Abstract
Strongyloidiasis is caused by the human infective nematodes Strongyloides stercoralis, Strongyloides fuelleborni subsp. fuelleborni and Strongyloides fuelleborni subsp. kellyi. The zoonotic potential of S. stercoralis and the potential role of dogs in the maintenance of strongyloidiasis transmission has been a topic of interest and discussion for many years. In Australia, strongyloidiasis is prevalent in remote socioeconomically disadvantaged communities in the north of the continent. Being an isolated continent that has been separated from other regions for a long geological period, description of diversity of Australian Strongyloides genotypes adds to our understanding of the genetic diversity within the genus. Using PCR and amplicon sequencing (Illumina sequencing technology), we sequenced the Strongyloides SSU rDNA hyper-variable I and hyper-variable IV regions using Strongyloides-specific primers, and a fragment of the mtDNA cox1 gene using primers that are broadly specific for Strongyloides sp. and hookworms. These loci were amplified from DNA extracted from Australian human and dog faeces, and one human sputum sample. Using this approach, we confirm for the first time that potentially zoonotic S. stercoralis populations are present in Australia, suggesting that dogs represent a potential reservoir of human strongyloidiasis in remote Australian communities.
Author summary
Strongyloides stercoralis is a soil-transmitted nematode that causes the disease strongyloidiasis. Due to the autoinfective nature of this parasite, it can re-infect a host causing chronic infection. If not diagnosed and treated it can be highly detrimental to human health and has a high mortality rate. Strongyloidiasis is common in remote communities in the north of Australia and has been an issue for decades. Despite various successful intervention programs to treat human strongyloidiasis, the disease remains endemic in those communities. Here for the first time we looked at the Australian dogs’ potential to infect humans and found that they carry two genetically distinct strains of Strongyloides spp., one of which also infects humans. This supports the hypothesis that dogs are a potential source for human strongyloidiasis. We also found that dogs in Australia might be carrying unique haplotypes. Whether these new haplotypes are also human infective is to be confirmed by further research.
Introduction
Strongyloidiasis is caused by the human infective nematodes Strongyloides stercoralis, Strongyloides fuelleborni subsp. fuelleborni and Strongyloides fuelleborni subsp. kellyi [1]. Worldwide, Strongyloides spp. are estimated to infect up to 370 million people, predominately in socioeconomically disadvantaged communities [2–4]. While S. stercoralis is a globally distributed nematode, S. f. fuelleborni has thus far only reported in Africa and Southeast Asia and S. f. kellyi from Papua New Guinea (PNG) [5–7].
In Australia, strongyloidiasis is prevalent in remote communities located across the Northern Territory, Queensland, Western Australia, northern South Australia and northern New South Wales [8]. Current estimates of infection rates in some communities are up to 41% or 60% based on microscopy or serology respectively [9–12]. Despite initially successful intervention programs targeting treatment to eliminate human strongyloidiasis in remote Australian communities, the disease remains endemic [13, 14]. Reappearance of the infection could possibly be as a result of zoonotic transmission from dog reservoirs given that dogs and humans share a close and intimate cultural bond in rural and remote Indigenous communities of Australia [15].
The zoonotic potential of S. stercoralis infected dogs and their potential role in the maintenance of strongyloidiasis transmission has been a topic of interest and discussion for many years [16–18]. Molecular investigation of human and dog derived S. stercoralis is useful for understanding the nature of cross infection. There are two regions of the S. stercoralis nuclear and mitochondrial genome that are considered to be conserved within the Strongyloides genus and can be used as markers for molecular typing of S. stercoralis. Hyper-variable regions (HVR) I and IV of the Small Subunit (SSU) ribosomal DNA and the cytochrome c-oxidase subunit 1 (cox1) gene of the mitochondrial DNA (mtDNA) have been widely used to study relationships between S. stercoralis from different hosts and different geographic locations [19–23]. Based on genetic analysis of these loci, it has been recently found that there are two genetically different S. stercoralis strains, one is dog and human infective, and the other is dog specific. These data were collected from dogs and humans in Cambodia and Myanmar [21, 22].
Being an isolated continent that has been separated from other regions for a long geological period, Australia could represent an interesting addition to our understanding of the genetic diversity within S. stercoralis and the Strongyloides genus more generally. Indigenous Australians have inhabited the continent for at least 40,000 years and dogs (in the form of dingoes) were likely introduced up to 12,000 years ago [24]. Given this long period of relative isolation, it might be expected that Australia could harbor unique endemic genotypes or unique sub-species of S. stercoralis that have evolved within dog and human populations over this period.
Using PCR and amplicon sequencing (Illumina sequencing technology), we sequenced the Strongyloides SSU rDNA hyper-variable I and hyper-variable IV regions using Strongyloides-specific primers, and a fragment of the mtDNA cox1 gene using primers that are broadly specific for Strongyloides sp. and hookworms. This approach was applied to DNA extracted from human and dog faeces, and one human sputum sample. The main focus of this study was to genotype Australian human and dog S. stercoralis strains to see whether dogs carry human S. stercoralis strains and/or vice versa. To our knowledge this is the first time human and dog S. stercoralis have been studied in Australia on a molecular level.
Methods
Study area and faeces collection
Dog faecal samples were collected from communities in the Northern Territory, Australia. Dog faeces were collected from the environment (i.e., the ground) in the selected communities and stored in the DESS (dimethyl sulfoxide, disodium EDTA, and saturated NaCL) solution to preserve the DNA [25]. For those dog faeces that were collected from privately owned land, written consent was obtained to collect the samples. The preserved faecal samples were express posted to the Environmental Health laboratory, Flinders University, South Australia, for further analysis.
Human faecal and sputum samples were provided by our colleagues at the Royal Darwin Hospital, NT, AusDiagnostics Pty Ltd, NSW, and Townsville Hospital, Queensland. While the personally-identifying information of the patients was de-linked from our analyses, their infections are known to have been locally acquired. Ethics approval from the Social and Behavioural Research Ethics Committee (SBREC) No 6852 dated 1st June 2015 was obtained for collecting dog faeces from the remote communities. Human ethical approval from the Southern Adelaide Clinical Human Research Ethics Committee (SAC HREC) No 309.17 dated 24th January 2018 was obtained for comparing S. stercoralis DNA extracted from human and dog tissues. CDC investigators were not engaged with sample collection and their participation did not include engagement with human or animal subjects.
DNA extraction
Prior to DNA extraction, faecal samples containing DESS were centrifuged for three minutes at 3000 x g rpm using an Orbital 400 Clements (Phoenix, Lidcombe, Australia). The supernatant consisting of the preservative solution was removed. The remaining faecal sample was washed with sterile saline solution. DNA was extracted using the Power Soil DNA isolation kit (QIAGEN, Hilden, Germany) following the manufacturer’s instructions with slight modifications that included incubating samples at 56°C overnight after the cell lysis step, followed by vortexing of samples for three minutes. Approximately 250 milligrams of the pellet was placed into a PowerBead tube containing lysis buffer (included in the Power Soil DNA extraction kit). The remainder of the extraction process was performed according to the manufacturer’s instructions. Approximately 100 μL of extracted DNA was stored at -20°C prior to real-time PCR (qPCR) analysis.
