Abstract
Background
Mobile accelerometry is a powerful and promising option to capture long-term changes in gait in both clinical and real-world scenarios. Increasingly, gait parameters have demonstrated their value as clinical outcome parameters, but validation of these parameters in elderly patients is still limited.
Objective
The aim of this study was to implement a validation framework appropriate for elderly patients and representative of real-world settings, and to use this framework to test and improve algorithms for mobile accelerometry data in an orthogeriatric population.
Methods
Twenty elderly subjects wearing a 3D-accelerometer completed a parcours imitating a real-world scenario. High-definition video and mobile reference speed capture served to validate different algorithms.
Results
Particularly at slow gait speeds, relevant improvements in accuracy have been achieved. Compared to the reference the deviation was less than 1% in step detection and less than 0.05 m/s in gait speed measurements, even for slow walking subjects (< 0.8 m/s).
Conclusion
With the described setup, algorithms for step and gait speed detection have successfully been validated in an elderly population and demonstrated to have improved performance versus previously published algorithms. These results are promising that long-term and/or real-world measurements are possible with an acceptable accuracy even in elderly frail patients with slow gait speeds.
Introduction
Independence, mobility and physical activity are important factors for the health of orthogeriatric patients, especially in existing osteoporosis. Treatment of orthogeriatric patients aims to achieve satisfactory mobility and pain relief with surgical or non-surgical treatment methods [1]. In the field of musculoskeletal research, physical activity is a parameter directly influenced by various treatment options and is increasingly recognised as an important outcome measure [2,3].
Gait speed is one possible parameter to describe physical functional ability of patients. It has been used in the evaluation of multiple sclerosis and other neurological diseases [4] to objectively measure physical health status, and has been shown to be prognostic of increased risk of mortality [5]. In practice, gait speed is often measured in controlled environments as part of the Short Physical Performance Battery or other clinical procedures like the 6-minute walk test [6,7]. These tests are commonly used, but they only capture specific, short periods of time and do not quantify the usual, real-world gait speed [8]. Partially, also standardized questionnaires are used to conclude about the mobility of patients. Multiple studies showed that there is no correlation between a questionnaire and the measurement of physical activity in patients. Patients significantly overestimated their daily activity and walking time [9,10]. But only with reliable information about real-life walking behaviour, conclusions can be drawn about how different treatments influence the mobility of patients and whether mobility parameters are relevant for the long-term outcome of patients.
Elderly people or patients with slow or impaired real-world gait speed, typical orthogeriatric patients, have not been addressed so far, despite the relevance of gait speed to management and treatment of those patients. In this group of patients, the gait pattern is often more difficult to record and associated with high technical requirements due to the physiological peculiarities of ageing. Due to this, the accuracy of the detection is limited, especially with slow gait speed [11].
Accelerometry is a frequent component of modern portable devices and various activity parameters can be calculated with the help of specific algorithms. High-resolution accelerometry (100 Hz) is a simple and robust technique, and can provide parameters like step count, activity count or caloric expenditure [12]. The assessment of gait speed from accelerometry data is technically challenging and requires validation in the intended patient population, for example Multiple Sclerosis [13]. In addition, a reliable recording of step count is also possible, which is a generally understandable measure of the physical activity [14].
The aim of this study is to improve and validate continuous measurements of mobility in an orthogeriatric population using accelerometry data for real-world gait speed estimation. Simultaneous assessment of reference speed in a real-life walking parcours, which simulates real-world situations, is used to improve performance of step detection and real-world gait speed estimation algorithms for application in capturing real-world gait speed of elderly, slow-walking patients.
Methods
The study was approved by the local ethical committee (Ref. 627–16) and written consent was obtained by every subject.
For this study, 20 elderly subjects without walking aids or current gait impairment due to neurological disease or acute injury, were recruited from an orthogeriatric population suffering osteoporosis.
The subjects were asked to walk along a gait course (“parcours”) which was specifically designed to include real-world environments and scenarios and included both indoor and outdoor sections. The goal was to replicate everyday life as closely as possible, the parcours therefore excludes the motivational and other psychological aspects that are usually used during gait tests in a fully controlled clinical environment.
