013 | 0.001 | 0.006 | 0.006 | 9% |
| Improved sanitation | −0.015 | 0.463 | −0.007 | 4% | −0.036 | 0.328 | −0.012 | 12% | −0.021 | −0.135 | 0.002 | −0.007 | −0.005 | −7% |
| Clean environment | −0.075 | 0.078 | −0.006 | 3% | −0.027 | 0.104 | −0.003 | 3% | 0.048 | 0.026 | −0.002 | 0.005 | 0.003 | 4% |
| >1 smoker in HH | 0.022 | −0.028 | −0.001 | 0% | 0.041 | −0.041 | −0.002 | 2% | 0.019 | −0.014 | 0.000 | −0.001 | −0.001 | −2% |
| Short birth interval | 0.084 | −0.028 | −0.002 | 1% | 0.119 | −0.016 | −0.001 | 1% | 0.035 | 0.012 | 0.001 | −0.001 | 0.000 | 1% |
| Long birth interval | 0.007 | −0.036 | 0.000 | 0% | 0.057 | −0.046 | 0.000 | 0% | 0.049 | −0.011 | 0.000 | −0.002 | −0.002 | −3% |
| Large HH size | 0.006 | −0.036 | 0.000 | 0% | −0.018 | −0.050 | 0.001 | −1% | −0.024 | −0.014 | 0.000 | 0.001 | 0.001 | 2% |
| Middle third | −0.054 | 0.034 | −0.002 | 1% | −0.026 | −0.002 | 0.000 | 0% | 0.027 | −0.036 | 0.002 | 0.000 | 0.002 | 3% |
| Richest third | −0.083 | 0.884 | −0.073 | 43% | −0.007 | 0.901 | −0.005 | 5% | 0.076 | 0.017 | −0.001 | 0.069 | 0.067 | 93% |
| Electricity | −0.020 | 0.101 | −0.002 | 1% | −0.080 | 0.020 | −0.002 | 2% | −0.060 | −0.082 | 0.002 | −0.001 | 0.000 | 1% |
| Mother's education min. JHS | −0.041 | 0.347 | −0.014 | 8% | −0.054 | 0.236 | −0.013 | 13% | −0.013 | −0.112 | 0.005 | −0.003 | 0.002 | 2% |
| Mother's age at birth <20 years | 0.028 | −0.073 | −0.002 | 1% | 0.085 | −0.069 | −0.006 | 6% | 0.056 | 0.004 | 0.000 | −0.004 | −0.004 | −5% |
| Male HH head | 0.020 | −0.012 | 0.000 | 0% | −0.018 | −0.006 | 0.000 | 0% | −0.038 | 0.006 | 0.000 | 0.000 | 0.000 | 0% |
| Male Child | 0.020 | −0.005 | 0.000 | 0% | 0.012 | −0.019 | 0.000 | 0% | −0.008 | −0.014 | 0.000 | 0.000 | 0.000 | 0% |
| Child's age: 6–11 months | 0.004 | −0.009 | 0.000 | 0% | 0.031 | 0.011 | 0.000 | 0% | 0.027 | 0.020 | 0.000 | 0.000 | 0.000 | 1% |
| Child's age: 12–23 months | 0.158 | 0.016 | 0.003 | −1% | 0.239 | −0.002 | −0.001 | 1% | 0.081 | −0.018 | −0.003 | 0.000 | −0.003 | −4% |
| Child's age: ≥24 months | 0.103 | −0.011 | −0.001 | 1% | 0.158 | −0.029 | −0.005 | 5% | 0.056 | −0.018 | −0.002 | −0.002 | −0.003 | −5% |
| Mother short | 0.170 | −0.072 | −0.012 | 7% | 0.229 | −0.066 | −0.015 | 15% | 0.059 | 0.006 | 0.001 | −0.004 | −0.003 | −4% |
| Urban | −0.024 | 0.418 | −0.010 | 6% | −0.035 | 0.346 | −0.012 | 12% | −0.011 | −0.072 | 0.002 | −0.004 | −0.002 | −3% |
| Islanda | −0.001 | 1% | −0.001 | 1% | 0.000 | 0.000 | 0.000 | 0% | ||||||
| Residual | −0.006 | 3% | −0.012 | 12% | −0.001 | −1% | ||||||||
| Total | −0.172 | 100% | −0.099 | 100% | 0.073 | 100% | ||||||||
Total aggregate contribution from all dummy island variables with Java as the reference category.
