Abstract
Objective
To explore and compare residents’ interaction with electronic health records during primary care encounters and whether those behaviors differ by residency year level.
Methods
A field study was conducted in which thirty-eight patient visits with 12 family medicine resident physicians were observed and video recorded in two primary care clinics under the umbrella of a university-based department of family medicine. Videos were then coded for gaze behaviors in which patients’ and physicians’ gazes at electronic health records and at each other were coded using a pre-established objective coding scheme.
Results
Third year residents spent the greatest percentage of visit time looking at EHR screens when compared to first and second year residents. Third year residents also spent significantly more time typing or inputting information into the records during the clinical visit when compared to first and second year residents.
Conclusion
This study illustrated that patterns for using the EHR and interacting with patients may change over time for residents. These changes may be due to increased EHR proficiency or increased workload that incentivizes using the EHR to retrieve information and to complete charting in front of the patient.
Keywords: Residents, EHRs, Primary care
INTRODUCTION
The United States health care system is undergoing a major transition from paper-based to electronic health records (EHR). The EHR adoption rate was estimated to be 68% in 2011 among family physicians.1 Government funding and incentives have fostered this growth. Studies have reported the potential benefits of EHRs, including cost savings, efficiency and safety2–4, and enriched patient data5. However, concerns have also been raised about potential negative impact on the physician-patient relationship and communication.6–8
There is a small but growing literature on teaching of EHR skills to medical students and residents9–14 However, no study to date has objectively examined differences between residents at different levels of training in regards to how they interact with the EHR and patients. Rouf et al15 found that patients of internal medicine residents, compared to those of faculty physicians, were more likely to feel that the computer adversely affected the amount of time physicians spent talking, looking at and examining them. This suggests that with experience—either clinical or specifically with the use of the EHR–physicians become more skillful in incorporating the EHR into patient encounter. However, Rouf et al did not employ objective measures of physician behavior nor did it examine differences in residents of different year levels. To address this gap, we undertook the present exploratory, cross-sectional study in which we compared first, second and third year family medicine residents’ in the exam room. In so doing, we employed technology and methods our group has employed in previous studies.16,17
METHODS
Study Setting and Participants
This study was performed during a 4 month period from February to May in 2012 at two primary care clinics under the umbrella of the University of Wisconsin-Madison. At each site, physicians used the same EHR system, physical space and clinical support system. The physical set-up of the exam rooms was as follows: The physician sat centered at a small desk while the patient sat at one end of the desk, facing forward. All EHRs’ screens are located on the wall between patient and the physician and facing toward them. All the screens also have the ability to be moved around by the physicians.
A convenience sampling strategy was used to recruit physicians and patients. An instruction form was sent to all residents via email (36) explaining the study, and follow up reminders were also sent. Those who agreed to participate signed an informed consent form allowing the researchers to video record their patient visits. For patient recruitment, we focused on established, adult patients of residents who agreed to participate to the study. Eligibility requirements for the patients were: 1) being between 18–65 years old; 2) having had at least 1 previous visit with respective participating resident; 3) being scheduled for a 30 min for PG-2 and PG-3 and 45 min for PG-1 follow up visit for the current appointment. In addition, per IRB requests, patients who discussed or planned to discuss socially stigmatizing conditions such as substance abuse, illegal activity, abortion, or mental illness were also excluded from participating in the study and were not recorded. Study procedures and activities were approved and monitored by university and clinic Institutional Review Boards (IRB). We used three high-resolution video cameras-each placed at a different angle- to record the visits, and created one single multichannel video for analysis.18 In addition, we had a short open ended survey with residents involving questions regarding their demographics, training about EHR use and how they develop their EHR use style. Finally, validated survey items were used to assess patients’ overall satisfaction, perceptions of physician use of EHR, and physicians’ communication skills.19,20
Data Analysis
A systematic coding methodology was employed to quantify human-human and human-technology interactive behaviors in the visit.18 In this study, a coding scheme was adapted from a previous study.18 All coders were trained well and their coded video were checked constantly to maintain at least 0.60 kappa reliability score.18 Each video was coded temporally for the entire visit length with using multichannel stream with a half speed (1/2 sc) in order to allow the coders to capture and quantify all behaviors accurately. The two variables we used for analysis were eye gaze and typing. For quantified video data, the average percentage rates for each behavior were reported. In addition, we used “Welch’s t test” to estimate significant differences across the resident groups. Significant values were reported with using a p value of at least .05.