Subjects started their walk in a hallway of the hospital, at the end of which they reached a staircase with 23 steps descending to reach the lobby of the clinic. Crossing the lobby, the subjects went outdoors, where they walked down a pathway towards a road. On their way to the road, subjects walked down a ramp to reach the pavement and ascended 5 steps to reach the pathway back to the clinic. From here on the subjects turned and walked the same path back to the starting point.
While performing the parcours, the subjects wore an actibelt®; a tri-axial accelerometer with a sampling frequency of 100 Hz, placed inside the belt buckle, and fixed around the waist by either a leather or elasticated belt, in order to be both discreet and located close to the subject’s centre of mass.
Reference standard data for the distance walked and the real-world gait speed during the parcours was collected using a “perambulator”: an actibelt® mounted on a calibrated measurement wheel (M10, Geofennel, Baunatal, Germany) to enable the development and cross-validation of algorithms for the estimation of real-world gait speed, based on the accelerometry data, and operated by an observer following the subject. Based on these data, precise mean values for the real-world gait speed of the subjects can be derived from the sinusoidal acceleration signals of the accelerometer placed near the rotational axis of the wheel for up to every 25 cm of the parcours. This can be considered a sufficiently accurate measure, since the step length of a person usually exceeds a length of 25 cm [15].
To assess the quality of step detection algorithms and their derived output for gait characteristics, such as the step, stance or swing time and the step count, the subject‘s walk was documented on video with a high-definition smartphone (Huawei, Mate 9, Shenzhen, China). Reference data using video annotation is well established for validation of accelerometry data since many years [16]. We have therefore opted for this method, which allows several possibilities in the post-processing.
Statistical analysis was performed with SPSS Version 24 and R version 3.3.3.
Results
19 of the 20 subjects recruited, were female, which is not unexpected as osteoporosis is more frequently observed in women. The demographic data of the population is shown in Table 1.
Table 1. Orthogeriatric study population.
| Demographics | Median (SD) |
|---|---|
| N | 20 |
| Age | 75.5 (7.817) |
| Height (cm) | 162.5 (7.409) |
| Weight (kg) | 67 (11.119) |
| BMI | 26.175 (3.575) |
Different comorbidities are also to be expected within the given patient group, Table 2 displays a summary of comorbidities and indicators observed for the subjects of the study.
Table 2. List of comorbidities.
| Comorbidity | Proportion (%) |
|---|---|
| Hip fracture | 20 |
| Vertebral body fracture | 20 |
| Wrist fracture | 35 |
| Cardiovascular disease | 45 |
| Neurological disease | 20 |
| Musculoskeletal disease | 70 |
| Previous falls | 30 |
| Joint arthroplasty | 25 |
| Sports on a regular base | 55 |
Range of speed
Six out of 20 subjects were in the gait speed range below 1.0 m/s. Most subjects (n = 14) are in the range between 0.9 m/s and 1.2 m/s. Mean speed values for each segment of the parcours based on the reference measurements are shown in Fig 1.
Fig 1. Range of speed.
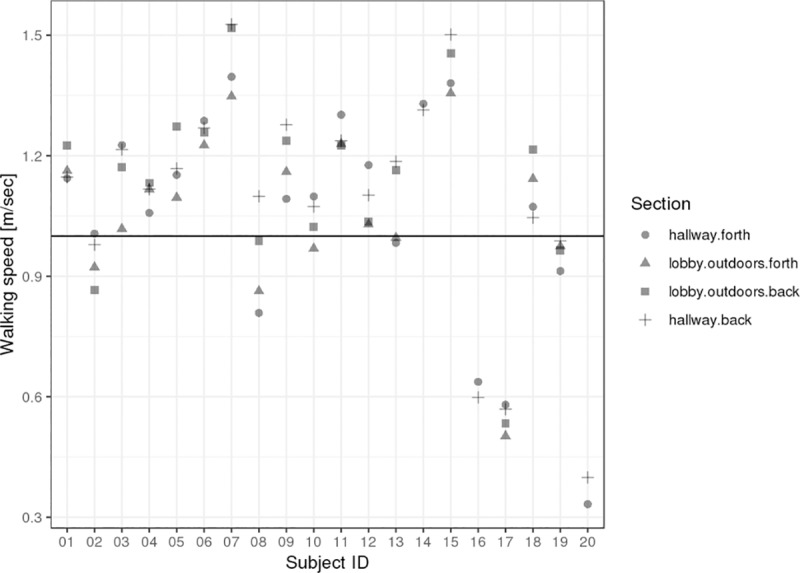
Variability of the mean reference speed per parcours section as measured with the measurement wheel for each subject.
