Abstract
OBJECTIVE
To assess the effects of comprehensive lifestyle modification on low-density lipoprotein cholesterol (LDL-C) levels and whether greater participation in counseling sessions was associated with greater LDL-C reductions.
METHODS
Multicenter trial of Pre- or Stage 1 hypertensive adults randomized to: (1)Advice alone, (2)’Established’ lifestyle intervention implementing physical activity, sodium reduction, and weight loss, if overweight, or (3)’Established+DASH’ lifestyle intervention with DASH diet counseling. Both intervention groups received behavioral counseling. We used generalized estimating equations to model the intervention’s effects on lipid outcomes. Analyses of number of sessions and lipids were adjusted for demographics and medical history.
RESULTS
Among 756 participants (mean age 49.7, 63.2% women, 34.7% black), both lifestyle interventions reduced LDL-C, triglycerides, and total cholesterol (TC) at six months. Compared to the ‘Advice’ arm, net mean lipid changes in the Established group were: LDL-C of −5.6mg/dL (p=.001) and TC of −7.3mg/dL (p<.001). Similarly, changes in the ‘Established+DASH’ group were: LDL-C of −4.0mg/dL (p=.03) and TC of −5.7 mg/dL (p=.006). In dose-response analyses, for every 10-session increase, LDL-C changed by −6.2mg/dL (p=.003).
CONCLUSIONS
Comprehensive lifestyle modification lowers LDL-C with greater benefit among persons who attend more counseling sessions.
CLINICAL TRIAL REGISTRATION NUMBER:
Keywords: Cardiovascular Disease, Epidemiology, Lipids, Diet, Randomized Trial, Patient Engagement
1. INTRODUCTION
Over a third of adults in the United States have elevated levels of low-density lipoprotein cholesterol (LDL-C) with fewer than one in three having their lipid levels at goal.1 High cholesterol, particularly LDL-C, has been implicated as a risk factor in a number of cardiovascular diseases, including coronary artery disease,2 stroke,3 and peripheral vascular disease.4 Cardiovascular disease is the leading cause of death in both men and women,5 accounting for twenty five percent of deaths in the United States.6 As such, lowering LDL-C represents an important clinical and public health priority to effectively decrease the morbidity and mortality of cardiovascular disease.
Lifestyle modifications, i.e. adhering to a healthy diet, increasing physical activity, and weight reduction, are a mainstay of therapy in reducing levels of LDL-C.7 Specifically, the Dietary Approaches to Stop Hypertension (DASH) diet8 which is rich in “fruits, vegetables, low-fat dairy”8 and limited in saturated fats and cholesterol products has been shown to lower LDL-C.7 Physical activity recommendations consist of three to four 40-minute sessions of moderate to vigorous intensity.7 Both weight loss and physical activity have been shown to be effective tools in lowering LDL-C.9,10
The PREMIER trial tested the effects of a multi-component lifestyle interventions with and without the DASH diet on blood pressure compared to an, “advice only” control group.11 Both intervention groups had significantly reduced weight and reductions in systolic blood pressure compared to the control group.11 Our analysis seeks to determine: 1) the effects of the PREMIER interventions on lipids levels, 2) whether there is a dose-dependent response on lipid changes based on intervention adherence, and 3) whether there is a dose-dependent response on Atherosclerotic Cardiovascular Disease (ASCVD) 10-year risk based on intervention adherence. We hypothesize that those in the two treatment arms will have significant reductions in LDL-C and that these reductions will be directly related to the amount of intervention sessions attended.
2. METHODS
2.1. Study Design and Participants
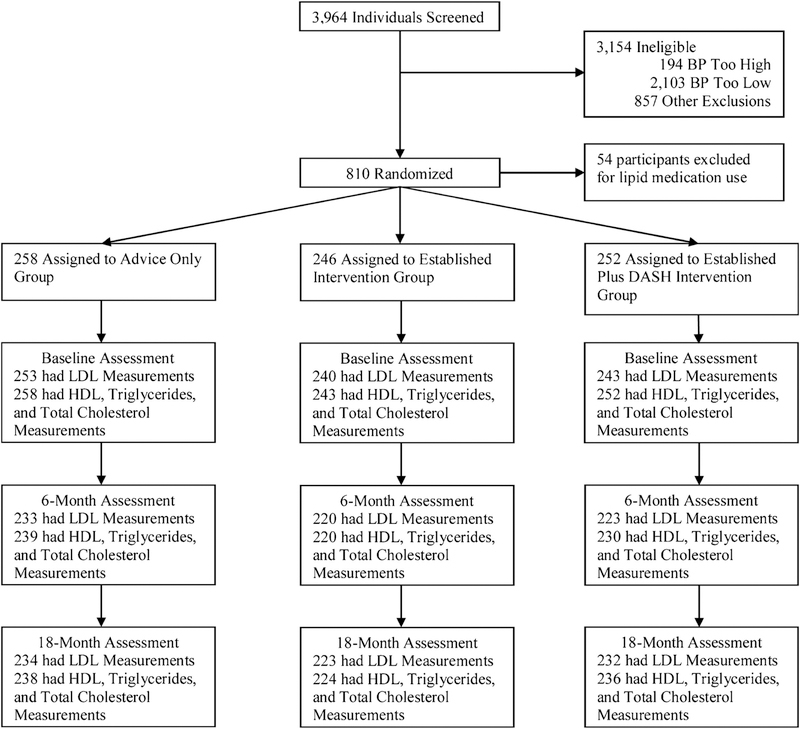
The PREMIER trial study design and methods have been described in detail.11,12 In brief, PREMIER was a multicenter randomized controlled trial enrolling 810 participants at four clinical sites conducted from September 1998 to August 2004.11 Individuals with pre- and Stage 1 hypertension who were not treated with antihypertensive medications were included.11 Individuals with prior cardiovascular history such as angina, peripheral arterial disease, heart failure; renal insufficiency; and glucose intolerance or those taking hypoglycemic agents were excluded.11 Full inclusion and exclusion criteria can be found, elsewhere.12 The study was approved by institutional review boards at all participating centers and all participants provided written informed consent.11 In our analysis conducted in 2016–2017, participants treated with a lipid lowering medication (N = 54) were excluded from the analysis. These participants were evenly distributed among intervention arms.
2.2. Intervention Groups
Participants were randomized to one of three arms: (1) an “Advice Only” control group, (2) an “Established” group, and (3) an “Established Plus DASH” group.12 The participants assigned to the “Advice Only” group were given information regarding dietary sodium reduction, weight loss, increased exercise, and eating a healthful diet at the study’s onset and at six-month follow-up.12 Those in the “Established” group and the “Established Plus DASH” group received a combination of individual and group counseling sessions focused on behavior change that emphasized comprehensive lifestyle changes including increased physical activity, weight reduction, reduced sodium intake, and a reduced fat/calorie diet.12,13 Those in the “Established Plus DASH” also received counseling on the DASH diet.12
2.3. Subgroups Used in Analysis
Subgroups were constructed based on the following cut points: 1) LDL-C≥ 130mg/dL, 2) HDL cholesterol (HDL-C)< 40mg/dL for men and< 50mg/dL for women, 3) Triglycerides≥ 200mg/dL, and 4) Total cholesterol≥ 240mg/dL.