RESULTS
Twelve residents (4 residents from each year) agreed to participate out of 36 residents in total (participation rate: 33 %). The age range of the participating residents was 28–31 years old (mean= 29.5). Five of the residents were male. Thirty-eight out of 90 approached patients (43%) agreed to participate (9 patients by PG-1, 15 patients by PG-2, 14 patients by PG-3). The age range of the patients was 20–31 years old (mean= 39).
We used the terminology as “adjusted visit length”, which was defined as the length of the time the physician spent in the exam room with the patient excluding physical exam period and the time when physician was out of the room. The average adjusted visit length for all visits was 1286 seconds (21 min.). The average adjusted visit length for each resident group were as follows: 1737 sec. (PG-1), 1352 sec. (PG-2), and 977 sec. (PG-3). Significant differences were found in adjusted visit length between PG-1-PG-2 (p=0.003), PG-1-PG-3 (p=0.003), and PG2-PG3 (p=0.009).
Residents’ interaction with EHR
Residents reported that they each developed their own EHR use style due to lack of formal training on how to interact with the EHRs and patients. The values were calculated as percentages of adjusted visit length rather than duration in order to obtain a more accurate estimate of the amount of time physicians interacted with patients. Figure 1 illustrates all percentage values for interaction with EHRs for each resident group as a ratio to adjusted visit length. “Overall” indicates the mean across the all visits (38 visits) in the study collapsed across resident group.
Figure 1.
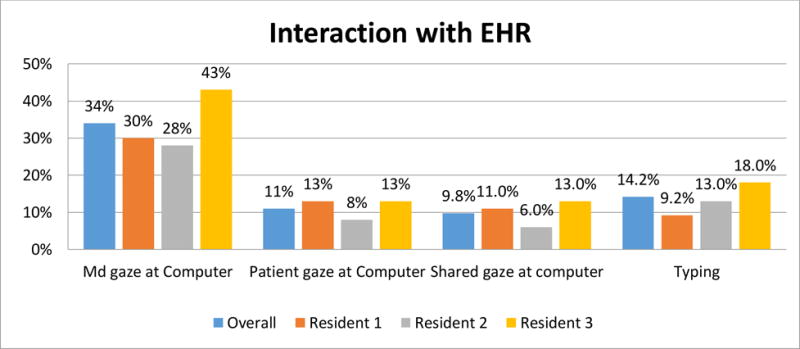
Percentage values for interaction with EHR behaviors
Across resident groups, PG-3’s gazed at the EHR significantly longer than PG-1’s (p=0.003) and PG-2’s (p= 0.002). PG-3 also typed significantly more during the visit than PG-1 (p= 0.001). There were no significant differences between groups for “patient gaze at EHR” (PGE) and “shared gaze at EHR” (SE).
Residents’ interaction with Patients
Figure 2 illustrates all values regarding interpersonal communication for overall sample and each resident group.
Figure 2.
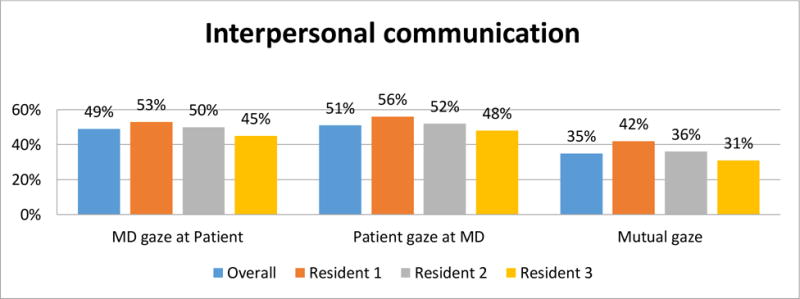
Percentage values for interpersonal communication behaviors
Although there were remarkable percentage differences across some groups, we did not observe any significant differences presumably because of the small sample size.
