Abstract
Teaching status/academic ranking may play a role in the variations in trauma center (TC) outcomes. Our study aimed to determine the relationship between TC teaching status and injury-adjusted, all-cause mortality in a national sampling.
Retrospective review of the National Sample Program (NSP) from the National Trauma Data bank (NTDB). TCs were categorized based on teaching status. Adjusted mortality was determined by observed/expected (O/E) mortality ratios, derived using TRauma Injury Severity Score methodology from the Injury Severity Score and Revised Trauma Score. Chi-square and t test analyses were utilized with a statistical significance defined as P <.05.
Of the 94 TCs in the NSP, 46 were university, 38 were community teaching, and 10 were community nonteaching. For the University TCs, 62.8% were American College of Surgeons (ACS) level 1 and 81.2% state level 1. Of the community teaching TCs, 39.0% was ACS level 1 and 35.1% was state level 1. Of the community nonteaching TCs, 0% was ACS level 1 and 11.1% was state level 1. University TCs had a significantly higher O/E mortality rate than community teaching (0.75 vs 0.71; P = .04). There were no differences in O/E between community teaching and nonteaching TCs (0.71 vs 0.70; P = .70).
Community teaching and nonteaching TCs have lower injury-adjusted, all-cause mortality rates than University Centers. Future studies should further investigate key differences between University TCs and community teaching TC to evaluate possible quality and performance improvement measures.
Keywords: National Trauma Data Bank, observed/expected (O/E) mortality, trauma center teaching status
1. Introduction
Teaching status is a vital component in the development and advancement of trauma centers (TCs). The teaching status of a TC influences its designation, yet is infrequently examined as a contributor to TC outcomes. Teaching status, such as whether a TC is a University TC, community teaching TC, or community nonteaching TC, may be key in understanding the variations in TC outcomes. The current clinical consensus on the impact of teaching status on patient outcomes is both limited and conflicting.
There is some evidence suggesting that teaching hospitals have superior outcomes as compared with nonteaching hospitals in certain nontrauma diseases. Dimick et al[1] evaluated outcomes after esophageal resection, liver resection, and pancreases resection performed in teaching hospitals compared with nonteaching hospitals and determined that procedures done in teaching centers had lower raw operative mortality. Similarly, Polanczyk et al[2] determined the effect of teaching status on mortality and outcomes. They found that mortality rates for heart failure, myocardial infarction, and stroke in New York were significantly lower in major teaching hospitals than in nonteaching hospitals.[2] Looking at traumatic injuries, Kelley-Quon et al[3] examined clinical outcomes observed for injured children treated at a single community facility before and after the hospital became an academic-community partner. For their pediatric trauma care, this change was associated with improved outcomes for injured children, but no change in mortality.[3] These studies provide support for the claim that teaching status may have better outcomes than nonteaching status.
Kupersmith[4] reviewed 15 studies that evaluated mortality in teaching hospitals and nonteaching hospitals. Looking at a variety of diseases, 9 of the 15 studies showed significantly lower morality in teaching hospitals. They also found better quality of care in teaching hospitals compared with nonteaching hospitals.[4] Comparably, Silber et al[5] found that for Medicare patients with general surgery, orthopedic, and vascular surgery admission, teaching hospitals had lower mortality than nonteaching hospitals. They also uncovered that survival after surgery is higher at teaching hospitals with higher teaching intensity due to lower mortality after complications and generally not because of fewer complications.[5]
Alternatively, some evidence indicates there is no difference in outcomes between teaching and nonteaching hospitals. Khuri et al[6] examined Veterans Administration (VA) teaching and nonteaching hospitals for noncardiac surgery. This was to determine whether education and training places patients at risk for worse outcomes than nonteaching settings and found that teaching and nonteaching VA hospitals have comparable risk-adjusted mortality rates.[6] Likewise, Papanikola et al,[7] and also Au et al[8] both conducted a literature review of outcome differences between teaching and nonteaching hospitals for a variety of diseases. They both determined that there were no significant differences in outcomes between teaching and nonteaching centers.[7,8] Thus, some evidence suggests there might not be difference in performance between teaching and nonteaching hospitals for a variety of diseases.