2.4. Lipid Measures
Fasting blood samples were obtained at baseline, 6 and 18 months post randomization.12 Collected samples were processed and sent to a central laboratory for analysis.12 Total cholesterol, HDL-C, and triglycerides were measured directly using standard assays. LDL-C was estimated using the Friedewald equation.14
2.5. Intervention Adherence
Intervention adherence was based on attendance at group and individual sessions. There were a total of 33 possible sessions for those in the “Established” and “Established Plus DASH” groups to attend—26 group sessions and 7 individual sessions.15 In the first six months, these intervention sessions were provided in roughly every one to two weeks.15 There were 18 total meetings during this time consisting of 14 group meetings and 4 individual meetings.15 In the subsequent twelve months, there were 15 additional counseling sessions consisting of 12 group meetings and 3 individual meetings, which occurred roughly monthly.15
2.6. Other Covariates
Age, sex, race, alcoholic intake, household income, education, and current tobacco use were self-reported. Height was measured at baseline, weight and waist circumference were measured at baseline and follow-up visits. Smoking status was assessed at baseline. ASCVD score was calculated at each time point using the necessary continuous variables. Missing data was not imputed for this analysis and smoking status at baseline was carried forward for each time point. Body mass index (BMI) was calculated as weight, in kilograms, divided by height squared, in meters. Weight classifications utilized by the National Heart, Lung, and Blood Institute were utilized: Normal or non-overweight was classified as a BMI less than 25kg/m2, overweight as a BMI of 25 to 29.9kg/m2, obesity Class I as a BMI of 30.0 to 34.9kg/m2, obesity Class II as a BMI of 35.0 to 39.9kg/m2, and obesity Class III as a BMI equal to or greater than 40kg/m2.16
2.7. Outcomes
The primary outcome for this study was between group changes in LDL-C at 6 months. Secondary outcomes were between group blood lipid changes (HDL-C, Triglycerides, and Total Cholesterol) at 6 months and between group lipid changes (LDL-C, HDL-C, Triglycerides, and Total Cholesterol) overall (6 and 18 months). Additionally, we present information regarding change in waist circumference as visceral adiposity is associated with blood lipid changes.
2.8. Statistical Analysis
Baseline characteristics across treatment arms were summarized using mean (SD) for continuous variables and frequency (%) for categorical variables. Continuous variables were compared across treatment arms using Student’s t-test and categorical variables were compared across treatment arms using the Chi square test. In order to account for repeat measurements within participants, generalized estimating equations (GEE) 17 were used to compare measurements at 6 months and 18 months, using a Huber and White robust variance estimator, which assumed an exchangeable working correlation matrix. Changes in lipid measurements were adjusted for baseline lipid values, indicators of the two intervention arms, and indicator variables for site and cohort.
For the intervention adherence analysis, the study population was limited to participants randomized to either of the two lifestyle modification interventions. Given that the analysis was no longer according to randomized groupings, we performed our analysis using three different GEE models—adjusting for known covariates. Model 1 included age, sex, race, baseline weight, alcohol intake, intervention group, baseline lipid values, site, and cohort. Model 2 was the same as Model 1, but also included weight change rather than baseline weight. Lastly, Model 3 had the same covariates as Model 1 with waist circumference change rather than baseline weight. Mediation was assessed using the 4-step model proposed by Baron and Kenny.18 We used a linear cubic spline based on the 18-month regression models to characterize the continuous relationship between number of intervention sessions attended and 18-month changes in weight and lipids.
3. RESULTS
3.1. Study Participants
Appendix Figure 1 displays participant flow over course of the study. Of the 810 randomized patients, 756 were included in analyses; the average age was 49.7 (SD 8.8) years old, 63.2% were female, 34.7% were black, and 94.6% were overweight or obese. The average 10-year Atherosclerotic Cardiovascular Disease (ASCVD) score was 4.6 (SD 4.8). Additional baseline characteristics are shown in Table 1. There were 55.4% of participants who met the dyslipidemia criteria for LDL-C, 47.1% who met the criteria for HDL-C, 18.9% who met the criteria for triglycerides, and 20.0% who met the criteria for total cholesterol.
Table 1.
Baseline Characteristics by Randomized Groupa
| Characteristic | Advice Only (n=258) | Established (n=246) | Established + DASH (n=252) | Overall (n=756) |
|---|---|---|---|---|
| Age, mean (SD) | 49.3 (8.7) | 49.8 (8.3) | 49.9 (9.3) | 49.7 (8.8) |
| Sex | ||||
| Male | 93 (36.1) | 81 (32.9) | 104 (41.3) | 278 (36.8) |
| Female | 165 (64.0) | 165 (67.1) | 148 (58.7) | 478 (63.2) |
| Race | ||||
| Black | 96 (37.2) | 89 (36.2) | 77 (30.6) | 262 (34.7) |
| White | 159 (61.6) | 157 (63.8) | 169 (67.1) | 485 (64.2) |
| All Others | 3 (1.2) | 0 (0) | 6 (2.4) | 9 (1.2) |
| BMI, mean (SD)b | 33.0 (5.6) | 33.0 (5.7) | 33.3 (6.4) | 33.1 (5.9) |
| Weight Classification | ||||
| Non-overweight (BMI <25) | 13 (5.0) | 13 (5.3) | 15 (6.0) | 41 (5.4) |
| Overweight (BMI 25–29.9) | 73 (28.3) | 74 (30.1) | 39 (31.4) | 226 (29.9) |
| Obesity Class I (BMI 30–34.9) | 83 (32.2) | 71 (28.9) | 64 (25.4) | 218 (28.8) |
| Obesity Class II (BMI 35–39.9) | 54 (20.9) | 51 (20.7) | 48 (19.1) | 153 (21.2) |
| Obesity Class III (BMI 40+) | 35 (13.6) | 37 (15.0) | 46 (18.3) | 118 (15.6) |
| Waist Circumference in cm, mean (SD) | 107 (14.8) | 107 (14.4) | 108.8 (16.4) | 107.6 (15.2) |
| Alcoholic Drinks/Week, mean (SD) | 1.5 (2.8) | 1.7 (3.4) | 2.0 (3.7) | 1.7 (3.3) |
| Annual household Income | ||||
| <$30,000 | 30 (11.6) | 26 (10.6) | 26 (10.3) | 82 (10.9) |
| $30,000-$59,999 | 88 (34.1) | 76 (30.9) | 76 (30.2) | 240 (31.7) |
| $60,000-$89,999 | 86 (33.3) | 82 (33.3) | 77 (30.6) | 245 (32.4) |
| $90,000+ | 46 (17.8) | 54 (22.0) | 61 (24.2) | 161 (21.3) |
| No Answer | 8 (3.1) | 8 (3.3) | 12 (4.8) | 28 (3.7) |
| Education | ||||
| High School or less | 18 (7.0) | 18 (7.3) | 31 (12.3) | 67 (8.9) |
| Some College | 171 (66.3) | 148 (60.2) | 137 (54.4) | 456 (60.3) |
| Some Graduate School | 69 (26.7) | 80 (32.5) | 84 (33.3) | 233 (30.8) |
| Current Tobacco Use | 15 (5.8) | 21 (8.5) | 12 (4.8) | 48 (6.4) |
| ASCVD Score, mean (SD) | 4.3 (4.5) | 4.6 (4.6) | 4.9 (5.3) | 4.6 (4.8) |
| Dyslipidemiac | ||||
| LDL Cholesterol | 139 (53.9) | 138 (56.1) | 142 (56.4) | 419 (55.4) |
| HDL Cholesterol | 113 (43.8) | 112 (45.5) | 131 (52.0) | 356 (47.1) |
| Triglyceride | 46 (17.8) | 45 (18.3) | 52 (20.6) | 143 (18.9) |
| Total Cholesterol | 46 (17.8) | 55 (22.4) | 50 (19.8) | 151 (20.0) |
Data are presented as No. (%) unless otherwise indicated
Abbreviations: BMI= Body Mass Index, DASH = Dietary Approaches to Stop Hypertension
Body mass index is calculated by dividing the weight in kilograms by the square of the height in meters
Dyslipidemia defined as:
LDL cholesterol of ≥ 130mg/dL
HDL cholesterol of < 40 mg/dL for men and 50 mg/dL for women Triglyceride of ≥ 200mg/dL
Total cholesterol of ≥ 240mg/dL
For the adherence analysis, 450 of the 498 participants who were randomized to either lifestyle modification group were included as they had complete data for the model variables. Mean age was 50.4 (SD 8.7), 63.1% were women and 31.2% were black.
