Abstract
Background
This multi-institutional retrospective real life study was conducted in 22 Italian Oncology Centers and evaluated the role of Axitinib in second line treatment in not selected mRCC patients.
Methods
148 mRCC patients were evaluated. According to Heng score 15.5%, 60.1% and 24.4% of patients were at poor risk, intermediate and favorable risk, respectively.
Results
PFS, OS, DCR and ORR were 7.14 months, 15.5 months, 70.6% and 16.6%, respectively. The duration of prior sunitinib treatment correlated with a longer significant mPFS, 8.8 vs 6.3 months, respectively. Axitinib therapy was safe, without grade 4 adverse events. The most frequent toxicities of all grades were: fatigue (50%), hypertension (26%), and hypothyroidism (18%). G3 blood pressure elevation significantly correlated with longer mPFS and mOS compared to G1-G2 or no toxicity. Dose titration (DT) to 7 mg and 10 mg bid was feasible in 24% with no statistically significant differences in mPFS and mOS. The sunitinib-axitinib sequence was safe and effective, the mOS was 41.15 months. At multivariate analysis, gender, DCR to axitinib and to previous sunitinib correlated significantly with PFS; whereas DCR to axitinib, nephrectomy and Heng score independently affected overall survival.
Conclusions
Axitinib was effective and safe in a not selected real life mRCC population.
Trial registration INT – Napoli – 11/16 oss. Registered 20 April 2016. http://www.istitutotumori.na.it
Keywords: Axitinib, Sunitinib, Metastatic, Renal cancer, Treatment
Background
The Target Therapies (TTs) have revolutionized the metastatic Renal Cell Carcinoma (mRCC) treatment with a significant advantage in Overall Survival (OS), from about 9 months in 1995, to a median of 28–29 months in 2013 [1–9]. Axitinib, a selective TKi of VEGFR-1, 2, 3, has been approved in Italy in second line treatment after sunitinib or cytokines failure. The phase III AXIS trials showed a significantly prolonged mPFS with axitinib, 6.7 months vs 4.7 months with sorafenib. In the subgroup of patients, pre-treated with sunitinib, median PFS was 4.8 months with axitinib vs 3.4 months with sorafenib (p = 0.011) [10]. The mOS was 20.1 months with axitinib (95% CI 16.7–23.4) vs 19.2 months with sorafenib (95% CI 17.5–22.3) (HR 0.969, 95% CI 0.800–1.174; p = 0.3744) [11]. Axitinib showed a good safety profile with diarrhea, fatigue and hypertension, as main side effects. At the time of this study analysis, the only registered drugs in this setting were: axitinib, everolimus and sorafenib. To date there are no head-to-head studies or randomized clinical trials, that provide conclusive information about the best second-line. Several ‘real world’ studies confirmed the efficacy and safety of Axitinb in a not selected population [12–24].
Patients and methods
Our multi-Institutional, retrospective study evaluated the outcomes of mRCC patients all treated in second-line therapy with axitinib after first-line sunitinib failure. Eligible patients were: age ≥ 18 years; histologically confirmed RCC; axitinib for at least 2 months, started between January 2014 and May 2017; at least one radiological assessment (CT scan) of disease (RECIST 1.1 criteria) repeated every 2–3 months; only sunitinib as previous treatment in first line. Axitinib was administered at starting dose of 5 mg bid (10 mg/die). Dose titration (DT) was performed every 2 weeks up to a final step of 10 mg bid in patients without adverse events ≥ grade 2. Primary endpoints were: progression free survival (PFS), overall survival (OS), objective response rate (ORR), disease control rate (DCR), and the safety profile of Axitinib and Sunitinib–Axitinib sequence. ORR was defined as the percentage of partial response (PR) and complete response (CR) during treatment and disease control rate (DCR) as the percentage of PR, CR and stable disease (SD) upon axitinib. Progressive disease (PD) was defined as: radiological tumor progression, or clinical progression, including death. PFS was defined as the interval between the date of the first dose of Axitinib and the date of the disease progression or death from any cause. Overall survival (OS) was defined from the start of axitinib to the date of death from any cause. The secondary objectives included the evaluation of a possible relationship between patients demographic and baseline characteristics, AEs and response to treatment. AEs were graded according to Common Terminology Criteria for Adverse Events (CTCAE version 4.0). Patients demographic and baseline characteristics, treatment patterns and AEs were collected, with categorical variables being described by patients counts and percentages. Univariate analysis for median progression free survival and overall survival was performed by Kaplan–Meier estimator: PFS and OS curves were obtained and selected variables were compared using two-sided log-rank test. Hazard ratios (HR) were calculated by Cox Regression multivariable analysis, performed according to a backward elimination of factors showing a p value ≥ 0.10, and adjusted for age (continuous variable) and center. A p value ≤ 0.05 was considered statistically significant. The SPSS statistical package version 23.0 (SPSS Inc., Chicago, IL) was used for all statistical analysis.
Results
Between January 2014 and May 2017, twenty-two Italian Oncology Centers collected clinical data regarding 148 patients, after approval by the Institutional Board of National Cancer Institute “G. Pascale”–IRCCS of Napoli, Italy. All patients gave consent to participate. Patients demographic and baseline characteristics were collected in Table 1: median age was 62 years (range: 35–85 years), with good balance between males and females (50.7% vs 49.3%, respectively); 55.4% had ECOG 0 Performance Status. 134/148 (90.5%) patients had undergone prior nephrectomy and only 6% (9/148) had a histological diagnosis other than clear cell carcinoma. Lung was the most affected site of metastases (56.8%) and 22.3% (33/148) of patients had liver metastases. 11.5%, 60.8% and 27.7% patients were MSKCC high risk, intermediate and favorable, respectively otherwise, according to Heng score, 15.5%, 60.1% and 24.4% patients were poor, intermediate and favorable risk, respectively. All patients received sunitinib as first line treatment according to the Italian guidelines: 18% of patients received modified schedule of sunitinib (2 week on 1 week off). All patients started axitinib at standard dose of 5 mg bid. Dose titration to 7 and 10 mg bid was performed in 23.6% of patients. Forty-nine percentage patients received further treatment lines (Table 2).
Table 1.
SAX patients characteristics
| N = 148 | % | |
|---|---|---|
| Median age years (range) | 62 | (35–85) |
| Age | ||
| < 75 | 126 | 85% |
| ≥ 75 | 22 | 15% |
| Gender | ||
| Male | 75 | 50.7% |
| Female | 73 | 49.3% |
| ECOG PS | ||
| 0 | 82 | 55.4% |
| 1 | 61 | 41.3% |
| 2 | 5 | 3.3% |
| Nephrectomy | ||
| Yes | 134 | 90.5% |
| No | 14 | 9.5% |
| MOTZER score | ||
| Poor | 17 | 11.5% |
| Intermediate | 90 | 60.8% |
| Favorable | 41 | 27.7% |
| Heng score | ||
| Poor | 23 | 15.5% |
| Intermediate | 89 | 60.1% |
| Favorable | 36 | 24.3% |
| Principal sites of disease | ||
| Lung | 84 | 56.8% |
| Lymph node | 55 | 37.2% |
| Bone | 39 | 26.4% |
| Liver | 33 | 22.3% |
| Adrenal glands | 10 | 6.8% |
| Brain | 9 | 6.1% |
| Local recurrence | 8 | 5.4% |
| Pancreas | 7 | 4.7% |
| Peritoneum | 6 | 4.1% |
| Contralateral kidney | 5 | 3.4% |
| Skin | 3 | 2% |
| Spleen | 2 | 1.4% |
Table 2.