How did these developments in determinants over time contribute to the observed decline in stunting inequality? From the Oaxaca-like decomposition of change (shown in column “Equation (4)” of Table 4), we derive the total contribution of each determinant from two components: (1) its contribution through the change in its inequality by wealth (EI) weighted by its partial effect () in 2007, and (2) its contribution from the change in coefficients weighted by its inequality (EI) in 2014.
In general, household wealth and institutional delivery stand out as the two most important drivers of the reduction of stunting inequality. Household wealth contributes to +93% of the change and this derives mostly from the smaller regression coefficient (which dropped from -0.083 to -0.007). This suggests that stunting differences between children in the richest third relative to the poorest third were much smaller in 2014 than in 2007. Meanwhile, the contribution of institutional delivery (19%) mainly results from its lower inequality in the second period ( fell from 0.450 to 0.242). Full immunization, safe drinking water source, and clean household environment also show positive contributions of 4%, 9%, and 4% respectively. The share of full immunization is mostly due to its more equal distribution in 2007 while the other factor contribution changes mainly stem from their lower partial effects. We also observe a considerable inequality reduction in maternal education and antenatal care, but that effect is neutralized by their larger coefficients (in absolute terms) in the second period.
On the other hand, there are no major negative contributors to the fall of stunting inequality. By far the largest share comes from child's age (-8%), improved sanitation (-7%) and maternal age at birth (-5%). The contribution of older children and younger maternal age at birth is explained by its greater ‘harmful effect’ in the second period – since its inequality did not change substantially. As for improved household sanitation, the fall in its inequality did not translate into lower stunting inequality because its ‘protective effect’ against stunting also grew (from -0.015 to -0.036). Other environmental factors such as the presence of smokers in the household, a clean household environment, and safe drinking water all show positive contributions to the inequality reduction, mostly due to their smaller association with stunting in 2014.
Discussion
Our analysis has led to a number of relevant findings with respect to changes in the unequal distribution of childhood stunting in Indonesia. First, both the prevalence of under-five stunting and severe stunting declined between 2007 and 2014. However, this drop was modest, and only statistically significant for severe stunting. The mean level of stunting is still considered (too) high and the reductions were small compared to the drops observed in similar periods in neighboring countries such as Cambodia (from 41.6% to 33.9% in 2005–2014) and Vietnam (from 36.7% to 22.7% in 2000–2011) (Kien et al., 2016; Zanello, Srinivasan, & Shankar, 2016). Secondly, we find that the presence of under-five stunting in Indonesia is more concentrated in poorer households. However, we also observe a significant decline in its inequality by wealth over the seven years period, suggesting that more of the stunting reduction occurred in poorer households. This observation contrasts with recent findings for Vietnam (Kien et al., 2016) and Bangladesh (Huda et al., 2017): in both countries stunting inequality by wealth increased. In other words, in these countries, the (greater) improvements in stunting primarily benefited the better-off households.
Third, our findings on the determinants of stunting are generally consistent with earlier evidence for Indonesia as reviewed by Beal et al. (2018, pp. 1–10). What our study adds to those is the potential risk of the presence of human and animal faeces around the residence as indicated by the clean household environment variable – apart from the adequacy of sanitation. This finding squares with results by Headey et al. (2017) and Penakalapati et al. (2017) who also document the association, particularly for animal faeces, with child health and nutritional status, possibly via its role in transmitting infectious diseases.
Fourth, regarding the contributing factors to the inequality reduction, our decomposition analysis suggests that household wealth plays the most important role. This was almost entirely due to the reduction in its partial association with stunting, and not to a reduction in wealth inequality, implying that the poor kids were relatively less likely to be stunted in the second period. But how can this be explained? One explanation might be that in the 2005 to 2015 period, Indonesia experienced quite a steady economic improvement with 5% average annual GDP growth, a significant decline in poverty rate from 19.1% to 11.2%. The substantial widening of the income gap over this period suggested by the growing Gini index from 0.36 to 0.41 estimated on National Socioeconomic Surveys (OECD Economic, 2016) is not confirmed in our analysis: the Gini estimate for the IFLS households included in this study fell from 0.353 in 2007 to 0.327 in 2014. Thus, living standards in general have improved and, at least in the IFLS sample, also the poorest households benefited from this growth. This can also be seen from the beneficial contributions of safer drinking water and cleaner environments (though not in improved sanitation).