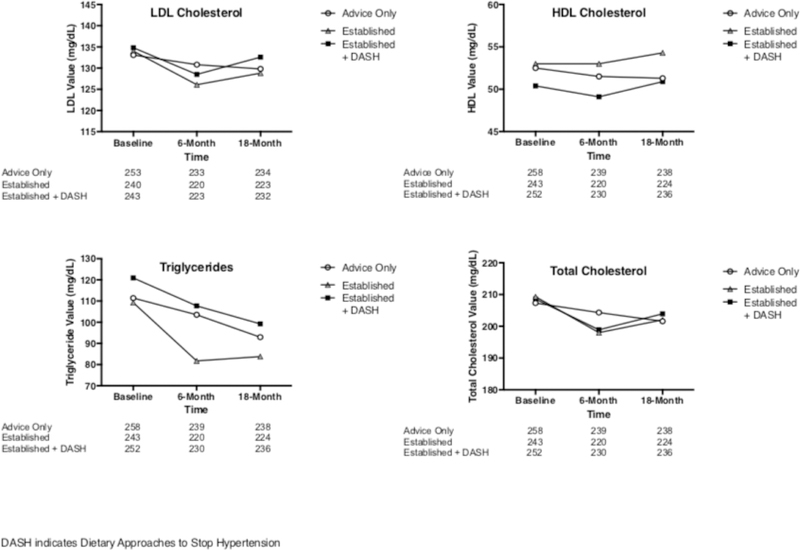
3.2. LDL-C Changes
Lipid values at each time point by randomized group are displayed in Appendix Figure 2 and Appendix Table 1a. From baseline to 6 months, mean change in LDL-C was −2.3mg/dL (95% CI −6.2 to 1.7) in the Advice Only group, −7.9mg/dL (95% CI −11.7 to −4.0) in the Established Group, and −6.3mg/dL (95% CI −10.4 to −2.2) in the Established Plus DASH group. At 6 months, compared to the Advice Only group, the Established group had an LDL-C change of −5.6mg/dL (95% CI −9.0 to −2.2, p=.001) and the Established Plus DASH group had an LDL-C change of −4.0mg/dL (95% CI −7.6 to −0.4, p=.03).
From baseline to 18 months, mean change in LDL-C was −3.3mg/dL (95% CI −7.0 to 0.5) in the Advice Only group, −5.2mg/dL (95% CI −9.2 to −1.2) in the Established Group, and −2.2mg/dL (95% CI −6.2 to 1.9) in the Established Plus DASH group. There were no statistically significant LDL-C differences in pairwise comparisons of randomized groups at 18 months.
Both intervention groups in the subgroup with LDL-C ≥130mg/dL showed statistically significant differences compared to the advice only group at 6 months, but not at 18 months. Among those with a baseline LDL-C <130mg/dL, there was no difference in lipid levels between intervention groups and the advice only group. Full results are shown in Tables 2 and Appendix Table 2.
Table 2.
Pairwise Comparisons by Treatment Group at 6 Monthsa
| Established vs. Advice Only Mean (95% CI) | P-Value | Established + DASH vs. Advice Only Mean (95% CI) | P-Value | Established + DASH vs. Established Mean (95% CI) | P-Value | |
|---|---|---|---|---|---|---|
| LDL Cholesterol (mg/dL) | ||||||
| All | −5.6 (−9.0 to −2.2) | .001 | −4.0 (002D7.6 to −0.4) | .03 | 1.6 (−2.0 to 5.2) | .39 |
| LDL ≥ 130 mg/dL | −8.9 (−14.0 to −3.8) | .001 | −8.4 (−13.6 to −3.3) | .001 | 0.5 (−4.7 to 5.7) | .85 |
| LDL < 130 mg/dL | −2.1 (−6.5 to 2.4) | .37 | 1.7 (−3.0 to 6.4) | .49 | 3.7 (−1.0 to 8.5) | .12 |
| HDL Cholesterol (mg/dL) | ||||||
| All | 1.0 (−0.0 to 2.1) | .06 | −0.3 (−1.3 to 0.8) | .58 | −1.3 (−2.4 to −0.2) | .02 |
| HDL ≥ 40 mg/dL (Male) and 50 mg/dL (Female) | 1.3 (−0.4 to 2.9) | .13 | −0.8 (−2.4 to 0.8) | .34 | −2.1 (−3.9 to −0.3) | .02 |
| HDL < 40 mg/dL (Male) and 50 mg/dL (Female) | 0.7 (−0.6 to 1.9) | .32 | 0.3 (−1.0 to 1.6) | .68 | −0.4 (−1.7 to 0.9) | .57 |
| Triglycerides (mg/dL) | ||||||
| All | −19.7 (−30.6 to −8.8) | <.001 | −5.3 (−18.3 to 7.6) | .42 | 14.4 (2.7 to 26.0) | .02 |
| Triglyceride ≥ 200 mg/dL | −71.0 (−120.4 to −21.7) | .005 | −23.2 (−82.3 to 35.9) | .44 | 47.9 (−0.5 to 96.2) | .05 |
| Triglyceride < 200 mg/dL | −9.2 (−17.2 to −1.2) | .02 | −2.7 (−10.7 to 5.3) | .51 | 6.5 (−1.4 to 14.5) | .11 |
| Total Cholesterol (mg/dL) | ||||||
| All | −7.3 (−11.1 to −3.5) | <.001 | −5.7 (−9.7 to −1.7) | .006 | 1.6 (−2.6 to 5.8) | .45 |
| Total Cholesterol ≥ 240 mg/dL | −17.5 (−27.9 to −7.0) | .001 | −19.1 (−30.6 to −7.6) | .001 | −1.7 (−13.1 to 9.7) | .77 |
| Total Cholesterol < 240 mg/dL | −5.0 (−9.1 to −0.9) | .02 | −2.4 (−6.4 to 1.7) | .26 | 2.6 (−1.6 to 6.9) | .23 |
Data are presented as mean difference (95% Confidence Interval) unless otherwise indicated
3.3. Adherence
Of the 18 visits that occurred during the initial 6 months, those in the Established group attended an average of 14.2 visits (SD 3.5) and those in the Established Plus DASH group attended an average of 14.6 visits (SD 3.8). Of the 15 possible intervention visits during months 6 to 18, those in the established group attended an average of 9.6 sessions (SD 3.9), while those in the Established Plus DASH group attended an average of 10.1 sessions (SD 3.8). There was no difference in the attendance between either intervention groups.
