Abstract
Electroencephalographic neurofeedback (EEG-NFB) represents a broadly used method that involves a real-time EEG signal measurement, immediate data processing with the extraction of the parameter(s) of interest, and feedback to the individual in a real-time. Using such a feedback loop, the individual may gain better control over the neurophysiological parameters, by inducing changes in brain functioning and, consequently, behavior. It is used as a complementary treatment for a variety of neuropsychological disorders and improvement of cognitive capabilities, creativity or relaxation in healthy subjects. In this review, various types of EEG-NFB training are described, including training of slow cortical potentials (SCPs) and frequency and coherence training, with their main results and potential limitations. Furthermore, some general concerns about EEG-NFB methodology are presented, which still need to be addressed by the NFB community. Due to the heterogeneity of research designs in EEG-NFB protocols, clear conclusions on the effectiveness of this method are difficult to draw. Despite that, there seems to be a well-defined path for the EEG-NFB research in the future, opening up possibilities for improvement.
Keywords: Biofeedback, electroencephalography, frequency neurofeedback training, coherence training, slow cortical potential training
INTRODUCTION
The first attempts of electroencephalographic neurofeedback (EEG-NFB) implementation began in the 1960s. Initially, the method was called EEG biofeedback, but now the term biofeedback represents an umbrella term for all the methods that enable an individual to train physiological activity to improve health and performance. Aside from neurophysiological processes, self-regulation of muscle tone, skin conductance, heart rate, pain perception, and others can be trained, using the appropriate instrument and a real-time feedback loop protocol. EEG-NFB was the first biofeedback method, and it rapidly received much attention due to its potential therapeutic capabilities [1, 2]. However, after this initial enthusiasm, EEG-NFB experienced a period of decline of interest in the 1980s, as it did not meet the expectations [3]. From then on, the technology has been improving, causing the revival of the method in the new millennium. Today, the method is implemented in many private clinical practices around the world [4].
The main purpose of the EEG-NFB, particularly in the clinical environment, is for the individual to learn self-regulation of the neurophysiological parameter(s) with the most substantial deviation from the rest of the population. It is based on the causality hypothesis which proposes that the deviations in the brain functioning cause behavioral symptoms of the neuropsychological disorders. The subject is taught how to enhance or inhibit specific, atypical electrophysiological parameter(s) through operant conditioning, i.e., the learning process in which the strength of behavior is modified using immediate feedback and positive reinforcement [4-7].
It works as a feedback loop (Figure 1), starting with the subject’s EEG data acquisition, which, in private practice, is usually done using 1- or 2-channel system, while in a research setting 32 or more channel system is used. Afterward, the acquired EEG signal is analyzed either offline or in real-time (Z-score online training [8]) to extract the parameter of interest. Most often the frequency of the brainwaves in a specific brain area is being modulated, but other possible parameters will be discussed in the proceeding section. Next, the activity of a chosen parameter is presented back to the subject in the form of a visual, auditory, or tactile stimulus, or a combination thereof, which assists the subject to control the parameter(s). Typical examples would be a video game, where the speed of the car is controlled by the brain activity or a bar showing the raw activity of the parameter(s), alongside a threshold, which the subject aims to achieve. When the threshold is reached, additional feedback (e.g., a pleasant tone) or a reward can be given to the subject, reinforcing a desired mental state [9-12]. For a detailed description of the neurofeedback protocol, readers are referred to the review article by Enriquez-Geppert, Huster, and Herrmann [6].
Figure 1.
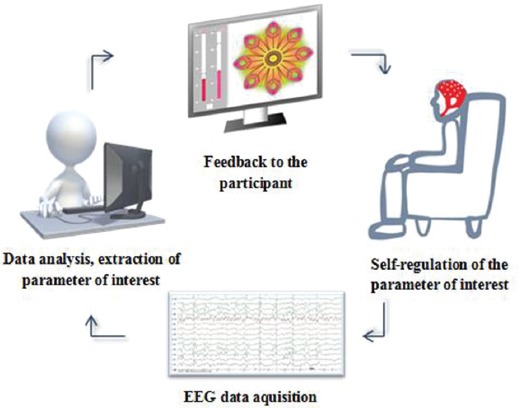
A diagram presenting the neurofeedback training loop.
This review aims to give an overview of the current status of the EEG-NFB by introducing its common types, the problems that it faces and possible future perspective.
TYPES OF EEG-NFB TRAINING
This paragraph briefly summarizes the most commonly used EEG-NFB types and their clinical applications and effectiveness. Three major EEG-NFB protocols are widely used to modulate different electrophysiological parameters. Firstly, the training of slow cortical potentials (SCPs) aims to modulate specific event-related potentials called slow cortical potentials. These potentials may be negative (e.g., contingent negative variation, CNV) or positive, reflecting the level of local cortical arousal and attention [13]. The purpose of such training is to improve the self-regulating capabilities of SCP, which consequently increases the ability to regulate cortical excitability to some extent. It has been used mainly for people with attention deficit hyperactivity disorder (ADHD) to increase cortical negativity and subsequently improve their attentional abilities [14, 15]. Also, it may be used for patients with epilepsy, targeting a decrease of cortical negativity power, hence increasing their threshold level for a seizure [13].
The second type of EEG-NFB training is called coherence training, which aims to change the connectivity patterns among brain areas. Coherence, in our context, represents the degree of correlation between two or more brain regions, based on the similarities in phase, amplitude, and frequency of the brainwaves in time. [16, 17]. Distorted connectivity has been shown in various neurologic disorders compared to healthy controls [18]. EEG-NFB protocol has been tested in children with dyslexia [19], autistic spectrum disorder [20, 21], patients with epilepsy [22], traumatic brain injury [23], brain stroke [24], and healthy individuals [25].
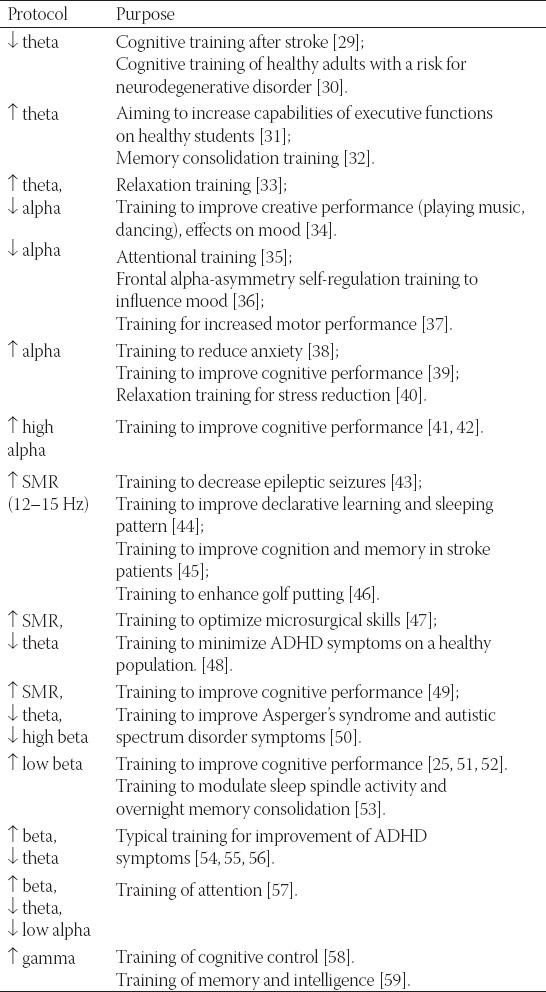
The third and by far most commonly used training is the frequency training, which aims to change the power ratio of the EEG frequency bands, classically divided into delta (< 4 Hz), theta (4–8 Hz), alpha (8–13 Hz), beta (14–30 Hz) and gamma (> 40 Hz) [26]. The rationale for this type of training is the proposed association between the amplitudes of specific frequencies and corresponding cognitive functions (frequency-to-function mapping) [27].