Patients’ survey result
Table 2 depicts results of several items from the questionnaires.
Table 2.
Descriptive results of several survey questions
| Overall | PGT-1 | PGT-2 | PGT-3 | |
|---|---|---|---|---|
| How satisfied were you with overall visit? | 4.81 | 4.86 | 4.79 | 4.86 |
| How would you rate the doctor’s manners during the visit? | 4.92 | 5.00 | 5.00 | 4.86 |
| How satisfied were you with the doctor? | 4.94 | 5.00 | 4.93 | 5.00 |
| The doctor pretends to know things when he/she is really not sure. | 1.94 | 1.57 | 1.50 | 2.43 |
| The doctor does not always give me a chance to say everything I think he/she needs to know. | 1.66 | 1.29 | 1.46 | 2.00 |
| I am satisfied with how the doctor and I communicated. | 4.69 | 4.29 | 4.93 | 4.69 |
| I want to know what the doctor is typing into the computer. | 3.72 | 3.43 | 3.57 | 4.07 |
| I felt frustrated when the doctor used the computer. | 1.67 | 1.43 | 1.29 | 2.07 |
| The doctor’s computer use was distracting. | 1.92 | 2.29 | 1.36 | 2.21 |
| I felt comfortable speaking to the doctor while he/she was typing. | 4.47 | 3.86 | 4.71 | 4.57 |
| The doctor was knowledgeable about the computer. | 4.53 | 4.14 | 4.71 | 4.57 |
| The doctor was successful in their use of the computer. | 4.58 | 4.14 | 4.71 | 4.71 |
| The doctor was confident using the computer. | 4.42 | 3.86 | 4.71 | 4.50 |
| The doctor relied heavily on the computer. | 2.69 | 2.29 | 2.50 | 3.00 |
| Because of the computer, the doctor spent less time looking at me than I liked. | 1.86 | 2.00 | 1.57 | 2.07 |
| Because of the computer, he doctor spent less time talking with me than I liked. | 1.89 | 1.71 | 1.57 | 2.29 |
| Computer use made the visit feel less personal. | 2.44 | 2.57 | 1.71 | 3.00 |
Note: Likert scales, with 1 being “strongly disagree” and 5 being “strongly agree”.
Furthermore, statistical analysis yielded several significant differences between items: “I felt frustrated when the doctor used the computer” PG2 and PG3 (p=0.036), “computer use made visit less personal” PG2 and PG3 (p= 0.023), “the doctor’s computer use was distracting” PG2 and PG3 (p=0.044).
DISCUSSION
The present study found that more senior family medicine residents spent more time gazing at the computer screen and more time typing than more junior residents, which might suggest that there may be a linear progression of these behaviors across the 3 years of the residency. While the patient survey data yielded largely non-significant results, the patients of the most senior (PG-3) residents felt their physicians’ computer use was distracting, were the most frustrated with their physicians’ computer use, and felt their visits were the least personal. Quantified video data also showed that PG-3 residents has highest amount of interaction with EHR (which was significant) and lowest percentage of gazing at patient (this was not statistically significant) compared to other PG groups. It may be that the increase use of the computer by the third year residents reflected increased knowledge of and, perhaps, comfort with their patients, compared to the more junior residents. However, it would appear from the results that this may not be appreciated by the most senior residents’ patients. In addition, the patient survey results suggest that patients of senior residents felt frustrated by the use of the computer and felt the visits were less personal, which might influence caring relationship and some of the patient outcomes negatively. Finally, we should also note that we only examined nonverbal aspect of the visit, we did not explore verbal communication.