The teaching status of a TC is important in the state designation and American College of Surgeons (ACS) verification of TCs. According to the ACS, level 1 TCs have a major responsibility for providing leadership in medical education programs, clinical research, and prevention programs, which is not expected of level 2 TCs. Although, it is clarified that level 1 and level 2 TCs are expected to be clinically equivalent. Additionally, most state verifications follow similar guidelines. Therefore, teaching status is a particularly important factor in the characterization of a TC and may be a key in understanding the variations in TC outcomes.
To date, there are no national studies examining injury-adjusted all-cause mortality differences between TCs of differing levels of teaching status. Our study aimed to determine the relationship between TC teaching status and observed/expected (O/E) mortality for university, community teaching, and community nonteaching TCs. We hypothesize that teaching TCs performance measured by O/E mortality is superior to nonteaching TCs.
1.1. Study design and methods
A retrospective cohort review was done using the National Sample Program (NSP) from the National Trauma Data Bank (NTDB) of the year 2013, the most recent year of which all data were available at the inception of this study. Use of the 2013 NSP provided the most current data analysis of TC teaching status. The NSP, established as a nationally representative sample of US TCs, is a stratified sample of TCs drawn based on probability-proportional-to-size methodology. The NSP undergoes enhanced data validation screening. All identifying information has been concealed by the ACS to ensure confidentiality while including demographics, injury information, and outcomes to allow accurate analyses. This study received an exempt determination from our institutional review board.
The 94 TCs provided by the NSP were categorized based on teaching status into University TC, community teaching TC, or community nonteaching TC categories. This study analyzed all centers available in the NTDB NSP; there were no centers excluded. Adjusted mortality was determined by using O/E mortality ratios, derived using TRauma Injury Severity Score (TRISS) methodology from the Injury Severity Score (ISS) and Revised Trauma Score (RTS).
The most commonly used analysis to determine expected outcomes from the NTDB is O/E ratios. To determine expected this, the vital signs and injury pattern are utilized to predict survivability. The initial vital signs are combined in a scoring system called the RTS. The formula for RTS uses the initial Glasgow Coma Score with the initial systolic blood pressure (SBP) and initial spontaneous respiratory rate. Each of the 3 components is indexed to a value between 0 and 4. The formula is as follows:
Next, the injury pattern is quantified using the anatomically oriented Abbreviated Injury Scale (AIS) created by the Association for the Advancement of Automotive Medicine. The body is divided into 8 regions and the injuries are rated from 1 (most mild) to 5 (most severe). The single highest scored injury from up to 3 body regions is then used to calculate the ISS. The formula is:
where A, B, and C represent the AIS scores of the 3 most severely injured body regions. Now, the final step to have a predicted probability of survival (Ps) is to combine the RTS with the ISS in a valued labeled TRISS or Ps. In this formula,
where b = b0 + b1 (RTS) + b2 (ISS) + b3 (age index) and b0 = −0.4489 for blunt and −2.5355 for penetrating; b1 = 0.8085 for blunt and 0.9934 for penetrating; b2 = −0.0835 for blunt and −0.0651 for penetrating; b3 = −1.7430 for blunt and −1.1360 for penetrating; and age index = 0 for 54 or younger and 1 for age >54.
The O/E mortality rates were compared among TCs of differing teaching status. Chi-square and t test analyses were used for categorical variables, with a statistical significance defined as P <.05. This study was reported according to the STROBE guidelines.