Fifth, apart from household wealth and living standards, and more importantly from a health policy point of view, some proxy measures of health care access show some improvement. Various measures of health services use (like immunization rates) have improved but, perhaps surprisingly, the most significant contributor was delivery of births in health facilities. By 2014, birth deliveries in a facility have become less of a privilege of the richer households than in 2007. Research from Bangladesh (Heady et al., 2014) and Nepal (Headey & Hoddinott, 2015) also found that being born in hospital or in a health facility was significantly negatively associated with stunting. While the mechanism for such an effect maybe unclear, one possible explanation is that it might be a proxy for closeness to health care service in general and that it raises the exposure of mothers to professional health care providers, leading to better child health and nutrition awareness. Our finding that the level and distribution of maternal and child care were getting better is supported by a study on the trends in maternal health care utilization from 1986 to 2012 based on the Indonesian DHS (Demographic and Health Survey) data (Nababan et al., 2018). This trend is possibly related to the expansion of national health insurance for the poor program (Jamkesmas) since 2008 (previously named Askeskin). Several studies have documented a positive association of Jamkesmas with the use of antenatal care, skilled birth attendance, and delivery in a health facility in Indonesia (Brooks et al., 2017; Wang, Temsah, & Mallick, 2017). Another specific scheme for maternal care – known as Jampersal – was implemented for a brief period (2011–2013), but its impact was considered limited (Achadi et al., 2014).
Since 2007, Indonesia also started a Conditional Cash Transfer (CCT) scheme –– the Family Hope Program (Program Keluarga Harapan, PKH) for poor households and Generasi for communities. It was steadily expanded to reach more than 10 million households in 2018 (Cahyadi et al., 2018). Health indicators that were included as a conditionality for this program are 4 ANC visits, taking iron tablets during pregnancy, professionally-assisted birth, two postnatal visits, complete childhood immunization, adequate monthly weight increases for infants, vitamin A supplementation twice a year for under-five children, and routine weighing (Kusuma, McConnell, Berman, & Cohen, 2017). After 6 years of implementation, it was found that PKH had significantly reduced the stunting and severe stunting level among children aged 0–60 months (Cahyadi et al., 2018). Lastly, Indonesia also started to adopt the multisectoral framework of Scaling Up Nutrition (SUN) in 2012 in the form of a national movement of the first thousand days of life (Gerakan 1000 Hari Pertama Kehiduoan). This program mainly aims to improve the coordination between stakeholders to ensure the sufficiency of nutritional needs of mothers and children (Bappenas, 2012). While we cannot in our seven-year change study attribute any of the observed changes specifically to any of these programs, it does seem likely that at least some of these have helped to improve the distribution of maternal and child health services in the relevant period.
Limitations of the study
As the IFLS sample is representative of only about 83% of Indonesian population (excluding some eastern provinces), the generalizability of its findings is somewhat limited. Second, the use of the wealth index as a measure of socioeconomic status is sometimes questioned. However, we argue that its use for ranking households and individuals by wealth is defendable for a long term outcome like stunting, for which other socioeconomic indicators like income or consumption suffer from obvious disadvantages like seasonality, underreporting, etc (Houweling et al., 2003; O’Donnell, Van Doorslaer, Wagstaff, & Lindelow, 2008). Finally, a regression-based decomposition analysis as used in this study is limited by its inability to establish causal links for all required effects of determinants. As such, it mainly presents a sophisticated way of describing the main interactions between presumed determinants of an outcome and their unequal distributions.
Conclusion
While Indonesia's overall improvement in stunting levels was modest in the recent decade, the stunting distribution by wealth became somewhat less unequal. Our study suggests that, apart from general improvements in both the level and distribution of wealth, it may also have resulted from targeted efforts at improving the access of poorer mothers and children to effective health services. The hope is that the combination of these programs in the recent rollout of Jaminan Kesehatan Nasional (JKN) since 2014 will continue to improve the accessibility of essential mother and child health services to the poorer sections of the Indonesian population.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgements
The authors acknowledge the financial support of The Netherlands Initiative for Capacity development in Higher Education (NICHE) NUFFIC for a project subsidy on “Strengthening Capacity in Health Insurance and Finance for Universal Health Coverage in Indonesia” (NUFFIC project nr NICHE/IDN/226: CF 9900). They also thank to Adelia Ulya Rachman for her input during the analysis and Novat Pugo Sambodo for his help with IFLS datasets.