SAX treatments characteristics
| N = 148 | (%) | |
|---|---|---|
| First line | ||
| Sutent | 148 | 100 |
| Sutent schedule | ||
| Modified | 27 | 18 |
| Standard | 121 | 82 |
| Axitinib dose | ||
| Standard | 113 | 76.4 |
| Titration | 35 | 23.6 |
| Therapy after axitinib | 73 | 49 |
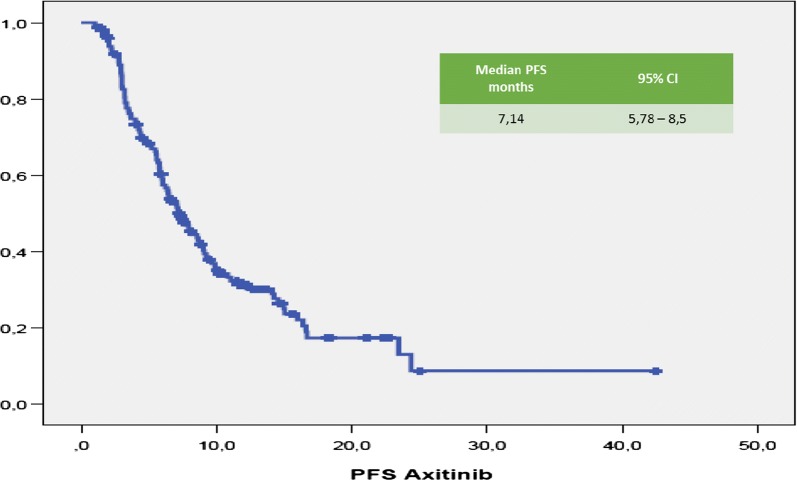
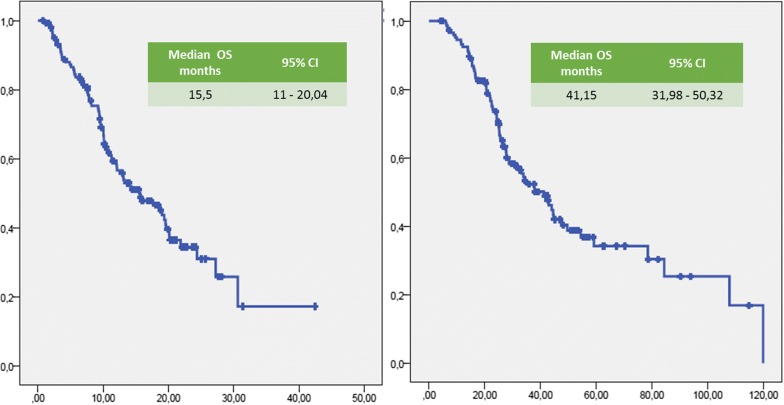
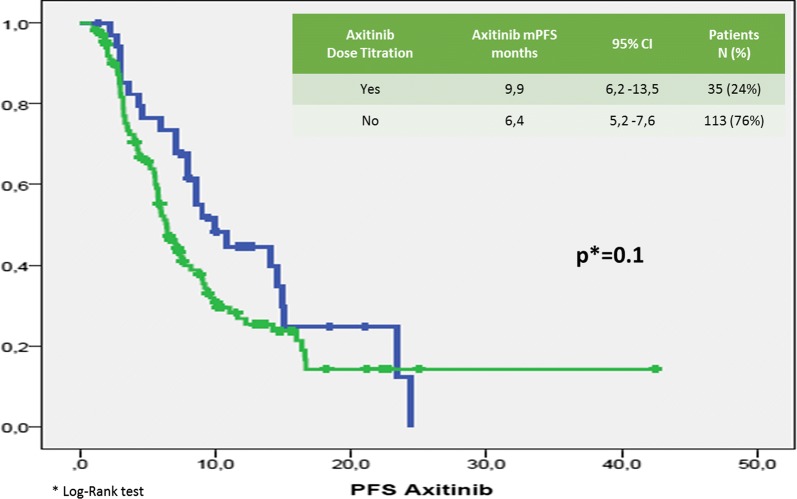
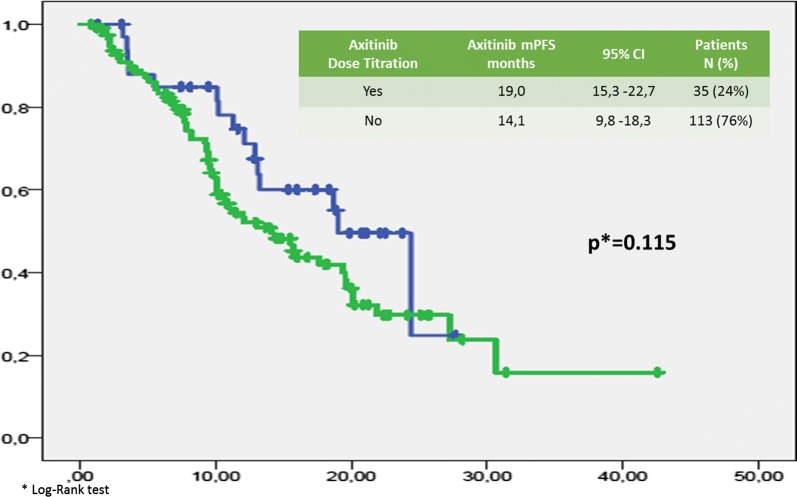
Median (m) PFS was 7.14 months (95% CI 5.78–8.5 months; Fig. 1). Median (m) OS from the start of Axitinib was 15.5 months (95% CI 11–20 months; Fig. 2). The median time of axitinib treatment duration was 8.1 months. The ORR, according to RECIST criteria version 1.1 [25] was 16.6%, with 16% of PR and one patient reached a CR (Table 3) and correlated to a statistically longer (p < 0.0000001) mPFS, 15.5 months (95% CI 7.9–22.1 months) vs 3.2 months (95% CI 2.95–3.445 months), respectively. The DCR with Axitinib was 70.6% and correlated to a statistically longer (p < 0.0000001) mPFS, 9.9 months (95% CI 7.59–12.22 months) vs 3.2 months (95% CI 2.95–3.44 months), respectively. mOS according to DCR and ORR upon axitinib was 20.1 vs 7.83 months (p < 0. 0000001) and 27.2 vs 7.8 months (p = 0. 000026), respectively. DCR and ORR to previous Sunitinib treatment were associated with longer statistically mPFS, 7.96 months (95% CI 6.49–9.42 months, p = 0. 00031) and 7.7 months (95% CI 5.8–9.7 months, p = 0.0011) vs 4.0 months (95% CI 1.14–6.68 months) and 4.0 months (95% CI 1.4–6.7 months), respectively; no statistically significant differences in mOS according to DCR upon sunitinib was recorded, 17.6 months (95% CI 12.9–22.4 months, p = 0.094) vs 7.8 months (95% CI 4.9–10.8 months); conversely, patients who achieved ORR with first line sunitinib had a significant longer median OS, 19.0 months (95% CI 12.7–25.4 months, p = 0.049) vs 4.0 months (95% CI 4.9–10.7 months). With stratifying patients by duration of prior sunitinib therapy (≤ vs > median duration), a statistically significant difference in mPFS was reported: patients with a median duration of Sunitinib ≥ 13.1 months experienced disease progression upon axitinib later than ones who progressed within 13 months (8.8 months vs 6.3 months, p = 0.021), without any difference in mOS (p = 0.151). We reported no differences in terms of mPFS according to previous sunitinib administration schedule, 13.1 months (95% CI 11.7–14.6 months) vs 12.7 (95% CI 9.7–15.7 months) (standard schedule vs modified schedule; p = 0.096); no difference in mOS (p = 0.205) according to alternative schedule vs standard, 17.6 months (95% CI 12.6–22.7 months) vs 10.2 months (95% CI 8.7–11.7 months). When patients were stratified by Heng score, mPFS was 5.8, 7.0 and 9.0 months according to poor, intermediate and favorable risk group (p = 0.066), with statistically significant difference in mOS (9.4 vs 14.3 vs 20.1 months, respectively p = 0.002); similar results were obtained by using Motzer score. Patients with better ECOG PS (0) experienced longer mPFS, 9.08 months (95% CI 6.80–11.3 months, p = 0.026) vs 6.2 months (95% CI 5.5–6.9 months) and mOS, 27.2 months (95% CI 12.0–42.4 months, p = 0.003) vs 10.9 months (95% CI 8.3–13.6 months). Prior nephrectomy significantly correlated to a longer mPFS, 7.7 vs 4.4 months (p = 0.001), as well as to longer mOS, 