There might be two potential explanations of the findings regarding the differences in the residents across year levels. First, first year residents spend less time looking at the computer screen and typing because of their lack of confidence in and lack of facility with the EHR. This is also suggested by the patient perceptions (patient survey) that residents’ success in using the EHR increased with year level. As a result, less experienced residents may avoid using the EHR (including writing their notes) while they are in the exam room. As they become more skillful and confident over time in the use of the EHR, they might feel more comfortable utilizing the EHR and entering data in the presence of patients.
The second the explanation of the results relates to the scheduling templates for the different year levels of the residents. Residents are required to see more patients per session as they progress through the years. As a result, they are expected to spend progressively less time per patient as they advance through the program. These differential expectations are reflected in the lengths of the visits we found for the residents of various year levels. It is also plausible that the differences between less and more advanced residents reflected greater time pressure experienced by the latter. For example, a third year resident would have less time to review a patient’s chart before the visit and less time to write a note afterwards than a first year resident. Thus, the more experienced residents would have greater incentives to utilize EHR information and do their charting in front of the patient. The alternative may be doing their charting after hours.
There are several limitations to this study. First, this was a cross sectional study in that we did not follow the residents as they progressed through the program. Second, the sample size is small, which resulted in lower statistical power. Third, the low participation rate of residents might call to question the attitudes and skills of residents who did not participate to the study. The low participation rate could be due to their busy schedules and/or no precedent for their being taped in a research project. Thus, it may not have been a representative sample. Forth, the fact that one ergonomic setup was used in all of the exam rooms makes generalization uncertain to other arrangements, especially those that are more conducive to direct physician-patient gaze. Finally, we acknowledge that the behaviors we examined—as important as they may be–do not constitute the totality of the clinical encounter. As Zoppi and Epstein (2002) asserted, there are other “intangible” elements of the physician “way[s] of being” that impact patients’ perceptions that cannot be objectively observed.21 Further, we did not evaluate such important elements as clinical judgment or the thoroughness of physical examinations.
With these limitations in mind, to our knowledge, this is the first study that compared EHR behavior of residents of various levels of experience. The fact that none of the 12 participating residents had any formal instruction on how to incorporate the EHR into their communications with patients is, in itself, revealing and, we believe, may indicate a larger neglect of this topic.9,13 In spite of the growth of the use of EHRs, our review of the literature revealed an absence of studies on how to best teach residents use the EHR in their interactions with patients, let alone on the outcome teaching programs in this area. The present study might stimulate future research in this area.
Table 1.
Patient demographics
| N (%) | |
|---|---|
| Gender | |
| Male | 16 (42 %) |
| Female | 22 (58 %) |
|
| |
| Race | |
| White | 16 (42%) |
| African American | 16 (42%) |
| Hispanic | 3 (8 %) |
| Asian | 1 (2 %) |
| N/A | 2 (6 %) |
|
| |
| Education level | |
| High school | 21 (56%) |
| Bachelor/Some college | 14 (38 %) |
| Graduate degree | 2 (6 %) |
Footnotes
Conflict of Disclosure: None
References
- 1.Xierali IM, Hsiao C-J, Puffer JC, et al. The rise of electronic health record adoption among family physicians. Ann Fam Med. 2013;11(1):14–19. doi: 10.1370/afm.1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hillestad R, Bigelow J, Bower A, et al. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff. 2005;24(5):1103–17. doi: 10.1377/hlthaff.24.5.1103. [DOI] [PubMed] [Google Scholar]
