Abstract
Background
Sleep disturbance in adults with no health concerns is often linked to the thermal environment. This study assesses the impact on sleep quality of sleepwear made from fibers with different thermal insulation and hygral properties. This randomized cross-over study investigated the effects on sleep quality of sleepwear made from cotton, polyester and Merino wool in adults aged 50–70 years, at an ambient temperature of 30 °C and a relative humidity of 50%.
Methods
Thirty-six healthy participants completed four nights of sleep study with polysomnography. Participants were categorized by body mass index as <25 kg·m−2 or ≥25 kg·m−2, age as <65 years or ≥65 years, and by Pittsburgh Sleep Quality Index (PSQI) as poor sleepers (PSQI≥5) or good sleepers (PSQI<5).
Results
Small, but statistically significant sleep benefits were observed for wool over cotton and polyester sleepwear for multiple sleep parameters, while neither cotton nor polyester was responsible for any statistically significant sleep benefit over the 11 sleep parameters examined. The key findings were: 1) A significant sleepwear effect was observed for sleep onset latency (SOL), p=0.04. 2) For older participants, sleeping in wool significantly reduced SOL (12.4 mins) compared with cotton (26.7 mins, p=0.001) or polyester (21.6 mins, p=0.001). 3) A statistically significant effect was found for sleep fragmentation index (p=0.01) in which wool sleepwear (12.1 no·h−1) was lower than polyester (13.7 no·h−1) (p=0.005), but not different to cotton (13.3 no·h−1). 4) Poor sleepers had less wakefulness when sleeping in wool compared to cotton (p=0.047). 5) And Poor sleepers had higher rapid eye movement sleep latency in polyester than in cotton (p=0.037) or in wool (p=0.036).
Conclusion
Statistically significant benefits for wool sleepwear were observed on average for all participants and, in particular, for the older and poorer sleepers. There were no significant differences in any sleep variables between sleepwear types for the BMI sub-group.
Keywords: cotton, polyester, wool, polysomnography, thermal comfort
Introduction
In general, the quality of sleep decreases with aging. The sleep of older adults, compared to younger adults, is more fragmented and lighter with increased duration of sleep stages 1 and 2, and reduced duration of deep sleep (sleep stage N3), delta activity and rapid eye movement (REM) sleep.1,2 Reduced sleep efficiency (SE) and total sleep time (TST) with frequent shifts in sleep stages have also been reported1,2 in polysomnography (PSG) studies.
In older adults with no health concerns, sleep disturbances are often linked to the thermal environment that is vital for sleep maintenance.3 Sleeping outside the optimum range of temperature for thermal comfort can negatively impact sleep. Older adults suffer this impact more than younger adults, as they are more vulnerable to heat stress.4,5 The reduced thermoregulatory ability in older adults under hot conditions is due to a combined decreased sweat rate, reduced skin blood flow and overall decrease in physical fitness and increases in body adiposity that may accompany aging.4,6 In addition, reduced hydration levels7 and diminished sweating capacity8 increase the risk of developing hyperthermia and heat stroke6 in older adults. Where bedcovers and clothing were used, older adults have experienced more disturbed sleep in warmer than in cooler conditions.9 Increased wakefulness and decreased REM sleep and SE were observed when sleeping at 32 °C compared to 26 °C10 and when sleeping in summer compared to autumn or winter.9
Higher average summer temperatures and the frequency and intensity of hot days are now observed in Australia11 and globally.12 The night-time bedroom temperature in Australia can exceed 30 °C with a maximum of 38.2 °C without air conditioning.11 A review reported a positive relationship between heat/heat waves and increasing mortality among the elderly and its relationship appeared consistent globally.13 The use of air-conditioning to control temperature is both consumptive of energy and is associated with both direct and indirect negative effects on human health including Legionnaires’ disease and sick building syndrome, with symptoms such as chronic headaches and fatigue.14 It is therefore of interest to investigate alternative healthy and environmentally-friendly strategies for older adults to cope with sleeping under warm ambient conditions.
Sleepwear influences thermal comfort in several crucial ways. Fabrics allow varying rates of heat and moisture transfer.15,16 As each fiber type has its inherent thermal insulation and hygral properties, fabrics made from different fiber types can yield differential effects on thermal insulation.16 These effects could potentially alter sleep quality.
Natural fibers, such as cotton and wool, are hygroscopic with the ability to absorb and transfer large quantities of moisture. Wool has the highest moisture regain of the common textile fibers, with polyester having the lowest regain and cotton having an intermediate regain level.17 Dry wool fiber absorbs moisture up to about 35% of its dry weight in saturated air, whereas cotton can absorb around 24% and polyester below 1%.17 A previous study investigated the influence of sleepwear (cotton vs wool) and bedding type (polyester vs wool) on the sleep quality of healthy young participants.18 Although no effect on sleep of bedding type was observed, sleep onset latency (SOL) was significantly shortened when sleeping in wool sleepwear with less stage 3 sleep observed for wool than for cotton. However, the effects of fiber type on the sleep of older adults have not been studied.
The aims of this study were:
to determine if sleepwear fiber type (cotton, polyester or Merino wool) influences sleep quality for adults aged 50–70 years, at an ambient temperature of 30 ºC and a relative humidity (RH) of 50%; and,
to determine if there is an interaction effect on sleep quality between sleepwear fiber type and BMI (>25 vs ≤25 kg·m−2), age (>65 vs ≤65 years) and sleep self-ratings (PSQI >5 (poor sleepers) vs ≤5 (good sleepers)).
Materials and methods
Participants
Thirty-six healthy participants aged between 50 and 70 years with a mean and standard deviation (SD) of 60.0±6.2 years, a body mass index (BMI) of 25.6±4.1 kg·m−2 and mean Pittsburgh Sleep Quality Index (PSQI)19 of 4.4±2.6 completed four nights of study. The female participants (n=18) had a mean age of 59.8±6.7 years and BMI of 25.3±5.4 kg·m−2, while similar values for the male participants were (n=18) 60.2±5.9 years and a BMI of 25.8±2.3 kg·m−2. Participants with certain pre-existing medical conditions were excluded. These conditions were sleep disorders (insomnia, sleep apnea, periodic limb movement disorders, restless legs syndrome and bruxism), cardio-respiratory conditions (severe hypertension, cardiovascular diseases, respiratory infections and chronic obstructive pulmonary diseases), metabolic conditions (uncontrolled diabetes and metabolic syndrome), and psychiatric or neurological disorders (depression, dementia and Parkinson disease). Female participants with regular menstruation were tested on the follicular phase (between menstruation and ovulation) to minimize hormonal and temperature effects on sleep. Females who were on hormone replacement therapy were included. Individuals on nightshifts or medications/drugs (eg, anti-depressants, hypnotics, stimulants which interfere with sleep), or who smoked or had travelled across trans-meridian borders in the last 2 weeks were also excluded. Participants abstained from alcohol on the study days and from caffeinated beverages and vigorous exercise eight hours prior to their averaged bedtimes. Ethics approval for this study was granted by the University of Sydney Human Research Ethics Committee (Project no. 2012/562). Written informed consent was obtained from all participants prior to study commencement.