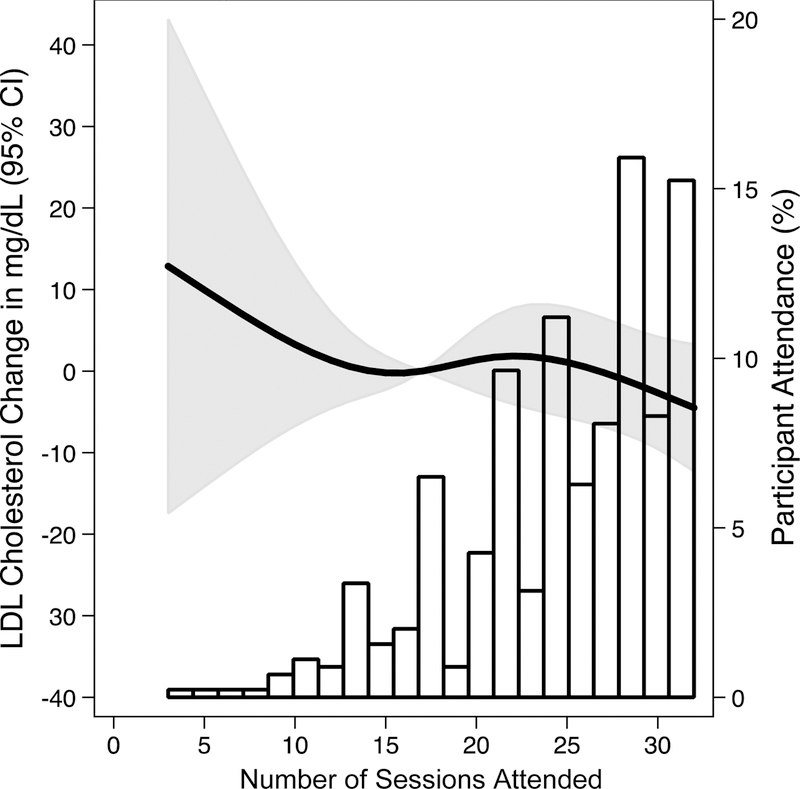
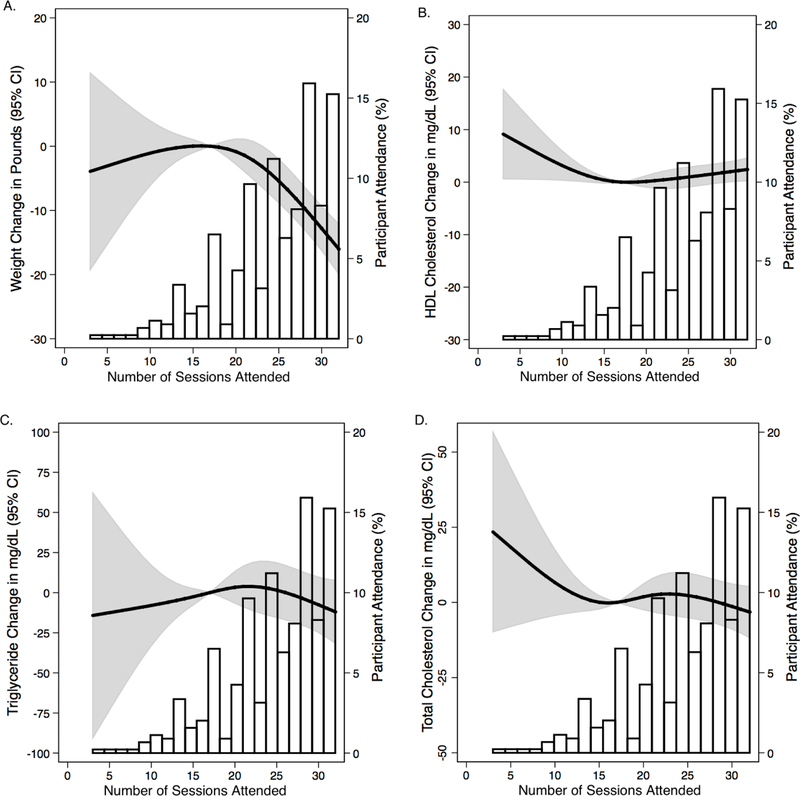
After adjusting for the pre-specified covariates in Model 1, every 10 intervention sessions attended were associated with a lower LDL-C of 6.2mg/dL (95% CI −10.4 to −2.1, P = .003), a lower triglycerides of 19.1mg/dL (95% CI −33.5 to −4.7, P = .009), a lower total cholesterol of 8.6mg/dL (95% CI −13.2 to −4.1, P < .001), and a waist circumference reduction of 0.2cm (95% CI −0.3 to −0.1, p<.001). There was no significant association of sessions with HDL-C (p=0.95) (Table 3). When adjusted for change in weight rather than baseline weight (Model 2), there was no significant association between attendance and any of the lipid values, and the mean reduction in waist circumference was attenuated to 0.1cm (95% CI −0.2 to 0.0, p=.06). When adjusted for change in waist circumference rather than baseline weight, every 10 intervention sessions attended was associated with significant LDL-C reductions of 5.2mg/dL (95% CI −9.5 to −0.9, p=.02) and total cholesterol reductions of 7mg/dL (95% CI −11.7 to −2.4, p=.003). Waist circumference appears to partially mediate the relationship of intervention session with LDL-C and total cholesterol; waist circumference appears to fully mediate the relationship between intervention sessions and triglycerides (Appendix Table 3).
Table 3.