The most often used frequency training today are EEG theta/beta ratio NFB training used for ADHD and enhancement of the sensorimotor (SMR)frequency (12–15 Hz), which is mostly used for ADHD and autistic spectrum disorder [28]. Table 1 summarizes the already used protocols with references for further information. The intention is not to show the effectiveness of the listed studied methods but rather the variety of different protocols that have been used up to date. As further described at the end of the review, the results vary between studies.
TABLE 1.
An overview of already used protocols of frequency EEG NFB training with the references to exemplary studies and their main therapeutical purpose
EFFECTIVENESS OF EEG-NFB
The assumption that the cause of neuropsychological disorders lays in the dysfunction of the nervous system receives increasing support, especially due to EEG connectivity and fMRI resting-state studies [60-62]. The idea that EEG-NFB therapy can change disorder-specific electrophysiological activity has already been tested in many neurologic disorders, such as ADHD, [63-66], epilepsy [67], autistic spectrum disorder [68], traumatic brain injury [5], post-stroke treatment [29], depression and anxiety disorders [69]. Some studies have also researched the therapeutic effects on sleep disorders [70], chronic pain [71], learning difficulties [19, 72], different neurodevelopmental challenges in children [73], addiction [74], schizophrenia [75-77], migraine, and others [78, 79, 80].
The usage of and the research in the field of EEG-NFB have extended further to the healthy population, such as in cases of training memory capabilities [32, 42, 74, 81], attention, and other cognitive capabilities in young adults [42, 81-83] or in elderly population [30]. Moreover, the method has been used to improve performance training in athletes [46], improve creativity [84], or optimize microsurgical skills [47].
Despite a large body of research literature and a wide diversity of treatment possibilities, many studies on EEG-NFB either do not show effective outcome or have many limitations, such as a small number of subjects, small set of training sessions, non-blinded or non-randomized design of the study. As such, despite the positive outcomes, these studies do not allow the conclusion on the effectiveness of the method. Opinions in recent review articles [64, 65, 85] and meta-analyses [78] are similar. In a recent article by Begemann et al. [78] effectiveness of EEG-NFB treatment could not be confirmed for any of the neuropsychological disorders. For some of them, specifically schizophrenia, Tourette’s syndrome, anorexia, anxiety disorders, bipolar disorder and addiction, a lack of methodologically robust studies prevented the analysis of the method’s effectiveness. Other mentioned review articles have a somewhat more optimistic view of the future of the method, but similar conclusions.
CRITIQUES AND METHODOLOGICAL ISSUES OF THE EEG-NFB
EEG-NFB receives many critiques from the science community, which raises questions on the validity of its therapeutic effect. Although there have been numerous EEG-NFB experiments conducted, the authors of reviews or meta-analyses reject many papers due to methodological problems. Rogala et al. have included only 28 out of 84 papers when conducting their review on EEG-NFB effects in a healthy population [11]. Tan et al. used only 10 out of 63 available studies in their review of the literature on EEG-NFB effects in epilepsy, [67]. Begemann et al. have reviewed 169 research papers but used only 30 of them in reviewing the effects of EEG-NFB treatment in psychiatric disorders [78].
Nevertheless, Schoenberg and David excluded only 10 out of 76 articles on this topic [65]. Baydala and Wikman considered invalid all the EEG-NFB studies, except one, that had been researching the effects of the treatment on ADHD, in the period between 1966 and 2000 [86]. One important reason seems to be the poor description of EEG-NFB protocols, which is frequently seen in the older research papers. Vernon et al. [12] conclude their review paper with the statement that in EEG-NFB studies the effect of the placebo or other non-specific factors cannot be excluded. Similar conclusions appear in other papers as well [3, 7, 63, 87].
The lack of standardized protocols is the further issue in the field of EEG-NFB research and therapy. Parameters used in training are often chosen individually by a therapist or a researcher by their reasoning, sometimes without real foundations in the EEG-NFB scientific literature. Dempster [88] and Holtmann with colleagues [87] have stated that studies vary to the extent that it prevents them from being comparable in meta-analyses. There are still open questions on determining specific protocols for specific conditions; this variability may be seen in Table 1. Also, the number and placement of the electrodes need to be defined, as well as the modality and timing of the feedback information, the type of reward, the duration of each session, and the number of sessions in the whole therapy [10-12, 88]. Recently, step-by- step guidelines for performing EEG-NFB training were published in a review article by Enriquez-Geppert et al. [31], yet, many variables remained undetermined.
Nevertheless, the technical issues described above present a minor barrier, considering that protocol optimization and careful description of methodology have significantly improved over the years. The biggest concern remains the validity of EEG-NFB training regarding the regulation of brain activity.
In that context, a transfer problem describes an uncertainty on how the modulation of the brain activity with EEG-NFB causes behavioral changes. Some research shows successful voluntary modulation of brain activity (change in the EEG signal) but no effects in the behavior (e.g., symptom reduction) [33, 53, 59]. On the other hand, there are trials not showing changes in brain activity but demonstrating significant changes in behavior. For instance, Rogala et al. have found that 17 out of 28 studies had only EEG modulation effects, while in 10 out of 20 studies only behavior was affected [11]. They did not find a significant correlation between successful modulation of brain activity and changes in behavior. However, many studies are showing both effects [42, 44, 89, 90, 91]. Many factors may influence these variations in results. Demographic, physiological or psychological factors had not been much investigated [87], but there is some evidence that the feeling of being able to control technological devices affects the performance [92], as makes the choice of mental strategy during training [93].
Furthermore, Paluch et al. have discovered that subjects who train at high-frequencies often learn to control muscle activity instead of brain activity [94]. Since muscle activity can easily disturb the EEG signal, the training can be perceived as successful whereas, in reality, the subject does not modulate brain activity. EEG-NFB studies and therapies controlling for the muscle activity are still scarce, although the authors argue that it is essential to measure the muscle activity.