Procedure
Participants wore an Actiwatch 2 (Phillips-Respironics, Murryville, PA) on the non-dominant arm for a week, prior to study commencement, to assess their average bedtimes and wake times. Subjective sleep quality was assessed using PSQI. Eligible participants attended the sleep laboratory for PSG testing on four occasions: an adaptation night where participants were confirmed free of sleeping disorders, and three testing nights. Their height and body mass were recorded. On testing nights, participants slept in either cotton, polyester or wool sleepwear in a random order. Participants were blind to the type of sleepwear. Participants ate a standardized mixed macronutrient meal 4 hrs before their average bedtime. They changed into their sleepwear 2 hrs prior to bedtime, during which they had PSG electrodes attached in the sleep monitoring room, which recorded a temperature of ~25 °C and an RH of ~40%. The participants went to bed and woke up according to their averaged times, collected during 5–7 nights prior to the study by Actiwatch 2. Participants in their sleepwear were weighed at bedtime and on waking, and overnight urine was collected and measured (to the nearest 0.01 kg). These measurements were used in the estimation of whole body sweat evaporation loss and rate of loss (see Data and Statistical analysis).
Sleepwear and bedding
Cotton, polyester and Merino wool sleepwear knitted from singles yarn in single jersey structure, were finished clean, plain colored and visibly similar. Both the fabric mass per unit area (g·m−2) and thickness (mm) were taken into consideration in matching the fabrics.20,21 The lightest fabric, cotton, was also the thickest, while the heaviest fabric, polyester, was the thinnest, as shown in Table 1. Fabric thickness was prioritised as the characteristic to be most closely matched, with the largest difference, 0.08 mm, being between the cotton and polyester fabrics. This small difference was considered acceptable for the purposes of this study. All sleepwear was custom-tailored to be loose-fitting using the same pattern in long sleeves and long pants in four sizes (small, medium, large, and extra-large). Participants were allocated a size that was similar to that of their usual sizing in sleepwear. Conforming to cultural conventions, female participants wore cotton knickers, while male participants wore only sleepwear without underwear. Participants slept on a sheet but without a cover to avoid confounding effects arising from participants inadvertently kicking off the cover to achieve comfort. The bed comprised a king size innerspring mattress covered by a cotton underlay and cotton bedsheet.
Table 1.
Fabric characteristics of washed sleepwear
| Mass per unit area (g·m−2) | Thickness (mm) | Thermal Resistance (m2·K·W−1) | |
|---|---|---|---|
| Cotton | 140.0±0.0 | 0.57±0.03 | 0.030 |
| Polyester | 150.5±0.7 | 0.49±0.04 | 0.025 |
| Wool | 143.5±2.1 | 0.52±0.01 | 0.030 |
Note: Data presented as mean ± SD.
Ambient conditions
The temperatures and RH levels in the sleep monitoring room and the two bedrooms (both identically equipped and of similar size) were monitored continuously by means of iButtons (type DS1923; Maxim/Dallas Semiconductor Corporation) in each room. In the bedrooms, the temperatures were controlled by a wall mounted air conditioner (Email Air, Australia) and RH by a stand-alone humidifier/dehumidifier (Munters, Sweden) with a steam vaporizer (Vicks, USA). The ambient conditions of the bedrooms were independently verified using an Indoor Climate Analyzer - Type1213 (Brüel&Kjær, Denmark), which showed temperature and RH readings were consistent with the iButton readings. The air speed recorded (Brüel&Kjær, Denmark) over a two-hour period in the bedroom was low (below 0.04 m·s−1). Temporal changes in air speed would be expected to be minimal, given the constant readings obtained over the two hours in bedrooms that had no windows and had their doors shut throughout the study period. The radiant wall temperature was, as expected, similar to the set ambient room temperature. The ambient conditions in both bedrooms were 30.1±0.5 °C and 50.2±2.9% RH.
Measurements
PSG
Sleep parameters were measured using the Compumedics E-series or Grael Sleep system (Compumedics Australia Pty Ltd., Australia). Electroenceophalogram (EEG) electrode placement (C3/A2, O2/A1 and F3/A2) was conducted in accordance with the International 10–20 system. Electrooculogram, chin electromyogram (EMG) and electrocardiogram were continuously recorded. All electrode sites were referenced to the vertex (Cz), and a ground electrode was attached to the forehead (Fpz). The impedance of EEG recording electrodes was checked prior to data collection, and the threshold was <5 kΩ. On the adaptation night, left and right leg EMG, oxygen saturation, thoracic and abdominal breathing movements and airflow were also recorded to determine sleep disorders. PSG data were scored blind by two experienced scorers according to the American Academy of Sleep Medicine (AASM) guidelines.22 The sleep variables included SOL, TST, SE, wake after sleep onset (WASO), and the proportion of each sleep stage including non-rapid eye movement (NREM) sleep: stages 1 (N1), 2 (N2) and 3(N3), and REM sleep.
EEG arousal index (AI, number of arousals per hour (no. h−1)) was defined as an abrupt shift in EEG frequency that lasts between 0.5 and a maximum of 14.9 seconds.22 An EEG arousal that is longer than 15 seconds would be considered an awake epoch. A minimum of 10 seconds of intervening sleep between arousals was required. The scoring process for the AI was relatively time consuming and has been associated with high inter-scorer variability. The sleep fragmentation index (SFI) was also assessed in this study as in clinical practice. The SFI has previously been reported to be significantly correlated with the AI with a test-retest reproducibility of r=0.77. It was calculated as the sum of any sleep stage shift and the total number of awakenings, divided by TST (hours). A shift in sleep stage refers to a change from a higher to a lower stage. The number of sleep stage shifts was computed for the whole night sleep recording after manual sleep scoring. In REM sleep, a stage shift was defined as a shift to sleep stage 1.
Actigraphy
Actiwatch 2 (Phillips-Respironics, Murryville, PA) was placed on the non-dominant wrist. Actigraphic data were scored using Respironics Actiware v6.09 (Phillips-Respironics). Data were collected in 30 s epochs with the sensitivity set to the medium level. Rest intervals were manually set based on the timing of lights-out and lights-on in accordance with a previous study,23 and sleep variables were estimated by the Actiware software.
