Abstract
Aim of this study was to determine if surface electromyography (sEMG) could provide objective data in monitoring the alteration of signal amplitude of myoelectric activity of the paraspinal muscles in the patients with acute nonspecific lower back pain (ANLBP), and to explore the correlation between sEMG data and symptom relief in the ANLBP patients before and after massage therapy.
Forty-five ANLBP patients and 20 healthy subjects were enrolled into this study. Patients were given massage therapy for 1 week. The average electromyography (AEMG), visual analogue scale (VAS), and distance of finger to floor (DFTF) were measured before and after treatment.
AEMG at flexion and maintained flexion positions were significantly higher in the ANLBP group compared to that in the control group. At extension position, in contrast, AEMG was significantly lower in the ANLBP patients than that of control group, and there was no significant difference between the 2 groups at upright position. After massage therapy for the ANLBP patients, AEMG was significantly reduced at flexion and maintained flexion positions, but significantly increased at extension position than that before treatment. VAS and DFTF were also significantly reduced after treatment. In addition, AEMG alteration at maintained flexion position was significantly correlated with improvement of VAS or DFTF.
Myoelectric activity of the paraspinal muscles in the ANLBP patients was different from that of healthy subjects. Massage therapy not only relived patients’ symptoms, but also normalized myoelectric activity of the paraspinal muscles in the ANLBP patients.
Keywords: low back pain, massage therapy, paraspinal muscles, surface electromyography
1. Introduction
Lower back pain is a common and complicated disorder with high prevalence rates in many countries.[1,2] Acute nonspecific lower back pain (ANLBP) is a disease caused by soft tissue injury, which is hardly visualized by any objective examination including X-ray, computed tomography, or magnetic resonance imaging (MRI). Almost 85% of lower back pain is ANLBP.[2] Symptoms of ANLBP include severe lower back pain, paraspinal muscle spasm, and limited lower back movement.
Although the exact pathophysiology of ANLBP is still not clearly understood and lack of objective methods to detect injured muscles, it seems that evaluation of myoelectric activity of the paraspinal muscles by surface electromyography (sEMG) is of great value in the assessment of such patients. In this regard, it has been reported that characteristics of myoelectric activity of the paraspinal muscles in the patients with lower back pain assessed by sEMG was different from that in healthy subjects.[3]
Physical therapy, such as spinal manipulation and massage, have been used to treat lower back pain and to reset the tone of muscles associated with palpable tissue texture and tenderness.[4] The present study was designed to explore if sEMG could provide objective data in monitoring the alteration of signal amplitude of myoelectric activity of the paraspinal muscles in the ANLBP patients, and to explore its correlation with symptom relief in response to massage therapy in the patients.
2. Materials and methods
2.1. Patients
Total 45 patients with acute lower back pain, who visited Wuhan No. 1 Hospital between June 2012 and June 2013, were enrolled into this study. Twenty healthy volunteers were also enrolled. Informed consent form was obtained from each participant. This study was approved by The Institutional Review Board of Ethics Committee of Wuhan No. 1 Hospital.
2.2. Diagnosis of ANLBP
Patients with the following symptoms and signs were diagnosed as ANLBP: lower back pain, which did not radiate beyond the knees; had history of lower back injury; lumbar deformity, lower back muscle spasm, and limited movement; and significant lower back pain when pressed at physical examination.
2.3. Inclusion and exclusion criteria
Inclusion: patients diagnosed with acute lower back injury; aged from 20 to 60 years old; and willing to participate into the study and signed consent form.
Exclusion: bone damage and lumbar spine disc disease; had history of lower back surgery; severe diseases of nervous system or cardiovascular system, or severe metabolic disease; lower back skin disease; or pregnant.
2.4. Treatment method
Patients were positioned prone on a massage table and treated by experienced physical therapists twice a week by the following steps: circular friction and kneading motions on lower back muscles for 3 to 5 minutes; thumb compression on the pain points; stretch lumbar spine and muscles by pulling and extending patient's lower body; kneading and friction motion again for 3 to 5 minutes.
