ABSTRACT
Background:
Early discharge from psychiatric inpatient care may pose challenges for the patient's recovery and may incite a rapid return to the hospital. This study identified demographic, clinical, and the continuing of care characteristics associated with rapid readmission into a sample of psychiatric inpatient hospitals.
Methods:
Cross-sectional analysis of 60,254 discharges from state psychiatric hospitals. Logistic regression explored the relationship between predictors of rapid readmission.
Results:
Eight percent of discharges were readmitted to the same hospital within 30 days after discharge. Factors significantly related with rapid readmission included white (odds ratio, 1.23; 95% confidence interval, 1.13–1.34), non-Hispanic (1.48, 1.26–1.73), not married (1.53, 1.32–1.76), voluntarily admitted (1.18, 1.05–1.33), with length of stay (LOS) ≤ 7 days (3.52, 3.04–4.08), or LOS 8–31 days (3.20, 2.79–3.66), or LOS 32–92 days (1.91, 1.65–2.22), with a schizophrenia or other psychotic disorders (1.69, 1.46–1.96) or personality disorder (1.76, 1.50–2.06), referred to a setting different from the outpatient (1.27, 1.16–1.40), or with a living arrangement different from private residence (1.54, 1.40–1.68).
Conclusions:
Disparities in rapid readmission rates exist among state psychiatric hospitals. A national overview of the individuals with mental illness at risk of being prematurely discharged may suggests insights into quality initiatives aimed at reducing rapid readmissions into psychiatric inpatient care.
Keywords: 30-day readmission rate, state psychiatric inpatient hospitals, patient predictors, next level of care
Introduction
State psychiatric hospitals provide mental health care for diverse populations.1,2 These hospitals have undergone continuous mental health care reforms to accommodate the needs of their service populations. The current mental health policy agenda promotes a recovery-oriented model focused on community-based solutions, continuing the deinstitutionalization movement.3,4 Today, nearly 200 state psychiatric hospitals serve more than 140,000 patients and an array of patient populations on an annual basis.2 The deinstitutionalization has decreased the length of hospitalizations and the number of inpatient stays and has increased the number of readmissions after discharge.5-7
Rapid readmissions or those that occur within 30 days after discharge are considered indicators of poor psychiatric care and of inadequate linkage with community-based care.8,9 If appropriate inpatient psychiatric care occurs within the continuum of care, the mental health condition is stabilized and patients are equipped for outpatient recovery.5 Rapid readmissions are associated with adverse events, because they require new treatment options and are more restrictive, which drives costs higher.7,10
Rapid readmissions are amenable to reduction when a change in practice is implemented.11 Knowing the group at risk is the first step. At least two systematic reviews have identified predictors of readmission.11,12 Although Bridge and Barbe (2004) focused on patients experiencing depression and schizophrenia, Durbin et al (2007) expanded the diagnostic groups, but most discharges were from acute care units. Exploration of predictive factors has continued in public, private, teaching, and general hospitals and uses health insurance claims data.5-8,10,13-21
Data from state psychiatric hospitals were made available from a behavioral health care performance measurement system, a comprehensive proprietary national database of patient-level data.22 This study is the first to publish data from a multistate, national sample of state psychiatric hospitals using a discharge cohort with regard to readmission status and the individuals at risk of inpatient readmission for psychiatric care. This could inform best service models to ensure the delivery of complete mental health treatments, crisis stabilization, and community-based service supports. When individuals are discharged after a hospitalization episode, it is indicative of the improved stability of the mental health condition, functionality level, and the ability of the individual to be reintegrated into his/her family environment back in the community.5,13 When patients are abruptly readmitted, this disrupts the readaptation into the personal and community environments and the recovery process of the individual.13 This study explored the readmission rates of a national sample of state psychiatric inpatient hospitals for a discharge cohort. The study identified the demographic factors, clinical attributes, and the next level of care components associated with rapid readmission to state psychiatric hospitals. The study also explored previous concerns about recipients of inpatient psychiatric services being discharged too early and without fully completing the psychiatric treatment.