- 3.Buntin MB, Jain SH, Blumenthal D. Health information technology: laying the infrastructure for national health reform. Health Aff. 2010;29(6):1214–19. doi: 10.1377/hlthaff.2010.0503. [DOI] [PubMed] [Google Scholar]
- 4.Lown BA, Rodriguez D. Commentary: Lost in translation? How electronic health records structure communication, relationships, and meaning. Acad Med. 2012;87(4):392–4. doi: 10.1097/ACM.0b013e318248e5ae. [DOI] [PubMed] [Google Scholar]
- 5.Ventres W, Kooienga S, Marlin R, et al. Clinician style and examination room computers: a video ethnography. Fam Med. 2005;37(4):276–81. [PubMed] [Google Scholar]
- 6.Als AB. The desk-top computer as a magic box: patterns of behaviour connected with the desk-top computer; GPs’ and patients’ perceptions. Fam Prac. 1997;14(1):17. doi: 10.1093/fampra/14.1.17. [DOI] [PubMed] [Google Scholar]
- 7.Saleem JJ, Flanagan ME, Russ AL, et al. You and me and the computer makes three: variations in exam room use of the electronic health record. J Am Med Inform Assoc. 21(e1):e147–e151. doi: 10.1136/amiajnl-2013-002189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.White A, Danis M. Enhancing Patient-Centered Communication and Collaboration by Using the Electronic Health Record in the Examination RoomEnhancing Patient-Centered Communication With the EHR. JAMA. 2013;309(22):2327–28. doi: 10.1001/jama.2013.6030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Graham-Jones P, Jain SH, Friedman CP, et al. The need to incorporate health information technology into physicians’ education and professional development. Health Aff (Millwood) 2012;31(3):481–7. doi: 10.1377/hlthaff.2011.0423. [DOI] [PubMed] [Google Scholar]
- 10.Hammoud MM, Dalrymple JL, Christner JG, et al. Medical student documentation in electronic health records: a collaborative statement from the Alliance for Clinical Education. Teach Learn Med. 2012;24(3):257–66. doi: 10.1080/10401334.2012.692284. [DOI] [PubMed] [Google Scholar]
- 11.Pageler NM, Friedman CP, Longhurst CA. Refocusing Medical Education in the EMR EraViewpoint. JAMA. 2013;310(21):2249–50. doi: 10.1001/jama.2013.282326. [DOI] [PubMed] [Google Scholar]
- 12.Embi PJ, Yackel TR, Logan JR, et al. Impacts of computerized physician documentation in a teaching hospital: perceptions of faculty and resident physicians. J Am Med Inform Assoc. 2004;11(4):300–09. doi: 10.1197/jamia.M1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morrow JB, Dobbie AE, Jenkins C, et al. First-year medical students can demonstrate EHR-specific communication skills: a control-group study. Fam Med. 2009;41(1):28–33. [PubMed] [Google Scholar]
- 14.Thornton JD, Schold JD, Venkateshaiah L, et al. The Prevalence of Copied Information by Attendings and Residents in Critical Care Progress Notes. Crit Care Med. 2013;41(2):382. doi: 10.1097/CCM.0b013e3182711a1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rouf E, Whittle J, Lu N, et al. Computers in the exam room: differences in physician patient interaction may be due to physician experience. J Gen Intern Med. 2007;22(1):43–48. doi: 10.1007/s11606-007-0112-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Asan O, Montague E. Physician interactions with electronic health records in primary care. Health Systems. 2012;1(2):96–103. doi: 10.1057/hs.2012.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Proceedings of the Human Factors and Ergonomics Society Annual Meeting. SAGE Publications; 2012. Assessing Patient and Doctor Eye Gaze Patterns Between Two Styles of Doctor Ehr Use in Primary Care Encounters. [Google Scholar]
- 18.Asan O, Montague E. Technology-mediated information sharing between patients and clinicians in primary care encounters. Behav Inform Tech. 2013;33(3):259–70. doi: 10.1080/0144929X.2013.780636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hall MA, Zheng B, Dugan E, et al. Measuring patients’ trust in their primary care providers. Medical care research and review. 2002;59(3):293–318. doi: 10.1177/1077558702059003004. [DOI] [PubMed] [Google Scholar]
- 20.Montague EN, Winchester WW, III, Kleiner BM. Trust in medical technology by patients and healthcare providers in obstetric work systems. Behav Inform Tech. 2010;29(5):541–54. doi: 10.1080/01449291003752914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zoppi K, Epstein RM. Is Com m unification a Skill? Com mu nication Behaviors and Being in Relation. Fam Med. 2002;34(5):319–24. [PubMed] [Google Scholar]