Another issue, related to the transfer problem, is confusion caused by the use of the term sensorimotor rhythm (SMR). SMR was initially described in cats as the 12–16 Hz rhythm, recorded most prominently at central electrodes, reflecting motor inactivity over the cat’s sensorimotor cortex [95]. The human analog signal, named mu (µ) rhythm, which also increases with motor inactivation, has been shown to be similar in topography and morphology but not in frequency [96]. Human mu rhythm has a lower frequency of 8–12 Hz. Overall, researchers in the field of the classical electrophysiology use the term SMR for some animals, while mu rhythm is used for humans [97].
Interestingly, the researchers in the field of brain-computer interface adopted the term SMR as complex brain activity in human sensory and motor cortices, for which activity is equally dependent on movement and motoric imaginations. It is described as a combination of mu (8–12 Hz) and beta rhythms (18–26 Hz) [98] and, according to some research, also gamma rhythms, [99]. The question then arises, if the purpose of training in the range of 12–15 Hz stays the same as it is postulated or is this another issue that decreases the validity of the method and needs to be resolved.
Furthermore, the problem of generalization tackles the issue of how to generalize the behavioral change, made during the EEG-NFB training, to everyday life. It is known that the environment plays a significant role in learning and that a certain level of learned capabilities cannot be transferred to other settings [7]. In EEG-NFB, this has been attempted to be resolved with additional training without the reward signal during the session, but only at the end. Some therapists give their clients DVDs or associative cards which remind clients of the desired psychophysiological state [7].
The next unresolved issue is the amount of specificity of the EEG-NFB therapies. It raises a question of how much success in the modulation of the brain activity or behavior is due to actual training as opposed to non-specific factors that can significantly contribute to the results [5, 10, 11, 12, 78, 85, 86, 100]. Although there are studies showing effects of EEG-NFB therapies, these are often not blind or double-blind randomized controlled experiments [66]. The fact that the therapy is composed of multiple training sessions, where active attention is involved, is on its own a very important stimulation for participants (or clients), increasing one’s cognitive flexibility and maintenance of attention. Moreover, the setting of the therapy, the state-of-the-art equipment, and the relationship with the therapist are also relevant factors, especially when treating children. Finally, the internal subject’s expectations or placebo effect needs to be mentioned. An interesting study on ADHD was conducted where the non-blinded parents rated the therapy as effective, whereas blinded teachers did not observe any significant differences [64].
Long-term effects of the therapy are another issue that needs to be addressed, as the data concerning this issue are scarce. There have been claims from the private companies that the EEG-NFB training have sustainable effects as soon after ten training sessions. One of the recent randomized controlled studies, in which 10 healthy participants were trained on enhancing the beta level, reported significant changes even three years after the training ended [101]. In a study by Monastra et al. they have done the theta/beta ratio NFB training in children with ADHD. Significant lasting effects in EEG measurement and children’s attention maintenance capabilities were seen on examination after one week. [102]. Also, some other studies have reported long-lasting improvements in ADHD symptoms after six months [55, 89] and two years after the training [103]. Using EEG-NFB for decreasing epileptic seizures has been found to have essential effects one year [104] and ten years after the treatment [105]. Moreover, Lubar also observed positive effects 10 years later [106]. Contrary to this, some studies do not show long-term effects [107, 108]. Finally, mixed results come from the latest review papers [5, 87].
Looking at EEG-NFB training success, it is worth noting that there is always a proportion of people unable to learn how to modulate the brain activity [10, 11, 28]. A similar phenomenon is observed when trying to control different brain-computer interface devices [5]. Studies are estimating that about a third [10] or about a half of participants [28, 41, 89] are the so-called non-responders or non-performers. The reason is not fully explained yet; however, there is a hypothesis that the proportion of non-responders decreases with establishing more personalized protocols [11]. Supposedly, the level of attention, a locus of control, well-being and motivation are also important factors to consider [5].
CONCLUSION AND FUTURE PERSPECTIVE
We discussed several issues related to the EEG-NFB method, that is, according to some research, coming mostly from private companies, considered unquestionably useful in the treatment of some disorders. Our aim was not to argue against the method itself, but rather to highlight the importance of further research to establish an optimal methodology and address the unresolved issues before the advertisement of the method in the private clinical practices.
On the other hand, the direction of the ongoing EEG-NFB research seems to be well-defined [5, 73]. Increased efforts are being made to shift from the classical clinical standard of evaluating the effectiveness of the method, which sees a standardized double-blind, randomized experiment as an optimal approach, to the use of other assessment methods that seem more appropriate for the neuropsychological treatments. In other words, the variability between the subjects and the need for the individual treatment prevent the use of the same protocol for all subjects, although they have been diagnosed with the same neuropsychological disorder. The primary reason for that comes from the contradictions between the positive outcomes of single-case studies and the ineffectiveness of studies with large numbers of subjects [80, 109]. Individualized treatment protocols, where also the effect of the treatment is assessed within the single case, has become more broadly accepted with the launch of the e Research Domain Criteria project (RDoC) in 2008, which is coordinated by the National Institute of Mental Health [62]. This ongoing project proposes a new understanding of mental disorders, which would replace the currently used classification of The Diagnostic and Statistical Manual of Mental Disorders (DSM V), published by the American Psychiatric Association (APA). The major critique of the DSM V is a low validity of the currently used categories for mental disorders since they have not been created by objective physiological measurements but rather behavioral symptoms and questionnaires, of which results are unavoidably subjective and culturally biased.
Similarly, a perceived heterogeneity among disorders leads to the broadening of the categories to new spectrums (autism spectrum disorder, schizophrenia spectrum) and new categories, that try to capture complex features of human neuropsychological disorders. For the above reasons, RDoC aims to understand mental disorders not by classifying people but rather by measuring individual neurophysiological features, finding possible extremes in comparisons with the data from the human population and, based on the assessment, implementing a personalized treatment [62]. Within a paradigm that accepts a research methodology with individually adapted protocols, EEG-NFB effects might show a different trend.
DECLARATION OF INTERESTS
The authors declare no conflict of interests.
REFERENCES
- 1.Budzynski TH. From EEG to neurofeedback. In: Evans JR, Arbarbanel A, editors. Introduction to Quantitative EEG Neurofeedback. 1st ed. San Diego: Academic Press Inc; 1999. pp. 65–79. https://doi.org/10.1016/B978-012243790-8/50004-3. [Google Scholar]
- 2.Kamiya J. The first communications about operant conditioning of the EEG. J Neurother. 2011;15(1):65–73. https://doi.org/10.1080/10874208.2011.545764. [Google Scholar]
- 3.Thibault RT, Lifshitz M, Birbaumer N, Raz A. Neurofeedback, self-regulation, and brain imaging:Clinical science and fad in the service of mental disorders. Psychother Psychosom. 2015;84(4):193–207. doi: 10.1159/000371714. https://doi.org/10.1159/000371714. [DOI] [PubMed] [Google Scholar]
- 4.ISNR|International Society for Neurofeedback and Research. Definition of Neurofeedback. 2010. [[Last accessed on 2017 Mar 20]]. Available from: https://www.isnr.org/neurofeedback-introduction .