Methods
Secondary data were extracted from a behavioral health care performance measurement system, comprising patient-level data submitted by psychiatric inpatient hospitals in the United States. Every month, hospital staff submits demographic data, diagnosis, medications, and follow-up information to participate in common quality of care measures. All data extracted from the behavioral health care performance measurement system were de-identified and anonymous. Hospital staffs from psychiatric inpatient hospitals who participate in the behavioral health care performance measurement system approve researchers' use of limited data sets to conduct secondary research and publicly disseminate the findings. Therefore, Institutional Review Board approval was waived for current analysis. All analyses were conducted using the SPSS statistical tool, version 22. Because of the very large sample, all comparisons were based on α set at p < .01 (two-sided).
Procedure
The independent variables included demographic factors, clinical attributes, and next level of care components, which were extracted from the behavioral health care performance measurement system using the hospital identification number, patient identification number, and admission date. Demographic factors and clinical attributes have been identified as risk factors for hospital rapid readmission.6,8,11-13,23 Recent research has emphasized the role of the next level of care components.7,11,15 The 30-day readmission may represent a shortened length of stay that in turn may be indicative of premature discharge representing a high risk for readmission.11
Demographic factors included age, sex, race, ethnicity, marital status, and admission legal status. The admission legal status indicates if the patient was admitted voluntarily (by self or by others) or involuntarily (civil, sexual, and criminal status including patients in pretrial, incompetent to stand trial, not guilty for reason of insanity, guilty but mentally ill, and dangerous but mentally ill).
The clinical attributes included length of stay and mental health diagnosis. Length of stay was calculated from the admission and discharge dates. Hospital staff submitted the mental health diagnosis at discharge using the International Classification of Diseases 9th Version, Clinical Modification (ICD-9-CM). A mental health disorder multilevel variable was created based on the frequency of the mental health disorders among discharges using a vectoring algorithm. The diagnosis hierarchy defined by the algorithm was as follows: (1) schizophrenia or other psychotic disorders, (2) personality disorder, (3) bipolar disorder, (4) depressive disorder, and (5) anxiety disorder. An “other mental health disorders” category was created for those patients with none of the previous five disorders.
The next level of care included various components. The discharge referral status indicated whether or not the patient was referred to the next level of care provider on discharge. The discharge disposition is the primary follow-up service to which the patient was referred for mental health care after discharge. The living arrangement after discharge indicated the type of residential arrangements the patient had immediately after discharge. A complete continuing care plan included elements such as the reason for hospitalization, discharge diagnosis, discharge medications, and next level of care recommendations. The quality measure components for the continuing care plan for a discharge require all components and must be transmitted within 5 days after discharge to be categorized as transmitted on time. Otherwise, the continuing care plan could have been transmitted late (after 5 days after discharge) or not transmitted.
The dependent variable, 30-day readmission after discharge or rapid readmission, included any patient discharged from a psychiatric hospital during the previous reporting period for whom an admission to the same hospital was reported within 30 days after that discharge. It was a dichotomous variable whose rating indicated if the patient was (1) or was not (0) readmitted within 30 days after discharge.
Study Sample
Discharges from psychiatric hospitals were included for analysis if, at the time of the study, the hospital was (1) classified as a state-operated or state-supported hospital and (2) enrolled in the behavioral health care performance measurement system. The study sample included all discharges for adults aged 18 to 64 years, between January 1 and December 31, 2014.
Descriptive Analysis
Frequency analysis was used to describe the sample under study. The Chi-square test tested the relationship between the categorical predictors and rapid readmission. The independent samples t test tested the relationship between the outcome variable and age.
Inferential Analysis
A binary logistic regression was performed to test the null hypothesis of no statistically significant predictive relationship between the predictors and rapid readmission and to generate odds ratios and 95% confidence intervals. The independent variables were entered in a stepwise format. Mental health disorders and length of stay showed to be strongly related to 30-day readmission, therefore they were each entered separately and as interaction terms in Step 1. Demographic factors were entered in Step 2. The next level of care components were entered in Step 3. To determine whether discharges with short length of stays were discharged earlier than predicted by their clinical status, a hierarchical multiple linear regression was performed.