18.7 vs 8.2 months, (p = 0.000004). Axitinib at standard schedule of 5 mg bid was safe without grade 4 toxicity. Dose reduction occurred in 24% (35/148): the most common adverse events of all grades were fatigue (50.7%), gastro-intestinal disorders (36.5%), hypertension (26.4%), hypothyroidism (18.2%), dysphonia (12.2%), hand-foot syndrome (14.2%) (Table 5). At univariate analysis G3 blood pressure elevation (systolic ≥ 160 mmHg and/or diastolic ≥ 100 mmHg) significantly correlated with longer mPFS and mOS compared to G1–G2 or no toxicity (mean PFS 28.8 months, p = 0.017—mean 6 OS 38.15 months, p = 0.017—median survival times not reached for both analysis). Noteworthy, men compared to women showed both a longer mPFS (9 vs 5.8 months, p = 0.014) and mOS (19.5 vs 12 months, p = 0.048). The Sunitinib–Axitinib sequence, was well-tolerated, without worsening in side effects, particularly in terms of hypertension and hand–foot syndrome, with a mOS of 41.15 months (95% CI 32–50.32 months; Fig. 2). Tables 5 and 6 summarized the adjusted hazard ratios (HR) for PFS and OS: the Cox multivariate model, performed according to a backward elimination of factors showing a p value ≥ 0.10, was then adjusted for age, gender, and center; gender (male vs female: HR 0.567, 95% CI 0.378–0.851, p value = 0. 006), DCR upon axitinib (HR 0.171, 95% CI 0.107–0.272, p value < 0.0000001) and upon prior sunitinib (HR 0.549, 95% CI 0.308–0.977, p value = 0.04) showed a significant independent impact in terms of PFS; on the other hand, DCR upon axitinib (HR 0.336, 95% CI 0.192–0.590, p value = 0.0001), Heng score (poor prognosis vs favorable prognosis: HR 3.4, 95% CI 1.374–8.541, p value = 0.008—intermediate prognosis vs favorable prognosis: HR 2.06, 95% CI 1.04–4.0, p value = 0.04) and prior nephrectomy (HR 0.319, 95% CI 0.153–0.664, p value = 0.0022) independently affected overall survival (Table 4). Dose escalation to 7 or 10 mg bid was feasible in 35/148 patients (24.2%). mPFS was longer, but not statistically significant, than patients without dose titration, 9.9 months (95% CI 6.2–13.5 months, p = 0.1) vs. 6.4 months (95% CI 5.2–7.6 months), respectively. No difference in mOS was observed too (p = 0.115, Figs. 3, 4). Dose titration was well-tolerated without significant increase in side effects (Tables 5, 6, 7).
Fig. 1.
Kaplan-Meier curve of median PFS in our study population
Fig. 2.
Kaplan-Meier curve of median OS of the patients under study from the start of axitinib
Table 3.
Objective response in our study population
| Patient n = 148 | |
|---|---|
| Best response, (%) | |
| CR | 0.6 |
| PR | 16 |
| SD | 54 |
| PD | 29.4 |
| DCR (CR + PR + SD) | 70.6 |
| ORR (CR + PR) | 16.6 |
Table 5.
Axitinib toxicity
| Adverse event (%) | Standard dose | Titration | ||||
|---|---|---|---|---|---|---|
| Grade 1–2 87.3% |
Grade 3 12.7% |
Grade 4 0% |
Grade 1–2 86.6% |
Grade 3 13.4% |
Grade 4 0% |
|
| Haematologic | 9.5 | 0.7 | – | 11.4 | 2 | – |
| Hypertension | 20.9 | 5.4 | – | 25.7 | 5.7 | – |
| Gastro-intestinal | 32.4 | 4.1 | – | 34.3 | – | – |
| Hypothyroidism | 17.6 | 0.7 | – | 25.7 | – | – |
| Stomatitis/mucositis | 8.1 | – | – | 8.5 | – | – |
| Fatigue | 43.2 | 7.4 | – | 48.6 | 8.6 | – |
| Hepatic | 2.8 | 2 | – | 2.9 | 5.7 | – |
| Hand-foot syndrome | 12.2 | 2 | – | 17.2 | 2.9 | – |
| Dysphonia | 11.5 | 0.7 | – | 11.4 | 2.9 | – |
Table 6.