2. Results
The 2013 NSP contained 94 TCs with 172,387 total trauma patients who had blunt and penetrating injuries. Among the trauma patients analyzed, 63.6% were male, 70.6% white, and the mean age was 41 years old. Of the trauma patients, 89% had blunt injuries and 11% had penetrating injuries. The teaching status breakdown of the 94 TCs in the NSP were that 46 were university, 38 were community teaching, and 10 were community nonteaching TCs. Mean age did not significantly differ for university (40.1 years, standard deviation [SD] 32.0) versus community teaching (42.0 years, SD 39.1) versus community nonteaching TCs (41.0 years, SD 35.4).
When stratified by TC designation, the majority of University TCs were ACS and state level 1, whereas the community teaching and nonteaching centers were both majority ACS and state level 2. Of the TCs with university status, 62.8% were ACS level 1 and 81.2% state level 1, 7.5% were ACS level 2 and 9.9% were state level 2, the remaining were classified as not applicable. Of the community teaching TCs, 39.0% were ACS level 1 and 35.1% were state level 1, 39.4% were ACS level 2 and 42.7% state level 2, the remaining were classified as not applicable. Of the community nonteaching TCs, 0% was ACS level 1 and 11.1% were state level 1, whereas 54.3% were ACS level 2 and 78.4% were state level 2, the remaining were classified as not applicable.
University TCs had a higher raw death rate compared with community teaching (3.24% vs 2.70%); this may be expected as the university hospitals had a higher injury burden based on ISS. After adjustment for injury and RTS, the university TCs had a significantly higher O/E mortality rate than community teaching (0.75 vs 0.71; P = .04). There were no differences in O/E mortality between community teaching and nonteaching TCs (0.71 vs 0.70; P = .70) (Table 1 and Fig. 1). The mean ISS for University TCs was significantly higher at 7.68 versus community teaching TCs (6.69; P < .0007) and versus community nonteaching TCs (6.45; P = .0001) (Table 2). There was, however, no significant difference in the mean RTS for University centers 7.47 versus community teaching centers (7.55; P = .05) versus community nonteaching centers (7.57; P = .13) (Table 2).
Table 1.
Teaching status and O/E injury-adjusted mortality.
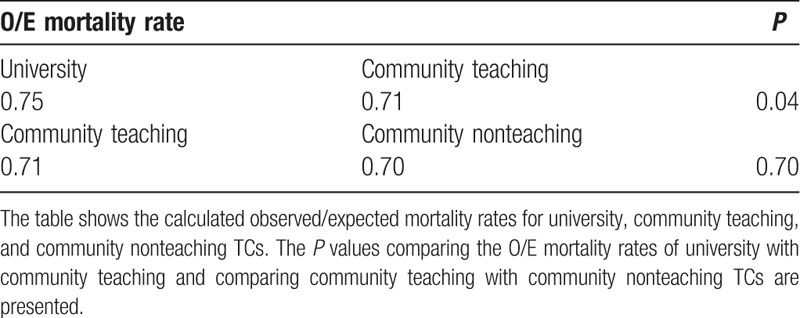
Figure 1.
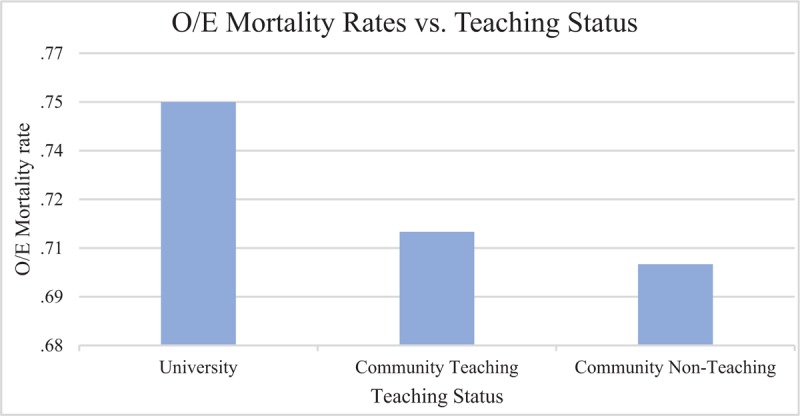
Teaching status and O/E injury-adjusted mortality shows the comparison of university, community teaching, and community nonteaching O/E mortality rates. The university TC O/E mortality rates are significantly higher than that of the community teaching TC. O/E = observed/expected; TC = trauma center.