Results
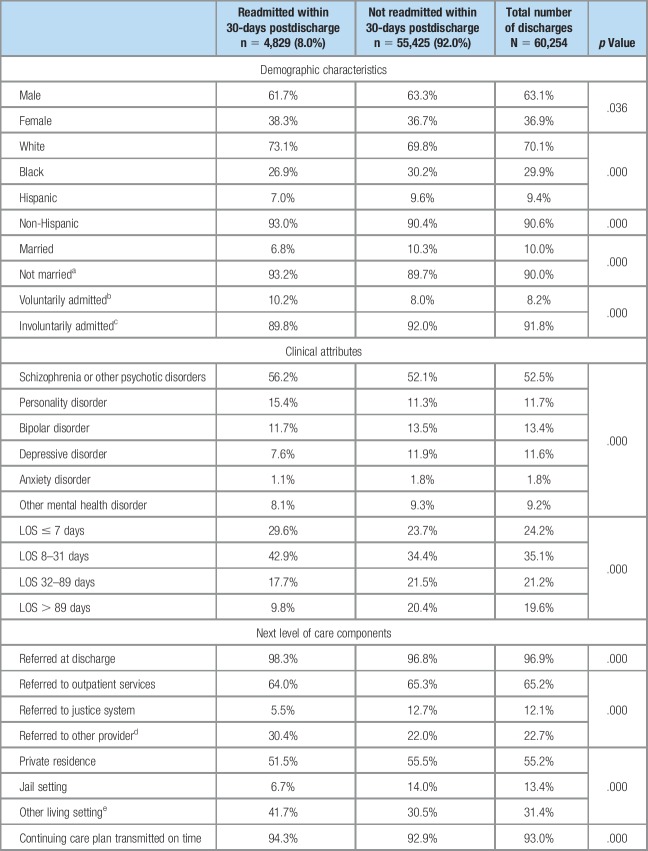
This study analyzed a sample of 60,254 discharges from 127 state psychiatric hospitals in 39 states. Table 1 presents the discharges' characteristics by study group and for the overall sample. The majority were men (63%), white (67%), non-Hispanic (91%), and not married (90%). Individuals were, on average, aged 38 years and had a length of stay of 106 days. Of the 97% of patient discharges with a referral, 65% were made to outpatient services. For 93% of discharges, the continuing care plan to the next level of care was transmitted on time. More than half of the discharges had a diagnosis of schizophrenia or other psychotic disorders (52%).
Table 1.
Discharge Characteristics
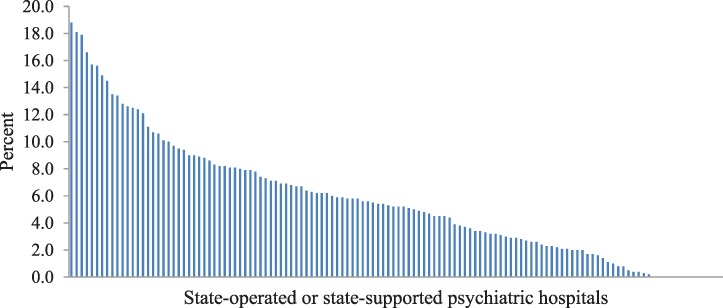
Readmission Rates for State-Operated or State-Supported Psychiatric Hospitals
Figure 1 presents the 30-day readmission rates for each psychiatric hospital in the sample. Overall, 8% of all discharges in the sample were readmitted to psychiatric inpatient care within 30 days after discharge. The rapid readmission rates range from 0% to 18.8%.
Figure 1. 30-day Readmission Rates.