Real-time PCR
The samples (273 dog and 4 human DNA samples) were first screened for Strongyloides spp. using qPCR in the Environmental Health laboratory at Flinders University, SA, Australia. The real-time PCR assay was adopted from Verweij et al. [26] using S. stercoralis—specific primers targeting a 101 base pair region of 18S rRNA. The 20 μL reaction contained 10 μL Supermix (SSoAdvanced, Universal Probes Supermix, Foster City, Bio-Rad Laboratories, CA, USA), 1 μL primers and probe mixture (1x) (Stro18S-1530F, Stro18S-1630R and Stro18S-1586T FAM) (Sto 18S PrimePCR probe assay, Bio-Rad Laboratories, CA, USA), 4 μL deionised H2O, and 5 μL DNA template. All qPCR reactions were performed in triplicate on the Corbett Rotor-Gene 6000 machine (QIAGEN, Hilden, Germany). S. stercoralis primers and probes and qPCR conditions used are shown in Table 1. A sample was considered positive when the Ct value was lower than the mean negative Ct minus 2.6 standard deviations of a mean negative control Ct. Positive samples were amplified in every qPCR reaction.
Table 1. Primers and probes and PCR conditions.
| Primer | Amplicon | Sequence | Reaction conditions |
|---|---|---|---|
| Stro18S-1530F |
rDNA 101 bp |
5’-GAATTCCAAGTAAACGTAAGTCATTAGC-3’ | Step 1: 95°C for 15 min, Step 2: 95°C for 15 s, Step 3: 60°C for 30 s. Repeat steps two and three 40 times. |
| Stro18S-1630R | 5’-TGCCTCTGGATATTGCTCAGTTC-3’ | ||
| Stro18S-1586T FAM | 5’-ACACACCGGCCGTCGCTGC-3’-BHQ1 | ||
| SSP_COX1_F * | mtDNA ~270 bp | 5’-TTTGATCCTAGTTCTGGTGGTAATCC-3’ | Step 1: 98°C for 30 s, Step 2: 98°C for 10 s, Step 3: 60°C for 10 s, Step 4: 72°C for 10 s, Step 5: 72°C for 2 min. Repeat steps two to four 45 times. |
| SSP_COX1_R * | 5’-GTAGCAGCAGTAAAATAAGCACGAGA-3’ | ||
| NEW_HVR_I_F | rDNA ~500 bp | 5’-GCTCATTATAACAGCTATAGACTACACGGTA-3’ | Step 1: 98°C for 30 s, Step 2: 98°C for 10 s, Step 3: 60°C for 10 s, Step 4: 72°C for 10 s, Step 5: 72°C for 2 min. Repeat steps two to four 45 times. |
| NEW_HVR_I_R | 5’-CCACAACAATCATTTTATGCACTTGG-3’ | ||
| NEW_HVR_IV_F | rDNA ~320 bp | 5’-CGGGCCGGACACTATAAGG-3’ | Step 1: 98°C for 30 s, Step 2: 98°C for 10 s, Step 3: 63°C for 10 s, Step 4: 72°C for 10 s, Step 5: 72°C for 2 min. Repeat steps two to four 45 times. |
| NEW_HVR_IV_R | 5’-ATCTCTAAACAGGAACATAATGATCACTAC-3’ |
*Broadly specific primers for amplification of Strongyloides sp. cox1 sequences as well as those of several hookworms
Conventional PCR for amplification of SSU HVR-I and HVR-IV, and cox1 sequences
Extracted DNA from samples that were qPCR positive for Strongyloides spp. (47 dog and four human DNA samples) was shipped on dry ice to the Centers for Disease Control and Prevention (CDC), Georgia, USA for conventional PCR, sequencing and bioinformatics analysis. Hyper-variable regions (HVR) I and IV in the small Subunit (SSU) ribosomal DNA and a fragment of the mitochondrial cytochrome c-oxidase subunit 1 (cox1) gene were amplified using conventional PCR and then sequenced using Illumina technology. All PCR reactions were performed on a GeneAmp PCR System 9700 Thermo Cycler, version 3.12 (Applied Biosystems, USA). S. stercoralis primers and PCR conditions used for qPCR and conventional PCR are shown in Table 1. For the cox1 gene, PCR reactions were performed in a total volume of 50 μL containing 10 μL NEB 5X Q5 Buffer (New England BioLabs, USA), 10 μL NEB 5X Q5 High GC Enhancer (New England BioLabs, USA), 4 μL NEB Deoxynucleotide Solution Mix (10 mM each nt) (New England BioLabs, USA), 1 μL Q5 High-Fidelity DNA Polymerase (New England BioLabs, USA), 2.5 μL 10 μM forward primer (SSP_COX1_F), 2.5 μL 10 μM reverse primer (SSP_COX1_R), 18 μL deionised H2O, and 2 μL DNA template. For the HVR-I and HVR-IV regions, PCR reactions were performed in a 25 μL reaction containing 12.5 μL of NEBNext Q5 Hot Start HiFI PCR Mastermix, MO543L (New England BioLabs, USA), 1.5 μL 10 μM forward primer (NEW_HVR_I_F or NEW_HVR_IV_F), 1.5 μL 10 μM reverse primer (NEW_HVR_I_R or NEW_HVR_IV_R), 7.5 μL deionised H2O, and 2 μL DNA template.
The amplified PCR products were separated by 1.5% agarose gel electrophoresis and stained with ethidium bromide. The stained DNA bands were visualised by UV illumination using a Ugenious 3 (SYNGENE, Japan). For quality control, each PCR run included a positive control containing Strongyloides genomic DNA as template, a non-template control containing autoclaved sterile water instead of template, and a negative control containing DNA extracted from a parasite-free specimen. Amplicons for each of the three markers were also generated for Strongyloides ratti as an additional control for the sequencing and in silico analysis steps.
Next generation sequencing (NGS)
Ten microliters of PCR amplicon was purified and normalized for concentration prior to library preparation using a SequalPrep Normalization Plate Kit (Thermo Fisher Scientific, USA). DNA libraries were prepared using the NEBNext Ultra DNA Library Prep Kit for Illumina (New England BioLabs, USA), and NEBNext Multiplex Oligos for Illumina Index kit (New England BioLabs, USA). The NEBNext Ultra DNA Library Prep Kit was used as it does not include a tagmentation step. Consequently, adapters and indices are added to the ends of the amplicon without fragmenting the DNA. This produces paired reads with each mate spanning approximately 250 bases up each end of the amplicon, so that when overlapping reads are merged, the entire length of our short amplicons is covered (Table 1). The sequencing reactions were prepared using the MiSeq reagent Nano Kit v2 (PE250bp), and performed on the Illumina MiSeq platform (Illumina). The Illumina MiSeq reads generated for successfully sequenced specimens were uploaded to NCBI and are available under BioProject accession number PRJNA531959.