- 5.Sitaram R, Ros T, Stoeckel L, Haller S, Scharnowski F, Lewis-Peacock J, et al. Closed-loop brain training:The science of neurofeedback. Nat Rev Neurosci. 2017;18(2):86–100. doi: 10.1038/nrn.2016.164. https://doi.org/10.1038/nrn.2016.164. [DOI] [PubMed] [Google Scholar]
- 6.Enriquez-Geppert S, Huster RJ, Herrmann CS. EEG-neurofeedback as a tool to modulate cognition and behavior:A review tutorial. Front Hum Neurosci. 2017;11:51. doi: 10.3389/fnhum.2017.00051. https://doi.org/10.3389/fnhum.2017.00051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sherlin LH, Arns M, Lubar J, Heinrich H, Kerson C, Strehl U, et al. Neurofeedback and basic learning theory:Implications for research and practice. J Neurother. 2011;15(4):292–304. https://doi.org/10.1080/10874208.2011.623089. [Google Scholar]
- 8.Thatcher RW, Lubar JF. Z Score Neurofeedback:Clinical Applications. San Diego, CA: Academic Press Inc; 2014. [Google Scholar]
- 9.Bagdasaryan J, Quyen Mle V. Experiencing your brain:Neurofeedback as a new bridge between neuroscience and phenomenology. Front Hum Neurosci. 2013;7:680. doi: 10.3389/fnhum.2013.00680. https://doi.org/10.3389/fnhum.2013.00680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gruzelier JH. EEG-neurofeedback for optimising performance. III:A review of methodological and theoretical considerations. Neurosci Biobehav Rev. 2014;44:159–82. doi: 10.1016/j.neubiorev.2014.03.015. https://doi.org/10.1016/j.neubiorev.2014.03.015. [DOI] [PubMed] [Google Scholar]
- 11.Rogala J, Jurewicz K, Paluch K, Kublik E, Cetnarski R, Wróbel A, et al. The do's and don'ts of neurofeedback training:A review of the controlled studies using healthy adults. Front Hum Neurosci. 2016;10:301. doi: 10.3389/fnhum.2016.00301. https://doi.org/10.3389/fnhum.2016.00301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vernon D, Frick A, Gruzelier J. Neurofeedback as a treatment for ADHD:A methodological review with implications for future research. J Neurother. 2004;8(2):53–82. https://doi.org/10.1300/J184v08n02_04. [Google Scholar]
- 13.Birbaumer N. Slow cortical potentials:Plasticity, operant control and behavioral effects. Neuroscientist. 1999;5(2):74–8. https://doi.org/10.1177/107385849900500211. [Google Scholar]
- 14.ISNR|International Society for Neurofeedback and Research. [[Last accessed on 2017 Mar 20]];Definition of Biofeedback. 2008 Available from: https://www.isnr.org/neurofeedback-introduction . [Google Scholar]
- 15.Mayer K, Wyckoff SN, Strehl U. One size fits all?Slow cortical potentials neurofeedback:A review. J Atten Disord. 2013;17(5):393–409. doi: 10.1177/1087054712468053. https://doi.org/10.1177/1087054712468053. [DOI] [PubMed] [Google Scholar]
- 16.Heinrich H, Gevensleben H, Strehl U. Annotation:Neurofeedback-train your brain to train behaviour. J Child Psychol Psychiatry. 2007;48(1):3–16. doi: 10.1111/j.1469-7610.2006.01665.x. https://doi.org/10.1111/j.1469-7610.2006.01665.x. [DOI] [PubMed] [Google Scholar]
- 17.Bowyer SM. Coherence a measure of the brain networks:Past and present. Neuropsychiatr Electrophysiol. 2016;2(1):1. doi:10.1186/s40810-015-0015-7. [Google Scholar]
- 18.Decker SL, Fillmore PT, Roberts AM. Coherence:The measurement and application of brain connectivity. NeuroRegulation. 2017;4(1):3–13. https://doi.org/10.15540/nr.4.1.3. [Google Scholar]
- 19.Breteler MH, Arns M, Peters S, Giepmans I, Verhoeven L. Improvements in spelling after QEEG-based neurofeedback in dyslexia:A randomized controlled treatment study. Appl Psychophysiol Biofeedback. 2010;35(1):5–11. doi: 10.1007/s10484-009-9105-2. https://doi.org/10.1007/s10484-009-9105-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coben R, Padolsky I. Assessment-guided neurofeedback for autistic spectrum disorder. J Neurother. 2007;11(1):5–23. https://doi.org/10.1300/J184v11n01_02. [Google Scholar]
- 21.Coben R, Wright EK, Decker SL, Morgan T. The impact of coherence neurofeedback on reading delays in learning disabled children:A randomized controlled study. NeuroRegulation. 2015;2(4):168. https://doi.org/10.15540/nr.2.4.168. [Google Scholar]
- 22.Walker JE, Kozlowski GP. Neurofeedback treatment of epilepsy. Child Adolesc Psychiatr Clin N Am. 2005;14(1):163–76, 8. doi: 10.1016/j.chc.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 23.Rostami R, Salamati P, Yarandi KK, Khoshnevisan A, Saadat S, Kamali ZS, et al. Effects of neurofeedback on the short-term memory and continuous attention of patients with moderate traumatic brain injury:A preliminary randomized controlled clinical trial. Chin J Traumatol. 2017;20(5):278–82. doi: 10.1016/j.cjtee.2016.11.007. https://doi.org/10.1016/j.cjtee.2016.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mottaz A, Solcà M, Magnin C, Corbet T, Schnider A, Guggisberg AG, et al. Neurofeedback training of alpha-band coherence enhances motor performance. Clin Neurophysiol. 2015;126(9):1754–60. doi: 10.1016/j.clinph.2014.11.023. https://doi.org/10.1016/j.clinph.2014.11.023. [DOI] [PubMed] [Google Scholar]
- 25.Cannon R, Congedo M, Lubar J, Hutchens T. Differentiating a network of executive attention:LORETA neurofeedback in anterior cingulate and dorsolateral prefrontal cortices. Int J Neurosci. 2009;119(3):404–41. doi: 10.1080/00207450802480325. https://doi.org/10.1080/00207450802480325. [DOI] [PubMed] [Google Scholar]
- 26.Noachtar S, Binnie C, Ebersole J, Mauguière F, Sakamoto A, Westmoreland B, et al. A glossary of terms most commonly used by clinical electroencephalographers and proposal for the report form for the EEG findings. The international federation of clinical neurophysiology. Electroencephalogr Clin Neurophysiol Suppl. 1999;52:21–41. [PubMed] [Google Scholar]