Cox multivariate analysis for PFS
| Progression-free survival (PFS) | |||
|---|---|---|---|
| HR | (95% CI) | p value | |
| DCR axitinib | 0.171 | (0.107–0.272) | < 0.0000001 |
| DCR sunitinib | 0.549 | (0.308–0.977) | 0.041 |
| Heng score | |||
| Good prognosis | 1 | 0.174 | |
| Poor prognosis | 1.909 | (0.964–3.779) | 0.064 |
| Intermediate | 1.249 | (0.752–2.073) | 0.391 |
| Nephrectomy | |||
| Yes | 0.572 | (0.305–1.072) | 0.081 |
| Gender | |||
| Male | 0.567 | (0.378–0.851) | 0.006 |
Table 4.
Univariate analysis of PFS and OS in our study population
| p value | ||
|---|---|---|
| mPFS | mOS | |
| Tumor response rate to axitinib | ||
| DCR | < 0.0000001 | < 0.0000001 |
| ORR | < 0.0000001 | 0.000026 |
| Tumor response rate to prior sunitinib | ||
| DRC | 0.00031 | 0.094 |
| ORR | 0.0011 | 0.049 |
| Duration prior sunitinib treatment ≥ 13.1 vs < 13.1 mo | 0.21 | 0.151 |
| HENG score | 0.066 | 0.002 |
| ECOG PS | 0.026 | 0.003 |
| Prior nephrectomy | 0.001 | 0.000004 |
| G3 blood pressure | 0.017 | 0.017 |
Fig. 3.
PFS by axitinib dose titration
Fig. 4.
OS by axitinib dose titration
Table 7.
Cox multivariate analysis for OS
| Overall survival (OS) | |||
|---|---|---|---|
| HR | (95% CI) | p-value | |
| DCR axitinib | 0.336 | (0.192–0.590) | 0.00015 |
| Performance status | |||
| ECOG 0 | 1 | 0.058 | |
| ECOG 1 | 0.872 | (0.183–4.160) | 0.863 |
| ECOG 2 | 1.706 | (0.359–8.108) | 0.502 |
| Heng score | |||
| Good | 1 | 0.025 | |
| Poor | 3.426 | (1.374–8.541) | 0.008 |
| Intermediate | 2.057 | (1.040–4.068) | 0.038 |
| Nephrectomy | |||
| Yes | 0.319 | (0.153–0.664) | 0.002 |
| Istology | |||
| Clear cell carcinoma | 0.402 | (0.149–1.079) | 0.070 |
| Gender | |||
| Male | 0.629 | (0.371–1.066) | 0.085 |
Discussion
Currently the goal of mRCC treatment strategy is represented by the correct use of the approved drugs in a sequential algorithm [26, 27]. Axitinib is licensed in Italy for the treatment of mRCC patients only after failure of sunitinib or cytokines therapy. We report herein the retrospective data of axitinib in Italian real-life practice for mRCC: despite our population was more “battered” than the one investigated in AXIS trial, our results are consistent with AXIS ones, confirming the efficacy of axitinib in second line treatment [10, 11], with ORR, mPFS and mOS of 16.6%, 7.14 and 15.5 months, respectively. Fifteen percentage of our study population was over 75 years, normally under-represented in clinical trials [28]. The elderly patients are usually a frail population with a lower performance status (PS), poor tolerance to medical treatments and multiple co-morbidities [29]. To date few data are available concerning the use of axitinib in elderly mRCC patients [30–32]. Our results showed no differences in both mPFS [6.4 months (95% CI 4. 95–7.95, p = 0.74)] and mOS [13.0 months (95% CI 5.9–20.15, p = 0.72)] than younger patients. In addition, there was no significant difference in the incidence of AEs or dose reduction, or discontinuation. The efficacy and safety of the VEGF-TKI -VEGF-TKI treatment sequence has been confirmed by various trials, showing a statistically longer mPFS and in some of these mOS too [10, 11, 26, 33, 34]. Leung et al. indicated axitinib as more appropriate TTs option, compared to sorafenib and pazopanib, in the second line setting; in particular, axitinib is associated with the lowest risk of withdrawal due to adverse events [35]. In post hoc analysis of the AXIS trial, Escudier et al. evaluated the efficacy of axitinib by response and duration of prior sunitinib or cytokines treatment, showed no statistically significant differences in PFS or OS in responders vs non-responders, although a significantly longer PFS and OS was reported in patients who had received a longer prior cytokines treatment [36]. On the contrary, our analysis showed that longer previous sunitinib duration (≤ vs > median duration), correlated with a statistically significant difference in mPFS (8.8 vs 6.3 months, p = 0.021), without any difference in mOS (p = 0.151). The same conclusion was reached by Elaidi et al. who showed that patients who remained on first-line TKI treatment between 11 and 22 months benefited from a TKI rechallenge rather than from second-line mTORi (PFS: 9.4 vs 3.9 months, p = 0.003) [37]. Higher ORR (20–30%) was reported with VEGF-TKI compared to mTORi (≤ 10%), which is supported by our analysis [38]. Dose titration to 7 or 10 mg bid was feasible in 24% (35/148) of our patients, lower than the axitinib Asian trial (61.5%) [39] or the AXIS trial (37%) [10], but higher than other real-world studies (16%) [21–23, 40, 41]. We reported no differences in both mOS (p = 0.115) and mPFS (p = 0.1), in accordance to the phase II study of first-line axitinib [17, 23] but in contrast to Matias et al. results, in which dose escalation at 2-weeks was associated to better ORR, PFS and TTF, but not OS. Patients with better ECOG PS (0) experienced longer mPFS, 9.08 (p = 0.026) vs 6.2 months and mOS, 27.2 (p = 0.003) vs 10.9 months. Prior nephrectomy significantly correlated with longer mPFS, 7.7 vs 4.4 months (p = 0.001), as well as longer mOS, 18.7 vs 8.2 months, (p = 0.000004). Axitinib at standard dose of 5 mg bid was safe, a dose reduction occurred in 24% (35/148), without any case of discontinuation: the most common AEs of all grades were: fatigue (50.7%), gastro-intestinal disorders (36.5%), hypertension (26.4%), hypothyroidism (18.2%), dysphonia (12.2%), hand-foot syndrome (14.2%) (Table 5). Our data showed a lower incidence of AEs than AXIS trial, the higher incidence of fatigue in our experience, was probably due to the difficulty to distinguish and explain to the patients the difference between fatigue and asthenia. All these results suggest that axitinib treatment is feasible and safe in this unselected real-world population. At univariate analysis hypertension G3 blood pressure elevation (systolic ≥ 160 mmHg and/or diastolic ≥ 100 mmHg) significantly correlated with longer mPFS and mOS compared to G1-G2 or no toxicity (mean PFS 28.8 months, p = 0.017—mean OS 38.15 months, p = 0.017—median survival times not reached for both analysis Table 6, 7). Our data are consistent with other real-world studies [42, 43] and AXIS trial, suggesting that the development of hypertension during the treatment could be a surrogate of survival in this population. It was interesting to note that the 18% (27/148) of patients enrolled in our study, adopted a modified schedule of sunitinib in first line (2 weeks on 1 week off), without showing any difference in outcomes. These data confirm those of others retrospective studies that evaluated sunitinib alternative schedules, showing a reduction in the AEs and achieving