Footnotes
Shorr measuring boards Model 420 was used for the measurement of child's length/height, and Seca Model 770 scales (SECA, Los Angeles, CA, USA) was used for measuring the weight.
We also performed the same decomposition for non-severe stunting measure. The results in terms of relative contributions of determinants were very similar to those for severe stunting (results available in supplementary material).
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2019.100469.
Contributor Information
Muhammad Fikru Rizal, Email: m.fikru.rizal@mail.ugm.ac.id.
Eddy van Doorslaer, Email: vandoorslaer@eshpm.eur.nl.
Appendix A. Operational Definition of Variables
| Variable | Variable Type | Definition |
|---|---|---|
| Outcome | ||
| HAZ Score | Continuous | Child height/length-for-age z-score, compared to WHO reference population. |
| Stunting | Binary | 1 if child's HAZ score less than -2 SD from the reference population median. |
| Severe Stunting | Binary | 1 if child's HAZ score less than -3 SD from the reference population median. |
| Underlying Determinants | ||
| Feeding Practice | ||
| Age-appropriate feeding | Binary | 1 if children aged 0–5 months are exclusively breastfeed; or if children aged 6–23 months still on breastfeeding and got minimum 4 types of foods in past day before the interview with minimum frequency of 2 times a day; or if children aged ≥24 months, they have already stoppedbreastfeeding, got minimum 4 types of foods in the past day before the interview with minimum frequency of 3 times a day. |
| Health care services | ||
| Full immunization | Binary | 1 if children aged ≥12 months already got minimum number of vaccination (1 measles, 1 BCG, 3 DPT, 3 Polio, and 3 Hepatitis B); children aged 0–11 months coded as 0 to keep them in the sample. |
| 4 + ANC | Binary | 1 if during the pregnancy mother received at least 4 times of antenatal care. |
| Institutional delivery | Binary | 1 if a child was born in any healthcare facility. |
| Posyandu participation | Binary | 1 if a child ever participated in Posyandu (a) community program for child's growth monitoring) in past 4 weeks before the interview. |
| Healthy environment | ||
| Safe drinking water | Binary | 1 if household using boiled water from bottled water or either pipe water, well water, spring water, or rain water (WHO/UNICEF, 2006). |
| Improved sanitation | Binary | 1 if household had private toilet with septic tank (WHO/UNICEF, 2006). |
| Clean HH environment | Binary | 1 if interviewer did not observe any human or animal feces around the house where the child lived. |
| >1 smoker in Household | Binary | 1 if there was more than 1 smoker in the household |
| Intrahousehold food competition | ||
| Birth order and interval | Categorical | Categorized as: (1) “first-borns”, (2) “Short birth interval” for subsequent children with less than 24 months of birth interval with their older siblings, and (3) “Long birth interval” if the birth interval is more than or equal to 24 months. |
| Large Household size | Binary | 1 if household consisted of more than 4 members. |
| Non-modifiable factors | ||
| Male Child | Binary | 1 if a child is male |
| Child's age | Categorical | Child's age when interviewed, coded as 1 for children aged 0–5 months, 2 for 6–11 months, 3 for 12–23 months, and 4 for ≥24 months. |
| Mother's short stature | Binary | 1 if mother's height is less than 145 cm |
| Basic determinants | ||
| Household and parental factors | ||
| Household Wealth | Categorical | Tertile of wealth index, grouped at household level observation. Coded as 1 for “Poorest third”, 2 for “Middle third”, and 3 for “Richest third”. |
| Electricity | Binary | 1 if household had any access to electricity |
| Mother's education: Min. Junior High Schl. | Binary | 1 if child's mother had minimum of Junior High School Degree |
| Mother's age at birth: <20 years | Binary | 1 if child's mother was a teenager (aged <20 years old) when giving birth. Mother's age at birth was calculated from the date of birth of the mother subtracted by the date of birth of the child. |
| Male HH head | Binary | 1 if the gender of household head was male. |
| Regional factors | ||
| Urban | Binary | 1 if a child lived in urban area |
| Island | Categorical | Dummy variable for island where the child lived namely: Sumatra, Java, Kalimantan, Bali and Nusa Tenggara, and Sulawesi |
Appendix B. Supplementary data
The following is the Supplementary data to this article:
References
- Achadi E.L., Achadi A., Pambudi E., Marzoeki P. A Study on the Implementation of jampersal Policy in Indonesia (health, nutrition, and population discussion paper) 2014. https://openknowledge.worldbank.org/handle/10986/20740 Washington, DC. Retrieved from.
