Abstract
Objective
High under-five mortality has been identified as a major problem in many developing countries including Ethiopia. The main purpose of this study is to examine the effect of modern contraceptive use on under-five mortality in Ethiopia.
Methods
The study draws on data from the 2011 and 2016 Ethiopia Demographic and Health Surveys. The Kaplan-Meier survival function was used to demonstrate the survival probabilities of children while a multivariate analysis using the Cox proportional hazards model was used to estimate the under-five mortality risks for various predictors.
Results
The results show consistently higher survival probabilities for children of mothers who use modern contraceptives for all survival periods. Significant predictors of under-five mortality include modern contraceptive use, tetanus vaccinations, mother's age, child's sex, parity, postnatal checkup, marital status, and source of drinking water.
Conclusion
Modern contraceptive use has a notable implication for the chances of under-five survival in Ethiopia. This underscores the importance of modern contraceptive use in the pursuit of a substantial reduction in under-five mortality in the country.
Keywords: Public health, Contraceptive use, Implication, Under-five mortality, Ethiopia
1. Introduction
Globally 5.6 million children under the age of 5 died in 2016 [1]. The global under-five mortality rate declined by 56 percent from 93 deaths per 1,000 live births in 1990 to 41 in 2016 [2]. In the same year, the under-five mortality rate in low-income countries was 73.1 deaths per 1000 live births – almost 14 times the average rate in high-income countries (5.3 deaths per 1000 live births). Sub-Saharan Africa is, by far, the region with the highest level of under-five mortality in the world; approximately 41% of the global under 5 mortality occurs in sub-Saharan Africa (SSA) [3]. Although under-five mortality rate declined by 52% between 1990 and 2015 (from 179 to 86 per 1000 live births) in sub-Saharan Africa, the region still has the highest rate in the world [4].
Ethiopia is among the five developing countries that accounted for half of all newborn deaths including India, Pakistan, Nigeria, and the Democratic Republic of the Congo [2]. About 472,000 Ethiopian children die each year before their fifth birthday, which places Ethiopia sixth among the countries in the world in terms of the absolute number of child deaths [5]. In Ethiopia, the under-five mortality rate has declined by two thirds from the 1990 figure of 204 per 1,000 live births to 58 per 1,000 live births in 2016; thus, meeting the target for Millennium Development Goal 4 (MDG 4) [6-8]. However, the under-five mortality rate in Ethiopia is still higher compared to the mortality rate in many developing countries.
Family planning has been found to significantly contribute to the prevention of maternal and child mortality [9]. Globally, birth spacing through increased use of modern family planning methods has been found to save the lives of more than 2 million newborns and children every year [10]. Therefore, scale-up of family planning improves maternal health and empowerment and benefits child survival [11]. Improved access to family planning could also be a primary prevention measure to reduce under-five deaths, particularly in regions such as sub-Saharan Africa where high fertility is still prevalent [10]. Initiatives such as Family Planning 2020 to enable 120 million more women and girls to use contraceptives by 2020 could have an important effect on child survival, reducing the number of deaths due to reduction in numbers of births mainly through birth spacing [11].
While many studies have examined contraceptive use and its effects in Ethiopia, there is a gap in knowledge on whether the contraceptive use and intention to use have any implication for under-five mortality in Ethiopia. Research documented that contraceptive use has the potential to improve perinatal outcomes and child survival by widening the interval between successive pregnancies [11]. It has been found that the risk of death in ages 1–4 years would fall by 21% in developing countries if all children were spaced by at least 2 years age gap [11]. Also, a study conducted in Nigeria shows that under-five mortality for children whose mothers had an unmet need for family planning had a higher risk of dying than those whose mothers have met the need for family planning [12]. Similarly, family planning is found to be a major factor in reducing the overall rate of under-five mortality in Bangladesh [13]. Moreover, evidence shows that birth interval, an index of contraceptive use and intention to use, has implication for childhood mortality [14, 15, 16]. In this paper, we examine the effect of contraceptive use and intention to use on under-five mortality in Ethiopia. We also controlled for other factors that may confound the effect of contraceptive use on under-five mortality. We, therefore, hypothesize that contraceptive use and intention to use may have a significant negative effect on under-five mortality in Ethiopia.