In silico analysis
The Illumina reads were analyzed using Geneious (www.geneious.com) by means of a workflow that performed read quality control, assembly of contigs and genotype assignment. As part of this workflow, quality trimming to a minimum phred score of 20 and removal of adapter sequence was performed using BBDuk (v 37.64). Reads less than 50 bases in length were discarded. Paired reads were then merged using BBMerge (v 37.64) and all reads (merged and unmerged) were mapped to a reference sequence. For cox1 amplicons, reads were mapped to a S. stercoralis sequence with the GenBank (GB) accession number LC050212.1. For SSU HVR-I and SSU HVR-IV, reads were mapped to a S. stercoralis with the accession AF279916.2. Prior to mapping, each reference sequence was trimmed to the length of the amplicon, excluding the primer sequences. Mapping was performed using the Geneious mapper under the Medium sensitivity / Fast default settings. This mapping served as a read filtering step to exclude reads derived from spurious PCR artifacts, off target amplifications, or DNA from the fecal extract. Merged reads (and their corresponding mates for reads that could not be merged) that successfully mapped were retained for de novo assembly. These reads were assembled using the Geneious de novo assembler with the following customized parameters; minimum overlap: 50 bases, minimum overlap identity: 100%, maximum number of mismatches per read: 0%, and the maximum number of ambiguities: 1. Contigs were split if coverage fell below 50 bases and sub-variants with coverage less than 50 were not considered. The short amplicon lengths facilitated generation of merged reads that spanned the entire amplicon in most cases. Consequently, these de novo assembled contigs represent a consensus of large numbers of identical reads. To identify multiple haplotypes within a single specimen using these reads, the option to merge contigs with coverage less than 100 was selected during de novo assembly. According to Geneious documentation, setting this value to 100 requires that at least 100 reads, each with a Phred base quality score of 30 at a potential variant site, map to that variant site before a new variant is considered real and used to construct a new contig (i.e., a new haplotype). Consequently, variant bases were supported by a cumulative Phred quality score of greater than 3,000 before a new haplotype was generated. If some reads supporting a variant site had a Phred quality score less than 30 at this site, more reads were required to support the variant and call the new haplotype (i.e., until the cumulative Phred quality score exceeded 3,000). Contigs were trimmed to the primer sequence using the ‘Trim Ends’ function in Geneious. These high-quality contigs were validated further by taking the trimmed and merged reads and mapping them back to the contigs generated using the Geneious mapper, and the following custom parameters: minimum mapping quality: 30 bases, minimum overlap: 150 bases, minimum overlap identity: 100%, maximum number of mismatches: 0%, and the maximum number of ambiguities: 1. Contigs were split or discarded if the coverage fell below approximately 300 to 500 depending on the depth obtained for a particular specimen (~500 for specimens that obtained >10k reads, ~300 bases for specimens with <10k reads). Following mapping, each alignment was manually examined in Geneious for misalignments and gaps. Contigs were considered valid if the coverage obtained approached or exceeded these thresholds, and if misalignments and gaps were absent upon manual examination. The number of merged reads that mapped back to each contig during this final validation step are listed in S1 File. Finally, haplotypes were assigned by performing a local BLASTN search (within Geneious) against a database constructed from all unique Strongyloides sp. 18S and cox1 sequences available in GenBank and the DNA Databank of Japan. The cox1 sequences used to construct this BLAST database are provided in S2 File and GenBank accession numbers for sequences used to construct the 18S database are listed in Tables 2 and 3. A set of homologous sequences from several other roundworms (parasitic and free-living) were also included in this database. Sequences were only added to the BLASTN database if they overlapped our 217 bp cox1 amplicon by more than 95%. This included several previously published cox1 haplotypes that had matching SSU HVR-I and HVR-IV haplotypes assigned [21].
Table 2. HVR I haplotypes assigned to Strongyloides sp. based on current data.
| Haplotypes | GenBank Accession/s | Notes |
|---|---|---|
| I | AB923888.1, AF279916.2, AJ417023.1, | Found in dogs and humans. |
| II | KF926659.1, MK468655, MK468656, MK468657, MK468658, MK778085 | Found in dogs and humans. |
| III | AB453315.1 | Found in dogs and humans. |
| IV | AB272234.1, KU724124.1, MK468663 | This haplotype has been detected in dogs though not in humans. It has also been described in a badger where it was assigned to S. procyonis. |
| V | Jaleta et al. (2017) | Described by Jaleta et al. (2017) but the sequence of this type was not available in GenBank prior to this study. This is potentially a dog-specific haplotype. |
| VI | AB453316.1, AB453314.1, MH932098.1, MH932099.1, MH932100.1, MK468660 | Assigned only to S. stercoralis. Identified in dog 18 from this study. Described predominantly in dogs but also in a chimpanzee (AB453314.1). |
| VII | AB205054.1 | A S. procyonis sequence greater than 99% similar to S. stercoralis Haplotype I and Haplotype IV. |
| VIII | MK468661 | Novel Strongyloides sp. sequence from Dog 22 most similar to Haplotype VII. |
| IX | LC038066.1 | Strongyloides sp. Okayama isolated from a Japanese striped snake. This sequence is greater than 99% identical to sequences of S. stercoralis and S. procyonis. Similar to Haplotype X (see below) identified in an Australian dog. |
| X |
MK468662 |
Sequence identified in dog 45 in present study. Most similar to Strongyloides sp. Okayama (Haplotype IX). |
Table 3. HVR IV haplotypes assigned to Strongyloides sp. based on current data.
| Haplotypes | GenBank Accession/s | Notes |
|---|---|---|
| A | KY081221.1, KU724128.1, KU724125.1, LC085483.1, LC085482.1, LC085481.1, KU962182.1, KU962181.1, KU962180.1, KU962179.1, AB923888.1, KF926662.1, KF926661.1, AF279916.2, MH932097.1, MH932097.1, MH932095.1, KY081223.1, AB526826.1, AB453316.1, AB453315.1, AB453314.1, MK468664—MK468671 | Identified in dogs, humans and chimpanzees. A S. stercoralis- specific haplotype |
| B | KU724129.1 | Identified only in dogs. Consistently assigned to S. stercoralis |
| C | M84229.1 | This sequence was published in GenBank in 1993 and assigned to S. stercoralis. It has not appeared in the literature since based on our knowledge, though we assigned to haplotype C for its historic value. It shares one SNP difference to type A (Fig 2). |
| D | AB272234.1, AB205054.1 | Includes two sequences assigned to S. procyonis. This type is 99% similar to Haplotype B. |
| E | MK468674 | Novel haplotype identified in dog 18. Most similar to Haplotype A. |
| F | MK468675 | Novel haplotype identified in dog 22. Most similar to Haplotype D. |
| G | MK468676 | Novel haplotype identified in dog 13. Most similar to Haplotype A. |
| H | LC038066.1 | Strongyloides sp. Okayama isolated from a Japanese striped snake. |
| I | MK468677 | Novel haplotype identified in dog 45. Most similar to Haplotype H. |
Any specimens for which Strongyloides ratti sequences were detected as part of this workflow were considered to be at risk of contamination from our positive control and potentially from other specimens included in the study. Any contaminated specimens were excluded from further analysis.
Construction of a cox1 cluster dendrogram
Sequences of cox1 were exported from Geneious as a fasta file and were aligned using the ‘msa’ package in R. The ‘dist.alignment’ function from the ‘seqinr’ package was used to compute a pairwise identity matrix, considering gaps in the identity measure. The resulting matrix was clustered using the agglomerative nested clustering approach performed with the ‘agnes’ R package, using “euclidean” distances and the “average” clustering method. A cluster dendrogram was generated using the ‘ggtree’ R package. Vector images (i.e. graphics) used for annotation of the dendrogram were either generated in house at CDC or obtained from PhyloPic (http://phylopic.org).
Results
Real-time PCR, conventional PCR and sequencing
We screened 273 dog and four human samples using real-time PCR. Forty-seven (47) dog and four human samples that were positive or presumed positive (higher Ct values) by qPCR were selected for conventional PCR with further sequencing of their cox1, SSU rDNA HVR-I and HVR-IV regions. For some of the 47 dog samples useable sequences were not generated due to poor amplification of the PCR product. Sequence data was obtained for 24 specimens including four human specimens and twenty dog specimens. The complete set of amplified sequence variants (ASVs) of all specimens analyzed in this study is shown in Fig 1 and summarized in Table 4.