- Alderman H., Headey D.D. How important is parental education for child nutrition? World Development. 2017;94:448–464. doi: 10.1016/j.worlddev.2017.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali Naser I., Jalil R., Wan Muda W.M., Wan Nik W.S., Mohd Shariff Z., Abdullah M.R. Association between household food insecurity and nutritional outcomes among children in Northeastern of peninsular Malaysia. Nutrition Research and Practice. 2014;8(3):304–311. doi: 10.4162/nrp.2014.8.3.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bappenas . 2012. Pedoman perencanaan program gerakan 1000 Hari Pertama kehidupan (guideline of program planning on the first 1000 Days of life movement) (Jakarta) [Google Scholar]
- Beal T., Tumilowicz A., Sutrisna A., Izwardy D., Neufeld L.M. 2018. A review of child stunting determinants in Indonesia, Maternal and Child Nutrition. October 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Best C.M., Sun K., De Pee S., Sari M., Bloem M.W., Semba R.D. Paternal smoking and increased risk of child malnutrition among families in rural Indonesia. Tobacco Control. 2008;17(1):38–45. doi: 10.1136/tc.2007.020875. [DOI] [PubMed] [Google Scholar]
- Brooks M.I., Thabrany H., Fox M.P., Wirtz V.J., Feeley F.G., Sabin L.L. Health facility and skilled birth deliveries among poor women with Jamkesmas health insurance in Indonesia : A mixed- methods study. BMC Health Services Research. 2017;17(105):1–12. doi: 10.1186/s12913-017-2028-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cahyadi N., Hanna R., Olken B.A., Prima R.A., Satriawan E., Syamsulhakim E. 2018. Cumulative Impacts of conditional Cash transfer programs: Experimental Evidence from Indonesia (No. 24670)http://www.nber.org/papers/w24670 Cambridge, MA. Retrieved from. [Google Scholar]
- Campbell R.K., Aguayo V., Kang Y., Dzed L., Joshi V., Waid J. Infant and young child feeding practices and nutritional status in Bhutan. Maternal and Child Nutrition. 2017;(May) doi: 10.1111/mcn.12580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaparro C., Oot L., Sethuraman K. Overview of the nutrition situation in seven countries in Southeast Asia. 2014. https://www.fantaproject.org/sites/default/files/download/Southeast-Asia-Nutrition-Overview-Apr2014.pdf Washington, DC. Retrieved from.
- De Silva I., Sumarto S. Child malnutrition in Indonesia: Can education, sanitation and healthcare augment the role of income? Journal of International Development. 2018;30(5):837–864. doi: 10.1002/jid.3365. [DOI] [Google Scholar]
- Erreygers G. Correcting the concentration index. Journal of Health Economics. 2009;28(2):504–515. doi: 10.1016/j.jhealeco.2008.02.003. [DOI] [PubMed] [Google Scholar]
- Filmer D., Pritchett L.H. Estimating wealth effects without expenditure data - or tears. Demography. 2001;38(1):115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- Frankenberg E., Karoly L., Gertler P., Peterson C., Wesley D. California; 1995. The 1993 Indonesian family life survey: Overview and field report. [Google Scholar]
- Hangoma P., Aakvik A., Robberstad B. Vols. 1–21. 2017. (Explaining changes in child health inequality in the run up to the 2015 Millennium Development Goals (MDGs): The case of Zambia). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harimurti P., Pambudi E., Pigazzini A., Tandon A. 2013. The nuts & bolts of Jamkesmas Indonesia ’ s government- financed health coverage program (UNICO studies series No. 8) (Washington, DC) [Google Scholar]
- Headey D.D., Hoddinott J. Understanding the rapid reduction of undernutrition in Nepal, 2001-2011. PLoS One. 2015;10(12):2001–2011. doi: 10.1371/journal.pone.0145738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Headey D., Hoddinott J., Ali D., Tesfaye R., Dereje M. The other asian enigma: Explaining the rapid reduction of undernutrition in Bangladesh. World Development. 2014;66:749–761. doi: 10.1016/j.worlddev.2014.09.022. [DOI] [Google Scholar]