Lipid Value Change Per 10 Intervention Sessions Attendeda
| Model 1b | P-Value | Model 2c | P-Value | Model 3d | P-Value | |
|---|---|---|---|---|---|---|
| LDL Cholesterol (mg/dL) | ||||||
| All | −6.2 (−10.4 to −2.1) | .003 | −3.5 (−7.8 to 0.8) | .11 | −5.2 (−9.5 to −0.9) | .02 |
| LDL ≥ 130 mg/dL | −5.9 (−12.0 to 0.2) | .06 | −4.1 (−10.2 to 2.0) | .18 | −5.2 (−11.4 to 1) | .1 |
| LDL < 130 mg/dL | −7.5 (−13.2 to −1.8) | .01 | −3.4 (−9.4 to 2.6) | .27 | −6.2 (−12.1 to −0.3) | .04 |
| HDL Cholesterol (mg/dL) | ||||||
| All | 0.04 (−1.3 to 1.4) | .95 | −0.4 (−1.8 to 1.0) | .56 | −0.1 (−1.5 to 1.3) | .87 |
| HDL ≥ 40 mg/dL (Male) and 50 mg/dL (Female) | −0.05 (−2.5 to 2.4) | .97 | −0.3 (−2.6 to 2.1) | .83 | 0.08 (−2.3 to 2.5) | .95 |
| HDL < 40 mg/dL (Male) and 50 mg/dL (Female) | 0.08 (−1.4 to 1.5) | .91 | −0.5 (−2.0 to 1.0) | .53 | −0.2 (−1.6 to 1.3) | .83 |
| Triglycerides (mg/dL) | ||||||
| All | −19.1 (−33.5 to −4.7) | .009 | −9.5 (−23.1 to 4.1) | .17 | −12.7 (−25.8 to 0.4) | .06 |
| Triglyceride ≥ 200 mg/dL | −72.3 (−122.9 to −21.7) | .006 | −36.1 (−90.5 to 18.3) | .19 | −28.1 (−76.5 to 20.4) | .25 |
| Triglyceride < 200 mg/dL | −2.9 (−10.7 to 4.9) | .47 | 3.1 (−4.5 to 10.7) | .43 | −1.8 (−9.3 to 5.8) | .65 |
| Total Cholesterol (mg/dL) | ||||||
| All | −8.6 (−13.2 to −4.1) | <.001 | −4.3 (−8.9 to 0.3) | .07 | −7.0 (−11.7 to −2.4) | .003 |
| Total Cholesterol ≥ 240 mg/dL | −10.4 (−22.3 to 1.5) | .09 | −0.3 (−11.4 to 10.8) | .96 | −7.7 (−20.3 to 4.8) | .22 |
| Total Cholesterol < 240 mg/dL | −8.5 (−13.3 to −3.7) | .001 | −4.9 (−9.5 to −0.4) | .03 | −7.1 (−11.6 to −2.7) | .002 |
Data are presented as mean different (95% Confidence Interval), unless otherwise indicated
Adjusted for Baseline Weight, Age, Sex, Race, Alcohol Intake, Intervention Group, Baseline Lipid Value, Site, Cohort, Visit
Adjusted for Weight Change, Age, Sex, Race, Alcohol Intake, Intervention Group, Baseline Lipid Value, Site, Cohort, Visit
Adjusted for Waist Circumference Change, Age, Sex, Race, Alcohol Intake, Intervention Group, Baseline Lipid Value, Site, Cohort, Visit
Last, LDL-C change as a function of intervention sessions attended is shown in Appendix Figure 3. A higher number of sessions was not associated with change in LDL-C. Ultimately a higher number of sessions attended was not associated with HDL-C, triglycerides or total cholesterol, although a higher number of sessions attended was associated with greater reduction in weight (Appendix Figure 4A–D).
For each intervention session attended, there was a reduction of 0.9% (95% CI −1.5 to −0.2, p=<.001) in 10-year ASCVD score per 10 intervention sessions attended when adjusting for the characteristics specified in Model 1 (including baseline weight). When adjusted for weight change, rather than baseline weight (Model 2), the magnitude of this change was reduced to 0.6% (95% CI −1.2 to 0.07, p=0.08). When adjusting for baseline waist circumference (Model 3), a marker of visceral adiposity, the reduction in ASCVD score per 10 intervention sessions attended is 1% (95% CI −1.6 to −.3, p=0.001) (Appendix Table 4).
3.4. Other Lipid Changes and Waist Circumference Change
Analyses were repeated for HDL-C, triglycerides, total cholesterol (Table 2, Appendix Table 1a, Appendix Table 2), and waist circumference (Table 4, Appendix Table 1b). At 6 months, the Established group had a significant change in triglycerides of −19.7mg/dL (95% CI −30.6 to −8.8, p<.001), a significant change in total cholesterol of −7.3mg/dL (95% CI −11.1 to −3.5, p<.001), and a significant reduction in waist circumference of 3.6cm (95%CI −4.7 to −2.5, p<.001) compared to the Advice Only group. For the Established Plus DASH group, there was a significant change in total cholesterol of −5.7mg/dL (95% CI −9.7 to −1.7, p=.006) and in waist circumference of −3.2cm (95%CI −4.3 to −2.2, p<.001) compared to the Advice Only group. At 18 months, HDL-C had remained significantly changed between the Established group and the Advice Only group with a change of 1.5mg/dL (95% CI 0.3 to 2.8, p=0.01), as did the reduction in waist circumference for each intervention group compared to the Advice Only group (Table 4).
Table 4.
Pairwise Comparisons of Waist Circumference by Treatment Group at 6 Months
| 6-Month Comparison Mean (95% CI) | P-Value | 18-Month Comparison Mean (95% CI) | P-Value | |
|---|---|---|---|---|
| Waist Circumference | ||||
| Established vs. Advice Only | −3.6 (−4.7 to −2.5) | <.001 | −2.2 (−3.5 to −0.9) | .001 |
| Established + DASH vs. Advice Only | −3.2 (−4.3 to −2.2) | <.001 | −2.2 (−3.4 to −0.9) | .001 |
| Established + DASH vs. Established | 0.4 (−0.7 to 1.5) | .52 | 0.04 (−1.2 to 1.3) | .95 |
4. DISCUSSION and CONCLUSION
4.1. Discussion
In this trial of individuals with pre- or Stage 1 hypertension, we documented that comprehensive lifestyle modification effectively reduces LDL-C, triglyceride levels, and total cholesterol levels compared to the “Advice Only” group at the primary end point of 6 months. Between the two intervention groups, the “Established Plus DASH” group had significantly lower HDL-C and significantly higher triglyceride levels than the “Established” group. We also found reductions in waist circumference between the two intervention groups and the “Advice Only” group at 6 months, which persisted at 18 months.
Although stepwise reductions were seen in blood pressure between the “Advice Only” group, the “Established” group, and the “Established Plus DASH” group, previously,11 we did not find similar results for lipid changes. In fact, the “Established” group had larger changes than the “Established Plus DASH” group with HDL and triglyceride values being significantly different. As was described in a prior analysis of the PREMIER trial, this may have occurred because those in the DASH arm may have received an “inadequate dose”11 compared to the original DASH trial, a feeding study.19
A dose dependent association was observed for LDL-C, triglyceride levels, and total cholesterol per each intervention session attended. This dose dependent relationship was no longer significant when weight change was included in the model (Model 2) instead of baseline weight (Model 1). It does appear some of this relationship is mediated through waist circumference as Model 3 demonstrates slightly smaller effect size of intervention sessions attended on lipid levels, with significant changes still persisting for LDL-C and total cholesterol. Using the Baron and Kenny assessment for mediation, our finding suggests that waist circumference partially mediates the association between intervention attendance and LDL-C, as well as total cholesterol. The relationship between intervention sessions and triglycerides appears to be fully mediated by waist circumference.