Sweat evaporation rate
Whole body sweat evaporation loss during the sleep period was calculated in the established manner24 from the loss of body mass during sleep according to the parameters of whole body mass while clothed in sleepwear and overnight urine volume, assuming a specific gravity of urine to be approximately 1.0. No corrections were made for respiratory ‘insensible’ water loss, or weight changes due to metabolism.25 Whole body sweat evaporation rate (WBSER) was calculated by dividing evaporation loss by total time in bed (in hours):
Subjective ratings on tactile sensations
On each test night, participants rated the tactile sensation of their sleepwear immediately after changing into the sleepwear (approximately 2.5 hrs before bedtime), at bedtime and on waking. Tactile sensations including the surface texture (“very soft” to “very rough”), prickliness, clamminess and clinginess of the sleepwear (“not at all” to “extremely”) were assessed on a five-point Likert scale.
Data and statistical analysis
Participants were categorized into one of two groups for each subgroup as follows:
BMI (as BMI<25 kg·m−2 (but ≥18.5 kg·m−2), and BMI≥25 kg·m−2); Age (Middle-age and Old age); and, PSQI (Good and Poor sleepers). The BMI cut-off of 25 was applied based on World Health Organization definition of overweight (World Health Organization, 1999). Age was grouped as Middle-age (50–64 years) and Old age (≥65 years).26,27 A PSQI global score of <5 was considered as good quality of sleep and a score ≥5 was classified as poor quality of sleep.19,24,25
A linear mixed model (SPSS v21; IBM Corporation, Armonk, NY, USA) was applied to compare the effects of sleepwear fiber types on WBSER and the following sleep variables: SOL; TST; percentage of TST of sleep stages N1, N2, N3, and REM; SE; WASO; AI; and SFI. In the linear mixed model the following fixed factors were used: sleepwear fiber type (categorical: cotton, wool and polyester), BMI (categorical), Age (categorical) and PSQI (categorical) to test main and interaction effects on sleep variables. Further post-hoc analysis on interaction results was performed using Fisher’s least significant difference for pairwise comparisons. Subjective ratings were analysed by means of the Kruskal-Wallis test, with the Mann-Whiney U test for post-hoc analysis (SPSS).
Results
Of the 36 participants, 13 had BMI<25 while 23 had BMI≥25 kg·m−2; 23 participants were Middle-age (50–64 years) while 13 were Old-age (65 years and above); and 20 participants were Good sleepers (PSQI <5) while 16 were Poor sleepers (PSQI ≥5, range 5–11).
Main effects on sleep of sleepwear type, BMI, age and PSQI
Sleepwear type
Table 2 shows mean ± SD values for all sleep variables for each type of sleepwear. Statistically significant sleepwear effects were observed for only SOL (p=0.044) and SFI (p=0.006). While on average cotton sleepwear had the highest and wool the lowest SOL, a post-hoc test with pairwise comparisons did not reveal any significant differences in SOL among the sleepwear types. SFI was significantly lower when sleeping in wool than in polyester (p=0.005) with no statistically significant difference between wool and cotton or between cotton and polyester (p>0.05) in the post-hoc pairwise comparisons.
Table 2.
Effect on sleep parameters of sleepwear fiber type
| Cotton | Polyester | Wool | p-value | |
|---|---|---|---|---|
| SOL (min) | 18.5±23.5 | 18.2±15.5 | 16.0±15.5 | 0.04 |
| REM sleep latency (min) | 82.5±34.2 | 88.9±46.7 | 82.6±49.0 | 0.33 |
| N1 (%) | 5.3±4.0 | 4.6±2.5 | 4.6±2.7 | 0.57 |
| N2 (%) | 58.6±9.0 | 57.5±8.6 | 57.8±8.0 | 0.70 |
| N3 (%) | 15.9±5.4 | 16.1±6.8 | 16.5±5.7 | 0.91 |
| REM sleep (%) | 20.2±5.7 | 21.5±6.3 | 21.1±6.1 | 0.58 |
| TST (min) | 363.4±56.0 | 364.2±62.6 | 373.1±60.4 | 0.30 |
| SE (%) | 76.2±11.0 | 76.4±12.4 | 78.4±12.6 | 0.32 |
| WASO (min) | 97.0±52.3 | 95.8±56.6 | 89.1±57.0 | 0.76 |
| AI (no.h−1) | 10.3±7.1 | 9.6±6.0 | 10.5±6.4 | 0.36 |
| SFI (no. h−1) | 13.3±5.8 | 13.7±4.4* | 12.1±4.2* | 0.01 |
Notes: Data presented as mean ± SD, N=36. *p<0.05 for difference between polyester and wool.
Bold values indicate significant sleepwear effect on SOL but there was no significant difference among sleepwear types in the post-hoc pairwise comparisons.
Abbreviations: SOL, sleep onset latency; REM, rapid eye movement; TST, total sleep time; N1(%), sleep stage 1 as a percentage of TST; N2(%), sleep stage 2 as a percentage of TST; N3(%), sleep stage 3 as a percentage of TST; SE, sleep efficiency; WASO, wake after sleep onset; AI, arousal index; SFI, sleep fragmentation index.
Subgroups of BMI, age and PSQI
Table 3 shows the effect on sleep parameters of sleepwear fiber type for the subgroups BMI, Age and PSQI. Participants with a BMI≥25 kg·m−2 had a statistically significantly higher AI, more N1% and less N3% than those with BMI<25 kg·m−2. The main effects for Age showed that the Old age group took significantly longer to fall asleep but had higher N3% than the Middle-age group. Significant PSQI main effects showed Poor sleepers had significantly higher N2% and SFI than Good sleepers.
Table 3.
Effect on sleep parameters of sleepwear fiber type for subgroup BMI, Age and PSQI
| BMI<25 (n=13) | BMI≥25 (n=23) | p-value | Middle-age (n=23) | Old age (n=13) | p-value | PSQI<5 (n=20) | PSQI≥5 (n=16) | p-value | |
|---|---|---|---|---|---|---|---|---|---|
| SOL (min) | 17.8±26.1 | 17.5±12.4 | 0.14 | 16.1±12.9 | 20.2±25.4 | 0.03 | 11.0±7.0 | 25.8±24.2 | 0.17 |
| REM sleep latency (min) | 83.3±36.9 | 85.4±47.0 | 0.84 | 86.4±46.5 | 81.6±38.0 | 0.92 | 71.1±33.7 | 101.6±48.5 | 0.07 |
| N1 (%) | 3.3±1.8 | 5.7±3.4 | 0.03 | 4.5±3.0 | 5.5±3.2 | 0.42 | 4.9±2.9 | 4.8±3.4 | 0.84 |
| N2 (%) | 57.8±8.1 | 58.1±8.7 | 0.35 | 59.1±8.1 | 56.0±8.8 | 0.05 | 56.0±8.2 | 60.5±8.2 | 0.01 |
| N3 (%) | 18.2±7.0 | 15.0±5.0 | 0.02 | 15.8±5.9 | 16.8±6.0 | 0.03 | 16.3±6.1 | 16.0±5.8 | 0.12 |
| REM sleep (%) | 20.7±4.8 | 21.1±6.6 | 0.87 | 20.6±6.2 | 21.4±5.7 | 0.87 | 22.7±5.4 | 18.8±6.1 | 0.05 |
| TST (min) | 381.7±62.6 | 358.6±56.1 | 0.31 | 364.4±63.6 | 371.3±51.4 | 0.71 | 379.4±46.1 | 351.4±70.0 | 0.56 |
| SE (%) | 78.2±10.4 | 76.3±12.7 | 0.88 | 77.2±13.5 | 76.6±8.7 | 0.15 | 81.0±9.7 | 71.9±12.6 | 0.23 |
| WASO (min) | 88.1±43.9 | 97.3±60.4 | 0.89 | 95.3±63.3 | 91.6±36.4 | 0.42 | 79.3±46.3 | 112.3±59.6 | 0.37 |
| AI (no./h) | 6.8±2.9 | 12.1±7.1 | 0.04 | 9.3±7.1 | 11.6±5.0 | 0.32 | 9.2±4.9 | 11.3±7.9 | 0.55 |
| SFI (no./h) | 11.2±2.8 | 14.1±5.5 | 0.09 | 12.2±5.0 | 14.6±4.2 | 0.32 | 11.4±3.8 | 15.1±5.2 | 0.01 |
Notes: Data presented as mean ± SD.