- Headey D., Nguyen P., Kim S., Rawat R., Ruel M., Menon P. Is exposure to animal feces harmful to child nutrition and health Outcomes ? A multicountry observational analysis. The American Journal of Tropical Medicine and Hygiene. 2017;96(4):961–969. doi: 10.4269/ajtmh.16-0270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houweling T.A.J., Kunst A.E., Mackenbach J.P. Measuring health inequality among children in developing countries : Does the choice of the indicator of economic status matter ? International Journal for Equity in Health. 2003;12:1–12. doi: 10.1186/1475-9276-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huda T.M., Hayes A., Dibley M.J. Social determinants of inequalities in child undernutrition in Bangladesh : A decomposition analysis. Maternal and Child Nutrition. 2017:1–12. doi: 10.1111/mcn.12440. August 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kien V.D., Lee H.Y., Nam Y.S., Oh J., Giang K.B., Van Minh H. Trends in socioeconomic inequalities in child malnutrition in Vietnam: Findings from the multiple indicator cluster surveys, 2000-2011. Global Health Action. 2016;9(1):1–9. doi: 10.3402/gha.v9.29263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kjellsson G., Gerdtham U.G. On correcting the concentration index for binary variables. Journal of Health Economics. 2013;32(3):659–670. doi: 10.1016/j.jhealeco.2012.10.012. [DOI] [PubMed] [Google Scholar]
- Kusuma D., McConnell M., Berman P., Cohen J. The impact of household and community cash transfers on children's food consumption in Indonesia. Preventive Medicine. 2017;100:152–158. doi: 10.1016/j.ypmed.2017.04.020. [DOI] [PubMed] [Google Scholar]
- Mani S. Socioeconomic determinants of child Health : Empirical evidence from Indonesia. Journal of the East Asian Economic Association. 2014;28(1):81–104. [Google Scholar]
- Mboi N. Indonesia: On the way to universal health care. Health Systems & Reform. 2015;1(2):91–97. doi: 10.1080/23288604.2015.1020642. [DOI] [PubMed] [Google Scholar]
- Nababan H.Y., Hasan M., Marthias T., Dhital R., Rahman A., Anwar I. Trends and inequities in use of maternal health care services in Indonesia, 1986 – 2012. International Journal of Women's Health. 2018;10:11–24. doi: 10.2147/IJWH.S144828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIHRD . 2013. Riset kesehatan dasar (basic health Research) 2013. (Jakarta) [Google Scholar]
- OECD Economic OECD economic surveys Indonesia. 2016. [DOI]
- Olken B.A., Onishi J., Wong S. Should aid reward performance? Evidence from a field experiment on health and education in Indonesia. American Economic Journal: Applied Economics. 2014;6(4):1–34. doi: 10.1257/app.6.4.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onah S., Osuorah D.I.C., Ebenebe J., Ezechukwu C., Ekwochi U., Ndukwu I. Infant feeding practices and maternal socio-demographic factors that influence practice of exclusive breastfeeding among mothers in nnewi south-east Nigeria: A cross-sectional and analytical study. International Breastfeeding Journal. 2014;9(1):1–10. doi: 10.1186/1746-4358-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Onis M. Assessment of differences in linear growth among populations in the WHO Multicentre Growth Reference Study. Acta Paediatrica. 2007;95(782034067):56–65. doi: 10.1111/j.1651-2227.2006.tb02376.x. [DOI] [PubMed] [Google Scholar]
- de Onis M., Branca F. Childhood stunting: A global perspective. Maternal and Child Nutrition. 2016;12:12–26. doi: 10.1111/mcn.12231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Onis M., Dewey K.G., Borghi E., Onyango A.W., Blössner M., Daelmans B. The world health organization's global target for reducing childhood stunting by 2025: Rationale and proposed actions. Maternal and Child Nutrition. 2013;9(S2):6–26. doi: 10.1111/mcn.12075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Donnell O., O'Neill S., Van Ourti T., Walsh B. conindex: Estimation of concentration indices. STATA Journal. 2016;16(1):112–138. doi: 10.1177/1536867x1601600112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Donnell O., Van Doorslaer E., Wagstaff A., Lindelow M. Washington. WBI Learning Resource Series; Washington, DC: 2008. Analyzing health equity using household survey data. The World Bank. [DOI] [Google Scholar]