The combined lipid changes, coupled with significant blood pressure changes, reduced Framingham cardiovascular risk, as reported by Maruthur, et al.13 Our study sought to see if this previously noted reduction decreased in a dose-dependent fashion. Given the introduction of the ASCVD risk score in recent years, we used this risk score. We demonstrated a decrease in 10-year ASCVD score per intervention session attended (Model 1), which was partially mediated by change in weight (Model 2).
Multiple studies have shown that individual aspects of a comprehensive lifestyle intervention, such as increased physical activity and weight reduction are associated with favorable lipid changes in a dose dependent manner.20–22 Few studies have demonstrated benefits of comprehensive lifestyle interventions on blood lipid levels. Recently, Dehghani et al. demonstrated the effects of comprehensive lifestyle interventions on a number of cardiovascular risk factors, including decreasing the prevalence of dyslipidemia, which others have previously noted, as well.23,24 Gómez-Pardo et al. also recently showed that comprehensive lifestyle interventions can positively affect cardiovascular risk factors, though they were unable to demonstrate a significant dose-response relationship.25 While prior studies have demonstrated a relationship between comprehensive lifestyle changes and blood lipid levels, our study further demonstrates a potential dose response with more sessions being associated with greater reductions in LDL cholesterol. To our knowledge, our study is the first to demonstrate this significant dose-response relationship with LDL cholesterol. In contrast, there appears to be a dose response relationship of aerobic exercise intensity with HDL-c, with an apparent threshold effect at high levels of aerobic exercise.26
One limitation of our study is that the original inclusion criteria selected participants based on blood pressure cutoffs, not lipid values. Our study generally demonstrated greater benefits in patients in the dyslipidemia subgroups, which suggests that future studies may benefit from this specific inclusion criteria. Additionally, our adherence analysis is observational, as subjects were not analyzed by randomized group, and thus could be subject to residual confounding.
Strengths of this study include its randomized design and diverse population, which included a wide range of educational and income levels. Additionally, this study had very high rates of follow-up. Although adherence to the intervention was high, there was sufficient variation to detect a dose response relationship.
This study provides evidence that comprehensive lifestyle changes may be effective for a large, diverse group of patients, ultimately leading to favorable changes in blood lipid levels. These combined changes may lead to significant reductions in cardiovascular mortality, as those with higher LDL cholesterol and triglycerides have been reported to have higher rates of cardiovascular mortality.27–29 However, our findings underscore the importance of dose, which may explain some of the conflicting reports regarding lifestyle interventions and LDL-C.
30 Given the high prevalence of dyslipidemia in the United States31, engaged participation in comprehensive lifestyle counseling represents an important preventive strategy at both population and individual levels.
Lastly, this study suggests that although the interventions themselves may be effective, patient engagement is critical in the success of comprehensive lifestyle changes as evidenced by the dose dependent response. The POWER study is one such example where investigators were able to efficiently increase the frequency of contact with patients through coaching, web-based modules, and both in person individual and group sessions.32 Additional studies that test innovative and efficient approaches to enhance frequency of lifestyle counseling, e.g. use of clinic staff and contemporary technology, are warranted.
4.2. Conclusion
In summary, the overall findings from the PREMIER trial show that simultaneous implementation of lifestyle interventions may be an effective strategy for reducing LDL-C, triglycerides, and total cholesterol in adults at risk of cardiovascular disease. Research on efficient strategies to increase frequency of counseling, potentially though clinic staff and contemporary technology, should be conducted.
4.3. Practice Implications
Hyperlipidemia, and in particular, LDL-C, is associated with atherosclerosis and cardiovascular disease. Comprehensive lifestyle changes implemented by a diverse clinical staff, including nutritionists and health educators, can improve upon the traditional model of counseling by incorporating a combination of multilevel providers in individual and group counseling sessions. These interventions are associated with greater reductions in LDL-C with greater participation, which highlights the importance of patient engagement in effective lifestyle interventions for that reduce LDL-C and ASCVD risk.
Highlights.
Compared to control, comprehensive lifestyle changes significantly reduced LDL-C
These changes diminished from 6 months to 18 months
Higher intervention session attendance was associated with larger reductions in LDL-C
Patient engagement is an important aspect of effective lifestyle interventions
PRACTICE IMPLICATIONS.
Patient engagement is a critical aspect of effective lifestyle interventions.
ACKNOWLEDGMENTS
The authors would like to thank Professor John McGready of the Department of Biostatistics at the Bloomberg School of Public Health at Johns Hopkins University for his help with statistical analysis.
FINANCIAL SUPPORT
The original trial was funded through NIH Grants: UO1 HL60570, UO1 HL60571, UO1 HL60573, UO1 HL60574, UO1 HL62828, and MO1 RR00052. No additional funding was utilized for secondary analysis. SPJ is supported by NIH/NHLBI Grant 7K23 HL135273–02.
Financial Support and Conflict of Interest: SPJ is supported by NIH/NHLBI Grant 7K23 HL135273–02. LA reports a relationship with Healthways, Inc.
ABBREVIATIONS
- ASCVD
Atherosclerotic Cardiovascular Disease
- BMI
Body Mass Index (units of kg/m2)
- CI
Confidence Interval
- DASH
Dietary Approaches to Stop Hypertension
- LDL-C
Low-density lipoprotein cholesterol
- HDL-C
High-density lipoprotein cholesterol
- NIH
National Institutes of Health
- SD
Standard Deviation
- SE
Standard Error
Appendix
FIGURE 1.
Participant Flow in the Clinical Trial
Figure 2.
Mean Lipid values At Baseline and follow Up by Randomized Group
Figure 3.
LDL-C Change as a Function of Total Sessions Attended
Figure 4A-D.
Lipid Variables as a Function of Total Sessions Attendance
Appendix Table 1(A).
Lipid Values and Within Group Changes by Randomized Group and Timepointa
| Baseline | Absolute Lipid Values | Within Group Change | |||
|---|---|---|---|---|---|
| 6 Months | 8 Months | 6 Months Change | 18 Months Change | ||
| LDL Cholesterol (mg/dL) | |||||
| Advice Only | 133.1 (3.5) | 130.8 | 129.8 | −2.3 (2.0) | −3.3 (1.9) |
| Established | 134.0 (3.3) | 126.1 | 128.8 | −7.9 (2.0) | −5.2 (2.0) |
| Established + DASH | 134.8 (3.4) | 128.5 | 132.6 | −6.3 (2.1) | −2.2 (2.1) |
| HDL Cholesterol (mg/dL) | |||||
| Advice Only | 52.5 (1.5) | 51.5 | 51.3 | −1.0 (0.6) | −0.2 (0.7) |
| Established | 53.0 (1.5) | 53.0 | 54.3 | −0.02 (0.6) | 1.3 (0.7) |
| Established + DASH | 50.4 (1.4) | 49.1 | 50.9 | −1.3 (0.6) | 0.5 (0.6) |
| Triglycerides (mg/dL) | |||||
| Advice Only | 111.4 (9.2) | 103.5 | 92.9 | −7.9 (6.5) | −18.5 (5.8) |
| Established | 109.3 (8.5) | 81.7 | 83.8 | −27.6 (5.6) | −25.5 (5.0) |
| Established + DASH | 120.9 (8.2) | 107.7 | 99.2 | −13.2 (6.2) | −21.7 (5.5) |
| Total Cholesterol (mg/dL) | |||||
| Advice Only | 207.3 (3.6) | 204.3 | 201.6 | −4.0 (2.1) | −5.7 (2.0) |
| Established | 209.3 (3.7) | 198.0 | 202.0 | −11.3 (2.2) | −7.3 (2.2) |
| Established + DASH | 208.6 (3.6) | 198.9 | 203.9 | −9.7 (2.3) | −4.7 (2.2) |
Data are presented as mean difference (SE) unless otherwise indicated
Appendix Table 1(B).