Before and after massage therapy, patient's symptom visual analogue scale (VAS) and distance of finger to floor (DFTF) were evaluated and sEMG was performed.
2.5. Surface electromyography
sEMG was conducted using a device (TE-TB0810) purchased from Anhui Bioforcen Intelligent Technology (Anhui, China) as following. Before electrode placement, skin on both side of L4 spine was abraded with fine sandpaper, and cleansed with 75% alcohol. Two disposable surface recording electrodes (diameter of the electrode paste was 15 mm) were applied on both side of the spine with 4 cm apart. Reference electrode was place 4 cm aside of the measuring electrodes. Each participant was familiarized the following body movement before placing the electrodes and instructed during the test: stood upright, slowly flexion till maximum (Flexion position), and maintained at the maximum flexion point for 5 seconds (Maintained Flexion position), then straightened up (Extension position) to upright position (Upright position). Data at aforementioned 4 positions were collected before the massage therapy and 1 week after the therapy followed by analyzing with a software. By fast Fourier transform, spectrum analysis was converted to average electromyography (AEMG) for the muscles along the spine at the aforementioned 4 positions.
2.6. Distance of finger to floor
Patients stood upright, slowly flexion with arms straiten down toward the floor. The patients stopped flexion movement when he/she felt back pain. The distance of finger to the floor was then measured. Each patient had 3 measurements.
2.7. Visual analogue scale
The intensity of back pain was measured using the VAS from 0 to 10, with 0 was no pain and 10 was extreme pain. VAS was also assessed before and after treatment.
2.8. Statistical analysis
Statistical analysis was performed using SPSS 17.0 software (Chicago, IL). Continuous data was compared by Student t test and counting data was compared by Chi-squared analysis. Correlation was analyzed by Pearson correlation coefficient analysis.
3. Results
3.1. Comparison of AEMG between ANLBP and control group
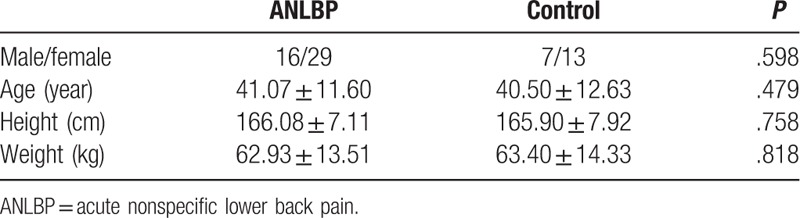
As shown in Table 1, there were no significant differences between the ANLBP and healthy groups in gender ratio, age, height, and weight.
Table 1.
Demographic characteristics of the participants.
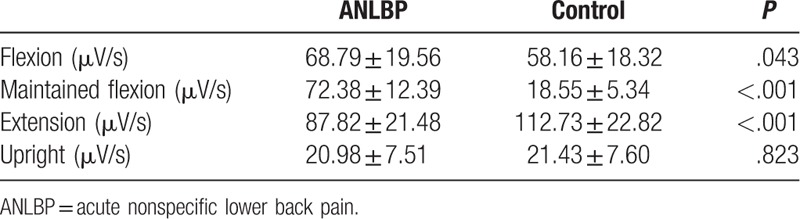
As shown in Table 2, AEMG at positions of flexion and maintained flexion were significantly higher in the ANLBP group (68.79 ± 19.56 μV/s at flexion and 72.38 ± 12.39 μV/s at maintained flexion) than that in the control group (58.16 ± 18.32 μV/s at flexion and 18.55 ± 5.34 μV/s at maintain flexion position, both P < .05 or .001, respectively). At extension position, however, AEMG was significantly lower in the ANLBP group (87.82 ± 21.48 μV/s) compared to that in control group (112.73 ± 22.82 μV/s, P < .001). There was no significant difference between the 2 groups at upright position.