2. Methods
2.1. Data
This study is based on data derived from two rounds of the Ethiopian Demographic and Health Surveys (2011 and 2016) obtained from the Central Statistical Agency, Ethiopia [7, 17]. Our analysis is, therefore, based on data from the demographic and health surveys (DHS) collected between 2011 and 2016 from 11 regions. The sample is, therefore, limited to mothers aged 15 to 49 who had at least one child (10,896 in 2011; and 10,274 in 2016). Details of the sampling design and data collection procedures for each survey are available in the individual country DHS of AIS reports [7].
2.2. Study variables
In this study, the outcome variable is under-five mortality, defined as the probability of dying before the fifth birthday. Globally, under-5 mortality is regarded as a good measure of well-being and socio-economic development of a nation. In terms of exposure, the main explanatory variable is modern contraceptive use and intention to use. Contraceptive use and intention to use is classified into three: using modern method, non-user - intends to use later, and does not intend to use. Respondents who were using traditional method were considered as non-users of modern contraceptives while missing responses were dropped from the analysis.
In addition, other independent variables capable of influencing or confounding the association between the outcome variable (under-five mortality) and the key explanatory variable (contraceptive use and intention to use) were included in the analysis. These variables include: maternal age at birth, maternal education, marital status, parity, sex of child, birth rank/interval, place/mode of delivery, previous birth interval, previous death of sibling, water source, Tetanus vaccination, antenatal care, postnatal care, place of residence, and region of residence. Since the study used secondary data, ethical clearance was not applicable.
2.3. Statistical analysis
The data analysis was done using the R programming language (version 3.5.2) [18]. Cox proportional hazards model (survival analysis) is appropriate in analyzing non-censored and censored observations. Using Cox proportional hazards regression analysis, both occurrences of childhood mortality and the time when the child died were combined to generate the outcome variable. The children's survival status and the age at death in months (if the child had died) or the last month the child was known to be alive (if the child was still living at the time of the survey) were combined to generate the outcome variable for the survival analysis. Children known to have died before 60 months of age (i.e. non-censored) were regarded as the cases while children who were still alive at the time of the survey were treated as right-censored observations. The probability of childhood death was regarded as a hazard. The hazard was modeled using the following equations:
| H(t) = H0(t) exp(b1x1 + b2x2 + b3x3 + ... + bkxk) | (1) |
where X1 ... Xk is a collection of explanatory variables and H0(t) is the baseline hazard at time t, representing the hazard for a person with the value of the reference level for all the explanatory variables. However, by dividing both sides of Eq. (1) by H0(t) and taking logarithms, Eq. (1) becomes:
| ln (H(t)/H0(t)) = (b1x1 + b2x2 + b3x3 + ... + bkxk) | (2) |
where H(t)/H0(t) is regarded as the hazard ratio. The coefficients bi...bk are estimated by partial likelihood. At the bivariate level, Kaplan-Meier survival plots were used to present the survival function between under-five mortality and contraceptive use. Hazard models were fitted at the multivariate level of analysis and measures of association between the outcome variable and explanatory variables were expressed as hazard ratios (HR) at 95% confidence intervals.
3. Results
3.1. Descriptive results
In the descriptive analysis, 38.8% of the respondents were aged 20–29 whereas 3.7% were aged 15–19 (Table 1). The majority of the respondents had no formal education (63.0%) whereas about one-tenth (10.6%) had secondary school or higher education. Christianity (57.6%) was the dominant religious affiliation among the respondents whereas traditional religion was the least represented (0.7%). Also, the majority (85.3%) were in marital union whilst only a few were never married (1.0%) with about 39% of the respondents having 5 or more children. About 45% had never had antenatal care while the majority (92.9%) had never had postnatal care either. The respondents were predominantly from rural settings (74.0%) with the highest proportion coming from the Oromia region (13.4%). With regard to their modern contraceptive use rate, those aged 20–29 (34.1%) tend to use modern contraceptives than their counterparts while respondents who had secondary or higher education (49.7%) tend to use contraceptives more than those who were less educated or had no formal education. Contraceptive use was more prevalent among the Christians, particularly the orthodox Christians (35.2%), but was lowest among the traditional respondents (4.9%).