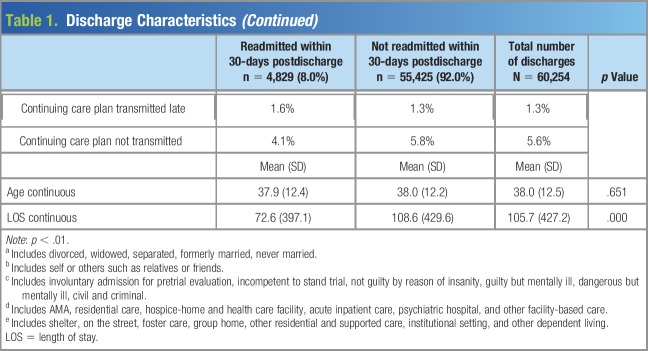
Predictors of 30-Day Hospital Readmission
Table 2 presents the results of the binary logistic regression. The logistic regression model correctly classified 92% of patient discharges. None of the mental health disorders and length of stay interaction terms were significant and therefore are not presented in Table 2. The results indicate that a patient who is white (odds ratio [OR] = 1.228), non-Hispanic (OR = 1.478), not married (OR = 1.525), or voluntary admitted (OR = 1.178) is more likely to be rapidly readmitted for inpatient psychiatric care after discharge. As the inpatient stay increases, from less than or equal to 7 days (OR = 3.523), 8–31 days (OR = 3.197), and 32–92 days (OR = 1.914), the likelihood of being rapidly readmitted decreases. Patients discharged with schizophrenia or other psychotic disorders are 1.692 times more likely to be rapidly readmitted. Patients discharged with personality disorder are 1.758 times more likely to be readmitted within 30 days after discharge. Patients referred to another provider are 1.270 times more likely to return to inpatient psychiatric care. Patients with a living arrangement other than a private residence or jail are 1.535 times more likely to be readmitted within 30 days after discharge. Therefore, the null hypothesis was rejected and the alternative accepted.
Table 2.
Binary Logistic Regression Results: Prediction of Rapid Readmission Into State Psychiatric Hospitals
Readmission as an Effect of Premature Discharge
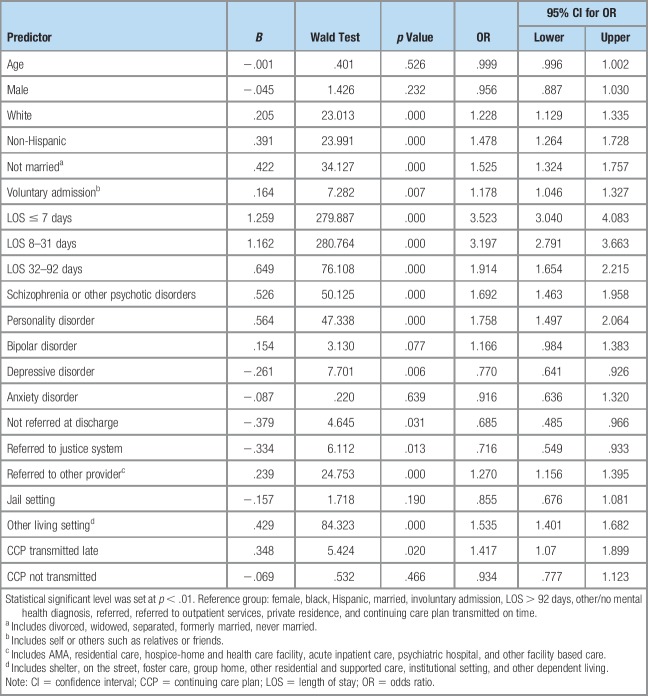
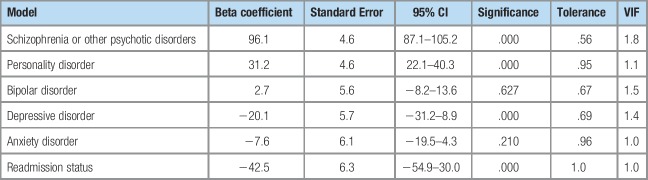
Since a very short length of stay was the strongest factor associated to a 30-day readmission, a hierarchical multiple linear regression was performed to test whether rapid readmission was due to psychiatric treatment factors when controlling for the patients' clinical attributes. Preliminary analyses were performed to ensure that there was no violation to the assumption of normality and linearity. In the model, the clinical characteristics of discharges (i.e., the mental health disorders) were used to predict length of stay and were entered in Model 1. A dummy variable was created for each of the five mental health categories representing the presence (1) of the disorder or not (0). Model 2 included readmission status; a dummy variable identifying those readmitted within 30 days (1) or not (0) was created. Length of stay was entered as a continuous variable.