comparable outcomes to the standard schedule [44–46]. The identification of effective prognostic factors in mRCC patients receiving axitinib represents a new challenge. In these series we identified the following independent prognostic indicators: gender (male), DCR upon axitinib and prior sunitinib for PFS, and DCR upon axitinib, Heng score (poor prognosis vs intermediate vs good prognosis) and prior nephrectomy for OS. The sequence TKI–TKI (sunitinib-axitinib) was well tolerated without worsening in side effects, the global mOS was 41.15 months, higher than AXIS trial (33.7 months). The main limitation of our analysis was represented by the small patient numbers, selection bias, the retrospective nature, without centralized data review. Recently the results of three major clinical trials involving nivolumab, cabozantinib, and lenvatinib plus everolimus, showed superior efficacy in terms of response rates (RR) and OS in second-line setting [47–50] and these will change dramatically the therapeutic sequence in second-line setting. To date, there are few data about the best sequential therapeutic algorithm beyond first-line VEGF TKIs, and no head-to-head study between these new drugs and the currently approved agents are ongoing [51–54]. The mTORi everolimus is the only drug tested head-to-head with nivolumab, cabozantinib and lenvatinib plus everolimus, and no data are available with axitinib as comparator. Treatment selection in second line-setting, is based on several factors, including patient health status, contraindications and comorbidities, histologic RCC subtype, safety profiles, and previous treatment. Recently, Bracarda et al. published a Prognostic Factor Analyses from the AXIS Trial, that as well as our data, identified a subgroup of patients who had a long-term benefit with axitinib treatment. Therefore, axitinib could be suitable (post sunitinib) 2nd line treatment option for mRCC selected patients with VEGF-dependent mRCC, favourable/intermediate risk, low tumour burden, and no bone or liver metastases and with long life expectancy [55]. In the new era of Immunotherapy, are VEGF-TKIs still a valid option for mRCC treatment? The angiogenesis plays a central role in the RCC tumorigenesis and immunogenicity. The prevalence of pro-angiogenic factors over anti-angiogenic signals promotes an immunosuppressive tumor microenvironment, through abnormal tumor vessel formation and dysregulation of various immune cells. Therefore, anti-angiogenic therapy remains the gold standard in selected patients (VEGF-dependent favourable mRCC in all setting) and increases the efficacy of immunotherapy, modulating immune responses, increasing anticancer immune-trafficking and activity, through the regulation of tumor vessels and reducing suppressing cytokines and infiltrating T regs [54, 56, 57]. Different phase 3 trials evaluated or are evaluating combination of immune checkpoint inhibitors, such as anti PD-1 nivolumab and anti CTLA-4 ipilimumab, or anti PD-1/PDL-1 and VEGFR-TKI in first-line treatment, with impressive results that will dramatically impact on the choice of the first and second-line treatments (Table 8).
Table 8.
Real world trial data comparison
| mPFS (mo) | mOS (mo) | DCR (CR + PR + SD) (%) | |
|---|---|---|---|
| SAX real world | 7.14 | 15.5 | 70.6 |
| Spanish real world | 4.4 | 10.8 | 65.7 |
| France real world | 8.3, | 16.4, | 72 |
| AXIS | 6.5 | 15.2 | 69.3 |
Conclusions
Evidences emerging from our retrospective analysis are consistent with the available literature and confirm the efficacy and safety of axitinib in a not selected population, particularly in patients who most benefited from first-line sunitinib (VEGF-dependent mRCC). The advent of new drugs such as nivolumab and cabozantinib has further improved the therapeutic landscape of second line setting. Prospective trial will be needed to assess the right sequence of anti PD-1/PD-L1 and VEGF/VEGFRi and moreover, head to head studies will be needful to determine the best VEGFRi (cabozantinib vs axitinib) in second line setting, mostly after the impressive results of the combination trials of immune checkpoint inhibitors and immune checkpoint inhibitors with VEGFR-TKIs, in first-line therapy.
Acknowledgements
Not applicable.
Authors’ contributions
FG: Conceptualization, formal analysis, writing—original draft, and writing—review and editing, project administration, supervision, validation. RS, CC: Conceptualization, data curation, writing—original draft, and writing—review and editing, resources, validation. SS, CA: investigation, methodology, validation. VMG, CC, DLG, PE, CV, BU, NE,FA, AM, BN, LTL, IG, BL, GD, RE, DTM, DVR, LRG, GF, MP, DVF, SC, SC, PS, GV, BM, MA, GL. DGU, IR, CG, BC, D’AC: investigation, validation.
Funding
No funding for the research to declare.
Availability of data and materials
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The study was approved by the Institutional Board of National Cancer Institute “G. Pascale” – IRCCS - of Napoli Italy and all patients gave consent to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Barata PC, Rini BI. Treatment of renal cell carcinoma: current status and future directions. CA Cancer J Clin. 2017 doi: 10.3322/caac.21411. [DOI] [PubMed] [Google Scholar]
- 2.Rodriguez-Vida A, Hutson TE, Bellmunt J, Strijbos MH. New treatment options for metastatic renal cell carcinoma. ESMO Open. 2017;2(2):e000185. doi: 10.1136/esmoopen-2017-000185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bedke J, Gauler T, Grünwald V, Hegele A, Herrmann E, Hinz S, Janssen J, Schmitz S, Schostak M, Tesch H, Zastrow S, Miller K. Systemic therapy in metastatic renal cell carcinoma. World J Urol. 2017;35(2):179–188. doi: 10.1007/s00345-016-1868-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cavaliere C, D Aniello C, Pepa CD, Pisconti S, Berretta M, Facchini G. Current and emerging treatments for metastatic renal cell carcinoma. Curr Cancer Drug Targets. 2017 doi: 10.2174/1568009617666170209094030. [DOI] [PubMed] [Google Scholar]
- 5.Gill DM, Agarwal N, Vaishampayan U. Evolving treatment paradigm in metastatic renal cell carcinoma. Am Soc Clin Oncol Educ Book. 2017;37:319–329. doi: 10.14694/EDBK_174469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brugarolas J. Molecular genetics of clear-cell renal cell carcinoma. J Clin Oncol. 2014;32(18):1968–1976. doi: 10.1200/JCO.2012.45.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cavaliere C, D’Aniello C, Cecere S, Di Napoli M, Berretta M, De Domenico R, et al. Renal cancer: prognostic and predictive biomarkers. In: Islam R, et al., editors. Prognostic and predictive response therapy factors in cancer disease (Colorectal, Breast, Liver, Lung, Gastric, Renal and Prost ate Cancers) New York: Nova Science Publishers; 2015. pp. 147–174. [Google Scholar]