Bold values indicate significant BMI, Age and PSQI effect on sleep variables.
Abbreviations: BMI, body mass index; PSQI, Pittsburgh Sleep Quality Index; SOL, sleep onset latency; REM, rapid eye movement; TST, total sleep time; N1(%), sleep stage 1 as a percentage of TST; N2(%), sleep stage 2 as a percentage of TST; N3(%), sleep stage 3 as a percentage of TST; SE, sleep efficiency; WASO, wake after sleep onset; AI, arousal index; SFI, sleep fragmentation index.
Interaction effects on sleep between sleepwear and BMI, age or PSQI
A significant interaction between sleepwear fiber type and Age group was observed for SOL (p=0.001), as shown in Figure 1A. Further post-hoc testing with pairwise comparisons revealed that within the Old age group, SOL was significantly reduced when sleeping in wool compared to sleeping in cotton (p=0.011) or polyester (p=0.011). In addition, when both Age groups slept in cotton sleepwear, Middle-aged fell asleep significantly quicker than Old age (p=0.008), as shown in Figure 1A.
Figure 1.

Interaction effects between sleepwear and Age/PSQI on sleep variables.
Notes: (A) Sleep onset latency, between sleepwear and Age; (B) Wake after sleep onset, between sleepwear and PSQI; (C) REM sleep latency, between sleepwear and PSQI. Error bars with standard deviations are displayed. Comparison between sleepwear conditions indicated by *p<0.05 between cotton and wool; †p<0.05 between polyester and wool; ±p<0.05 between cotton and polyester; α, p<0.05 between groups.
Abbreviations: PSQI, Pittsburgh Sleep Quality Index; REM, rapid eye movement.
Significant interactions between sleepwear and PSQI group were found for WASO (p=0.049) and REM sleep latency (p=0.038) as shown in Figure 1B and C. In the comparison of sleepwear types, Poor sleepers had significantly reduced WASO in wool than in cotton (p=0.047). In the comparison between Good and Poor sleepers, Poor sleepers had significantly more wake time during the sleep period (WASO) than Good sleepers when sleeping in cotton (p=0.010), as shown in Figure 1B. Additionally, REM sleep latency was significantly longer when Poor sleepers slept in polyester than either in cotton (p=0.037) or in wool (p=0.036). When participants slept in polyester, Poor sleepers had significantly higher REM sleep latency than Good sleepers (p=0.010), as shown in Figure 1C. There were no significant differences in any sleep variables between sleepwear types for the BMI sub-group.
Whole body sweat evaporation rate (WBSER)
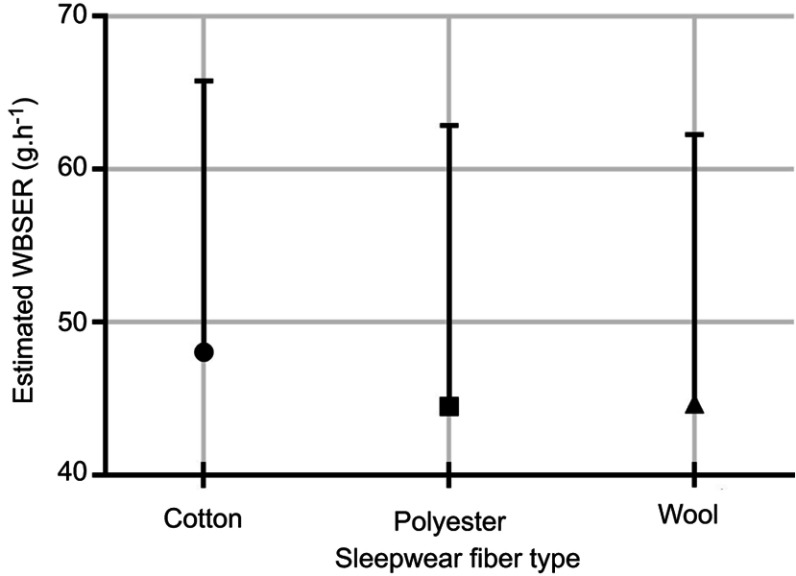
WBSER was 48.0±17.7 g·h−1 when sleeping in cotton compared to wool (44.7±17.6 g·h−1) and polyester (44.5±18.4 g·h−1), p=0.068 (Figure 2). There were no statistically significantly different differences among the three fiber types in WBSER.
Figure 2.
Estimated whole body sweat evaporation rate (WBSER) (g·h−1).
Notes: Error bars with standard deviations are displayed. The equation used for the calculation of WBSER can be found in the section Data and Statistical Analysis.
Subjective ratings
Participants reported average ratings between 1 (“Not at all”) and 2 (“Slightly”) for perceived prickliness, clamminess and clinginess for all fabrics at each evaluation point in the study. The average ratings for surface texture were between 1 (“Very soft”) and 2 (“Soft”) for the polyester fabric and between 2 and 3 (“Neutral”) for the cotton and wool fabrics, indicating that the polyester fabric was slightly smoother than the cotton and wool fabrics. Though small, there were statistically significantly different tactile ratings between sleepwear fiber types as shown in Table 4. The post-hoc test with Mann-Whitney U showed that wool was perceived to be slightly (0.4 units), but statistically significantly, pricklier than the other two fabrics (p=0.004) at all three time points of measurement. Participants rated cotton sleepwear immediately after donning as less clingy (0.25 units) than polyester (p=0.021) and wool (p=0.021). They rated wool significantly rougher (0.47 units) than polyester (p=0.037) at bedtime, and both cotton and wool were rated significantly rougher (0.42 units in each case) than polyester on waking (p=0.031, p=0.032 respectively) (refer to Table 4). No significantly different average ratings were observed for “clamminess.”