For subject 16 and 20 the parcours had to be shortened to a simpler back and forth walk in the hallway section, thus data is only shown for the completed sections of the parcours.
Algorithms
We tested two sets of algorithms for step detection and speed estimation. As a reference we used the original algorithms developed for use with actibelt® and validated in healthy volunteers [17] and MS patients [13] and we tested a new set of algorithms designed to improve step detection and speed estimation in elderly, slow-walking adults.
The accelerometer is placed in a specific position inside the belt buckle. Therefore if the belt is correctly worn one of the axis of the accelerometer approximately corresponds to the direction of gravity. We therefore use the reference frame of the accelerometer as our algorithm does not correct the direction of gravity.
The original algorithms consist of the algorithm for step detection, named stepslc, and for speed estimation, named speedsvr. The step detection algorithm stepslc applies a sliding window approach with adaptive thresholds for magnitude and frequency to detect minima in the vertical acceleration signal, which are assumed to correspond to heel strike events. Detected steps are subsequently used to estimate a mean speed per step using speedsvr, a support vector regression machine trained normal walking volunteers to estimate the walking speed based on 4 different features extracted from the accelerometer signal [18].
The newly developed algorithm, named stepwave, builds on the feature extraction approach for step detection and speed estimation. Individual raw acceleration data files for a given patient were processed using an algorithm similar to Sabatini et al where first steps are detected and parameterized, before a Hilbert transform is used to calculate an analytical signal from which gait speed is projected per step using a linear model [19]. In the first step, a short time Fourier Transform is used to extract dominant frequencies from the raw signal: a broad band (0.7 Hz– 3 Hz) filter pass removes some noise from the signal before it is divided into overlapping windows of approximately 2.5 seconds, a Fast Fourier transform (FFT) then calculates the frequency domain for each axis. For each window, these results are then combined to determine the dominant frequencies, removing windows where the angle toward gravity or overall activity is not plausible for upright walking, or where there is no dominant frequency. For windows that pass these checks, a Butterworth filter is applied and a Hilbert transform is used to determine the frequency (F), phase (P) and amplitude (A) for each axis (vertical, x; lateral, y; and longitudinal, z). Ax, Ay, Az give good indication of the force involved in a step, independent of the exact timepoint, while F indicates step frequency, and P yields the relative position within a step. Finally, to predict gait speed, a linear model is fit to the parameters Ax, Ay and Az and their interaction terms from our training set (see below). Those features can subsequently be used to detect steps in the signal and estimate mean speeds per step. For the speed estimation a linear model has been fitted to the extracted features using a different dataset (see validation dataset [18]).
Comparison of step counts
Annotations for gait events such as the heel strikes, the toe offs and the overall step count was extracted from video data captured during each parcours and used to cross-validate step detection algorithms. Since the current implementations of the step detection algorithms do not yet yield toe-off events as an output, to compare the methods within the context of this paper only the overall step count is used. During the video documentation one of the subjects (subject 14) could not be recorded throughout the outdoors sections of the parcours due to a technical issue, and hence these sections were removed from this subject from the comparison displayed in Fig 2.
Fig 2. Comparison of step counts.
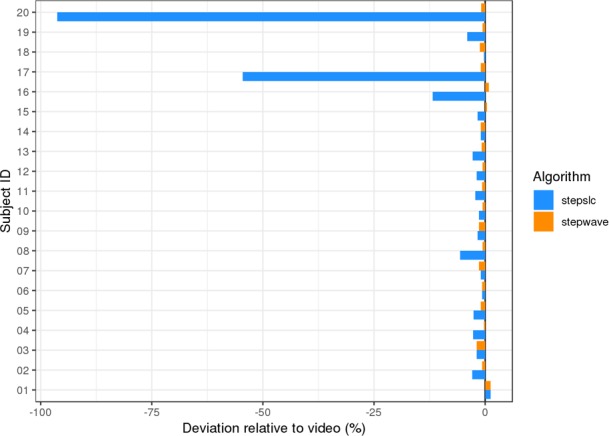
Comparison of the deviation from the video recorded steps (estimated steps divided by video steps minus 1) in percent for the two step detection algorithms. The vertical line at 0 depict identical step counts for video and algorithm.