Table 3 presents the results of the hierarchical multiple linear regression. The overall regression model was significant (F = 149.8, df = 6, p = .000). The following clinical characteristics were positively related with length of stay: presence of schizophrenia or other psychotic disorders (t = 20.8, df = 60,247, p = .000) and presence of personality disorder (t = 6.7, df = 60,247, p = .000). The presence of a depressive disorder was negatively associated (t = −3.5, df = 60,247, p = .000). The readmission status was significantly and negatively associated with length of stay after controlling for the clinical attributes (t = −6.7, df = 60,247, p = .000), thus suggesting a contributing effect of early discharge.
Table 3.
Predictors of Length of Stay
Limitations
This study exhibits some limitations. The researcher analyzed data from state psychiatric hospitals; therefore, generalization could be limited for other psychiatric inpatient providers. The data analysis included discharges, not the unique count of patients. Differences may exist between patients readmitted once and those with multiple readmissions.20 The readmission period was limited to 30 days after discharge; predictors may vary over a shorter or longer term.11 Hospital staff submit specific data to the performance system; other possible predictors were not available. Seventeen percent of hospitals were not included because they submitted samples for the continuing care plan data. However, there were no significant demographic differences between discharges included versus excluded, except for the Hispanic ethnicity. More Hispanics were observed among discharges not included compared with those included. Finally, the analysis accounted for a small part of the variability in the outcome measure, indicating the complexity of the construct. Future research could explore if predictors remain significant with longer periods before readmission to the same hospital. Service data from the outpatient setting could assist to identify the levels of support that may contribute to rapid readmission.
Discussion
This study explored the readmission rates within 30 days after discharge among a large, multistate sample of psychiatric hospitals. An overall readmission rate to the same hospital of 8% was found, which is lower than the findings from previous research on state psychiatric hospitals.13,16,17,20 This was expected because the study focused on readmission to the same hospital. Previous research also analyzed readmission of an admission cohort, whereas this study used a discharge cohort and looked forward in time to determine the readmission status of patients. This is important because it takes into consideration the length of hospital stay, the clinical attributes of patients, and the full continuum of care. A wide range was observed among hospitals' readmission rates, suggesting opportunities for performance improvement.
Research about race and rapid readmission is very limited.24 It was found that whites were at higher risk of readmission and also had a shorter length of stay. New emphasis could be placed on race-specific interventions. Another novel finding was that marital status was related to rapid readmission. This is important because marital status could suggest the practical role of a support system after discharge.13 The majority in the sample were not married, and the results underscore the need for alternative supports to reinforce the outpatient care.
The length of stay was the strongest predictor of rehospitalization within 30 days. An increase in the length of stay from 31 to 89 days was associated with 25% reduction in the proportion of discharges with rapid readmission consistent with the findings of Vasudeva et al (2009) that shorter length of stay was associated with shorter time to readmission. Forty-five percent of the patients with a diagnosis of schizophrenia were discharged within 31 days or less after admission. This may suggest that a large number of patients with schizophrenia are being discharged without proper crisis stabilization.23 Of those who were readmitted and referred to services in settings that were not outpatient or the justice system, 30% were readmitted to residential care and 36% left the hospital against medical advice. Although these findings may suggest improvements in the discharge planning process,11 those who left without medical advice require a more complex understanding. These patients may be experiencing severe symptoms and unstable behaviors and could pose a danger to themselves and to others. It was also found that two of five patients were discharged to a living setting that was not private residence or jail. Living arrangement may have serious implications for individuals without stable housing.13 This could propose that other living arrangements such as shelters, foster and group homes, and other institutional settings may not be equipped to care for the multifaceted mental health needs of this population group.
Different from Lyons et al (1997) and Byrne et al (2010), this study found a significant and negative relationship between being discharged earlier than expected based on the patient's clinical status. However, it cannot be concluded that it is indicative of suboptimal service provision rather than suggesting that discharges might not be adequately linked to the outpatient specialty mental health care.7,25 A study that analyzed patients who were admitted for inpatient care for a psychiatric condition found that patients who did not have an outpatient appointment after discharge were two times more likely to be rehospitalized in the same year.7 An opportunity for process improvement could focus on the discharging provider ensuring an aftercare appointment date as a best practice, although this does not guarantee that the patient will keep such appointment. Future research could also explore the adequacy of the linkage with the next level of care provider.