Table 4.
Subjective ratings on tactile sensation for each sleepwear
| Cotton | Polyester | Wool | p-value | ||
|---|---|---|---|---|---|
| Surface texture | After donning | 2.08±0.73 | 1.75±0.73 | 2.22±0.96 | 0.065 |
| At bedtime | 2.19±0.62 | 1.81±0.75 | 2.28±0.94† | 0.037 | |
| On waking | 2.36±0.80 | 1.94±0.79†‡ | 2.36±0.87 | 0.045 | |
| Prickliness | After donning | 1.17±0.45 | 1.17±0.45 | 1.64±0.90*† | 0.002 |
| At bedtime | 1.28±0.57 | 1.28±0.62 | 1.64±0.83*† | 0.024 | |
| On waking | 1.33±0.76 | 1.36±0.68 | 1.72±0.85*† | 0.022 | |
| Clamminess | After donning | 1.13±0.48 | 1.19±0.62 | 1.16±0.56 | 0.912 |
| At bedtime | 1.28±0.66 | 1.44±0.84 | 1.22±0.54 | 0.454 | |
| On waking | 1.42±0.77 | 1.64±0.83 | 1.53±0.81 | 0.339 | |
| Clinginess | After donning | 1.11±0.40‡* | 1.36±0.64 | 1.36±0.59 | 0.043 |
| At bedtime | 1.19±0.47 | 1.42±0.84 | 1.44±0.65 | 0.182 | |
| On waking | 1.42±0.73 | 1.67±0.96 | 1.61±0.96 | 0.456 |
Notes: Data presented as mean ± SD, N=36. Tactile sensations included surface texture (1=“very soft” to 5=“very rough”), prickliness, clamminess and clinginess of the sleepwear (1=“not at all” to 5=“extremely”) and were assessed on a five-point Likert scale. Bold values indicate significant sleepwear effect on subjective ratings.*p<0.05 for difference between cotton and wool; †p<0.05 for difference between polyester and wool; ‡p<0.05 for difference between cotton and polyester.
Discussion
The study compared the effect on sleep quality of sleepwear fiber type (cotton, polyester and wool) in warm conditions (30 ºC and 50% RH) for healthy participants aged 50–70 years old.
Main effects on sleep of sleepwear type, BMI, age and PSQI
Statistically significant differences among sleepwear type were observed in two of the 11 sleep quality parameters, SOL and SFI, as illustrated in Table 2.
Sleepwear type
Sleep onset latency
The shortest sleep onset duration was observed for wool sleepwear (16.0 mins) followed in order by polyester (18.2 mins) and cotton (18.5 mins), although post-hoc analysis showed that the differences between each pair of fiber types were statistically non-significant due to the high values of SD compared to the mean values (Table 2).
It is known that sleep onset initiation is associated with a fall in core body temperature,28 and heat dissipation via peripheral vasodilation reflected in a rise in the distal skin temperature.29 Thus, it would be expected that participants who dissipate heat at a faster rate should fall asleep more quickly. Two factors may explain the ease of sleep onset when sleeping in wool and cotton compared to polyester sleepwear: the physical transition from the sleep monitoring room to the bedroom, and the fiber properties of the sleepwear. In this study, the participants stayed in the monitoring room (at 25 °C and 40% RH) before entering the warm bedroom (30 °C and 50% RH). This process, although unusual in a “real life” situation, permitted an abrupt transition from a warm to hot condition. There may have been marginally more cool air from the monitoring room trapped within the wool and cotton fabrics compared to polyester fabrics due to the crimped nature, three-dimensional waviness providing bulkiness (loft), and rough scaly surface of wool fibers17 and the uneven twisted structure of cotton fibers17 compared to the smooth surface of both polyester fibers and fabrics.17 Also, a recently published study related to the breathability of fabrics has highlighted the differing dynamic moisture buffering potential of cotton, polyester and wool fabrics.30 Values of the dynamic moisture buffering potential quoted for matched lightweight single jersey fabrics very similar to those used in this study were 0.6 KJ·m−2, 6.9 KJ·m−2, and 9.9 KJ·m−2 for polyester, cotton and wool fabrics respectively. These results show the relatively poor moisture buffering of polyester fibers compared to the more hygroscopic natural fibers, cotton and wool, and also quantify the approximately 30% higher value for wool compared to cotton. Thus, during this short transition from bedtime to sleep onset (average 18 mins, Table 2), it is possible that the participants in the wool or cotton sleepwear were relatively well buffered from the higher temperature and RH in the sleeping room compared to when they were in the polyester sleepwear.
Sleep Fragmentation Index, SFI
The lowest value of SFI was observed for wool followed by cotton and polyester, with a significant difference observed between wool and polyester sleepwear in the pairwise comparisons. Again, wool sleepwear was associated with the higher sleep quality with an SFI of 12.1 h−1 compared with 13.3 h−1 and 13.7 h−1 for the cotton and polyester sleepwear, respectively. SFI reflected stage shifts plus awakenings. The higher rates of SFI suggested a greater thermal stress when sleeping in cotton or polyester sleepwear than in wool sleepwear, consistent with reports of increased thermal stress when sleeping under hot humid conditions.24 Thus, the lower SFI when sleeping in wool would suggest lower thermal stress that may be linked to the beneficial moisture transfer and wicking properties of wool.31 In this study, WBSER was not statistically significantly different among the sleepwear. Thus no explanation is supported about the link between WBSER and thermal stress experienced by the participants (Figure 2). We were also unable to confirm respiratory “insensible” loss or changes in metabolic rates, since any measurements during the sleep period may interfere with sleep per se or would require specialized equipment which was unavailable. In addition, individual WBSER response to sleeping under warm conditions differed between subjects; Sagot and colleagues reported that not all subjects sweated under sleeping conditions of 30 °C where participants were not covered.32 The observation in this study differed from earlier findings where greater sweat loss and higher microclimate relative humidity were observed for sleeping in polyester compared to wool31 or cotton.33 A further study showed an initial rapid increase in sweating for both wool and polyester, although the subsequent rate decreased for wool due to the higher moisture absorption rate of wool31 compared to the slower moisture transfer capacity of polyester.34,35
Other indicators of sleep fragmentation are the AI and WASO. Non-significant changes were observed for the AI between fiber types. This observation may be linked to the greater variability observed for AI compared to that for SFI (Table 2). Haba-Rubio et al reported that the scoring process for AI was associated with high inter-scorer variability, whereas the SFI had a good test-retest reproducibility and that SFI was significantly correlated with AI.