- 27.Groppe DM, Bickel S, Keller CJ, Jain SK, Hwang ST, Harden C, et al. Dominant frequencies of resting human brain activity as measured by the electrocorticogram. Neuroimage. 2013;79(1):223–33. doi: 10.1016/j.neuroimage.2013.04.044. https://doi.org/10.1016/j.neuroimage.2013.04.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weber E, Köberl A, Frank S, Doppelmayr M. Predicting successful learning of SMR neurofeedback in healthy participants:Methodological considerations. Appl Psychophysiol Biofeedback. 2011;36(1):37–45. doi: 10.1007/s10484-010-9142-x. https://doi.org/10.1007/s10484-010-9142-x. [DOI] [PubMed] [Google Scholar]
- 29.Doppelmayr M, Nosko H, Pecherstorfer T, Fink A. An attempt to increase cognitive performance after stroke with neurofeedback. Biofeedback. 2007;35(4):126–30. [Google Scholar]
- 30.Becerra J, Fernández T, Roca-Stappung M, Díaz-Comas L, Galán L, Bosch J, et al. Neurofeedback in healthy elderly human subjects with electroencephalographic risk for cognitive disorder. J Alzheimers Dis. 2012;28(2):357–67. doi: 10.3233/JAD-2011-111055. https://doi.org/10.3233/JAD-2011-111055. [DOI] [PubMed] [Google Scholar]
- 31.Enriquez-Geppert S, Huster RJ, Figge C, Herrmann CS. Self-regulation of frontal-midline theta facilitates memory updating and mental set shifting. Front Behav Neurosci. 2014;8:420. doi: 10.3389/fnbeh.2014.00420. https://doi.org/10.3389/fnbeh.2014.00420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reiner M, Rozengurt R, Barnea A. Better than sleep:Theta neurofeedback training accelerates memory consolidation. Biol Psychol. 2014;95:45–53. doi: 10.1016/j.biopsycho.2013.10.010. https://doi.org/10.1016/j.biopsycho.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 33.Egner T, Strawson E, Gruzelier JH. EEG signature and phenomenology of alpha/theta neurofeedback training versus mock feedback. Appl Psychophysiol Biofeedback. 2002;27(4):261–70. doi: 10.1023/a:1021063416558. https://doi.org/10.1023/A:1021063416558. [DOI] [PubMed] [Google Scholar]
- 34.Gruzelier J. A theory of alpha/theta neurofeedback, creative performance enhancement, long distance functional connectivity and psychological integration. Cogn Process. 2009;10(Suppl 1):S101–9. doi: 10.1007/s10339-008-0248-5. https://doi.org/10.1007/s10339-008-0248-5. [DOI] [PubMed] [Google Scholar]
- 35.Ros T, Théberge J, Frewen PA, Kluetsch R, Densmore M, Calhoun VD, et al. Mind over chatter:Plastic up-regulation of the fMRI salience network directly after EEG neurofeedback. Neuroimage. 2013;65:324–35. doi: 10.1016/j.neuroimage.2012.09.046. https://doi.org/10.1016/j.neuroimage.2012.09.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Peeters F, Ronner J, Bodar L, van Os J, Lousberg R. Validation of a neurofeedback paradigm:Manipulating frontal EEG alpha-activity and its impact on mood. Int J Psychophysiol. 2014;93(1):116–20. doi: 10.1016/j.ijpsycho.2013.06.010. https://doi.org/10.1016/j.ijpsycho.2013.06.010. [DOI] [PubMed] [Google Scholar]
- 37.Ring C, Cooke A, Kavussanu M, McIntyre D, Masters R. Investigating the efficacy of neurofeedback training for expediting expertise and excellence in sport. Psychol Sport Exerc. 2015;16:118–27. https://doi.org/10.1016/j.psychsport.2014.08.005. [Google Scholar]
- 38.Hardt JV, Kamiya J. Anxiety change through electroencephalographic alpha feedback seen only in high anxiety subjects. Science. 1978;201(4350):79–81. doi: 10.1126/science.663641. https://doi.org/10.1126/science.663641. [DOI] [PubMed] [Google Scholar]
- 39.Angelakis E, Stathopoulou S, Frymiare JL, Green DL, Lubar JF, Kounios J, et al. EEG neurofeedback:A brief overview and an example of peak alpha frequency training for cognitive enhancement in the elderly. Clin Neuropsychol. 2007;21(1):110–29. doi: 10.1080/13854040600744839. https://doi.org/10.1080/13854040600744839. [DOI] [PubMed] [Google Scholar]
- 40.van Boxtel GJ, Denissen AJ, Jäger M, Vernon D, Dekker MK, Mihajlović V, et al. A novel self-guided approach to alpha activity training. Int J Psychophysiol. 2012;83(3):282–94. doi: 10.1016/j.ijpsycho.2011.11.004. https://doi.org/10.1016/j.ijpsycho.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 41.Hanslmayr S, Sauseng P, Doppelmayr M, Schabus M, Klimesch W. Increasing individual upper alpha power by neurofeedback improves cognitive performance in human subjects. Appl Psychophysiol Biofeedback. 2005;30(1):1–10. doi: 10.1007/s10484-005-2169-8. https://doi.org/10.1007/s10484-005-2169-8. [DOI] [PubMed] [Google Scholar]
- 42.Zoefel B, Huster RJ, Herrmann CS. Neurofeedback training of the upper alpha frequency band in EEG improves cognitive performance. Neuroimage. 2011;54(2):1427–31. doi: 10.1016/j.neuroimage.2010.08.078. https://doi.org/10.1016/j.neuroimage.2010.08.078. [DOI] [PubMed] [Google Scholar]
- 43.Sterman MB, Macdonald LR, Stone RK. Biofeedback training of the sensorimotor electroencephalogram rhythm in man:Effects on epilepsy. Epilepsia. 1974;15(3):395–416. doi: 10.1111/j.1528-1157.1974.tb04016.x. https://doi.org/10.1111/j.1528-1157.1974.tb04016.x. [DOI] [PubMed] [Google Scholar]
- 44.Hoedlmoser K, Pecherstorfer T, Gruber G, Anderer P, Doppelmayr M, Klimesch W, et al. Instrumental conditioning of human sensorimotor rhythm (12-15 hz) and its impact on sleep as well as declarative learning. Sleep. 2008;31(10):1401–8. [PMC free article] [PubMed] [Google Scholar]
- 45.Kober SE, Schweiger D, Witte M, Reichert JL, Grieshofer P, Neuper C, et al. Specific effects of EEG based neurofeedback training on memory functions in post-stroke victims. J Neuroeng Rehabil. 2015;12(1):107. doi: 10.1186/s12984-015-0105-6. https://doi.org/10.1186/s12984-015-0105-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cheng MY, Huang CJ, Chang YK, Koester D, Schack T, Hung TM, et al. Sensorimotor rhythm neurofeedback enhances golf putting performance. J Sport Exerc Psychol. 2015;37(6):626–36. doi: 10.1123/jsep.2015-0166. https://doi.org/10.1123/jsep.2015-0166. [DOI] [PubMed] [Google Scholar]
- 47.Ros T, Moseley MJ, Bloom PA, Benjamin L, Parkinson LA, Gruzelier JH, et al. Optimizing microsurgical skills with EEG neurofeedback. BMC Neurosci. 2009;10(1):87. doi: 10.1186/1471-2202-10-87. https://doi.org/10.1186/1471-2202-10-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.de Zambotti M, Bianchin M, Magazzini L, Gnesato G, Angrilli A. The efficacy of EEG neurofeedback aimed at enhancing sensory-motor rhythm theta ratio in healthy subjects. Exp Brain Res. 2012;221(1):69–74. doi: 10.1007/s00221-012-3148-y. https://doi.org/10.1007/s00221-012-3148-y. [DOI] [PubMed] [Google Scholar]