Table 1.
Background characteristics and prevalence of modern contraceptive use.
| Variables | Percent of respondents | Modern contraceptive use |
|---|---|---|
| Mother's Age | (%) | |
| 15–19 | 3.7 | 23.7 |
| 20–29 | 38.8 | 34.1 |
| 30–39 | 36.2 | 31.1 |
| 40–49 | 21.3 | 19.1 |
| Education | ||
| No education | 63.0 | 24.8 |
| Primary | 26.4 | 35.2 |
| Secondary/higher | 10.6 | 49.7 |
| Religion | ||
| Catholic | 0.9 | 30.9 |
| Orthodox Christian | 38.4 | 35.2 |
| Protestant | 18.3 | 34.1 |
| Muslim | 41.7 | 19.4 |
| Traditional | 0.7 | 4.9 |
| Marital status | ||
| Never married | 1.0 | 31.8 |
| In union | 85.3 | 16.0 |
| Widowed/divorced/separated | 13.7 | 13.3 |
| Parity | ||
| 1–2 | 35.5 | 34.6 |
| 3–4 | 25.6 | 32.9 |
| 5+ | 38.9 | 23.2 |
| Antenatal care visits | ||
| No visits | 45.1 | 21.3 |
| 1-4 visits | 37.2 | 37.0 |
| 5 + visits | 17.7 | 46.4 |
| Postnatal care | ||
| Yes | 7.1 | 24.8 |
| No | 92.9 | 35.2 |
| Type of place of residence | ||
| Urban | 26.0 | 43.2 |
| Rural | 74.0 | 26.4 |
| Region of residence | ||
| Addis Ababa | 7.1 | 44.8 |
| Afar | 8.4 | 10.3 |
| Amhara | 12.2 | 35.5 |
| Ben-Gumuz | 8.1 | 25.2 |
| Dire Dawa | 6.3 | 25.2 |
| Gambella | 7.5 | 27.6 |
| Harari | 6.1 | 30.8 |
| Oromia | 13.4 | 28.2 |
| SNNP | 12.2 | 31.7 |
| Somali | 7.9 | 2.3 |
| Tigray | 10.8 | 26.7 |
3.2. Contraceptive use and under-five survival
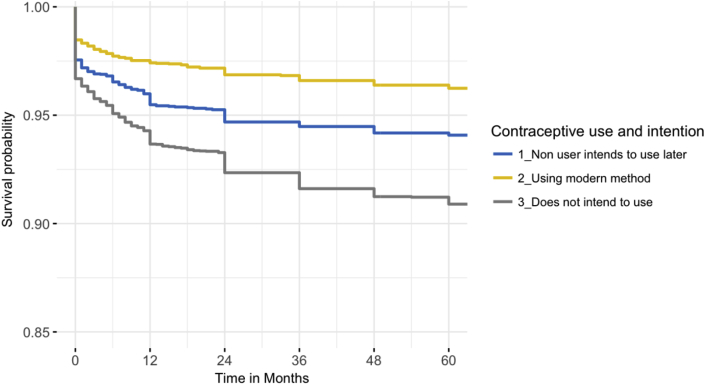
This section seeks to determine the relationship between child survival probability and contraceptive use over the duration of survival (0–59 months). A diagrammatic presentation of the mortality risks among children who did not survive beyond the age of five by contraceptive use is provided in Fig. 1. From the diagram, it is observable that the probability of survival gradually declined for all children irrespective of the status of contraceptive use. However, at 0 month old, children whose mothers used modern contraceptives had the highest probability of survival, followed by children whose mothers intend to use contraceptives later. Children whose mothers did not intend to use modern contraceptives had the least probability of survival. This trend persisted over the course of all the ages of survival for all children.
Fig. 1.
Kaplan-Meier survival function of under-5 mortality by contraceptive use and intention to use, Ethiopia.