Based on Figs 1 and 2, the original stepslc algorithm shows reduced step detection performance for gait speeds below 0.8 m/s (in particular subjects 16, 17 and 20).Relative to this, the stepwave algorithm demonstrates good performance in the lower speed range and a more consistent performance over the different subjects and gait speeds.
Comparison of gait speed estimation
The original speed estimation algorithm combines the step detection by stepslc with the speed estimation performed by speedsvr for the detected steps. However, for the comparison of speed estimates we combined step detection from stepwave with speedsvr to eliminate the discrepancies in stepslc step detection. We call this combination of algorithms wavesvr. Fig 3 displays the estimates of the original speed algorithm in comparison to the reference speeds as captured with the measurement wheel. Since speedsvr has been trained with data from a healthy population walking in a normal speed range, the original speed algorithm is expected to perform reasonably well in a similar speed range [17]. However, this combination is known to overestimate speeds in the lower range (<0.8 m/sec) [13], hence the increasing deviation from the reference (black diagonal in Fig 3) with decreasing gait speed. Thus, the development of the new stepwave algorithm has been especially focused on the lower speed range.
Fig 3. Scatter plot of mean speeds for each section of the parcours.
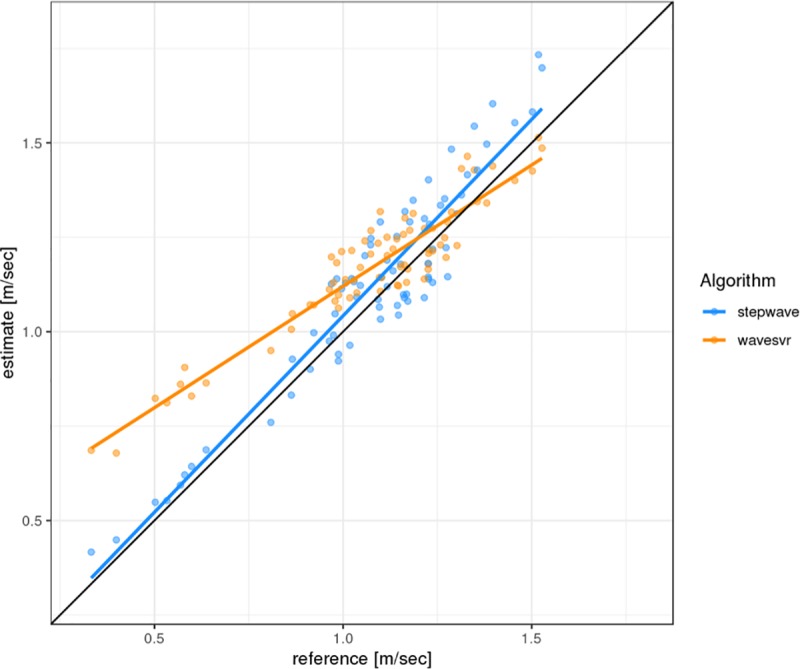
Displayed are the speed estimates of the two algorithm combinations with identical step detection plotted against the corresponding reference measures. The algorithms use the accelerometry signal from the belt mounted actibelt®.
The stepwave algorithm consists of step detection and speed estimation, but only the speed estimation part requires training. For the training of speed estimation we used the original dataset published by Schimpl et. al. [18].
While stepwave was trained on a similar dataset as speedsvr with healthy subjects and includes some artificially slow walks, speed estimates are close to the reference speed even below 0.5 m/sec of observed gait speed in the independent validation data (Fig 3). The linear fit for stepwave estimates is much closer to the diagonal (intercept of 0.002 and slope 1.040) compared to wavesvr (intercept of 0.477 and slope of 0.643) indicating an overall performance improvement in stepwave.