- 49.Vernon D, Egner T, Cooper N, Compton T, Neilands C, Sheri A, et al. The effect of training distinct neurofeedback protocols on aspects of cognitive performance. Int J Psychophysiol. 2003;47(1):75–85. doi: 10.1016/s0167-8760(02)00091-0. https://doi.org/10.1016/S0167-8760(02)00091-0. [DOI] [PubMed] [Google Scholar]
- 50.Thompson L, Thompson M, Reid A. Neurofeedback outcomes in clients with asperger's syndrome. Appl Psychophysiol Biofeedback. 2010;35(1):63–81. doi: 10.1007/s10484-009-9120-3. https://doi.org/10.1007/s10484-009-9120-3. [DOI] [PubMed] [Google Scholar]
- 51.Cannon R, Lubar J, Congedo M, Thornton K, Towler K, Hutchens T, et al. The effects of neurofeedback training in the cognitive division of the anterior cingulate gyrus. Int J Neurosci. 2007;117(3):337–57. doi: 10.1080/00207450500514003. https://doi.org/10.1080/00207450500514003. [DOI] [PubMed] [Google Scholar]
- 52.Jurewicz K, Paluch K, Kublik E, Rogala J, Mikicin M, Wróbel A, et al. EEG-neurofeedback training of beta band (12-22Hz) affects alpha and beta frequencies-A controlled study of a healthy population. Neuropsychologia. 2018;108:13–24. doi: 10.1016/j.neuropsychologia.2017.11.021. https://doi.org/10.1016/j.neuropsychologia.2017.11.021. [DOI] [PubMed] [Google Scholar]
- 53.Berner I, Schabus M, Wienerroither T, Klimesch W. The significance of sigma neurofeedback training on sleep spindles and aspects of declarative memory. Appl Psychophysiol Biofeedback. 2006;31(2):97–114. doi: 10.1007/s10484-006-9013-7. https://doi.org/10.1007/s10484-006-9013-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lubar JF, Swartwood MO, Swartwood JN, O'Donnell PH. Evaluation of the effectiveness of EEG neurofeedback training for ADHD in a clinical setting as measured by changes in T.O.V.A. Scores, behavioral ratings, and WISC-R performance. Biofeedback Self Regul. 1995;20(1):83–99. doi: 10.1007/BF01712768. https://doi.org/10.1007/BF01712768. [DOI] [PubMed] [Google Scholar]
- 55.Leins U, Goth G, Hinterberger T, Klinger C, Rumpf N, Strehl U, et al. Neurofeedback for children with ADHD:A comparison of SCP and theta/beta protocols. Appl Psychophysiol Biofeedback. 2007;32(2):73–88. doi: 10.1007/s10484-007-9031-0. https://doi.org/10.1007/s10484-007-9031-0. [DOI] [PubMed] [Google Scholar]
- 56.Schönenberg M, Wiedemann E, Schneidt A, Scheeff J, Logemann A, Keune PM, et al. Neurofeedback, sham neurofeedback, and cognitive-behavioural group therapy in adults with attention-deficit hyperactivity disorder:A triple-blind, randomised, controlled trial. Lancet Psychiatry. 2017;4(9):673–84. doi: 10.1016/S2215-0366(17)30291-2. https://doi.org/10.1016/S2215-0366(17)30291-2. [DOI] [PubMed] [Google Scholar]
- 57.Rasey H, Lubar JF, McIntyre A, Zoffuto A, Abbott PL. EEG biofeedback for the enhancement of attentional processing in normal college students. J Neurother. 1995;1(3):15–21. https://doi.org/10.1300/J184v01n03_03. [Google Scholar]
- 58.Keizer AW, Verment RS, Hommel B. Enhancing cognitive control through neurofeedback:A role of gamma-band activity in managing episodic retrieval. Neuroimage. 2010;49(4):3404–13. doi: 10.1016/j.neuroimage.2009.11.023. https://doi.org/10.1016/j.neuroimage.2009.11.023. [DOI] [PubMed] [Google Scholar]
- 59.Staufenbiel SM, Brouwer AM, Keizer AW, van Wouwe NC. Effect of beta and gamma neurofeedback on memory and intelligence in the elderly. Biol Psychol. 2014;95:74–85. doi: 10.1016/j.biopsycho.2013.05.020. https://doi.org/10.1016/j.biopsycho.2013.05.020. [DOI] [PubMed] [Google Scholar]
- 60.Buckholtz JW, Meyer-Lindenberg A. Psychopathology and the human connectome:Toward a transdiagnostic model of risk for mental illness. Neuron. 2012;74(6):990–1004. doi: 10.1016/j.neuron.2012.06.002. https://doi.org/10.1016/j.neuron.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 61.Hughes JR, John ER. Conventional and quantitative electroencephalography in psychiatry. J Neuropsychiatry Clin Neurosci. 1999;11(2):190–208. doi: 10.1176/jnp.11.2.190. https://doi.org/10.1176/jnp.11.2.190. [DOI] [PubMed] [Google Scholar]
- 62.Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, et al. Research domain criteria (RDoC):Toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167:748–51. doi: 10.1176/appi.ajp.2010.09091379. https://doi.org/10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- 63.Arns M, de Ridder S, Strehl U, Breteler M, Coenen A. Efficacy of neurofeedback treatment in ADHD:The effects on inattention, impulsivity and hyperactivity:A meta-analysis. Clin EEG Neurosci. 2009;40(3):180–9. doi: 10.1177/155005940904000311. https://doi.org/10.1177/155005940904000311. [DOI] [PubMed] [Google Scholar]
- 64.Micoulaud-Franchi JA, McGonigal A, Lopez R, Daudet C, Kotwas I, Bartolomei F, et al. Electroencephalographic neurofeedback:Level of evidence in mental and brain disorders and suggestions for good clinical practice. Neurophysiol Clin. 2015;45:423–33. doi: 10.1016/j.neucli.2015.10.077. https://doi.org/10.1016/j.neucli.2015.10.077. [DOI] [PubMed] [Google Scholar]
- 65.Schoenberg PL, David AS. Biofeedback for psychiatric disorders:A systematic review. Appl Psychophysiol Biofeedback. 2014;39:109–35. doi: 10.1007/s10484-014-9246-9. https://doi.org/10.1007/s10484-014-9246-9. [DOI] [PubMed] [Google Scholar]
- 66.Sonuga-Barke EJ, Brandeis D, Cortese S, Daley D, Ferrin M, Holtmann M, et al. Nonpharmacological interventions for ADHD:Systematic review and meta-analyses of randomized controlled trials of dietary and psychological treatments. Am J Psychiatry. 2013;170(3):275–89. doi: 10.1176/appi.ajp.2012.12070991. https://doi.org/10.1176/appi.ajp.2012.12070991. [DOI] [PubMed] [Google Scholar]