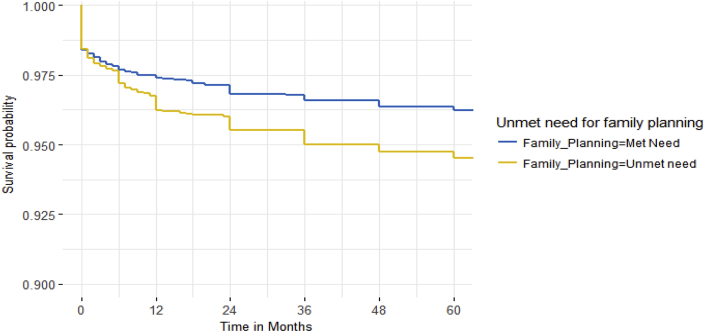
This trend also emerged in the relationship between child survival and unmet need for family planning which is often used to measure the extent of contraceptive use or non-use (Fig. 2). This can be seen as the survival function for children whose mothers had an unmet need for family planning consistently lagged behind children whose mothers had met the need for family planning in terms of survival probability over the entire duration of survival. Thus, children whose mothers had access to family planning services had higher chances of under-five survival.
Fig. 2.
Kaplan-Meier survival function of under-5 mortality by unmet need for family planning, Ethiopia.
3.3. Contraceptive use and risk factors for under-5 mortality
A multivariate analysis of risk factors of under-five mortality using contraceptive use as the variable of interest in combination with other maternal and child-related characteristics showed a number of significant factors. The factors that are significantly associated with the risk of under-five mortality include the use of modern contraceptives, marital status, parity, sex of a child, two or more Tetanus vaccinations, place/mode of delivery, postnatal care within two months, and the household source of drinking water. The risk of child deaths was higher among children whose mothers had been formerly married, male children, mothers who had more than five children, children born in health facilities without a cesarean section, and mothers who used unimproved water sources (Table 2).
Table 2.
Cox Proportional Hazard model showing the effects of modern contraceptive use and intention and other selected characteristics on child mortality in Ethiopia.
| Variables | Hazard ratio | 95% CI | P-value |
|---|---|---|---|
| Contraceptive use and intention (Ref: Non-user intends to use later) | |||
| Using modern method | 0.65 | 0.45–0.96 | 0.03* |
| Does not intend to use | 0.93 | 0.69–1.26 | 0.66 |
| Age at first birth (Ref: <20) | |||
| 20+ | 0.79 | 0.59–1.06 | 0.12 |
| Maternal education (Ref: No education) | |||
| Primary education | 1.17 | 0.87–1.56 | 0.31 |
| Secondary/higher | 0.77 | 0.26–2.28 | 0.63 |
| Marital status (Ref: Married/In union) | |||
| Never married | 0.36 | 0.10–1.37 | 0.13 |
| Widowed/divorced/separated | 1.76 | 1.15–2.69 | 0.01* |
| Parity (Ref: 1–2) | |||
| 3–4 | 1.39 | 0.82–2.38 | 0.95 |
| 5+ | 1.98 | 0.99–3.99 | 0.05* |
| Sex of child (Ref: Female) | |||
| Male | 1.60 | 1.25–2.05 | 0.00** |
| Birth rank/interval (Ref: 1st birth order) | |||
| 2nd/3rd birth rank, < 2 years | 0.81 | 0.39–1.65 | 0.56 |
| 2nd/3rd birth rank, < 2 years | 0.85 | 0.46–1.55 | 0.60 |
| 4 + birth rank | 0.65 | 0.29–1.29 | 0.20 |
| Tetanus vacination (Ref: Never) | |||
| One TT | 1.17 | 0.73–1.87 | 0.51 |
| 2 + TT | 0.72 | 0.52–1.01 | 0.05* |
| Combined place & mode of delivery (Ref: Health facility with cesarean) | |||
| Health facility without cesarean | 2.38 | 1.02–5.54 | 0.04* |
| Home | 1.47 | 0.80–2.69 | 0.21 |
| Previous death of a sibling (Ref: Alive) | |||
| Dead | 1.14 | 0.85–1.52 | 0.38 |
| Antenatal care (Ref: Yes) | |||
| No | 1.04 | 0.75–1.45 | 0.79 |
| Postnatal care (Ref: Yes) | |||
| No | 1.92 | 0.98–3.75 | 0.05* |
| Water source (Ref: Piped water) | |||
| Rain/well/surface water/tanker | 1.56 | 0.95–2.57 | 0.07* |
| River/stream/lake/spring | 1.51 | 0.95–2.41 | 0.07* |
| Type of residence (Ref: Rural) | |||
| Urban | 1.37 | 0.78–2.40 | 0.28 |
| Region (Ref: Addis Ababa) | |||
| Region | |||
| Afar | 2.02 | 0.75–5.44 | 0.16 |