BMI, age and PSQI
The findings in this study, with respect to the BMI, Age and PSQI factors generally conform to published literature. Participants with BMI≥25 kg·m−2 had poorer sleep than those with BMI<25 kg·m−2 as shown by a higher N1, lower N3 and a higher AI. A previous study has shown that a low amount of slow wave sleep (N3) was associated with high BMI in insomniacs.36 The Old age subgroup took longer to fall asleep as indicated by a longer SOL than the Middle-age subgroup. This result was consistent with data found in a meta-analysis.2 However, unexpectedly this subgroup recorded more N3 than the Middle-age subgroup, indicating better sleep quality using this parameter. Poor sleepers had higher SFI and less REM sleep than Good sleepers indicating that the Poor sleepers had lower sleep quality than the Good sleepers in this trial. This finding is consistent with previous studies that reported less REM sleep time was associated with a higher rectal temperature in poor sleepers.37,38
Interaction effects on sleep quality between sleepwear and BMI, age or PSQI
Several statistically significant differences were observed in the interactions between sleepwear fiber type and two of the three subgroups, Age and PSQI, as shown in Figure 1. When examined according to the Age factor, the Old age subgroup showed significantly lower SOL in wool than in polyester or cotton (Figure 1A). Thus the older participants (≥65 years) in this cohort fell asleep within 12 mins on average in wool compared to 22 mins or 27 mins for polyester or cotton, respectively. As noted in the earlier discussion of the SOL results, the different thermal insulation and moisture management properties of the three fiber types may have contributed to the ease of falling asleep in wool compared with the other fiber types. The SOL findings for sleepwear between the Old age and Middle-age group may have significant, practical implications, since this Old age group, who generally took longer to fall asleep than the Middle-age group, may have preferentially benefitted from wearing wool sleepwear.
There was also an indication that Poor sleepers benefitted from wool sleepwear over the other fiber types. The lowest WASO in Poor sleepers was observed for wool (90 mins) with a statistically significant difference between wool and cotton (116 mins), but no significant difference between wool and polyester (99 mins) as shown in Figure 1B. These differences in sleep quality may be related to the superior moisture management of the wool sleepwear compared to the cotton and polyester sleepwear, which would assist heat dissipation. Even though cotton and wool are both natural fibers they differ greatly in their hygroscopicity. Dry wool fibers absorb moisture up to about 35% of its dry weight in saturated air, whereas cotton can absorb around 24%.17 Polyester, an oil-based synthetic fiber, has a relatively low ability to absorb and release water vapour quickly with a fiber hygroscopicity39 of 8–9%.40 A previous study has shown that Poor sleepers had more wake time when they had a higher core body temperature.41
Poor sleepers also had significantly shorter latency to REM sleep when sleeping in wool (88 mins) and cotton (92 mins) than sleeping in polyester (111 mins). Given that REM sleep latency was increased at high ambient temperatures,42 the shortened latency in Poor sleepers would suggest that sleeping in wool favored an early appearance of the first REM sleep episode that may be related to fiber properties of wool mentioned earlier. Whilst the relationship of this result to sleep quality is unclear, a reduction in the time to the first REM sleep episode may also be linked to increased REM sleep pressure.43
Perception of tactile sensations
The average ratings for perceived prickliness, clamminess and clinginess for all sleepwear at each evaluation point in the study were between “Not at all” and “Slightly”, indicating that all fabrics were suitable for sleepwear. Participants rated the average surface texture of the polyester sleepwear as between “Very Soft” and “Soft” while the cotton and wool sleepwear was rated on average to be between “Soft” and “Neutral”.
Participants perceived the wool sleepwear to be slightly pricklier than the cotton and polyester sleepwear. The prickle sensation in textiles has been shown to be related to the incidence of stiff fibers on the product’s surface rather than to fiber type.44 For wool fabrics the occurrence of coarse surface fibers has been shown to be related to the mean and variation in diameter of the wool fibers within the fabric.45,46 Moreover, participants reported wool felt pricklier and rougher than the other sleepwear at bedtime and on waking on exposure to a warm condition. This observation is supported by previous literature that the sensations of prickliness and roughness were increased with warmth.47,48
It appears that there is a dissociation between perceived tactile sensations (prickliness, roughness or clinginess) during the waking period and objectively measured sleep. Sleeping in wool promoted sleep onset with the least sleep fragmentation compared to cotton or polyester sleepwear.
The cotton sleepwear was perceived to be slightly less clingy than the other sleepwear after the participants changed into their sleepwear. The subjective feeling of clinginess may be caused by a build-up of static electricity between the skin surface and the fiber.49 There was no difference in the clinginess between polyester and wool even though electrical resistance has been shown to be highest for polyester, followed by wool, then cotton at a constant RH of 35%.49,50
The study was designed to blind the sleepwear fiber type. Nonetheless, participants may detect differences in sleepwear fiber type (cotton, polyester or wool) by the sense of touch, which could consciously or subconsciously affect their attitude and potentially their sleep quality. However, participants did not provide any feedback about their prediction of fiber types.
Summary and conclusion
This study compared the effect on sleep quality of sleepwear fiber type (cotton, polyester and wool) in warm conditions (30 ºC and 50% RH) for healthy participants aged 50–70 years old. As would be expected from the literature2,36 higher BMI, older and poorer sleepers were found to have poorer sleep quality in hot, moist conditions than lower BMI, younger and better sleepers in this study. Sleeping in wool compared to sleeping in polyester resulted in less fragmented sleep for all participants. Sleeping in wool compared to polyester and cotton promoted a quicker sleep onset (SOL) in participants ≥65 years. Poor sleepers had less wake time during the sleep period (WASO) in wool than in cotton sleepwear and had a more delayed REM sleep latency in polyester than in cotton or wool sleepwear. Non-significant differences between cotton and polyester were observed for all sleep variables apart from that observed in Poor sleepers. It is suggested that the superior moisture buffering and moisture management properties of wool compared to cotton and polyester may be responsible for the different sleep outcomes observed in this study.
In conclusion, wool sleepwear was shown to promote better sleep in warm ambient conditions, particularly for adults aged 65 years and older and for poor sleepers. Thus, subgroups known to experience poorer sleep quality may enjoy an extra benefit from using wool sleepwear. Judicious selection of sleepwear fiber type may therefore offer an alternative, healthy and natural strategy for older adults sleeping under warm ambient conditions.51–54
Future studies could investigate the effects on sleep quality of sleepwear fiber type in, for example, menopausal women who often experience hot flashes and disturbed sleep,51,52 shift workers who have disrupted circadian timing,53 in patients with hypothyroidism who have low metabolic rates or in nursing home residents who often experience inefficient heating and cooling systems.54
Disclosure
This study was supported by Australian Wool Innovation Ltd (AWI) which is funded by Australian woolgrowers and by the Australian Government. CMC received funding from AWI and MS was employed under that funding. TM and AI are employees of AWI. The authors report no other conflicts of interest in this work.