It cannot be concluded that readmission within 30 days is an indicator of poor quality care, however, readmission within 30 days is a measure used for quality performance. In 2017, the Centers for Medicare and Medicaid Services (CMS) adopted a 30-day all-cause readmission rate measure for performance reporting as part of the Inpatient Psychiatric Facility Quality Reporting program.25 Data from this study will provide additional comparison for state psychiatric hospitals because the CMS measure is calculated based on Medicare claims data and includes readmission to any facility.
Conclusions
Disparities in rapid readmission rates exist among state psychiatric hospitals. A national overview of the individuals with mental illness at risk of being prematurely discharged may suggests insights into quality initiatives aimed at reducing rapid readmissions into psychiatric inpatient care.
Implications for Practice
Nearly 5,000 patients may be prematurely discharged for outpatient services each year. This outcome could be alleviated with greater understanding of the evolving service populations. Demographic and clinical factors are essential for designing effective interventions. Discharging to other providers and other living settings may be more successful with a more comprehensive continuing care plan and scheduled follow-up appointment date. If this study had set the p value at less than .05, the timely transmission of the continuing care plan would have been a protective factor against rapid readmission. This could represent the anticipated connection between the inpatient and the outpatient providers. Length of stay continues to be the strongest predictor of rapid readmission, thus underscoring the value of the long-term care support that should be provided in state psychiatric hospitals.
Acknowledgments
The author thanks Lucille Schacht, PhD and Missy Rand, LPC, CSAC for their careful review of the drafts.
Footnotes
This research study was fully funded by the Behavioral Healthcare Performance Measurement System of the National Association of State Mental Health Program Directors Research Institute, Inc.
The author declares no conflicts of interest.
Author's Biography
Glorimar Ortiz, MS, Principal Biostatistician, National Association of State Mental Health Program Directors Research Institute, Inc. (NRI), Falls Church, Virginia. Current roles and accountabilities: To design, implement, and lead primary and secondary research projects using data from the Behavioral Healthcare Performance Measurement System, a proprietary national database of the NRI. To provide statistical expertise on data analysis from descriptive to exploratory and confirmatory factor analysis, structural equation modeling, reliability and validity, and predictive and survival analyses.
References
- 1.Haupt MB. The vital role of state psychiatric hospitals. 2014. https://www.nasmhpd.org/sites/default/files/The%20Vital%20Role%20of%20State%20Psychiatric%20HospitalsTechnical%20Report_July_2014.pdf.
- 2.Hollen V, Ortiz G. Characteristics of state-operated or supported psychiatric hospital inpatient care. Falls Church, VA: National Association of State Mental Health Program Directors Research Institute, Inc; 2013. [Google Scholar]
- 3.Fisher WH, Geller JL, Pandiani JA. The changing role of the state psychiatric hospital. Health Aff. 2009;28(3):676-684. [DOI] [PubMed] [Google Scholar]
- 4.Vasudeva S, Kumar MSN, Sekhar KC. Duration of first admission and its relation to the readmission rate in a psychiatric hospital. Indian J Psychaitry. 2009;51(4):280-284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lyons JS, O'Mahoney MT, Miller SI, Neme J, Kabat J, Miller F. Predicting readmission to the psychiatric hospital in a managed care environment: Implications for quality indicators. Am J Psychiatry. 1997;154(3):337-340. [DOI] [PubMed] [Google Scholar]
- 6.Mojtabai R, Nicholson RA, Neesmith DH. Factors affecting relapse in patients discharged from a public hospital: Results from survival analysis. Psychiatr Q. 1997;68(2):117-129. [DOI] [PubMed] [Google Scholar]