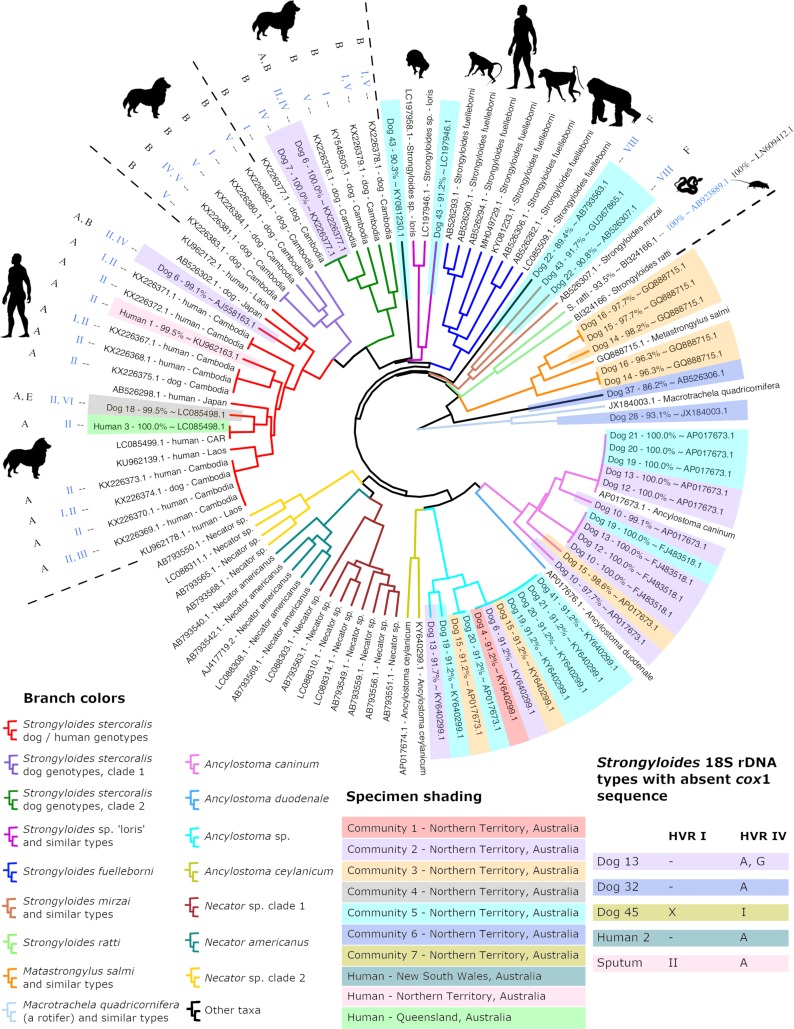
Fig 1. Dendrogram of clustered cox1 amplicons from Australian dog and human specimens.
This dendrogram includes cox1 sequences generated in this study and a selection of previously published cox1 sequences that overlap with our 217 base pair cox1 amplicon by 100%. Specimens analyzed as part of this study are shaded according to their site of collection. Branches are color coded according to their identity; either a species assignment, a proposed genus assignment, or their S. stercoralis genotype. When available, Strongyloides sp. cox1 sequences are annotated with their associated SSU haplotypes, with their HVR-I type shown in blue and their HVR-IV type shown in black. Specimens for which a cox1 sequence was not obtained are shown in a table embedded in the figure (bottom right), which includes two specimens possessing unique 18S haplotypes; dog 13 (HVR-IV, type G) and dog 45 (HVR-I, type X). A dash (-) shown in this table indicates failed amplification and/or sequencing of that marker. ‘Sputum’ refers to the sole sputum sample from a human patient (human 4) included in this study. Sequences published in previous studies that are not from S. stercoralis are labelled with their GenBank and/or DNA Data Bank of Japan accession numbers followed by their species name. Strongyloides stercoralis sequences from previous studies are labelled with their accession number, host species, and country of origin. Note that ‘CAR’ means Central African Republic. Names of specimens collected as part of this study begin with a host name and a unique number assigned in this study, followed by a percentage similarity to (~) a near BLASTN hit identifiable by its accession number.
Table 4. Human and dog samples analyzed in this study and their haplotypes.
| Sample | HVR-I haplotype | HVR-IV haplotype | Cox1 Accessions |
|---|---|---|---|
| Human 1 | Haplotype II | Haplotype A | MK434219† |
| Human 2 | NA (excluded due to S. ratti contamination) | Haplotype A | NA |
| Human 3 | Haplotype II | Haplotype A | MK434218 |
| Sputum (Human 4) | Haplotype II | Haplotype A | NA |
| Dog 4 | NA | NA | MK434258† |
| Dog 6 | Haplotype II and Haplotype IV | Haplotype A and Haplotype B |
MK434255 MK434256† MK434257† |
| Dog 7 | Haplotype IV | Haplotype B | MK434254 |
| Dog 10 | NA | NA |
MK434251 MK434252† MK434253† |
| Dog 12 | NA | NA |
MK434249 MK434250 |
| Dog 13 | NA | Haplotype A and Haplotype G* |
MK434246 MK434247 MK434248† |
| Dog 14 | NA (excluded due to S. ratti contamination) | NA |
MK434244† MK434245† |
| Dog 15 | NA | NA | MK434240† |
|
MK434241† MK434242† MK434243† |
|||
| Dog 16 | NA | NA |
MK434238† MK434239† |
| Dog 18 | Haplotype II and Haplotype VI |
Haplotype A and Haplotype E* |
MK434237† |
| Dog 19 | NA | NA |
MK434233 MK434234 MK434235† MK434236† |
| Dog 20 | NA | NA |
MK434230 MK434231† MK434232† |
| Dog 21 | NA | NA |
MK434228 MK434229† |
| Dog 22 | Haplotype VIII* | Haplotype F* |
MK434226† MK434227† |
| Dog 28 | NA | NA | MK434225† |
| Dog 32 | NA | Haplotype A | NA |
| Dog 37 | NA | NA | MK434224† |
| Dog 41 | NA | NA | MK434223† |
| Dog 43 | NA | NA |
MK434220† MK434221† MK434222† |
| Dog 45 | Haplotype X* | Haplotype I* | NA |
* Novel SSU haplotypes
†Novel cox1 sequences
Note: All GenBank Accession numbers associated with the sequences generated in this study are provided in S1 File
SSU HVR-I haplotypes detected among S. stercoralis from Australian dogs and humans
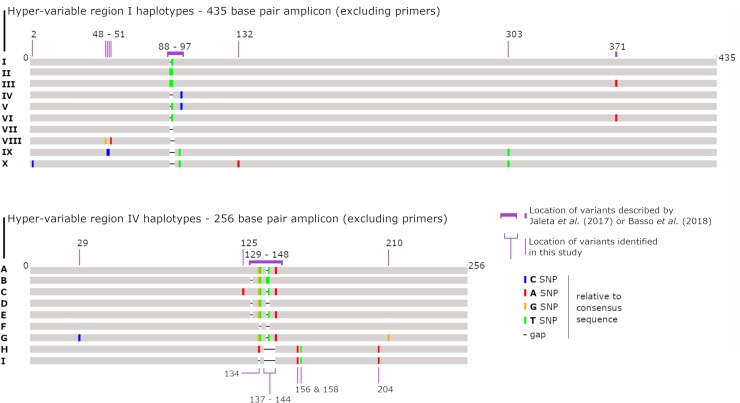
Jaleta et al. previously sequenced the SSU HVR-I region of S. stercoralis worms from Cambodian dog and human specimens and identified five different haplotypes (HVR-I haplotypes I-V) [21]. A recent study of European dogs identified a haplotype from the HVR-I region (haplotype VI) [23], that was previously mentioned by Hasegawa et al. (2009) (AB453316.1 and AB453314.1) [19] (Table 2). In our Australian samples we found haplotype II in both human and dog samples and haplotype IV in dog samples only, which is consistent with the findings from Jaleta et al. [21]. We also identified haplotype VI in a single Australian dog. Following the haplotype nomenclature used by Jaleta et al. [21] and Basso et al. [23], we discovered two new HVR-I haplotypes; haplotypes VIII and X (Fig 2, Table 4), in addition to these six haplotypes previously described [21, 23]. Due to the existence of noteworthy similarities (> 99% in all cases) between sequences of S. stercoralis, Strongyloides procyonis, a sequence assigned to Strongyloides sp. Okayama (GB: LC038066.1), and our novel dog sequences, we expanded the Jaleta et al. typing scheme to include these sequences [21]. This involved inclusion of haplotypes that could not be confidently assigned to S. stercoralis given the information on hand, yet are highly similar to known S. stercoralis 18S haplotypes. This adjustment was also required because a sequence attributed to S. procyonis (GB: AB272234.1) possesses HVR-I haplotype IV, which is identical to a S. stercoralis haplotype assigned to a Cambodian dog (GB: KU724124.1). For details, refer to Fig 2, and Tables 2 and 4.