References
- 1.Cooke JR, Ancoli-Israel S. Normal and abnormal sleep in the elderly In: Vinken PJ, Bruyn GW, editors. Handbook of Clinical Neurology. Elsevier B.V. Amsterdam, The Netherlands. Vol. 98; 2011:653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ohayon MM, Carskadon MA, Guilleminault G, Vitiello MV. Meta-analysis of quantitative sleep parameters from chidlhood to old age in healthy individuals: developing normative sleep-values across the human lifespan. Sleep. 2004;27(7):1255–1273. doi: 10.1093/sleep/27.7.1255 [DOI] [PubMed] [Google Scholar]
- 3.Okamoto-Mizuno K, Mizuno K. Effects of thermal environment on sleep and circadian rhythm. J Physiol Anthropol. 2012;31(1):14. doi: 10.1186/1880-6805-31-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kenny GP, Yardley J, Brown C, Sigal RJ, Jay O. Heat stress in older individuals and patients with common chronic diseases. Can Med Assoc J. 2010;182(10):1053–1060. doi: 10.1503/cmaj.081050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Havenith G, Inoue Y, Luttikholt V, Kenney WL. Age predicts cardiovascular, but not thermoregulatory, responses to humid heat stress. Eur J Appl Physiol Occup Physiol. 1995;70(1):88–96. [DOI] [PubMed] [Google Scholar]
- 6.Havenith G. Temperature regulation and technology. Gerontechnology. 2001;1(1):41–49. doi: 10.4017/gt.2001.01.01.004.00 [DOI] [Google Scholar]
- 7.Collins K, Cowen T. Disorders of the auto-nomic nervous system In: Tallis R, Fillit H, Brocklehurs JC, editors. Geriatric Medicine and Gerontology. Edinburgh. Churchill Livingstone; 1992; 539-563. [Google Scholar]
- 8.Inoue Y. Longitudinal effects of age on heat-activated sweat gland density and output in healthy active older men. Eur J Appl Physiol Occup Physiol. 1996;74(1):72–77. [DOI] [PubMed] [Google Scholar]
- 9.Okamoto-Mizuno K, Tsuzuki K. Effects of season on sleep and skin temperature in the elderly. Int J Biometeorol. 2010;54(4):401–409. doi: 10.1007/s00484-009-0291-7 [DOI] [PubMed] [Google Scholar]
- 10.Okamoto-Mizuno K, Tsuzuki K, Mizuno K. Effects of mild heat exposure on sleep stages and body temperature in older men. Int J Biometeorol. 2004;49:32–36. doi: 10.1007/s00484-004-0209-3 [DOI] [PubMed] [Google Scholar]
- 11.Saman W, Boland J, Pullen S, et al. A Framework for Adaptation of Australian Households to Heat Waves. National Climate Change Adaptation Research Facility. Gold Coast, QLD; 2013. [Google Scholar]
- 12.McMichael AJ, Woodruff RE, Hales S. Climate change and human health: present and future risks. Lancet. 2006;367(9513):859–869. doi: 10.1016/S0140-6736(06)68079-3 [DOI] [PubMed] [Google Scholar]
- 13.Astrom DO, Forsberg B, Rocklov J. Heat wave impact on morbidity and mortality in the elderly population: a review of recent studies. Maturitas. 2011;69(2):99–105. doi: 10.1016/j.maturitas.2011.03.008 [DOI] [PubMed] [Google Scholar]
- 14.Ito N, Yabe T, Nagai T, Oikawa T, Yamada H, Hanawa T. A possible mechanism underlying an antidepressive-like effect of Kososan, a Kampo medicine, via the hypothalamic orexinergic system in the stress-induced depression-like model mice. Biol Pharm Bull. 2009;32(10):1716–1722. doi: 10.1248/bpb.32.1716 [DOI] [PubMed] [Google Scholar]
- 15.Rees WH Physical factors determining the comfort performance of textiles. Paper presented at: Shirly Institute 3rd Seminar; 1971; Manchester. [Google Scholar]
- 16.Holmer I. Heat exchange and thermal insulation compared in woollen and nylon garments during wear trials. Text Res J. 1985;55:511–518. doi: 10.1177/004051758505500901 [DOI] [Google Scholar]
- 17.Morton WE, Hearle JWS. Physical Properties of Textile Fibres. Manchester: Textile Institute; 1986. [Google Scholar]
- 18.Shin M, Halaki M, Swan P, Ireland AH, Chow CM. The effects of fabric for sleepwear and bedding on sleep at ambient temperatures of 17 c and 22 c. Nat Sci Sleep. 2016;8:121. doi: 10.2147/NSS.S100271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buyssee DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. [DOI] [PubMed] [Google Scholar]
- 20.International Organization for Standardization. ISO 3801: 1977: Textiles-Woven Fabrics-Determination of Mass per Unit Length and Mass per Unit Area. Geneva: International Organization for Standardization; 1977. [Google Scholar]
- 21.International Organization for Standardization. ISO 5084: 1996: Textiles-Determination of Thickness of Textiles and Textile Products. Geneva: International Organization for Standardization; 1996. [Google Scholar]
- 22.Iber C, Ancoli-Israel S, Chesson A, Quan SF. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology, and Technical Specification. 1st ed. Illinois: American Academy of Sleep Medicine; 2007. [Google Scholar]
- 23.Haba-Rubio J, Ibanez V, Sforza E. An alternative measure of sleep fragmentation in clinical practice: the sleep fragmentation index. Sleep Med. 2004;5(6):577–581. doi: 10.1016/j.sleep.2004.06.007 [DOI] [PubMed] [Google Scholar]
- 24.Okamoto-Mizuno K, Mizuno K, Michie S, Maeda A, Iizuka S. Effects of humid heat exposure on human sleep stages and body temperature. Sleep. 1999;22:767–773. [PubMed] [Google Scholar]
- 25.Henane R, Buguet A, Roussel B, Bittel J. Variations in evaporation and body temperatures during sleep in man. J Appl Physiol Respir Environ Exerc Physiol. 1977;42(1):50–55. doi: 10.1152/jappl.1977.42.1.50 [DOI] [PubMed] [Google Scholar]
- 26.Prineas RJ, Le A, Soliman EZ, et al. United States national prevalence of electrocardiographic abnormalities in black and white middle-age (45-to 64-year) and older (≥65-year) adults (from the reasons for geographic and racial differences in stroke study). Am J Cardiol. 2012;109(8):1223–1228. doi: 10.1016/j.amjcard.2011.11.061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fang J, Wheaton AG, Keenan NL, Greenlund KJ, Perry GS, Croft JB. Association of sleep duration and hypertension among US adults varies by age and sex. Am J Hypertens. 2012;25(3):335–341. doi: 10.1038/ajh.2011.201 [DOI] [PubMed] [Google Scholar]