- 7.Nelson EA, Maruish ME, Axler JL. Effects of discharge planning and compliance with outpatient appointments on readmission rates. Psychiatr Serv. 2000;51(7):885-889. [DOI] [PubMed] [Google Scholar]
- 8.Donisi V, Tedeschi F, Salazzari D, Amaddeo F. Pre- and postdischarge factors influencing early readmission to acute psychiatric wards: Implications for quality-of-care indicators in psychiatry. Gen Hosp Psychiatry. 2016;39:53-58. [DOI] [PubMed] [Google Scholar]
- 9.Heslin KC, Weiss AJ. Hospital Readmissions Involving Psychiatric Disorders, 2012 (Statistical Brief #189). Rockville, MD: Agency for Healthcare Research and Quality; 2015. [PubMed] [Google Scholar]
- 10.Figueroa R, Harman J, Engberg J. Use of claims data to examine the impact of length of inpatient psychiatric stay on readmission rate. Psychiatr Serv. 2004;55(5):560-565. [DOI] [PubMed] [Google Scholar]
- 11.Durbin J, Lin E, Layne C, Teed M. Is readmission a valid indicator of quality of inpatient psychiatric care? J Behav Health Serv Res. 2007;34(2):137-150. [DOI] [PubMed] [Google Scholar]
- 12.Bridge JA, Barbe RP. Reducing hospital readmission in depression and schizophrenia: Current evidence. Curr Opin Psychiatry. 2004;17:505-511. [Google Scholar]
- 13.Adams JD. Risk factors contributing to the 30 day readmission rate at the Alaska Psychiatric Institute for fiscal year 2008. (Master's thesis). 2010. Available from ProQuest Dissertations and Thesis database. (UMI No. 1485380). [Google Scholar]
- 14.Byrne SL, Hooke GR, Page AC. Readmission: A useful indicator of the quality of inpatient psychiatric care. J Affective Disord. 2010;126:206-231. [DOI] [PubMed] [Google Scholar]
- 15.Hamilton JE, Rhoades H, Galvez J, et al. Factors differentially associated with early readmission at a university teaching psychiatric hospital. J Eval Clin Pract. 2015;21:572-578. [DOI] [PubMed] [Google Scholar]
- 16.Hillman SL. Predictors of rapid psychiatric readmission. (Doctoral dissertation, University of Houston). 2000. Available from Bell & Howell Information and Learning Company. (UMI No. 9989826). [Google Scholar]
- 17.Holsten AW. Modifiable Predictors of Rapid Readmission to a State Psychiatric Inpatient Facility: Doctoral dissertation, Fielding Graduate University. 2011.Available from ProQuest dissertations and thesis database. (UMI No. 3454576). [Google Scholar]
- 18.Lauber C, Lay B, Rossler W. Length of first admission and treatment outcome in patients with unipolar depression. J Affective Disord. 2006;93:43-51. [DOI] [PubMed] [Google Scholar]
- 19.Lieberman PB, Wiitala SA, Elliot B, McCoemick S, Goyette SB. Decreasing length of stay: Are there effects on outcome of psychiatric hospitalization?. Am J Psychiatry. 1998;155(7):905-909. [DOI] [PubMed] [Google Scholar]
- 20.Moore CO. Factors associated with rapid readmission among Nevada State Psychiatric Hospital patients. (Master's thesis). 2014. Available from ProQuest Dissertations and Thesis database. (UMI No. 1585490). [DOI] [PubMed] [Google Scholar]
- 21.Moss J, Li A, Tobin J, Weinstein IS, Harimoto T, Lanctot KL. Predictors of readmission to a psychiatric inpatient unit. Compr Psychiatry. 2014;55:426-430. [DOI] [PubMed] [Google Scholar]
- 22.Lorine K, Goenjian H, Kim S, Steinberg AM, Schmidt K, Goenjian AK. Risk factors associated with psychiatric readmission. J Nervous Ment Dis. 2015;203(6):425-430. [DOI] [PubMed] [Google Scholar]
- 23.Yamada MM, Korman M, Hughes CW. Predicting rehospitalization of persons with severe mental illness. J Rehabil. 2000;66(2):32-39. [Google Scholar]
- 24.Boyer CA, McAlpine DD, Pottick KJ, Olfdon M. Identifying risk factors and key strategies in linkage to outpatient psychiatric care. Am J Psychiatry. 2000;157(10):1592-1598. [DOI] [PubMed] [Google Scholar]
- 25.cms.gov. Inpatient psychiatric facility quality reporting (ipfqr) program. 2017. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/IPFQR.html. Accessed on April 27, 2018.