- 8.Liao L, Testa JR, Yang H. The roles of chromatin-remodelers and epigenetic modifiers in kidney cancer. Cancer Genet. 2015;208(5):206–214. doi: 10.1016/j.cancergen.2015.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.D’Aniello C, Cavaliere C, Licchetta A, Gnoni A, Pisconti S, Facchini G. Metastatic renal cancer: prognostic and predictive biomarkers. World Cancer Res J. 2014;1:e289. [Google Scholar]
- 10.Rini BI, Escudier B, Tomczak P, Kaprin A, Szczylik C, Hutson TE, Michaelson MD, Gorbunova VA, Gore ME, Rusakov IG, Negrier S, Ou YC, Castellano D, Lim HY, Uemura H, Tarazi J, Cella D, Chen C, Rosbrook B, Kim S, Motzer RJ. Comparative effectiveness of axitinib versus sorafenib in advanced renal cell carcinoma (AXIS): a randomised phase 3 trial. Lancet. 2011;378(9807):1931–1939. doi: 10.1016/S0140-6736(11)61613-9. [DOI] [PubMed] [Google Scholar]
- 11.Motzer RJ, Escudier B, Tomczak P, Hutson TE, Michaelson MD, Negrier S, Oudard S, Gore ME, Tarazi J, Hariharan S, Chen C, Rosbrook B, Kim S, Rini BI. Axitinib versus sorafenib as second-line treatment for advanced renal cell carcinoma: overall survival analysis and updated results from a randomised phase 3 trial. Lancet Oncol. 2013;14(6):552–562. doi: 10.1016/S1470-2045(13)70093-7. [DOI] [PubMed] [Google Scholar]
- 12.Sherman S, Amzal B, Calvo E, Wang X, Park J, Liu Z, Lin C, Casciano R. An indirect comparison of everolimus versus axitinib in US patients with advanced renal cell carcinoma in whom prior sunitinib therapy failed. Clin Ther. 2015 doi: 10.1016/j.clinthera.2015.09.013. [DOI] [PubMed] [Google Scholar]
- 13.Heng DY, Signorovitch J, Swallow E, Li N, Zhong Y, Qin P, Zhuo DY, Wang X, Park J, Stergiopoulos S, Kollmannsberger C. Comparative effectiveness of second-line targeted therapies for metastatic renal cell carcinoma: a systematic review and meta-analysis of real-world observational studies. PLoS ONE. 2014;9(12):e114264. doi: 10.1371/journal.pone.0114264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Basso U, Calvani N, De Giorgi U, De Tursi M, De Vivo R, Facchini G, et al. Trattamento di seconda linea del carcinoma renale metastatico me gestione del paziente: focus su axitinib. Future Oncol. 2014;1:5–74. [Google Scholar]
- 15.Wang H, Man L, Li G, Huang G, Wang J. Comparative efficacy and safety of axitinib versus sorafenib in metastatic renal cell carcinoma: a systematic review and meta-analysis. Onco Targets Ther. 2016;9:3423–3432. doi: 10.2147/ott.s100706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maroto P, Lainez N, Esteban E, Espinosa M, Juan MJ, Etxaniz O, Suarez C, Sepúlveda JM, Rubio G, Arranz Arija JA, Jimenez L, Saez MI, Puente J, Chirivella Gonzalez I, Gallardo E, Jurado JM, Garcia-Donas J, López Brea M, Garrido M, de Soto Prado Y, Otero D. Real life efficacy and safety of axitinib (AXI) in patients with renal cell carcinoma (RCC): results from the Spanish compassionate use program. Ann Oncol. 2014;25(suppl_4):iv280–iv304. doi: 10.1093/annonc/mdu337.42. [DOI] [Google Scholar]
- 17.Hutson Thomas, Jiao Xiaolong, Wilson Thomas, Cisar Laura A., MacLean Elizabeth A. Axitinib treatment among patients with mRCC in a U.S. community oncology setting: A retrospective study of 135 patients. Journal of Clinical Oncology. 2016;34(2_suppl):569–569. doi: 10.1200/jco.2016.34.2_suppl.569. [DOI] [Google Scholar]
- 18.Guida A, Albiges L, Loriot Y, Massard C, Fizazi K, Escudier BJ. Everolimus (E) versus axitinib (A) as second-line therapy (2L) in metastatic renal cell carcinoma (mRCC): retrospective experience at Gustave Roussy. Clin Genitourin Cancer. 2017;15(6):e1081–e1088. doi: 10.1016/j.clgc.2017.07.015. [DOI] [PubMed] [Google Scholar]
- 19.Vogl UM, Ponhold L, Locker GL, Zielinski C, Klingler C, Kramer G, Schmidinger M. Safety and efficacy of axitinib in pretreated patients with metastatic renal cell carcinoma: a single center experience of the Medical University of Vienna, Austria. J Clinical Oncol. 2017;31(15_suppl):e15535–e15535. [Google Scholar]
- 20.Signorovitch JE, Kumar Pal S, Reichmann WM, Li N, Liu Z, Perez JR, Vogelzang NJ, Jonasch E. Comparative effectiveness of everolimus (EVE) and axitinib (AXI) for 2nd targeted therapy (TT) of metastatic renal cell carcinoma (mRCC) in the US: A retrospective chart review. J Clin Oncol. 2015; 33:(suppl) (abstract e15612).
- 21.Matias M, Le Teuff G, Albiges L, Guida A, Brard C, Bacciarelo G, Loriot Y, Massard C, Lassau N, Fizazi K, Escudier B. Real world prospective experience of axitinib in metastatic renal cell carcinoma in a large comprehensive cancer centre. Eur J Cancer. 2017;79:185–192. doi: 10.1016/j.ejca.2017.04.015. [DOI] [PubMed] [Google Scholar]
- 22.Hutson TE, Jiao X, Wilson T, Cisar L, MacLean EA. Axitinib in metastatic renal cell carcinoma: patient characteristics and treatment patterns in US community oncology centers. Future Oncol. 2017;13(15):1323–1332. doi: 10.2217/fon-2016-0566. [DOI] [PubMed] [Google Scholar]
- 23.Miyake H, Harada KI, Ozono S, Fujisawa M. Assessment of efficacy, safety, and quality of life of 124 patients treated with axitinib as second-line therapy for metastatic renal-cell carcinoma: experience in real-world clinical practice in Japan. Clin Genitourin Cancer. 2017;15(1):122–128. doi: 10.1016/j.clgc.2016.06.019. [DOI] [PubMed] [Google Scholar]
- 24.D’Aniello C, Vitale MG, Farnesi A, Calvetti L, Laterza MM, Cavaliere C, Della Pepa C, Conteduca V, Crispo A, De Vita F, Grillone F, Ricevuto E, De Tursi M, De Vivo R, Di Napoli M, Cecere SC, Iovane G, Amore A, Piscitelli R, Quarto G, Pisconti S, Ciliberto G, Maiolino P, Muto P, Perdonà S, Berretta M, Naglieri E, Galli L, Cartenì G, De Giorgi U, Pignata S, Facchini G, Rossetti S. Axitinib after sunitinib in metastatic renal cancer: preliminary results from Italian “Real-World” SAX study. Front Pharmacol. 2016;7:331. doi: 10.3389/fphar.2016.00331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1) Eur J Cancer. 2009;45(2):228–247. doi: 10.1016/j.ejca.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 26.Jain RK, Gandhi S, George S. Second-line systemic therapy in metastatic renal-cell carcinoma: a review. Urol Oncol. 2017;35(11):640–646. doi: 10.1016/j.urolonc.2017.08.010. [DOI] [PubMed] [Google Scholar]
- 27.Zarrabi K, Fang C, Wu S. New treatment options for metastatic renal cell carcinoma with prior anti-angiogenesis therapy. J Hematol Oncol. 2017;10(1):38. doi: 10.1186/s13045-016-0374-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Surveillance Epidemiology and End Results Program. Cancer stat facts: kidney and renal pelvis cancer. 2017. https://seer.cancer.gov/statfacts/html/kidrp.html. Accessed 31 Oct 2016.