Overall stepwave shows less bias over the whole range of speeds and in particular in the speed range below 1.0 m/s. A comparison of the mean deviations for a given speed range is shown in Table 3, the difference of wavesvr is about five times higher than for stepwave for speed < 1.0 m/sec (t-test of the difference with from the mean of 0 p < 0.0001) whereas for speed ≥ 1.0 m/sec the difference is about the same (p > 0.9). This shows that stepwave significantly improves estimation of low gait speed, for higher gait speed the two algorithms do not perform significantly differently in our sample.
Table 3. Mean difference between reference speed and estimated, grouped by speed range.
Both listed speed estimation algorithms utilize the stepwave step detection approach.
| Speed range | Mean reference speed (m/s) | Mean estimated speed (m/s) | Difference (m/s) | Algorithm |
|---|---|---|---|---|
| Reference speed < 1 m/s | 0.779 | 0.985 | -0.206 | wavesvr |
| 1 m/s ≤ Reference speed < 1.5 m/s | 1.200 | 1.250 | -0.045 | wavesvr |
| Reference speed < 1 m/s | 0.779 | 0.818 | -0.039 | stepwave |
| 1 m/s ≤ Reference speed < 1.5 m/s | 1.200 | 1.250 | -0.048 | stepwave |
The Bland-Altman plot in Fig 4 indicates an overall increased accuracy between the reference and stepwave estimates, since the errors mostly agglomerate within the limits of agreement or barely lie beyond, as opposed to the wavesvr estimates for lower speed.
Fig 4. Bland-Altman plots of the applied algorithm combinations.
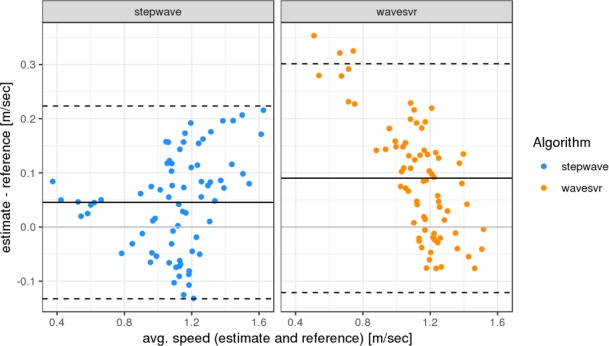
The plot for the original speed algorithm wavesvr and stepwave. The solid horizontal lines are the mean differences between estimated and reference speed, and the dashed lines the 1.96 fold standard deviations.
Discussion
This study aimed at implementation of a validation framework appropriate for elderly patients and representative of real-world settings, and to use this framework to test and improve algorithms for mobile accelerometry data in an orthogeriatric population. We present a study setup for the collection of high resolution accelerometry and reference data from elderly patients under realistic everyday walking conditions. We then describe how these data can be used to improve of speed estimation and step detection in slow walking orthogeriatric patients.
In previous studies, the original algorithms stepslc and speedsvr showed a speed overestimation, e.g. in multiple sclerosis patients with moderate to severe disability [13]. With the new algorithm stepwave, step detection notably improved for slow walkers (for subjects 16, 17 and 20 with gait speed < 0.8 m/s) compared to the original stepslc algorithm (see Figs 1 and 2). The accuracy of speed estimation was significantly higher than with the original algorithm speedsvr (Figs 3 and 4). Gait speed estimation improved for subjects with slow gait speeds (see Table 3. The linear regression figure and Bland-Altman plots (Figs 3 and 4), highlight the improvement in speed estimation.
Recently published algorithms for speed estimation, using accelerometry on a treadmill providing the ground-truth speed values, showed lower accuracy (RMSE 0.11–0.16 m/s vs. 0.09 m/s in our study) [20]. To our knowledge, there is no other algorithm published which transforms accelerometry data from an elderly population into gait speed with comparable accuracy in ecologically valid settings.