Table 2.
TC Characteristics by teaching status.
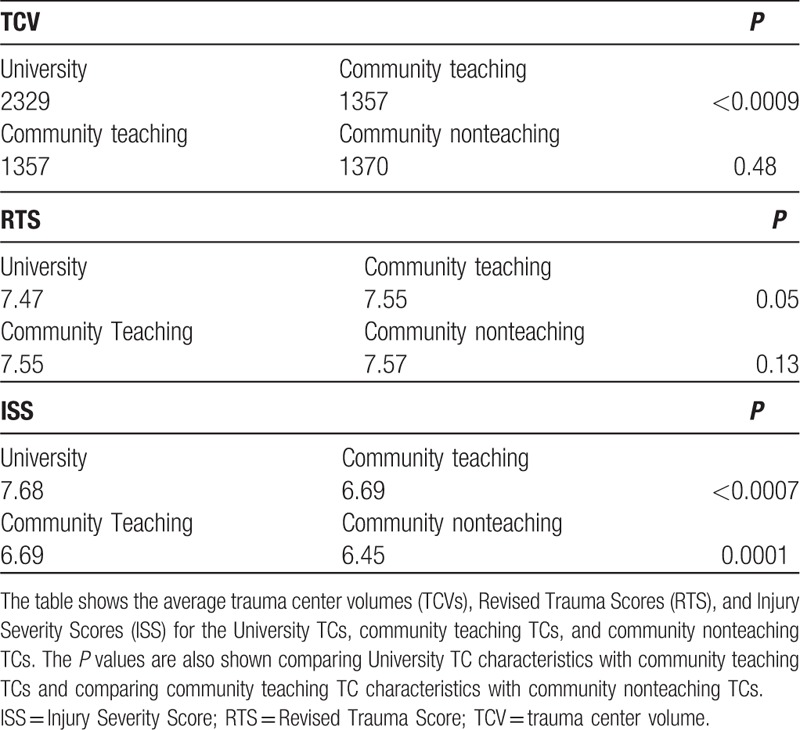
Concerning TC volume (TCV), university teaching TCs cared for a significantly higher annual trauma patient volume compared with community teaching TCs (2329 vs 1357; P < .0009), whereas community nonteaching TCs had 1370 average annual patient volume (Table 2).
3. Discussion
There is a long-standing debate concerning the outcome differences between teaching and nonteaching TCs, primarily due to the fundamental role teaching TCs play in the future of medicine and the inherit risk that comes with apprentice physicians. It is disputed whether teaching hospitals had superior outcomes to nonteaching hospitals. Recently, Burke et al[9] examined risk-adjusted outcomes for Medicare patients with a variety of diseases admitted to teaching and nonteaching hospitals, and found that major teaching status was associated with lower mortality rates for common conditions compared with nonteaching status. Similarly, Allison et al[10] examined the association of teaching status with quality of care and mortality for Medicare patients with an acute myocardial infarction, and determined admission to a teaching hospital was associated with better quality of care based on quality indicators and lower mortality.
In our study, there was no significant difference in injury-adjusted mortality rates between community teaching TCs and nonteaching TCs. However, the differences emerged when considering university TCs. University TCs had both a higher raw death rate and significantly higher O/E mortality rate than community teaching TCs. This is currently the only contemporary study to uncover this difference between university TC outcomes and community teaching TC outcomes. This demonstrates that a component of the community teaching TCs is associated with lower injury-adjusted mortality rates, and if determined, may help to lower the mortality rates in all TCs.