Fig 2. Schematic detailing the proposed modifications to the previously described S. stercoralis genotyping scheme.
A graphical representation of the novel Strongyloides haplotypes discovered in this study compared to haplotypes identified in previous reports. The location of sites that were genotypically informative based on the original genotyping method described by Jaletta et al. (2017) and Basso et al. (2018) are indicated, as well as new SNP/indel sites that have been incorporated into the typing scheme based on the results of this study [21, 23]. For hypervariable region I, we introduce two novel types (VIII and X), and assign new haplotype names to published sequences that had not been previously considered in this typing scheme (VII and IX). For hypervariable region IV, we introduce three novel types (E, F, G and I), and assign new haplotype names to published sequences that had not been previously considered in this typing scheme (C, D and H) (see Tables 3 and 4 for details).
SSU HVR-IV haplotypes detected among S. stercoralis from Australian dogs and humans
In the Australian samples we identified HVR-IV haplotype A in both humans and dogs, and haplotype B only in dogs, as previously observed [21]. Supporting the findings of Jaleta et al. [21], our results also showed that haplotype II of HVR-I is found in combination with haplotype A of HVR-IV, and haplotype IV of the HVR-I region is only found in combination with haplotype B of the HVR-IV region [21]. We observed that a unique sequence attributed to S. stercoralis had been submitted to GenBank in 1993, and its HVR-IV sequence was assigned to haplotype C (GB: M84229.1). Next, given the strong similarity between HVR-IV sequences of S. procyonis and S. stercoralis and the fact that HVR-I haplotype IV is also found in S. procyonis SSU sequences, we assigned the HVR-IV sequence from S. procyonis SSU DNA to haplotype D (GB: AB272234.1 and AB205054.1) (Table 3). A HVR-IV haplotype 99% similar to the Strongyloides sp. Okayama (GB: LC038066.1) was detected in dog 45. Therefore, the HVR-IV sequence of Strongyloides sp. Okayama was assigned to haplotype H, and the sequence from dog 45 was assigned to Haplotype I. Consequently, four new haplotypes detected in four Australian dog samples were assigned to HVR-IV haplotypes E, F, G and I (Fig 1, Tables 3 and 4).
Clustering of Strongyloides stercoralis based on cox1 sequences
A 217 base pair fragment of cox1 was sequenced from 20 Australian specimens including those from 18 dogs and two humans, plus the S. ratti control (21 cox1 sequences in total). Multiple cox1 types were obtained from a single specimen in many cases, revealing infections caused by multiple helminth species and multiple S. stercoralis genotypes in a single host (Fig 1). Dendrogram construction by agglomerative nested clustering revealed three distinct S. stercoralis clades, including one occupied predominantly by worms possessing the II/A SSU genotype, which constituted sequences obtained from dogs and humans. Four cox1 sequences obtained in this study (one from each of human 1, human 3, dog 6, and dog 18), were assigned to the dog and human-infecting S. stercoralis clade. A S. stercoralis clade occupied mostly by specimens possessing the I/B and V/B SSU genotypes was also apparent (one specimen possessed the IV/B genotype), representing dog infections only (dog clade 1). None of the Australian specimens were assigned to this clade (Fig 1). A final S. stercoralis clade containing cox1 sequences obtained from only dogs (dog clade 2) was also dominated by specimens possessing the I/B and V/B genotypes, though two specimens were also assigned the IV/B. A single cox1 sequence from each of dogs 6 and 7 was assigned to this clade (Fig 1).
Cryptic cox1 sequences potentially from Strongyloides sp. helminths that could not be assigned to a genus or species
Sequences were obtained from two dog fecal specimens (dogs 22 and 43) that potentially belong to a Strongyloides sp. helminth but could not be confidently assigned to a species given the information available. Two cox1 sequences were obtained for dog 22. One of these clustered with a cox1 sequences from Strongyloides mirzai (GB: AB526307.1), a nematode that infects a Japanese pit viper. The second sequence from dog 22 clustered between the S. mirzai clade and the S. fuelleborni clade yet also clustered in a position immediately basal to all hookworms (Fig 1). This sequence also obtained a nearest BLASTN hit to a Necator sp. sequence (GB: AB793563.1), though its next best hit based on an online BLASTN search was to a sequence from S. stercoralis (GB: LC179452.1). Three unique cox1 sequences were obtained from dog 43 (GB: MK434220, MK434221; MK434222), one clustering with S. mirzai and a second clustering with two sequences of the Strongyloides sp. ‘loris’ clade (GB: LC197958.1, LC197946.1). When submitted to an online BLASTN search, the sequence clustering alongside S. mirzai also obtained top hits to free living nematodes (Ektaphelenchus sp. and Bursaphelenchus populi, GB: JX979197.1 and HQ699854.1 respectively), yet several of its top hits were also to S. fuelleborni cox1 sequences. The third sequence from dog 43 clustered between the Strongyloides sp. ‘loris’ clade and a clade containing all S. stercoralis sequences (Fig 1).
Mixed genotype infections with Strongyloides stercoralis
In two samples, dog 6 and dog 18, a complete set of sequences was obtained (a sequence for cox1, HVR-I and HVR-IV), which revealed mixed S. stercoralis genotype infections. When examining the number of reads that mapped to each haplotype for these specimens (S1 File), for dog 6 approximately 20% of reads were assigned to haplotype II and 80% to haplotype IV for the HVR-I region. For the HVR-IV region, approximately 20% of reads were assigned to haplotype A and 80% to haplotype B. With this information it can be assumed that this dog was infected with two strains of S. stercoralis, one from the human / dog clade (genotype II/A) and another from a dog-specific clade (genotype IV/B). However, it should be noted that the assays for amplification of HVR-I and HVR-IV could possess different amplification efficiencies, though this is difficult to confirm. Interestingly, two cox1 sequences were obtained from this dog, one assigned to the human / dog clade and another assigned to dog clade 2, supporting our deduction. Dog 18 was also infected with two types of S. stercoralis, with a genotype of II + VI / A + E assigned to this specimen. Given that the number of reads assigned to each of these types fell between 40% and 50%, it is difficult to link the HVR-I types identified here to their corresponding HVR IV type. While the specimen from dog 18 possessed two 18S haplotypes for HVR-I and HVR-IV, evidence was only found for a single cox1 sequence. There were two S. stercoralis haplotypes found in the HVR-IV region of the dog 13. Approximately 50% of reads were assigned to the haplotype A and 50% to a new haplotype G.
Detection of non-Strongyloides sp. cox1 sequences in remote Australian communities
Dog samples were collected from seven remote communities in Australia. While all specimens included in this study tested positive or presumed positive for S. stercoralis using a published real-time PCR assay [26], deep sequencing found no evidence of S. stercoralis infection in several cases where instead, an infection with another helminth (usually Ancylostoma spp.) was confirmed based on cox1 sequences. Some of these sequences clustered closely to A. ceylanicum yet appeared to be distinct. However, it should be noted that these sequences were identical to a published sequence assigned to A. caninum (GB: AJ407962.1) which did not overlap completely with our amplicon (50 bases short), so we cannot be sure they possess the same sequence type. This necessitates the conservative assignment of these sequences to Ancylostoma sp.