- 29.Extermann M. Basic assessment of the older cancer patient. Curr Treat Options Oncol. 2011;12(3):276–285. doi: 10.1007/s11864-011-0161-5. [DOI] [PubMed] [Google Scholar]
- 30.Vogelzang NJ, Pal SK, Ghate SR, Swallow E, Li N, Peeples M, Zichlin ML, Meiselbach MK, Perez JR, Agarwal N. Clinical and economic outcomes in elderly advanced renal cell carcinoma patients starting pazopanib or sunitinib treatment: a retrospective medicare claims analysis. Adv Ther. 2017 doi: 10.1007/s12325-017-0628-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khambati HK, Choueiri TK, Kollmannsberger CK, North S, Bjarnason GA, Vaishampayan UN, Wood L, Knox JJ, Tan MH, MacKenzie MJ, Donskov F, Rini BI, Heng DY, International mRCC Database Consortium Efficacy of targeted therapy for metastatic renal cell carcinoma in the elderly patient population. Clin Genitourin Cancer. 2014;12(5):354–358. doi: 10.1016/j.clgc.2014.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miyake H, Harada K, Ozono S, Fujisawa M. Efficacy and safety of axitinib in elderly patients with metastatic renal cell carcinoma. Med Oncol. 2016;33(8):95. doi: 10.1007/s12032-016-0813-1. [DOI] [PubMed] [Google Scholar]
- 33.Hutson TE, Escudier B, Esteban E, Bjarnason GA, Lim HY, Pittman KB, Senico P, Niethammer A, Lu DR, Hariharan S, Motzer RJ. Randomized phase III trial of temsirolimus versus sorafenib as second-line therapy after sunitinib in patients with metastatic renal cell carcinoma. J Clin Oncol. 2014;32(8):760–767. doi: 10.1200/JCO.2013.50.3961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eichelberg C, Vervenne WL, De Santis M, von Weikersthal LF, Goebell PJ, Lerchenmüller C, Zimmermann U, Bos MM, Freier W, Schirrmacher-Memmel S, Staehler M, Pahernik S, Los M, Schenck M, Flörcken A, van Arkel C, Hauswald K, Indorf M, Gottstein D, Michel MS. SWITCH: a randomised, sequential, open-label study to evaluate the efficacy and safety of sorafenib–sunitinib versus sunitinib–sorafenib in the treatment of metastatic renal cell cancer. Eur Urol. 2015;68(5):837–847. doi: 10.1016/j.eururo.2015.04.017. [DOI] [PubMed] [Google Scholar]
- 35.Leung HW, Chan AL, Lin SJ. Indirect comparisons of efficacy and safety between seven newer targeted agents for metastatic renal cell carcinoma: a network meta-analysis of randomised clinical trials. Mol Clin Oncol. 2014;2(5):858–864. doi: 10.3892/mco.2014.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Escudier B, Michaelson MD, Motzer RJ, Hutson TE, Clark JI, Lim HY, Porfiri E, Zalewski P, Kannourakis G, Staehler M, Tarazi J, Rosbrook B, Cisar L, Hariharan S, Kim S, Rini BI. Axitinib versus sorafenib in advanced renal cell carcinoma: subanalyses by prior therapy from a randomised phase III trial. Br J Cancer. 2014;110(12):2821–2828. doi: 10.1038/bjc.2014.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Elaidi R, Harbaoui A, Beuselinck B, Eymard JC, Bamias A, De Guillebon E, Porta C, Vano Y, Linassier C, Debruyne PR, Gross-Goupil M, Ravaud A, Aitelhaj M, Marret G, Oudard S. Outcomes from second-line therapy in long-term responders to first-line tyrosine kinase inhibitor in clear-cell metastatic renal cell carcinoma. Ann Oncol. 2015;26(2):378–385. doi: 10.1093/annonc/mdu552. [DOI] [PubMed] [Google Scholar]
- 38.Grünwald V, McKay RR, Krajewski KM, Kalanovic D, Lin X, Perkins JJ, Simantov R, Choueiri TK. Depth of remission is a prognostic factor for survival in patients with metastatic renal cell carcinoma. Eur Urol. 2015;67(5):952–958. doi: 10.1016/j.eururo.2014.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Qin S, Bi F, Jin J, Cheng Y, Guo J, Ren X, Huang Y, Tarazi J, Tang J, Chen C, Kim S, Ye D. Axitinib versus sorafenib as a second-line therapy in Asian patients with metastatic renal cell carcinoma: results from a randomized registrational study. Onco Targets Ther. 2015;8:1363–1373. doi: 10.2147/ott.s83302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pal SK, Jonasch E, Signorovitch JE, Reichmann WM, Li N, Liu Z, Perez JR, Vogelzang NJ. Real-world dosing and drug costs with everolimus or axitinib as second targeted therapies for advanced renal cell carcinoma: a retrospective chart review in the US. J Med Econ. 2016;19(5):462–468. doi: 10.3111/13696998.2015.1131705. [DOI] [PubMed] [Google Scholar]
- 41.Rini BI, Tomita Y, Melichar B, Ueda T, Grünwald V, Fishman MN, Uemura H, Oya M, Bair AH, Andrews GI, Rosbrook B, Jonasch E. Overall survival analysis from a randomized phase II study of axitinib with or without dose titration in first-line metastatic renal cell carcinoma. Clin Genitourin Cancer. 2016;14(6):499–503. doi: 10.1016/j.clgc.2016.04.005. [DOI] [PubMed] [Google Scholar]
- 42.Rini BI, Quinn DI, Baum M, Wood LS, Tarazi J, Rosbrook B, Arruda LS, Cisar L, Roberts WG, Kim S, Motzer RJ. Hypertension among patients with renal cell carcinoma receiving axitinib or sorafenib: analysis from the randomized phase III AXIS trial. Target Oncol. 2015;10(1):45–53. doi: 10.1007/s11523-014-0307-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Eto M, Uemura H, Tomita Y, Kanayama H, Shinohara N, Kamei Y, Fujii Y, Umeyama Y, Ozono S, Naito S, Akaza H, Japan Axitinib Phase II Study Group Overall survival and final efficacy and safety results from a Japanese phase II study of axitinib in cytokine-refractory metastatic renal cell carcinoma. Cancer Sci. 2014;105(12):1576–1583. doi: 10.1111/cas.12546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee JL, Kim MK, Park I, Ahn JH, Lee DH, Ryoo HM, Song C, Hong B, Hong JH, Ahn H. Randomized phase II trial of sunitinib four weeks on and two weeks off versus two weeks on and one week off in metastatic clear-cell type REnal cell carcinoma: RESTORE trial. Ann Oncol. 2015;26(11):2300–2305. doi: 10.1093/annonc/mdv357. [DOI] [PubMed] [Google Scholar]