The community teaching TC injury-adjusted mortality rate, as compared with university TC mortality rate, is remarkable. From the present study, university TCs had a higher annual TCV, possibly explaining the difference in mortality. TCV is a reporting of the annual number of trauma admissions at a TC. Generally, high TCV centers admit greater than 1200 patients annually, whereas low TCV centers admit less.[11] This higher volume could result in higher complication rates and cause the higher mortality rates. For instance, Tepas et al[12] evaluated the relationship between case volume and outcome as measured by mortality, and found a trend of increasing mortality with increasing volume, despite a consistent proportion of severe injury. This study exemplifies that high-volume centers may have an over demand of resources which results in higher mortality. Conversely, other studies have demonstrated higher TCV improve outcomes. Brown et al[13] recently evaluated the association of TCV change over time with mortality and uncovered that increasing volume was associated with improved outcomes, whereas decreasing volume was associated with worsened outcomes. This demonstrates that university TCs should theoretically have lower mortality than community teaching TCs based on corresponding annual volume. The finding that university TCs have a higher injury-adjusted mortality rate denotes a need to expand quality improvement efforts in university teaching centers.
The majority of university TCs in this study were designated and verified level 1 TCs, whereas the majority of community teaching TCs were designated and verified level 2 TCs. Considering that level 1 and level 2 trauma centers are expected to be clinically equivalent, it is notable that the community teaching TCs, which are mostly level 2 TCs, have lower mortality rates. Future studies should further examine the impact of both teaching status and TC designation and verification level on trauma outcomes to better define the relationship between teaching TC level and patient mortality.
In this analysis, university TCs had a similar RTS, but a higher ISS, indicating the patients were more severely injured. This would explain the higher raw mortality rate because more severely injured patients often necessitate more resources and predictably result in poorer outcomes. University TCs have a significantly higher injury-adjusted mortality compared with community teaching TCs. Although, the question may not be what university TCs are doing wrong, but rather what community teaching TCs are doing better. Future studies should further investigate key differences, such as patient care, administrative handling, and policies and procedures, between university TCs and community teaching TCs to evaluate possible quality and performance improvement measures.
While this study demonstrates a significant finding, there are some limitations. In the analysis of retrospective data from the NTDB, limitations arise that are common to the use of any large dataset. This includes potential misclassification of injuries or complications, inconsistency, unrepresentativeness, and variability. Further, this study included only 1 year of NTDB data. There are limitations inherent with TRISS methodology and TRISS is vulnerable to missing data; TRISS discriminates well between survivors and nonsurvivors, but lacks predictive reliability, and TRISS is particularly limited for predicting outcome in some specific subsets of patients.[14] Nevertheless, TRISS continues to be used widely in the trauma community and was used here because there is not a generally accepted comparable alternative.
Teaching TCs are vital in the development and advancement of medicine in trauma care settings; nevertheless, it is important to monitor quality improvement in those teaching TCs. Community teaching TCs, as demonstrated in this study, provide evidence that both training and quality care can be accomplished with even lower injury-adjusted mortality rates.
4. Conclusions
Community teaching and non-teaching trauma centers have lower injury-adjusted, all-cause mortality rates than university centers. Community teaching centers demonstrate that both training and quality care can be accomplished with even lower injury-adjusted mortality rates. Future studies should further investigate fundamental differences between university and community teaching TC care to identify possible quality improvement measures.
Author contributions
Conceptualization: Adel Elkbuli, Brianna Dowd, Rudy Flores, Dessy Boneva, Mark McKenney.
Data curation: Adel Elkbuli, Brianna Dowd, Rudy Flores, Mark McKenney.
Formal analysis: Adel Elkbuli, Rudy Flores.
Investigation: Adel Elkbuli, Brianna Dowd, Rudy Flores, Dessy Boneva, Mark McKenney.
Methodology: Adel Elkbuli, Brianna Dowd, Rudy Flores, Dessy Boneva, Mark McKenney.
Project administration: Adel Elkbuli, Brianna Dowd, Mark McKenney.
Resources: Adel Elkbuli, Dessy Boneva, Mark McKenney.