Twenty-three cox1 sequences were attributed to Ancylostoma spp. and one dog (dog 6) was infected with an Ancylostoma sp. clustering closely with Anyclostoma ceylanicum (Fig 1, cyan clade), and two distinct types of S. stercoralis. Sequences were obtained from dogs 14, 15 and 16 that belong to a Metastrongylus-like helminth, possibly Metastrongylus salmi. Two sequences attributed to Ancylostoma caninum were also obtained from dog 15, and a fourth sequence belonging to an Ancylostoma sp. was also detected in this dog. A sequence was obtained from dog 37 that obtained BLASTN hits to S. fuelleborni sequences (e.g., GB: AB526303.1, 86.2% identity). Agglomerative nested clustering placed this sequence in a position basal to all Strongyloides and hookworm sequences included in this analysis. This cox1 sequence also obtained close BLASTN hits (87% identity) to Aphelenchoides sp. (GB: KX356839.1) and Bursaphelenchus luxuriosae (AB097863.1) which are free living mycophagous and/or potentially plant parasitic nematodes. The cox1 sequence from dog 28 does not appear to be helminth in origin and most closely resembles a cox1 sequence from a rotifer; Macrotrachela quadricornifera (GB: JX184003.1), which served as a convenient outgroup for the clustering analysis (Fig 1).
Two dogs from community 2 were also infected with S. stercoralis while in one dog from community 5, a cryptic Strongyloides sp. possessing a unique SSU haplotype for both HVR-I and HVR-IV was detected (dog 22, genotype VIII/F). Interestingly, a Metastrongylus-like cox1 sequence was detected in all dogs from community 3 that were tested, and a single dog (dog 15) from this same community was infected with A. caninum and at least one other Ancylostoma sp. (Fig 2, cyan clade). We propose that sequences obtained from community 6 are from environmental organisms, possibly representing extraneous contaminants given that one represents a rotifer-like sequence (dog 28) (GB: MK434225) and the other obtained BLASTN hits to free-living nematodes (dog 37) (GB: MK434224). Community 4 and community 7 are each represented by a single typed specimen each (dog 18 and dog 45 respectively), that include unique sequences from a helminth that we can confidently assign to the genus Strongyloides (Fig 1).
Discussion
In our study we observed that HVR-IV haplotype A is associated with strains infective for both humans and dogs, while HVR-IV haplotype B is restricted to strains that are only infectious to dogs. The same was discovered in a recent study on S. stercoralis from humans and dogs in Cambodia, where two genetically distinguishable S. stercoralis populations were identified based on the HVR-IV region. The HVR-IV haplotype A strain was found to be dog and human infective, while HVR-IV haplotype B strain was shown to be dog specific [21]. Supporting earlier findings, our results also showed that haplotype II of HVR-I is found in combination with haplotype A of the HVR-IV region, and haplotype IV of the HVR I region is only found in combination with haplotype B, which is specific to dogs. One dog had a mixed S. stercoralis infection, presumably with worms of the genotype II/A (a type infectious to dogs and humans) and others with the genotype IV/B (a dog specific type). The detection of two cox1 sequences that cluster in the dog / human and dog specific clades respectively supports this assessment. In an Australian dog, we also identified HVR-I haplotype VI which has only been previously reported in European dogs. Interestingly, this dog (dog 18) also had a mixed genotype infection that included a novel S. stercoralis HVR-IV haplotype (haplotype E), that was linked to a cox1 sequence clustering in the dog / human S. stercoralis clade.
In agreement with previous reports, the current study demonstrated that the HVR-IV region in the SSU rDNA can be used to detect within species differences that correspond with the genetic clades that appear when the same specimens are analyzed at the cox1 locus [21, 27] (Fig 1). To support analysis of the cox1 locus by deep sequencing, the cox1 PCR assay described here was designed so that merged paired-end Illumina reads span the entire length of the amplicon. This greatly reduces the complexity of in silico analysis when mixed cox1 haplotypes are encountered. A trade-off of using a short amplicon for this analysis is that it may capture less diversity. Additionally, short sequences are of limited use in phylogenetic analysis. However, phylogenies are only truly relevant for inferring the evolutionary history of taxa and because evolutionary analysis was not the objective of this study, agglomerative nested clustering was used to group cox1 sequences based on their pairwise sequence identity. Despite its limitations, our cox1 assay clearly resolved the dog and human infective S. stercoralis types into a clade that is distinct from the dog-specific types, which was our primary objective, and allowed us to compare our results to those obtained in previous studies. Furthermore, we show that the cox1 fragment amplified here clearly distinguishes S. stercoralis-derived cox1 amplicons from other helminth species including S. fuelleborni and multiple species of hookworm.
As part of this study, we included certain SSU sequences previously published in GenBank in order to incorporate our novel haplotypes into the typing scheme. A sequence published in 1993 by Putland et al. (1993) (GB: M84229.1) has been assigned Haplotype C at its HVR-IV region in this study, differing from HVR-IV haplotype A by one SNP at position 125 (Fig 2) [28]. This sequence was later found to be a PCR induced hybrid sequence with the HVR-I region derived from a fungal contaminant [28, 29]. Our analysis confirmed that its HVR-I sequence is so drastically different to that of other S. stercoralis haplotypes (and to that of any other Strongyloides spp. in general), and was not added to the typing scheme. Next, we observed that S. stercoralis HVR-I haplotype IV (reportedly a dog-specific type) is also found in sequences assigned to S. procyonis from a Japanese badger (GB: AB272234.1). To reconcile this observation, we incorporated the HVR-IV region of sequences assigned to S. procyonis into the typing scheme, referring to them as haplotype D (Table 4, GB: AB272234.1 and AB205054.1). This also meant that the HVR-I sequence of the S. procyonis SSU (GB: AB205054.1) became HVR-I haplotype VII. Hence, the new SSU HVR-I haplotype from dog 22 (GB: MK468661) became SSU HVR-I haplotype VIII. A novel SSU HVR-I haplotype from dog 45 was also discovered as part of this study (GB: MK468662), and its sequence was most similar to the SSU HVR-I region from Strongyloides sp. Okayama, isolated from a Japanese striped snake (GB: LC038066.1). As this sequence was already in GenBank prior to the commencement of this study, the HVR-I region of LC038066.1 was assigned to haplotype IX, while the novel sequence obtained from dog 45 was assigned to haplotype X (GB: MK468662). As haplotypes A to D for HVR-IV had been assigned to other sequences, the novel haplotypes discovered in dogs 18, 22 and 13 were assigned to HVR-IV haplotype E, F and G respectively (GB: MK468674, MK468675, and MK468676). Finally, the HVR-IV sequence from Strongyloides sp. Okayama (GB:LC038066.1) was assigned to haplotype H because it obtained a nearest match to the HVR-IV regions sequenced from dog 45, which was consequently assigned to haplotype I (GB: MK468677). Also note that all HVR-I and HVR-IV types discussed above (both novel and previously published) are more similar to each other than they are to the corresponding SSU regions from S. ratti. Consequently, they do not provide enough information on their own to make confident species assignments (Fig 2).