| Amhara | 1.43 | 0.53–3.87 | 0.48 |
| Ben-Gumuz | 1.25 | 0.46–3.38 | 0.66 |
| Dire | 1.88 | 0.69–5.11 | 0.22 |
| Gambella | 1.51 | 0.57–3.96 | 0.40 |
| Harari | 1.45 | 0.55–3.82 | 0.45 |
| Oromia | 1.89 | 0.71–5.02 | 0.20 |
| SNNP | 1.74 | 0.66–4.60 | 0.27 |
| Somali | 1.58 | 0.59–4.27 | 0.36 |
| Tigray | 1.43 | 0.55–3.73 | 0.47 |
NB: Ref = Reference Category *p ≤ 0.05; **p ≤ 0.01; ***p ≤ 0.001.
Under-five children whose mothers used modern contraceptives were less likely (hazard ratio (HR) = 0.65, CI: [0.45, 0.96]) to die than those whose mothers’ never used modern contraceptives. Male children were significantly more likely to die than their female counterparts in the first five years of their life (HR = 1.60, CI: [1.25, 2.05] for male under-5 children). There was a significant increase in the hazard of dying for children of widowed/divorced/separated mothers (HR = 1.76; CI: [1.15, 2.69]) compared to those of married mothers. Children who were born in health facilities without a cesarean section were significantly more likely (HR = 2.38; CI: [1.02, 5.54]) to die than those who were born in health facilities with a cesarean section. There was also a significantly higher hazard of dying (HR = 1.92; CI: [1.16 to 4.50]) among children who never receive postnatal care within 2 months after delivery compared to their counterparts who received postnatal care within 2 months after delivery.
Furthermore, the risk factors of under-five mortality by contraceptive use and intention to use were controlled separately for child characteristics in three models (Table 3). This is to examine the association between contraceptive use and intention to use and child survival while adjusting for the effects of selected child characteristics. As shown in models 1–3 (Table 3), after adjusting for the effects of selected child characteristics, contraceptive use and intention to use remained significantly associated with under-five mortality. Results in Model 3, for instance, indicated significantly lower risks of dying before the age of five years for children whose mothers used modern contraceptives (HR: 0.66, CI [0.51, 0.87], p < 0.001) and higher risk of dying for children whose mothers did not intend to use modern contraceptives (HR: 1.20, CI [0.97, 1.49], p < 0.001) compared to children whose mothers were non-users but intend to use later.
Table 3.
Cox Proportional Hazard model showing the effects of contraceptive use and intention on child mortality, adjusting for selected child's characteristics.
| Variables | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Contraceptive use & intention (Ref: Non-user intends to use) | HR[95%CI] | HR[95%CI] | HR[95%CI] |
| Using modern method | 0.66** [0.51,0.87] | 0.63** [0.45,0.88] | 0.63** [0.45,0.88] |
| Does not intend to use | 1.20* [0.97,1.49] | 0.95 [0.71,1.28] | 0.96 [0.72,1.29] |
| Previous birth interval (Ref:<2yrs) | |||
| 2–3 | 0.68*** [0.54,0.84] | 0.72* [0.54,0.97] | 0.72* [0.54,0.97] |
| 4+ | 0.47*** [0.36,0.61] | 0.58** [0.40,0.84] | 0.59** [0.41,0.84] |
| Parity (Ref:1–2) | |||
| 3–4 | 1.27 [0.92,1.75] | 1.30 [0.85,1.98] | 1.30 [0.85,1.97] |
| 5+ | 1.56** [1.16,2.09] | 1.53* [1.03,2.29] | 1.52* [1.02,2.28] |
| Antenatal care (Ref: No) | |||
| Yes | 0.37* [0.17,0.81] | 0.92 [0.70,1.21] | |
| Postnatal care (Ref: No) | |||
| Yes | 0.92 [0.70,1.21] | 0.37* [0.17,0.82] | |
| Sex of child (Ref: Female) | |||
| Male | 1.74*** [1.36,2.24] | ||
NB: Ref = Reference Category; HR = Hazard ratios *p ≤ 0.05; **p ≤ 0.01; ***p ≤ 0.001.