- 67.Tan G, Thornby J, Hammond DC, Strehl U, Canady B, Arnemann K, et al. Meta-analysis of EEG biofeedback in treating epilepsy. Clin EEG Neurosci. 2009;40(3):173–9. doi: 10.1177/155005940904000310. https://doi.org/10.1177/155005940904000310. [DOI] [PubMed] [Google Scholar]
- 68.Holtmann M, Steiner S, Hohmann S, Poustka L, Banaschewski T, Bölte S, et al. Neurofeedback in autism spectrum disorders. Dev Med Child Neurol. 2011;53(11):986–93. doi: 10.1111/j.1469-8749.2011.04043.x. https://doi.org/10.1111/j.1469-8749.2011.04043x. [DOI] [PubMed] [Google Scholar]
- 69.Hammond DC. Neurofeedback with anxiety and affective disorders. Child Adolesc Psychiatr Clin N Am. 2005;14(1):105–23, 7. doi: 10.1016/j.chc.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 70.Hammer BU, Colbert AP, Brown KA, Ilioi EC. Neurofeedback for insomnia:A pilot study of Z-score SMR and individualized protocols. Appl Psychophysiol Biofeedback. 2011;36(4):251–64. doi: 10.1007/s10484-011-9165-y. https://doi.org/10.1007/s10484-011-9165-y. [DOI] [PubMed] [Google Scholar]
- 71.Ibric VL, Dragomirescu LG. Neurofeedback in pain management. In: Budzynski TH, Budzynski HK, Evans JR, Abarbanel A, editors. Introduction to Quantitative EEG Neurofeedback Advanced Theory and Application. 2nd ed. United States: Elsevier Science Publishing Co Inc; 2009. pp. 417–51. https://doi.org/10.1016/B978-0-12-374534-7.00016-2. [Google Scholar]
- 72.Orlando PC, Rivera RO. Neurofeedback for elementary students with identified learning problems. J Neurother. 2004;8(2):5–19. https://doi.org/10.1300/J184v08n02_02. [Google Scholar]
- 73.Landes JK, Reid CL, Arns M, Badcock NA, Ros T, Enriquez-Geppert S, et al. EEG neurofeedback for executive functions in children with neurodevelopmental challenges. Cochrane Database Syst Rev. 2017;12:CD012890. https://doi.org/10.1002/14651858.CD012890. [Google Scholar]
- 74.Dehghani-Arani F, Rostami R, Nadali H. Neurofeedback training for opiate addiction:Improvement of mental health and craving. Appl Psychophysiol Biofeedback. 2013;38(2):133–41. doi: 10.1007/s10484-013-9218-5. https://doi.org/10.1007/s10484-013-9218-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.McCarthy-Jones S. Taking back the brain:Could neurofeedback training be effective for relieving distressing auditory verbal hallucinations in patients with schizophrenia? Schizophr Bull. 2012;38(4):678–82. doi: 10.1093/schbul/sbs006. https://doi.org/10.1093/schbul/sbs006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Surmeli T, Ertem A, Eralp E, Kos IH. Schizophrenia and the efficacy of qEEG-guided neurofeedback treatment:A clinical case series. Clin EEG Neurosci. 2012;43(2):133–44. doi: 10.1177/1550059411429531. https://doi.org/10.1177/1550059411429531. [DOI] [PubMed] [Google Scholar]
- 77.Gil Y, Li G, Lee J. Integrated real-time neurofeedback system to raise the frontal lobe activity:Design and implementation. Conf Proc IEEE Eng Med Biol Soc. 2009;2009:845–8. doi: 10.1109/IEMBS.2009.5333098. [DOI] [PubMed] [Google Scholar]
- 78.Begemann MJ, Florisse EJ, Van Lutterveld R, Kooyman M, Sommer IE. Translational brain rhythmicity efficacy of EEG neurofeedback in psychiatry:A comprehensive overview and meta-analysis. Transl Brain Rhythm. 2016;1(1):19–29. https://doi.org/10.15761/TBR.1000105. [Google Scholar]
- 79.Marzbani H, Marateb HR, Mansourian M. Neurofeedback:A comprehensive review on system design, methodology and clinical applications. Basic Clin Neurosci. 2016;7(2):143–58. doi: 10.15412/J.BCN.03070208. https://doi.org/10.15412/J.BCN.03070208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Yucha C, Montgomery D. Evidence-Based Practice in Biofeedback and Neurofeedback. Wheat Ridge, CO: Association for Applied Psychophysiology and Biofeedback; 2008. [Google Scholar]
- 81.Escolano C, Navarro-Gil M, Garcia-Campayo J, Minguez J. The effects of a single session of upper alpha neurofeedback for cognitive enhancement:A sham-controlled study. Appl Psychophysiol Biofeedback. 2014;39(3-4):227–36. doi: 10.1007/s10484-014-9262-9. https://doi.org/10.1007/s10484-014-9262-9. [DOI] [PubMed] [Google Scholar]
- 82.Vernon DJ. Can neurofeedback training enhance performance?An evaluation of the evidence with implications for future research. Appl Psychophysiol Biofeedback. 2005;30(4):347–64. doi: 10.1007/s10484-005-8421-4. https://doi.org/10.1007/s10484-005-8421-4. [DOI] [PubMed] [Google Scholar]
- 83.Gruzelier JH. EEG-neurofeedback for optimising performance. I:A review of cognitive and affective outcome in healthy participants. Neurosci Biobehav Rev. 2014;44:124–41. doi: 10.1016/j.neubiorev.2013.09.015. https://doi.org/10.1016/j.neubiorev.2013.09.015. [DOI] [PubMed] [Google Scholar]
- 84.Gruzelier JH. EEG-neurofeedback for optimising performance. II:Creativity, the performing arts and ecological validity. Neurosci Biobehav Rev. 2014;44:142–58. doi: 10.1016/j.neubiorev.2013.11.004. https://doi.org/10.1016/j.neubiorev.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 85.Niv S. Clinical efficacy and potential mechanisms of neurofeedback. Personal Individ Dif. 2013;54(6):676–86. https://doi.org/10.1016/j.paid.2012.11.037. [Google Scholar]
- 86.Baydala L, Wikman E. The efficacy of neurofeedback in the management of children with attention deficit/hyperactivity disorder. Paediatr Child Health. 2001;6(7):451–5. doi: 10.1093/pch/6.7.451. https://doi.org/10.1093/pch/6.7.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Holtmann M, Sonuga-Barke E, Cortese S, Brandeis D. Neurofeedback for ADHD:A review of current evidence. Child Adolesc Psychiatr Clin N Am. 2014;23(4):789–806. doi: 10.1016/j.chc.2014.05.006. https://doi.org/10.1016/j.chc.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 88.Dempster T. An Investigation into the Optimum Training Paradigm for Alpha Electroencephalographic Biofeedback. Canterbury Christ Church University Thesis. 2012 [Google Scholar]