In contrast to gait speed, for which there are few published studies, step detection is well studied with multiple devices on multiple populations [21–26], however different validation protocols, populations and test scenarios make a comparison between existing results challenging, and there is no consensus about standardized setting [21,27,28]. Khan et al. and Lipperts et al. tested and validated their algorithms in an elderly population[27,28]. Lipperts et al. used a skin-mounted device in a healthy population and compared it to an orthopaedic target population in a real-life scenario, reporting accuracy in step detection above 92%[27]. Khan et al. tested their algorithm on healthy elderly home-living persons without abnormal gait patterns and showed accuracy of 94.4%[28]. However, impaired gaits with asymmetry and slow gait speeds downgrade the accuracy of algorithms detecting steps significantly [23]. In contrast to this, the presented stepwave algorithm is still highly accurate for step detection in elderly people including slow gait speeds (see Fig 2). In order to generate evidence on various surgical and non-surgical treatment options, objective, longitudinal measurements of a patient’s physical function are needed. Wearable physical activity monitors (PAMs) can now deliver long-term information about the activity of the individual [29]. This is a new opportunity to constantly monitor patient’s outcome over a certain time period and collect data on daily activity patterns and real-world behaviour [30]. Increasingly, these devices are finding their way into medical applications [31].
The presented assessment protocol in our study includes a real-world walking scenario and thus stands out clearly from other scenarios, e.g. testing on a treadmill or in the gait laboratory which can deviate strongly from walking representative of real-world gait speed [23,32]. The difficulty is to measure the physical activity under real-life conditions in a highly accurate manner.
A clear limitation of our study is that the number of patients included is low. As a result, few people are available for validation of slow gait speeds. Whether the described stepwave algorithm achieves a similarly high accuracy in a larger number of slow walking patients or in patients with even severe more gait impairment and very slow gait speeds is the subject of further studies. Furthermore, we excluded the stairs from the speed calculation. Here measurement with a rolling perambulator wheel is not working, so for this part of the parcours only the step detection is included.
Conclusion
The applied study setup and reference measurements have proven to deliver reliable and high-quality data, which can be fully used to improve algorithms to extract objective measures from accelerometry data.
Further analysis including an analysis of gait characteristics using annotated video data, as well as a comparison of the performance of various step detection and real-world gait speed estimation algorithms is warranted. Future research, for example in orthogeriatric and frail patient populations are necessary to achieve more detail and data especially for slow walking speeds and impaired gaits.
By improving accuracy of mobility assessment with accelerometer devices we can achieve a magnitude of insight information about long-term mobility in different populations including frail and elderly patients.
Acknowledgments
MS, IC, HH, AM are employees of Novartis Pharma AG, and may hold stock in, Novartis Pharma AG. MS is Professor and member of the medical faculty at University of Munich (LMU). We thank Martin Daumer and Christian Lederer from Trium Analysis Online GmbH and the Sylvia Lawry Center for MS Research e.V. in Munich for providing the actibelt® and technical support. The dataset is available under https://doi.org/10.5281/zenodo.3153170.
Data Availability
Data are available from Zenodo (https://doi.org/10.5281/zenodo.3153170).
Funding Statement
The authors received no specific funding for this work. Arne Mueller, Holger Hoefling, Matthias Schieker and Ieuan Clay are employed by Novartis Institute for Biomedical Research. Novartis Institute for Biomedical Research provided support in the form of salaries for authors MS, IC, HH and AM, but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of these authors are articulated in the ‘author contributions section.