Waist Circumference and Within Group Changes by Randomized Group and Timepointa
| Absolute Waist Circumference Values | Within Group Change | ||||
|---|---|---|---|---|---|
| Baseline | 6 Months | 18 Months | 6 Month Change | 18 Month Change | |
| Waist Circumference (cm) | |||||
| Advice Only | 104.8 (1.5) | 103.9 | 103.9 | −0.9 (0.6) | −0.9 (0.6) |
| Established | 104.6 (1.5) | 100.1 | 101.6 | −4.5 (0.6) | −3.0 (0.6) |
| Established + DASH | 106.4 (1.6) | 102.3 | 103.4 | −4.1 (0.6) | −3.0 (0.6) |
Data are presented as mean difference (SE) unless otherwise indicated
Appendix Table 2.
Pairwise Comparisons by Treatment Group at 18 Monthsa
| Established vs. Advice Only Mean (95% CI) | P-Value | Established + DASH vs. Advice Only Mean (95% CI) | P-Value | Established + DASH vs. Established Mean (95% CI) | P-Value | |
|---|---|---|---|---|---|---|
| LDL Cholesterol (mg/dL) | ||||||
| All | −2.0 (−5.3 to 1.4) | .25 | 1.1 (−2.4 to 4.6) | .54 | 3.1 (−0.7 to 6.8) | .11 |
| LDL ≥ 130 mg/dL | −5.0 (−10.1 to 0.0) | .05 | −0.7 (−5.6 to 4.2) | .79 | 4.4 (−1.2 to 9.9) | .12 |
| LDL < 130 mg/dL | 1.3 (−3.1 to 5.6) | .56 | 3.4 (−1.6 to 8.4) | .18 | 2.1 (−3.0 to 7.2) | .42 |
| HDL Cholesterol (mg/dL) | ||||||
| All | 1.5 (0.3 to 2.8) | .01 | 0.7 (−0.4 to 1.8) | .19 | −0.8 (−2.1 to 0.4) | .19 |
| HDL ≥ 40 mg/dL (Male) and 50 mg/dL (Female) | 1.4 (−0.5 to 3.3) | .16 | −0.2 (−1.9 to 1.5) | .84 | −1.5 (−3.5 to 0.5) | .13 |
| HDL < 40 mg/dL (Male) and 50 mg/dL (Female) | 1.7 (0.2 to 3.2) | .02 | 1.8 (0.3 to 3.2) | .01 | 0.03 (−1.4 to 1.5) | .97 |
| Triglycerides (mg/dL) | ||||||
| All | −7.0 (−15.9 to 1.9) | .12 | −3.2 (−13.5 to 7.0) | .53 | 3.8 (−5.7 to 13.3) | .44 |
| Triglyceride ≥ 200 mg/dL | −17.7 (−58.7 to 23.2) | .39 | −16.0 (−61.4 to 29.5) | .49 | 1.8 (−36.0 to 39.6) | .93 |
| Triglyceride < 200 mg/dL | −5.7 (−12.3 to 1.0) | .09 | −0.7 (−8.0 to 6.6) | .85 | 5.0 (−2.5 to 12.6) | .19 |
| Total Cholesterol (mg/dL) | ||||||
| All | −1.5 (−5.3 to 2.2) | .42 | 1.9 (−2.9 to 4.9) | .62 | 2.5 (−1.6 to 6.7) | .23 |
| Total Cholesterol ≥ 240 mg/dL | −3.1 (−13.6 to 7.5) | .57 | −0.8 (−12.2 to 10.7) | .90 | 2.3 (−9.1 to 13.7) | .69 |
| Total Cholesterol < 240 mg/dL | −1.1 (−5.1 to 2.9) | .58 | 1.5 (−2.6 to 5.5) | .47 | 2.6 (−1.8 to 7.0) | .24 |
Data are presented as mean difference (95% Confidence Interval) unless otherwise indicated
Appendix Table 3.
Baron and Kenny Mediation Analysisa
| LDL-C | HDL-C | Triglycerides | Total Cholesterol | |
|---|---|---|---|---|
| Step 1: Intervention Sessions (IS) & lipids | −0.68 (−0.98 to −0.37), p<.001 | −0.09 (−0.19 to 0.01), p=.09 | −1.3 (−2.3 to −0.4), p=.004 | −0.92 (−1.3 to −0.57), p<.001 |
| Step 2: IS & waist circumference (WC) | −0.40 (−050 to −0.30), p<.001 | N/A (as no relationship, above) | −0.40 (−050 to −0.30), p<.001 | −0.40 (−050 to −0.30), p<.001 |
| Step 3: WC & lipids | 0.46 (0.31 to 0.61), | N/A | 2.0 (1.5 to 2.4), p<.001 | 0.71 (0.55 to 0.88), |
| p<.001 | p<.001 | |||
| Step 4: Model with both IS and WC | ||||
| Intervention Sessions | −0.62 (−1.1 to −0.16), p=0.009 | N/A | −0.32 (−1.2 to 0.62), p=.505 | −0.70 (−1.1 to −0.34), p<.001 |
| Waist Circumference | 0.56 (0.24 to 0.89), p=.001 | N/A | 2.3 (1.7 to 2.9), p<.001 | 0.64 (0.41 to 0.88), p<.001 |
Data are presented as β-coefficient (95% Confidence Interval), p-value unless otherwise indicated
Appendix Table 4.