- 89.Gevensleben H, Holl B, Albrecht B, Vogel C, Schlamp D, Kratz O, et al. Is neurofeedback an efficacious treatment for ADHD?A randomised controlled clinical trial. J Child Psychol Psychiatry. 2009;50(7):780–9. doi: 10.1111/j.1469-7610.2008.02033.x. https://doi.org/10.1111/j.1469-7610.2008.02033.x. [DOI] [PubMed] [Google Scholar]
- 90.Steiner NJ, Frenette EC, Rene KM, Brennan RT, Perrin EC. In-school neurofeedback training for ADHD:Sustained improvements from a randomized control trial. Pediatrics. 2014;133:483–92. doi: 10.1542/peds.2013-2059. https://doi.org/10.1542/peds.2013-2059. [DOI] [PubMed] [Google Scholar]
- 91.Strehl U, Leins U, Goth G, Klinger C, Hinterberger T, Birbaumer N, et al. Self-regulation of slow cortical potentials:A new treatment for children with attention-deficit/hyperactivity disorder. Pediatrics. 2006;118(5):e1530–40. doi: 10.1542/peds.2005-2478. https://doi.org/10.1542/peds.2005-2478. [DOI] [PubMed] [Google Scholar]
- 92.Witte M, Kober SE, Ninaus M, Neuper C, Wood G. Control beliefs can predict the ability to up-regulate sensorimotor rhythm during neurofeedback training. Front Hum Neurosci. 2013;7:478. doi: 10.3389/fnhum.2013.00478. https://doi.org/10.3389/fnhum.2013.00478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kober SE, Witte M, Ninaus M, Neuper C, Wood G. Learning to modulate one's own brain activity:The effect of spontaneous mental strategies. Front Hum Neurosci. 2013;7:695. doi: 10.3389/fnhum.2013.00695. https://doi.org/10.3389/fnhum.2013.00695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Paluch K, Jurewicz K, Rogala J, Krauz R, Szczypińska M, Mikicin M, et al. Beware:Recruitment of muscle activity by the EEG-neurofeedback trainings of high frequencies. Front Hum Neurosci. 2017;11:119. doi: 10.3389/fnhum.2017.00119. https://doi.org/10.3389/fnhum.2017.00119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Roth SR, Sterman MB, Clemente CD. Comparison of EEG correlates of reinforcement, internal inhibition and sleep. Electroencephalogr Clin Neurophysiol. 1967;23(6):509–20. doi: 10.1016/0013-4694(67)90017-x. https://doi.org/10.1016/0013-4694(67)90017-X. [DOI] [PubMed] [Google Scholar]
- 96.Kaplan BJ. Morphological evidence that reline SMR and human mu are analogous rhythms. Brain Res Bull. 1979;4(3):431–3. doi: 10.1016/s0361-9230(79)80021-0. https://doi.org/10.1016/S0361-9230(79)80021-0. [DOI] [PubMed] [Google Scholar]
- 97.Schomer DL, Lopes da Silva FH. Niedermeyer's Electroence-phalography:Basic Principles, Clinical Applications, and Related Fields. London: Lippincott Williams and Wilkins; 2012. [Google Scholar]
- 98.Wolpaw JR, Birbaumer N, McFarland DJ, Pfurtscheller G, Vaughan TM. Brain-computer interfaces for communication and control. Clin Neurophysiol. 2002;113(6):767–91. doi: 10.1016/s1388-2457(02)00057-3. https://doi.org/10.1016/S1388-2457(02)00057-3. [DOI] [PubMed] [Google Scholar]
- 99.Yuan H, He B. Brain-computer interfaces using sensorimotor rhythms:Current state and future perspectives. IEEE Trans Biomed Eng. 2014;61(5):1425–35. doi: 10.1109/TBME.2014.2312397. https://doi.org/10.1109/TBME.2014.2312397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Arns M, Heinrich H, Strehl U. Evaluation of neurofeedback in ADHD:The long and winding road. Biol Psychol. 2014;95:108–15. doi: 10.1016/j.biopsycho.2013.11.013. https://doi.org/10.1016/j.biopsycho.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 101.Engelbregt HJ, Keeser D, van Eijk L, Suiker EM, Eichhorn D, Karch S, et al. Short and long-term effects of sham-controlled prefrontal EEG-neurofeedback training in healthy subjects. Clin Neurophysiol. 2016;127(4):1931–7. doi: 10.1016/j.clinph.2016.01.004. https://doi.org/10.1016/j.clinph.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 102.Monastra VJ, Monastra DM, George S. The effects of stimulant therapy, EEG biofeedback, and parenting style on the primary symptoms of attention-deficit/hyperactivity disorder. Appl Psychophysiol Biofeedback. 2002;27(4):231–49. doi: 10.1023/a:1021018700609. https://doi.org/10.1023/A:1021018700609. [DOI] [PubMed] [Google Scholar]
- 103.Gani C, Birbaumer N, Strehl U. Long term effects after feedback of slow cortical potentials and of theta/beta-amplitudes in children with attention deficit hyperactivity disorder (ADHD) Int J Bioelectromagn. 2008;10(4):209–232. [Google Scholar]
- 104.Kotchoubey B, Strehl U, Uhlmann C, Holzapfel S, König M, Fröscher W, et al. Modification of slow cortical potentials in patients with refractory epilepsy:A controlled outcome study. Epilepsia. 2001;42(3):406–16. doi: 10.1046/j.1528-1157.2001.22200.x. https://doi.org/10.1046/j.1528-1157.2001.22200.x. [DOI] [PubMed] [Google Scholar]
- 105.Strehl U, Birkle SM, Wörz S, Kotchoubey B. Sustained reduction of seizures in patients with intractable epilepsy after self-regulation training of slow cortical potentials-10 years after. Front Hum Neurosci. 2014;8:604. doi: 10.3389/fnhum.2014.00604. https://doi.org/10.3389/fnhum.2014.00604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lubar JF. Neocortical dynamics:Implications for understanding the role of neurofeedback and related techniques for the enhancement of attention. Appl Psychophysiol Biofeedback. 1997;22(2):111–26. doi: 10.1023/a:1026276228832. https://doi.org/10.1023/A:1026276228832. [DOI] [PubMed] [Google Scholar]
- 107.Kouijzer M, De Moor J, Gerrits B, Congedo M, Van Schie H. Neurofeedback improves executive functioning in children with autism spectrum disorders. Res Autism Spectr Disord. 2009;3(1):145–62. https://doi.org/10.1016/j.rasd.2008.05.001. [Google Scholar]
- 108.Wadhwani S, Radvanski DC, Carmody DP. Neurofeedback training in a case of attention deficit hyperactivity disorder. J Neurother. 1998;3(1):42–9. https://doi.org/10.1300/J184v03n01_05. [Google Scholar]
- 109.Rossiter T. The effectiveness of neurofeedback and stimulant drugs in treating AD/HD:Part I. Review of methodological issues. Appl Psychophysiol Biofeedback. 2004;29(2):95–112. doi: 10.1023/b:apbi.0000026636.13180.b6. https://doi.org/10.1023/B:APBI.0000026636.13180.b6. [DOI] [PubMed] [Google Scholar]