References
- 1.Peri K, Kerse N, Robinson E, Parsons M, Parsons J, Latham N. Does functionally based activity make a difference to health status and mobility? A randomised controlled trial in residential care facilities (The Promoting Independent Living Study; PILS). Age and Ageing. 2007. October 11;37(1):57–63. 10.1093/ageing/afm135 [DOI] [PubMed] [Google Scholar]
- 2.Jeong J-N, Kim S-H, Park K-N. Relationship between objectively measured lifestyle factors and health factors in patients with knee osteoarthritis. Medicine. 2019. Jun;98(26):e16060 10.1097/MD.0000000000016060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paudel S, Owen AJ, Owusu-Addo E, Smith BJ. Physical activity participation and the risk of chronic diseases among South Asian adults: a systematic review and meta-analysis. Scientific Reports. 2019. December 5;9(1):9771 10.1038/s41598-019-46154-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goldman MD, Motl RW, Rudick RA. Possible clinical outcome measures for clinical trials in patients with multiple sclerosis. Therapeutic Advances in Neurological Disorders. 2010. July 23;3(4):229–39. 10.1177/1756285610374117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Afilalo J, Eisenberg MJ, Morin J-FF, Bergman H, Monette J, Noiseux N, et al. Gait Speed as an Incremental Predictor of Mortality and Major Morbidity in Elderly Patients Undergoing Cardiac Surgery. Journal of the American College of Cardiology. 2010. November;56(20):1668–76. 10.1016/j.jacc.2010.06.039 [DOI] [PubMed] [Google Scholar]
- 6.Lauretani F, Ticinesi A, Gionti L, Prati B, Nouvenne A, Tana C, et al. Short-Physical Performance Battery (SPPB) score is associated with falls in older outpatients. Aging clinical and experimental research. 2018. December 4; [DOI] [PubMed] [Google Scholar]
- 7.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. American journal of respiratory and critical care medicine. 2002. July 1;166(1):111–7. 10.1164/ajrccm.166.1.at1102 [DOI] [PubMed] [Google Scholar]
- 8.Takayanagi N, Sudo M, Yamashiro Y, Lee S, Kobayashi Y, Niki Y, et al. Relationship between Daily and In-laboratory Gait Speed among Healthy Community-dwelling Older Adults. Scientific reports. 2019. March 5;9(1):3496 10.1038/s41598-019-39695-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sievi NA, Brack T, Brutsche MH, Frey M, Irani S, Leuppi JD, et al. Accelerometer- versus questionnaire-based assessment of physical activity and their changes over time in patients with COPD. International journal of chronic obstructive pulmonary disease. 2017;12:1113–8. 10.2147/COPD.S130195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koolhaas CM, van Rooij FJAJ, Cepeda M, Tiemeier H, Franco OH, Schoufour JD. Physical activity derived from questionnaires and wrist-worn accelerometers: Comparability and the role of demographic, lifestyle, and health factors among a population-based sample of older adults. Clinical Epidemiology. 2018;10:1–16. 10.2147/CLEP.S147613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cyarto E V, Myers AM, Tudor-Locke C. Pedometer accuracy in nursing home and community-dwelling older adults. Medicine and science in sports and exercise. 2004. February;36(2):205–9. 10.1249/01.MSS.0000113476.62469.98 [DOI] [PubMed] [Google Scholar]
- 12.Plasqui G, Westerterp KR. Physical activity assessment with accelerometers: an evaluation against doubly labeled water. Obesity (Silver Spring, Md). 2007. Oct;15(10):2371–9. [DOI] [PubMed] [Google Scholar]
- 13.Motl RW, Weikert M, Suh Y, Sosnoff JJ, Pula J, Soaz C, et al. Accuracy of the actibelt(®) accelerometer for measuring walking speed in a controlled environment among persons with multiple sclerosis. Gait & posture. 2012. February;35(2):192–6. [DOI] [PubMed] [Google Scholar]
- 14.Bassett DR, Toth LP, LaMunion SR, Crouter SE, Crouter SE. Step Counting: A Review of Measurement Considerations and Health-Related Applications. Sports medicine (Auckland, NZ). 2017. July 22;47(7):1303–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aigner G, Grimm B, Lederer C, Daumer M. Method to collect ground truth data for walking speed in real-world environments: description and validation. PeerJ Preprints. 2019;7:e27558v1. [Google Scholar]
- 16.Aminian K, Robert P, Buchser EE, Rutschmann B, Hayoz D, Depairon M. Physical activity monitoring based on accelerometry: validation and comparison with video observation. Medical & Biological Engineering & Computing. 1999. May;37(3):304–8. [DOI] [PubMed] [Google Scholar]