While the typing scheme developed by Jaleta et al. (2017) was originally designed to consider S. stercoralis haplotypes alone, the detection of several novel cryptic haplotypes that: (1) cannot be confidently assigned to a species, (2) are nonetheless greater than 99% similar to each other and to known S. stercoralis haplotypes and (3), are haplotypes detected in the same host (dogs), means that the adjustments made here represent the most straightforward solution to the issue at hand. Being an isolated continent, it is possible that Australian dogs might be infected with genetically distinct S. stercoralis strains [30]. Consequently, it is not unreasonable to suggest that some of the cryptic dog Strongyloides types described herein (i.e., from dogs 18, 22, 13 and 45) might be attributable to truly novel S. stercoralis genotypes restricted to Australia. We also propose that some of the cryptic Strongyloides sp. haplotypes we discovered in this study are potentially unique to the Australian continent and may have diverged from Southeast Asian Strongyloides populations as a result of vicariance. Discovery of a cox1 sequence that clusters most closely to a Strongyloides sp. identified from a slow loris might support this (dog 43, GB: MK434221), given that lorises are endemic to southeast Asia, yet the lack of any SSU sequences associated with this specimen makes it difficult to draw any solid conclusions in that regard. A larger sample number is needed along with additional sequences and morphological analysis of multiple specimens before these sequences can be assigned to a species of helminth.
This study employed an alteration of the Jaleta et al. [21] genotyping assay developed at the Centers for Disease Control and Prevention (J. Barratt) for adaptation to NGS technologies. The assay was designed to genotype Strongyloides sp. and potentially detect mixed helminth infections (e.g., hookworm and Strongyloides) when applied directly to DNA extracted from faeces and other biological specimens. This method has great advantages over previous genotyping techniques in that it can be undertaken directly from faecal DNA extracts and does not require culture of larvae for extraction of DNA from individual worms. Furthermore, the depth of sequencing provided by NGS allows the detection of all genotypes in a single sample [31]. However, it is also worth mentioning that no information about the genotype of individual worms is obtained using this method. If two 18S haplotypes are found in one sample it remains unclear if they occur in the same individuals (heterozygous) or if they represent different populations. Also, if multiple variants are detected for more than one of the genotyping loci analysed here (i.e., SSU and cox1), it remains unclear which SSU sequence belongs to which cox1 sequence.
This study had a number of limitations including the collection of dog stool samples from the environment where they could have possibly become contaminated with extraneous environmental organisms or their DNA. As noted in Table 1, the cox1 PCR employed in this study also detects multiple hookworm species, and was even found to amplify the cox1 sequence of a Metastrongylus-like helminth. This may represent an advantage of the method if simultaneous detection and genotyping of multiple pathogenic intestinal nematodes from dogs and humans is required. However, these results should be viewed with caution. Given the sensitivity of deep sequencing, we suspect that detection of cox1 sequences resembling those of Metastrongylus salmi could be attributable to the consumption of pig offal by dogs in community 3. While Metastrongylus sp. are known to occasionally infect other species including humans [32], the genus is generally thought to be specific to pigs. We also note that the haplotypes from dog 45 closely resembles that of a reptile-infecting Strongyloides sp. and its presence in a dog could be due to consumption of reptiles or reptile feces by the dog. Consequently, these cases may represent incidental findings rather than true infections with a Metastrongylus-like helminth or a Strongyloides sp. resembling those found in reptiles. Similarly, the cox1 assay described here detected DNA from potentially free–living nematodes. A sequence obtained from dog 37 received a BLASTN hit to S. fuelleborni (GB: AB526306.1), though with only 86.2% identity. However, agglomerative nested clustering placed this sequence in a position basal to all Strongyloides and hookworm sequences included in this analysis. This sequence also obtained close BLASTN hits (87% identity) to Aphelenchoides sp. (GB: KX356839.1) and Bursaphelenchus luxuriosae (AB097863.1) which are mycophagous and/or potentially plant parasitic nematodes. This sequence could therefore represent a free-living nematode that came into contact with the fecal specimens in the environment between when the stool was passed and collected. Surprisingly, a sequence similar to one obtained from a rotifer; a free-living, extremely distant relative of nematodes, was detected in the specimen from dog 28 using this assay. This also likely represents contamination of the stool specimen from the local environment prior to its collection.
Our study was able to independently support previous reports of at least two genetically distinct groups of S. stercoralis; one infecting both dogs and humans and another group that is specific to dogs. While this study does not demonstrate direct transmission of S. stercoralis from dogs to humans or vice versa, it supports the hypothesis of zoonotic transmission in remote Australian communities. As discussed previously and with respect to the One Health approach [33], we suggest that humans and dogs should be treated concomitantly in these communities to control strongyloidiasis [16, 21]. Ultimately, we confirm for the first time that potentially zoonotic S. stercoralis populations are present in Australia and suggest that dogs might represent a potential reservoir of human strongyloidiasis in remote Australian communities.
Supporting information
The GenBank accession numbers are provided for the SSU HVR I and IV haplotypes generated in this study (MK468654-MK468677). The GenBank accession numbers are provided for the cox1 haplotypes generated in this study (MK434217- MK434258). Read mapping statistics are also provided to support the validity of each sequence.
(XLSX)
Fasta file containing sequences used to construct the cox1 BLAST database.
(FASTA)
Acknowledgments
The authors would like to thank Professor Robert W. Baird and Dr Richard Sullivan at the Royal Darwin Hospital, Darwin Pathology, NT and Dr Gemma Robertson at the Health Support Queensland, QLD for providing us human S. stercoralis DNA samples We would also like to acknowledge the contribution of Animal Management in Rural and Remote Indigenous Communities, Environmental Health Branch at the Department of Health, NT and all the other lovely veterinarians across Australia for helping us collecting dog faecal samples in the remote communities. We acknowledge the help of Dr Rogan Lee, Dr Matthew Watts, John Clancy and Vishal Ahuja at the Westmead Hospital, NSW with sending us S. ratti infected rat faeces. We wish to thank staff at the Centers for Disease Control and Prevention in Atlanta, USA.
Data Availability
All relevant data are within the manuscript and its Supporting Information files. All Accession numbers are available from the Genbank and are provided in S1 File.
Funding Statement
The work has been supported by the Australian Government Research Training Program Scholarship and Flinders University Overseas Travelling Fellowship. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Sequencing, bioinformatics, and genotyping assay design were funded by the Centers for Disease Control and Prevention's Advanced Molecular Detection Initiative.
References
- 1.Grove DI. Human strongyloidiasis Advances in Parasitology. 38: Elsevier; 1996. p. 251–309. [DOI] [PubMed] [Google Scholar]
- 2.Olsen A, van Lieshout L, Marti H, Polderman T, Polman K, Steinmann P, et al. Strongyloidiasis–the most neglected of the neglected tropical diseases? Transactions of the Royal Society of Tropical Medicine and Hygiene. 2009;103(10):967–72. 10.1016/j.trstmh.2009.02.013 [DOI] [PubMed] [Google Scholar]
- 3.Bisoffi Z, Buonfrate D, Montresor A, Requena-Méndez A, Muñoz J, Krolewiecki AJ, et al. Strongyloides stercoralis: a plea for action. PLoS Neglected Tropical Diseases. 2013;7(5):e2214 10.1371/journal.pntd.0002214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beknazarova M, Whiley H, Ross K. Strongyloidiasis: A Disease of Socioeconomic Disadvantage. International Journal of Environmental Research and Public Health. 2016;13(5):517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thanchomnang T, Intapan PM, Sanpool O, Rodpai R, Tourtip S, Yahom S, et al. First molecular identification and genetic diversity of Strongyloides stercoralis and Strongyloides fuelleborni in human communities having contact with long-tailed macaques in Thailand. Parasitology Research. 2017;116(7):1917–23. 10.1007/s00436-017-5469-z [DOI] [PubMed] [Google Scholar]
- 6.Pampiglione S, Ricciardi M. The presence of Strongyloides fuelleborni von Linstow, 1905, in man in Central and East Africa. Parassitologia. 1971;13(1/2). [PubMed] [Google Scholar]
- 7.Ashford R, Barnish G, Viney M. Strongyloides fuelleborni kellyi: Infection and disease in Papua New Guinea. Parasitology Today. 1992;8(9):314–8. [DOI] [PubMed] [Google Scholar]
- 8.Page W, Shield J, O’Donahoo F, Miller A, Judd J, Speare R. Strongyloidiasis in Oceania Neglected Tropical Diseases-Oceania: Springer; 2016. p. 69–99. [Google Scholar]
- 9.Heydon G, Green A. Some Worm Infestations of Man. in Australia. Medical Journal of Australia. 1931;1(21). [Google Scholar]
- 10.Sampson I, Smith D, MacKenzie B, editors. Serological diagnosis of Strongyloides stercoralis infection. Second National Workshop on Strongyloidiasis, Royal Brisbane Hospital, Hernston, Australia; 25–26 June 2003.