Table 2.
Comparison of average electromyography in the 2 groups.
3.2. Comparison of AEMG and symptoms in ANLBP patients before and after treatment
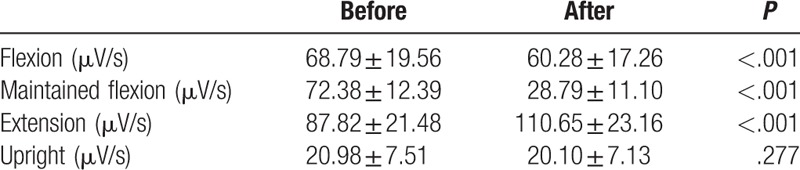
As expected, after massage therapy for the patients with ANLBP, AEMG was significantly decreased at flexion (60.28 ± 17.26 μV/s) and maintained flexion positions (28.79 ± 11.10 μV/s), but it was increased at extension position (110.65 ± 23.16 μV/s) compared to that before the therapy (68.79 ± 19.56 μV/s at flexion, 72.38 ± 12.39 μV/s at maintained flexion, and 87.82 ± 21.48 μV/s at extension, P < .001 in all, Table 3). AEMG at upright position did not significantly change after the treatment (Table 3).
Table 3.
Average electromyography in acute nonspecific lower back pain before and after therapy.
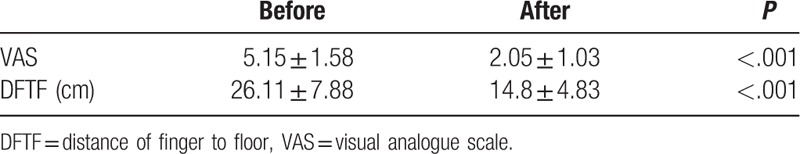
As shown in Table 4, VAS and DFTF were also significantly decreased after treatment (VAS: 5.15 ± 1.58 vs. 2.05 ± 1.03, P < .001; DFTF: 26.11 ± 7.88 cm vs. 14.8 ± 4.83 cm, P < .001).
Table 4.
Comparison of visual analogue scale and distance of finger to floor before and after therapy.
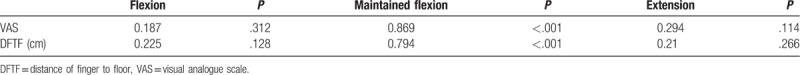
3.3. Correlation between AEMG change and symptom improvement
As shown in Table 5, there was significant correlation between AEMG change at maintained flexion position and VAS improvement (r = 0.869, P < .001) or DFTF (r = 0.794, P < 0.001). However, there was no significant correlation between VAS or DFTF and AEMG at flexion, extension, or upright position.
Table 5.
Correlation between changes of electromyography and symptom improvement.
4. Discussion
The purpose of this study was to analyze the myoelectric activity level of the paraspinal muscles by sEMG in the patients with ANLBP before and after massage therapy, and to determine if sEMG data is associated with therapeutic improvement of ANLBP. It was found that signal amplitude of the paraspinal muscles at flexion, maintained flexion, and extension positions was significantly different in the ANLBP patients in comparison to healthy subjects. Massage therapy could normalize the signal amplitude of the myoelectric activity of the paraspinal muscles, and improvements of VAS as well as DFTF were significantly correlated with the alteration of AEMG at maintained flexion position.
Signal amplitude of sEMG is positively related to the amount of force produced by the muscle.[5] Studies have reported both linear and nonlinear relationships between electromyography (EMG) signal amplitude and force production during the contraction of skeletal muscles.[6,7] In the patients with recurrent lower back pain, it has been reported that either general exercises for trunk muscle activation or with specific lumbar stabilization exercises resulted in improvement in function and reduced pain.[8,9] In the present study, ANLBP patients had significant improvement in VAS and DFTF after 1 week massage therapy, which positively reflected by the changing of the sEMG of the muscles in maintained flexion position, suggesting sEMG could be used to objectively assess lower back muscle functional change.