- 17.Schimpl M, Moore C, Lederer C, Neuhaus A, Sambrook J, Danesh J, et al. Association between walking speed and age in healthy, free-living individuals using mobile accelerometry—a cross-sectional study. PloS one. 2011;6(8):e23299 10.1371/journal.pone.0023299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schimpl M, Lederer C, Daumer M. Development and validation of a new method to measure walking speed in free-living environments using the actibelt platform. PLoS ONE. 2011. August 5;6(8):e23080 10.1371/journal.pone.0023080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sabatini AM, Ligorio G, Mannini A. Fourier-based integration of quasi-periodic gait accelerations for drift-free displacement estimation using inertial sensors. BioMedical Engineering OnLine. 2015. December 23;14(1):106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McGinnis RS, Mahadevan N, Moon Y, Seagers K, Sheth N, Wright JA, et al. A machine learning approach for gait speed estimation using skin-mounted wearable sensors: From healthy controls to individuals with multiple sclerosis. Yang J-M, editor. PLoS ONE. 2017. June 1;12(6):e0178366 10.1371/journal.pone.0178366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Raymond M, Winter A, Holland AE. Validation of an Activity Monitor in Older Inpatients Undergoing Slow Stream Rehabilitation. Journal of Physical Activity and Health. 2015;12(9):1298–303. 10.1123/jpah.2014-0347 [DOI] [PubMed] [Google Scholar]
- 22.Feng Y, Wong CK, Janeja V, Kuber R, Mentis HM. Comparison of tri-axial accelerometers step-count accuracy in slow walking conditions. Gait and Posture. 2017;53:11–6. 10.1016/j.gaitpost.2016.12.014 [DOI] [PubMed] [Google Scholar]
- 23.Thorup CB, Andreasen JJ, Sørensen EE, Grønkjær M, DInesen BI, Hansen J. Accuracy of a step counter during treadmill and daily life walking by healthy adults and patients with cardiac disease. BMJ Open. 2017. March 31;7(3):e011742 10.1136/bmjopen-2016-011742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Storti KL, Pettee KK, Brach JS, Talkowski JB, Richardson CR, Kriska AM. Gait speed and step-count monitor accuracy in community-dwelling older adults. Medicine and Science in Sports and Exercise. 2008. January;40(1):59–64. 10.1249/mss.0b013e318158b504 [DOI] [PubMed] [Google Scholar]
- 25.Fortune E, Lugade V, Morrow M, Kaufman K. Validity of using tri-axial accelerometers to measure human movement—Part II: Step counts at a wide range of gait velocities. Medical Engineering and Physics. 2014;36(6):659–69. 10.1016/j.medengphy.2014.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mueller A, Hoefling H, Nuritdinow T, Holway N, Schieker M, Daumer M, et al. Continuous Monitoring of Patient Mobility for 18 Months Using Inertial Sensors following Traumatic Knee Injury: A Case Study. Digital Biomarkers. 2018. August 2;2(2):79–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lipperts M, van Laarhoven S, Senden R, Heyligers I, Grimm B. Clinical validation of a body-fixed 3D accelerometer and algorithm for activity monitoring in orthopaedic patients. Journal of Orthopaedic Translation. 2017. October 1;11:19–29. 10.1016/j.jot.2017.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khan AM, Lee YK, Lee S, Kim TS. Accelerometer’s position independent physical activity recognition system for long-term activity monitoring in the elderly. Medical and Biological Engineering and Computing. 2010;48(12):1271–9. 10.1007/s11517-010-0701-3 [DOI] [PubMed] [Google Scholar]
- 29.Grimm B, Bolink S. Evaluating physical function and activity in the elderly patient using wearable motion sensors. EFORT Open Reviews. 2016. May 31;1(5):112–20. 10.1302/2058-5241.1.160022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Clay I. Impact of Digital Technologies on Novel Endpoint Capture in Clinical Trials. Clinical pharmacology and therapeutics. 2017. December 1;102(6):912–3. 10.1002/cpt.866 [DOI] [PubMed] [Google Scholar]
- 31.Pitta F, Troosters T, Probst V, Spruit M, Decramer M, Gosselink R. Quantifying physical activity in daily life with questionnaires and motion sensors in COPD. European Respiratory Journal. 2006. May 1;27(5):1040–55. 10.1183/09031936.06.00064105 [DOI] [PubMed] [Google Scholar]
- 32.Greig C, Butler F, Skelton D, Mahmud S. Treadmill Walking in Old Age May Not Reproduce the Real Life Situation. Journal of the American Geriatrics Society. 1993. January 1;41(1):15–8. 10.1111/j.1532-5415.1993.tb05941.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available from Zenodo (https://doi.org/10.5281/zenodo.3153170).