ASCVD Score and Waist Circumference Change Per 10 Intervention Sessions Attendeda
| ASCVD Change Mean (95% CI) | P-Value | Waist Circumference Change Mean (95% CI) | P-Value | |
|---|---|---|---|---|
| Unadjusted Model | −1 (−2 to −0.01) | <.001 | −0.5 (−0.6 to −0.3) | <.001 |
| Model 1b | −0.9 (−1.5 to −.2) | <.001 | −0.2 (−0.3 to −0.1) | <.001 |
| Model 2c | −0.6 (−1.2 to 0.07) | .08 | −0.1 (−0.2 to 0.0) | .06 |
| Model 3d | −1 (−1.6 to −.3) | .001 | n/a |
Data are presented as mean different (95% Confidence Interval), unless otherwise indicated
Adjusted for Baseline Weight, Age, Sex, Race, Alcohol Intake, Intervention Group, Baseline Lipid Value, Site, Cohort, Visit
Adjusted for Weight Change, Age, Sex, Race, Alcohol Intake, Intervention Group, Baseline Lipid Value, Site, Cohort, Visit
Adjusted for Baseline Waist circumference, Age, Sex, Race, Alcohol Intake, Intervention Group, Baseline Lipid Value, Site, Cohort, Visit
Footnotes
CONFLICTS OF INTEREST
LA reports a relationship with Healthways, Inc.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics−−2015 update: a report from the American Heart Association. Circulation 2015;131:e29–322. [DOI] [PubMed] [Google Scholar]
- 2.Treasure CB, Klein JL, Weintraub WS, et al. Beneficial effects of cholesterol-lowering therapy on the coronary endothelium in patients with coronary artery disease. N Engl J Med 1995;332:481–7. [DOI] [PubMed] [Google Scholar]
- 3.Expert Panel on Detection Evaluation Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). J Amer Med Assoc 2001;285:2486–97. [DOI] [PubMed] [Google Scholar]
- 4.Gornik HL, Beckman JA. Cardiology patient page. Peripheral arterial disease. Circulation 2005;111:e169–72. [DOI] [PubMed] [Google Scholar]
- 5.Death and Mortality Center for Disease Control and Prevention, 2015. (Accessed March 31, 2016, at http://www.cdc.gov/nchs/fastats/deaths.htm.) [Google Scholar]
- 6.Heart Disease Facts Centers for Disease Control and Prevention, 2014. (Accessed March 31, 2016, at http://www.cdc.gov/heartdisease/facts.htm.) [Google Scholar]
- 7.Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63:2960–84. [DOI] [PubMed] [Google Scholar]
- 8.Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 2001;344:3–10. [DOI] [PubMed] [Google Scholar]
- 9.Stefanick ML, Mackey S, Sheehan M, Ellsworth N, Haskell WL, Wood PD. Effects of diet and exercise in men and postmenopausal women with low levels of HDL cholesterol and high levels of LDL cholesterol. N Engl J Med 1998;339:12–20. [DOI] [PubMed] [Google Scholar]
- 10.Blackburn G Effect of degree of weight loss on health benefits. Obes Res 1995;3 Suppl 2:211s–6s. [DOI] [PubMed] [Google Scholar]
- 11.Appel LJ, Champagne CM, Harsha DW, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA 2003;289:2083–93. [DOI] [PubMed] [Google Scholar]
- 12.Svetkey LP, Harsha DW, Vollmer WM, et al. Premier: a clinical trial of comprehensive lifestyle modification for blood pressure control: rationale, design and baseline characteristics. Ann Epidemiol 2003;13:462–71. [DOI] [PubMed] [Google Scholar]
- 13.Maruthur NM, Wang NY, Appel LJ. Lifestyle interventions reduce coronary heart disease risk: results from the PREMIER Trial. Circulation 2009;119:2026–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Warnick GR, Knopp RH, Fitzpatrick V, Branson L. Estimating low-density lipoprotein cholesterol by the Friedewald equation is adequate for classifying patients on the basis of nationally recommended cutpoints. Clin Chem 1990;36:15–9. [PubMed] [Google Scholar]
- 15.Funk KL, Elmer PJ, Stevens VJ, et al. PREMIER--a trial of lifestyle interventions for blood pressure control: intervention design and rationale. Health Promot Pract 2008;9:271–80. [DOI] [PubMed] [Google Scholar]
- 16.Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. National Institutes of Health. Obes Res 1998;6 Suppl 2:51S–209S. [PubMed] [Google Scholar]
- 17.Hanley JA, Negassa A, Edwardes MDd, Forrester JE. Statistical Analysis of Correlated Data Using Generalized Estimating Equations: An Orientation. Am J Epidemiol 2003;157:364–75. [DOI] [PubMed] [Google Scholar]
- 18.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986;51:1173–82. [DOI] [PubMed] [Google Scholar]
- 19.Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med 1997;336:1117–24. [DOI] [PubMed] [Google Scholar]
- 20.LeBlanc AG, Janssen I. Dose-response relationship between physical activity and dyslipidemia in youth. Can J Cardiol 2010;26:201–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aadahl M, Kjaer M, Jorgensen T. Associations between overall physical activity level and cardiovascular risk factors in an adult population. Eur J Epidemiol 2007;22:369–78. [DOI] [PubMed] [Google Scholar]
- 22.Griffin BA. Nonpharmacological approaches for reducing serum low-density lipoprotein cholesterol. Curr Opin Cardiol 2014;29:360–5. [DOI] [PubMed] [Google Scholar]
- 23.Dehghani A, Kumar Bhasin S, Dwivedi S, Kumar Malhotra R. Influence of Comprehensive Life Style Intervention in Patients of CHD. Glob J Health Sci 2015;7:6–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bijlani RL, Vempati RP, Yadav RK, et al. A brief but comprehensive lifestyle education program based on yoga reduces risk factors for cardiovascular disease and diabetes mellitus. J Altern Complement Med 2005;11:267–74. [DOI] [PubMed] [Google Scholar]
- 25.Gomez-Pardo E, Fernandez-Alvira JM, Vilanova M, et al. A Comprehensive Lifestyle Peer Group-Based Intervention on Cardiovascular Risk Factors: The Randomized Controlled Fifty-Fifty Program. J Am Coll Cardiol 2016;67:476–85. [DOI] [PubMed] [Google Scholar]
- 26.A Review of the Impact of Exercise on Cholesterol Levels (Accessed April 24, 2019, at https://www.unm.edu/~lkravitz/Articlefolder/cholesterolNEW.html.)
- 27.Cholesterol Treatment Trialists C, Baigent C, Blackwell L, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 2010;376:1670–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Heart Protection Study Collaborative G, Bulbulia R, Bowman L, et al. Effects on 11-year mortality and morbidity of lowering LDL cholesterol with simvastatin for about 5 years in 20,536 high-risk individuals: a randomised controlled trial. Lancet 2011;378:2013–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Austin MA, McKnight B, Edwards KL, et al. Cardiovascular disease mortality in familial forms of hypertriglyceridemia: A 20-year prospective study. Circulation 2000;101:2777–82. [DOI] [PubMed] [Google Scholar]
- 30.U. S. Preventive Services Task Force, Grossman DC, Bibbins-Domingo K, et al. Behavioral Counseling to Promote a Healthful Diet and Physical Activity for Cardiovascular Disease Prevention in Adults Without Cardiovascular Risk Factors: US Preventive Services Task Force Recommendation Statement. J Amer Med Assoc 2017;318:167–74. [DOI] [PubMed] [Google Scholar]
- 31.Toth PP, Potter D, Ming EE. Prevalence of lipid abnormalities in the United States: the National Health and Nutrition Examination Survey 2003–2006. J Clin Lipidol 2012;6:325–30. [DOI] [PubMed] [Google Scholar]
- 32.Appel LJ, Clark JM, Yeh HC, et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med 2011;365:1959–68. [DOI] [PMC free article] [PubMed] [Google Scholar]