Supervision: Adel Elkbuli, Dessy Boneva, Mark McKenney.
Validation: Adel Elkbuli, Brianna Dowd, Rudy Flores, Mark McKenney.
Writing – original draft: Adel Elkbuli, Brianna Dowd, Rudy Flores, Dessy Boneva, Mark McKenney.
Writing – review & editing: Adel Elkbuli, Brianna Dowd, Rudy Flores, Dessy Boneva, Mark McKenney.
Adel Elkbuli orcid: 0000-0001-7730-617X.
Footnotes
Abbreviations: ACS = American College of Surgeons, AIS = Abbreviated Injury Scale, ISS = Injury Severity Score, NSP = National Sample Program, NTDB = National Trauma Data Bank, O/E = observed/expected, Ps = probability of survival, RTS = Revised Trauma Score, SD = standard deviation, TC = trauma center, TCV = trauma center volume.
The authors have no conflicts of interest to disclose.
References
- [1].Dimick JB, Cowan JA, Jr, Colletti LM, et al. Hospital teaching status and outcomes of complex surgical procedures in the United States. Arch Surg 2004;139:137–41. [DOI] [PubMed] [Google Scholar]
- [2].Polanczyk CA, Lane A, Coburn M, et al. Hospital outcomes in major teaching, minor teaching, and nonteaching hospitals in new york state. Am J Med 2002;112:255–61. [DOI] [PubMed] [Google Scholar]
- [3].Kelley-Quon LI, Crowley MA, Applebaum H, et al. Academic-community partnerships improve outcomes in pediatric trauma care. J Pediatr Surg 2015;50:1032–6. [DOI] [PubMed] [Google Scholar]
- [4].Kupersmith J. Quality of care in teaching hospitals: a literature review. Acad Med 2005;80:458–66. [DOI] [PubMed] [Google Scholar]
- [5].Silber JH, Rosenbaum PR, Romano PS, et al. Hospital teaching intensity, patient race, and surgical outcomes. Arch Surg 2009;144:113–20. [discussion 121]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Khuri SF, Najjar SF, Daley J, et al. Comparison of surgical outcomes between teaching and nonteaching hospitals in the Department of Veterans Affairs. Ann Surg 2001;234:370–82. [discussion 382-383]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Papanikolaou PN, Christidi GD, Ioannidis JP. Patient outcomes with teaching versus nonteaching healthcare: a systematic review. PLoS Med 2006;3:e341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Au AG, Padwal RS, Majumdar SR, et al. Patient outcomes in teaching versus nonteaching general internal medicine services: a systematic review and meta-analysis. Acad Med 2014;89:517–23. [DOI] [PubMed] [Google Scholar]
- [9].Burke LG, Frakt AB, Khullar D, et al. Association between teaching status and mortality in US hospitals. JAMA 2017;317:2105–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Allison JJ, Kiefe CI, Weissman NW, et al. Relationship of hospital teaching status with quality of care and mortality for medicare patients with acute MI. JAMA 2000;284:1256–62. [DOI] [PubMed] [Google Scholar]
- [11].Elkbuli A, Eily A, Hai S, et al. The impact of trauma center volume on observed/expected mortality: does size matter? Am Surg 2018;84:1236–9. [PubMed] [Google Scholar]
- [12].Tepas JJ, 3rd, Patel JC, DiScala C, et al. Relationship of trauma patient volume to outcome experience: can a relationship be defined? J Trauma 1998;44:1. [DOI] [PubMed] [Google Scholar]
- [13].Brown JB, Rosengart MR, Kahn JM, et al. Impact of volume change over time on trauma mortality in the United States. Ann Surg 2017;266:173–8. [DOI] [PubMed] [Google Scholar]
- [14].Gabbe BJ, Cameron PA, Wolfe R. TRISS: does it get better than this? Acad Emerg Med 2004;11:181–6. [PubMed] [Google Scholar]