4. Discussion
This study examines the implication of contraceptive use and intention to use for under-five mortality in Ethiopia. The data were based on live births among women who reported met need or unmet need for family planning during the period under study. The study first generated survival functions between under-five mortality and contraceptive use as well as unmet need for family planning. The results reveal a higher childhood survival probability for children of mothers who use modern contraceptives and mothers who have met the need for family planning than children of their counterparts who never used contraceptives or had unmet need, across all survival ages. Also, after adjusting for the effects of important covariates, such as maternal education, wealth status, and marital status among others in the multivariate analysis, the results still show a significant association between under-five mortality and contraceptive use and intention to use. This finding implies that contraceptive use and intention is associated with lower under-five mortality in Ethiopia which provides support for our hypothesis. A similar association is observed elsewhere in Bangladesh and Nigeria [12, 13]. Children of mothers who did not intend to use contraceptives had a higher likelihood of under-five mortality than those who were users and those who intend to use later. This implies that contraceptive use and met need for family planning have a considerable impact on child survival in Ethiopia. This may not be due to the use of the contraceptive in itself, but may be due to the substantial biological and socioeconomic benefits that are concomitant with contraceptive use which may promote both maternal and child health.
Additionally, the study found lower under-five mortality risk in children who were delivered in health facilities without a Caesarean section. Previous studies have associated high mortality risks with home delivery of babies [19]. This may be mostly due to delivery complications at home. In this regard, delivering at health facilities without caesarean section services may have similar risks to delivering at home when there are complications. Health facilities with Caesarean section services are considered to be quite scarce in Ethiopia. The unavailability of obstetric services has been considered as the key reason why women may continue to prefer home delivery even when facility-based delivery is available at minimal cost [20].
Divorced or separated and widowed women are found to be significantly more likely to experience under-five mortality than their married or in-union counterparts. Even though many studies have not yet been conducted on the effect of the mother's marital status on under-five mortality, it is evident that being in a union is a protective factor against under-five mortality. Thus, marriage may proffer advantages such as pooling of resources to either patronise good health services or provide adequate care with respect to providing good nutrition to infants and children [21]. Widowed and divorced women, on the other hand, may have comparatively limited economic resources due to the unavailability of their male partners to provide support. Consequently, they may mostly live on a very limited income to secure the daily food consumption of the household and to take care of their children [22].
Furthermore, children of mothers who have not received post-natal care within two months after delivery are found to be significantly more likely to experience under-five mortality than their counterparts whose mothers attended post-natal checkups after delivery. Conversely, children of mothers who made postnatal visits within the first 2 months after birth are found to be significantly associated with a lower risk of under-five mortality [23]. Also, children whose mothers did not have Tetanus immunizations have a significantly higher risk of under-five mortality. Immunization of pregnant women or women of childbearing age with at least two doses is found to reduce under-five mortality due to tetanus by 94% [24]. The mortality risk of a child is also found to increase as the size of children ever born increases. The risk of under-five deaths increased significantly among mothers who have more than five children. Similar findings have been well documented in the literature, showing a positive relationship between family size and child mortality [16, 25]. It has been established that mothers with two or more children are 40% less likely to receive professionally-assisted delivery services compared to women with only one child [26]. This may be due to the limited ability to patronize professionally-assisted delivery services as the number of children increases. This may have serious implications for the levels of under-five mortality in the country.