- 11.Miller A, Young E, Tye V, Cody R, Muscat M, Saunders V, et al. A community-directed integrated Strongyloides control program in Queensland, Australia. Tropical Medicine and Infectious Disease. 2018;3(2):48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holt DC, Shield J, Harris TM, Mounsey KE, Aland K, McCarthy JS, et al. Soil-Transmitted Helminths in Children in a Remote Aboriginal Community in the Northern Territory: Hookworm is Rare but Strongyloides stercoralis and Trichuris trichiura Persist. Tropical Medicine and Infectious Disease. 2017;2(4):51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kearns TM, Currie BJ, Cheng AC, McCarthy J, Carapetis JR, Holt DC, et al. Strongyloides seroprevalence before and after an ivermectin mass drug administration in a remote Australian Aboriginal community. PLoS Neglected Tropical Diseases. 2017;11(5):e0005607 10.1371/journal.pntd.0005607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Page WA, Dempsey K, McCarthy JS. Utility of serological follow-up of chronic strongyloidiasis after anthelminthic chemotherapy. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2006;100(11):1056–62. 10.1016/j.trstmh.2005.12.006 [DOI] [PubMed] [Google Scholar]
- 15.Constable S, Dixon R, Dixon R. For the love of dog: the human–dog bond in rural and remote Australian indigenous communities. Anthrozoös. 2010;23(4):337–49. [Google Scholar]
- 16.Beknazarova M, Whiley H, Ross K. Mass drug administration for the prevention human strongyloidiasis should consider concomitant treatment of dogs. PLoS Neglected Tropical Diseases. 2017;11(8):e0005735 10.1371/journal.pntd.0005735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goncalves A, Machado G, Goncalves-Pires M, Ferreira-Junior A, Silva D, Costa-Cruz J. Evaluation of strongyloidiasis in kennel dogs and keepers by parasitological and serological assays. Veterinary Parasitology. 2007;147(1):132–9. [DOI] [PubMed] [Google Scholar]
- 18.Takano Y, Minakami K, Kodama S, Matsuo T, Satozono I. Cross infection of Strongyloides between humans and dogs in the Amami Islands, Japan. Tropical Medicine and Health. 2009;37(4):149–52. [Google Scholar]
- 19.Hasegawa H, Hayashida S, Ikeda Y, Sato H. Hyper-variable regions in 18S rDNA of Strongyloides spp. as markers for species-specific diagnosis. Parasitology Research. 2009;104(4):869–74. 10.1007/s00436-008-1269-9 [DOI] [PubMed] [Google Scholar]
- 20.Hasegawa H, Sato H, Fujita S, Nguema PPM, Nobusue K, Miyagi K, et al. Molecular identification of the causative agent of human strongyloidiasis acquired in Tanzania: dispersal and diversity of Strongyloides spp. and their hosts. Parasitology International. 2010;59(3):407–13. 10.1016/j.parint.2010.05.007 [DOI] [PubMed] [Google Scholar]
- 21.Jaleta TG, Zhou S, Bemm FM, Schär F, Khieu V, Muth S, et al. Different but overlapping populations of Strongyloides stercoralis in dogs and humans—Dogs as a possible source for zoonotic strongyloidiasis. PLoS Neglected Tropical Diseases. 2017;11(8):e0005752 10.1371/journal.pntd.0005752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nagayasu E, Htwe MPPTH, Hortiwakul T, Hino A, Tanaka T, Higashiarakawa M, et al. A possible origin population of pathogenic intestinal nematodes, Strongyloides stercoralis, unveiled by molecular phylogeny. Scientific Reports. 2017;7(1):4844 10.1038/s41598-017-05049-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Basso W, Grandt L-M, Magnenat A-L, Gottstein B, Campos M. Strongyloides stercoralis infection in imported and local dogs in Switzerland: from clinics to molecular genetics. Parasitology research. 2018;118(1):255–66. 10.1007/s00436-018-6173-3 [DOI] [PubMed] [Google Scholar]
- 24.Clutton-Brock J. Origins of the dog: domestication and early history. The domestic dog: Its evolution, behaviour and interactions with people. 1995:7–20. [Google Scholar]
- 25.Beknazarova M, Millsteed S, Robertson G, Whiley H, Ross K. Validation of DESS as a DNA Preservation Method for the Detection of Strongyloides spp. in Canine Feces. International Journal of Environmental Research and Public Health. 2017;14(6):624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Verweij JJ, Canales M, Polman K, Ziem J, Brienen EA, Polderman AM, et al. Molecular diagnosis of Strongyloides stercoralis in faecal samples using real-time PCR. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2009;103(4):342–6. 10.1016/j.trstmh.2008.12.001 [DOI] [PubMed] [Google Scholar]
- 27.Hasegawa H, Kalousova B, McLennan MR, Modry D, Profousova-Psenkova I, Shutt-Phillips KA, et al. Strongyloides infections of humans and great apes in Dzanga-Sangha Protected Areas, Central African Republic and in degraded forest fragments in Bulindi, Uganda. Parasitology International. 2016;65(5):367–70. [DOI] [PubMed] [Google Scholar]
- 28.Putland R, Thomas S, Grove D, Johnson A. Analysis of the 18S ribosomal RNA gene of Strongyloides stercoralis. International Journal for Parasitology. 1993;23(1):149–51. [DOI] [PubMed] [Google Scholar]
- 29.Dorris M, Viney ME, Blaxter ML. Molecular phylogenetic analysis of the genus Strongyloides and related nematodes. International journal for parasitology. 2002;32(12):1507–17. [DOI] [PubMed] [Google Scholar]
- 30.Cawood PA, Korsch R. Assembling Australia: Proterozoic building of a continent. Precambrian Research. 2008;166(1–4):1–35. [Google Scholar]
- 31.Zahedi A, Gofton AW, Jian F, Paparini A, Oskam C, Ball A, et al. Next Generation Sequencing uncovers within-host differences in the genetic diversity of Cryptosporidium gp60 subtypes. International Journal for Parasitology. 2017;47(10–11):601–7. 10.1016/j.ijpara.2017.03.003 [DOI] [PubMed] [Google Scholar]
- 32.Calvopina M, Caballero H, Morita T, Korenaga M. Human pulmonary infection by the zoonotic Metastrongylus salmi Nematode. The first reported case in the Americas. The American Journal of Tropical Medicine and Hygiene. 2016;95(4):871–3. 10.4269/ajtmh.16-0247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rock M, Buntain BJ, Hatfield JM, Hallgrímsson B. Animal–human connections, “one health,” and the syndemic approach to prevention. Social science & medicine. 2009;68(6):991–5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The GenBank accession numbers are provided for the SSU HVR I and IV haplotypes generated in this study (MK468654-MK468677). The GenBank accession numbers are provided for the cox1 haplotypes generated in this study (MK434217- MK434258). Read mapping statistics are also provided to support the validity of each sequence.
(XLSX)
Fasta file containing sequences used to construct the cox1 BLAST database.
(FASTA)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files. All Accession numbers are available from the Genbank and are provided in S1 File.