- 45.Atkinson BJ, Kalra S, Wang X, Bathala T, Corn P, Tannir NM, Jonasch E. Clinical outcomes for patients with metastatic renal cell carcinoma treated with alternative sunitinib schedules. J Urol. 2014;191(3):611–618. doi: 10.1016/j.juro.2013.08.090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bracarda S, Iacovelli R, Boni L, Rizzo M, Derosa L, Rossi M, Galli L, Procopio G, Sisani M, Longo F, Santoni M, Morelli F, Di Lorenzo G, Altavilla A, Porta C, Camerini A, Escudier B, Rainbow Group Sunitinib administered on 2/1 schedule in patients with metastatic renal cell carcinoma: the RAINBOW analysis. Ann Oncol. 2016;27(2):366. doi: 10.1093/annonc/mdv589. [DOI] [PubMed] [Google Scholar]
- 47.Choueiri TK, Escudier B, Powles T, Mainwaring PN, Rini BI, Donskov F, Hammers H, Hutson TE, Lee JL, Peltola K, Roth BJ, Bjarnason GA, Géczi L, Keam B, Maroto P, Heng DY, Schmidinger M, Kantoff PW, Borgman-Hagey A, Hessel C, Scheffold C, Schwab GM, Tannir NM, Motzer RJ, METEOR Investigators Cabozantinib versus everolimus in advanced renal-cell carcinoma. N Engl J Med. 2015;373(19):1814–1823. doi: 10.1056/nejmoa1510016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Choueiri TK, Escudier B, Powles T, Tannir NM, Mainwaring PN, Rini BI, Hammers HJ, Donskov F, Roth BJ, Peltola K, Lee JL, Heng DYC, Schmidinger M, Agarwal N, Sternberg CN, McDermott DF, Aftab DT, Hessel C, Scheffold C, Schwab G, Hutson TE, Pal S, Motzer RJ, METEOR investigators Cabozantinib versus everolimus in advanced renal cell carcinoma (METEOR): final results from a randomised, open-label, phase 3 trial. Lancet Oncol. 2016;17(7):917–927. doi: 10.1016/s1470-2045(16)30107-3. [DOI] [PubMed] [Google Scholar]
- 49.Escudier B, McDermott DF, George S, Hammers HJ, Srinivas S, Tykodi SS, Sosman JA, Procopio G, Plimack ER, Castellano D, Choueiri TK, Gurney H, Donskov F, Bono P, Wagstaff J, Gauler TC, Ueda T, Tomita Y, Schutz FA, Kollmannsberger C, Larkin J, Ravaud A, Simon JS, Xu LA, Waxman IM, Sharma P, CheckMate 025 Investigators Nivolumab versus everolimus in advanced renal-cell carcinoma. N Engl J Med. 2015;373(19):1803–1813. doi: 10.1056/nejmoa1510665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Escudier B, Sharma P, McDermott DF, George S, Hammers HJ, Srinivas S, Tykodi SS, Sosman JA, Procopio G, Plimack ER, Castellano D, Gurney H, Donskov F, Peltola K, Wagstaff J, Gauler TC, Ueda T, Zhao H, Waxman IM, Motzer RJ, CheckMate 025 investigators CheckMate 025 Randomized Phase 3 Study: Outcomes by key baseline factors and prior therapy for nivolumab versus everolimus in advanced renal cell carcinoma. Eur Urol. 2017 doi: 10.1016/j.eururo.2017.02.010. [DOI] [PubMed] [Google Scholar]
- 51.Amzal B, Fu S, Meng J, Lister J, Karcher H. Cabozantinib versus everolimus, nivolumab, axitinib, sorafenib and best supportive care: a network meta-analysis of progression-free survival and overall survival in second line treatment of advanced renal cell carcinoma. PLoS ONE. 2017;12(9):e0184423. doi: 10.1371/journal.pone.0184423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Porta C, Szczylik C, Casciano R, Fu S, Amzal B, Lister J, Karcher H, Meng J, Neumann M, Dinet J. Second-line cabozantinib versus nivolumab in advanced renal cell carcinoma: systematic review and indirect treatment comparison. Crit Rev Oncol Hematol. 2019;139:143–148. doi: 10.1016/j.critrevonc.2018.10.004. [DOI] [PubMed] [Google Scholar]
- 53.Stukalin I, Wells JC, Graham J, Yuasa T, Beuselinck B, Kollmansberger C, Ernst DS, Agarwal N, Le T, Donskov F, Hansen AR, Bjarnason GA, Srinivas S, Wood LA, Alva AS, Kanesvaran R, Fu SYF, Davis ID, Choueiri TK, Heng DYC. Real-world outcomes of nivolumab and cabozantinib in metastatic renal cell carcinoma: results from the International Metastatic Renal Cell Carcinoma Database Consortium. Curr Oncol. 2019;26(2):e175–e179. doi: 10.3747/co.26.4595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lalani AA, McGregor BA, Albiges L, Choueiri TK, Motzer R, Powles T, Wood C, Bex A. Systemic treatment of metastatic clear cell renal cell carcinoma in 2018: current paradigms, use of immunotherapy, and future directions. Eur Urol. 2019;75(1):100–110. doi: 10.1016/j.eururo.2018.10.010. [DOI] [PubMed] [Google Scholar]
- 55.Bracarda S, Bamias A, Casper J, Negrier S, Sella A, Staehler M, Tarazi J, Felici A, Rosbrook B, Jardinaud-Lopez M, Escudier B. Is Axitinib still a valid option for mRCC in the second-line setting? prognostic factor analyses from the AXIS trial. Clin Genitourin Cancer. 2019;17(3):e689–e703. doi: 10.1016/j.clgc.2019.03.017. [DOI] [PubMed] [Google Scholar]
- 56.Aparicio LMA, Fernandez IP, Cassinello J. Tyrosine kinase inhibitors reprogramming immunity in renal cell carcinoma: rethinking cancer immunotherapy. Clin Transl Oncol. 2017;19(10):1175–1182. doi: 10.1007/s12094-017-1657-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gao X, McDermott DF, Michaelson MD. Enhancing antitumor immunity with antiangiogenic therapy: a clinical model in renal cell carcinoma? Oncologist. 2019;24(6):725–727. doi: 10.1634/theoncologist.2019-0165. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request.