Lack of access to clean water has been considered to be one of the important factors that contribute to more than 80 percent of childhood deaths in the world [27], and this has reflected in this study. The use of an unimproved source of drinking water is found to be associated with increased risk of under-five mortality. There is also considerable evidence from studies in developing countries that show the role of household sanitation and clean water supply in promoting child health and survival [28, 29, 30]. In Ethiopia, the proportion of the population using improved drinking-water sources is only about 57%, and those who use improved sanitation are less than five percent [31]. Thus, access to improved source of water and sanitation may have positive effects on under-five mortality risks in Ethiopia.
This study has one notable limitation that should be taken with caution when interpreting the results. There is a possibility of the time difference between the occurrence of the outcome and the main independent variable (under-five mortality and contraceptive use), as mothers' contraceptive use behaviour may not always coincide with the occurrence of under-five mortality which may affect the results. However, we believe that this provides the best scenario of the phenomenon as we do not expect mothers’ contraceptive use behaviour to change considerably within the five years preceding the survey.
5. Conclusions
The findings of this study show that contraceptive use and intention to use has indispensable implication for under-five mortality risk in Ethiopia. The use of contraceptives significantly improves the survival chances of children under age five. This underscores the importance of contraceptive-use in the pursuit of a substantial reduction in under-five mortality in Ethiopia. It also intensifies the need to address the present level of contraceptive use and unmet need for family planning in the country. Special intervention is, therefore, required for mothers who have unmet need for contraception and mothers who do not intend to use contraceptives. Implementing a cost-effective public health-related intervention to improve household environmental conditions, such as access to improved source of drinking water may have a positive effect on reducing under-five mortality in the country. Further research on non-users may help to understand the personal, cultural as well as possible religious factors that may militate against the use of modern contraceptives, which in turn may be adversely affecting under-five survival.
Declarations
Author contribution statement
Fikrewold Bitew: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Samuel H. Nyarko: Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
Data for this study were obtained from the DHS Program.
References
- 1.WHO . 2018. Global Health Observation Data: Under-five Mortality.http://www.who.int/gho/child_health/mortality/mortality_under_five_text/en/ [Google Scholar]
- 2.UNICEF, WHO, World Bank Group and United Nations . UNICEF; New York: 2017. Levels and Trends in Child Mortality: Report 2017. [Google Scholar]
- 3.Rutherford M.E., Mulholland K., Hill P.C. How access to health care relates to under-five mortality in sub-Saharan Africa: systematic review. Trop. Med. Int. Health. 2010;15(5):508–519. doi: 10.1111/j.1365-3156.2010.02497.x. [DOI] [PubMed] [Google Scholar]
- 4.Issaka A.I., Agho K.E., Renzaho A.M. The impact of internal migration on under-five mortality in 27 sub-Saharan African countries. PLoS One. 2016;11(10) doi: 10.1371/journal.pone.0163179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National MoH. MoH; Addis Ababa: 2015. Strategy for Child Survival in Ethiopia. [Google Scholar]
- 6.You D. Global, regional, and national levels and trends in under-5 mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Inter-agency Group for Child Mortality Estimation. The Lancet. 2015;386(10010):2275–2286. doi: 10.1016/S0140-6736(15)00120-8. [DOI] [PubMed] [Google Scholar]
- 7.CSA, ICF International . Central Statistical Agency and ICF International; Addis Ababa and Calverton: 2016. Ethiopia Demographic and Health Survey 2016. [Google Scholar]