Lower back pain is a common and complicated disorder with high prevalence worldwide. Although the exact pathophysiology of lower back pain is still not clearly understood, evaluation of paraspinal muscles seems of great value in assessing outcomes of treatment in such patients. Among the objective methods, MRI,[10] ultrasonography,[11,12] and needle and sEMG[13,14] have become increasingly common methods to assess muscle activity in healthy subjects and in patients with lower back pain. Of these methods, sEMG appears to be more convenient for both the patients and the researchers to analyze lower back muscles activity in laboratory studies as well as in clinical trials.[15] Therefore, in the present study, sEMG was used to assess myoelectric activity of the paraspinal muscles in the ANLBP patients before and after treatment. It was found that signal amplitude of the paraspinal muscles analyzed by sEMG was significantly different before and after massage therapy in the patients with ANLBP, and that improvement of patients’ symptoms was significantly correlated with the alteration of EMG at maintained flexion position.
When a healthy person is at full body flexion position, the paraspinal muscles do not contract and thus no myoelectric activity is detectable because spine is stabilized by anatomic structure of spine including intervertebral disc, posterior longitudinal ligament, interspinous ligament, spinal ligament, and muscles. In contrast, at upright position, mild myoelectric activity can be detected in the paraspinal muscles by sEMG. When the body is in flexion movement, the paraspinal muscles act as antagonistic muscles to maintain compliance of the movement. During such a movement, gratitude and time length of myoelectric activity at flexion is less than that at extension position because the paraspinal muscles act as active muscles at extension, which results in increased myoelectric activity.[16]
Accumulating studies have shown that patient with lower back pain have the following 2 characteristics: decrease of muscle tolerance and imbalance of trunk muscle activity.[17] Spectrum analysis and time domain parameters of sEMG have been widely used to assess muscle functions. AEMG is the mean of sEMG signal amplitude, it reflects the motor unit action potential and myoelectric activity, and it is determined by muscle force and physiological function of the motor unit in the muscles. The present study, therefore, used AEMG to analyze the muscle activity. In addition, because the signal amplitude corresponds to the muscle force, time domain indicator is used to reflect muscle activity and status.
In the 20 normal subjects enrolled into this study, the signal of myoelectric activity was in alternative change between active and relaxed status when the muscle was at flexion position. Signal amplitude was significantly smaller at flexion position compared to that at extension in that the paraspinal muscles act as antagonistic force during flexion but active force during extension. In the ANLBP patients, pain, which was caused or worsened by flexion and extension movement, lead to increased antagonistic activity of the paraspinal muscles in order to reduce the pain. Such an activity resulted in significantly increased AEMG in the ANLBP patients compared to that of normal subjects. In contrast, the paraspinal muscle activity and myoelectric signal was smaller at extension, and thus, AEMG amplitude was decreased during extension. After 1-week massage therapy, symptoms were remarkably relieved and lower back function was recovered, which was reflected by the normalized AEMG signal of the paraspinal muscles and positive correlation between the symptom relief and AEMG signal change.
Taken together, the present study demonstrated that sEMG could objectively reflect lower back muscle activity, massage was effective for the treatment of ANLBP, and sEMG could be used for diagnosis of lower back tissue injury as well as for monitoring the recovery of the injury.
Author contributions
Conceptualization: Jie Qiao.
Data curation: Jun Zhang.
Formal analysis: Jun Zhang.
Investigation: Jie Qiao.
Methodology: Dan Feng.
Resources: Dan Feng.
Supervision: Shu-Li Zhang.
Validation: Dan Feng.
Visualization: Shu-Li Zhang.
Writing – original draft: Shu-Li Zhang.
Footnotes
Abbreviations: ANLBP = acute nonspecific low back pain, DFTF = distance of finger to floor, EMG = electromyography, sEMG = surface electromyography, VAS = visual analogue scale.
JQ and S-LZ contributed equally to this paper.