- Penakalapati G., Swarthout J., Delahoy M.J., Wodnik B., Levy K., Freeman M.C. Exposure to animal feces and human health : A systematic review and proposed research priorities exposure to animal feces and human health : A systematic review and proposed research priorities. Environmental Science and Technology. 2017;51(20):11537–11552. doi: 10.1021/acs.est.7b02811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rachmi C.N., Agho K.E., Li M., Baur L.A. Stunting, underweight and overweight in children aged 2.0-4.9 years in Indonesia: Prevalence trends and associated risk factors. PLoS One. 2016;11(5):1–17. doi: 10.1371/journal.pone.0154756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinhardt K., Fanzo J. Addressing chronic malnutrition through multi-sectoral, sustainable approaches: A review of causes and consequences. Frontiers in Nutrition. 2014;1(August):120–121. doi: 10.1159/000441823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha B., Taneja S., Chowdhury R., Mazumder S., Rongsen-Chandola T., Upadhyay R.P. Low-birthweight infants born to short-stature mothers are at additional risk of stunting and poor growth velocity: Evidence from secondary data analyses. Maternal and Child Nutrition. 2018;14(1):1–9. doi: 10.1111/mcn.12504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith L.C., Haddad L. Reducing child undernutrition: Past drivers and priorities for the post-MDG era. World Development. 2015;68(1):180–204. doi: 10.1016/j.worlddev.2014.11.014. [DOI] [Google Scholar]
- Strauss J., Beegle K., Sikoki B., Wattie A.M. The fourth wave of the Indonesia family life survey (IFLS4) 2009. [DOI]
- Strauss J., Witoelar F., Sikoki B. The fifth wave of the Indonesia family life survey (IFLS5): Overview and field report. 2016. [DOI]
- The World Bank . Vol. 2. 2017. Operationalizing a multi-sectoral approach for the reduction of stunting in Indonesia.http://documents.worldbank.org/curated/en/580081492008988764/an-application-using-the-2007-and-2013-Riskesdas ( : An application using the 2007 and 2013 riskesdas (English)). Washington, DC. Retrieved from. [Google Scholar]
- Torlesse H., Cronin A.A., Sebayang S.K., Nandy R. Determinants of stunting in Indonesian children: Evidence from a cross-sectional survey indicate a prominent role for the water, sanitation and hygiene sector in stunting reduction. BMC Public Health. 2016;16(1):1–11. doi: 10.1186/s12889-016-3339-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF . 1990. Strategy for improved Nutrition of Children in developing countries (UNICEF policy review paper) (New York.) [Google Scholar]
- Van Doorslaer E., Van Ourti T. Measuring inequality and inequity in health and health care. In: Glied S., Smith P.C., editors. The oxford handbook of health economics. Oxford University Press; 2011. pp. 837–869. [DOI] [Google Scholar]
- Victora C.G., de Onis M., Hallal P.C., Blossner M., Shrimpton R. Worldwide timing of growth faltering: Revisiting implications for interventions. Pediatrics. 2010;125(3):e473–e480. doi: 10.1542/peds.2009-1519. [DOI] [PubMed] [Google Scholar]
- Wagstaff A., Van Doorslaer E., Watanabe N. On decomposing the causes of health sector inequalities with an application to malnutrition inequalities in Vietnam. Journal of Econometrics. 2003;112(1):207–223. doi: 10.1016/S0304-4076(02)00161-6. [DOI] [Google Scholar]
- Wang W., Temsah G., Mallick L. Indonesia and Rwanda; 2017. The impact of health insurance on maternal health care utilization : Evidence from Ghana. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . WHO; Geneva: 2006. WHO Anthro 2005, Beta version Feb 17th, 2006: Software for assessing growth and development of the world's children.http://www.who.int/childgrowth/software/en/ Retrieved from. [Google Scholar]
- WHO . Infant and young child feeding: Model chapter for textbooks for medical students and allied health professionals. World Health Organization; Geneva: 2009. ANNEX 4, Indicators for assessing infant and young child feeding practices; pp. 1–99. [DOI] [PubMed] [Google Scholar]
- WHO/UNICEF . Vol. 25. World Health Organization; 2006. (Core questions on drinking-water). [Google Scholar]
- Zanello G., Srinivasan C.S., Shankar B. What explains Cambodia's success in reducing child stunting-2000-2014? PLoS One. 2016;11(9):1–21. doi: 10.1371/journal.pone.0162668. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.