- 8.Deribew A. Trends, causes, and risk factors of mortality among children under 5 in Ethiopia, 1990–2013: findings from the Global Burden of Disease Study 2013. Pop Health Met. 2016;14(1):42. doi: 10.1186/s12963-016-0112-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chola L. Scaling up family planning to reduce maternal and child mortality: the potential costs and benefits of modern contraceptive use in South Africa. PLoS One. 2015;10(6) doi: 10.1371/journal.pone.0130077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu L. Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: an updated systematic analysis. The Lancet. 2015;385(9966):430–440. doi: 10.1016/S0140-6736(14)61698-6. [DOI] [PubMed] [Google Scholar]
- 11.Cleland J. Contraception and health. The Lancet. 2012;380(9837):149–156. doi: 10.1016/S0140-6736(12)60609-6. [DOI] [PubMed] [Google Scholar]
- 12.Adedini S.A. Unmet need for family planning: implication for under-five mortality in Nigeria. J. Health Popul. Nutr. 2015;33(1):187. [PMC free article] [PubMed] [Google Scholar]
- 13.Abir T. Risk factors for under-5 mortality: evidence from Bangladesh demographic and health survey, 2004–2011. BMJ Open. 2015;5(8) doi: 10.1136/bmjopen-2014-006722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ayele D.G., Zewotir T.T. Childhood mortality spatial distribution in Ethiopia. J. Appl. Stat. 2016;43(15):2813–2828. [Google Scholar]
- 15.Ayele D.G., Zewotir T.T., Mwambi H.G. Structured additive regression models with spatial correlation to estimate under-five mortality risk factors in Ethiopia. BMC Public Health. 2015;15(1):268. doi: 10.1186/s12889-015-1602-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ayele D.G., Zewotir T.T., Mwambi H.G. Survival analysis of under-five mortality using Cox and frailty models in Ethiopia. J. Health Popul. Nutr. 2017;36(1):25. doi: 10.1186/s41043-017-0103-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.CSA, ICF International . Central Statistical Agency and ICF International; Addis Ababa and Calverton: 2012. Ethiopia Demographic and Health Survey 2011. [Google Scholar]
- 18.R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2018. R: A Language and Environment for Statistical Computing.www.r-project.org Available at: [Google Scholar]
- 19.Filippi V. Maternal health in poor countries: the broader context and a call for action. The Lancet. 2006;368(9546):1535–1541. doi: 10.1016/S0140-6736(06)69384-7. [DOI] [PubMed] [Google Scholar]
- 20.Shiferaw S. Why do women prefer home births in Ethiopia? BMC Pregnancy Childbirth. 2013;13(1):5. doi: 10.1186/1471-2393-13-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kanmiki E.W. Socio-economic and demographic determinants of under-five mortality in rural northern Ghana. BMC Int. Health Hum. Right. 2014;14(1):24. doi: 10.1186/1472-698X-14-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bitew F.H., Telake D.S. ICF Macro; Calverton, Maryland, USA: 2010. Undernutrition Among Women in Ethiopia: Rural-Urban Disparity. DHS Working Papers No. 77. [Google Scholar]
- 23.Baqui A.H. Effect of timing of first postnatal care home visit on neonatal mortality in Bangladesh: an observational cohort study. BMJ. 2009;339:b2826. doi: 10.1136/bmj.b2826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blencowe H. Tetanus toxoid immunization to reduce mortality from neonatal tetanus. Int J Epidem. 2010;39(suppl_1):i102–i109. doi: 10.1093/ije/dyq027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bereka S.G., Habtewold F.G. Under-five mortality of children and its determinants in Ethiopian Somali regional state, Eastern Ethiopia. Health Sci. J. 2017;11(3) [Google Scholar]
- 26.Mekonnen Y., Mekonnen A. Factors influencing the use of maternal healthcare services in Ethiopia. J. Health Popul. Nutr. 2003;21(4):374–382. [PubMed] [Google Scholar]
- 27.UNICEF. Every . UNICEF; New York: 2017. Child Alive: the Urgent Need to End Newborn Deaths. [Google Scholar]
- 28.Sastry N. What explains rural-urban differentials in child mortality in Brazil? Soc. Sci. Med. 1997;44(7):989–1002. doi: 10.1016/s0277-9536(96)00224-9. [DOI] [PubMed] [Google Scholar]
- 29.Ezeh O.K. The impact of water and sanitation on childhood mortality in Nigeria: evidence from demographic and health surveys, 2003–2013. Int. J. Environ. Res. Public Health. 2014;11(9):9256–9272. doi: 10.3390/ijerph110909256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mugo N.S. Determinants of neonatal, infant and under-five mortality in a war-affected country: analysis of the 2010 Household Health Survey in South Sudan. BMJ Glob Health. 2018;3(1) doi: 10.1136/bmjgh-2017-000510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.WHO . WHO; Geneva: 2017. World Health Statistics. [Google Scholar]