The authors have no conflicts of interest to disclose.
References
- [1].Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain 2000;84:95–103. [DOI] [PubMed] [Google Scholar]
- [2].Walker BF. The prevalence of low back pain: a systematic review of the literature from 1966 to 1998. J Spinal Disord 2000;13:205–17. [DOI] [PubMed] [Google Scholar]
- [3].Chiou SY, Koutsos E, Georgiou P, Strutton PH. Association between spectral characteristics of paraspinal muscles and functional disability in patients with low back pain: a cohort study. BMJ Open 2018;8:e017091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Koes BW, van Tulder MW, Ostelo R, et al. Clinical guidelines for the management of low back pain in primary care: an international comparison. Spine (Phila Pa 1976) 2001;26:2504–13. [DOI] [PubMed] [Google Scholar]
- [5].Seroussi RE, Pope MH. The relationship between trunk muscle electromyography and lifting moments in the sagittal and frontal planes. J Biomech 1987;20:135–46. [DOI] [PubMed] [Google Scholar]
- [6].Alkner BA, Tesch PA, Berg HE. Quadriceps EMG/force relationship in knee extension and leg press. Med Sci Sports Exerc 2000;32:459–63. [DOI] [PubMed] [Google Scholar]
- [7].Marras WS, Davis KG. A non-MVC EMG normalization technique for the trunk musculature: Part 1. Method development. J Electromyogr Kinesiol 2001;11:1–9. [DOI] [PubMed] [Google Scholar]
- [8].Koumantakis GA, Watson PJ, Oldham JA. Trunk muscle stabilization training plus general exercise versus general exercise only: randomized controlled trial of patients with recurrent low back pain. Phys Ther 2005;85:209–25. [PubMed] [Google Scholar]
- [9].Cairns MC, Foster NE, Wright C. Randomized controlled trial of specific spinal stabilization exercises and conventional physiotherapy for recurrent low back pain. Spine (Phila Pa 1976) 2006;31:E670–81. [DOI] [PubMed] [Google Scholar]
- [10].Lewis SE, Fowler NE. Changes in intervertebral disk dimensions after a loading task and the relationship with stature change measurements. Arch Phys Med Rehabil 2009;90:1795–9. [DOI] [PubMed] [Google Scholar]
- [11].Ghamkhar L, Emami M, Mohseni-Bandpei MA, Behtash H. Application of rehabilitative ultrasound in the assessment of low back pain: a literature review. J Bodyw Mov Ther 2011;15:465–77. [DOI] [PubMed] [Google Scholar]
- [12].Javanshir K, Amiri M, Mohseni-Bandpei MA, et al. Ultrasonography of the cervical muscles: a critical review of the literature. J Manipulative Physiol Ther 2010;33:630–7. [DOI] [PubMed] [Google Scholar]
- [13].Lariviere C, Arsenault AB. On the use of EMG-ratios to assess the coordination of back muscles. Clin Biomech (Bristol, Avon) 2008;23:1209–19. [DOI] [PubMed] [Google Scholar]
- [14].Koumantakis GA, Arnall F, Cooper RG, Oldham JA. Paraspinal muscle EMG fatigue testing with two methods in healthy volunteers. Reliability in the context of clinical applications. Clin Biomech (Bristol, Avon) 2001;16:263–6. [DOI] [PubMed] [Google Scholar]
- [15].Farina D, Gazzoni M, Merletti R. Assessment of low back muscle fatigue by surface EMG signal analysis: methodological aspects. J Electromyogr Kinesiol 2003;13:319–32. [DOI] [PubMed] [Google Scholar]
- [16].Li S. Effect of early continuous cold compress on the acute ankle injury. Guangxi Med 2007;29:1130–1. [Google Scholar]
- [17].Cass JR, Settles H. Ankle instability: in vitro kinematics in response to axial load. Foot Ankle Int 1994;15:134–40. [DOI] [PubMed] [Google Scholar]