- 28.Krauchi K, Wirz-Justice A. Circadian rhythm of heat production, heart rate, and skin and core temperature under unmasking condtions in men. Am J Physiol. 1994;267(3):R819–R826. doi: 10.1152/ajpregu.1994.267.3.R819 [DOI] [PubMed] [Google Scholar]
- 29.Krauchi K, Cajochen C, Werth E, Wirz-Justice A. Functional link between distal vasodilation and sleep-onset latency? Am J Physiol Regul Integr Comp Physiol. 2000;278(3):R741–R748. doi: 10.1152/ajpregu.2000.278.3.R741 [DOI] [PubMed] [Google Scholar]
- 30.Naylor GR. Measurement of the dynamic moisture buffering potential of fabrics. Text Res J. 2019;89(5):739–747. doi: 10.1177/0040517518755784 [DOI] [Google Scholar]
- 31.Li Y, Holcombe BV, Apcar F. Moisture buffering behavior of hygroscopic fabric during wear. Text Res J. 1992;62(11):619–627. doi: 10.1177/004051759206201101 [DOI] [Google Scholar]
- 32.Sagot JC, Amoros C, Candas V, Libert JP. Sweating responses and body temperatures during nocturnal sleep in humans. Am J Physiol. 1987;252:R462–R470. doi: 10.1152/ajpregu.1987.252.3.R462 [DOI] [PubMed] [Google Scholar]
- 33.Ha M, Tokura H, Yamashita Y. Effect of two kinds of clothing made from hydrophobic and hydrophilic fabrics on local sweating rates at an ambient temperature of 37°C. Ergonomics. 1995;38:1445–1455. doi: 10.1080/00140139508925201 [DOI] [PubMed] [Google Scholar]
- 34.Behmann FW. Influence of the sorption properties of clothing on sweat loss and the subjective feeling of sweating. Appl Polym Symp. 1971;18:477–482. [Google Scholar]
- 35.Barnes JC, Holcombe BV. Moisture sorption and transport in clothing during wear. Text Res J. 1996;66(12):777–786. [Google Scholar]
- 36.Huang L, Zhou J, Sun Y, et al. Polysomnographically determined sleep and body mass index in patients with insomnia. Psychiatry Res. 2013;209(3):540–544. doi: 10.1016/j.psychres.2012.12.012 [DOI] [PubMed] [Google Scholar]
- 37.Monroe LJ. Psychological and physiological differences between good and poor sleepers. J Abnorm Psychol. 1967;72(3):255. doi: 10.1037/h0024563 [DOI] [PubMed] [Google Scholar]
- 38.Ogawa T, Satoh T, Takagi K. Sweating during night sleep. Jpn J Physiol. 1967;17:135–148. [DOI] [PubMed] [Google Scholar]
- 39.Li Y, Plante AM, Holcombe BV. Fiber hygroscopicity and perceptions of dampness. Part II: physical mechanisms. Text Res J. 1995;65(6):316–324. doi: 10.1177/004051759506500602 [DOI] [Google Scholar]
- 40.Zimniewska M, Huber J, Krucinska I, Torlinska T, Kozlowski R. The influence of clothes made from natural and synthetic fibres on the activity of the motor units in selected muscles in the forearm-preliminary studies. Fibres Text East Eur. 2002;10(4):55–59. [Google Scholar]
- 41.Adam K, Tomeny M, Oswald I. Physiological and psychological differences between good and poor sleepers. J Psychiatr Res. 1986;20(4):301–316. [DOI] [PubMed] [Google Scholar]
- 42.Haskell E, Palca J, Walker J, Berger R, Heller H. The influence of ambient temperature on electrophysiological sleep in humans. Sleep Res. 1978;7:169. [Google Scholar]
- 43.Vogel GW, Vogel F, McAbee RS, Thurmond AJ. Improvement of depression by REM sleep deprivation. New findings and a theory. Arch Gen Psychiatry. 1980;37(3):247–253. doi: 10.1001/archpsyc.1980.01780160017001 [DOI] [PubMed] [Google Scholar]
- 44.Garnsworthy R, Gully R, Kenins P, Mayfield R, Westerman R. Identification of the physical stimulus and the neural basis of fabric-evoked prickle. J Neurophysiol. 1988;59(4):1083–1097. doi: 10.1152/jn.1988.59.4.1083 [DOI] [PubMed] [Google Scholar]
- 45.Naylor G, Veitch C, Mayfield RJ, Kettlewell R. Fabric-evoked prickle. Text Res J. 1992;62(8):487–493. doi: 10.1177/004051759206200809 [DOI] [Google Scholar]
- 46.Naylor G, Phillips D. Fabric-evoked prickle in worsted spun single jersey fabrics part II: the role of fiber length, yarn count, and fabric cover factor. Text Res J. 1997;67(5):354–358. doi: 10.1177/004051759706700508 [DOI] [Google Scholar]
- 47.Gwosdow A, Stevens J, Berglund L, Stolwijk J. Skin friction and fabric sensations in neutral and warm environments. Text Res J. 1986;56(9):574–580. doi: 10.1177/004051758605600909 [DOI] [Google Scholar]
- 48.Kenins P. Influence of fiber type and moisture on measured fabric-to-skin friction. Text Res J. 1994;64(12):722–728. doi: 10.1177/004051759406401204 [DOI] [Google Scholar]
- 49.Ballou J. Static electricity in textiles. Text Res J. 1954;24(2):146–155. doi: 10.1177/004051755402400209 [DOI] [Google Scholar]
- 50.Asanovic KA, Mihajlidi TA, Milosavljevic SV, Cerovic DD, Dojcilovic JR. Investigation of the electrical behavior of some textile materials. J Electrostat. 2007;65(3):162–167. doi: 10.1016/j.elstat.2006.07.008 [DOI] [Google Scholar]
- 51.Freedman RR, Roehrs TA. Effects of REM sleep and ambient temperature on hot flash-induced sleep disturbance. Menopause. 2006;13(4):576–583. doi: 10.1097/01.gme.0000227398.53192.bc [DOI] [PubMed] [Google Scholar]
- 52.Thurston RC, Blumenthal JA, Babyak MA, Sherwood A. Association between hot flashes, sleep complaints, and psychological functioning among healthy menopausal women. Int J Behav Med. 2006;13(2):163–172. doi: 10.1207/s15327558ijbm1302_8 [DOI] [PubMed] [Google Scholar]
- 53.Akerstedt T. Shift work and disturbed sleep/wakefulness. Occup Med (Chic Ill). 2003;53(2):89–94. doi: 10.1093/occmed/kqg046 [DOI] [PubMed] [Google Scholar]
- 54.Tartarini F, Cooper P, Fleming R. Thermal environment and thermal sensations of occupants of nursing homes: a field study. Procedia Eng. 2017;180:373–382. doi: 10.1016/j.proeng.2017.04.196 [DOI] [Google Scholar]